Professional Documents
Culture Documents
Tinea Incognito
Uploaded by
Aan Sii DiademsCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tinea Incognito
Uploaded by
Aan Sii DiademsCopyright:
Available Formats
Tinea Incognito
1-year-old male child had a past medical history of
mild atopic dermatitis in the first months of life,
successfully treated with intermittent topical steroid
therapy. Because of the reappearance of similar lesions in
the recent period, he was treated with antibiotics and oral
steroids by the general practitioner. Despite such therapy,
skin eruption worsened and expanded, and the patient
was then referred to our institution. Initial evaluation revealed a child in good general condition with sharply
demarcated, scaly erythematous patches on the upper trunk,
shoulders, and back (Figure 1); small pustules were also
evident. Remaining physical examination was negative.
The patient was apyretic. Laboratory tests showed no
alterations of white blood cells count, lymphocyte
subpopulations, erythrocyte sedimentation rate, and Creactive protein. Pustular psoriasis was suspected, and
topical corticosteroid therapy was undertaken. Despite
treatment, skin lesions progressed; a diagnostic skin
biopsy was then performed, revealing dermatophytic
fungal hyphae of Trichophyton mentagrophytes species.
Such findings suggested a primary diagnosis of tinea
incognito (TI), worsened by steroid therapy and
mimicking pustular psoriasis. Oral fluconazole (6 mg/kg/
d) and topical miconazole were then started. After
4 weeks, complete resolution of skin erythema and
pustules was observed on trunk and back (Figure 2;
available at www.jpeds.com).
TI is a dermatophytosis with atypical features because
of the absence of classic appearance of cutaneous tinea
(ringworm), usually caused by prolonged use of steroids.1
Mistreatment of tinea infection with topical corticosteroid
therapy may lead to a variety of skin presentations, including
lichenoid, rosacea-like, eczema-like, and psoriasis-like TI.2
The mechanism by which dermatophytes lead to pustular
lesion development in psoriasis-like TI is poorly understood.
It is known that dermatophytes are able to stimulate
production of interleukin 8 by human keratinocytes3 which,
in turn, induces neutrophil chemotaxis. Local neutrophil
activation may contribute to the development of pustules.4
Two published cases of TI characterized by pustular
inflammatory skin lesions are similar to our patient.5,6 The
presentation of pustular psoriasis-like TI may cause
potential confusion in the initial diagnosis, which includes
juvenile-type pustular psoriasis, subcorneal pustular
dermatosis, and impetigo (Figures 3 and 4; available at
www.jpeds.com). Skin swab and/or skin punch biopsy are
advisable to detect fungal hyphae in all psoriasis-like
clinical pictures unresponsive to steroid therapy; correct
diagnosis of TI allows, in turn, onset of appropriate
antimicotic treatment and skin lesions healing. n
Giulia Paloni, MD
Institute for Maternal and Child Health
IRCCS Burlo Garofolo
Trieste, Italy
Enrico Valerio, MD
Department of Pediatrics Salus Pueri
University of Padova
Padua, Italy
Irene Berti, MD
Institute for Maternal and Child Health
IRCCS Burlo Garofolo
Trieste, Italy
Mario Cutrone, MD
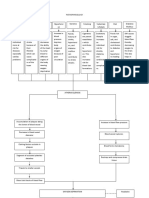
Figure 1. A, Clinical picture at admission: sharply demarcated, scaly erythematous patches on the upper trunk,
B, shoulders, and back.
Pediatric Dermatology Department
Ospedale dellAngelo
Venice, Italy
References available at www.jpeds.com
J Pediatr 2015;-:---.
0022-3476/$ - see front matter. Copyright 2015 Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.jpeds.2015.08.062
THE JOURNAL OF PEDIATRICS
www.jpeds.com
References
1. Romano C, Asta F, Massai L. Tinea incognito due to Microsporum gypseum in three children. Pediatr Dermatol 2000;17:41-4.
2. Gorani A, Schiera A, Oriani A. Case report. Rosacea-like tinea incognito.
Mycoses 2002;45:135-7.
3. Tani K, Adachi M, Nakamura Y, Kano R, Makimura K, Hasegawa A, et al.
The effect of dermatophytes on cytokine production by human
keratinocytes. Arch Dermatol Res 2007;299:381-7.
Vol. -, No. 4. Davies RR, Zaini F. Drugs affecting Trichophyton rubrum-induced
neutrophil chemotaxis in vitro. Clin Exp Dermatol 1988;13:228-31.
5. Kawakami Y, Oyama N, Sakai E, Nishiyama K, Suzutani T, Yamamoto T.
Childhood tinea incognito caused by Trichophyton mentagrophytes var.
interdigitale mimicking pustular psoriasis. Pediatr Dermatol 2011;28:
738-9.
6. Serarslan G. Pustular psoriasis-like tinea incognito due to Trichophyton
rubrum. Mycoses 2007;50:523-4.
Figure 2. A, Resolution of skin erythema and pustules on trunk and B, back after 4 weeks of antimicotic therapy.
1.e1
Paloni et al
- 2015
REDISCOVERING THE PHYSICAL EXAM
Figure 3. Juvenile-type pustular psoriasis.
Figure 4. Diffuse impetigo.
Tinea Incognito
1.e2
You might also like
- Jacquet Erosive DermatitisDocument15 pagesJacquet Erosive DermatitisRitchie StefanusNo ratings yet
- Tinea incognito misdiagnosed as pemphigus foliaceus due to immunosuppressive therapyDocument3 pagesTinea incognito misdiagnosed as pemphigus foliaceus due to immunosuppressive therapyYelvi Novita RozaNo ratings yet
- Fde CedDocument2 pagesFde CedmdpavlovicNo ratings yet
- Tinea Cruris and Tinea Corporis Masquerading As Tinea Indecisiva: Case Report and Review of The LiteratureDocument8 pagesTinea Cruris and Tinea Corporis Masquerading As Tinea Indecisiva: Case Report and Review of The LiteratureKhairunnisa WijayaNo ratings yet
- Therapeutic Hotline: Tinea Profunda of The Genital Area. Successful Treatment of A Rare Skin DiseaseDocument3 pagesTherapeutic Hotline: Tinea Profunda of The Genital Area. Successful Treatment of A Rare Skin Diseasesoekarnohatta94No ratings yet
- Bizkova 2009Document8 pagesBizkova 2009mario256No ratings yet
- Journal Reading 1Document22 pagesJournal Reading 1RetnoSFadhillahNo ratings yet
- Congenital Nevus Skull Defect Risk MelanomaDocument3 pagesCongenital Nevus Skull Defect Risk MelanomaAna Flavia BaptistaNo ratings yet
- Therapy Selection For Tinea Corporis and Cruris With CommorbidityDocument9 pagesTherapy Selection For Tinea Corporis and Cruris With CommorbidityShimie Shimie KokobopNo ratings yet
- Pi Is 0190962214011566Document2 pagesPi Is 0190962214011566LewishoppusNo ratings yet
- Clinical and Laboratory Observations: Guttate Psoriasis Associated With Perianal Streptococcal DiseaseDocument3 pagesClinical and Laboratory Observations: Guttate Psoriasis Associated With Perianal Streptococcal DiseaseTaufiq AgungNo ratings yet
- Thymoma-Associated Exfoliative Dermatitis in A Rabbit (Pages 281-284)Document4 pagesThymoma-Associated Exfoliative Dermatitis in A Rabbit (Pages 281-284)jenNo ratings yet
- An Unusual Case of Transient Neonatal Pustular Melanosis: A Diagnostic PuzzleDocument4 pagesAn Unusual Case of Transient Neonatal Pustular Melanosis: A Diagnostic PuzzlecebadawitNo ratings yet
- Prevalence of Tinea Corporis and Tinea Cruris in Outpatient Department of Dermatology Unit of A Tertiary Care HospitalDocument3 pagesPrevalence of Tinea Corporis and Tinea Cruris in Outpatient Department of Dermatology Unit of A Tertiary Care HospitalRetno WahyudiNo ratings yet
- PDF DocumentDocument4 pagesPDF DocumentAditya Yudha PratamaNo ratings yet
- Lipophagic Panniculitis of Childhood: Chronic Actinic DermatitisDocument8 pagesLipophagic Panniculitis of Childhood: Chronic Actinic DermatitisHellgenius SantomauroNo ratings yet
- Robinson HC CT105003132Document5 pagesRobinson HC CT105003132Francesca BizzocoNo ratings yet
- Childhood Erythrodermic Lichen Planus Pemphigoides After Nonavalent Human Papillomavirus VaccinationDocument3 pagesChildhood Erythrodermic Lichen Planus Pemphigoides After Nonavalent Human Papillomavirus Vaccinationnurul hidayatiNo ratings yet
- Feline Herpes Virus-1 Associated Facial and Perianal Dermatitis in A CatDocument4 pagesFeline Herpes Virus-1 Associated Facial and Perianal Dermatitis in A CatIndah frysay marbunNo ratings yet
- 10.1007@s40257 017 0309 6Document3 pages10.1007@s40257 017 0309 6shf.mxlikNo ratings yet
- A Case of Secondary Syphilis With The Extragenital Chancre On The NippleDocument3 pagesA Case of Secondary Syphilis With The Extragenital Chancre On The NipplePipim BayasariNo ratings yet
- Dermatophyte Case ReportDocument8 pagesDermatophyte Case ReportnikfarisNo ratings yet
- Tinea Pedis and Tinea Unguium in a 7-Year-Old ChildDocument2 pagesTinea Pedis and Tinea Unguium in a 7-Year-Old ChildHendri FauzikNo ratings yet
- Cutaneous Lesions of The Canine ScrotumDocument14 pagesCutaneous Lesions of The Canine ScrotumLuciana Diegues100% (1)
- Pityriasis AlbaDocument6 pagesPityriasis AlbaLee Eng SiangNo ratings yet
- E Tra: Diagnosis and Management of Cutaneous Tinea InfectionsDocument8 pagesE Tra: Diagnosis and Management of Cutaneous Tinea InfectionsFuad hadyanNo ratings yet
- JurnalDocument15 pagesJurnalevimeilisaNo ratings yet
- Tinea Incognito Hidden Under Apparently Treatment-Resistant Pemphigus FoliaceusDocument2 pagesTinea Incognito Hidden Under Apparently Treatment-Resistant Pemphigus FoliaceusdayangNo ratings yet
- Transient Eosinophilic Nodulomatosis A Report of Two CasesDocument6 pagesTransient Eosinophilic Nodulomatosis A Report of Two CasesAthenaeum Scientific PublishersNo ratings yet
- Autoimmune Diseases A Late Complication of Toxic Epidermal Necrolysis A Case ReportDocument4 pagesAutoimmune Diseases A Late Complication of Toxic Epidermal Necrolysis A Case ReportAthenaeum Scientific PublishersNo ratings yet
- Acrodermatitis EnteropathicaDocument4 pagesAcrodermatitis EnteropathicaIntan FajrinNo ratings yet
- Bacterial interweb infection of the feetDocument3 pagesBacterial interweb infection of the feetUmmi RinandariNo ratings yet
- Lichenoid Skin Lesions - A Rare Manifestation in Secondary SyphilisDocument3 pagesLichenoid Skin Lesions - A Rare Manifestation in Secondary SyphilisShintaNo ratings yet
- Atopic Dermatitis: A Review of Diagnosis and TreatmentDocument11 pagesAtopic Dermatitis: A Review of Diagnosis and TreatmentLeona NgadiahNo ratings yet
- UC Davis: Dermatology Online JournalDocument4 pagesUC Davis: Dermatology Online JournalAyu MuskitaNo ratings yet
- Childhood PsioriasisDocument6 pagesChildhood PsioriasisYuliana DaisongNo ratings yet
- Rare Cutaneous Tuberculosis FormsDocument6 pagesRare Cutaneous Tuberculosis FormsinggitsiregarNo ratings yet
- Atopic Dermatitis Seminar GuideDocument7 pagesAtopic Dermatitis Seminar GuidetazzycaNo ratings yet
- TPMD 200176Document2 pagesTPMD 200176Marcelita DuwiriNo ratings yet
- Case Report: Staphylococcal Scalded Skin Syndrome in A NeonateDocument7 pagesCase Report: Staphylococcal Scalded Skin Syndrome in A NeonateKenNo ratings yet
- Acne Urticata and Chronic Myelogenous LeukemiaDocument4 pagesAcne Urticata and Chronic Myelogenous LeukemiaGo McFlyNo ratings yet
- Dangers of CuppingDocument4 pagesDangers of CuppingTejaswiNo ratings yet
- artigo psoríase 1Document2 pagesartigo psoríase 1Eli MoreiraNo ratings yet
- (2017) BELOUSOVA, Irena E. Mycosis Fungoides Manifesting As Giant Cell Lichenoid DermatitisDocument3 pages(2017) BELOUSOVA, Irena E. Mycosis Fungoides Manifesting As Giant Cell Lichenoid DermatitisCassandra VérasNo ratings yet
- The Skin Group 2 Patho Reporting QuestionsDocument9 pagesThe Skin Group 2 Patho Reporting QuestionsBatch ElysianNo ratings yet
- J Clindermatol 2017 10 005Document29 pagesJ Clindermatol 2017 10 005Nada SejatiNo ratings yet
- 17.pityriasis RoseaDocument5 pages17.pityriasis RoseahaidarTRVNo ratings yet
- Lucivero Et Al 2011 Lupus Mastitis in Systemic Lupus Erythematosus A Rare Condition Requiring A Minimally InvasiveDocument5 pagesLucivero Et Al 2011 Lupus Mastitis in Systemic Lupus Erythematosus A Rare Condition Requiring A Minimally Invasiveruthdaniel6041No ratings yet
- Darier-White Disease: A Rare Genetic DisorderDocument4 pagesDarier-White Disease: A Rare Genetic Disorderanis utamiNo ratings yet
- Congenital Ichthyosis in Newborns 2020Document8 pagesCongenital Ichthyosis in Newborns 2020Ismail SultanNo ratings yet
- Lancet Atopic DermatitisDocument10 pagesLancet Atopic DermatitisRui CarmoNo ratings yet
- Guide to Diagnosing and Treating Atopic DermatitisDocument20 pagesGuide to Diagnosing and Treating Atopic DermatitisSilvan SilvaNo ratings yet
- Atypical Manifestations of Tinea Corporis: Case ReportsDocument5 pagesAtypical Manifestations of Tinea Corporis: Case ReportsMuhammad HafizuddinNo ratings yet
- 42thilak EtalDocument3 pages42thilak EtaleditorijmrhsNo ratings yet
- Annular Erythema and Papules in Infantile Atopic Dermatitis: Short CommunicationDocument2 pagesAnnular Erythema and Papules in Infantile Atopic Dermatitis: Short CommunicationsnrarasatiNo ratings yet
- Human Protothecosis Case Report of A Rare Algal InfectionDocument4 pagesHuman Protothecosis Case Report of A Rare Algal InfectionAthenaeum Scientific PublishersNo ratings yet
- Dermatilomania ComplicationDocument3 pagesDermatilomania Complicationkristie.kankenNo ratings yet
- Langerhans Cell Histiocytosis Presented As Persistent Diaper DermatitisDocument6 pagesLangerhans Cell Histiocytosis Presented As Persistent Diaper DermatitisAyuNo ratings yet
- Practical Insights into Atopic DermatitisFrom EverandPractical Insights into Atopic DermatitisKwang Hoon LeeNo ratings yet
- EaglesDocument2 pagesEaglesAan Sii DiademsNo ratings yet
- angsuran pinjaman koperasi maju terus stikes kurnia jayaDocument2 pagesangsuran pinjaman koperasi maju terus stikes kurnia jayaAan Sii DiademsNo ratings yet
- Conjunctivitis Is Inflammation of The Conjunctiva Caused by Either A Virus or A BacteriumDocument4 pagesConjunctivitis Is Inflammation of The Conjunctiva Caused by Either A Virus or A BacteriumAan Sii DiademsNo ratings yet
- Type Your Title Here: Back Panel HeadingDocument2 pagesType Your Title Here: Back Panel HeadingAan Sii DiademsNo ratings yet
- VirtualDJ 7 - Getting Started PDFDocument11 pagesVirtualDJ 7 - Getting Started PDFSanthia MoralesNo ratings yet
- Demi Lovato Heart AttackDocument1 pageDemi Lovato Heart AttackaguslabNo ratings yet
- Fifa World Cup Brazil 2014: Jadwal Piala Dunia Perdelapan FinalDocument3 pagesFifa World Cup Brazil 2014: Jadwal Piala Dunia Perdelapan FinalAan Sii DiademsNo ratings yet
- Informed Consent TimetableDocument11 pagesInformed Consent TimetableAkita C.No ratings yet
- Perbandingan Pengenceran Larutan Giemsa 3% Dan 5% Terhadap Pemeriksaan Morfologi PlasmodiumDocument9 pagesPerbandingan Pengenceran Larutan Giemsa 3% Dan 5% Terhadap Pemeriksaan Morfologi PlasmodiumMuti WahyuNo ratings yet
- Sat-Asatkaryavada in DiseaseDocument7 pagesSat-Asatkaryavada in DiseaseSamhitha Ayurvedic ChennaiNo ratings yet
- ACCIDENT REPORTING AND INVESTIGATION PROCEDUREDocument23 pagesACCIDENT REPORTING AND INVESTIGATION PROCEDUREkirandevi1981No ratings yet
- Activity Intolerance Care Plan For CFDocument8 pagesActivity Intolerance Care Plan For CFapi-314197645No ratings yet
- 9 Hair CleanseDocument11 pages9 Hair CleanseSeetha ChimakurthiNo ratings yet
- Maria Garcia Dolphin Pose (Ardha Pincha Mayurasana) & Plough Pose (Halasana) Spring 2016 M 2:30-4:00Document5 pagesMaria Garcia Dolphin Pose (Ardha Pincha Mayurasana) & Plough Pose (Halasana) Spring 2016 M 2:30-4:00api-301722320No ratings yet
- Comparison of Roth Appliance and Standard Edgewise Appliance Treatment ResultsDocument9 pagesComparison of Roth Appliance and Standard Edgewise Appliance Treatment ResultsseboistttNo ratings yet
- Gastric and Duodenal Disorders - Test 4Document21 pagesGastric and Duodenal Disorders - Test 4Vickie BuckerNo ratings yet
- Cranial Base Dan Emergency CaseDocument34 pagesCranial Base Dan Emergency Caserahmad wahyuNo ratings yet
- Pathophysiology Tia VS CvaDocument6 pagesPathophysiology Tia VS CvaRobby Nur Zam ZamNo ratings yet
- 2021-2022 Sem 2 Lecture 2 Basic Tests in Vision Screenings - Student VersionDocument123 pages2021-2022 Sem 2 Lecture 2 Basic Tests in Vision Screenings - Student Versionpi55aNo ratings yet
- PharmacologyDocument9 pagesPharmacologyAishwarya MenonNo ratings yet
- Oral and Maxillofacial PathologyDocument79 pagesOral and Maxillofacial PathologyMai AnhNo ratings yet
- Pharma Module 1 PDFDocument22 pagesPharma Module 1 PDFSheryhan Tahir BayleNo ratings yet
- Analytical Standardization of Brahmi Nei and Effect of Siddha Methodologies On Spasticity in Cerebral PalsyDocument8 pagesAnalytical Standardization of Brahmi Nei and Effect of Siddha Methodologies On Spasticity in Cerebral PalsytrinitysugumarNo ratings yet
- Barack Huessein Obama Is The Most Dangerous Man To Ever LiveDocument3 pagesBarack Huessein Obama Is The Most Dangerous Man To Ever LivetravisdannNo ratings yet
- Golden NumbersDocument89 pagesGolden NumbersjoobazhieNo ratings yet
- World03 30 16Document40 pagesWorld03 30 16The WorldNo ratings yet
- 3 Radiographic Dental Assessment For The Child Patient PDFDocument21 pages3 Radiographic Dental Assessment For The Child Patient PDFFamodimu Funbi SamuelNo ratings yet
- Breast Assessment Learning ObjectivesDocument6 pagesBreast Assessment Learning Objectivesalphabennydelta4468No ratings yet
- 10 0000@Www Quintpub Com@ejed@18638Document23 pages10 0000@Www Quintpub Com@ejed@18638Víctor Rodríguez67% (3)
- Reproductive Health BillDocument22 pagesReproductive Health BillPhoebe CasipitNo ratings yet
- 1.agglutination ReactionDocument30 pages1.agglutination ReactionEINSTEIN2DNo ratings yet
- Guppy Brain Atlas SmallerDocument4 pagesGuppy Brain Atlas Smallerapi-394354061No ratings yet
- Tfios Mediastudyguide v4Document7 pagesTfios Mediastudyguide v4api-308995770No ratings yet
- Health and its failure: Causes, Types, and Prevention of DiseasesDocument9 pagesHealth and its failure: Causes, Types, and Prevention of DiseasesAbhimanyu BahreeNo ratings yet
- Webster Uretroplastia en 4 Etapas.Document13 pagesWebster Uretroplastia en 4 Etapas.LuisamdNo ratings yet
- And Technical Description: User ManualDocument100 pagesAnd Technical Description: User ManualYouness Ben TibariNo ratings yet
- VMC Customer Service Complaint and Letter of DemandDocument3 pagesVMC Customer Service Complaint and Letter of DemandJames Alan BushNo ratings yet