Professional Documents
Culture Documents
NCP of Cav
Uploaded by
Henry Roque TagalagOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP of Cav
Uploaded by
Henry Roque TagalagCopyright:
Available Formats
saline lock does not prevent you from pushing fluids, but there are some places that
do not hang IV fluids on CVA patients. They start saline locks only! Risk for skin integrity related to physical immobility4 I t i s t h e 4 th because it may causeof bedsore Readiness for enhanced power 5It is the last prioritized diagnoses because the patient wants to gainhis power Ncp1 15
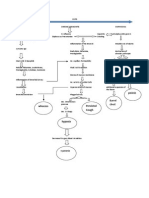
Thrombosis, embolism, and hemorrhage are the primary causes for CVA, with thrombosis being the main cause of both CVAs and transient ischemic attacks (TIAs). The most common vessels involved are the carotid arteries and those of the vertebrobasilar system at the base of the brain. A thrombotic CVA causes a slow evolution of symptoms, usually over several hours, and is completed when the condition stabilizes. An embolic CVA occurs when a clot is carried into cerebral circulation and causes a localized cerebral infarct. Hemorrhagic CVA is caused by other conditions such as a ruptured aneurysm, hypertension, arteriovenous (AV) malformations, or other bleeding disorders. Symptoms depend on distribution of the cerebral vessel(s) involved. Ischemia may be (1) transient and resolve within 24 hours, (2) reversible with resolution of symptoms over a period of 1 week (reversible ischemic neurological deficit [RIND]), or (3) progress to cerebral infarction with variable effects and degrees of recovery. NURSING PRIORITIES 1. Promote adequate cerebral perfusion and oxygenation. 2. Prevent/minimize complications and permanent disabilities. 3. Assist patient to gain independence in ADLs. 4. Support coping process and integration of changes into self-concept. 5. Provide information about disease process/prognosis and treatment/rehabilitation needs. DISCHARGE GOALS 1. Cerebral function improved, neurological deficits resolving/stabilized. 2. Complications prevented or minimized. 3. ADL needs met by self or with assistance of other(s). 4. Coping with situation in positive manner, planning for the future. 5. Disease process/prognosis and therapeutic regimen understood. Nursing diagnosis for Cerebrovascular Accident (CVA): Infective Cerebral Tissue Perfusion may be related to Interruption of blood flow: occlusive disorder, hemorrhage; cerebral vasospasm, cerebral edema possibly evidenced by Altered level of consciousness; memory loss; Changes in motor/sensory responses; restlessness; Sensory, language, intellectual, and emotional deficits; and Changes in vital
signs. Desired Outcomes 1. Maintain usual/improved level of consciousness, cognition, and motor/sensory function. 2. Demonstrate stable vital signs and absence of signs of increased ICP. 3. Display no further deterioration/recurrence of deficits Nursing intervention with rationale: 1. Determine factors related to individual situation/cause for coma/decreased cerebral perfusion and potential for increased ICP. Rationale: Influences choice of interventions. Deterioration in neurological signs/symptoms or failure to improve after initial insult may reflect decreased intracranial adaptive capacity requiring patient be transferred to critical care area for monitoring of ICP, other therapies. If the stroke is evolving, patient can deteriorate quickly and require repeated assessment and progressive treatment. If the stroke is completed, the neurological deficit is nonprogressive, and treatment is geared toward rehabilitation and preventing recurrence. 2. Monitor/document neurological status frequently and compare with. Rationale: Assesses trends in level of consciousness baseline (LOC) and potential for increased ICP and is useful in determining location, extent, and progression/resolution of CNS damage. May also reveal presence of TIA, which may warn of impending thrombotic CVA. 3. Monitor vital signs, i.e., note: Hypertension/hypotension, compare BP readings in both arms. Rationale: Fluctuations in pressure may occur because of cerebral pressure/injury in vasomotor area of the brain. Hypertension or postural hypotension may have been a precipitating factor. Hypotension may occur because of shock (circulatory collapse). Increased ICP may occur because of tissue edema or clot formation. Subclavian artery blockage may be revealed by difference in pressure readings between arms. 4. Evaluate pupils, noting size, shape, equality, light reactivity. Rationale: Pupil reactions are regulated by the oculomotor (III) cranial nerve and are useful in determining whether the brainstem is intact. Pupil size/equality is determined by balance between parasympathetic and sympathetic enervation. Response to light reflects combined function of the optic (II) and oculomotor (III) cranial nerves. 5. Document changes in vision, e.g., reports of blurred vision, alterations in visual field/depth perception. Rationale: Specific visual alterations reflect area of brain involved, indicate safety concerns, andinfluence choice of interventions. 6. Assess higher functions, including speech, if patient is alert. Rationale: Changes in cognition and speech content are an indicator of location/degree of cerebral involvement and may indicate deterioration/increased ICP. 7. Position with head slightly elevated and in neutral position. Rationale: Reduces arterial pressure by promoting venous drainage and may improve cerebral
circulation/perfusion. 8. Maintain bedrest; provide quiet environment; restrict visitors/activities as indicated. Provide rest periods between care activities, limit duration of procedures. Rationale: Continual stimulation/activity can increase ICP. Absolute rest and quiet may be needed to prevent rebleeding in the case of hemorrhage. 9. Assess for nuchal rigidity, twitching, increased restlessness, irritability, onset of seizure activity. Rationale: Indicative of meningeal irritation, especially in hemorrhage disorders. Seizures may reflect increased ICP/cerebral injury, requiring further evaluation and intervention. 10. Administer supplemental oxygen as indicated. Rationale: Reduces hypoxemia, which can cause cerebral vasodilation and increase pressure/edema formation.
You might also like
- NCPDocument6 pagesNCPBon BonNo ratings yet
- Burns - Skin Integrity, ImpairedDocument2 pagesBurns - Skin Integrity, Impairedmakyofrancis20No ratings yet
- Nursing Care Plan: Group 4-Open Wound Head Injury After Debris FallDocument3 pagesNursing Care Plan: Group 4-Open Wound Head Injury After Debris FallNicole Villanueva, BSN - Level 3ANo ratings yet
- Hydrocephalus 9Document9 pagesHydrocephalus 9Shesly PhilominaNo ratings yet
- Nursing Care Plan: Imbalanced Nutrition: Less Than Body Requirements Disturbed Body Image Ineffective DenialDocument6 pagesNursing Care Plan: Imbalanced Nutrition: Less Than Body Requirements Disturbed Body Image Ineffective DenialBrix ValdrizNo ratings yet
- Jake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersDocument8 pagesJake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersJake Yvan DizonNo ratings yet
- Senile Cataract (Age-Related Cataract) - Practice Essentials, Background, PathophysiologyDocument5 pagesSenile Cataract (Age-Related Cataract) - Practice Essentials, Background, PathophysiologyAhmad FahroziNo ratings yet
- X. Nursing Care Plan: ObjectiveDocument6 pagesX. Nursing Care Plan: ObjectiveRenea Joy ArruejoNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocument14 pagesAssessment Diagnosis Planning Implementation Rationale EvaluationJennifer ArdeNo ratings yet
- Nursing Care Plan for Diverticulitis PatientDocument3 pagesNursing Care Plan for Diverticulitis PatientLeny GallardoNo ratings yet
- Code Green Introduction Reviewer - RedDocument4 pagesCode Green Introduction Reviewer - RedJamieNo ratings yet
- Types, Causes and Treatments of ComasDocument3 pagesTypes, Causes and Treatments of ComasgcsNo ratings yet
- Decreased Cardiac OutputDocument4 pagesDecreased Cardiac OutputAdnan Khan100% (1)
- NCPDocument15 pagesNCPCamille PinedaNo ratings yet
- Scribd 020922 Case Study-Oncology A&kDocument2 pagesScribd 020922 Case Study-Oncology A&kKellie DNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Risk For ConstipationDocument4 pagesNursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Risk For Constipationkenneth_bambaNo ratings yet
- Prostate Cancer CaseDocument32 pagesProstate Cancer CaseEbere EnyinnaNo ratings yet
- NCP CvaDocument4 pagesNCP CvaMariquita BuenafeNo ratings yet
- NCP-Case Presentation (CHF)Document4 pagesNCP-Case Presentation (CHF)Jessamine EnriquezNo ratings yet
- Nursing Care Plan for Diabetic Patient with DehydrationDocument2 pagesNursing Care Plan for Diabetic Patient with DehydrationRodolfo Bong SemaneroNo ratings yet
- Impaired Gas Exchange NCPDocument3 pagesImpaired Gas Exchange NCPRomel BaliliNo ratings yet
- Nursing Care Acute PancreatitisDocument2 pagesNursing Care Acute PancreatitisJamaica SaranquinNo ratings yet
- Nursing Care Plan for Labor and DeliveryDocument8 pagesNursing Care Plan for Labor and DeliveryRosemarie R. ReyesNo ratings yet
- Spina Bifida, Meningocele MyelomeningoceleDocument1 pageSpina Bifida, Meningocele MyelomeningocelesmilingstarsNo ratings yet
- Case Study Ugib Lower MBDocument65 pagesCase Study Ugib Lower MBQuolette Constante100% (1)
- Nursing Care Plan for Pre-operative AnxietyDocument1 pageNursing Care Plan for Pre-operative AnxietyVoid LessNo ratings yet
- Risk For Decreased Cardiac Tissue PerfusionDocument3 pagesRisk For Decreased Cardiac Tissue PerfusionKarina MadriagaNo ratings yet
- NURSING CARE PLAN - Risk For Fluid Volume DeficitDocument2 pagesNURSING CARE PLAN - Risk For Fluid Volume DeficitDaniel Andre S. SomorayNo ratings yet
- Velez College of Nursing F. Ramos Street, Cebu CityDocument57 pagesVelez College of Nursing F. Ramos Street, Cebu Cityinah krizia lagueNo ratings yet
- Pontine BleedingDocument99 pagesPontine BleedingJeffrey Dela CruzNo ratings yet
- NCPDocument10 pagesNCPCristina L. JaysonNo ratings yet
- Assessment Nsg. Diagnosis Sci. Explanation Planning Intervention Rationale EvaluationDocument6 pagesAssessment Nsg. Diagnosis Sci. Explanation Planning Intervention Rationale EvaluationRoMarie AbainzaNo ratings yet
- Acute Respiratory Distress SyndromeDocument40 pagesAcute Respiratory Distress SyndromeDavid Seroney100% (1)
- Case Study, Chapter 70, Management of Patients WithOncologic or Degenerative Neurologic DisordersDocument1 pageCase Study, Chapter 70, Management of Patients WithOncologic or Degenerative Neurologic Disordersclyde i am100% (1)
- Managing Fatigue Through Activity Pacing and RestDocument2 pagesManaging Fatigue Through Activity Pacing and ResthaniehaehaeNo ratings yet
- Diverticular DiseaseDocument8 pagesDiverticular Diseasenurse_enzo100% (1)
- Intussusception: PathophysiologyDocument8 pagesIntussusception: PathophysiologyNaufal AndaluNo ratings yet
- NCP Risk For InjuryDocument2 pagesNCP Risk For Injurycristina_galang_2No ratings yet
- Infectious Diarrhoea: Laboratory Investigation ofDocument36 pagesInfectious Diarrhoea: Laboratory Investigation ofputra nisaNo ratings yet
- 1 Ineffective Peripheral Tissue PerfusionDocument1 page1 Ineffective Peripheral Tissue Perfusionjean_fabulaNo ratings yet
- Basilar Skull Fractures DiagnosisDocument16 pagesBasilar Skull Fractures DiagnosisRindahMDNo ratings yet
- Nutrition and Metabolic Nursing Diagnosis and InterventionsDocument4 pagesNutrition and Metabolic Nursing Diagnosis and InterventionsKathrina CraveNo ratings yet
- 6 Nursing Care Plan 1Document2 pages6 Nursing Care Plan 1Denise Louise PoNo ratings yet
- 3 NCP Ineffective Tissue PerfusionDocument2 pages3 NCP Ineffective Tissue PerfusionSteffi MurielNo ratings yet
- Ineffective Cerebral Tissue Perfusion Related ToDocument7 pagesIneffective Cerebral Tissue Perfusion Related TohannahNo ratings yet
- Nursing Care Plan for Diabetic KetoacidosisDocument3 pagesNursing Care Plan for Diabetic KetoacidosisHanz AlecNo ratings yet
- Knowledge DeficitDocument5 pagesKnowledge DeficitteamstrocaNo ratings yet
- Growth and DevelopmentDocument5 pagesGrowth and DevelopmentGabrielLopezNo ratings yet
- Impaired Tissue PerfusionDocument2 pagesImpaired Tissue PerfusionLyka Mae Imbat - PacnisNo ratings yet
- NCP Cavernous Sinus ThrombosisDocument3 pagesNCP Cavernous Sinus ThrombosisVencel Mae Famas Villahermosa50% (2)
- Failure To ThriveDocument11 pagesFailure To ThriveFiraFurqaniNo ratings yet
- Thoracentesis Reflective EssayDocument2 pagesThoracentesis Reflective EssayAnjae GariandoNo ratings yet
- Impaired Skin IntegrityDocument3 pagesImpaired Skin IntegrityAubrey SungaNo ratings yet
- SeizuresDocument2 pagesSeizureskaythe08No ratings yet
- NCP FVDDocument1 pageNCP FVDsisjing88510No ratings yet
- Nursing Care Plan: Subjective: Nabalaka Ko Short Term: Independent: Goal Met Short TermDocument3 pagesNursing Care Plan: Subjective: Nabalaka Ko Short Term: Independent: Goal Met Short Termgeng gengNo ratings yet
- Managing Electrolyte Imbalances: A Case of Self-Induced HyperkalemiaDocument3 pagesManaging Electrolyte Imbalances: A Case of Self-Induced HyperkalemiaPaul JacksonNo ratings yet
- Ineffective Cerebral Tissue PerfusionDocument3 pagesIneffective Cerebral Tissue PerfusionHanya Bint Potawan88% (25)
- Ineffective Cerebral Tissue Perfusion - Stroke (CVA) Nursing Care Plan (NCP)Document6 pagesIneffective Cerebral Tissue Perfusion - Stroke (CVA) Nursing Care Plan (NCP)Alba ArjunNo ratings yet
- Sin CopeDocument3 pagesSin CopeCarouselofTinaNo ratings yet
- RetinalDocument11 pagesRetinalHenry Roque TagalagNo ratings yet
- RiskDocument1 pageRiskHenry Roque TagalagNo ratings yet
- Case Study On Ob Ward PreeclampsiaDocument12 pagesCase Study On Ob Ward PreeclampsiaNimrod83% (6)
- Wesleyan University - Philippines: Delivery Cases (Assist)Document6 pagesWesleyan University - Philippines: Delivery Cases (Assist)Henry Roque TagalagNo ratings yet
- Thesis Study Habits Ms WordDocument2 pagesThesis Study Habits Ms WordHenry Roque TagalagNo ratings yet
- Copd PathoDocument1 pageCopd PathoHenry Roque TagalagNo ratings yet
- Diseases Affecting Mhjkkthe Circulatory SystemDocument4 pagesDiseases Affecting Mhjkkthe Circulatory SystemHenry Roque TagalagNo ratings yet
- Act NorhrhhDocument1 pageAct NorhrhhHenry Roque TagalagNo ratings yet
- Undifferentiated SchizophreniaDocument190 pagesUndifferentiated Schizophreniaallexiscampaner100% (16)
- Checklist-Ncm 104 (Skills) (2hjjhjDocument10 pagesChecklist-Ncm 104 (Skills) (2hjjhjHenry Roque TagalagNo ratings yet
- Act NorhrhhDocument1 pageAct NorhrhhHenry Roque TagalagNo ratings yet
- Drug StudyDocument40 pagesDrug Studyapi-374468390% (61)
- Tracheostomy Skin Care (Stoma Care)Document4 pagesTracheostomy Skin Care (Stoma Care)Henry Roque TagalagNo ratings yet
- NCP RHDDocument7 pagesNCP RHDHenry Roque Tagalag80% (5)
- Azithromycin (Drug Study)Document2 pagesAzithromycin (Drug Study)Franz.thenurse688893% (15)
- Pathophysiology BPH Case StudyDocument3 pagesPathophysiology BPH Case Studyyhanne100% (24)
- MultivitaminDocument1 pageMultivitaminKatie McPeek88% (8)
- Case Study RheumaticDocument46 pagesCase Study RheumaticJill Anne Balderosa91% (11)
- Dada Choose My PlateDocument1 pageDada Choose My PlateHenry Roque TagalagNo ratings yet
- FluimucilDocument2 pagesFluimucilianecunar86% (7)
- Drug Study AminophyllineDocument1 pageDrug Study Aminophyllinejunie100% (3)
- FluimucilDocument2 pagesFluimucilianecunar86% (7)
- Drug Study AminophyllineDocument1 pageDrug Study Aminophyllinejunie100% (3)
- Pathophysiology BPH Case StudyDocument3 pagesPathophysiology BPH Case Studyyhanne100% (24)
- Risk Factors in AtherosclerosisDocument1 pageRisk Factors in AtherosclerosisHenry Roque TagalagNo ratings yet
- Nursing Minimum Data Set SystemDocument4 pagesNursing Minimum Data Set SystemHenry Roque Tagalag100% (3)
- A Nursing Care Plan VaDocument3 pagesA Nursing Care Plan VaArianne Paola QuindoyNo ratings yet
- DB13 - Pathophysiology of AtherosclerosisDocument2 pagesDB13 - Pathophysiology of Atherosclerosisi_vhie03No ratings yet
- Drug Study AminophyllineDocument1 pageDrug Study Aminophyllinejunie100% (3)
- Anticoagulation in OrthopedicsDocument32 pagesAnticoagulation in Orthopedicsehabede6445No ratings yet
- Cerebrovascular AccidentDocument17 pagesCerebrovascular Accidentmanisha paikarayNo ratings yet
- Thrombophilia Testing and VenousDocument11 pagesThrombophilia Testing and VenousneurojuancarfabNo ratings yet
- Diseases of Arteries ExplainedDocument377 pagesDiseases of Arteries ExplainedBhuvana MohanamurthyNo ratings yet
- Management of Patients With Vascular Disorders: Venous ArterialDocument56 pagesManagement of Patients With Vascular Disorders: Venous ArterialHamss AhmedNo ratings yet
- An Atlas of Gross Pathology PDFDocument113 pagesAn Atlas of Gross Pathology PDFZuhri MardiahNo ratings yet
- Anticoagulant Therapy For Deep Vein Thrombosis (DVT-2Document7 pagesAnticoagulant Therapy For Deep Vein Thrombosis (DVT-2Rahma AnwarNo ratings yet
- Haemodynamics Embolism and Infarction GuideDocument27 pagesHaemodynamics Embolism and Infarction GuideAsutosh PradhanNo ratings yet
- Falla Respiratoria & Embarazo - Lapinsky 2015Document7 pagesFalla Respiratoria & Embarazo - Lapinsky 2015Fabiola Buelna GaxiolaNo ratings yet
- MRCP-2 July 2021 Recall QsDocument10 pagesMRCP-2 July 2021 Recall Qszehra khowajaNo ratings yet
- AIM GuidelinesDocument235 pagesAIM GuidelinesTurkiNo ratings yet
- PeripheralVascularDisease NotesDocument6 pagesPeripheralVascularDisease NotesNoah PontinoNo ratings yet
- Tranexamic Acid in Gynaecology & ObstetricDocument26 pagesTranexamic Acid in Gynaecology & ObstetricsivaNo ratings yet
- Lapsus Fraktur Neck FemurDocument32 pagesLapsus Fraktur Neck FemurZóélkårnåín PhåntómhívéNo ratings yet
- 111Document80 pages111Amrut HosmaniNo ratings yet
- Double-Outlet Left Ventricle and Vascular MalformationsDocument3 pagesDouble-Outlet Left Ventricle and Vascular MalformationsRaul UrietaNo ratings yet
- Doyle Pre Hospital Emergency Care June 2008 2Document17 pagesDoyle Pre Hospital Emergency Care June 2008 2andreipassNo ratings yet
- VTE Risk Assessment Tool Caprini Score Card Eng 30apr2018Document2 pagesVTE Risk Assessment Tool Caprini Score Card Eng 30apr2018Ahmed MohammedNo ratings yet
- Oestradiol As Hemihydrate + DrospirenoneDocument15 pagesOestradiol As Hemihydrate + Drospirenoneddandan_2No ratings yet
- Quick Guide DVTDocument26 pagesQuick Guide DVTdrkrsticNo ratings yet
- Occurrence of Infection Among Children With Nephrotic Syndrome During HospitalizationsDocument8 pagesOccurrence of Infection Among Children With Nephrotic Syndrome During HospitalizationsViswas ChhapolaNo ratings yet
- Nursing diagnosis impaired mobilityDocument2 pagesNursing diagnosis impaired mobilityAi Rou100% (1)
- D-dimer and platelet aggregation predict thrombotic risk in PADDocument8 pagesD-dimer and platelet aggregation predict thrombotic risk in PADlidawatiNo ratings yet
- Defense Against Infectious Disease: Skin As A Barrier To InfectionDocument8 pagesDefense Against Infectious Disease: Skin As A Barrier To InfectionFranchesca Rosabel BudimanNo ratings yet
- HomeFit BrochureDocument5 pagesHomeFit BrochureSarah M. WaymanNo ratings yet
- 3.8.06 Aortoiliac DiseaseDocument21 pages3.8.06 Aortoiliac DiseaseAndri Feisal NasutionNo ratings yet
- (9781585284894 - Anticoagulation Therapy) Preliminary Material PDFDocument22 pages(9781585284894 - Anticoagulation Therapy) Preliminary Material PDFAkram Sh. AhmedNo ratings yet
- Articles On Wheat ToxicityDocument96 pagesArticles On Wheat ToxicityDr. Heath MotleyNo ratings yet
- Dental Management of Children Undergoing Liver TransplantationDocument9 pagesDental Management of Children Undergoing Liver Transplantationwahyudi_donnyNo ratings yet
- Therapeutic Plasmapheresis: A Revision of Literature: Review ArticleDocument13 pagesTherapeutic Plasmapheresis: A Revision of Literature: Review Articlemuhammad24fayazNo ratings yet