Professional Documents
Culture Documents
15
Uploaded by
anjozzCopyright
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
15
Uploaded by
anjozzCopyright:
Med Oral Patol Oral Cir Bucal 2007;12:E154-9.
Management of odontogenic infection
Management of odontogenic infection of pulpal and periodontal origin
Roberto Lpez-Priz 1, Lorenzo Aguilar 2, Maria Jos Gimnez 3
(1) Degree in Medicine and Surgery. Degree in Odontology. Doctoral student (2) Doctor in Medicine and Surgery (3) Doctor in Pharmacy. Microbiology Department, Faculty of Medicine, UCM
Correspondence: Dr. Roberto Lpez-Priz. C/ General lvarez de Castro, n 5, 1 B. 28010. Madrid. E-mail: lopezpiriz@telefonica.net Lpez-Priz R, Aguilar L, Gimnez MJ. Management of odontogenic infection of pulpal and periodontal origin. Med Oral Patol Oral Cir Bucal 2007;12:E154-9.
Medicina Oral S. L. C.I.F. B 96689336 - ISSN 1698-6946
Received: 12-11-2006 Accepted: 25-01-2007
Indexed in: -Index Medicus / MEDLINE / PubMed -EMBASE, Excerpta Medica -SCOPUS -Indice Mdico Espaol -IBECS
ABSTRACT
The dental biofilm is a complex bacterial ecosystem that undergoes evolution, maturing and development, and thus leads to odontogenic infection. The infection is normally located in the tissues of the dental organ itself, and follows a chronic course of evolution. However, bacterial pathogens express virulence factors in the biofilm, and this together with changes in host immunity, may cause clinical exacerbations and spread of infection to other areas of the body. Odontogenic infection management should take into consideration the fact that therapeutic success lies in the control of the infectious aetiologic agent, using mechanical-surgical debridement and/or antimicrobial therapy. Debridement techniques have a fundamentally quantitative effect (by reducing the size of the inoculum) and therefore if these techniques are used alone to control infection, despite an initial clinical improvement that is sometimes prematurely considered as therapeutic success, odontopathogens may persist and the process may recur or become chronic. Microbiological examination may be helpful in defining therapeutic success in a more reliable way, it could define the prognosis of recurrence more precisely, and could enable the most appropriate antibiotic to be selected, thus increasing therapeutic efficacy. Antimicrobial therapy brings about a quantitative and qualitative change in the bacterial composition of the biofilm, in addition to being able to act on sites that are inaccessible through mechanical debridement. However, incorrect antimicrobial use can lead to a selection of resistant bacterial species in the biofilm, in addition to side effects and ecological alterations in the host. In order to minimise this risk, and obtain maximum antimicrobial effect, we need to know in which clinical situations their use is indicated, and the efficacy of different antibiotics with regard to bacteria isolated in odontogenic infection. Key words: Odontogenic infection, treatment, odontogenic infection, microbiological diagnosis, dental biofilm, dental abscess.
RESUMEN
La biopelcula dental es un ecosistema bacteriano complejo cuya evolucin, maduracin y desarrollo ocasiona la infeccin odontognica. Habitualmente la infeccin se encuentra localizada en los tejidos del propio rgano dentario y sigue un curso evolutivo crnico, aunque la expresin de factores de virulencia bacterianos en la biopelcula o cambios en la situacin inmune del husped pueden ocasionar exacerbaciones clnicas y la extensin de la infeccin a otras zonas del organismo. En el abordaje de la infeccin odontognica debemos tener presente que el xito teraputico radica en el control del agente etiolgico infeccioso, mediante desbridamiento con tcnicas mecnico-quirrgicas y/o administracin de antimicrobianos. El efecto de las tcnicas de desbridamiento sobre la biopelcula es fundamentalmente de tipo cuantitativo (disminuye el tamao del inculo) de modo que su empleo como nico medio de control de la infeccin puede suponer la persistencia de odontopatgenos y la recurrencia o cronificacin del proceso, aunque obtengamos una mejora clnica inicial que en ocasiones consideramos xito teraputico de modo precipitado. Realizar un estudio micro-
E154
Med Oral Patol Oral Cir Bucal 2007;12:E154-9.
Management of odontogenic infection
biolgico podra ayudar a definir el xito teraputico con mayor fiabilidad, dar ms exactitud a nuestros pronsticos de recurrencia, y seleccionar el antibitico ms apropiado aumentando la eficacia teraputica. El tratamiento antimicrobiano ocasiona un cambio cuantitativo y cualitativo en la composicin bacteriana de la biopelcula, adems de poder actuar en lugares no accesibles al desbridamiento mecnico. Sin embargo, un mal uso de los antimicrobianos puede ocasionar seleccin de especies bacterianas resistentes en la biopelcula adems de efectos secundarios y alteraciones ecolgicas en el husped. Para minimizar este riesgo y obtener el mximo rendimiento del empleo de antimicrobianos es preciso conocer las situaciones clnicas que indican su uso y la eficacia de los distintos antibiticos frente a los aislados en la infeccin odontognica. Palabras clave: Infeccin odontognica/tratamiento, infeccin odontognica, diagnstico microbiolgico, biopelcula dental, absceso dental.
EPIDEMIOLOGY
Odontogenic infection is the most prevalent disease worldwide and it is the principal reason for seeking dental care. The commonest emergency odontogenic infections are periapical abscess (25%), pericoronitis (11%) and periodontal abscess (7%). Its significance in health problems is also reflected by the fact that 12% of antibiotics are prescribed for odontological reasons. (1)
AETIOLOGY OF ODONTOGENIC INFECTION
The World Health Organisation accepts that the dental biofilm is the aetiological agent of odontogenic infection, and defines biofilm as a proliferative bacterial, enzymeactive ecosystem. As soon as a baby is born, a colonisation process commences and this results in the development of a pioneer community in the mouth with predominance of Streptococcus salivarius. At the age of six months (when the first teeth appear) this community has a majority presence of S. sanguis and S. mutans, and by the time dentition has been completed, there is a heterogeneous aerobic and anaerobic community. It is estimated that up to 700 species may colonise the mouth, 400 of which colonise the subgingival area. Biofilm evolution is an autogenic succession process based on bacterial interactions that occur through physical contact, metabolic exchange, communication through signalling (quorum sensing) and genetic material exchange. Coaggregation is based on specific recognition of different bacterial species and one of the principle mechanisms of evolution and maintenance of the biofilm. (2) Odontogenic infection is polymicrobial and mixed. It is the result of biofilm maturing that consists of a change in the predominant bacterial species (from predominantly gram-positive, facultative and saccharolytic flora to predominantly gram-negative, anaerobic and proteolytic flora), the association of different bacterial morphotypes and increased bacterial diversity. Fusobacterium nucleatum is considered as the central structural component of biofilm because it coaggregates with the biofilm components that do not cause disease and with periodontal pathogens, thus permitting biofilm evolution into odontogenic infection. In 1992, Socransky modified Kochs postulates, laying down criteria for identifying periodontal pathogens. (3) Biofilm study using DNA hybridisation techniques enabled detection of associations of specific bacterial species
and their relation with health or disease. Purple (with fundamentally aerobic and immobile flora), yellow and green complexes are not associated with disease, whilst orange (F. nucleatum/periodonticum, P. intermedia, P. micros) and red (P. gingivalis, T. forsythia, T. denticola) complexes cause disease in the presence of virulent clones with intra- and extrachromosomic genetic information in a sufficient quantity to overcome the immune resistance of the host. A. actinomycetemcomitans is also considered as a periodontal pathogen although it is not included in any particular group.
PATHOGENICS OF ODONTOGENIC INFECTION
The supragingival biofilm is fundamentally gram-positive, facultative and saccharolytic, which means that in the presence of sugars, it produces acids that demineralise enamel, facilitating biofilm infiltration of dentin and pulp. With the bacterial invasion of the tooths internal tissue, the biofilm evolves, and thus root canals are infected with predominantly gram-negative, anaerobic and proteolytic bacteria. Some of these bacteria have virulence factors that enable them to invade periapical tissues through the apical foramen. (3) More than half of active periapical lesions cannot be detected on X-ray because they measure less than 0.1 mm2. (4) If the host immune response causes an accumulation of neutrophils, this will cause a periapical abscess, which is a destructive tissue lesion. But if the response is predominantly mediated by macrophages and T-cells, an apical granuloma will develop, characterised more by tissue reorganisation than by tissue destruction. Changes in host immunity or in bacterial virulence may cause reactivation of silent periapical lesions. Odontogenic infection may also originate in periodontal tissues. When the subgingival biofilm evolves and incorporates periodontal pathogens that express virulence factors, this triggers an immune response in the host causing damage tending to chronicity that finally causes periodontal bone loss. The periodontal abscess may originate from an exacerbation of chronic periodontitis, the presence of dental defects that facilitate bacterial invasion (e.g. development grooves, root fusion, etc.) or it may be of iatrogenic origin, due to impaction of a calculus in the epithelium of the periodontal pocket during scaling or incorrect debridement E155
Med Oral Patol Oral Cir Bucal 2007;12:E154-9.
Management of odontogenic infection
that only solves gingival distension at a coronal level, preventing drainage of apical zone of the pocket. (5) Some abscesses form a fistula and become chronic. They are generally asymptomatic or paucisymptomatic. A special form of recurrent periodontal abscess is pericoronitis, caused by bacterial invasion of the coronal pouch during molar eruption. It is sometimes unclear as to whether the infection has a periodontal or pulpar origin, and therefore the term endoperiodontal lesions are used. (4) There is some controversy as to whether a pulpar lesion can cause periodontal damage and vice versa, which raises several questions at a clinical level: should we perform prophylactic canal treatment of teeth with moderate or advanced periodontitis? Should a tooth with pulpar necrosis be replaced by an implant in order to prevent periodontal bone loss? The pulp can be invaded from the periodontium through dentin tubules, lateral canals and the apical foramen, but it is very rare to find a tooth without pulp vitality and free of caries, restoration work or trauma to justify it, and therefore periodontal disease and periodontal mechanical debridement do not appear to have a significant influence on pulp vitality. Teeth without pulp vitality and with active periapical lesions present greater marginal bone loss / year than teeth with pulp vitality, but these differences are not significant enough in periodontal prognosis to justify preventive tooth extraction. Pulpar infection can form a fistula in the periodontium, causing a deep and narrow periodontal lesion. In general, the presence of pulp vitality indicates that the bacterial invasion has occurred from or through the periodontium, and the absence of pulp vitality suggests an endodontic origin of infection. If an in-depth clinical examination is carried out, few lesions will actually be classified as endoperiodontal lesions.
fractures that are perpendicular or oblique to the X-ray may not be detected. In addition, pulp vitality tests help to identify target tooth and also the likely origin of bacterial invasion: infection may be of pulpar origin if the test is negative or if there is an exaggerated response to stimulus; it may be of periodontal origin if positive test without discrepancies with that of other teeth. However, there is some controversy regarding the utility and indication of microbiology diagnostic tests in odontogenic infections. Clearly there is no need to perform a microbiology examination in order to diagnose periodontitis, but a microbiological analysis of the infection may be useful if results enable us to improve our therapeutic strategies and ensure successful treatment, and in any case it serves to provide epidemiological data. (6) Microbiological analysis can help to identify the origin of infection. Although all odontogenic infections are result of biofilm evolution, and there are therefore marked similarities in the bacterial composition of odontogenic infections, regardless of their tissue of origin (Table 1), some bacterial species are specific to abscesses with pulpar origin (e.g. Porphiromonas endodontalis); while others will rule out this origin (e.g. A. actinomycetemcomitans). (7,8) However, odontological microbiological studies are complex to perform. Sampling is a difficult task since samples often become contaminated, thus altering results. Samples must be transported in appropriate media for mixed flora.
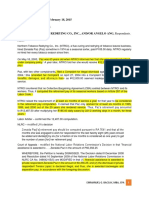
Table 1. Type of odontogenic infections and organims responsible.
Infectious process
Predominant odontopathogens
DIAGNOSIS OF ODONTOGENIC INFECTION
Diagnosing the origin of odontogenic infection is fundamental in order to manage treatment appropriately. The problem tooth needs to be identified, as well as the tissue where the biofilm bacteria have commenced their invasion. Clearly, a thorough physical examination is required, along with X-rays and pulp vitality tests. Clinical manifestations may be useful when they are referred to a specific tooth (e.g. periodontal abscess), but manifestations are often diffuse or even refer to areas that are adjacent to the origin of the infection (e.g. pulpitis). Odontogenic infection may also occur without symptoms (e.g. chronic periodontitis) or with very few symptoms (e.g. periapical abscess that has formed a fistula), and this could only be manifested on clinical examination. A clinical examination consisting in inspection and percussion of teeth is essential to identify the origin of infection. X-rays provide essential information but certain limitations should be considered: 1. Some periapical cysts may be larger than a periapical X-ray film, and therefore only the contents will be observed; 2. During early stages of infection changes in bone density may not be noticeable; 3. Only bidimensional information can be gained, and therefore E156
Periodontitis
Porphiromonas gingivalis. Tannerella forsythensis Actinomyces actinomycetemcomitans Prevotella intermedia Fusobacterium nucleatum Veionella parvula Treponema dentcola Streptococcus spp.
Fusobacterium nucleatum Prevotella intermedia Peptostretococcus micros Capnociytophaga ochracea Selenomonas sputigena Porphiromonas endodontalis Streptococcus spp.
Pulpitis with periapical abscess
Pericoronitis
Prevotella intermedia Veionella parvulaPrevotella melaninogenica Fusobacterium nucleatum Actinomyces israelii/odontolyticus Streptococcus spp.
Fusobacterium nucleatum Prevotella intermedia Pseudomona aeruginosa Staphilococcus spp Actinomyces actinomycetemcomitans
Periimplantitis
Med Oral Patol Oral Cir Bucal 2007;12:E154-9.
Management of odontogenic infection
Differences in bacterial identification methods are also the cause of discrepancy in conclusions drawn by different studies that have analysed the bacterial composition of odontogenic infections. Bacterial culture is the traditional method of identification, but some bacteria require special culture methods (e.g. T. forsythia) and others can only be identified using immunofluorescent techniques or DNA hybridisation. (6) Keyes used differential darkfield microscopy to determine the level of spirochetes and motile rods, thus ending treatment when there was a reduced number found on the biofilm examined. (6) It is now known that some bacteria behave as exogeneous pathogens and some bacterial associations related to a low treatment response or high rate of recurrence. (3) For example, the presence of A. actinomycetemcomitans; P. gingivalis; or P. intermedia is associated with recurrence in periodontal disease activity. Thus, since the microbiological examination can identify odontopathogens and determine their numbers in the biofilm, then it can help to make decisions on a specific therapeutic strategy and to monitor results of clinical studies. In short, microbiology helps to define therapeutic success and the risk of relapse more precisely, thus avoiding a prognosis based exclusively on clinical data (i.e. initial improvement following debridement). Microbiological cultures also allow the study of susceptibility of odontopathogenic isolates to different antibiotics. They can determine which antimicrobial agents are the most effective in odontogenic infections, by determining minimum inhibitory concentrations. These data are the basis of studies relating odontopathogenic susceptibility and antimicrobial pharmacokinetics/pharmacodynamics, in order to establish the most effective therapeutic regimen.
TREATMENT OF ODONTOGENIC INFECTION
The objective of antibacterial treatment is to control (reduce or eliminate) the infective bacterial load. To achieve this, in the case of odontogenic infection, therapeutic action combines mechanical debridement, and/or surgery, and/or systemic antibiotic therapy, where appropriate. The first step in the case of dental abscess is to drain and debride the abscess using mechanical-surgical techniques. Drainage is performed by making an incision in the area of greatest fluctuation. If the abscess is of an endodontic origin, drainage can be performed through the root canals. Tooth extraction provides a drainage route and eliminates the entrance route for the infection, but it is only indicated in the acute phase after having balanced these benefits against the risk of spreading bacterial inoculum during surgery. Tooth extractions that require flap surgery or ostectomy should be delayed until a second stage when infection has been controlled. Mechanical debridement eliminates necrotic tissue and bacterial residues, and consists in debridement of the root surface in the case of periodontal involvement, or of the bone canal in the case of pulpar infection. Mechanical-surgical techniques have a quantitative effect on bacterial load giving the host the opportunity to recover homeostasis through immune system action. (9) However,
these techniques do not modify the composition of the biofilm and the persistence of odontopathogens that could lead to recurrence or a chronic state. A. actinomycetemcomitans and P. gingivalis cannot be eliminated in the majority of deep periodontal lesions with root debridement alone. (7) The persistence of S. faecalis in root canals is related to the need to repeat endodontic treatment, and the percentage of failed root canal treatment according to X-ray results is estimated at about 50%. (4,8) Furthermore, some bacteria (Actinomyces israelii; Propionibacterium propionicum) are capable of reaching the dental periapex and remain there, requiring an apicectomy in an attempt to eliminate persistent infection. Additional techniques to complement mechanical treatment include chemical debridement by means of topical application of antiseptics and antimicrobial agents. It is recommended to use antiseptic irrigation concomitantly during mechanical debridement, but the use of topical substances is not indicated during the acute phase because they hinder drainage. (5) Root canals can be filled with antiseptic substances for a long period of time, but such substances have little or no action at a periapical level. The topical use of antimicrobials should be restricted because this favours the development of resistance and their clinical effect is limited to the application surface since they do not act on invasive bacteria. (4,5,7) The relevance of antimicrobials in the management of odontogenic infection lies in their clinical utility when administered systemically. Systemic antibiotic therapy prevents the infection from spreading and it acts in places that mechanical treatment cannot reach. It therefore act more specifically on odontopathogens than debridement does. (10) It is indicated for therapeutic purposes in fast-progressing and recurrent periodontitis, and in all odontogenic infections with rapidly evolving signs and symptoms (24-48 hours), trismus, oedema, and/or systemic manifestations such as malaise, fever, tachypnoea, dyspnoea, cellulites, lymphadenopathy and hypotension. (11) Systemic antibiotic therapy is also indicated in the prophylaxis of systemic or distant infection and as a preventive treatment of infection in immunodepressed patients or in patients with severe systemic disease undergoing an invasive or long time dental procedure. (10,12,13) It has been demonstrated that periodontal abscesses have resolved solely by means of systemic antibiotic therapy. (5,14,15) However, debridement should be the first step in therapy because draining the infection and eliminating necrotic waste will facilitate antimicrobial action. Treatment with antimicrobials alone is indicated when the severity of the infection advises delaying surgical techniques due to the risk of spreading the infection during debridement itself. (11) Antibiotic prophylaxis achieves better results if the antimicrobial agent is administered pre-operatively. (10,13) Paradoxically, treatment of chronic asymptomatic infection can cause an acute exacerbation of the infectious process. Periodontal scaling and endodontic over-instrumentation can cause bleeding and exudates in periodontal and E157
Med Oral Patol Oral Cir Bucal 2007;12:E154-9.
Management of odontogenic infection
periapical tissues, providing bacteria with nutrients, and thus stimulating proliferation, which may overcome the hosts immune resistance. This factor should be given special consideration in immunodepressed patients and in patients whose microbiological studies reveal odontopathogens or bacterial associations that are particularly resistant to therapy. In these cases, it is essential to use an effective antimicrobial agent. (10,13) Only physicians or dentists should select which antimicrobial agent to use, because it is a complex clinical process that is based on empirical evidence and clinical, microbiological and pharmacokinetic knowledge. (10) The use of an antibiotic with an inappropriate spectrum that does not act on certain resistant bacterial species will lead to excess proliferation of the latter by eliminating other sensitive species. This may trigger acute exacerbations or persistent infection. Wide spectrum antibiotics must be used in view of the polymicrobial, mixed nature of odontogenic infections, and such antibiotics must be especially active against the commonest odontopathogens. When selecting an antibiotic, consideration should be made for natural resistance (e.g. Strepococcus sp.; Actinomyces sp. and A. acinomycetemcomitans against metronidazole) and the possible presence of acquired resistance, which are those that take advantage of incorrect antibiotic use.
Some studies have analysed the susceptibility of bacterial species in the biofilm to antibiotics in Spain. (16) These studies show a high rate of resistance to certain antimicrobial agents and beta-lactamase production by Prevotella spp, Fusobacterium spp.; Capnocytophaga spp. and some strains of Veionella spp.(17-19). From results obtained (Table 2), there is consensus regarding the treatment and prophylaxis of odontogenic infection in which amoxicillin associated with clavulanic acid is indicated as the first choice antibiotic, and clindamycin as an alternative in the event of penicillin allergy. (12,13,20) Antimicrobial pharmacodynamics determine the most effective dosage regimen to attain bacterial eradication without encouraging the development of resistance. The most commonly used antibiotics in odontology are time-dependent, which means that to be effective, their physiological levels must exceed the minimum inhibitory concentration for at least 40% of the time between doses. (16) Taking into account the susceptibility of isolated bacteria, resistance mechanisms and antibiotic pharmacodynamics, high doses of amoxicillin / clavulanic acid (875/125 mg three times daily or 2000/125 mg twice daily) are the most appropriate treatment of caries-associated odontogenic infections (pulpitis, abscesses), and of periodontal infections when so required, and clindamycin provides an alternative choice, at a dose of 600 mg three times daily.
Table 2. Activity of different antimicrobial agents against odontopathogens.
A. actino- Peptostrepmycetemcomitans Penicillin G Amoxicillin Amoxicillin / Clavulanic acid Doxycycline Clindamycin Metronidazole Macrolides +/+ + + 0 0 +/tococcus spp + + + +/+ + +/-
Prevotella Porphiro- Fusobacspp monas spp +/+/+ +/+ + +/+/+/+ +/+ + +/terium spp +/+/+ + + + +/-
Streptococcus oralis +/+ + +/+ 0 +/-
+ More than 80% sensitive strains. // +/- 30 - 80% sensitive strains. // 0 Less than 30% sensitive strains.
E158
Med Oral Patol Oral Cir Bucal 2007;12:E154-9.
Management of odontogenic infection
REFERENCES
1. Matesanz P, Figuero E, Jimnez MJ, Aguilar L, Llor C, Prieto J, Bascones A. Del conocimiento de la etiologa bacteriana al tratamiento y la prevencin de las infecciones ms prevalentes en la comunidad: las infecciones odontognicas. Rev Esp Quimioterap 2005;18:136-45. 2. Kolenbrander P, Palmer R, Richard A, Jakubovics N, Chalmers N. Bacterial interactions and successions during plaque development. Periodontology 2000 2006;42:47-79. 3. Socransky S, Haffajee A. The bacterial ethiology of destructive periodontal disease: current concepts. J Periodontol 1992;63:322-31. 4. Harrinon G, Steiner D, Ammons W. The periodontal-endodontic controversy. Periodontology 2000 2002:30:123-30. 5. Herrera D, Roldn S, Sanz M. The periodontal abscess: a review. J Clin Periodontol 2000;27:377-86. 6. Winkelhoff A, Winkel E. Microbiologycal diagnostics in periodontics: biological significance and clinical validity. Periodontology 2000 2005;39:40-52. 7. Dahln G. Microbiology and treatment of dental abscesses and periodontal-endodontic lesions. Periodontology 2000 2002;28:206-39. 8. Vigil GV, Wayman B, Dazey S, Fowler C, Bradley D. Identification and antibiotic sensitivity of bacteria isolated from periapical lesions. Journal of Endodontics1997;23:110-4. 9. Goodson J, Palys M, Carpino E, Regan E, Sweeney M, Socransky S. Microbiological changes associated with dental prophilaxis. JADA 2004;135:1559-64. 10. Bascones A, Lpez Priz R. Abordaje desde atencin primaria de las enfermedades infecciosas ms prevalentes en la comunidad: infecciones odontognicas. En: Infecciones odontognicas en la comunidad y antibioticoterapia: dos factores a sincronizar. Madrid: Adalia farma S.L.; 2006. p. 99-112. 11. Flynn T, Shanti R, Levi M, Adamo A, Kraut R, Trieger N. Severe odontogenic infections. J Oral Maxillofac Surg 2006;64;1093-113. 12. Bascones Martnez A, Aguirre Urzar JM, Bermejo Fenoll A, Blanco Carrin A, Gay-Escoda C, Gonzlez Moles MA, et al. Documento de consenso sobre el tratamiento antimicrobiano de las infecciones bacterianas odontognicas. Med Oral Pat Oral Cir Bucal 2004;9:363-76. 13. Gutirrez JL, Bagn JV, Bascones A, Llamas R, Llena J, Morales A, et al. Documento de consenso sobre la utilizacin de profilaxis antibitica en ciruga y procedimientos dentales. Med Oral Pat Oral Cir Bucal 2006;11: E119-36. 14. Herrera D, Roldn S, Sanz M. The periodontal abscess (I). Clinical and microbilogical findings. J Clin Periodontol 2000;27:387-94. 15. Herrera D, Roldn S, Sanz M. The periodontal abscess (II). Short-term clinical and microbiologycal efficacy of 2 systemyc antibiotic regimes. J Clin Periodontol 2000;27:395-404. 16. Canut A. Antimicrobianos en las infecciones odontognicas: anlisis farmacocintica/farmacodinmico (PK/PD). Seguridad y tolerancia. En: Infecciones odontognicas en la comunidad y antibioticoterapia: dos factores a sincronizar. Madrid: Adalia farma S.L.; 2006. p. 51-69. 17. Sixou JL, Magaud C, Jolivet-Gourgeon A, Cormier M, Bonnaure-Mallet M. Microbiology of mandibular third molar pericoronitis: Incidence of -lactamase-producing bacteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:655-9. 18. Baumgartner JC, Xia T. Antibiotic susceptibility of bacteria associated with endodontic abscesses. Journal of endodontics 2003;29:44-7. 19. Winkellhof A, Herrera D, Oteo A, Sanz M. Antimicrobial profiles of periodontal pathogens isolated from patients in the Netherlands and Spain. J Clin Periodontol 2005;32:893-8. 20. Liares J, Martn Herrero JE. Bases farmacomicrobiolgicas del tratamiento antibitico de las enfermedades periodontales y periimplantarias Av. Odontoestomatol 2003; (especial):23-33.
E159
You might also like
- Uji Kepekaan Bakteri Terhadap AntibiotikaDocument18 pagesUji Kepekaan Bakteri Terhadap AntibiotikaanjozzNo ratings yet
- Tarrson Family Endowed Chair in PeriodonticsDocument102 pagesTarrson Family Endowed Chair in PeriodonticsKate OngNo ratings yet
- TetanusDocument30 pagesTetanusSaad MotawéaNo ratings yet
- Tooth Whitening Concepts andDocument9 pagesTooth Whitening Concepts andanjozzNo ratings yet
- Odontogenic InfectionsDocument11 pagesOdontogenic InfectionsanjozzNo ratings yet
- IndraDocument7 pagesIndrajukunkNo ratings yet
- Jurnal PDFDocument10 pagesJurnal PDFNayda FitrinaNo ratings yet
- Vital Tooth Bleaching An Update by StrasslerDocument12 pagesVital Tooth Bleaching An Update by StrassleranjozzNo ratings yet
- Periodontal Diseases As Bacterial Infection: Bascones Martinez A Figuero Ruiz EDocument8 pagesPeriodontal Diseases As Bacterial Infection: Bascones Martinez A Figuero Ruiz EWidaRostinaNo ratings yet
- Review - Dental ClinicsDocument13 pagesReview - Dental ClinicsAndrea UrgilesNo ratings yet
- Severe Odontogenic InfectionsDocument8 pagesSevere Odontogenic InfectionsmumunooNo ratings yet
- The Bleaching of Teeth-A Review of The LiteratureDocument8 pagesThe Bleaching of Teeth-A Review of The LiteratureanjozzNo ratings yet
- IntroductionDocument8 pagesIntroductionanjozzNo ratings yet
- CLP BookletDocument25 pagesCLP BookletanjozzNo ratings yet
- Effects of BleachingDocument7 pagesEffects of BleachinganjozzNo ratings yet
- 0003-3219 (2005) 075 0273 Ntoaob 2.0.co 2Document7 pages0003-3219 (2005) 075 0273 Ntoaob 2.0.co 2anjozzNo ratings yet
- Current Status ofDocument8 pagesCurrent Status ofanjozzNo ratings yet
- At-Home Vital Bleaching A Comparison of Hydrogen PeroxideDocument6 pagesAt-Home Vital Bleaching A Comparison of Hydrogen PeroxideanjozzNo ratings yet
- Maxillary DiastemDocument6 pagesMaxillary DiastemCici GustimoraNo ratings yet
- Open Bite TreatmentDocument6 pagesOpen Bite TreatmentanjozzNo ratings yet
- What Are Some Ways To Close Gaps in Your TeethDocument6 pagesWhat Are Some Ways To Close Gaps in Your TeethanjozzNo ratings yet
- Huang 17 03Document9 pagesHuang 17 03anjozzNo ratings yet
- 15840Document9 pages15840anjozzNo ratings yet
- LBM 4 Blok 17Document35 pagesLBM 4 Blok 17anjozzNo ratings yet
- Severe Gingival Recession Caused by Orthodontic Rubber Band: A Case ReportDocument5 pagesSevere Gingival Recession Caused by Orthodontic Rubber Band: A Case ReportanjozzNo ratings yet
- LBM 1 Blok 17Document21 pagesLBM 1 Blok 17anjozzNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Article Summary Assignment 2021Document2 pagesArticle Summary Assignment 2021Mengyan XiongNo ratings yet
- JDDocument19 pagesJDJuan Carlo CastanedaNo ratings yet
- (Section-A / Aip) : Delhi Public School GandhinagarDocument2 pages(Section-A / Aip) : Delhi Public School GandhinagarVvs SadanNo ratings yet
- Supreme Court Rules on Retirement Benefits ComputationDocument5 pagesSupreme Court Rules on Retirement Benefits Computationemman2g.2baccay100% (1)
- The Political Philosophy of Giorgio Agamben A Critical EvaluationDocument20 pagesThe Political Philosophy of Giorgio Agamben A Critical EvaluationLEANo ratings yet
- Evolution of The Indian Legal System 2Document7 pagesEvolution of The Indian Legal System 2Akhil YarramreddyNo ratings yet
- Term Paper On BF SkinnerDocument7 pagesTerm Paper On BF Skinnerc5rga5h2100% (1)
- Perilaku Ramah Lingkungan Peserta Didik Sma Di Kota BandungDocument11 pagesPerilaku Ramah Lingkungan Peserta Didik Sma Di Kota Bandungnurulhafizhah01No ratings yet
- LESSON 2 - Nguyễn Thu Hồng - 1917710050Document2 pagesLESSON 2 - Nguyễn Thu Hồng - 1917710050Thu Hồng NguyễnNo ratings yet
- Bhojpuri PDFDocument15 pagesBhojpuri PDFbestmadeeasy50% (2)
- STD Symptoms, Causes and PreventionDocument3 pagesSTD Symptoms, Causes and PreventionSakshi TyagiNo ratings yet
- Consolidation of AccountsDocument14 pagesConsolidation of Accountsram_alaways0% (1)
- Here Late?", She Asked Me.: TrangDocument3 pagesHere Late?", She Asked Me.: TrangNguyễn Đình TrọngNo ratings yet
- Amadora V CA Case DigestDocument3 pagesAmadora V CA Case DigestLatjing SolimanNo ratings yet
- Focus 4 Unit 2 Grammar Quiz 2.5 A GrupaDocument1 pageFocus 4 Unit 2 Grammar Quiz 2.5 A GrupaЕвгения КоноваловаNo ratings yet
- IT - Software DevelopmentDocument6 pagesIT - Software DevelopmentRubayet HassanNo ratings yet
- Dead Can Dance - How Fortunate The Man With None LyricsDocument3 pagesDead Can Dance - How Fortunate The Man With None LyricstheourgikonNo ratings yet
- XSI Public Indices Ocean Freight - January 2021Document7 pagesXSI Public Indices Ocean Freight - January 2021spyros_peiraiasNo ratings yet
- Annexure 2 Form 72 (Scope) Annexure IDocument4 pagesAnnexure 2 Form 72 (Scope) Annexure IVaghasiyaBipinNo ratings yet
- Financial Management Module - 3Document2 pagesFinancial Management Module - 3Roel AsduloNo ratings yet
- Relatório ESG Air GalpDocument469 pagesRelatório ESG Air GalpIngrid Camilo dos SantosNo ratings yet
- APP Eciation: Joven Deloma Btte - Fms B1 Sir. Decederio GaganteDocument5 pagesAPP Eciation: Joven Deloma Btte - Fms B1 Sir. Decederio GaganteJanjan ToscanoNo ratings yet
- WEEK 4 A. Family Background of Rizal and Its Influence On The Development of His NationalismDocument6 pagesWEEK 4 A. Family Background of Rizal and Its Influence On The Development of His NationalismVencint LaranNo ratings yet
- Chapter 1Document30 pagesChapter 1Sneha AgarwalNo ratings yet
- Midland County Board of Commissioners Dec. 19, 2023Document26 pagesMidland County Board of Commissioners Dec. 19, 2023Isabelle PasciollaNo ratings yet
- Invoice Inv0006: Er. Mohamed Irshadh P MDocument1 pageInvoice Inv0006: Er. Mohamed Irshadh P Mmanoj100% (1)
- Dhikr or Zikr or Remembrance of AllahDocument27 pagesDhikr or Zikr or Remembrance of AllahMd. Naim KhanNo ratings yet
- Navavarana ArticleDocument9 pagesNavavarana ArticleSingaperumal NarayanaNo ratings yet
- Analyzing Transactions To Start A BusinessDocument22 pagesAnalyzing Transactions To Start A BusinessPaula MabulukNo ratings yet
- Archives of Gerontology and Geriatrics: Naile Bilgili, Fatma ArpacıDocument7 pagesArchives of Gerontology and Geriatrics: Naile Bilgili, Fatma ArpacıIsyfaun NisaNo ratings yet