Professional Documents
Culture Documents
Mercaptopurine
Uploaded by
BigBoostingCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mercaptopurine
Uploaded by
BigBoostingCopyright:
Available Formats
DRUG STUDY AND INFORMATION FORM Generic Name: 6-Mercaptopurine Trade Name: Purinethol Drug Class: Purine Analogs
(6-Thiopurine Analogs) Structure/Chemistry: Hypoxanthine analog with S substituted for O on carbon 6 for better transport into cells
Pharmacodynamics
Mechanism of Action: Excellent substrate for hypoxanthine guanine phosphoribosyl transferase (HGPRT), which converts mercaptopurine to 6-thioinosine-5-monophosphate (TIMP). T-IMP inhibits the new formation of ribosyl-5-phosphate, as well as conversion of inosine-5-monophosphate to adenine and guanine nucleotides.
Pharmacologic Effects: Inhibits purine synthesis and also becomes incorporated into nucleic acids, thereby preventing DNA and RNA synthesis.
Drug Resistance or Tolerance: Deficiency of the activating enzyme HGPRT or increased alkaline deficiency. Other possible mechanisms of resistance include decreased drug uptake, increased drug efflux, and alteration in allosteric inhibition of ribosylamine 5-phosphate synthase.
Pharmacokinetics
Absorption: For treatment of ALL, the oral dose is 50-100 mg/m2 and is thereafter adjusted according to white blood cell and platelet counts. Oral ingestion results in only 10-50% absorption due to first-pass metabolism by xanthine oxidase in the liver. Reduce dose by 75% when giving xanthine oxidase inhibitors such as allopurinol. Distribution: Efflux system prevents mercaptopurine from reaching the brain.
Elimination: t1/2 of 50 mins in plasma after IV dose; rapidly metabolized by xanthine oxidase and thiopurine methyltransferase (TPMT)
Metabolism: Rapidly metabolized by xanthine oxidase and thiopurine methyltransferase (TPMT). Xanthine oxidase oxidizes mercaptopurine to 6-thiouric acid, an inactive metabolite. TPMT is an enzyme with many polymorphic alleles that methylates the sulfur group on mercaptopurine.
Adverse Side Effects/Toxicity: Primarily bone marrow depression (delayed with folic acid antagonists) but also anorexia, nausea, vomiting. Possibly also jaundice and hepatic enzyme elevations in one-third of patients. Predisposes to opportunistic infections and is teratogenic during first trimester. Low activity of TPMT is associated with increased toxicity. Those with autoimmune disease and low TPMT may experience bone marrow aplasia and life-threatening toxicity. Drug Interactions: Food and oral antibiotics decrease absorption. Absorption increased when combined with high-dose methotrexate. Methotrexate is synergistic by inhibiting the earliest steps of purine synthesis and by increasing the cofactor PRPP (5-phosphoribosyl-1-pyrophosphate) for mercaptopurines activation. Therapeutic uses: ALL (acute lymphoblastic leukemia)
Miscellaneous:
You might also like
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Generic Name Therapeutic Classification Pharmacologic ClassificationDocument3 pagesGeneric Name Therapeutic Classification Pharmacologic ClassificationAnselle CasilNo ratings yet
- Chapter 13. Heartburn and DyspepsiaDocument22 pagesChapter 13. Heartburn and DyspepsiaMonica CiorneiNo ratings yet
- Cancer ChemotherapyDocument19 pagesCancer ChemotherapySamatha Mohan100% (1)
- Pa Tho Physiology of ParkinsonDocument2 pagesPa Tho Physiology of Parkinsoncuriosity_killsNo ratings yet
- Ranitidine, Acetaminophen, Albuterol Drug StudyDocument5 pagesRanitidine, Acetaminophen, Albuterol Drug StudyBea Andrea LarismaNo ratings yet
- Renal Concept MapDocument8 pagesRenal Concept MapXtine CajiNo ratings yet
- ClinicalOpiateWithdrawalScale PDFDocument2 pagesClinicalOpiateWithdrawalScale PDFRajamanitiNo ratings yet
- Flucloxacillin AFTcapssolnDocument6 pagesFlucloxacillin AFTcapssolnEliza ArmanNo ratings yet
- Acute Glomerulonephritis Case StudyDocument6 pagesAcute Glomerulonephritis Case StudyjakerzNo ratings yet
- Congenital Diaphragmatic Hernia (CDH) Information For Health ProfessionalsDocument5 pagesCongenital Diaphragmatic Hernia (CDH) Information For Health ProfessionalsMangku Liong GuanNo ratings yet
- Cushings SyndromeDocument51 pagesCushings SyndromeTina TalmadgeNo ratings yet
- ICU Case Study: 53-Year-Old Male with Organophosphate PoisoningDocument11 pagesICU Case Study: 53-Year-Old Male with Organophosphate PoisoningPrasyaanth RajanNo ratings yet
- Burn Injury PathophysiologyDocument1 pageBurn Injury PathophysiologyMonique Ann DanoyNo ratings yet
- VasopressinDocument2 pagesVasopressinKim LompotNo ratings yet
- Cardiovascular PharmacologyDocument20 pagesCardiovascular PharmacologyAliceAliceNo ratings yet
- 2 Acute Myocardial InfarctionDocument15 pages2 Acute Myocardial InfarctionpauchanmnlNo ratings yet
- Critical Care Drugs 1Document21 pagesCritical Care Drugs 1Asri ErnadiNo ratings yet
- Organophosphrous PoisoningDocument53 pagesOrganophosphrous Poisoningpriyashu78100% (1)
- Infective Endocarditis CaseDocument3 pagesInfective Endocarditis CaseMershen GaniaNo ratings yet
- Toxic Megacolon: Emergency Surgery Indications for Severe ColitisDocument10 pagesToxic Megacolon: Emergency Surgery Indications for Severe ColitisVikas MataiNo ratings yet
- Hepatic Encephalopathy: Prof. Huiling Yang Dept. PathophysiologyDocument46 pagesHepatic Encephalopathy: Prof. Huiling Yang Dept. PathophysiologyAshish PandeyNo ratings yet
- Epidural Anesthesia GuideDocument3 pagesEpidural Anesthesia GuidezooNo ratings yet
- 1 Cardiac FailureDocument18 pages1 Cardiac FailurepauchanmnlNo ratings yet
- FlagylDocument3 pagesFlagylAdrianne BazoNo ratings yet
- Electrolyte DisordersDocument10 pagesElectrolyte DisordersSlavicaNo ratings yet
- Mesna: Mesna, Sold Under The BrandDocument17 pagesMesna: Mesna, Sold Under The BrandAndry HamdaniNo ratings yet
- Group 5 - Hemodialysis - Chronic Kidney FailureDocument31 pagesGroup 5 - Hemodialysis - Chronic Kidney FailureKimberly Abella CabreraNo ratings yet
- Preoperative Assessment of Diabetic PatientsDocument2 pagesPreoperative Assessment of Diabetic PatientsShilpa Pradhan100% (1)
- HHNK and DkaDocument4 pagesHHNK and Dkagoya100% (1)
- NCM 106 - Case Analysis - Nursing Care Plan of Heart FailureDocument2 pagesNCM 106 - Case Analysis - Nursing Care Plan of Heart FailureMarisol Jane JomayaNo ratings yet
- Atom EcgDocument7 pagesAtom Ecgsutan IskandarsyahNo ratings yet
- Predisposing Conditions, Management and Prevention of Chronic Kidney DiseaseDocument52 pagesPredisposing Conditions, Management and Prevention of Chronic Kidney DiseaseSaad MotawéaNo ratings yet
- A Care Bundle Approach For Prevention of Ventilator-AssociatedDocument7 pagesA Care Bundle Approach For Prevention of Ventilator-AssociatedRestu Kusuma NingtyasNo ratings yet
- Pneumonia Management ProtocolDocument2 pagesPneumonia Management Protocolsky nuts100% (1)
- Dugs CVADocument10 pagesDugs CVAMarie AntoinetteNo ratings yet
- Heparin and WarfarinDocument2 pagesHeparin and WarfarinBaeyer100% (1)
- Anti Tubercular DrugsDocument63 pagesAnti Tubercular DrugsYasir KhanNo ratings yet
- General AnestheticsDocument36 pagesGeneral AnestheticsnidyaNo ratings yet
- Bacterial Pneumonia PharmacologyDocument70 pagesBacterial Pneumonia PharmacologyMarc Imhotep Cray, M.D.No ratings yet
- NocturiaDocument10 pagesNocturiaKousik AmancharlaNo ratings yet
- Plasminogen ActivatorDocument3 pagesPlasminogen ActivatorteocriNo ratings yet
- ParkinsonDocument2 pagesParkinsongoyaNo ratings yet
- Cardiovascular: Common Lab Tests For Cardiovascular DisordersDocument49 pagesCardiovascular: Common Lab Tests For Cardiovascular Disordersesruneitak100% (1)
- ShockDocument21 pagesShockMin-Joo Esther ParkNo ratings yet
- Concept Map 1Document2 pagesConcept Map 1yfortilus100% (1)
- Pharma - Drugs Affecting Git MotilityDocument6 pagesPharma - Drugs Affecting Git MotilityBobet ReñaNo ratings yet
- CABG Annotated Bibliography and BibliographyDocument23 pagesCABG Annotated Bibliography and BibliographyCM100% (1)
- Ketorolac AHFSDocument17 pagesKetorolac AHFSRIRINo ratings yet
- CholestyramineDocument1 pageCholestyramineKatie McPeekNo ratings yet
- Radio PharmaceuticalsDocument48 pagesRadio PharmaceuticalsKris Joy EbonNo ratings yet
- Psoriatic ArthritisDocument12 pagesPsoriatic ArthritisSelvia RosadiNo ratings yet
- Case Study FinalDocument77 pagesCase Study FinalMacey Malonzo100% (1)
- Norepinephrine Drug StudyDocument2 pagesNorepinephrine Drug StudyIrish LigayaNo ratings yet
- DiflucanDocument1 pageDiflucanSheri490No ratings yet
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Obgyn Abbreviations For RotationDocument2 pagesObgyn Abbreviations For RotationBigBoostingNo ratings yet
- The Mental Status ExaminationDocument16 pagesThe Mental Status Examinationeloisa.abcedeNo ratings yet
- Guideline Watch: Practice Guideline For The Treatment of Patients With Bipolar Disorder, 2Nd EditionDocument9 pagesGuideline Watch: Practice Guideline For The Treatment of Patients With Bipolar Disorder, 2Nd EditionBigBoostingNo ratings yet
- Guideline Watch: Practice Guideline For The Treatment of Patients With Bipolar Disorder, 2Nd EditionDocument9 pagesGuideline Watch: Practice Guideline For The Treatment of Patients With Bipolar Disorder, 2Nd EditionBigBoostingNo ratings yet
- GI High YieldDocument1 pageGI High YieldBigBoostingNo ratings yet
- Triangles of The Neck Vertebral ArteryDocument6 pagesTriangles of The Neck Vertebral ArteryBigBoostingNo ratings yet
- Neurologic Presentations of HIV/AIDSDocument23 pagesNeurologic Presentations of HIV/AIDSBigBoostingNo ratings yet
- GI NotesDocument19 pagesGI NotesBigBoostingNo ratings yet
- Lectura 1 PDFDocument73 pagesLectura 1 PDFgroudon_18No ratings yet
- Psychosomatic MedicineDocument14 pagesPsychosomatic MedicineGiuseppe RutiglianiNo ratings yet
- Psychiatric Genetics: Progress Amid Controversy: Margit Burmeister, Melvin G. Mcinnis and Sebastian ZöllnerDocument14 pagesPsychiatric Genetics: Progress Amid Controversy: Margit Burmeister, Melvin G. Mcinnis and Sebastian ZöllnerBigBoostingNo ratings yet
- The Mirror Neuron System: Luigi Cattaneo, MD Giacomo Rizzolatti, MDDocument4 pagesThe Mirror Neuron System: Luigi Cattaneo, MD Giacomo Rizzolatti, MDBigBoostingNo ratings yet
- NervesDocument139 pagesNervesBigBoostingNo ratings yet
- Bone Cancer Chart 2012Document8 pagesBone Cancer Chart 2012BigBoostingNo ratings yet
- Muscles NervesDocument3 pagesMuscles NervesBigBoostingNo ratings yet
- Blue Boxes For MusculoskeletalDocument16 pagesBlue Boxes For MusculoskeletalBigBoostingNo ratings yet
- Neuro Phase Notes MS-1Document43 pagesNeuro Phase Notes MS-1BigBoostingNo ratings yet
- Cross Sections of Upper LimbDocument12 pagesCross Sections of Upper LimbBigBoostingNo ratings yet
- Neoplasias TableDocument3 pagesNeoplasias TableBigBoostingNo ratings yet
- Cranial Nerve TractsDocument2 pagesCranial Nerve TractsBigBoostingNo ratings yet
- ThalidomideDocument2 pagesThalidomideBigBoostingNo ratings yet
- CNS PharmDocument16 pagesCNS PharmBigBoostingNo ratings yet
- ProcarbazineDocument2 pagesProcarbazineBigBoostingNo ratings yet
- TretinoinDocument2 pagesTretinoinBigBoostingNo ratings yet
- RituximabDocument2 pagesRituximabBigBoosting100% (2)
- NilotinibDocument2 pagesNilotinibBigBoostingNo ratings yet
- VincristineDocument2 pagesVincristineBigBoostingNo ratings yet
- S Mechanism of Action: Inhibits Adenosine Deaminase (ADA) Which Leads To The AccumulationDocument2 pagesS Mechanism of Action: Inhibits Adenosine Deaminase (ADA) Which Leads To The AccumulationBigBoostingNo ratings yet
- OfatumumabDocument2 pagesOfatumumabBigBoostingNo ratings yet
- Benzodiazepines and Hypnotics: Key PointsDocument4 pagesBenzodiazepines and Hypnotics: Key Pointssaman mousaviNo ratings yet
- 58 PDFDocument11 pages58 PDFMay MethaweeNo ratings yet
- Paper 1 Resource PackDocument22 pagesPaper 1 Resource PackHaw Feng ChanNo ratings yet
- Adult: PO 10 MG Once Daily or 5 MG Bid. Oral: Pregnancy Category (US FDA)Document4 pagesAdult: PO 10 MG Once Daily or 5 MG Bid. Oral: Pregnancy Category (US FDA)widiyaNo ratings yet
- Dipyridamole (Cardoxin Forte)Document6 pagesDipyridamole (Cardoxin Forte)asdwasdNo ratings yet
- BioassayDocument4 pagesBioassayAddictedto Nonsense50% (2)
- Orientation To Pharmacy 2014 - Part 1Document26 pagesOrientation To Pharmacy 2014 - Part 1Khairi Mustafa Salem100% (1)
- Brand Name: Ambrolex Generic Name: Ambroxol HCL Indication: Acute andDocument2 pagesBrand Name: Ambrolex Generic Name: Ambroxol HCL Indication: Acute andianecunar100% (1)
- Dexamethasone Neomed v2.0Document4 pagesDexamethasone Neomed v2.0dian kurniasariNo ratings yet
- Medicine Lecture One General Anaethsia 19th NovDocument102 pagesMedicine Lecture One General Anaethsia 19th NovIrene Zae MwandotoNo ratings yet
- General Prescribing Guidelines For Geriatric PatientsDocument41 pagesGeneral Prescribing Guidelines For Geriatric PatientsBharath Gowda100% (1)
- Quality and Equivalence of Topical ProductsDocument5 pagesQuality and Equivalence of Topical Productsblashyrkh_79No ratings yet
- OBATDocument3 pagesOBATCindy PrayogoNo ratings yet
- 9 Mô hình hai ngăn, Không tuyến tính, PKPDDocument45 pages9 Mô hình hai ngăn, Không tuyến tính, PKPDthuong nguyen thiNo ratings yet
- Ibuprofen Oral Use Immediate Release Formulations 200 800 MG Product Specific Bioequivalence Guidance Revision 1 - enDocument3 pagesIbuprofen Oral Use Immediate Release Formulations 200 800 MG Product Specific Bioequivalence Guidance Revision 1 - enkamara.ammariNo ratings yet
- Philippine Pharmacists AssociationDocument4 pagesPhilippine Pharmacists AssociationAbby LumanglasNo ratings yet
- IRANPHARMA EXPO 2019 EXHIBITORS LIST Company Name CountryDocument28 pagesIRANPHARMA EXPO 2019 EXHIBITORS LIST Company Name CountrySajal SarkarNo ratings yet
- Safe Medicate CalculationsDocument4 pagesSafe Medicate Calculationsbe_xx1450% (8)
- U.S. Pays Nearly 4 Times More for Drugs than Other NationsDocument77 pagesU.S. Pays Nearly 4 Times More for Drugs than Other NationsjosetelhadoNo ratings yet
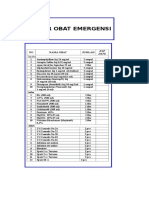
- Daftar Obat Alkes Trolley EmergencyDocument15 pagesDaftar Obat Alkes Trolley EmergencyPRIHATINNo ratings yet
- Genericsking Trading Inc Ampules Vials WholesaleDocument5 pagesGenericsking Trading Inc Ampules Vials Wholesaleapi-276695824No ratings yet
- Weekly Job AlertsDocument1 pageWeekly Job AlertsBilal Anjum ButtNo ratings yet
- Pharmacology and TherapyDocument149 pagesPharmacology and Therapydoni anandaNo ratings yet
- Review of Veterinary AntidotesDocument49 pagesReview of Veterinary AntidotesMarilena RaduNo ratings yet
- PROFESSIONAL PHARMACY PRACTICEDocument5 pagesPROFESSIONAL PHARMACY PRACTICEanon nymouseNo ratings yet
- Orange BookDocument70 pagesOrange BookAIMANIBRAHIM82No ratings yet
- Public Law 110-85 110th Congress An ActDocument156 pagesPublic Law 110-85 110th Congress An ActJames LindonNo ratings yet
- Biochemometrics and Required Tools in Botanical Natural Products Research A ReviewDocument17 pagesBiochemometrics and Required Tools in Botanical Natural Products Research A ReviewKevin WyssNo ratings yet
- Characterization of Acne Associated With UpadacitiDocument8 pagesCharacterization of Acne Associated With UpadacitiDo u know BTS?No ratings yet
- Monitored Anesthesia CareDocument22 pagesMonitored Anesthesia Caremichael100% (4)