Professional Documents
Culture Documents
AF
Uploaded by
Habiby Habibaty QolbiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AF
Uploaded by
Habiby Habibaty QolbiCopyright:
Available Formats
CARDIOLOGY PATIENT PAGE
Atrial Fibrillation
Johan E.P. Waktare, MB, ChB, MRCP
trial fibrillation (AF) is the most common cardiac arrhythmia and effects nearly 1% of the population. Its prevalence increases with increasing age; it is relatively infrequent in those under 40 years old, but occurs in up to 5% of those over 80 years of age.
can occur in people with otherwise normal hearts. Indeed, about half of younger patients with AF have no associated cardiac disorders. AF can occur with different patterns. Examples of case histories are given below to illustrate the wide clinical spectrum of AF. Paroxysmal AF In paroxysmal AF, the heart changes from sinus rhythm to AF for episodes lasting anywhere from seconds to days. The patient may only have 1 episode a year or be in AF most of the time, but the essential feature is that most episodes terminate spontaneously. Case Report: Paroxysmal AF in a Young Patient With No Other Heart Condition Patient A had no cardiac problems until she began to suffer episodes of palpitations at the age of 35. She stated that these were so bad that she thought she was going to die. Paroxysmal AF was diagnosed and drug treatment instituted. Her attacks are now much less frequent and less severe. Currently she is content to continue with drug therapy, but her cardiologist has explained that if the attacks worsen, she could be offered an ablation to try to cure the condition. Persistent AF Persistent AF does not stop spontaneously, but sinus rhythm can be restored by medical intervention in the form of medication or, more commonly, by an electrical shock to the heart (DC cardioversion). Case Report: The Vague Symptoms of Persistent AF Patient B had a severe, persistent chest infection. He became breathless walking on the smallest incline. At a routine check for his high blood pressure, his physician discovered the patient was in persistent AF. He was given anticoagulants and scheduled for a cardioversion. The cardioversion was successful, but after several days the patient showed no improvement. His physician explained that he had relapsed into AF and needed extra treatment with an antiarrhythmic medication and another cardioversion. After the second cardioversion, his effort capacity was back to normal, and 6 months later he had stopped taking the coumadin, although his 14
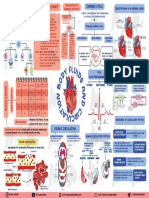
Normal Heart Electrical Activity and What Goes Wrong in AF
The heart is essentially a large muscular pump that drives blood around the body. To do this effectively, the hearts chambers must be precisely controlled electrically (Figure 1). The normal heartbeat begins with the natural pacemaker (the sinoatrial [SA] node) in the top right heart chamber (the right atrium). Activity spreads across the atria, causing them to contract. The contraction of the atria propels extra blood into the ventricles, which are the main pumping chambers. The electrical signal is delayed by about one tenth of a second by a special structure called the atrioventricular (AV) node, and then spreads rapidly across the ventricles to make them contract. Extra filling of the ventricles by the atria is not vital, but does serve to prime the ventricular pump and improve overall heart function. Normal heart rhythm is termed sinus rhythm. Most people have a resting heart rate of between 60 and 80 beats per minute (Figure 2). In AF, the atria contract rapidly and irregularly at rates of 400 to 600 beats per minute. Fortunately, the AV node will not allow many signals through to the ventricles; only about 1 or 2 out of every 3 atrial beats passes to the ventricles. The ventricles beat too fast, however, at rates of 110 to 180 beats per minute.
Who Gets AF and Patterns of AF
Cardiac disorders such as coronary heart disease, heart valve problems, and heart failure predispose patients to AF, but it
From the Cardiology Department, University Hospital Birmingham, Edgebaston, Birmingham, UK. Correspondence to Dr Johan E.P. Waktare, Cardiology Department, University Hospital Birmingham, Edgebaston, Birmingham, B15 2TH, UK. E-mail jwaktare@blueyonder.co.uk (Circulation. 2002;106:14-16.) 2002 American Heart Association, Inc. Circulation is available at http://www.circulationaha.org DOI: 10.1161/01.CIR.0000022730.66617.D9
Waktare
Atrial Fibrillation
15
risk of this occurring is greatly reduced by appropriate treatment. Adverse Symptoms Most, but not all, patients feel unwell with AF. It is not fully understood why the symptomatic impact is so variable. Palpitations (a sensation of a rapid and irregular heart beat) are the most frequent symptoms in those with paroxysmal AF. This can cause the patient to worry that they will have a heart attack or that their heart will stop. This rarely occurs, but urgent medical advice should be sought for any new cardiac symptom so that a precise diagnosis can be made. Those with persistent or permanent AF tend to notice palpitations less, perhaps because the heartbeat is constantly irregular. The switching back and forth between regular and irregular rhythms is what causes palpitations in many patients. When AF is persistent or permanent, patients more often suffer non-specific symptoms like poor effort tolerance, breathlessness on exertion, and lack of energy. Stroke The quivering atria beat too rapidly to contract effectively, and with time they tend to enlarge. Both of these factors can lead to blood clots forming within the atria, and if these break loose they may lodge in other parts of the circulation. The most common site for this is the brain, and this results in a stroke. Heart failure If the ventricles are allowed to beat rapidly for prolonged periods, they can weaken, and heart failure ensues. This is a rare complication, as most patients seek treatment before heart failure occurs. However, AF is a less efficient rhythm than sinus rhythm and can worsen preexisting heart failure.
Figure 1. The atria contain the hearts natural pacemaker, the SA node, and are the part of the heart affected by atrial brillation. The ventricles are the muscular part of the heart that actually pump the blood. They are electrically isolated from the atria, and the only way the electrical signal can reach them is via the AV node.
physician recommended that he stay on the antiarrhythmic medication for at least 2 years. Permanent AF Permanent AF is present all the time, and restoring sinus rhythm is either not possible or is not deemed appropriate. Case Report: Ablate and Pace for Permanent AF Patient C was elderly and had suffered from AF for many years. She had been cardioverted, but after consulting her physician, she decided to accept permanent AF. The problem was that her heart rate was still too fast despite rate limiting drugs. Her physician recommended AV nodal ablation and pacemaker implantation. After these procedures she felt much better. She is still taking coumadin but she has stopped all the other medication, and she reports that she feels better than she has for years.
Treatments Available for AF
AF is a very diverse condition effecting a wide range of patients, so there are few generalizations about what treatment is needed. With recent advances in drug and interventional treatments, a satisfactory outcome is now usually eventually obtained in most patients. DC Cardioversion DC cardioversion is used to restore sinus rhythm in those with persistent AF. A brief general anesthetic is given intravenously and a defibrillator (the electrical shocking device used to treat cardiac arrest) is used to put the heart back into normal rhythm. The treatment is highly effective, with over 90% of patients reverting to sinus rhythm. Over the ensuing hours, days, and months, however, patients may relapse into AF. Rate Limiting Drugs Rate limiting drugs limit the number of impulses transmitted through the AV node (Figure 2) and slow the heart rate to make the patient more comfortable. Antiarrhythmic Drugs In patients with paroxysmal AF, antiarrhythmic drugs reduce the frequency and duration of AF episodes. In those with persistent AF, they are administered primarily to prevent AF recurring after a DC cardioversion.
Is AF Bad for You?
For most people, AF causes unpleasant symptoms but causes no harm. Complications can arise in some patients, but the
Figure 2. A, Sinus rhythm. During normal sinus rhythm, the heartbeat is a single carefully coordinated process beginning in the SA node (1). The electrical signal spreads across the atria (2) and via the AV node (3) to the ventricles (4). B, Atrial brillation. When patients are in AF, the atria are constantly activating in a chaotic way because of multiple electrical signals ring at 400 to 600 beats per minute (1). The AV node (2) lters out most of these extra signals but still usually allows more beats to reach the ventricles than normal (3).
16
Circulation
July 2, 2002
Radiofrequency Ablation and Surgery Over the last 10 years, ablation has emerged as the optimal treatment for most forms of rapid heart rhythm, but its use in curing AF is very recent. As opposed to ablation of the AV node, the technique of radiofrequency ablation here refers to selective elimination of one or more sites in the atria to reduce the chance that AF will occur. Procedures for AF are currently prolonged and complex, and success rates only modest. It is therefore not always the best option; however, when it works, the AF is cured completely. Surgical approaches for curing AF are also considered in some cases. Reassurance and Explanation The importance of reassurance and explanation cannot be over-emphasized. Relatively simple treatment reduces enormously the risk of harm for those with persistent or permanent AF. Patients with infrequent episodes of short-lived paroxysmal AF may need no other treatment than proper evaluation followed by reassurance that the condition is benign. Finally, those with AF that is difficult to control need to be involved in decisions regarding which of the emerging treatments should be used and be reassured that, with time, satisfactory control of the AF can be achieved.
Anticoagulant and Antiplatelet Drugs Anticoagulant and antiplatelet medications thin the blood and make it less prone to clotting, thereby reducing the risk of stroke. Coumadin (warfarin) is the usual medication used but is not suitable or necessary for all patients. In these cases, aspirin or clopidogrel may be used, but if the risk of stroke is very small, no treatment may be recommended. Pacemakers Those patients whose natural pacemaker (SA node) is failing become prone to AF, and implanting a pacemaker can have the beneficial side effect of reducing the chance that AF will occur. Pacemakers can be used in combination with ablation of the AV node to treat AF. Ablation refers to a medical procedure where a very small (1 to 2 mm) portion of the hearts electrical conduction system (for example, the AV node) is eliminated in a carefully controlled fashion. This so-called ablate and pace strategy is usually highly effective at improving symptoms, but has drawbacks such as life-long requirement for anticoagulation and for pacemaker treatment.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Cardiovascular MneumonicsDocument10 pagesCardiovascular MneumonicsKaly RieNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Atrial FibrillationDocument19 pagesAtrial FibrillationAnwari MuhammadNo ratings yet
- Zoology Full PDF EMDocument108 pagesZoology Full PDF EMSmiruthi RavichandranNo ratings yet
- Blood Flow Through The HeartDocument2 pagesBlood Flow Through The HeartZah SchlafmützeNo ratings yet
- General.: Blood CirculationDocument3 pagesGeneral.: Blood CirculationJessica MichaelNo ratings yet
- PREECLAMPSIADocument60 pagesPREECLAMPSIAMary Grace MasNo ratings yet
- Pediatric Cardiovascular DisordersDocument9 pagesPediatric Cardiovascular Disorderscayla mae carlos0% (1)
- Analogue New Tools Challange Diabetes (Slide)Document67 pagesAnalogue New Tools Challange Diabetes (Slide)Habiby Habibaty QolbiNo ratings yet
- Novomix Tawang Mangu SW 12 Mei 2012Document39 pagesNovomix Tawang Mangu SW 12 Mei 2012Habiby Habibaty QolbiNo ratings yet
- Analogue New Tools Challange Diabetes (Slide)Document67 pagesAnalogue New Tools Challange Diabetes (Slide)Habiby Habibaty QolbiNo ratings yet
- Basal Insulin TreatmentDocument33 pagesBasal Insulin TreatmentHabiby Habibaty QolbiNo ratings yet
- Workshop Residen 1Document2 pagesWorkshop Residen 1Habiby Habibaty QolbiNo ratings yet
- Gagal Ginjal Akut Dan Kronik: Divisi Ginjal & Hipertensi SMF/Lab - Ilmu Penyakit Dalam FK - UNS / RSUD DR - MoewardiDocument29 pagesGagal Ginjal Akut Dan Kronik: Divisi Ginjal & Hipertensi SMF/Lab - Ilmu Penyakit Dalam FK - UNS / RSUD DR - MoewardiHabiby Habibaty QolbiNo ratings yet
- Workshop Residen 1Document2 pagesWorkshop Residen 1Habiby Habibaty QolbiNo ratings yet
- GESTASIONAL DIABETES MELLITUS SimposiumDocument18 pagesGESTASIONAL DIABETES MELLITUS SimposiumHabiby Habibaty QolbiNo ratings yet
- Student Registration List with Personal DataDocument8 pagesStudent Registration List with Personal DataHabiby Habibaty QolbiNo ratings yet
- 30-8 Final Ann Konker, PIT, Treg CetakDocument4 pages30-8 Final Ann Konker, PIT, Treg CetakHabiby Habibaty Qolbi100% (1)
- The Role of Rapid Acting Analogue in Basal-Bolus StrategyDocument39 pagesThe Role of Rapid Acting Analogue in Basal-Bolus StrategyHabiby Habibaty QolbiNo ratings yet
- Denah Kampus A UNAIRDocument1 pageDenah Kampus A UNAIRHabiby Habibaty QolbiNo ratings yet
- Takmir MasjidDocument5 pagesTakmir MasjidHabiby Habibaty QolbiNo ratings yet
- Cancers Related To Immunodeficiencies: Update and PerspectivesDocument13 pagesCancers Related To Immunodeficiencies: Update and PerspectivesHabiby Habibaty QolbiNo ratings yet
- Pi Is 0091674917309259Document8 pagesPi Is 0091674917309259Habiby Habibaty QolbiNo ratings yet
- Acute Coronary Syndrome: Widhy Puji H Bahan: - Pathophysiology of Heart Disease - ACS AHA 2010 - ACS AHA 2013Document17 pagesAcute Coronary Syndrome: Widhy Puji H Bahan: - Pathophysiology of Heart Disease - ACS AHA 2010 - ACS AHA 2013Habiby Habibaty QolbiNo ratings yet
- 3 Acute Coronary SyndromeDocument57 pages3 Acute Coronary SyndromestephaniedianNo ratings yet
- Insulin GarglineDocument28 pagesInsulin GarglineHabiby Habibaty Qolbi100% (1)
- Everything You Need to Know About Spine ExaminationDocument41 pagesEverything You Need to Know About Spine ExaminationHabiby Habibaty QolbiNo ratings yet
- HIP and BackDocument48 pagesHIP and BackHabiby Habibaty QolbiNo ratings yet
- Notes PediaDocument56 pagesNotes PediaDick Morgan FerrerNo ratings yet
- Circulatory System Packet BDocument5 pagesCirculatory System Packet BLouise SalvadorNo ratings yet
- Unit 4 (4) STRUCTURE & FUNCTION OF THE MAMMALIAN HEARTDocument9 pagesUnit 4 (4) STRUCTURE & FUNCTION OF THE MAMMALIAN HEARTDINAMANI 0inamNo ratings yet
- CARDIAC TUMORS Approach To ManagementDocument12 pagesCARDIAC TUMORS Approach To ManagementAnkit GulatiNo ratings yet
- Austin Journal of Clinical CardiologyDocument15 pagesAustin Journal of Clinical CardiologyAustin Publishing GroupNo ratings yet
- Lesson 5 - Respiratory and Circulatory SystemsDocument60 pagesLesson 5 - Respiratory and Circulatory SystemsBeng QuinnNo ratings yet
- Sean Burke - Virtual-Shark-Dissection QuestionsDocument5 pagesSean Burke - Virtual-Shark-Dissection Questionsapi-386190429No ratings yet
- REGULATION OF CARDIAC ACTIVITYDocument1 pageREGULATION OF CARDIAC ACTIVITYservoculus machatteNo ratings yet
- SWC12Document11 pagesSWC12vikkasNo ratings yet
- 3 MAJOR OPENINGS /right Atirum: Cardiovascular System Serious PericardiumDocument3 pages3 MAJOR OPENINGS /right Atirum: Cardiovascular System Serious PericardiumAebee Alcaraz100% (1)
- Anatomi Dan Fisiologi Sistem Kardiovaskular: Hendra FirmansyahDocument19 pagesAnatomi Dan Fisiologi Sistem Kardiovaskular: Hendra Firmansyahrandy sepasaciNo ratings yet
- DLL SCI9circulatory2Document2 pagesDLL SCI9circulatory2Mantikar IsmaelNo ratings yet
- Normal Oxygen Transport: Susanne A ClarkDocument256 pagesNormal Oxygen Transport: Susanne A Clarkghoncheh0% (1)
- DM Cardiology (Medicine) June 2018 PDFDocument17 pagesDM Cardiology (Medicine) June 2018 PDFAnil SharmaNo ratings yet
- 4 EL Husseinys Essentials of Cardiovascular System @eduwaves360Document236 pages4 EL Husseinys Essentials of Cardiovascular System @eduwaves360ahmed_abu_alrobNo ratings yet
- Circulatory System ReadingDocument4 pagesCirculatory System ReadingAlejandro PabonNo ratings yet
- Heart Anatomy LabDocument19 pagesHeart Anatomy LabDisshiNo ratings yet
- CARDIAC ARRHYTHMIA GUIDEDocument44 pagesCARDIAC ARRHYTHMIA GUIDEChinenye Akwue100% (1)
- Test Bank For Ekg Plain and Simple 3rd Edition EllisDocument8 pagesTest Bank For Ekg Plain and Simple 3rd Edition Elliscanebrutalfniy66No ratings yet
- Association Rule Mining To Detect Factors Which Contribute To Heart Disease in Males and Females 2013Document8 pagesAssociation Rule Mining To Detect Factors Which Contribute To Heart Disease in Males and Females 2013Great Ideas in 5 Minutes افكارعظيمة في 5 دقائقNo ratings yet
- MN - B4 Revision LessonDocument34 pagesMN - B4 Revision Lessonspamzz063No ratings yet
- Medicine National Competitive Entrance Examination 2018Document13 pagesMedicine National Competitive Entrance Examination 2018lalixs71No ratings yet
- Heart: Answers To Workbook ActivitiesDocument12 pagesHeart: Answers To Workbook Activitiesapi-20954241433% (3)