Professional Documents
Culture Documents
Bicipital Tendonitis: Lyn Paul Taylor, B.A., M.A., R.P.T
Uploaded by
gschiroOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bicipital Tendonitis: Lyn Paul Taylor, B.A., M.A., R.P.T
Uploaded by
gschiroCopyright:
Available Formats
BICIPITAL TENDONITIS
Lyn Paul Taylor, B.A., M.A., R.P.T.
(Editing Assistant and Computer Consultant: Joanna Soon, B.S.)
The biceps brachii muscle is formed from two heads placed along the anterior aspect of
the humerus. The short head originates as a thick flattened tendon from the apex of the coracoid process that it shares with the coracobrachialis muscle. The long head originates as a tendon from the supraglenoid tuberosity on the superior margin of the glenoid cavity. This origin occurs within the shoulder capsule and the initial segment of the tendon is enclosed in a synovial sheath. The tendon continues distally, arching over the head of the humerus and running down the intertubercular groove (sulcus) under the transverse humeral ligament and a fibrous prolongation from the pectoralis major tendon. It emerges from the shoulder capsule close to the humeral attachment of the capsular ligament, eventually attaching to its muscle belly. Each biceps head maintains a separate identity until they are within approximately 7.5 cm of the elbow joint. At this point, they become confluent and continue to end in a flattened tendon that inserts on the posterior portion of the radial tuberosity. A broad aponeurosis arises from the tendon medially to pass obliquely across the brachial artery, to become continuous with the deep fascia covering the origins of the flexor muscles originating on the forearm. Historically bicipital tendonitis has been defined as an inflammation of the tendon of the long head of the biceps brachii. It occurs most commonly to women in their early forties, but may occur to either gender at any adult age. An acute episode is generally brought on by strenuous activity (skiing, tennis, shoveling) following on the heels of long term wear and tear, degenerative changes in the tendon or the intertubercular groove (roughening of the channel). Recent authorities have suggested that bicipital tendonitis is misnamed and is, in fact, a bicipital tenosynovitis. They suggest that the inflammation occurs to the tendon sheath within the bicipital groove and not to the tendon itself, and offer as proof the frequent adhesions that form in the tendon's sheath. Regardless of which structures are involved, bicipital tendonitis initially demonstrates itself through pain when the arm is internally or externally rotated and placed either behind the back or above the head. Usually the pain first occurs over the anterior medial region of the shoulder and then radiates to the belly of the biceps muscle and distal to the flexor surface of the forearm. Some subjects may complain of additional pain radiating into the deltoid insertion, into the inferior angle of the scapula, or to the base of the neck. Digital probing of the intertubercular groove will elicit exquisite pain as will rolling the tendon between the fingers. The pain is aggravated by active supination of the forearm against resistance and active contraction or passive stretching of the biceps muscle.
The pain produced by bicipital tendonitis may limit the subject's ability to use the shoulder. Functional activities may be curtailed insofar as the patient may be unable to put on a shirt or lift anything that requires two hands. Even driving a car or brushing the teeth may be difficult. It should be noted that in spite of some orthopaedic opinions to the contrary, differential skin resistance (DSR) survey has demonstrated that inflammation may also occur to the short head's tendon. If it does, it usually occurs along with inflammation of the long head tendon (though exceptions have been found). Generally, the inflamed zone will extend distally two or three inches from the glenohumeral joint, and medially two inches from the lateral margin of the intertubercular groove along the path of the pectoralis major tendon (not pictured).
The high skin resistance pattern commonly associated with Bicipital Tendonitis (of the lateral tendon)
Treatment
Treatment should be directed at relieving any inflammation, and eliminating any
adhesions, that may be present. Application: A DSR survey should be performed to establish the existence of any inflamed zones.
The inflamed zone should be electrically stimulated. The electrical stimulator should first be preset to deliver wide-pulsed galvanic current at six cycles per second (Hz) for a ten-minute period. The negative electrode should be placed over the inflamed zone and the positive over the lower trapezius muscle, on the same side. The machine should be turned on and its amplitude gradually increased to produce visible bouncing contractions of the biceps. Following this stimulation, the electrical stimulation unit should then be preset to provide a medium frequency waveform, with a duty cycle of ten-seconds on and ten-seconds off. The electrodes should remain where they are. The stimulator should be turned on and the amplitude gradually increased until brisk maintainedcontractions of the biceps can be observed. The stimulation should continue for ten-minutes (refer to ELECTRICAL STIMULATION). The inflamed zone, and adjacent tissues, should be manipulated to eliminate any adhesions that are present. Successful manipulation should provide immediate restoration of normal or near normal ranges of motion in the shoulder joint (refer to SOFT TISSUE MANIPULATION). Phonophoresis of an effective non-steroid anti-inflammatory should be performed over the inflamed zone (topical ibuprofen is favorite). The ultrasound unit should be preset to provide a 1 Mhz pulsed waveform, for six minutes, at 1.5 W/cm (refer to ULTRAHIGH FREQUENCY SOUND, Precautions).
If bicipital tendonitis is the only component, the patient should, in most cases, be completely relieved of the bicipital tendonitis syndrome in one or two treatment sessions. Trigger Points:
The following trigger point formations may, singly or in combination, refer pain into
the areas usually affected by bicipital tendonitis: Levator scapulae, Scalenus, Scalenus (minimus), Infraspinatus, Infraspinatus (abnormal), Medial teres major, Lateral teres major, Coracobrachialis, Lower trapezius [A], Cervical multifidus (C4-C5), Supraspinatus (muscle), Supraspinatus (tendon), Subclavius, Posterior deltoid, Anterior deltoid, Pectoralis major, Pectoralis major (sternal portion), Pectoralis minor, Sternalis, Rhomboids, Biceps brachii, Brachialis, Palmaris longus, Flexor carpi radialis, Brachioradialis, Pronator teres, Multifidus (T4-T5), and Iliocostalis thoracis (T6). References:
C.M. Goss, Gray's Anatomy, Lea and Febiger, Philadelphia, Pa., 1968. p. 463 Merck Manual of Diagnosis and Therapy, Merck & Co., Inc., Pittsburgh, Pa., 1968. p. 1267 R.B. Salter, Textbook of Disorders and Injuries of the Musculoskeletal System, Williams & Wilkins, Baltimore, Md., 1983. p. 243 W.N. Scott, B. Nisonson and J.A. Nicholas, Principles of Sports Medicine, Williams & Wilkins, 1984. p. 120 A.R. Shands and R.B. Raney, Handbook of Orthopaedic Surgery, The C.V. Mosby Co., Saint Louis, Mo., 1967. Pp. 425-426 L.P. Taylor, T. Hui, The Taylor Technique of Soft Tissue Management, Inflammation: Evaluation & Treatment, 2002. Pp. 252-254
You might also like
- Elbow and Antebrachium NotesDocument8 pagesElbow and Antebrachium NoteschadNo ratings yet
- Some From Snells Upper Limb More Condensed 11oct2023 Prepation of Upper Limb CatDocument9 pagesSome From Snells Upper Limb More Condensed 11oct2023 Prepation of Upper Limb Catmwizerwaemmanuel7No ratings yet
- Physical Therapy For Sports Injuries (2012-2013)Document66 pagesPhysical Therapy For Sports Injuries (2012-2013)Mohammad EsmatNo ratings yet
- Impingement Syndrome: Epidemiology, Prevalance and IncidenceDocument6 pagesImpingement Syndrome: Epidemiology, Prevalance and Incidencemona khosraviNo ratings yet
- Upper Limb Joints & Muscles Clinical AnatomyDocument92 pagesUpper Limb Joints & Muscles Clinical Anatomygechanatomy100% (1)
- Arm anatomy and nerve supplyDocument116 pagesArm anatomy and nerve supplyHaania KhanNo ratings yet
- AnatomyRotatorCuff StatPearls NCBIBookshelfDocument7 pagesAnatomyRotatorCuff StatPearls NCBIBookshelfPraneeth KumarNo ratings yet
- Shoulder PainDocument6 pagesShoulder Painjrice003No ratings yet
- Supracondylar Humerus#Document56 pagesSupracondylar Humerus#Shisam PoudelNo ratings yet
- 7 Question OrthopaedyDocument11 pages7 Question OrthopaedyFadliArifNo ratings yet
- PBL 1 - Rotator CuffDocument11 pagesPBL 1 - Rotator CuffEmmanuel Saka100% (1)
- Upper Extremity Pain - Jack L RookDocument60 pagesUpper Extremity Pain - Jack L RookShauki AliNo ratings yet
- Project K Sciatic Nerve Pre Final Copy 2Document27 pagesProject K Sciatic Nerve Pre Final Copy 2Deepak NemaniNo ratings yet
- AnatomyDocument29 pagesAnatomyazeemNo ratings yet
- Ulnar Nerve Examination For Ulnar Nerve PalsyDocument14 pagesUlnar Nerve Examination For Ulnar Nerve Palsyalimran MahmudNo ratings yet
- Ulnar Nerve: Submitted To: Dr. Gurpreet Kaur. Submitted By: Manmeet Kaur BPT-7th Sem 16204124Document33 pagesUlnar Nerve: Submitted To: Dr. Gurpreet Kaur. Submitted By: Manmeet Kaur BPT-7th Sem 16204124Jagraj singhNo ratings yet
- Elbow ligaments and joint ultrasoundDocument9 pagesElbow ligaments and joint ultrasoundGhofran Ibrahim HassanNo ratings yet
- ANATOMY OF TRICEPSDocument5 pagesANATOMY OF TRICEPSspacefitnesscurepipeNo ratings yet
- Prometric ReviewerDocument134 pagesPrometric ReviewerWilyam SerilNo ratings yet
- Anatomia Clinica KneeDocument17 pagesAnatomia Clinica KneeMauricio OjedaNo ratings yet
- 47 High Yield RecallDocument45 pages47 High Yield Recallpriyarajan007No ratings yet
- ElbowDocument52 pagesElbowAbdallah Samir Mostafa٢٠١٩٠٢١٥٩No ratings yet
- Median NerveDocument40 pagesMedian Nervehumera100% (2)
- Splinting For Peripheral Nerve Injuries-PPT (2023)Document49 pagesSplinting For Peripheral Nerve Injuries-PPT (2023)KarisiNo ratings yet
- الفصل الثاني محاضرات PDFDocument20 pagesالفصل الثاني محاضرات PDFAZOZ 19No ratings yet
- Group 5Document70 pagesGroup 5Kathlene PamaNo ratings yet
- 15 - Mahima Bhatia - Radial Nerve InjuryDocument19 pages15 - Mahima Bhatia - Radial Nerve InjuryApoorvNo ratings yet
- TSP and RibsDocument7 pagesTSP and Ribsapi-238049665No ratings yet
- FasciotomyDocument17 pagesFasciotomyPrasojo JojoNo ratings yet
- Elbow Joint & Anastomosis Around Elbow Joint: ObjectivesDocument7 pagesElbow Joint & Anastomosis Around Elbow Joint: Objectiveschittsat39610% (1)
- New Biomechanics of Elbow - Wrist JointDocument33 pagesNew Biomechanics of Elbow - Wrist JointFatima AnjumNo ratings yet
- Clinical Anatomy of Upper Limb: Bones, Joints, Nerves & MusclesDocument22 pagesClinical Anatomy of Upper Limb: Bones, Joints, Nerves & MusclesgggghcNo ratings yet
- The OneDocument436 pagesThe OneSheena ChenNo ratings yet
- Anatomy of The Cubital FossaDocument10 pagesAnatomy of The Cubital FossaDaniella AwurumibeNo ratings yet
- Case Based Learning: I Hate AnatomyDocument9 pagesCase Based Learning: I Hate AnatomyHamza AhmedNo ratings yet
- Musculoskeletal and neurological anatomyDocument220 pagesMusculoskeletal and neurological anatomyRaymond Bernatowicz100% (2)
- Shoulder Joint Guide: Rotator Cuff, Movements & Common InjuriesDocument7 pagesShoulder Joint Guide: Rotator Cuff, Movements & Common InjuriesMary Grace OrozcoNo ratings yet
- Rotator Cuff Injury RehabilitationDocument29 pagesRotator Cuff Injury RehabilitationArko duttaNo ratings yet
- Approaches: 1. Anterior 2. Anterolateral 3. Lateral 4. PosteriorDocument25 pagesApproaches: 1. Anterior 2. Anterolateral 3. Lateral 4. PosteriorMelody JusticeNo ratings yet
- Elbow Joint Movements, Ligaments and Common InjuriesDocument26 pagesElbow Joint Movements, Ligaments and Common InjuriesAngelic khanNo ratings yet
- Summary Topographic Anatomy, Extras and Muscles To 1 Proof!!Document10 pagesSummary Topographic Anatomy, Extras and Muscles To 1 Proof!!Geovanna FernandesNo ratings yet
- Nerve Supply Upper ArmDocument13 pagesNerve Supply Upper Armdr.mumtazhussain78No ratings yet
- 1.5 DermatomesDocument2 pages1.5 DermatomesAngela CaguitlaNo ratings yet
- COMLEX OMM Shelf ReviewDocument373 pagesCOMLEX OMM Shelf ReviewJohn Doe60% (5)
- Lecture 4 Medical TerminologyDocument38 pagesLecture 4 Medical TerminologyAhmed KhaledNo ratings yet
- Gross Anatomy of The Forearm: A CAL Package Designed By-Pratik SinhaDocument24 pagesGross Anatomy of The Forearm: A CAL Package Designed By-Pratik SinhaManvi JogiNo ratings yet
- Knee Injury: By: Haspreet GillDocument18 pagesKnee Injury: By: Haspreet GillRoshandiep GillNo ratings yet
- Kuliah Kelainan PeriartikulerDocument20 pagesKuliah Kelainan PeriartikulerRoby KieranNo ratings yet
- Modul PlusDocument64 pagesModul PlusMuhamad BenyaminNo ratings yet
- Surgical Approaches ElbowDocument68 pagesSurgical Approaches ElbowPrakash AyyaduraiNo ratings yet
- Volkmann's Ischemic ContractureDocument41 pagesVolkmann's Ischemic ContractureKrishna Madhukar91% (11)
- Nerve InjuryDocument19 pagesNerve Injurybhavesh jain100% (2)
- Ali Danish DD PresentaionDocument13 pagesAli Danish DD PresentaionAli DanishNo ratings yet
- KneeDocument29 pagesKneedoctoradeeb18No ratings yet
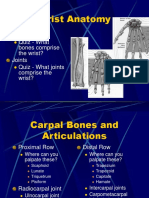
- Wrist Anatomy: Bones Quiz - What Bones Comprise The Wrist? Joints Quiz - What Joints Comprise The Wrist?Document63 pagesWrist Anatomy: Bones Quiz - What Bones Comprise The Wrist? Joints Quiz - What Joints Comprise The Wrist?Mnn SaabNo ratings yet
- Upper Limb Rapid RevisionDocument27 pagesUpper Limb Rapid RevisionIvarAtpugNo ratings yet
- Chap 8 - DiathermyDocument39 pagesChap 8 - DiathermyDavid SugiartoNo ratings yet
- SWDDocument8 pagesSWDshibuphysioNo ratings yet
- SLAP LesionDocument10 pagesSLAP LesionShibu MuhammadNo ratings yet
- MPT Syallbus For RGUHSDocument43 pagesMPT Syallbus For RGUHSWasemBhatNo ratings yet