Professional Documents
Culture Documents
Aac00083 0113
Uploaded by
Mossaab EZ Aldeen ArwanyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aac00083 0113
Uploaded by
Mossaab EZ Aldeen ArwanyCopyright:
Available Formats
ANTIMICROBIAL AGENTS AND CHEMOTHERAPY, Apr. 1988, p.
503-509
Vol. 32, No. 4
0066-4804/88/040503-07$02.00/0 Copyright C) 1988, American Society for Microbiology
Pharmacokinetics of Cefoperazone (2.0 g) and Sulbactam (1.0 g) Coadministered to Subjects with Normal Renal Function, Patients with Decreased Renal Function, and Patients with End-Stage Renal Disease on Hemodialysis
DONALD P. REITBERG,' DWIGHT A. MARBLE,2 ROBERT W. SCHULTZ,3 THOMAS J. WHALL,4 AND JEROME J. SCHENTAG2,5* Department of Pharmaceutics and Division of Clinical Pharmacy Sciences, School of Pharmacy, State University of New York at Buffalo,2 and Department of Medicine3 and Clinical Pharmacokinetics Laboratory,5 Millard Fillmore Hospital, Buffalo, New York 14209; Department of Clinical and Scientific Affairs, Pfizer Incorporated, New York, New York 100171; and Quality Control Division, Pfizer Incorporated, Groton, Connecticut 063404
Received 19 September 1987/Accepted 5 January 1988 The single-dose pharmacokinetics of intravenously administered cefoperazone (2.0 g) and sulbactam (1.0 g) were studied in normal subjects and in patients with various degrees of renal failure. In an open, parallel experimental design, six normal subjects (creatinine clearance, greater than 90 ml/min), two patients with mild renal failure (creatinine clearance, 31 to 60 mI/min), eight patients with moderate renal failure (creatinine clearance, 7 to 30 ml/min), and four functionally anephric patients (creatinine clearance, less than 7 mI/min) were studied. The functionally anephric patients were given two test doses to allow study of drug disposition both on and off hemodialysis. Serial blood and urine samples were collected from time zero to 12 h after dosing in normal subjects and from 0 to 72 h in renal patients. Serum concentrations of both drugs declined biexponentially. For cefoperazone, the terminal elimination half-lives averaged from 1.6 to 3.0 h and were similar in subjects and patients. No cefoperazone pharmacokinetic parameters were appreciably altered by renal failure or hemodialysis, and there was no correlation between the total body clearance of cefoperazone and estimated creatinine clearance. In contrast, the sulbactam total body clearance was highly correlated with estimated creatinine clearance (r = 0.92, P < 0.01) and was significantly higher in normal volunteers than in the renally impaired groups (P < 0.01). The sulbactam terminal elimination half-life in functionally anephric patients (9.7 5.3 h) differed significantly from that of normal volunteers (1.0 0.2 h) and patients with mild renal failure (1.7 0.7 h, P < 0.05). The sulbactam half-life in moderate renal failure was 4.6 2.2 h. The hemodialysis extraction ratio of sulbactam (0.44) was significantly higher than that of cefoperazone (0.05) (P < 0.01). The mean percentage of the dose recovered from dialysate was about 4% for cefoperazone and 30% for sulbactam. Hemodialysis patients showed a significantly higher sulbactam apparent volume of distribution at steady state and total body clearance during dialysis periods when compared with those in periods off dialysis. The sulbactam elimination half-life was appreciably altered during the hemodialysis period (mean, 2.0 h). Hemodialysis approximately doubled the sulbactam total body clearance. When cefoperazone and sulbactam are used in combination, adjustment of the dosing regimen for patients with estimated creatinine clearance of less than 30 ml/min can be made to compensate for reduced sulbactam total body clearance. An adjustment may be particularly appropriate at an estimated creatinine clearance of less than 15 ml/min. Under these conditions, the combination may be given once daily, with an additional dose of cefoperazone (given alone) 12 h later. This alternating regimen would not require further adjustment after hemodialysis treatment, but we recommend that dosing be scheduled to follow hemodialysis if possible.
Sulbactam is a P-lactamase inhibitor currently marketed in the United States in combination with ampicillin. With the exception of potent in vitro activity against Neisseria gonorrhoeae and Acinetobacter species (R. A. Venezia, D. Pisegna-Swift, G. E. Hollick, and W. W. Gregory, Abstr. Annu. Meet. Am. Soc. Microbiol. 1986, A90, p. 16), sulbactam lacks significant antibacterial activity as a single agent (7). Cefoperazone (Cefobid; Roerig Div., Pfizer Pharmaceuticals) is a marketed cephalosporin with a broad spectrum of activity against most gram-positive and gram-negative bacteria including Pseudomonas aeroginosa and most members of the family Enterobacteraceae (15). In vitro, the combination of cefoperazone and sulbactam shows a marked degree
*
Corresponding author.
503
of synergy against some organisms which are resistant to cefoperazone, including Enterobacter species, Serratia marcescens, Acinetobacter species, and Bacteroides fragilis (11). For this reason, simultaneous administration of cefoperazone and sulbactam may improve therapeutic outcome under certain clinical conditions. The objective of this study was to compare the pharmacokinetic profiles of primarily hepatically eliminated cefoperazone and renally eliminated sulbactam coadministered as an intravenous infusion to normal volunteers, to patients with various degrees of renal dysfunction, and to hemodialysis patients both during and between hemodialysis treatments. These data are utilized to provide dosage guidelines for the drug combination when administered to patients with normal renal function and to patients with various degrees of renal dysfunction.
504
REITBERG ET AL.
ANTIMICROB. AGENTS CHEMOTHER.
MATERIALS AND METHODS
Subjects. After subjects gave informed consent, the pharmacokinetics of cefoperazone and sulbactam given in combination were studied in six normal volunteers and 14 patients with various degrees of renal dysfunction. All subjects in this investigation were studied at a single site. There were 19 men and 1 woman, ranging in age from 21 to 71. Excluded from the study were premenopausal women and patients with evidence or history of hepatic disease, unstable congestive heart failure, endocrine disorders (except well-controlled diabetes), malignancy, allergy to penicillins or cephalosporins, blood dyscrasias, and drug or alcohol abuse. Renal dysfunction patients not requiring hemodialysis were divided into two groups based on estimated creatinine clearance (CLCR) (4). Before and upon completion of the study, the laboratory examinations performed included complete blood count with differential, blood chemistry screening, and urinalysis. Drug administration and blood sampling. After they fasted for at least 8 h, all subjects were given a single, simultaneous 15-min intravenous infusion of 2.0 g of cefoperazone and 1.0 g of sulbactam. Blood samples were collected from an indwelling venous catheter in the arm contralateral to the one into which the drug combination was infused. Samples were collected immediately before drug administration, at the midpoint and at the end of the infusion, 15 and 30 min postinfusion, and 1, 1.5, 2, 4, 6, 8, and 12 h postinfusion. Additional blood samples were collected at 24 and 48 h postinfusion from renal failure patients, and a 72-h sample was obtained from patients on hemodialysis. Patients requiring maintenance hemodialysis were administered the drug combination twice; once on a day of hemodialysis (during-dialysis dose) and once on a day after hemodialysis (between-dialyses dose). At least 5 days separated the two doses, and randomization determined which dose each hemodialysis patient received first. For the between-dialyses dose, drug was administered and blood samples were obtained as above. For the during-dialysis dose, blood samples were collected via an indwelling venous catheter before starting and at the end of the infusion and at 15, 30, and 60 min postinfusion. Hemodialysis was begun approximately 1 h after the end of the infusion. Sampling continued at 1, 2, 3, and 4 h after the beginning of hemodialysis, at 15, 30, 45, and 60 min postdialysis, and at 8, 12, 24, 48, and 72 h postinfusion. In addition, blood samples were taken simultaneously from the dialyzer affluent and effluent at 2 and 4 h into hemodialysis or just before the end of hemodialysis. Blood samples were either immediately centrifuged in a refrigerated centrifuge or put on ice and centrifuged as soon as possible thereafter. The maximum time that samples were in ice was 3 h. Serum was frozen at -70C before analysis. For normal volunteers, two 10-ml portions of cumulative urine specimens were collected before drug administration and at 0 through 2, 2 through 4, 4 through 8, and 8 through 12 h after dosing. Cumulative urine specimens were also collected at 12 through 24, 24 through 48, and 48 through 72 h for renal failure patients not requiring hemodialysis. During the between-dialyses dosing period, any urine produced by hemodialysis patients was collected up to 72 h and/or just before the next hemodialysis period. For the during-dialysis period, urine was collected from the beginning to the end of hemodialysis and then over 4-h intervals up to 12 h and then from 12 through 24, 24 through 48, or 48 through 72 h and/or
to the next hemodialysis treatment. Urine samples were frozen at -70C until assayed. Assays. Serum, dialysate, and urine samples were assayed for cefoperazone and sulbactam by high-performance liquid chromatography at Pfizer Quality Control, Groton, Conn. The method for serum and urine determinations was reported previously (16). Dialysate samples were analyzed for cefoperazone content according to the same methodology previously reported for urine sample analysis, except that the dilution factor was 2 rather than 10. The sulbactam concentration of dialysate samples was determined by using the high-performance liquid chromatography conditions described for serum analyses (16); however, no sample pretreatment or extraction was performed. Several mobilephase conditions were required to eliminate chromatographic interferences found in patients with renal failure; these were individually validated. Pharmacokinetic analysis. Both sulbactam and cefoperazone concentrations were analyzed by model-independent methods (9). The area under the serum concentration-time curve (AUC) and the area under the moment curve (AUMC) were determined by the LaGrange cubic polynomial interpolating function in conjunction with linear and log trapezoidal methods and by extrapolation of the terminal slope to infinity. Total body clearance (CL) was calculated by dose IV/AUC. The mean residence time was calculated from AUMC/AUC corrected for the intravenous infusion. Volume of distribution at steady-state (V..) was calculated by CL multiplied by the mean residence time. The rate at which drug was removed from the body by hemodialysis (dXhd/dt) was derived from Fick's law of diffusion by using equation 1. We assumed that ultrafiltration and back-diffusion from the dialysate were negligible (12). (1) dXhd/dt = Qe, (Ca- C,) where Qe is the effective serum perfusion rate of the dialyzer [dialyzer blood flow rate X(1 - hematocrit)] and Ca and C, are affluent (arterial) and effluent (venous) dialyzer serum drug concentrations, respectively. Hemodialysis clearance (CLhd) was obtained by dividing both sides of equation 1 by Ca (9) and was defined as CLhd = (dXhd/dt)ICa = Qe(ERhd), where the hemodialysis extraction ratio (ERhd) is defined as
Statistical analysis. For purposes of analysis, the subjects were divided into five groups by estimated creatinine clearance (CLCR) (Table 1) (4). Group 4 consisted of patients requiring hemodialysis studied in their between-dialyses period, and group 5 consisted of the same patients during dialysis. Pharmacokinetic parameters were compared between renal function groups by analysis of variance, taking into account unequal group sizes. When a significant F ratio was obtained, Tukey's honestly significant difference test was utilized. Since group sizes were unequal, the harmonic mean was used in calculating the honestly significant difference value. Pharmacokinetic parameters obtained from hemodialysis patients when dosed between dialyses and during dialysis were compared by using Student's paired t test. RESULTS
Based on CLCR, the normal volunteers and patients were divided into five different groups. Normal volunteers (group 1, n = 6) had CLCR values from 94.7 to 111.3 ml/min, mild renal failure patients (group 2, n = 2) had CLCR values of 53.5 and 56.3 ml/min, and patients with moderate renal
(Ca
Cv)ICa.
VOL. 32, 1988
PHARMACOKINETICS OF CEFOPERAZONE-SULBACTAM
505
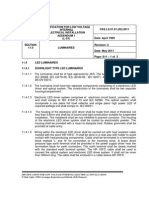
TABLE 1. Cefoperazone pharmacokinetic parameters after a 15-min intravenous infusion of cefoperazone-sulbactama
Groupb (n)
CLCRC t/2 (h) mi/mm)i/2() (range, 1.6 0.3 94.7-111.3 2.4, 1.9d 53.5, 56.3d 2.4 1.1 11.2-30.4 2.8 2.4 4.5-6.6 2.6 1.3 4.5-6.6
Cl V., (liters) (mi/mi)n(ltr)
h/mi) (jig AUC
356 52 10.2 1.0 95 14 1 (6) 8.7, 11.7d 734, 442" 45, 75d 2 (2) 9.9 1.7 672 333 61 30 3 (8) 542 457 13.1 1.7 97 66 4 (4) 429 202 12.5 1.4 90 35 5 (4) a Results are means standard deviations (except for CLCR). The dose was 2.0 g of cefoperazone plus 1.0 g of sulbactam. b Group 4 consists of functionally anephric patients tested between hemodialysis treatments; group 5 consists of the same patients tested during hemodialysis
treatment. I Estimated CLCR (5). d Individual values are shown due to small sample size.
failure (group 3, n = 8) had CLCR values from 11.2 to 30.4 ml/min. Groups 4 and 5 consisted of the same hemodialysis patients (n = 4) off and on hemodialysis, respectively. Their CLCR values ranged from 4.5 to 6.6 ml/min. After simultaneous intravenous infusion of cefoperazone (2 g) and sulbactam (1 g), serum concentrations of both drugs declined biexponentially with a brief distribution phase. Figure 1 shows the cefoperazone serum concentrations versus time for the five groups. Concentrations of cefoperazone did not appreciably change with renal dysfunction. Cefoperazone pharmacokinetic parameters for all groups are shown in Table 1. For cefoperazone, the terminal elimination half-life (t012), CL, Vs., and AUC were not statistically different between groups. There was no correlation between CL and CLCR (Fig. 2). Sulbactam pharmacokinetic parameters are shown in Table 2. For sulbactam, there were significant differences between the groups. The tl2 values for sulbactam in hemodialysis patients between treatments differed significantly from those of normal volunteers and patients with mild renal failure (P < 0.05). The sulbactam CL of the normal volunteers (mean, 267 ml/min) differed significantly from those of the other four groups (P < 0.01), and the sulbactam CL of
1000.
hemodialysis patients off hemodialysis (26 ml/min) differed significantly from that of the patients with mild renal failure (P < 0.05). The sulbactam V.s was significantly different between the hemodialysis patients on hemodialysis and the Vss of groups 1 to 4 (P < 0.05). The sulbactam serum concentration-versus-time profiles are illustrated in Fig. 3 for the five groups. The CL of sulbactam correlated significantly with CLCR (Fig. 4). The largest variations between CLCR and sulbactam CL occurred in the normal volunteers. When tested as an independent variable in a multiple linear regression analysis, age did not significantly influence the relationship between sulbactam CL and CLCR. Table 3 shows the pharmacokinetics of cefoperazone and sulbactam during and between hemodialysis treatments for the functionally anephric patients. There were considerable differences between the two drugs when pharmacokinetic behaviors during and between hemodialysis treatments were compared. Cefoperazone showed no differences (Table 3). During hemodialysis, the mean extraction ratio of cefoperazone was 0.05, and the mean hemodialysis clearance was 8.1 ml/min. The mean percentage of the dose recovered in dialysate was 3.6 2.4%.
i 10L
Hours After Dosing
GROUP -----1
-
2 ....e...3 --1-- 4
..- 5
FIG. 1. Cefoperazone concentrations in serum versus time for five subject groups with varied renal function. The mean values of concentration in serum are plotted for all patients in each group.
506
REITBERG ET AL.
2000
ANTIMICROB. AGENTS CHEMOTHER.
180
160.
140
I
120'0
1000 0
80
60
*00
0~~~~~
0 0
0
40
0
20-
0
0 20
40
60
100
120
Ceatinine Clearance (mllmin) FIG. 2. Correlation between CLCR and CL of cefoperazone in 20 human volunteers. The data are described by the regression equation CL = 0.2(CLCR) + 70.8 (r = 0.17, P = 0.46).
Sulbactam demonstrated pronounced pharmacokinetic changes during hemodialysis (Table 3). The mean extraction ratio was 0.44, and the mean hemodialysis clearance was 75 ml/min. The mean percentage of the dose recovered in dialysate was 30 + 9%. Comparing hemodialysis patients off and on hemodialysis, sulbactam CL and V., were significantly different (P < 0.05), as was the AUC (P < 0.05) (Table 3). Table 3 also lists the mean hemodialysis extraction ratio and hemodialysis clearance of cefoperazone and sulbactam. The hemodialysis extraction ratio of sulbactam was significantly different from that of cefoperazone (0.05 versus 0.44, P < 0.005). Hemodialysis clearance was significantly different between sulbactam and cefoperazone (8.1 versus 75 mi/mn, P < 0.01). The recovery of both drugs from urine was highly variable within the five groups (Table 4). Within each group, the percentage of the sulbactam dose recovered in the urine was much greater than the percentage of the cefoperazone dose recovered (P < 0.01). There was a trend toward decreasing recovery of both drugs in urine with decreased renal function. Recovery of both drugs in urine from hemodialysis patients was similar during and between hemodialysis treatments. TABLE 2. Sulbactam
Group (n)
There
were no
clinically relevant changes in laboratory
parameters associated with the single dose of the combina-
tion product. Likewise, the infusion over 15 min was well tolerated. However, after the infusion, all six of the normal volunteers in group 1 reported onset of loose stools within 24 to 48 h of administration, and these effects resolved by 96 h after dosing in all but one. Two of the patients also reported similar effects; one of these patients experienced two such episodes 5 days apart. One patient suffered a myocardial infarction and died 3 days after the study was completed. He had a long history of cardiovascular disease, and his death was not considered to be related to the study drugs.
DISCUSSION Cefoperazone pharmacokinetic parameters were not significantly affected by the varied degree of renal compromise presented by the volunteers and patients in this study. Since cefoperazone is not primarily excreted by the renal route, it was not surprising to find that cefoperazone CL did not correlate with CLCR. This finding is consistent with other reports (1, 2, 5, 10, 13, 14, 17, 18). Although the molecular weight of cefoperazone is 645 and thus it would be readily filterable, only a small percentage of the total serum concen-
pharmacokinetic parameters after a 15-min intravenous infusion of cefoperazone-sulbactama
tl2 (h)
1.0 0.2 1.6, 1.7 4.6 2.2 9.7 5.3b 8.3 1.7
CL (ml/min)
(range,mimLC )
V5 (liters)
(Ag
Sml)
1 (6) 2 (2) 3 (8) 4 (4) 5 (4)
94.7-111.3
53.5, 56.3 11.2-30.4 4.5-6.6 4.5-6.6
267 49
130, 137b
48 21b 26 1ob 56 2.8b
18.0 1.0 14.1, 20.6 15.3 2.6 18.6 2.9 30.0 3.2b
64 11
411 182b 709 271b 300 15b
129, 122b
a See footnotes a through d of Table 1. b Significantly different from group 1.
VOL. 32, 1988
PHARMACOKINETICS OF CEFOPERAZONE-SULBACTAM
507
E
100
_E~~
......
...
........
Hours After Dosing
GROUP --6
1 -o
2 **.... 3 --- -4
--5
FIG. 3. Sulbactam concentrations in serum versus time for five subject groups with varied renal function. The mean values of concentration in serum are plotted for all patients in each group.
tration is freely filtered due to its high protein binding and low free fraction. The free fraction of cefoperazone is approximately 7 to 13%, which is the approximate ratio of cefoperazone CL to CLCR (10). Both increased drug concentration (1) and displacement of cefoperazone from binding sites by bilirubin can increase the proportion of unbound cefoperazone (17). The amount of cefoperazone recovered in the urine has been directly related to the extent of hyperbilirubinemia, and in patients with complete biliary tract obstruction, 90% of an administered dose has been recovered in the urine over a 24-h period (10). When compared with
350-
normal volunteers, patients with severe biliary tract obstruction had approximately two-thirds lower CL, one-half lower nonrenal clearance, and one third greater renal clearance. As Shimizu has shown, probenecid has an insignificant effect on cefoperazone serum concentrations and tl2 (17). When cefoperazone pharmacokinetic parameters were calculated for the normal volunteers in this study, the ranges for t112, CL, and Vs, were consistent with previously published reports (1, 5, 10, 13, 16, 18). The present study showed that for end-stage renal disease patients, cefoperazone pharmacokinetic parameters did not change when
2500
200-
i
150-
100-
50~
20
40
60
80
100
120
Creatnine Clarance (ml/min)
FIG. 4. Correlation between CLCR and CL of sulbactam in 20 human volunteers. The data are described by the regression equation CL = 2.6(CLCR) - 1.17 (r = 0.96, P < 0.001.)
508
REITBERG ET AL.
ANTIMICROB. AGENTS CHEMOTHER.
TABLE 3. Pharmacokinetics of cefoperazone (2.0 g) and sulbactam (1.0 g) during and between hemodialysis treatments'
Drug Time of sampling
t4/2 (h)
(ml/mi)n
CL
v,, ) (liters)
ratio Hemodialysis clearance % inRecovered hIml) Extraction (ml/min) (~Lg AUC dialysate [(Ca, - Cv)ICaJ]
0.05 0.05
0.44 0.11
Cefoperazone During treatment 2.6 1.3 90 35 Between treatments 2.8 2.4b 97 66b
Sulbactam
12 1.4 429 202 13 1.7b 542 457b
8.1 8.1
75 19
3.6 2.4
30 9
30 3.2 300 + 15 During treatment 2.0 0.5c 56 2.8 Between treatments 9.7 5.3d 26 lod 18.6 3.0d 709 271d
a Results are means standard deviations. b Difference was not significant compared with results from samples taken during treatment. c During hemodialysis treatment period; not over dosing interval. d Significantly diffferent (P < 0.05) from results from samples taken during treatment.
patients were on or off hemodialysis. The low hemodialysis extraction ratio and low hemodialysis clearance observed in these patients is consistent with cefoperazone having high serum protein binding and a molecular weight of 645. The pharmacokinetic parameters of sulbactam are primarily dependent on renal function. Foulds et al. (8) gave both a 500-mg and a 1,000-mg dose of sulbactam to four healthy male volunteers and assayed serum and urine samples by bioassay for intact sulbactam. The renal clearance was 75.5 to 80.4% of the CL. The sulbactam pharmacokinetic data of the six normal volunteers participating in the present study were comparable. The V., values for these normal volunteers closely approximated extracellular water, that is, 0.23 liter per kg of ideal body weight (6). In contrast to cefoperazone, the protein binding of sulbactam is low and does not affect renal elimination. Several reports have indicated that the pharmacokinetics of sulbactam are not altered by coadministration of cefoperazone in normal volunteers (8, 16). The AUC and amount of cefoperazone recovered in urine are not appreciably altered by coadministration; this was found at the same intravenous infusion rate used in the present study, with assays conducted at the same site (16). Comparison of the cefoperazone and sulbactam pharmacokinetic parameters when these drugs were coadministered to our volunteers with the literature-derived volunteer pharmacokinetic parameters confirms that a significant pharmacokinetic interaction between these drugs is unlikely, since volunteer parameters are similar whether the drugs are given separately or coadministered. When administered alone, sulbactam has an average renal clearance greater than 200 ml/min, indicating that renal elimination occurs via glomerular filtration and renal tubular secretion (3, 19). Probenecid administered before sulbactam administration has been shown to increase the sulbactam t1l2 approximately 40%, further supporting the hypothesis that
TABLE 4. Cumulative percentage of cefoperazone and sulbactam recovered in urine after administration of 2.0 g of cefoperazone-1.0 g of sulbactam'
Group
1 2 3 4 5
(m/mn (mI/mm)
CLCR
Recovery (% of dose t SD) Sulbactam Cefoperazone
94.7-111.3 53.5, 56.3 11.2-30.4
4.5-6.6 4.5-6.6
19 3 6, 29 8 5 0.4 0.4 0.6 0.6
79 12 41, 95 73 + 22" 99 7 10
a See footnotes b, c, and d of Table 1. bIf one patient with an exceptionally high sulbactam recovery is excluded, the mean percent recovery for group 3 would be 59.3%.
renal tubular secretion plays a significant role in the renal clearance of sulbactam (V. A. Caine, K. K. Holmes, G. Foulds, and H. H. Handsfield, Abstr. Annu. Meet. Am. Soc. Microbiol. 1981, A72, p. 13). Considering that sulbactam is primarily eliminated renally, our finding that sulbactam CL correlated strongly with CLCR suggests that as renal failure begins and progresses toward end-stage renal disease, tubular secretion and glomerular filtration of sulbactam decrease proportionately. The differences found between the mean sulbactam tl2 of the patients on and off hemodialysis predominantly reflect the addition of hemodialysis clearance. Hemodialysis removes nearly a third of the sulbactam dose, as reflected by the differences in plasma AUC and dialysate recovery in these patients. The combination of 2.0 g of cefoperazone and 1.0 g of sulbactam is designed to be given every 12 h in patients with normal renal function. Based on our findings, this recommended regimen does not need to be altered in patients with CLCR of greater than 30 ml/min. For patients with a CLCR less than 30 ml/min, the total daily dose of sulbactam can be reduced by giving one dose of the 2:1 combination product followed in 12 h by an additional equivalent dose of cefoperazone alone. This adjustment may be particularly appropriate at a CLCR of less than 15 mlmin; patients with end-stage renal disease who are given this compensating, alternating regimen are expected to show accumulation of sulbactam to a maximal serum concentration approximately double that usually observed. Similar modest accumulation would be expected at CLCR values between 15 and 30 ml/min if the regimen is not adjusted. In summary, the elimination pharmacokinetic parameters found for sulbactam were significantly correlated with CLCR. This correlation was not observed for cefoperazone. Hemodialysis approximately doubled the CL of sulbactam, although it reduced the total amount of drug in the body by only one-third. The pharmacokinetics of cefoperazone were not altered by decreasing renal function or by hemodialysis. When the combination of cefoperazone and the P-lactamase inhibitor sulbactam is used to increase the antimicrobial spectrum of cefoperazone, the adjustment of the dosing regimen for patients with CLCR values of less than 30 ml/min can easily be made to compensate for the reduced CL of the sulbactam component of the combination. An adjustment may be particularly appropriate at a CLCR of less than 15 ml/min. It is clear that hemodialysis treatment does not remove enough sulbactam to require a supplemental dose after hemodialysis, and that the hemodialysis treatment need not further complicate this proposed dosing regimen, but it is recommended that dosing be scheduled to follow hemodialysis if possible to maximize the likelihood of predictable serum concentrations between hemodialysis treatments.
VOL. 32, 1988
PHARMACOKINETICS OF CEFOPERAZONE-SULBACTAM
ACKNOWLEDGMENT
509
This work was supported by a grant from Pfizer Pharmaceuticals, New York, N.Y. LITERATURE CITED Balant, L., P. Dayer, M. Rudhardt, A. F. Allay, and J. Fabre. 1980. Cefoperazone: pharmacokinetics in humans with normal and impaired renal function and pharmacokinetics in rats. Clin. Ther. (Special Issue) 3:50-59. Bolton, W. K., W. M. Scheld, D. A. Spyker, and M. A. Sande. 1981. Pharmacokinetics of cefoperazone in normal volunteers and subjects with renal insufficiency. Antimicrob. Agents Chemother. 19:821-825. Brown, R. M., R. Wise, J. M. Andrews, and J. Hancox. 1982. Comparative pharmacokinetics and tissue penetration of sulbactam and ampicillin after concurrent intravenous administration. Antimicrob. Agents Chemother. 21:565-567. Cockroft, D. W., and M. H. Gault. 1976. Prediction of creatinine clearance from serum creatinine. Nephron 16:34-41. Craig, W. A. 1980. Single-dose pharmacokinetics of cefoperazone following intravenous administration. Clin. Ther. (Special Issue) 3:46-49. Devine, B. 1974. Gentamicin therapy. Drug Intell. Clin. Pharm. 8:650. English, A. R., J. A. Retsema, A. E. Girard, J. E. Lynch, and W. E. Barth. 1978. CP-45,899, a beta-lactamase inhibitor that extends the antimicrobial spectrum of beta-lactams: initial bacteriological characterization. Antimicrob. Agents Chemother. 14:414 449. Foulds, G., J. P. Stankewich, D. C. Marshall, M. M. O'Brien, S. L. Hayes, D. J. Weidler, and F. G. McMahon. 1983. Pharmacokinetics of sulbactam in humans. Antimicrob. Agents Chemother. 23:692-699. Gibaldi, M., and D. Perrier (ed.). 1982. Pharmacokinetics, 2nd ed. Marcel Dekker, Inc., New York.
10. Greenfield, R. A., A. U. Gerber, and W. A. Craig. 1983. Pharmacokinetics of cefoperazone in patients with normal and impaired hepatic and renal function. Rev. Infect. Dis. 5
(Suppl.):S127-S136.
11. Jones, R. N., A. L. Barry, R. R. Packer, W. W. Gregory, and C. Thornsberry. 1987. In vitro antimicrobial spectrum, occurrence of synergy, and recommendations for dilution susceptibility testing concentrations of the cefoperazone-sulbactam combination. J. Clin. Microbiol. 25:1725-1729. 12. Lee, C. S., T. C. Marbury, L. Z. Benet. 1980. Clearance calculations in hemodialysis: application to blood, plasma and dialysate measurements of ethambutol. J. Pharmacol. Biopharm. 8:69-81. 13. Lode, H., B. Kemmerich, P. Koeppe, D. Belmega, and H. Jendroschek. 1980. Comparative pharmacokinetics of cefoperazone and cefotaxime. Clin. Ther. (Special Issue) 3:80-88. 14. Maksymiuk, A. W., B. M. LeBlanc, N. S. Brown, D. Ho, and G. P. Bodey. 1981. Pharmacokinetics of cefoperazone in patients with neoplastic disease. Antimicrob. Agents Chemother. 19:1037-1041. 15. Neu, H. C., K. P. Fu, N. Aswapokee, P. Aswapokee, and K. Kung. 1979. Comparative activity and beta-lactamase stability of cefoperazone, a piperazine cephalosporin. Antimicrob. Agents Chemother. 16:150-157. 16. Reitberg, D. P., T. J. Whall, M. Chung, D. Blickens, H. Swarz, and J. Arnold. 1988. Multiple-dose toleration and pharmacokinetics of intravenously administered cefoperazone and sulbactam when given as single agents and when given in combination. Antimicrob. Agents Chemother. 32:42-46. 17. Shimizu, K. 1980. Cefoperazone: absorption, excretion, distribution and metabolism. Clin. Ther. (Special Issue) 3:60-79. 18. Srinivasan, S., E. L. Francke, and H. C. Neu. 1981. Comparative pharmacokinetics of cefoperazone and cefamandole. Antimicrob. Agents Chemother. 19:298-301. 19. Wright, N., and R. Wise. 1983. The elimination of sulbactam alone and combined with ampicillin in patients with renal dysfunction. J. Antimicrob. Chemother. 11:583-587.
1.
2.
3.
4.
5.
6. 7.
8.
9.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Pankaj Screener 10 Oct 2014Document127 pagesPankaj Screener 10 Oct 2014Sadul Singh Naruka100% (1)
- Lake Isle of Innisfree Lesson Plan BV ZGDocument4 pagesLake Isle of Innisfree Lesson Plan BV ZGapi-266111651100% (1)
- CH 22 Solutions ManualDocument22 pagesCH 22 Solutions Manuallmbrn0415No ratings yet
- Argenti, P. Corporate Communication. Cap. 8-9Document28 pagesArgenti, P. Corporate Communication. Cap. 8-9juan100% (1)
- Ethics Book of TAMIL NADU HSC 11th Standard Tamil MediumDocument140 pagesEthics Book of TAMIL NADU HSC 11th Standard Tamil MediumkumardjayaNo ratings yet
- Technical Bro A4 UK LR NEW v2Document45 pagesTechnical Bro A4 UK LR NEW v2Roxana NegoitaNo ratings yet
- Principles of CHN New UpdatedDocument4 pagesPrinciples of CHN New Updatediheart musicNo ratings yet
- Chapter 1 - The Empirical Beginnings and Basic Contents of Educational PsychologyDocument9 pagesChapter 1 - The Empirical Beginnings and Basic Contents of Educational PsychologyJoshua Almuete71% (7)
- Automated Crime Reporting SystemDocument101 pagesAutomated Crime Reporting SystemDeepak Kumar60% (10)
- Mathematics Specimen Papers and Mark Schemes UG013054Document102 pagesMathematics Specimen Papers and Mark Schemes UG013054minnie murphy86% (7)
- Unit 01 Family Life Lesson 1 Getting Started - 2Document39 pagesUnit 01 Family Life Lesson 1 Getting Started - 2Minh Đức NghiêmNo ratings yet
- Makerwys - Exe Version 4.891: by Pete Dowson © 2019 InstructionsDocument11 pagesMakerwys - Exe Version 4.891: by Pete Dowson © 2019 InstructionsRafrol RamonNo ratings yet
- High Yield Pics For STEP 2 CKDocument24 pagesHigh Yield Pics For STEP 2 CKKinan Alhalabi96% (28)
- CP R77.30 ReleaseNotesDocument18 pagesCP R77.30 ReleaseNotesnenjamsNo ratings yet
- Morpho Full Fix 2Document9 pagesMorpho Full Fix 2Dayu AnaNo ratings yet
- Carmina GadelicaDocument37 pagesCarmina GadelicaoniricsNo ratings yet
- Hearing God Through Biblical Meditation - 1 PDFDocument20 pagesHearing God Through Biblical Meditation - 1 PDFAlexander PeñaNo ratings yet
- List of SQAC DQAC SISC DISC 2019 20Document39 pagesList of SQAC DQAC SISC DISC 2019 20Shweta jainNo ratings yet
- Polymer Science: Thermal Transitions in PolymersDocument20 pagesPolymer Science: Thermal Transitions in Polymerstanveer054No ratings yet
- JKR Specs L-S1 Addendum No 1 LED Luminaires - May 2011Document3 pagesJKR Specs L-S1 Addendum No 1 LED Luminaires - May 2011Leong KmNo ratings yet
- 1 Starter WBDocument88 pages1 Starter WBHYONo ratings yet
- Vivaldi - Genuis of BaroqueDocument279 pagesVivaldi - Genuis of Baroqueilcanto100% (4)
- 1 API 653 Exam Mar 2015 MemoryDocument12 pages1 API 653 Exam Mar 2015 MemorymajidNo ratings yet
- Key Elements of Participation and Conflict Resolution in a DemocracyDocument6 pagesKey Elements of Participation and Conflict Resolution in a DemocracyAbhinayNo ratings yet
- Lorain Schools CEO Finalist Lloyd MartinDocument14 pagesLorain Schools CEO Finalist Lloyd MartinThe Morning JournalNo ratings yet
- Component 2 Learner Statement Y2Document6 pagesComponent 2 Learner Statement Y2api-426152133No ratings yet
- MEC332-MA 3rd Sem - Development EconomicsDocument9 pagesMEC332-MA 3rd Sem - Development EconomicsRITUPARNA KASHYAP 2239239No ratings yet
- MAN 2 Model Medan Introduction to School Environment ReportDocument45 pagesMAN 2 Model Medan Introduction to School Environment ReportdindaNo ratings yet
- Why Leaders Should Look in the “MirrorDocument4 pagesWhy Leaders Should Look in the “MirrorCaryl Baylon EstreraNo ratings yet
- Gatk Pipeline Presentation: From Fastq Data To High Confident VariantsDocument8 pagesGatk Pipeline Presentation: From Fastq Data To High Confident VariantsSampreeth ReddyNo ratings yet