Professional Documents
Culture Documents
RENAL DIALYSIS - Body Image Disturbed Self-Esteem, Situational Low
Uploaded by
makyofrancis20Original Title
Copyright
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
RENAL DIALYSIS - Body Image Disturbed Self-Esteem, Situational Low
Uploaded by
makyofrancis20Copyright:
NURSING DIAGNOSIS: Body Image disturbed/Self-Esteem, situational low May be related to Situational crisis, chronic illness with changes
in usual roles/body image Possibly evidenced by Verbalization of changes in lifestyle; focus on past function, negative feelings about body; feelings of helplessness, powerlessness Continuous physical deterioration, premature aging, disfigurement Extension of body boundary to incorporate environmental objects (e.g., dialysis equipment) Change in social involvement Overdependence on others for care, not taking responsibility for self-care/lack of follow-through, self-destructive behavior DESIRED OUTCOMES/EVALUATION CRITERIAPATIENT WILL: Self-Esteem (NOC) Identify feelings and methods for coping with negative perception of self. Verbalize acceptance of self in situation. Demonstrate adaptation to changes/events that have occurred, as evidenced by setting realistic goals and active participation in care/life.
ACTIONS/INTERVENTIONS
Body Image [or] Self-Esteem Enhancement (NIC)
RATIONALE
Independent
Assess level of patients knowledge about condition and treatment and anxiety related to current situation. Support active information seeking by patient/SO. Identifies extent of problem/concern and necessary interventions. Concern/belief that sharing of information may be "controlled by healthcare providers perpetuates sense of a power differential, potentiating dependence/mistrust. Some patients may view situation as a challenge, although many have difficulty dealing with changes in life/role performance and loss of ability to control own body.
Discuss meaning of loss/change to patient.
ACTIONS/INTERVENTIONS
Body Image [or] Self-Esteem Enhancement (NIC)
RATIONALE
Independent
Note withdrawn behavior, ineffective use of denial, or behaviors indicative of overconcern with body and its functions. Investigate reports of feelings of depersonalization or the bestowing of human-like qualities on machinery. Assess use of addictive substances (e.g., alcohol), selfdestructive/suicidal behavior. Determine stage of grieving. Note signs of severe/prolonged depression. Indicators of developing difficulty handling stress of what is happening. Note: Some patients may feel tied to/controlled by technology central to their survival, even to the point of extending body boundary to incorporate dialysis equipment. May reflect dysfunctional coping and attempt to handle problems in an ineffective manner. Identification of stage patient is experiencing provides guide to recognizing and dealing appropriately with behavior as patient/SO work to come to terms with loss
and limitations associated with condition. Prolonged depression may indicate need for further intervention. Acknowledge normalcy of feelings. Recognition that feelings are to be expected helps patient accept and deal with them more effectively. Helps patient identify problems and problem-solve solutions. Long-term/permanent illness and disability alter patients ability to fulfill usual role(s) in family/work setting. Unrealistic expectations can undermine self-esteem and affect outcome of illness. Conveys expectation that patient is able to manage situation, and helps maintain sense of self-worth and purpose in life. Necessities of treatment assume a more normal aspect when they are a part of the daily routine. Focusing on these reminders of own ability to deal with problems can help patient deal with current situation. Provides sense of control over seemingly uncontrollable situation, fostering independence.
Encourage verbalization of personal and work conflicts that may arise. Active-listen concerns. Determine patients role in family constellation and patients perception of expectation of self and others.
Recommend SO treat patient normally and not as an invalid.
Assist patient to incorporate disease management into lifestyle. Identify strengths, past successes, previous methods patient has used to deal with life stressors. Help patient identify areas over which he or she has some measure of control. Provide opportunity to participate in decision-making process.
Collaborative
Recommend participation in local support group. Reduces sense of isolation as patient learns that others have been where patient is now. Provides role models for dealing with situation, problem solving and getting on with life. Reinforces that therapeutic regimen can be beneficial. Provides additional assistance for long-term management of chronic illness/change in lifestyle.
Refer to healthcare/community resources, e.g., social service, vocational counselor, psychiatric clinical nurse specalist.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Burns - Skin Integrity, ImpairedDocument2 pagesBurns - Skin Integrity, Impairedmakyofrancis20No ratings yet
- Renal Dialysis: Care SettingDocument1 pageRenal Dialysis: Care Settingmakyofrancis20No ratings yet
- Peritoneal DialysisDocument23 pagesPeritoneal Dialysismakyofrancis20No ratings yet
- Burns - Tissue Perfusion, IneffectiveDocument3 pagesBurns - Tissue Perfusion, Ineffectivemakyofrancis20100% (1)
- RENAL DIALYSIS - Self-Care Deficit (Specify)Document1 pageRENAL DIALYSIS - Self-Care Deficit (Specify)makyofrancis20No ratings yet
- Burns - Body Image Disturbed Role Performance, IneffectiveDocument2 pagesBurns - Body Image Disturbed Role Performance, Ineffectivemakyofrancis20No ratings yet
- Burns - Mobility, Impaired PhysicalDocument2 pagesBurns - Mobility, Impaired Physicalmakyofrancis20No ratings yet
- Burns - Pain, AcuteDocument3 pagesBurns - Pain, Acutemakyofrancis20No ratings yet
- Burns - Nutrition, Imbalanced, Less Than Body RequirementsDocument2 pagesBurns - Nutrition, Imbalanced, Less Than Body Requirementsmakyofrancis20No ratings yet
- Nursing diagnosis for fear and anxiety in hospitalized burn patientsDocument2 pagesNursing diagnosis for fear and anxiety in hospitalized burn patientsmakyofrancis20No ratings yet
- Burns - Infection, Risk ForDocument4 pagesBurns - Infection, Risk Formakyofrancis20No ratings yet
- RENAL DIALYSIS - Nutrition, Imbalanced, Less Than Body RequirementsDocument3 pagesRENAL DIALYSIS - Nutrition, Imbalanced, Less Than Body Requirementsmakyofrancis20No ratings yet
- Burns - Knowledge, DeficientDocument2 pagesBurns - Knowledge, Deficientmakyofrancis20No ratings yet
- Monitor for signs of fluid overload: increasing dyspnea, rales, edema, weight gain. Notify physician if presentDocument3 pagesMonitor for signs of fluid overload: increasing dyspnea, rales, edema, weight gain. Notify physician if presentmakyofrancis20No ratings yet
- Burns - Airway Clearance, Risk For IneffectiveDocument2 pagesBurns - Airway Clearance, Risk For Ineffectivemakyofrancis20No ratings yet
- BURNS: CARE FOR THERMAL, CHEMICAL, AND ELECTRICAL INJURIESDocument4 pagesBURNS: CARE FOR THERMAL, CHEMICAL, AND ELECTRICAL INJURIESmakyofrancis20No ratings yet
- RENAL DIALYSIS - Anxiety (Specify Level) FearDocument2 pagesRENAL DIALYSIS - Anxiety (Specify Level) Fearmakyofrancis20No ratings yet
- Nursing diagnosis: Mobility impaired physicalDocument2 pagesNursing diagnosis: Mobility impaired physicalmakyofrancis20No ratings yet
- RENAL DIALYSIS - Constipation, Risk ForDocument1 pageRENAL DIALYSIS - Constipation, Risk Formakyofrancis20No ratings yet
- Test 1Document1 pageTest 1makyofrancis20No ratings yet
- RENAL DIALYSIS - Thought Processes, Risk For DisturbedDocument2 pagesRENAL DIALYSIS - Thought Processes, Risk For Disturbedmakyofrancis20No ratings yet
- RENAL DIALYSIS - Knowledge, DeficientDocument2 pagesRENAL DIALYSIS - Knowledge, Deficientmakyofrancis20No ratings yet
- SeizureDocument9 pagesSeizuremakyofrancis20No ratings yet
- ROS ChecklistDocument2 pagesROS Checklistmindful33No ratings yet
- AbstractDocument1 pageAbstractmakyofrancis20No ratings yet
- Pathognomonic SignsDocument1 pagePathognomonic Signsmakyofrancis20No ratings yet
- Graham RecipeDocument2 pagesGraham Recipemakyofrancis20No ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Amazing DeclineDocument26 pagesThe Amazing DeclineSuzanne HumphriesNo ratings yet
- Health Psychology 10th Edition Taylor Solutions ManualDocument10 pagesHealth Psychology 10th Edition Taylor Solutions Manualbambinogittithhlmhvq100% (24)
- HESU OrganogramDocument29 pagesHESU OrganogramHEMS SAMCH100% (4)
- Academic Stress, Anxiety and Depression Among College StudentsDocument9 pagesAcademic Stress, Anxiety and Depression Among College StudentsSamar HamadyNo ratings yet
- Nursing EssayDocument11 pagesNursing Essayapi-255976823100% (1)
- Scope of clinical psychologyDocument29 pagesScope of clinical psychologyAnet Augustine AnetNo ratings yet
- World Health Organization Updated COVID-19 Report-March 25Document12 pagesWorld Health Organization Updated COVID-19 Report-March 25CityNewsTorontoNo ratings yet
- Summative Test in English for Academic and Professional PurposesDocument6 pagesSummative Test in English for Academic and Professional Purposesaubrey somozaNo ratings yet
- SCDPH Mass COVID19 Vaccination PlanDocument32 pagesSCDPH Mass COVID19 Vaccination PlanNewsTeam20100% (1)
- Health Disparities in The United States Social Class Race Ethnicity and The Social Determinants of Health 3rd Edition Ebook PDFDocument62 pagesHealth Disparities in The United States Social Class Race Ethnicity and The Social Determinants of Health 3rd Edition Ebook PDFtamra.miller558100% (43)
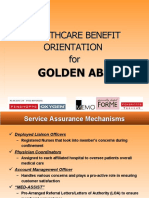
- Healthcare Benefit Orientation ForDocument14 pagesHealthcare Benefit Orientation Forapi-19650311100% (1)
- WRITING CAE - Summary With VocabularyDocument18 pagesWRITING CAE - Summary With VocabularySerenajly100% (1)
- 3 Sided Essay FinalDocument3 pages3 Sided Essay FinalDominique TaylorNo ratings yet
- FAMILY FUNCTION AND MEDICATION ADHERENCE IN PROLANIS PATIENTS IN PEKANBARU Rev 1Document16 pagesFAMILY FUNCTION AND MEDICATION ADHERENCE IN PROLANIS PATIENTS IN PEKANBARU Rev 1fakhirahfitri217No ratings yet
- Divine Intervention Episode 36 Usmle OphthalmologyDocument15 pagesDivine Intervention Episode 36 Usmle OphthalmologySwisskelly1No ratings yet
- Japanese Acupuncture: A Complementary Approach To The Meridian Balance MethodDocument7 pagesJapanese Acupuncture: A Complementary Approach To The Meridian Balance Methodme anonimus100% (1)
- English Language Dialogue On HIVDocument5 pagesEnglish Language Dialogue On HIVAFRI YUNIKANo ratings yet
- CoopMED Health Insurance Doctor Examination FormDocument2 pagesCoopMED Health Insurance Doctor Examination FormKammieNo ratings yet
- Unit 1 - AOS 2 Community Health and WellbeingDocument27 pagesUnit 1 - AOS 2 Community Health and WellbeingHaley JonesNo ratings yet
- YogSandesh February Eng2012Document68 pagesYogSandesh February Eng2012Manmohan Gupta100% (1)
- Killer Controversy - Why Orcas Should No Longer Be Kept in CaptivityDocument20 pagesKiller Controversy - Why Orcas Should No Longer Be Kept in CaptivityThe Orca Project Corp100% (1)
- Florence Nightingale's Environmental TheoryDocument10 pagesFlorence Nightingale's Environmental TheoryMANLANGIT, Bianca Trish A.No ratings yet
- Quantitative Research PaperDocument18 pagesQuantitative Research Paperapi-290348341No ratings yet
- ARI Varmam Therapy Mail Today Article 25jan 2011Document1 pageARI Varmam Therapy Mail Today Article 25jan 2011Arts Research InstituteNo ratings yet
- Wollo University College of Medicine and Health Scince Department of PhrmacyDocument16 pagesWollo University College of Medicine and Health Scince Department of Phrmacynegussie birieNo ratings yet
- Farm Safety Risk AssessmentDocument32 pagesFarm Safety Risk AssessmentnmmartinsaNo ratings yet
- CESAR AUGUSTO GALVEZ - Biblical Perspective On Health For The Contemporary WorldDocument11 pagesCESAR AUGUSTO GALVEZ - Biblical Perspective On Health For The Contemporary WorldDanielNo ratings yet
- Biochemistry of Aging Lab OutlineDocument1 pageBiochemistry of Aging Lab OutlineKeila RosalesNo ratings yet
- The Study of Human Sleep: A Historical Perspective: William C DementDocument6 pagesThe Study of Human Sleep: A Historical Perspective: William C DementKrisha ann MesanaNo ratings yet
- Franco Gera Hi An 93356145 Ethics EssayDocument13 pagesFranco Gera Hi An 93356145 Ethics EssayFranco GerahianNo ratings yet