Professional Documents
Culture Documents
Caring For The Client With Schizophrenia
Uploaded by
Ecaroh Hew SmailliwOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Caring For The Client With Schizophrenia
Uploaded by
Ecaroh Hew SmailliwCopyright:
Available Formats
Table of Content
Contents Introduction /Purpose/Aim of Study Literature Review Patients profile Past Medical History History of Present Illness Past Surgical History Sexual History Family History Family Psychiatric History Psychiatric History Education History Description of patients community Behaviour on Admission Medical management Nursing management Physical Assessment Mental Status Assessment Summary of Care Family Involvement in care Community Involvement in care Patients Outlook for the future Nursing Care Plan
Page 1 2 3
Conclusion Recommendations References
Appendices
Introduction
This Care Study looks at a client currently admitted to ward five (5) at the Bellevue Hospital. We shall refer to him as S.F, he was admitted on the seventh (7) 0f October 2008 (and diagnosed with schizophrenia) after he was brought in by mental health officers with a history of exposing and denuding himself on the compounds of a school on which he worked as the caretaker.
This Care study will also look at the nursing and medical management of Mr. S.F. as well as all the related therapies, these include; group therapy, one to one therapy, pharmacotherapy, and occupational therapy.
A profile of the clients community, his outcome/prognosis as well as his familys involvement in his care will also be looked at.
Purpose of this study This Care Study is being done in partial fulfilment of the course Post Basic Psychiatric Nursing. Its intent is to provide this student with the requisite skill and knowledge to manage the client with the above named diagnosis as well as others with similar mental health challenges.
Literature Review Schizophrenia is a severe mental illness that usually strikes between the ages of seventeen (17) and twenty five (25) years of age. (Ignatavicius, 2004). It is one of the large groups of severe mental disorders typified by gross distortion of reality, disturbance in language and breakdown of thought processes, perceptions and emotions. Delusions and hallucinations are usual as are apathy, confusion, incontinence, and strange behaviour. No single cause is known but genetic factors, chemical imbalance, structural brain abnormalities, and stressful events are probably important. (Frisch, Frisch, 2005) TheDSM-1V-TR list five subtypes: (1) Paranoid - this is where theres presence of hallucination and delusional thinking, but fairly organized speech and behaviour; may show some range in affect. (2) Disorganized - theres dominant manifestations of disorganized speech and behaviour, with flat or inappropriate affect; may also have hallucinations and delusions. (3) Catatonic theres the presence of bizarre motor activity, either excessive and purposeless or immobilized as if in a stupor; may be mute or show incoherent speech. (4) Undifferentiated theres the presence of two or more of the following signs and symptoms, but theres no marked feature as in the previously named subtypes: hallucinations, delusions, disorganized speech/behaviour and flattening of the affect. (5) Residual behaviours do not manifest obvious
hallucinations, delusions, or disorganization, but theres an alteration in the range of affect and thought patterns. (Black 2005).
In all cases, theres a profound deficit in an individuals ability to think and to communicate. Signs and symptoms are generally classified as either positive or negative symptoms or both. Positive signs and symptoms include the following: auditory/visual hallucinations, delusions, disorganized thinking and speech, which are all obvious signs of psychosis. Negative signs and symptoms include: blunted affect, avoidance of social contact, lack of attention to hygiene, and a decrease in speech, these are all lack of usual emotional/social responses.
The cause of schizophrenia is unknown, but several theories have been propagated, among these are: The genetic, psychoanalytic, organic, and neurotransmitter theories.
The genetic theory posits, that for the general population the chance of an individual becoming schizophrenic is 1%, while the individual with two parents stands a 40-50% chance of becoming ill with the condition, other family relations is also a risk factor. Of all the genetic permutations, studies have shown that monozygous twins stands the greatest chance of being affected with schizophrenia. (Frisch 2005).
The Psychoanalytic view states that childhood situations, such as, temper tantrums and unresolved aggression might ultimately lead to psychosis. Another view posits, that
inadequate maternal nuturance in early infancy could lead to psychosis. Further psychoanalytical research have evaluated a wide range of developmental, environmental and psychological factors, but those studies have not proved to be very definitive. ( Frisch et al., 2005)
The Organic theory, suggests that there is something physically and structurally wrong with the brain of the schizophrenic individual. Studies done, have shown (with the CT scanner) that there is an abnormality in the structure of the ventricles of the brain of male clients. Despite this finding, it is not clear that ventricular abnormality is the cause of schizophrenia, however, it has been shown that ventricular enlargement may occur in the schizophrenic client and may lead to cerebral atrophy. Studies have also shown that the hippocampus in the brain is larger in the schizophrenic client. (Delisi, 2000). It must be noted that while these findings are speculative, they could result in the view that schizophrenia is a neurologic degenerative disease.
The Neurotransmitter theory states that, brain chemicals, particularly dopamine is the major culprit. Dopamine is produced in the brain and serves as a signalling molecule or neurotransmitter, an excess or hyperactivity could be the cause of schizophrenia. Drugs effective in the control of positive symptoms in schizophrenia all seem to have a dopamine blocking action, that is, these drugs seem to work because they reduce the effect of the individuals own dopamine on his brain. It should be noted that while dopamine is speculated to be the major cause of schizophrenia, other neurotransmitters
such as GABA, and the neuropeptides cholecystokinin and somatostatin are also decreased. (Freeman, 2003).
Positive manifestations of schizophrenia are usually managed by both typical (Chlorpromazine, Haloperidol) and atypical (Resperidone, Clozapine ) psychotropic medications, but the negative manifestations are managed better by atypical medications and supportive therapy. (Black 2005). Antipsychotics have been in use since the 1950s, and several classes have evolved over time in an effort to reduce unpleasant side effects brought about by the older antipsychotics. ( Example Chlorpromazine). (Frisch, Frisch 2004). These antipsychotic are usually required to be taken over a lifetime to control the manifestations of schizophrenia, with medication some client report an absence of hallucinations, but for others internal voices become an unpleasant permanent experience. (Black 2005).
A major concern for most clients is the presence of side effects related to sedation and abnormal movements. Antipsychotics particularly, typicals, affect dopamine receptors and result in side effects known as extrapyramidal syndrome (EPS). Some of these side effects are: stiffness, tremors of the arms and legs, extreme restlessness with subjective discomfort, drooling and acute muscle spasm of the face, neck and tongue. These side effects are usually short termed and can be reversed with an anticholinergic (Benztropine). ( )
However, it should be noted that there is one long term side effect called tardive dyskinesia, which manifests itself with the following: involuntary movements of the tongue, face, hands or legs and occurs after long term antipsychotic use, usually it is irreversible. Treatment options include, changing the current medication to a less potent one or to one of the atypicals (these have a better side effect profile).
Neuroleptic malignant syndrome (NMS) is a rare, but serious, life threatening side effect that occurs from long-term use of antipsychotics, this manifest it self in the following ways: extreme muscle rigidity, hyperpyrexia, diaphoresis, high blood pressure and extreme fluctuation in conscious levels. Treatment option include, supportive therapy, to decrease temperature and keeping t with cool as well as monitoring clients vital signs and stopping the medication immediately. (Black, 2005).
Treatment options for impaired functioning include long term supportive therapy and psycho rehabilitation. Social withdrawal and lack of interest in school or work often signal the onset of the illness and may persist throughout treatment. For the schizophrenic client there is a need for development and maintenance of maximal functioning, individual counselling and support, psycho education and organized rehabilitation and family therapy.
The client experiencing schizophrenia has many remissions and exacerbations, exacerbations are compounded by medication non-compliance, denial of illness, stress life events, these will usually result in multiple admissions over a life time. With
consistent support of family and community resources, many clients can progress toward higher levels of independence. (Black, 2005) (Frisch, 2005).
Description of clients community Hope Road is one of the sub communities in the community located in Barbican in the parish of Saint Andrew. It is described as being moderately populated and is border by Halfway Tree to the left, and Liguanea to the right. It is one of the more affluent communities in Jamaica, and features mainly middle to upper class individuals. It has all the physical amenities such as light, water and sewer system, an adequate garbage disposal and telephone system as well as fine roads. Some of the facilities available in that community include: Entertainment center (Ronald Williams, Police Officers Club) Shops, Variety stores, Supermarkets, Shopping centers (Thank God its Friday, Baskin Robins, Devon House) Playing ground (Police Officers Club) Schools (including Basic, Primary and high) Churches (Seven Day Adventist, Pocomania, Faith of Light ,Church of God) The nearest Hospital is the Andrew Memorial Hospital (Private) The nearest Police Station is the Police Officers Club and Matildas corner Post Office is located in the shopping centre.
The people in the community of Hope Road are largely from middle to (lower) upper class socio-economic background. However, there are a few working class individuals
that include skilled workers who, work on construction sites and in the public and private sector. (These include professionals). Others are self employed which range from the vending of food to the keeping of shops and supermarkets.
The individuals of Hope Road are described as co-operative and friendly. Crime is not very prevalent in comparison to other parts of Jamaica.
Patients profile Name: S.F. Age: 31yrs. Gender: Male Religion: Church of God Marital Status: Single Medical Diagnosis: Schizophrenia Address: Mount Airy District Saint Thomas Next of Kin: Aunt, E.A. Occupation: worked as a caretaker and welder Height: Approximately 6ft. Weight: - 1781bs
History of present Illness Chief Complaint: According to docket and patient, he was brought to Bellevue hospital on the seventh (7th) of October 2008 by mental health officers, after they were called to say that he was on the compound of the Ardene preparatory school masturbating and denuding him in public view of the students.
History of present complaint: Client was picked up on the compound of the Ardene preparatory school on the seventh (7) of October 2008 at approximately 4:55pm. Mental health officers reported that Reverend Mr. Angling called them to lodge the complaint; he (Mr. Angling) stated that the clients parents had died about (4) four years ago. Previous to their death they had worked as caretaker at the same school, after they died he took their position. He lived in a home next door which belonged to his mother, but he burned it down in 2006, because he felt that that someone had bugged it, subsequently, he went to live on the school compound in early 2008. About 3/52 ago he began to neglect his personal hygiene, 2/52 he stated that, he started to hear voices in his head telling him to do various things, including throwing things at people and approximately 1/52 he began to denude himself as well as masturbate in front of all the school children. Parents and community members became quite concerned about the behaviour; subsequently he was brought to Emergency Room, Bellevue hospital, where he was admitted on the seventh (7) of October 2008. On examination: Young adult male sitting on chair, relatively calm and cooperative.
Temperature-97.7, Pulse rate-84 beats per minutes, Respiratory rate-20 breaths per minutes. Mucus membrane: pink, anicteric, acyanotic.
DSM IV Classification Axis I- R/O Psychotic disorder, Substance disorder, Depressive disorder, later diagnosed as Schizophrenia. Axis II- Nil Axis III- Nil Axis IV- Currently unemployed and has very little social support
Social/ developmental/Family History Client grew up with mother and father in a home that had all the physical amenities, such as electricity, piped water and adequate garbage disposal system. Mother had two (2) children, him and a younger female sibling, who is one year, his junior, she currently resides in England, but they are not in touch right now. According to client, home was a relatively happy place most of the time, with few squabbles between his sibling and himself.
Past Medical History Nil
Past Surgical History Nil
Psychosexual History Has no children and is currently not in any relationship, however, he said that he had about three relationships in the past, but they did not last very long because he was not working most of the time. His last relationship, which broke up about three years ago lasted for about six months and ended due to frequent quarrels, especially as it related to finances.
Past Psychiatric History Has never been treated for a psychiatric condition before.
Educational History Attended three primary schools, but he cannot remember their names or why he had to be moving from school to school. He looked a bit sad as he reflected on the fact that he did not do his common entrance exams. Clients docket stated that he attended Pembroke Hall, Ardene day and Extension as well as the Saint Josephs high schools however; he stated that he only attended the Saint Josephs High school where he sat 5 CXCs, and was successful in two, namely Accounts and Principle of Business. When client was spoken to again, he confirmed the high schools as stated in the dockets.
Employment History Worked as a welder for six years in Vineyard Town and as a Caretaker for the Ardene Preparatory School at 59 Hope Road. He went on to say that the last time he worked as a welder was three years ago. He left because business became very slow.
Forensic History Client was arrested for eight years, but cannot remember much about the incident.
Mental status examination Appearance: Clean and well put together, dressing appropriate for setting, age, climate and time of the day. Hair quite kempt and feet shod. Mood: Euthymic Affect: blunted/restricted (negative symptom) Speech: Low toned, clear and mainly rational Though form/process: No abnormalities detected Thought content: No delusions, paranoid ideations, however, expressed decreased self worth, as he feels that he has not maximized his full potential. Perception: Admitted to auditory hallucinations, (positive symptom) stated that he has heard voices speaking in his head from time to time, sometimes the voices tells him to throw things at staff as well as fellow patients. Orientation: Fully oriented in all spheres, time, place and person Behaviour: Very cooperative, answer questions asked,
Abstract/Cognition: Intact; was able to explain the idiomatic expressions, One, one coco full basket and Every tub must stand on its own bottom.
Memory: Recent, and remote memory are intact, he could recall events in his early childhood and could state currents events, such as the prime ministers of the recent past and the present.
Judgement: This is very good, when asked what he would do if he was locked in a room burning, he replied, that he would shout for help or try to break the window pane.
Insight: Client knows that something is wrong with him, but stated that he is not sure, but suggested that maybe something is wrong with his mind and could have resulted from his financial and social situation.
Summary of the care of A.F. Week One: 29.06. - 05.07.09 Mr. A.F. was met sitting quietly beside his bed by himself, when approached he was quiet reluctant to talk, however, after I introduced myself and what I wanted to do, he became more receptive and was quite willing to share his situation with me.
A.F. does not socialize much with the other clients, he generally takes his morning baths then sits by himself and wait for medication and breakfast to be served, at other times he may sit in the group sessions if he so inclined, then he comes back on the inside where he sits until its time for the afternoon meal and baths.
He said that most times when he is sitting by himself he hears a voice speaking in his head, this voice tells him many things, including throwing water on the staff and his fellow clients.
Mr. A.F. was encouraged to speak to at least one person each day, to attend and participate in the group therapy sessions, to assist in doing minimal ward chores, to watch television, to take his medications, and to try and not listen to the voices. In addition to these the client would, be engaged in a one to one conversation each day with yours truly.
So far the client has been very complaint with all the measures/therapies identified. He has sat in the group meetings for all the days so far and has actively participated; he has tried to speak to client N.T. who sleeps beside him.
The other aspect of his care such as hygienic needs, are done very early in the morning and in the afternoon, these the client usually accomplish by himself without any supervision.
Week Two: 06.07.2009-10.07.2009 Client received locked in seclusion room on the 06.07.2009. He reportedly threw Water at staff the previous day. When questioned why he threw the water, he gave no response but a blank stare.
Mr. A.F. was nursed in the seclusion room on a request made by the nurses from the doctor. The intent of this method was to provide behaviour modification for the client and to provide protection for him (from other patients, who wanted to beat him for the incident) for the other clients and staff. He was reviewed by the ward doctor and a decision is yet to be made concerning a change in his current medical management.
Client was allowed out of seclusion room each morning under close supervision for baths, meals, medication, and group therapy as well as one to one interaction with yours truly. On Friday client stated that he felt bad that he threw water at the staff, and that he would try very hard not to listen to the voice when it tells him to do things. (See nursing care plan for interventions).
Patients behaviour at admission On admission at the emergency Room, Young, tall, slimly built gentleman, sat very quietly and calmly in chair, was cooperative and spoke mainly rationally. He was able to indicate that the house that he lived in got burned down, and that he denuded himself because he wanted to take a bath, and not because he wanted to expose himself to the children or anybody.
Stated that he eats and sleeps very well, smokes cigarettes and smoked cocaine in the past. He also admitted to hearing voices in his head telling to do various things, however, he did not elaborate.
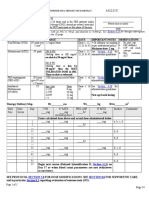
Medical Management
Medication Resperidol 4mg Cogentin 5mg
Frequency b/d (Twice daily) b/d (Twice
Mechanism of action
Side effects
Nursing Responsibility
daily) Chlorpromazine Nocte 100mg Fluphenazine Decanoate 1cc Monthly
Physical Status Examination Done: 10. 07.2009
General appearance: Client appeared alert, conscious and calm, sat by himself and seemed preoccupied with his own thoughts. Had no obvious signs of pulmonary or painful discomfort. Well nourished and appropriately dressed for setting, age, gender time of day and for season. Hair was well kempt and feet shod, however, posture was somewhat slouched and eye contact, intermittent.
Vital signs: T 37 deg. C; P-88bpm; R-20bpm; B/P-120/70 Growth (weight and height): Weight 178lbs. Height 6ft. 2 inches Skin (hair, nails): Skin colour was quite uniformed, no patches seen; same was smooth, moist with good skin turgor. No skin lesion or abrasions noted, warm to the touch. Hair was kempt and clean with adequate distribution, quantity, texture and colour. Nails were a bit long and dirty, same firmly attached to nail beds. Capillary refill of nails occurred in less than three seconds. Lymph nodes: None felt
Head: Normal, proportional to body size, skull contour smooth, no sign of trauma swelling, tenderness, nodules or lesions was seen. Neck: Symmetrical, skin intact, had no visible signs of abnormal pulsation, masses, swelling or venous distention. Thyroid gland non palpable, client was able to move neck through the entire range of motion, had no difficulty when swallowing. Trachea
remained in midline position.
Eyes: Symmetrical, no lacrimal drainage or swelling was noted. Equal distance apart, outer cantus in line with the ears. Pupils were equally round, had no tenderness on palpation, mucus membrane pink and moist.
Ears: Non tender touch, warm on palpation. No signs of hyper/hypo pigmentation, in line with the eyes, no signs of drainage nor swelling, no ceruman was seen on inspection. Nose: Colour uniformed, no signs of nasal drainage or discharge seen, no lesions or evidence of flaring. The sinus area was non tender on palpation and had no sign of swelling. Mouth and Throat: Lips were symmetrical, no swelling, same were moist, gum and mucus membranes were pink and moist, and no lesions were seen. Teeth were in line, no evidence of dental carries were noted. Tongue was pink and clean, no sign of swelling or lesions observed. Lungs: Chest expansion equal bilaterally, no abnormality was noted to chest wall, same was non- tender to touch. No flaring observed from the nares, breath sounds normal and vesicular. Client had no signs of respiratory distress/discomfort. Heart: Heart sounds were normal, S1 and S2 heard on auscultation. No obvious signs of cardiac distress detected, capillary refill was within three seconds. Chest/Thorax: Normal bilaterally, two nipples present, no hyper/hypo pigmentation or any other abnormality observed.
Abdomen/Gastrointestinal: Abdomen soft, flat and non-tender when touched, no signs of lumps bulges or masses felt or observed. Normal bowel sounds heard on auscultation, no obvious signs of abnormality were detected. Genitourinary: Made no complaint about genitalia, stated that he passed urine on a regular basis, No abnormality observed. Back and Extremities: Both sides were symmetrical, with uniformity in colour, spinal cord straight, no signs of scoliosis, kyphosis or lordosis observed. Arms and legs appeared to be of equal size, no deformities noted, however had very mild intermittent tremors of the hands. Range of motion, colour and sensation present in all four extremities. Neuromuscular: Reflex was good, range of motion to all four limbs good, although client appears sluggish at times, with intermittent tremors of the hands. Voiced no complaints of pain or tenderness on examination. Laboratory Test: Test for cocaine, marijuana and opoids was done, same was positive for cocaine.
Familys attitude towards client A.F. father is reportedly living in Portmore, but cannot be located at this time, he has not visited client since he has been admitted in hospital. Client has a sister who resides in United States, but they are not in contact with each other. There is an aunt A.F. who also lives in Greater Portmore she has visited A.F. once, but stated that she is unable to
accommodate him as there are three other persons who are mentally challenged living with her.
In terms of family support, there is no one to assist A.F. should he be discharged from the hospital; however, he stated that is just a small challenge he can over come.
Communitys attitude towards client Community was always receptive of client, but when he started to denude himself in front of the children, they became quite upset and intolerant of him and demanded that he should be treated. It should be noted that the church is quite willing to take him back as long as his condition improves. (so says Pastor Angling, the church pastor at 59 Hope Road) Clients outlook for the future/prognosis
A.E. has a very positive outlook for the future, he stated that the wants to go back to school and finish up his education so that he could provide for him, he also wants to continue working as a welder. He stated he knows that he will have challenges, but those can be overcome. Prognosis: Client will be able to live a functional life once he takes his medication, is gainfully employed, (his job at the church was given to someone else, prior to his admission), keeps his appointments at the clinic/health centre and stop the use of hard drugs.
Medical Diagnosis: Initially Psychosis, later, Schizophrenia Nursing Diagnosis: (1) Altered Sensory Perception (auditory) related to alteration in brain/neuro chemicals, (2) Risk for violence, directed against others related to auditory hallucination, (3) Social Isolation related to altered state of wellness/decreased self worth Plan of care: Medicate with antipsychotic, CPZ, 100mg. B/d, Resperidol 4mg. PO, Fluphenazine IM, 2cc, monthly, Benztropine 5mg, BD, PO, same to be finalized by doctor, Reality orientation, Group therapy, one to one and observation. Refer to Psychotherapy, Social worker and Occupational therapy when psychotic symptoms subside. Health education Evaluate level of education Identify what client knows about medication Educate about drug therapy including the name of the drug and dosage The length of time it takes to achieve therapeutic results The side effects of the drugs Report any unusual side effects Not to alter regime of the drug without first informing the doctor Encourage client to keep appointment at clinic/doctor Educate on taking sedative medication at nights Ensure that a balanced diet is consumed
Nursing Care Plan
ASSESSMENT 1. Client stated that he heard voices telling him to do things, including throwing water at people. 2. Client stated that he felt that he did not achieve as much as he could have, feels sad at times. 3. Client sits by himself most of the times, does not initiate conversation with fellow clients or staff.
DIAGNOSIS 1. Altered sensory perception (auditory) related to disturbed thought process secondary to an imbalance in neurotransmitter.
PATIENTS OBJECT. 1. Client will report/exhibit a decrease in auditory hallucinations following nursing and collaborative intervention throughout the next two weeks. 1.
INTERVENTIONS
EVALUATION Objective was
Establish one to one, for therapeutic relationship.
not achieved at the time I left the ward, client is still actively having hallucinations.
Medicate with Risperdol and Chlorpromazine to decrease psychotic symptoms.
Do not validate hallucination, to allow client to realize that they are not real.
Allow client to take part in ward chores, to take mind from off the hallucinations.
Allow client to attend group therapy session this will allow peers to evaluate condition and may help client to
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Proposal On Child ObesityDocument25 pagesProposal On Child ObesityEcaroh Hew Smailliw100% (1)
- New Adult NursingDocument14 pagesNew Adult NursingEcaroh Hew SmailliwNo ratings yet
- Diabetes Lesson PlanDocument31 pagesDiabetes Lesson PlanEcaroh Hew Smailliw0% (1)
- Study Glossary & Research QuestionsDocument58 pagesStudy Glossary & Research QuestionsEcaroh Hew SmailliwNo ratings yet
- QA Standards Nursing CareDocument57 pagesQA Standards Nursing CareEcaroh Hew SmailliwNo ratings yet
- Effecting Change in Health CareDocument17 pagesEffecting Change in Health CareEcaroh Hew SmailliwNo ratings yet
- Nursing Management of SeizuresDocument7 pagesNursing Management of SeizuresEcaroh Hew SmailliwNo ratings yet
- Care Study CompleteDocument33 pagesCare Study CompleteEcaroh Hew SmailliwNo ratings yet
- Teaching Plan For The Suicidal Client. 2018docxDocument24 pagesTeaching Plan For The Suicidal Client. 2018docxEcaroh Hew SmailliwNo ratings yet
- The Human Needs Approach, A Basic Handbook For Nursing StudentsDocument23 pagesThe Human Needs Approach, A Basic Handbook For Nursing StudentsEcaroh Hew SmailliwNo ratings yet
- Dimensions of Leadership Unit 5Document65 pagesDimensions of Leadership Unit 5Ecaroh Hew SmailliwNo ratings yet
- Teaching MethodologiesDocument2 pagesTeaching MethodologiesEcaroh Hew SmailliwNo ratings yet
- The Nursing Process IIDocument69 pagesThe Nursing Process IIEcaroh Hew SmailliwNo ratings yet
- Group Dynamics: Understanding Stages and CharacteristicsDocument75 pagesGroup Dynamics: Understanding Stages and CharacteristicsEcaroh Hew SmailliwNo ratings yet
- Politics and Power Bases Unit 2Document43 pagesPolitics and Power Bases Unit 2Ecaroh Hew SmailliwNo ratings yet
- Dosage and CalculationsDocument9 pagesDosage and CalculationsEcaroh Hew SmailliwNo ratings yet
- Learning StylesDocument21 pagesLearning StylesEcaroh Hew SmailliwNo ratings yet
- Study Glossary & Research QuestionsDocument58 pagesStudy Glossary & Research QuestionsEcaroh Hew SmailliwNo ratings yet
- The Significance of Research in Nursing Lesson PlanDocument21 pagesThe Significance of Research in Nursing Lesson PlanEcaroh Hew SmailliwNo ratings yet
- Ethical Issues Nursing ResearchDocument13 pagesEthical Issues Nursing ResearchEcaroh Hew Smailliw0% (1)
- Digoxin Cardiac Glycosides PO/IV: Sample Card For DigoxinDocument2 pagesDigoxin Cardiac Glycosides PO/IV: Sample Card For DigoxinEcaroh Hew SmailliwNo ratings yet
- Client Assessment ToolDocument10 pagesClient Assessment ToolEcaroh Hew SmailliwNo ratings yet
- Nursing Care of Anxiety DisordersDocument21 pagesNursing Care of Anxiety DisordersEcaroh Hew Smailliw0% (1)
- Nursing Management of Myomatous/Uterine FibroidsDocument38 pagesNursing Management of Myomatous/Uterine FibroidsEcaroh Hew Smailliw100% (1)
- Teaching MethodologiesDocument2 pagesTeaching MethodologiesEcaroh Hew SmailliwNo ratings yet
- Check For Medication StepsDocument2 pagesCheck For Medication StepsEcaroh Hew SmailliwNo ratings yet
- Group Communication PatternsDocument70 pagesGroup Communication PatternsEcaroh Hew Smailliw50% (2)
- Learning StylesDocument21 pagesLearning StylesEcaroh Hew SmailliwNo ratings yet
- Nursing Care of Anxiety DisordersDocument21 pagesNursing Care of Anxiety DisordersEcaroh Hew Smailliw0% (1)
- Alzheimer's Teaching PlanDocument22 pagesAlzheimer's Teaching PlanEcaroh Hew SmailliwNo ratings yet
- Package - Insert - 08586 - H - en - 30427 - CA 19-9 PDFDocument8 pagesPackage - Insert - 08586 - H - en - 30427 - CA 19-9 PDFadybaila4680No ratings yet
- I. Bedsores A. What Are Bedsores?Document3 pagesI. Bedsores A. What Are Bedsores?peter911xNo ratings yet
- Medication Instructions Prior To SurgeryDocument11 pagesMedication Instructions Prior To Surgeryhohj100% (1)
- BarlingFrone 2004 ThePsychologyofWorkplaceSafteyDocument336 pagesBarlingFrone 2004 ThePsychologyofWorkplaceSafteyfitrianiNo ratings yet
- Postnatal Exercises Improve Quality of LifeDocument4 pagesPostnatal Exercises Improve Quality of LiferohiniNo ratings yet
- Article. Neoadjuvant Treatment Response As An Early Response Indicator For Patients With Rectal CancerDocument7 pagesArticle. Neoadjuvant Treatment Response As An Early Response Indicator For Patients With Rectal CancerTrí Cương NguyễnNo ratings yet
- What is GastroschisisDocument6 pagesWhat is GastroschisisAnonymous MWd5UOUuiyNo ratings yet
- Resusciation Equipments in IcuDocument29 pagesResusciation Equipments in Icuvinoli100% (1)
- Forensic ToxicologyDocument7 pagesForensic ToxicologyLaiba Jahangir100% (2)
- PPM Action Plan - 13 - 01 - 2022Document128 pagesPPM Action Plan - 13 - 01 - 2022whoosh2008No ratings yet
- ImmerciDocument14 pagesImmercitextilessathishNo ratings yet
- Lecture Notes General SurgeryDocument16 pagesLecture Notes General SurgeryHamsa VeniNo ratings yet
- High Risk B-Precursor Acute Lymphoblastic Leukemia Interim Maintenance IIDocument1 pageHigh Risk B-Precursor Acute Lymphoblastic Leukemia Interim Maintenance IIRitush MadanNo ratings yet
- Sanaani, Wallie Jr.Document10 pagesSanaani, Wallie Jr.Nur SetsuNo ratings yet
- Nursing Care for High-Risk Pregnant MothersDocument40 pagesNursing Care for High-Risk Pregnant MothersAllyza EspirituNo ratings yet
- Fall Risk Factors and Fall Risk Assessment of InpatientsDocument9 pagesFall Risk Factors and Fall Risk Assessment of Inpatientskang soon cheolNo ratings yet
- Compilation Liver Cirrhosis (4) - 1Document45 pagesCompilation Liver Cirrhosis (4) - 1Nagabharana Hm HollattiNo ratings yet
- Policy: NUMBER: 3.3.2R3Document24 pagesPolicy: NUMBER: 3.3.2R3Myle26No ratings yet
- Daftar Pustaka Presentasi BokongDocument2 pagesDaftar Pustaka Presentasi BokongNando UspessyNo ratings yet
- Reaksi Hipersensitivitas Atau Alergi: RiwayatiDocument7 pagesReaksi Hipersensitivitas Atau Alergi: Riwayatiaulia nissaNo ratings yet
- Ejsr 72 3 04Document9 pagesEjsr 72 3 04Khalifa BakkarNo ratings yet
- Create PDFDocument10 pagesCreate PDFAthanasia SergouniotiNo ratings yet
- Nursing Case Study - With Final Slides.Document77 pagesNursing Case Study - With Final Slides.veejai_kumar100% (2)
- Antimicrobial Mouthwash - Google SearchDocument1 pageAntimicrobial Mouthwash - Google Searchbruce kNo ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakamemeeeyyyNo ratings yet
- Nursing Grand Rounds Reviewer PDFDocument17 pagesNursing Grand Rounds Reviewer PDFAlyssa Jade GolezNo ratings yet
- KKDAT LectureDocument46 pagesKKDAT Lecturejoshua fernandezNo ratings yet
- Sinusitis LectureDocument66 pagesSinusitis LectureDada Doni100% (2)
- Fi ADocument67 pagesFi AalfonsoNo ratings yet
- EMDR Scripted Protocols Index by Marilyn Luber PHDDocument4 pagesEMDR Scripted Protocols Index by Marilyn Luber PHDcebanova1994No ratings yet