Professional Documents
Culture Documents
Chemotherapy Response Evaluation in Metastatic Colorectal Cancer With FDG PET/CT and CT Scans
Uploaded by
Bagus OkaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chemotherapy Response Evaluation in Metastatic Colorectal Cancer With FDG PET/CT and CT Scans
Uploaded by
Bagus OkaCopyright:
Available Formats
ANTICANCER RESEARCH 29: 2563-2568 (2009)
Chemotherapy Response Evaluation in Metastatic Colorectal Cancer with FDG PET/CT and CT Scans
J. MONTEIL1, N. MAHMOUDI2, S. LEOBON2, P.Y. ROUDAUT3, A. EL BADAOUI1, S. VERBEKE1, L. VENAT-BOUVET2, J. MARTIN2, V. LE BRUN-LY2, S. LAVAU-DENES2, A. MAUBON3, P. BOUILLET3, M. POUQUET3, J.C. VANDROUX1 and N. TUBIANA-MATHIEU2
3Radiology
Departments of 1Nuclear Medicine, 2Medical Oncology, and Medical Imaging, University Hospital of Limoges, France
Abstract. Background: [18F]-fluorodeoxyglucose with positron-emission tomography (PET) and computed tomography (CT) scans were used to assess morphological and metabolic tumour response after chemotherapy in metastatic colorectal cancer. Patients and Methods: Twentyfive patients were evaluated after 4 courses of chemotherapy (target therapy), and among them 20 patients after 2 courses. Response Evaluation Criteria In Solid Tumors (RECIST) and European Organisazion for Research and Treatment of Cancer (EORTC) criteria were used to evaluate CT and PET respectively. Results: Discrepancies between the two procedures were noted after 4 courses of chemotherapy in patient-based analysis. Two morphologically complete responses (CR) were correlated with metabolic response. Seven morphological partial responses (PR) were evaluated as 3 metabolic PR, 2 CR and 1 progressive disease (PD). Seventeen cases of morphologically stable disease (SD) were evaluated as 3 metabolic CR, 13 PR and 1 PD. These discrepancies were confirmed in lesion-based analysis. Perfect concordance was noted between metabolic responses obtained after 2 and 4 cycles. Conclusion: Morphological and metabolic imaging does not permit concordant therapeutic assessment in metastatic colorectal cancer.
One of the major challenges in the treatment of metastatic colorectal cancer is the assessment of tumour response after chemotherapy. Positron-emission tomography (PET) with the glucose analogue 2-(F-18) fluoro-2-deoxy-D-glucose ([18F]-FDG) has emerged as a method for staging and
Correspondence to: Nicole Tubiana-Mathieu, Service dOncologie Mdicale, Hpital Dupuytren, 2 avenue Martin Luther King, 87042 Limoges Cedex, France. Tel: +33 555056100/Fax: +33 555056398, e-mail: oncologie@chu-limoges.fr Key Words: [18F]-FDG, PET-CT, CT scan, metastatic colorectal cancer, therapeutic assessment.
monitoring the response to treatment in a variety of cancer types. Increased glycolysis is one of the characteristics of tumour tissue (1). The enhanced uptake of [18F]-FDG is used for diagnosis, staging of cancer and detection of residual cancer. In colorectal cancer, PET has a higher sensitivity and specificity than computed tomography (CT) and is recommended before surgical resection mainly for metastatic liver lesions (2). PET modifies surgical indication in 20 to 30% of patients with colorectal cancer (3, 4), and 30 to 40% globally in the management of cancer regardless of origin (5). Within the last five years, PET/CT has nearly replaced standalone PET for imaging cancer patients due to its higher staging accuracy than PET or CT alone (6). PET allows for response assessment early after the beginning of chemotherapy, at the second course (7) and, in malignant lymphoma, even at the first course (8). In the majority of studies, no significant difference between the [18F]-FDG uptake of responding tumours and that of non-responding tumours was observed in the baseline scans, but most responding tumours show a decrease of FDG uptake early, after beginning chemotherapy or radio chemotherapy (9). Today, except for the European Association for Research and Treatment of Cancer (EORTC) recommendations, there are no generally accepted criteria for a metabolic response in [18F]-FDG PET studies (10). The EORTC published preliminary criteria for the assessment of tumour response in 1999 (7), however at that time, limited data on the use of [18F]-FDG PET for treatment monitoring were available. Since then, a large number of studies using different technologies and materials in treatment monitoring with [18F]-FDG PET have been published. Furthermore, targeted therapies used in colorectal cancer modify the response assessment. Morphological imaging modalities are not well suited compared to metabolic imaging to evaluating targeted therapy in cancer. The purpose of this study was to compare the evaluation of response after chemotherapy using FDG PET and
0250-7005/2009 $2.00+.40
2563
ANTICANCER RESEARCH 29: 2563-2568 (2009)
helicoidal CT in patients with metastatic colorectal cancer principally for liver metastases. RECIST (11) and EORTC criteria were used for CT and PET evaluation respectively. Thus, we analyzed standard uptake value (SUV) max parameter, SUV mean and metabolic tumour volume, to be compared with RECIST criteria.
Partial metabolic response (PMR): a reduction of a minimum of 1525% in tumour [18F]-FDG SUV after one cycle of chemotherapy, or greater than 25% after more than one treatment cycle. A reduction in the extent of the tumour [18F]-FDG uptake is not a requirement for partial metabolic response. Complete metabolic response (CMR): complete resolution of [18F]-FDG uptake within the tumour volume so that it was indistinguishable from surrounding normal tissue. CT analysis. CT scans were performed with a helical multidetector CT (Light Speed Ultra and Light Speed VCT, General Electrics, Fairfield, USA). All patients were intravenously injected with contrast material. Tumour size was evaluated for each lesion in the longest cross sectional dimension. Based on RECIST, the sum of the longest dimensions of selected lesions in each patient was computed, and the percentage change of the sum pre-treatment and after 4 cycles of treatment was calculated. The assessment of response evaluated by CT was performed according to RECIST criteria: Complete response (CR): disappearance of all target lesions. Partial response (PR): at least a 30% decrease in the sum of the longest diameters (LD) of target lesions, taking the baseline sum LD as a reference. Progressive disease (PD): at least a 20% increase in the sum of the LD of target lesions, taking as reference the smallest sum LD recorded since the treatment started or the appearance of one or more new lesions. Stable disease (SD): neither sufficient shrinkage to qualify for PR nor sufficient increase to quality for PD. CT scans were reviewed by a radiologist with a clinician blinded to patient outcome and results of PET scan. Carcinoembryonic antigen (CEA) and CA19-9 marker analysis. Markers were measured in serum with an automated immunofluorescent assay (Brahms CEA Kryptor and Brahms CA19-9 Kryptor). Kryptor is based on TRACE Technology (time-resolved amplified cryptate emission), which measures the signal that is emitted from an immunocomplex with time delay (Brahms Aktiengesellschaft, Hennigsdorf, Germany). Statistical analysis. Statistical analyses were performed with the Stat View system for Windows, version 9.1.3 (SAS Institute, Cary, NC, USA). Quantitative values were expressed as mean (range) and qualitative values as percentage.
Patients and Methods
The study was performed from September 2006 to December 2007. Twenty-five patients were included in our study, and a total of 90 metastatic lesions were selected on the basis of RECIST criteria. All the patients were treated for metastatic colorectal cancer. Patient characteristics are listed in Table I. Patients included 10 females and 15 males with a median age of 64 years (range 36-77 years). The primary tumour was located in the colon in 19 patients and in the rectum in 6 patients. The median delay between metastases and primary diagnosis was 13 months (range 0-66 months). The sites were principally hepatic, but many patients presented multiple sites (Table I). Twenty patients received chemotherapy for first-line therapy, and 5 patients for second- or third-line. The chemotherapy protocols were 5FU, leucovorin, irinotecan (FOLFIRI) (13 patients); 5-FU, leucovorin, oxaliplatin (FOLFOX) (12 patients); and chemotherapy associated with targeted therapy (bevacizumab in 9 and cetuximab in 1 patient). The patients were systematically evaluated with CT and PET before and after chemotherapy, principally after the fourth course. Evaluations performed with over 5 weeks between CT and PET imaging and/or less than 10 days between chemotherapy and PET imaging were excluded from the analysis. Some patients were also evaluated earlier (after the second course) to analyse early metabolic response (7). FDG-PET was performed using Biograph 6 PET/CT (Siemens Medical Imaging Systems, Knoxville, USA). Patients were injected with [18F]-FDG (5.5 MBq/kg). All patients had fasted for at least 6 hours before the examination. PET was performed only when the blood glucose level did not exceed 7.8 mol/l. After 60 to 115 minutes of uptake (mean=80 min 11), patients were scanned from neck to pelvis. All PET scans were blindly analysed by the same experienced nuclear medicine physician. PET analysis. As recommended by the EORTC PET study group, the tumour area defined on the pre-treatment PET was drawn on the region of high [18F]-FDG uptake, representing viable tumour. A lesion was considered malignant, if its glucose uptake was found to be above levels of the surrounding tissue, with a SUVmax higher than 2.5 (3.5 for the liver) supporting the diagnosis of malignancy. The SUV was calculated using the tumour radiotracer concentration (MBq/l), body surface area and injected activity SUV normalised for body surface area. SUVmean, SUVmax and metabolic volume of the viable tumour were systematically evaluated. EORTC response assessment criteria were used defined as follows: Progressive metabolic disease (PMD): an increase in [18F]-FDG tumour SUV of 25% within the tumour region defined on the baseline scan, visible increase in the extent of [18F]-FDG tumour uptake (20% in the longest dimension) or the appearance of new [18F]-FDG uptake in metastatic lesions. Stable metabolic disease (SMD): an increase in tumour [18F]FDG SUV of less than 25% or a decrease of less than 15% , and no visible increase in the extent of [18F]-FDG tumour uptake (20% in the longest dimension).
Results
All 25 patients were evaluated by CT and PET, before chemotherapy and after the fourth course, with a median delay between the two procedures of 14 days (range 0-37) and 4 days (range 0-9) respectively. Twenty patients were evaluated earlier, after the second course, by PET, with a median delay of 11 days (range 4-18) between chemotherapy course and PET. The total number of targets was 90 with PET and 76 with CT. Discordances were noted in 15 patients. In eleven patients, more sites were noted on PET than on CT: 2 peritoneal localizations, 5 in liver, 3 in nodes and 1 in pelvis.
2564
Monteil et al: Chemotherapy Evaluation by FDG-PET and CT
Table I. Patient characteristics. Variable Age (years) Median Gender Female/male Location of primary tumour, n (% ) Colon/rectum Histology: adenocarcinoma, n (% ) Mucinous Non-mucinous Unknown Differentiation of primary tumour, n (% ) Poor Intermediate Well Unknown Location of metastases, n (% ) Liver Lung Nodes Peritoneum Pelvis Other (bone, surrenal) Number of metastatic sites/patient Median Mean (range) N=25
Table II. Comparison between morphological RECIST and metabolic EORTC criteria. N=25 64 (range 36-77) 10 (40% )/15 (60% ) 19 (76% )/6 (24% ) 2 (8% ) 21 (84% ) 2 (8% ) 2 (8% ) 9 (36% ) 12 (48% ) 2 (8% ) 17 (68% ) 14 (56% ) 5 (20% ) 5 (20% ) 3 (12% ) 3 (12% ) 2 2 (1-5) Metabolic EORTC criteria CR PR SD PD Total Morphological RECIST criteria CR 2 0 0 0 2 PR 2 3 0 1 6 SD 3 13 0 1 18 Total 7 16 0 2 25
CR: Complete response; PR: partial response; SD: stable disease; PD: progressive disease.
parameters showed the same variations of response. Discordances were described in one patient classified in PD by a 118% increase of SUVmax analysis. This patient presented a 41% decrease of the metabolic volume and a stable diameter evaluation. Notably, this patient was considered as partial responder with CT. Evaluation by PET after the second course of chemotherapy: Twenty patients were evaluated after the second course. Fourteen patients presented the same response after the second and the fourth course. Four patients were PR after C2 and CR after C4, and two patients were stable after C2 and PR after C4. PET visual image analysis (lesion-based). Only 50 locations detected with the 2 modalities were compared. As shown in the patient-based analysis, all morphological CR were concordant with PET (3 targets). CT and PET discrepancies were noted for morphological PR and SD in 34/50 locations. In the liver, 11 morphological PR were considered as 9 metabolic CR and 2 PR; 9 morphological SD as 2 metabolic CR, 5 PR, 1 SD and 1 PD. In the lung, 16 morphological SD were considered as 4 metabolic CR, 8 PR and 4 SD. ACE and CA19-9 markers. Serum markers were systematically assessed prior to chemotherapy and when abnormal (13 patients) after the 4 courses of chemotherapy. Evaluation of tumour marker changes is presented in Table IV. Variations of only 7 markers were concordant with CT results and 11 with PET results. Variations of 6 markers were discordant with CT and 2 with PET evaluation. Follow-up. The median follow-up between first imaging and last contact was 20 months (range 6-29 months). Seven patients died in a median of 12 months. All patients in metabolic CR were alive with a median progression-free survival of 20 months (range 19-27 months). Survival analysis has not been performed because of the small number of patients and the different lines of treatment.
Four patients had more sites in CT than in PET: 2 liver localizations (around 1cm), 1 node and 1 lung target. Table II shows the treatment responses obtained on CT in the 25 patients: 8 patients were classified as responders (2 CR, 6 PR) and 17 presented SD. No patient presented PD during this study. We defined 3 groups of patients using RECIST criteria: groups I (CR), II (PR) and III (SD). PET analysis (patient-based). PET quantitative image analysis: Evaluation response by PET quantitative analysis using SUV max criteria is shown in Table II. In group I, the 2 patients were also considered to be in metabolic CR. In group II, 3 results were concordant and patients were considered to be in PR (with a median decrease in SUVmax of 70% (range 69-74)); of 2 patients considered to be in morphological PR, 1 was considered by PET to be in CR, and 1 to be in PD (SUVmax increase of 89% ). In group III, all 17 patients were classified otherwise by PET: 1 was progressive (increase in SUVmax of 118% ), 13 were considered in PR (decrease in SUVmax of 60% (range 22-89), and 3 in CR. Correlation between different parameters obtained with PET: Three other parameters were studied in PET analysis: volume, largest diameter and SUVmean. As shown in Table III, a good correlation was obtained between these three parameters and SUVmax. In CR and PR patients, the 3
2565
ANTICANCER RESEARCH 29: 2563-2568 (2009)
Table III. Correlation between different PET parameters. SUVmax Decrease n (% ) CR (n=7) PR (n=16) PD (n=2) 7 (100% ) 16 (14% -84% ) 2 (20% -93% ) SUVmean Increase n (% ) Metabolic volume Decrease n (% ) 7 (100% ) 16 (7% -96% ) 1 (41% )* Increase n (% ) Decrease n (% ) 7 (100% ) 16 (15% -78% ) 1 (60% ) 1 (0% )* 1 (74% ) Metabolic diameter Stable n (% ) Increase n (% )
n: Number of patients and (% ) is the percentage of variation. *Patient evaluated as partial responder by CT.
Discussion
Therapeutic response assessment in metastatic colorectal cancer is fundamental in order to change an ineffective but possibly toxic chemotherapy protocol or to decide surgical resection. Our study shows great discrepancies between CT and PET. CT is the gold standard procedure for diagnosis and chemotherapy response evaluation in this pathology (11). Metabolic response evaluation by FDG PET appears promising (10), but needs to be defined precisely. The aim of this study was the evaluation of our medical practices in metastatic colorectal cancer. Our study is considered retrospective, but all the data were prospectively registered as is usually performed in our institution. All patients tumours were metastatic, but differences were noted in locations, therapeutic lines and protocols (with or without target therapies). Discordant results obtained in our study could be related, in part, to these heterogeneities. However, our study reflects daily problems in the therapeutic management of metastatic patients. The two imaging modalities differ in their evaluation: CT determines tumour size, while PET assesses metabolic activity in whole-body scanning. Therapy response in solid tumours is currently assessed by measuring change in tumour size. RECIST defines standard measurement methods to evaluate response therapy by CT (11). But CT does not permit characterization of tumour heterogeneity and its change over time. CT measurements are dependent on the expertise of the observer, and discrepancies among observers have been described to be as high as 15 to 40% (12). FDG PET reflects glucidic metabolism of the tumor and FDG uptake clearly depends not only on the size and shape of the lesion, but also on the biological activity. Metabolic response criteria described by EORTC (7) have been developed from a great number of small studies, performed on multiple types of tumours (including metastatic colorectal cancer) prior to 2000. However, over the last decade, many
Table IV. Markers and treatment response evaluation by CT compared to PET. Serum markers Morphological RECIST criteria 2 RP 5 SD* 1 RC 2 RP 2 SD 1 SD* Metabolic EORTC criteria 1 RP, 1 PD* 2 RC, 3 RP 1 RC 2 RP 2 RP 1 RP*
Normalized (n=7)
Decrease from 36 to 50% (n=5)
Progression (n=1)
*Discordant result between marker evolution and imaging evaluation.
improvements were reported in machine performance and in therapy introducing targeted therapies. The limitations of PET are well known. The spatial resolution of PET is limited and lesions smaller than 1 cm often go undetected. Limitation in PET evaluation has been described particularly for nodes: false-positive findings in enlarged inflammatory nodes or false-negative findings in normalized nodes harbouring micrometastases are usual (13). This could explain the discrepancies in the number of targets selected by the two imaging modalities in our study. The SUV value is dependent on the lesion size: for a tumour smaller than 1.5 cm, the estimated SUV is 30% of real activity (14). The delay between injection of [18F]-FDG and imaging is a classical pitfall: there is an SUV increase of 50% between 40 and 90 min, and a plateau between 90 and 180 min (15); but in our study, no significant variation in acquisition delay was noted (80 min 11). Moreover, histological features could explain the variation in SUVmax levels (13). In our study, all tumours were adenocarcinomas (n=25) and only 2 contained mucinous contingent; regardless, all selected patients had PETpositive tumours before chemotherapy.
2566
Monteil et al: Chemotherapy Evaluation by FDG-PET and CT
Assessment of tumour metabolic boundaries is operator dependent (16). Measurement of the boundaries is complicated by necroses which cause internal heterogeneity (12). Another difficulty is the respiratory motion of the lungs, the thoracic wall and the liver during PET emission and CT acquisition (17). Chemotherapy may change FDG tumour uptake by altering cellular metabolism, with a significantly decrease in tumour cell hexokinase activity. To limit this effect, delay between chemotherapy and PET timings was superior or equal to 10 days. In spite of the technical limitations of PET, this metabolic imaging modality permits major improvement in tumour evaluation. PET has shown higher sensitivity than CT in pretreatment screening in metastatic colorectal cancer. In therapeutic evaluation, discordances between metabolic and morphological imaging have been underlined. In highgrade lymphoma, therapeutic evaluation by FDG/PET is a fundamental tool, routinely used (18). For solid tumours, metabolic imaging has still to confirm its place. In lung carcinomas, discrepancies have been described in 79 patients with non-small cell lung cancer treated by radiotherapy or chemoradiotherapy: 30 were in CR with PET, while only 10 were in CR by CT (19). In colorectal cancer, PET plays an important role in avoiding surgery in patients for whom curative surgery is not possible. In rectal cancer, PET response assessment of preoperative radiochemotherapy described by Guillem et al. confirmed a pathological response obtained by chemoradiotherapy in all patients by PET compared to 78% by CT (20). For the same assessment, PET was superior to endorectal ultrasound (21). Assessment of chemotherapy response in metastatic colorectal cancer is limited to a small series of patients with no resectable liver metastases. More recently, de Geus-Oei et al. noted that tumour glucose metabolism, prior and after 2 and 6 months of chemotherapy, was highly predictive of patient outcome (22). However, in another study performed with or without neoadjuvant chemotherapy before liver metastatic surgery, in patients without chemotherapy FDG-PET sensitivity was 93.3% and CT scan 87.5% . After chemotherapy, FDGPET sensitivity was 49% compared to 65.3% for CT (23). FDG uptake normalisation by colorectal liver metastases has been described to not usually indicate complete pathological response (24). Moreover, targeted therapy, major evolution in metastatic colorectal cancer treatment, is particularly well evaluated by metabolic imaging as in gastrointestinal stromal tumour treated by imatinib (25, 26). Early response evaluation is a challenge to adapt therapy in these aggressive diseases. To this aim, FDG-PET is more efficient than CT. In patients with different solid tumours treated by preoperative chemotherapy, a 35-50% FDG decrease within the initial weeks of chemotherapy has been found to provide the highest accuracy for prediction of histopathological complete or subtotal tumour regression (7).
Our results showed a nearly perfect concordance between the results obtained after the second and the fourth cycle; four cases showed a PR that was converted to a CR after the fourth course and two patients presented response only after 4 courses. These results confirm the feasibility of a very early evaluation with FDG-PET. The measurement of the level of serum markers (CA19-9 or ACE) is another conventional tool to evaluate therapeutic response. In our study, markers were systematically evaluated and their changes correlated more with PET than with CT results. In spite of numerous unsolved problems, the National Cancer Institute recently highlighted the importance of [18F]-FDG PET in assessing therapeutic efficacy and has published recommendations for acquiring PET imaging in clinical trials (10). Assessment of treatment response is still challenging and our study confirms the difficulties in selecting the best approach. At baseline, the best metastatic colorectal cancer staging should be the association of morphological and metabolic imaging modalities. Patient management, with possible metastasis resection or only therapy monitoring, must lead to the appropriate imaging. Randomized studies will be required to validate the impact of treatment monitoring with PET/CT on disease management.
References
1 Kelloff GJ, Hoffman JM, Johnson B, Scher HI, Siegel BA, Cheng EY, Cheson BD, OShaughnessy J, Guyton KZ, Mankoff DA, Shankar L, Larson SM, Sigman CC, Schilsky RL and Sullivan DC: Progress and promise of FDG-PET imaging for cancer patient management and oncologic drug development. Clin Cancer Res 11: 2785-2808, 2005. 2 Hustinx R, Paulus P, Jacquet N, Jerusalem G, Bury T and Rigo P: Clinical evaluation of whole-body 18F-fluorodeoxyglucose positron-emission tomography in the detection of liver metastases. Ann Oncol 9: 397-401, 1998. 3 Fong Y, Saldinger PF, Akhurst T, Macapinlac H, Yeung H, Finn RD, Cohen A, Kemeny N, Blumgart LH and Larson SM: Utility of 18F-FDG positron-emission tomography scanning on selection of patients for resection of hepatic colorectal metastases. Am J Surg 178: 282-287, 1999. 4 Ruers TJ, Langenhoff BS, Neeleman N, Jager GJ, Strijk S, Wobbes T, Corstens FH and Oyen WJ: Value of positronemission tomography with [F-18]fluorodeoxyglucose in patients with colorectal liver metastases: a prospective study. J Clin Oncol 20: 388-395, 2002. 5 Hillner BE, Siegel BA, Liu D, Shields AF, Gareen IF, Hanna L, Stine SH and Coleman RE: Impact of positron-emission tomography/computed tomography and positron-emission tomography (PET) alone on expected management of patients with cancer: initial results from the National Oncologic PET Registry. J Clin Oncol 26: 2155-2161, 2008. 6 Weber WA and Figlin R: Monitoring cancer treatment with PET/CT: does it make a difference? J Nucl Med 48(Suppl 1) : 36S-44S, 2007.
2567
ANTICANCER RESEARCH 29: 2563-2568 (2009)
7 Young H, Baum R, Cremerius U, Herholz K, Hoekstra O, Lammertsma AA, Pruim J and Price P: Measurement of clinical and subclinical tumour response using [18F]-fluorodeoxyglucose and positron-emission tomography: review and 1999 EORTC recommendations. European Organization for Research and Treatment of Cancer (EORTC) PET Study Group. Eur J Cancer 35: 1773-1782, 1999. 8 Hoekstra OS, Ossenkoppele GJ, Golding R, van Lingen A, Visser GW, Teule GJ and Huijgens PC: Early treatment response in malignant lymphoma, as determined by planar fluorine-18fluorodeoxyglucose scintigraphy. J Nucl Med 34: 1706-1710, 1993. 9 Weber WA: Use of PET for monitoring cancer therapy and for predicting outcome. J Nucl Med 46: 983-995, 2005. 10 Shankar LK, Hoffman JM, Bacharach S, Graham MM, Karp J, Lammertsma AA, Larson S, Mankoff DA, Siegel BA, Van den Abbeele A, Yap J and Sullivan D: Consensus recommendations for the use of 18F-FDG PET as an indicator of therapeutic response in patients in National Cancer Institute Trials. J Nucl Med 47: 1059-1066, 2006. 11 Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC and Gwyther SG: New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92: 205-216, 2000. 12 Jaffe CC: Measures of response: RECIST, WHO, and new alternatives. J Clin Oncol 24: 3245-3251, 2006. 13 Cachin F, Kelly A and Maublant J: Evaluation of the therapeutic response: role of isotopic imaging. Bull Cancer 93: 1191-1199, 2006 (in French). 14 Thie JA: Understanding the standardized uptake value, its methods, and implications for usage. J Nucl Med 45: 1431-1434, 2004. 15 Stahl A, Ott K, Schwaiger M and Weber WA: Comparison of different SUV-based methods for monitoring cytotoxic therapy with FDG PET. Eur J Nucl Med Mol Imaging 31: 1471-1478, 2004. 16 Jerusalem G and Belhocine TZ: Metabolic monitoring of chemosensitivity with 18F-FDG PET. Methods Mol Med 111: 417-440, 2005. 17 Boucher L, Rodrigue S, Lecomte R and Benard F: Respiratory gating for 3-dimensional PET of the thorax: feasibility and initial results. J Nucl Med 45: 214-219, 2004. 18 Jerusalem G, Beguin Y, Fassotte MF, Najjar F, Paulus P, Rigo P and Fillet G: Whole-body positron-emission tomography using 18F-fluorodeoxyglucose for posttreatment evaluation in Hodgkins disease and non-Hodgkins lymphoma has higher diagnostic and prognostic value than classical computed tomography scan imaging. Blood 94: 429-433, 1999. 19 Mac Manus MP, Hicks RJ, Matthews JP, McKenzie A, Rischin D, Salminen EK and Ball DL: Positron-emission tomography is superior to computed tomography scanning for response assessment after radical radiotherapy or chemoradiotherapy in patients with non-small cell lung cancer. J Clin Oncol 21: 12851292, 2003. 20 Guillem JG, Puig-La Calle J, Jr., Akhurst T, Tickoo S, Ruo L, Minsky BD, Gollub MJ, Klimstra DS, Mazumdar M, Paty PB, Macapinlac H, Yeung H, Saltz L, Finn RD, Erdi Y, Humm J, Cohen AM and Larson S: Prospective assessment of primary rectal cancer response to preoperative radiation and chemotherapy using 18-fluorodeoxyglucose positron-emission tomography. Dis Colon Rectum 43: 18-24, 2000. 21 Amthauer H, Denecke T, Rau B, Hildebrandt B, Hunerbein M, Ruf J, Schneider U, Gutberlet M, Schlag PM, Felix R and Wust P: Response prediction by FDG-PET after neoadjuvant radiochemotherapy and combined regional hyperthermia of rectal cancer: correlation with endorectal ultrasound and histopathology. Eur J Nucl Med Mol Imaging 31: 811-819, 2004. 22 de Geus-Oei LF, van Laarhoven HW, Visser EP, Hermsen R, van Hoorn BA, Kamm YJ, Krabbe PF, Corstens FH, Punt CJ and Oyen WJ: Chemotherapy response evaluation with FDG-PET in patients with colorectal cancer. Ann Oncol 19: 348-352, 2008. 23 Lubezky N, Metser U, Geva R, Nakache R, Shmueli E, Klausner JM, Even-Sapir E, Figer A and Ben-Haim M: The role and limitations of 18-fluoro-2-deoxy-D-glucose positron-emission tomography (FDG-PET) scan and computerized tomography (CT) in restaging patients with hepatic colorectal metastases following neoadjuvant chemotherapy: comparison with operative and pathological findings. J Gastrointest Surg 11: 472-478, 2007. 24 Tan MC, Linehan DC, Hawkins WG, Siegel BA and Strasberg SM: Chemotherapy-induced normalization of FDG uptake by colorectal liver metastases does not usually indicate complete pathologic response. J Gastrointest Surg 11: 1112-1119, 2007. 25 Benjamin RS, Choi H, Macapinlac HA, Burgess MA, Patel SR, Chen LL, Podoloff DA and Charnsangavej C: We should desist using RECIST, at least in GIST. J Clin Oncol 25: 1760-1764, 2007. 26 Choi H, Charnsangavej C, Faria SC, Macapinlac HA, Burgess MA, Patel SR, Chen LL, Podoloff DA and Benjamin RS: Correlation of computed tomography and positron-emission tomography in patients with metastatic gastrointestinal stromal tumor treated at a single institution with imatinib mesylate: proposal of new computed tomography response criteria. J Clin Oncol 25: 1753-1759, 2007.
Received February 24, 2009 Revised April 30, 2009 Accepted May 5, 2009
2568
You might also like
- Clinical Impact of FDG PET-CT On Management Decisions For Patients With Primary Biliary TumoursDocument10 pagesClinical Impact of FDG PET-CT On Management Decisions For Patients With Primary Biliary TumourslkitkatgirlNo ratings yet
- 11C MetioninaDocument8 pages11C MetioninaPUIGCOZARNo ratings yet
- PET in OncologyDocument70 pagesPET in Oncologyg_daniel119974No ratings yet
- Artigo de Pet No Monitoramento Precoce Do LinfomaDocument7 pagesArtigo de Pet No Monitoramento Precoce Do LinfomagustavoandradeambrosioNo ratings yet
- Diagnostic Accuracy of F-Methylcholine Positron Emission Tomography/Computed Tomography For Intra-And Extrahepatic Hepatocellular CarcinomaDocument11 pagesDiagnostic Accuracy of F-Methylcholine Positron Emission Tomography/Computed Tomography For Intra-And Extrahepatic Hepatocellular CarcinomaRais KhairuddinNo ratings yet
- Nodal - Multi-Institut Oligo - Plus COREDocument13 pagesNodal - Multi-Institut Oligo - Plus COREsilviuNo ratings yet
- Permenkes Tentang Penetapan Nilai KritisDocument34 pagesPermenkes Tentang Penetapan Nilai KritisMeutia sariNo ratings yet
- F-FDG PET CT As A Prognostic Factor in Hepatocellular CarcinomaDocument7 pagesF-FDG PET CT As A Prognostic Factor in Hepatocellular CarcinomaUvi Cancino RamosNo ratings yet
- PET-CT Radiomics in Breast Cancer - Promising Tool For PredictionDocument10 pagesPET-CT Radiomics in Breast Cancer - Promising Tool For Predictionmazda626 retrocarsNo ratings yet
- IMRT Part 2 BJRDocument6 pagesIMRT Part 2 BJRsusdoctorNo ratings yet
- Characterization of Adrenal Metastatic Cancer Using FDG PET CTDocument8 pagesCharacterization of Adrenal Metastatic Cancer Using FDG PET CTEngky ChristianNo ratings yet
- Concurrent Radiotherapy and Weekly Paclitaxel For Locally Advanced Squmous Cell Carcinoma of Uterine Cervix-Treated Patients at Rural Centre in IndiaDocument5 pagesConcurrent Radiotherapy and Weekly Paclitaxel For Locally Advanced Squmous Cell Carcinoma of Uterine Cervix-Treated Patients at Rural Centre in IndiaIjsrnet EditorialNo ratings yet
- Recist 1Document11 pagesRecist 1Kelik WagiyantoNo ratings yet
- (583950958) Journal Leucopenia Treatment Effiicacy NPCDocument8 pages(583950958) Journal Leucopenia Treatment Effiicacy NPCDaniel HoseaNo ratings yet
- ProtocolsummaryDocument3 pagesProtocolsummaryapi-644802109No ratings yet
- Rectal Cancer NLR and Lymphopenia Predict SurvivalDocument4 pagesRectal Cancer NLR and Lymphopenia Predict SurvivalRaul Matute MartinNo ratings yet
- 2018 Article 6554Document8 pages2018 Article 6554Raíla SoaresNo ratings yet
- Adaptative RT For Prostate Cancer Using KV CBCT - Jasper NijkampDocument8 pagesAdaptative RT For Prostate Cancer Using KV CBCT - Jasper NijkampMarcos sajcabunNo ratings yet
- 18F FDG PET CT Role in Staging of Gastric CancerDocument8 pages18F FDG PET CT Role in Staging of Gastric Cancermednuclpg mednuclpgNo ratings yet
- AsdasdDocument10 pagesAsdasdAdhi PratamaNo ratings yet
- Pathological complete response in recurrent colon cancer following neoadjuvant radiotherapy and intraperitoneal chemotherapyDocument4 pagesPathological complete response in recurrent colon cancer following neoadjuvant radiotherapy and intraperitoneal chemotherapyAlice AugustinNo ratings yet
- Prognostic Value of F-FDG Pet/Ct in Surgical Non-Small Cell Lung Cancer: A Meta-AnalysisDocument19 pagesPrognostic Value of F-FDG Pet/Ct in Surgical Non-Small Cell Lung Cancer: A Meta-AnalysisAmina GoharyNo ratings yet
- Ann Oncol 2010 Stupp v190 3Document4 pagesAnn Oncol 2010 Stupp v190 3Aryantii AntyNo ratings yet
- Bisa 1Document8 pagesBisa 1justforuroNo ratings yet
- Vera2020 Article MultidisciplinaryManagementOfLDocument16 pagesVera2020 Article MultidisciplinaryManagementOfLDiego Andres VasquezNo ratings yet
- Clinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypeDocument12 pagesClinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypesilviailieNo ratings yet
- Prognostic Factors in Nasopharyngeal Carcinoma With Synchronous Liver Metastasis: A Retrospective Study For The Management of TreatmentDocument7 pagesPrognostic Factors in Nasopharyngeal Carcinoma With Synchronous Liver Metastasis: A Retrospective Study For The Management of TreatmentChairul Nurdin AzaliNo ratings yet
- Moretto 2014Document8 pagesMoretto 2014Silvie WidyaNo ratings yet
- Pi Is 1879850016300947Document7 pagesPi Is 1879850016300947Daniela GordeaNo ratings yet
- Neoadjuvant chemoradiotherapy followed by surgery standard for esophageal cancerDocument14 pagesNeoadjuvant chemoradiotherapy followed by surgery standard for esophageal cancerkrsna2studyNo ratings yet
- Esofago Carvical Valmasoni 2018Document9 pagesEsofago Carvical Valmasoni 2018Carlos N. Rojas PuyolNo ratings yet
- Allen2021 Article ChemotherapyVersusChemotherapyDocument8 pagesAllen2021 Article ChemotherapyVersusChemotherapyXavier QuinteroNo ratings yet
- The OncologistDocument7 pagesThe OncologistManunart FeungpeanNo ratings yet
- 10 1016@j Amjsurg 2019 12 006Document24 pages10 1016@j Amjsurg 2019 12 006Ferdian PriantoNo ratings yet
- The Prognostic Value of 18F-FDG PET/CT in Postoperative Recurrence of Retroperitoneal Liposarcoma: A Single Center Retrospective StudyDocument17 pagesThe Prognostic Value of 18F-FDG PET/CT in Postoperative Recurrence of Retroperitoneal Liposarcoma: A Single Center Retrospective StudyAulia HudaNo ratings yet
- Local Control in Metastatic Neuroblastoma in Children Over 1 Year of AgeDocument8 pagesLocal Control in Metastatic Neuroblastoma in Children Over 1 Year of AgePutri ManurungNo ratings yet
- Radioterapia en CacUDocument6 pagesRadioterapia en CacUVicente RamosNo ratings yet
- Nej Mo A 0900043Document8 pagesNej Mo A 0900043anggiNo ratings yet
- FDG PET-CT in the Initial Staging and Restaging of soft tissue or bone sarcoma.Document7 pagesFDG PET-CT in the Initial Staging and Restaging of soft tissue or bone sarcoma.Anderson Ruben LizcanoNo ratings yet
- Pathologic Response When Increased by Longer Interva - 2016 - International JouDocument10 pagesPathologic Response When Increased by Longer Interva - 2016 - International Jouwilliam tandeasNo ratings yet
- Intergroup 0123Document8 pagesIntergroup 0123radonc17No ratings yet
- P. Wang Et Al.2019Document6 pagesP. Wang Et Al.2019Mai M. AlshalNo ratings yet
- Tratat ClorambucilDocument6 pagesTratat ClorambucilDiegoPeixotoNo ratings yet
- A Phase 1 Trial of Focal Salvage Stereotactic BodyDocument11 pagesA Phase 1 Trial of Focal Salvage Stereotactic BodyAhmedNo ratings yet
- Sequential Chemoradiotherapy With Gemcitabine and Cisplatin For Locoregionally Advanced Nasopharyngeal CarcinomaDocument9 pagesSequential Chemoradiotherapy With Gemcitabine and Cisplatin For Locoregionally Advanced Nasopharyngeal CarcinomadheaonyonNo ratings yet
- CK 193-2594-2-PBDocument6 pagesCK 193-2594-2-PBneeluNo ratings yet
- Use of FET-PET in Glioblastoma: Journal Club May 4 2011Document41 pagesUse of FET-PET in Glioblastoma: Journal Club May 4 2011tienloNo ratings yet
- Rtog 1112 Protocol SummaryDocument2 pagesRtog 1112 Protocol Summaryapi-633434674No ratings yet
- 1 s2.0 S0923753419363677 MainDocument6 pages1 s2.0 S0923753419363677 MainSamantha AdrianneNo ratings yet
- bfcr163 Pet-Ct PDFDocument34 pagesbfcr163 Pet-Ct PDFMirza BaigNo ratings yet
- 1 s2.0 S245210942100097X MainDocument7 pages1 s2.0 S245210942100097X MainhidayatullahhaqyaarNo ratings yet
- 1677 5538 Ibju 42 04 0694Document10 pages1677 5538 Ibju 42 04 0694Lucas VibiamNo ratings yet
- FgagfgafDocument9 pagesFgagfgafSean ChenNo ratings yet
- Lung Stereotactic Ablative Body Radiotheray SABR - Patient o - 2019 - ClinicalDocument1 pageLung Stereotactic Ablative Body Radiotheray SABR - Patient o - 2019 - ClinicalSENo ratings yet
- Comparative Treatment Planning Study of Photons and ProtonsDocument15 pagesComparative Treatment Planning Study of Photons and ProtonsJesse Helmut Hansen-BartelNo ratings yet
- 2019 Article 5894 PDFDocument8 pages2019 Article 5894 PDFGalgalo GarbichaNo ratings yet
- Journal Pre-Proofs: Radiotherapy and OncologyDocument21 pagesJournal Pre-Proofs: Radiotherapy and OncologyNik rabekNo ratings yet
- S1359634912X00028 S1359634912700253 MainDocument7 pagesS1359634912X00028 S1359634912700253 MainindracuangNo ratings yet
- Nej Mo A 1414882Document9 pagesNej Mo A 1414882Corina Hagiu-RaduNo ratings yet
- Radiotherapy of Liver CancerFrom EverandRadiotherapy of Liver CancerJinsil SeongNo ratings yet
- Lecture 1.1 - Introductory - Health Indicators and Health Services ProblemsDocument15 pagesLecture 1.1 - Introductory - Health Indicators and Health Services ProblemsBagus OkaNo ratings yet
- Damedicalpus Bells PalsyDocument2 pagesDamedicalpus Bells PalsyBagus OkaNo ratings yet
- Parasitic Infection in GI TractDocument123 pagesParasitic Infection in GI TractUtami HandayaniNo ratings yet
- Global Brief HypertensionDocument40 pagesGlobal Brief HypertensionkeynechristaNo ratings yet
- 1Document6 pages1Bagus OkaNo ratings yet
- Hyponatremic Dehydration PathoDocument4 pagesHyponatremic Dehydration PathoENo ratings yet
- Major Depressive Disorder in Adults: Diagnosis & Management: ScopeDocument19 pagesMajor Depressive Disorder in Adults: Diagnosis & Management: ScopeBadii AmamouNo ratings yet
- Cicatricial Atelectasis - Print Friendly - STATdxDocument2 pagesCicatricial Atelectasis - Print Friendly - STATdxmihaelaNo ratings yet
- Nursing Care Plan For AIDS/HIVDocument3 pagesNursing Care Plan For AIDS/HIVderic81% (16)
- PAVSDMAPCAsDocument3 pagesPAVSDMAPCAsRajesh SharmaNo ratings yet
- Differential Diagnosis of Neck SwellingsDocument24 pagesDifferential Diagnosis of Neck SwellingsDrArish Mahmood100% (3)
- Exam MCQs - A-1تمDocument12 pagesExam MCQs - A-1تممصطفى محمد جواد كاظمNo ratings yet
- University of Al-Ameed College of Medicine: Hematopathology Lecture PlanDocument226 pagesUniversity of Al-Ameed College of Medicine: Hematopathology Lecture PlanYousif AlaaNo ratings yet
- Ekstravasation AssesmentDocument2 pagesEkstravasation AssesmentHelena Christy100% (1)
- DUPUYTREN'S SYNDROME TestDocument15 pagesDUPUYTREN'S SYNDROME TestreyNo ratings yet
- Defining Treatment Response, Remission, Relapse, and RecoveryDocument21 pagesDefining Treatment Response, Remission, Relapse, and Recovery주병욱No ratings yet
- IDSA Molnupiravir GuidelineDocument10 pagesIDSA Molnupiravir GuidelineJaz ButuyanNo ratings yet
- Differential Diagnosis and Management of GlossodyniaDocument26 pagesDifferential Diagnosis and Management of GlossodyniaKoya Naren BabuNo ratings yet
- ECMO For COVID 19 Updated 2021 Guidelines From.98326Document42 pagesECMO For COVID 19 Updated 2021 Guidelines From.98326risanataliasiburianNo ratings yet
- Basic First Aid For Medical EmergenciesDocument27 pagesBasic First Aid For Medical EmergenciesCOngNo ratings yet
- Acute Lung Conditions ExplainedDocument14 pagesAcute Lung Conditions ExplainedMichelle LopezNo ratings yet
- Acute Myeloid LeukemiaDocument1 pageAcute Myeloid LeukemiaAlleah Salbo KepusNo ratings yet
- Is A Traditional Colonoscopy or A Virtual Colonoscopy BetterDocument1 pageIs A Traditional Colonoscopy or A Virtual Colonoscopy BetterPaul JensenNo ratings yet
- Pathology Outlines - Papillary Carcinoma - GeneralDocument6 pagesPathology Outlines - Papillary Carcinoma - Generalpatka1rNo ratings yet
- Basic Objectives of Color and Spectral DopplerDocument5 pagesBasic Objectives of Color and Spectral DopplerAsaad Baloch100% (2)
- Module 8-NSTP 1-Health Program, Common Illness & Their PreventionDocument46 pagesModule 8-NSTP 1-Health Program, Common Illness & Their PreventionLalaine AlonNo ratings yet
- Faktor-Faktor Yang Mempengaruhi Gangguan Tidur Pada Pasien Diabetes MelitusDocument6 pagesFaktor-Faktor Yang Mempengaruhi Gangguan Tidur Pada Pasien Diabetes MelitusImron BuhoriNo ratings yet
- Safety in Sports: Made By: Shrreya Swaarnim Class: XD Roll No.: 40Document5 pagesSafety in Sports: Made By: Shrreya Swaarnim Class: XD Roll No.: 40Shrreya SwaarnimNo ratings yet
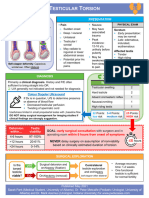
- Testicular Torsion, Peds Cases NotesDocument1 pageTesticular Torsion, Peds Cases NotesdzalhcNo ratings yet
- Nursing Students Peritonitis Care PlanDocument2 pagesNursing Students Peritonitis Care PlanJide Manuel100% (1)
- PDF Tablet Lepas LambatDocument13 pagesPDF Tablet Lepas Lambatannisya bubblesNo ratings yet
- Pernicious Anemia in Young: A Case Report With Review of LiteratureDocument5 pagesPernicious Anemia in Young: A Case Report With Review of LiteratureeditorijmrhsNo ratings yet
- PNSS Drug StudyDocument2 pagesPNSS Drug Studyrain peregrinoNo ratings yet
- Preeclampsia With Severe Features, Uncontrolled: University of The Cordilleras College of NursingDocument45 pagesPreeclampsia With Severe Features, Uncontrolled: University of The Cordilleras College of NursingAndrei MarcosNo ratings yet
- Tnkhetp LBLDocument2 pagesTnkhetp LBLvijayabhavani.sNo ratings yet