Professional Documents
Culture Documents
NCP Compilation
Uploaded by
Rene John FranciscoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP Compilation
Uploaded by
Rene John FranciscoCopyright:
Available Formats
BSN4A (GROUP 2) 33 XI.
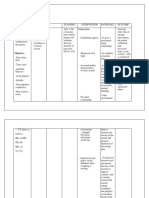
Nursing Care Plan Assessment Data Actual Abnormal Cues: Moderately advanced PTB on left lung, with gaseous necrosis formation Pleural effusion on right lungs with Chest Tube Thoracotomy(CTT) of 350 Anemia Ateriosclerotic aorta Difficulty breathing Verbalized, indi ko ka ginhawa tadlong kay sa kilid ko ni nga tubo, kasakit kung mag ginhawako Wheezing upon auscultation in left lower quadrant of the lungs Crackles upon auscultation in the left upper quadrant of lungs Nursing Diagnosis Impaired Gas Exchange related to altered oxygen supply due accumulation of fluid in the pleural space, presence of viscous secretions, decrease in effective lung surface as evidenced by difficulty of breathing, chest pain, tachypnea, wheezing and crackles upon auscultation, CTT of 350 cc Rationale Predisposing Factors Gender: Male Biological: History of TB infection Precipitating Factors Close contact with infected person Low income group Poor medical care Coexisting disease in the community Cigarette smoking Exposure or inhalation of infected aerosol through droplet by Mycobacterium tuberculosis Tubercle bacilli invasion in the apices of the lungs or near the pleurae of the lower lobes Bronchopneumonia develops in the lung tissue (phagocytised tubercle bacilli are ingested by Desired Outcome After 32 hours of nursing intervention, the client will be able to: 1. Report absence/ decrease dyspnea Nursing Intervention Justification Evaluation After 32 hours of nursing intervention, the client was be able to:
Independent:
Independent:
1.1 Asses respiratory 1.1 Manifestations rate, depth, and of respiratory ease distress are dependent on/ indicative of the degree of lung involvement and underlying health status. 1.2 Assess for dyspnea (using 0-10 scale), tachypnea, abnormal/dimini shed breath sound, increased respiratory effort, limited chest wall expansion, and fatigue
Definition: Excess or deficit in oxygenation and/or carbon dioxide elimination at the
1. Goal partially met. Experienced shallow breathing and pain upon inhalation due to his tube drainage as mentioned by the patient. He is not in labored breathing and does not use his 1.2 Pulmonary TB accessory muscle can cause a wide and exert not much range of effects effort upon in the lungs, inhalation. ranging from a small patch of bronchopneumo nia to diffuse inflammation, caseous necrosis, pleural effusion, and extensive fibrosis.
BSN4A (GROUP 2) 34 Wheezing to diminished breath sound on the right lung Limited chest wall expansion Shallow, rapid breathing RR of 36cpm Exert effort upon inhalation Lethargic Fatigue alveolar-capillary membrane (This may be an entity of its own, but it also be an end result of other pathology with an interrelatedness between airway clearance and/or breathing pattern problems) macrophages), bacterial cell wall binds with macrophages Inflammation of the lung tissues and pleura Necrotic degeneration occurs (production of cavities filled with cheese-like mass of tubercle bacilli. Dead WBCs, necrotic lung tissue) Impaired lung tissues and capillary function Impaired lymphatic drainage of the pleural space Transdiaphragmatic movement of inflammatory fluid from the peritoneal space Altered permeability of pleural membranes Increased capillary wall permeability or vascular disruption Respiratory effects can range from mild dyspnea to profound respiratory distress. 1.3 Maintain bed 1.3 Reducing rest/limit activity oxygen and assist with consumption. self-care Demand during activities as periods of necessary. respiratory compromise may reduce severity of symptoms.
Risk Related Factors: Malnutrition Infection History of smoking Poor family support Poor financial support
Strengths: Willingness to get well Good compliance to medication
Source: Nurses Pocket Guide 11th Edition by Doenges, Moorhouse and Murr
2. Demonstrate improved ventilation and adequate oxygenation of tissues
2.1 Observe color of skin, mucous membranes, and nail beds, noting presence of peripheral cyanosis (nailbeds) or central cyanosis (circumoral).
2.1 Cyanosis of nail beds may represent vasoconstrictio n or the bodys response to fever/chills; however, cyanosis of earlobes, mucous membranes, and skin around the
2. Goal partially met. Have a good capillary refill of less than 2 seconds and able to breathe on his own capacity. He was more calm and able to rest more without difficulty. But, patient still experienced fatigue, lethargy and dyspnea.
BSN4A (GROUP 2) 35 Increase accumulation of fluids in the lungs Impaired Gas Exchange 2.2 Avoid patient to lie down on operative side; instead , favor the good lung down position mouth (warm membranes) is indicative of systemic hypoxemia 2.2 Research shows that positioning patients following lung surgery with their good lung down maximizes oxygenation by using gravity to enhance blood flow to the healthy lung, thus creating the best possible match between ventilation and perfusion. 3. Goal met. Participate actively in the activities as tolerated. He tried to do deep breathing and coughing exercise
3. Participate in actions to maximize oxygenation.
3.1 Demonstrate/enc ourage purse-lip breathing during exhalation.
3.1 Creates resistance against outflowing or to prevent collapse/narrow
BSN4A (GROUP 2) 36 ing of the airways, thereby helping distribute air throughout the lungs and relieve/reduce shortness of breath. 3.2 Elevate head of bed, change position frequently. 3.2 Lowers diaphragm, promoting chest expansion, aeration of lung segments, mobilization and expectoration of secretions. 3.3 Deep breathing facilitates maximum expansion of the lungs/smaller airways. Coughing is a natural selfcleaning mechanism, assisting the cilia to even if he experience pain due to his chest tube. Also, he can follow instructions accordingly.
3.3 Assist patient with deepbreathing exercises. Demonstrate/hel p patient learns to perform activity, e.g., splinting chest and effective coughing while in upright position.
BSN4A (GROUP 2) 37 maintain patent airways. Splinting reduces chest discomfort, and upright position favors deeper, more forceful cough effort. 3.4 Provide appropriate chest physiotherapy, including postural drainage and breathing exercise. 3.4 Aids in clearing secretions, which improves ventilation, allowing excess CO2 to be eliminated.
Collaborative: 1. Provide supplemental oxygen as appropriate
Collaborative: 1. Aids in correcting the hypoxemia that may occur secondary to decrease ventilation/ diminished alveolar surface 2. Tube Care: Chest a. Drains fluid
2. Tube Care: Chest a. Maintain
BSN4A (GROUP 2) 38 patency of chest drainage system. from pleural cavity to promote reexpansion of remaining lung segments. b. Bloody drainage should decrease in amount and change to a more serous composition as recovery progresses. A sudden increase in amount of bloody drainage or return to frank bleeding suggests thoracic bleeding/ hemothorax; sudden cessation suggests blockage of tube, requiring further evaluation and intervention.
b.Note changes in amount/type of chest tube drainage.
BSN4A (GROUP 2) 39 c. Observe presence/degree of bubbling in water-seal chamber. c. Air leaks immediately postoperative are not uncommon; however this should diminish as healing progresses. Prolonged or new leaks require evaluation to identify problems in patient versus the drainage system.
BSN4A (GROUP 2) 40 Assessment Actual/ Abnormal Cues Diagnosis Rationale Predisposing Factors Gender: Male Biological: History of TB infection Precipitating Factors Close contact with infected person Low income group Poor medical care Coexisting disease in the community Cigarette smoking Presence of fluid in the lungs CTT is attached Inflammation of the CTT insertion site Tissue damage Activation of the Desired Outcome After 32 hours of nursing intervention patient will be able to: Nursing Intervention Justification Evaluation After 32 hours of nursing intervention patient was able to:
Acute pain related to presence of Patient insertion site of verbalized,kasaki CTT (Chest Tube tkaakondughanng Thoracotomy) as a may tubo evidenced by presence of guarding insertion site of behavior, facial CTT mask, reported guarding behavior sleep disturbance facial mask and restlessness. reported sleep disturbance restlessness PR= 100cpm RR= 40 cpm
1. Manage self when pain occurs.
1.1 Acknowledge the pain experience and convey acceptance of clients response to pain.
1.1Reduces defensive responses, promotes trust and enhances cooperation with regimen. 1.2Relaxation skills and techniques have no detrimental side effects. 1.3To provide patient education and to the S.O.
1. Goal met. Patient performs deep breathing exercise when he is in pain and was seen changing his position.
1.2 Review non pharmacologic measures for lessening pain. 1.3 Provide information/ discuss pain management.
Strengths: Willingness to get well Good compliance to medication Weakness: poor compliance to medication poor family support financial constraints
Definition: Unpleasant sensory and emotional experience arising from actual or potential tissue damage or described or in terms of such damage.
2. Verbalized non pharmacologic methods that provide pain relief.
2.1Instruct/ encourage use of relaxation techniques such as focused breathing and imaging. 2.2Provide health teaching regarding non pharmacologic methods to relieve pain.
2.1To distract attention and reduces tension.
2.2To provide information to the client so that he will be able to manage pain by himself.
2. Goal met. Patient verbalized. gaginhawa lang ko dalum para maibanan ang sakit kag kung kaisa gina lain ko ang konposisyon.
3. Report pain is
3.1Provide comfort
3.1To promote non
3. Goal met. Patient
BSN4A (GROUP 2) 41 peripheral nervous relieved/ controlled. system Activation of central nervous system and transmission of pain at the spinal cord level Transmission of pain signal to the brain Acute pain related to presence of insertion site of CTT measures such (eg. Touch, repositioning, use of heat/ cold packs), quiet environment and calm activities. 3.2Administer analgesics, as indicated, to maximum dosage, as needed. pharmacologic pain management. reports, gaka ibanan man ang sakit katapos kapilaka minute gakadula man ang sakit.
Source: Nurses Pocket Guide. 11th Ed. Doenges, Moorhouse and Murr.
3.2To maintain acceptable level of pain. Notify physician if regimen is inadequate to meet pain control goal.
BSN4A (GROUP 2) 42 Assessment Data Risk Related Factors Presence of right (CTT) Chest Tube Thoracotomy Foul smelling discharges coming out from the incision site Poor dressing of incision site Poor hygiene Nursing Diagnosis Risk for injury related to therapeutic puncture of lung secondary to iatrogenic pneumothorax Rationale Predisposing Factors Biological: History of TB infection Precipitating Factors Low income group Poor medical care Poor hygiene Presence of CTT Dislodgment in place of CTT in the pleural cavity Potential puncture of CTT to the intrapleural space or leakage in the lung Introduction of air to the intrapleural space Allow air to enter and gather around the lungs Desired Outcome After 32 hours of nursing intervention, the client will be able to: 1. Identify individual risk factors. 1.1 Ask about chest pain; determine its onset, intensity, and location. Ask if the patient has shortness of breath or difficulty in breathing or fatigue. 1.2 Check the patients history for bleeding disorders or anticoagulant therapy. 1.3Examine the patients chest for a visible wound that may have been caused by a penetrating object. 1.1Elicit a history of COPD or emphysema or if the patient has had a thoracotomy, thoracentesis, or insertion of a central line. Nursing Intervention Justification Evaluation After 32 hours of nursing intervention, the client was be able to:
Weakness: Malnutrition Infection History of smoking Poor family support Poor financial support
Definition: At risk for injury as a result of environmental conditions interacting with the individuals adaptive and defensive resources
1. Goal met. Patient verbalized, ang ginhalinan sang sakit ko guru amu ang pag-inom ko kg pag panigarilyo tapus gaubra pa ko sa kampo nga naga-tagi-ti ang init.
1.2 To properly manage of underlying conditions
Source: Nurses Pocket Guide 11th Edition by Doenges, Moorhouse and Murr
1.3Patients with an open pneumothorax also exhibit a sucking sound on inspiration.
Strengths: Willingness to get well
2. Modify environment , as indicated, to
2.1Elevate the head of the bed to facilitate breathing. Instruct client to lie on the unaffected side with the head of the bed elevated
2.1 This position facilitates expansion of the affected lung and eases respirations
2. Goal met. Patient elevates his head when he has difficulty in breathing and uses deep
BSN4A (GROUP 2) 43 Good compliance to medication Collapsed of the lungs Risk for injury related to therapeutic puncture of lung secondary to iatrogenic pneumothorax Source: Nurses Pocket Guide 11th Edition by Doenges, Moorhouse and Murr 3. Take safety precautions during the span of stay in the hospital enhance safety and use resources appropriatel y 30 degrees for at least 30 minutes 2.2 Obtain a chest X-ray. 2.2To determine the chest tube placement. 2.3To early manage symptoms and prevent further injury breathing exercises as instructed.
2.3Immediately report signs and symptoms of pneumothorax, tension pneumothorax, and pleural fluid reaccumulation such as difficulty of breathing and chest pain.
3.1Monitor vital signs, pulse oximetry, and breathe sounds.
3.1 To have baseline data and note any deviation of succeeding readings most especially the respiratory rate
3.2 Observe the puncture site and dressings. 3.2 To note for any leakage and discharges that may precipitate pneumothorax
3. Goal met. Patient observes safety precautions in the hospital and the folk never leave the patient alone.
You might also like
- Nursing ManagementDocument16 pagesNursing ManagementNica Marie LumbaNo ratings yet
- Ineffective Airway Clearance Nursing Care PlanDocument2 pagesIneffective Airway Clearance Nursing Care Planrois romaNo ratings yet
- NCP - Ineffective Airway ClearanceDocument2 pagesNCP - Ineffective Airway ClearanceEmirose Fatima TagabNo ratings yet
- NCP SicuDocument6 pagesNCP SicuChoco MuchoNo ratings yet
- Acc Phu Case NCP HyperthermiaDocument1 pageAcc Phu Case NCP Hyperthermiamacy_bautistaNo ratings yet
- Impaired Gas Exchange NCPDocument3 pagesImpaired Gas Exchange NCPRomel BaliliNo ratings yet
- Pain NCP BillrothDocument2 pagesPain NCP BillrotharjayNo ratings yet
- NCP #1 Acute Pain Related To Decreased Blood Supply Nursing Diagnosis Scientific Explanation Planning Interventions Rationale Expected OutcomeDocument22 pagesNCP #1 Acute Pain Related To Decreased Blood Supply Nursing Diagnosis Scientific Explanation Planning Interventions Rationale Expected OutcomeAnnNo ratings yet
- NCP BronchopneumoniaDocument8 pagesNCP BronchopneumoniaCrisantaCasliNo ratings yet
- Decreased Cardiac OutputDocument5 pagesDecreased Cardiac Outputshuang81No ratings yet
- Assessment Nursing Diagnosis Planning Nursing Intervention Rationale Evaluation Subjective DataDocument6 pagesAssessment Nursing Diagnosis Planning Nursing Intervention Rationale Evaluation Subjective DataDeinielle Magdangal RomeroNo ratings yet
- Nursing Care Plan for Peritonsillar AbscessDocument2 pagesNursing Care Plan for Peritonsillar AbscessKevin Leo Lucero AragonesNo ratings yet
- Tuberculous Meningitis Nursing AssessmentDocument1 pageTuberculous Meningitis Nursing AssessmentMark Adrian D. DizorNo ratings yet
- NCPDocument3 pagesNCPNikki del Rosario100% (2)
- Impaired Skin IntegrityDocument3 pagesImpaired Skin IntegrityAubrey SungaNo ratings yet
- OPD Case Study SummaryDocument35 pagesOPD Case Study SummaryMicah MagallanoNo ratings yet
- Pneumo Hemoperitoneum Stab Wound Case StudyDocument7 pagesPneumo Hemoperitoneum Stab Wound Case StudyMari Jasmeen Estrada Noveda100% (1)
- Ineffective Airway ClearanceDocument1 pageIneffective Airway ClearanceVittena Eloisa VibarNo ratings yet
- Elena Ocyo (Pedia - NCP)Document3 pagesElena Ocyo (Pedia - NCP)elle leliNo ratings yet
- Risk For Infection NCP Ortho JadDocument1 pageRisk For Infection NCP Ortho JadjadpauloNo ratings yet
- Nursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleDocument8 pagesNursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleTrysna Ayu SukardiNo ratings yet
- Appendectomy NCPDocument4 pagesAppendectomy NCPPersha Perez ArabaniNo ratings yet
- NCPDocument9 pagesNCPLeolene Grace BautistaNo ratings yet
- Manage Bronchiectasis Nursing Care PlanDocument5 pagesManage Bronchiectasis Nursing Care PlanPaola Marie VenusNo ratings yet
- Postpartal Thrombophlebitis: Client Assessment Data Base Activity/RestDocument8 pagesPostpartal Thrombophlebitis: Client Assessment Data Base Activity/RestLei OrtegaNo ratings yet
- NCP1 CHFDocument2 pagesNCP1 CHFapi-27015740100% (5)
- Focus Charting (F-DAR) : How To Do Focus Charting or F-DAR: Notes Fundamentals of NursingDocument6 pagesFocus Charting (F-DAR) : How To Do Focus Charting or F-DAR: Notes Fundamentals of NursingMichael Angelo SeñaNo ratings yet
- Chorioamnionitis NCPDocument8 pagesChorioamnionitis NCPjunard258067% (3)
- Allergic RhinitisDocument1 pageAllergic RhinitisprettylittlenurseNo ratings yet
- Cap MRDocument4 pagesCap MRKit BarcelonaNo ratings yet
- Fatigue Care Plan HIVDocument2 pagesFatigue Care Plan HIVDaryl Paglinawan100% (1)
- SP CSDocument4 pagesSP CSKhan HansNo ratings yet
- Nursing Care Plan For Tissue InjuryDocument2 pagesNursing Care Plan For Tissue InjuryJobelle AcenaNo ratings yet
- Postoperative Nursing Care Plan For Cesarian Section Patient Case Pres orDocument6 pagesPostoperative Nursing Care Plan For Cesarian Section Patient Case Pres orLoren EstefanNo ratings yet
- Pleural Effusion FdarDocument1 pagePleural Effusion FdarvanessabdeveraNo ratings yet
- NICU Nursing Care PlanDocument3 pagesNICU Nursing Care Planlorence_cachoNo ratings yet
- Impaired Breathing PatternDocument1 pageImpaired Breathing PatternHanya Bint PotawanNo ratings yet
- NCP BMDocument1 pageNCP BMSourabh MehraNo ratings yet
- Case Study PnuemoniaDocument10 pagesCase Study PnuemoniaKyle B. Nacionales Ü100% (1)
- Impaired Skin IntegrityDocument2 pagesImpaired Skin IntegrityEli AyaseNo ratings yet
- NCP TBDocument7 pagesNCP TBLorraine CilloNo ratings yet
- NCP Acute Pain-HyperthermiaDocument6 pagesNCP Acute Pain-HyperthermiarhegellNo ratings yet
- Nursing Care Plan Ineffective Airway Clearance Related To Tracheobronchial Secretions CAPDocument2 pagesNursing Care Plan Ineffective Airway Clearance Related To Tracheobronchial Secretions CAPLP Benoza100% (2)
- Pregnant Aerobics Instructor Case StudyDocument25 pagesPregnant Aerobics Instructor Case StudyGerly LagutingNo ratings yet
- NCP For Impaired Oral Mucous MembraneDocument11 pagesNCP For Impaired Oral Mucous MembraneRYAN SAPLADNo ratings yet
- NCP Copd FinalDocument3 pagesNCP Copd FinalGiselle EstoquiaNo ratings yet
- NCPDocument2 pagesNCPNaidin Catherine De Guzman-AlcalaNo ratings yet
- A Case PresentationDocument50 pagesA Case PresentationAnaleah MalayaoNo ratings yet
- Impaired Gas Exchange NCPDocument4 pagesImpaired Gas Exchange NCPkimglaidyl bontuyanNo ratings yet
- NCP (BPH)Document8 pagesNCP (BPH)NataCo50% (2)
- Aaa Gastrectomy NCP FinalDocument13 pagesAaa Gastrectomy NCP Finallexzaf100% (1)
- NCP PainDocument1 pageNCP Painsitz04No ratings yet
- NCP PleuralDocument5 pagesNCP Pleuraljanine_valdezNo ratings yet
- BronchiectasisDocument40 pagesBronchiectasisyana jaeNo ratings yet
- Pneumonia Assessment and Care PlanDocument7 pagesPneumonia Assessment and Care PlanAkun NyampahNo ratings yet
- PneumoniaDocument7 pagesPneumoniaJhgrace Mary Pacaña GalloNo ratings yet
- Bronchitis 170709131740Document28 pagesBronchitis 170709131740Viji MNo ratings yet
- Pneumonia: Case PresentationDocument12 pagesPneumonia: Case PresentationgelaneNo ratings yet
- Below Are 8 Pneumonia Nursing Care Plans (NCP)Document16 pagesBelow Are 8 Pneumonia Nursing Care Plans (NCP)Diana CarinoNo ratings yet
- Nursing Management of Patients WithDocument8 pagesNursing Management of Patients Withfunky goodNo ratings yet
- Genexpert TestDocument2 pagesGenexpert TestRene John FranciscoNo ratings yet
- Bloom's TaxonomyDocument26 pagesBloom's TaxonomyRene John FranciscoNo ratings yet
- Slides Surgical Instruments Update 1.7Document43 pagesSlides Surgical Instruments Update 1.7Paul Christian P. Santos, RN100% (32)
- Scientific Death of JesusDocument7 pagesScientific Death of JesusRene John FranciscoNo ratings yet
- Basic Surgical InstrumentsDocument37 pagesBasic Surgical Instrumentsapi-2658787991% (33)
- Basic Delivery Set (Nullipara)Document1 pageBasic Delivery Set (Nullipara)Rene John FranciscoNo ratings yet
- MSPPP 12913337842396 Phpapp01Document26 pagesMSPPP 12913337842396 Phpapp01RI NANo ratings yet
- Gifts of the Holy Spirit ExplainedDocument4 pagesGifts of the Holy Spirit ExplainedMauricio Rojas ValdiviaNo ratings yet
- Surgical InstrumentsDocument8 pagesSurgical InstrumentsSharmaine Simon91% (11)
- Surgical Instrumentation - R. ILADODocument54 pagesSurgical Instrumentation - R. ILADOrhenier_ilado100% (1)
- OR EquipmentsDocument8 pagesOR EquipmentsRene John FranciscoNo ratings yet
- Stress ManagementDocument17 pagesStress Managementanon_469843072No ratings yet
- Dressing For Job Interview and ResignationDocument7 pagesDressing For Job Interview and ResignationRene John FranciscoNo ratings yet
- Facts of The RealityDocument11 pagesFacts of The RealityRene John FranciscoNo ratings yet
- Drug Study For Paracetamol, Omeprazole and Vitamin B ComplexDocument3 pagesDrug Study For Paracetamol, Omeprazole and Vitamin B ComplexMichelle Manibale R.N100% (4)
- Potassium ChlorideDocument2 pagesPotassium ChlorideRene John FranciscoNo ratings yet
- Drug Study - Paracetamol Ambroxol, Ascorbic Acid, CefuroximeDocument4 pagesDrug Study - Paracetamol Ambroxol, Ascorbic Acid, Cefuroximeapi-3701489100% (12)
- Drug Study for Psychosis and Bipolar DisorderDocument4 pagesDrug Study for Psychosis and Bipolar DisorderJowel Cruz De LeonNo ratings yet
- Omeprazole and Polynerv (B1,6,12)Document3 pagesOmeprazole and Polynerv (B1,6,12)Rene John Francisco100% (1)
- NCP-Impaired Physical Mobility - E+ ImbalanceDocument3 pagesNCP-Impaired Physical Mobility - E+ ImbalanceRene John FranciscoNo ratings yet
- Chapter 45 - Drugs For HypertensionDocument14 pagesChapter 45 - Drugs For Hypertensiondlneisha61100% (1)
- Naloxone, MorphineDocument7 pagesNaloxone, MorphineRene John FranciscoNo ratings yet
- Drug Study (Seretide)Document1 pageDrug Study (Seretide)Rene John Francisco100% (1)
- Omeprazole and Polynerv (B1,6,12)Document3 pagesOmeprazole and Polynerv (B1,6,12)Rene John Francisco100% (1)
- Drug Study On Emergency DrugsDocument14 pagesDrug Study On Emergency DrugsRene John FranciscoNo ratings yet
- Diazepam, Lanoxin, Hemostan, NaprexDocument6 pagesDiazepam, Lanoxin, Hemostan, NaprexRene John Francisco100% (1)
- ErythromycinDocument6 pagesErythromycinapi-3797941100% (1)
- Drug Study - MirceraDocument2 pagesDrug Study - MirceraRene John FranciscoNo ratings yet
- Drug Study (Combivent)Document2 pagesDrug Study (Combivent)Rene John Francisco100% (3)
- Drug Study (Budesonide)Document1 pageDrug Study (Budesonide)Rene John Francisco33% (3)
- Harga ObatDocument21 pagesHarga ObatRizamdhani AptNo ratings yet
- Guide To Genetic CounselingDocument24 pagesGuide To Genetic Counselingmady_elenutza0% (1)
- Sample Birthing PlanDocument2 pagesSample Birthing PlanChuohNo ratings yet
- Labor Pain ManagementDocument1 pageLabor Pain ManagementKenneth Sy100% (5)
- Insights Into Veterinary Endocrinology - Diagnostic Approach To PU - PD - Urine Specific GravityDocument4 pagesInsights Into Veterinary Endocrinology - Diagnostic Approach To PU - PD - Urine Specific GravityHusnat hussainNo ratings yet
- Repositioning an Inverted UterusDocument5 pagesRepositioning an Inverted Uterusshraddha vermaNo ratings yet
- The Truth About The Flu ShotDocument5 pagesThe Truth About The Flu ShotPoorMexicanNo ratings yet
- Adult Early Warning Score Observation Chart For High Dependency UnitDocument2 pagesAdult Early Warning Score Observation Chart For High Dependency Unitalexips50% (2)
- ENL 110 APA In-Text-Citations and References ActivityDocument5 pagesENL 110 APA In-Text-Citations and References ActivityNajat Abizeid SamahaNo ratings yet
- Postterm Pregnancy - UpToDateDocument16 pagesPostterm Pregnancy - UpToDateCarlos Jeiner Díaz SilvaNo ratings yet
- Manage Ophthalmia NeonatorumDocument2 pagesManage Ophthalmia NeonatorumEjay BautistaNo ratings yet
- NCP For SchizoDocument6 pagesNCP For SchizoGILIANNE MARIE JIMENEANo ratings yet
- DR Jignesh ShahDocument6 pagesDR Jignesh ShahBhavesh PatelNo ratings yet
- Visitor Health Declaration FormDocument2 pagesVisitor Health Declaration FormKaryl Eunice Macabale IboniaNo ratings yet
- Autism AssessmentDocument37 pagesAutism AssessmentRafael Martins94% (16)
- d1 QuestionsDocument6 pagesd1 QuestionsaruNo ratings yet
- Virtual Hematology Slide AtlasDocument57 pagesVirtual Hematology Slide Atlasdangrabell86% (7)
- Differences in Housemen Performance from CUCMS and Other Medical SchoolsDocument10 pagesDifferences in Housemen Performance from CUCMS and Other Medical SchoolsAfif AizatNo ratings yet
- Trigger Finger1Document2 pagesTrigger Finger1fahriitoNo ratings yet
- Open Bone Grafting: Papineau TechniqueDocument7 pagesOpen Bone Grafting: Papineau TechniqueAlireza MirzasadeghiNo ratings yet
- Reference TapDocument7 pagesReference TapCharles FestoNo ratings yet
- Lazy Leucocyte SyndromeDocument2 pagesLazy Leucocyte SyndromeDragos BourosNo ratings yet
- Sarawuth Noppiboon ID 56070700020 BioPhEPs SystemsDocument5 pagesSarawuth Noppiboon ID 56070700020 BioPhEPs SystemsSarawuth NoppiboonNo ratings yet
- Strategi RS Dalam Pemenuhan Dan Pengaturan SDM CompressedDocument37 pagesStrategi RS Dalam Pemenuhan Dan Pengaturan SDM CompressedLilik SeptiyaNo ratings yet
- Miliaria Pustulosa (Infetrop)Document11 pagesMiliaria Pustulosa (Infetrop)Muhammad mukramNo ratings yet
- Govind AmbiGen PosterDocument1 pageGovind AmbiGen PosterYolanda MNo ratings yet
- Nursing Documentation for Wina Purnamasari's Immunization and Vital Signs CheckDocument6 pagesNursing Documentation for Wina Purnamasari's Immunization and Vital Signs Checkilah keciNo ratings yet
- Update On Importance of Diet in Gout: ReviewDocument6 pagesUpdate On Importance of Diet in Gout: ReviewIoana IonNo ratings yet
- Nails Diagnosis, Therapy, Surgery Richard K Scher MD, C Ralph DanielDocument319 pagesNails Diagnosis, Therapy, Surgery Richard K Scher MD, C Ralph DanieldrNo ratings yet
- Thesis On HPV VaccineDocument8 pagesThesis On HPV Vaccinegjftqhnp100% (2)