Professional Documents
Culture Documents
Dengue Fever and Some Case Reports From Delhi Govt. Homoeopathic Dispensaries
Uploaded by
Homoeopathic PulseOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dengue Fever and Some Case Reports From Delhi Govt. Homoeopathic Dispensaries
Uploaded by
Homoeopathic PulseCopyright:
Available Formats
Dengue fever and some case reports from Delhi Govt.
homoeopathic dispensaries
Dr Sudha Bala#1, Dr Gyandas G. Wadhwani#2, Dr Jithesh T.K.#3, Dr Parul G. Wadhwani#4, Dr Vandana Awasthi#5
#1 Chief Medical Officer (H) I/c Homoeo unit Sanjay Gandhi Hospital #2 Chief Medical Officer (H) I/c DGHD South Campus & Aali village #3 Chief Medical Officer (H) I/c DGHD Batla House #4 Reader (H) Deptt of Obs & Gynae NHMC & Hospital #5 Chief Medical Officer (H) I/c DGHD Mangol Puri
Introduction Dengue fever, also known as break-bone fever, is an infectious tropical disease with flu like features transmitted by the bite of an infected female Aedes mosquito. Symptoms appear in 314 days (average 47 days) after the infective bite.
The virus causing Dengue fever (DENV) is an RNA virus of the family Flaviviridae; genus Flavivirus. There are four distinct serotypes of the dengue virus (DEN 1, DEN 2, DEN 3 and DEN 4). Infection with one type usually gives lifelong immunity to that type, but only short-term immunity to the others. Subsequent infection with a different type increases the risk of severe complications. Dengue epidemiology The incidence of dengue has grown dramatically around the world in recent decades. Before 1970, only nine countries had experienced severe dengue epidemics. The disease is now endemic in more than 100 countries in Africa, the Americas, the Eastern Mediterranean, South-east Asia and the Western Pacific. The American, South-east Asia and the Western Pacific regions are the most seriously affected. In India, the first epidemic of clinical dengue-like illness was recorded in Madras (now Chennai) in 1780 and the first virologically proved epidemic of dengue fever (DF) occurred in Calcutta (now Kolkata) and eastern Coast of India in 1963-1964. During the last 50 years number of dengue fever incidences increased tremendously. This year's dengue outbreak in the country was the worst in at last six years, with 55,063 cases reported till October 2013. According to health ministry data, the number of dengue cases has been steadily rising since 2008. Health specialists attribute the steady increase in dengue cases to a number of factors, including heavy rains, intense construction activity in cities and a better surveillance system that enables detection of more cases.
According to the World Health Organization (WHO): Dengue is found in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas. Dengue prevention and control solely depends on effective vector control measures. Dengue infection rates among people who have not been previously exposed to the virus are commonly 40% to 50% during epidemics, but may sometimes reach 80% to 90%. Approximately 2.5 billion people, or two-fifths of the world's population, are now at risk from dengue. Dengue hemorrhagic fever (DHF) is a leading cause of serious illness and death among children in some Asian countries. Approximately half-a-million people with DHF are hospitalized each year, of which many are children. About 2.5% of these patients die. DHF fatality reads may exceed 20% if untreated. If there is access to medical care with health care professionals trained in treating DHF, the death rate may be less than 1%. Vector The Aedes aegypti mosquito is the primary vector of dengue. The virus is transmitted to humans through the bites of infected female mosquitoes. After virus incubation for 410 days, an infected mosquito is capable of transmitting the virus for the rest of its life. Infected humans are the main carriers and multipliers of the virus, serving as a source of the virus for uninfected mosquitoes. Patients who are already infected with the dengue virus can transmit the infection (for 45 days; maximum 12) via Aedes mosquitoes after their first symptoms appear. The Aedes aegypti mosquito lives in urban habitats and breeds mostly in manmade containers. Unlike other mosquitoes Aedes aegypti is a daytime feeder; its peak biting periods are early in the morning and in the evening before dusk. Female Aedes aegypti bites multiple people during each feeding period. Signs and symptoms of Dengue Fever As there are different severities of dengue fever, the clinical features can vary: Mild Dengue Fever Symptoms can appear up to seven days after the bite, and usually last for a week. This form of the disease hardly ever results in serious or fatal complications. The symptoms are: Aching muscles and joints Body rash that can disappear and then reappear High fever Intense headache Pain behind the eyes Vomiting and feeling nauseous DHF Symptoms during onset may resemble mild dengue fever, but gradually worsen. DHF can result in death if not treated in time. Suggestive clinical features are: Bleeding from the mouth/gums 2
Nosebleeds Clammy skin Considerably damaged lymph and blood vessels Internal bleeding, which can result in black vomit and feces Lower number of platelets in blood Sensitive stomach Small blood spots under the skin Weak pulse
Dengue shock syndrome This is the worst form of dengue which can also result in death, again mild dengue fever symptoms may be there, but others suggestive features are: Intense stomach pain Disorientation Sudden hypotension Heavy bleeding Regular vomiting Blood vessels leaking fluid Death Warning Signs of Dengue Fever These usually occur before the onset of severe dengue fever Worsening of abdominal pain Ongoing vomiting Liver enlargement Mucosal bleeding High hematocrit with low platelets Lethargy or restlessness Diagnosing Dengue Fever The diagnosis of dengue is typically made clinically, on the basis of reported symptoms and physical examination, this applies especially in endemic areas. However, early disease can be difficult to differentiate from other viral infections. Investigations may be required to exclude other conditions that cause similar symptoms, such as malaria, leptospirosis, viral hemorrhagic fever, typhoid fever, meningococcal disease, measles, and influenza. It may be difficult to distinguish dengue fever and chikungunya, a similar viral infection that shares many symptoms and occurs in similar parts of the world to dengue. A probable diagnosis may be based on the findings of fever plus any two of the following: nausea and vomiting, rash, generalized pains, low white blood cell count, positive tourniquet test, or any warning sign. The tourniquet test is particularly useful in settings where no laboratory investigations are readily available. Inflate blood pressure cuff to a point midway between systolic and diastolic pressure for 5 minutes. After deflating the cuff, wait for the skin to return to its normal color, and then count the number of petechiae visible in one inch square area on the ventral surface of the forearm. A higher number makes a diagnosis of dengue more likely with the cut off being more than 10 to 20 per 2.5 cm2 (1 inch2).
The earliest change detectable on laboratory investigations is a low white blood cell count, which may then be followed by low platelets and metabolic acidosis. A moderately elevated level of aminotransferase (AST and ALT) from the liver is commonly associated with low platelets and white blood cells. In severe disease, plasma leakage results in hemoconcentration as indicated by a rising hematocrit and hypoalbuminemia. A laboratory confirmation of diagnosis may be made by any of the following tests: 1. Isolation of virus in cell cultures 2. Detection of dengue virus genomic sequences / nucleic acid detection by Real-time PCR (Note: Virus isolation and nucleic acid detection are more accurate than antigen detection, but these tests are not widely available due to their greater cost) 3. Viral antigen detection (Platelia Dengue NS1 Ag assay) allows rapid detection of dengue on the first day of fever, before antibodies appear some 5 or more days later. 4. Detection of IgM & IgG antibodies: Both IgG and IgM are produced after 5 7 days. The highest levels of IgM are detected following a primary infection, but IgM is also produced in reinfection. IgM becomes undetectable 3090 days after a primary infection, but earlier following re-infections. IgG, by contrast, remains detectable for over 60 years and, in the absence of symptoms, is a useful indicator of past infection. After a primary infection IgG reaches peak levels in the blood after 1421 days. In subsequent reinfections, levels peak earlier and the titres are usually higher. Both IgG and IgM provide protective immunity to the infecting serotype of the virus. The detection of IgG alone is not considered diagnostic unless blood samples are collected 14 days apart and a greater than fourfold increase in levels of specific IgG is detected. In a person with symptoms, the detection of IgM is considered diagnostic. Pleural effusion or ascites may be detected by physical examination. The demonstration of fluid on ultrasound may assist in the early identification of dengue shock syndrome. The use of ultrasound is limited by lack of availability in many settings. Dengue shock syndrome is present if pulse pressure drops to 20 mm Hg along with peripheral vascular collapse. Prevention of dengue fever The emphasis for dengue prevention is on sustainable, community-bases, integrated mosquito control, with limited reliance on insecticides. It requires a coordinated community effort to increase awareness about dengue fever / DHF, how to recognise it, and how to control the mosquitoes that transmit it. Residents are responsible for keeping their surroundings free of standing water where mosquitoes can be produced. The transmission of the virus to mosquitoes must be interrupted to prevent the illness. To this end, patients are kept under mosquito netting until the second bout of fever is over and they are no longer contagious. The prevention of dengue requires control or eradication of the mosquitoes carrying the virus that causes dengue. In nations plagued by dengue fever, 4
people are urged to empty stagnant water from old tires, trash cans, and flower pots. Governmental initiatives to decrease mosquitoes also help to keep the disease in check. To prevent mosquito bites, wear long pants and long sleeves. Use mosquito netting while resting. For personal protection, use mosquito repellant sprays that contain DEET (N-diethyl-m-toluamide) when visiting places where dengue is endemic. Some case reports from Delhi Govt homoeopathic dispensaries 1. Ms S., 27yrs, consulted on 23/09/13, for fever with chills since 1week with vomitings and stool frequency 3-4 times/ day and heaviness in head. She was thirstless. She was undergoing allopathic medicines from private practitionner. When homoeopathic treatment was started she was advised her to consume plenty of fluids & hydropathy in case temperature rose. She was advised to stop all allopathic medicines. On 22/09/13, her platelet count was 35,000. Rx Gelsemium 30/2hrly/one day 24/09/13 Fever better; stool frequency decreased. Platelet count 50,000. Rx Gelsemium 30/2hrly/one day 25/09/13 Temp normal; complaining of general weakness. Platelet count 60,000 Rx China30/qid /2days 27/09/13 feeling better. Platelet count on 26th was 75,000 and today 90,000 Rx China30/qid /2days 28/09/13 no complaints; Platelet count 125,000 2. Mr S, 19 yrs, consulted on 17/09/13 for high grade fever since 5days with vomiting, bodyache and weakness. Thirst was good. His Dengue NS1Ag test was positive. Advised to consume lot off fluids & hydrotherapy if fever goes above 100F. Platelet count on 16th was 99,000 and today had come down to 85,000. Rx Arsenic alb 30/ 2hrly for 1 day 18/09/13 No Fever or vomitings. Platelet count 70,000. Rx Ars Alb 30 /qid /one day
19/09/13 General weakness. Platelet count 90,000/Rx China 30 for 2 days 20/09/13 reported with platelet count of 113,000. 3. Mr MP of 36 yrs consulted for fever (101.4 F) with headache and bodyache on 24.9.13. He complained of restlessness and sore feeling over the body esp. back and was unable to lie in one position. His head was hot and extremities cold to touch. He was advised to undergo Dengue NS1 antigen test. Rx Arnica 200 three hourly He reported with a positive Dengue NS1 Antigen test on the following day. Patient complained of persistent fever (around 101F), headache, intense pain was felt all through the body and bones on the basis of which Eupatorium perf 30 was prescribed 2hrly for two days. He was advised to montor his platelet counts daily. The Platelet count on day 3 was 92000. On fourth day the platelet count was 89000 and the patient reported with slight relief in headache and bodyache. Since the fever (101 F) was still present he was now prescribed Eupatorium perf 200 every 2hrs. On day 5 platelet count was 71000 but the headache was absent and bodyache was much better, however fever (101F) was still present. Eupatorium perf 200 was continued. On day 6 the platelet count decreased further to 60000. The patient complained of weakness fever subsided. He was then prescribed Eupatorium perf 1000, 3 doses. On day 7 the platelet count showed a increasing trend and was 66000. The patient was afebrile and asymptomatic. This increasing trend continued and the platelet count was last reported on 4.10.13 as 1.66 lac. Throughout the illness the patient was advised to increase fluid intake and maintain adequate hydration. 4.Ms MS, age 21, years presented with high fever (102F), extreme weakness, pain in lower limbs and severe retching without vomiting on 7/0/13. She was feeling hungry but eating produced severe retching. she was so weak that she had to be supported for slight movements. Her thirst was for small quantities of water at short intervals and drinking also produced retching. Ars alb 30/ 2 hourly was prescribed. Temperature came down to 100.8F on day 2 but she didn't feel better. On 9/10/13 (day 3) dengue profile was done. Dengue NS1 Ag test was positive, platelets were 4 lacs/cumm, TLC was 4000/cumm. Rx Ars alb 200/ 2 hourly was prescribed as the picture was same and patient showed response with the medicine in 30th potency but did not hold. On 12/10/13 (day 6) platelets fell down to 1.5 lacs/cumm. Temperature was 100F, retching was same, weakness was persisting but was less. Ars alb 200 was continued. By day 9 the patient was afebrile, could retain food and water without retching and do her chores without help. 6
On 16/10/13 (day 10) platelets raised upto 3.52 lacs/cumm. Patient's entire demeanour was quite good except that she was having pain and weakness in her lower limbs. Ars alb 1M/tds was prescribed for two days. 2 days later patient reported feeling much better with good thirst, appetite and sleep. 5.Ms S, 21 years presented with fever (102F), sleepiness, bodyache and severe headache since 1 day on 7/10/13 (day 2). She had lost appetite and thirst and was prescribed Gelsemium 200 three hourly. On 9/10/13 (day 4) she presented with dengue profile report Dengue NS1 Ag test was positive, platelets were 1.2 lacs/cumm, TLC was 3400/cumm. Her fever persisted (101-103F) along with all symptoms except that she did not feel sleepy anymore. She was more disturbed by pain in forehead and post-orbital region, which was not affected by movements of eyeballs but aggravated with any movement of head or neck. She was then prescribed Spigelia 200 three hourly. She was afebrile by the following morning (day 5) and reported with platelet count of 80,000. Same medicine was continued. By day 7 her headache was over, she had been afebrile for nealry 48 hours and platelet count was 1.6 lacs. Bibliography: 1. http://www.cdc.gov/dengue/ as accessed on 4-11-13 2. http://www.cdc.gov/Dengue/clinicalLab/ as accessed on 4-11-13 3. http://www.who.int/topics/dengue/en/ as accessed on 4-11-13 4. http://icmr.nic.in/ijmr/2012/september/0905.pdf as accessed on 4-11-13 5. http://www.icmr.nic.in/pinstitute/niv/DENGUE.pdf as accessed on 4-11-13 6. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3510884/ as accessed on 4-1113 7. http://www.nlm.nih.gov/medlineplus/ency/article/001374.htm as accessed on 4-11-13 8. http://www.medicinenet.com/dengue_fever/article.htm as accessed on 4-1113 9. http://en.wikipedia.org/wiki/Dengue_fever as accessed on 4-11-13
You might also like
- Test Bank For Therapeutic Exercise Foundations and Techniques 6th Edition by KisnerDocument6 pagesTest Bank For Therapeutic Exercise Foundations and Techniques 6th Edition by Kisnera33085258962% (13)
- My Thesis Mm2Document179 pagesMy Thesis Mm2Karthik SelvamNo ratings yet
- Acute Case TakingDocument5 pagesAcute Case TakingSumanta KamilaNo ratings yet
- ICR Booklet FinalDocument2 pagesICR Booklet FinalAtit ShethNo ratings yet
- IMCI child health strategyDocument11 pagesIMCI child health strategyIvy100% (2)
- Dermatologic and Cosmetic SurgeryDocument77 pagesDermatologic and Cosmetic SurgeryDr.Tawheed100% (3)
- Vocational Rehabilitation Programs for People with DisabilitiesDocument44 pagesVocational Rehabilitation Programs for People with DisabilitiesKannappa Shetty MudiyanuruNo ratings yet
- A Clinical Experience Natrum Mur Cures A Female With MenorrhagiaDocument4 pagesA Clinical Experience Natrum Mur Cures A Female With MenorrhagiaHomoeopathic PulseNo ratings yet
- My Experience in A Case of Naso-Bronchial AllergyDocument5 pagesMy Experience in A Case of Naso-Bronchial AllergyHomoeopathic Pulse100% (2)
- Experience With Homoeopathy in A Case of Fibroadenoma of BreastDocument8 pagesExperience With Homoeopathy in A Case of Fibroadenoma of BreastHomoeopathic PulseNo ratings yet
- Mumps and Homoeopathy - Short Case SeriesDocument10 pagesMumps and Homoeopathy - Short Case SeriesHomoeopathic PulseNo ratings yet
- National Homoeopathy Seminar On Non Communicable Diseases - A ReportDocument3 pagesNational Homoeopathy Seminar On Non Communicable Diseases - A ReportHomoeopathic PulseNo ratings yet
- A CASE of Acne VulgarisDocument4 pagesA CASE of Acne VulgarisHomoeopathic Pulse100% (1)
- Gibson Miller R - A Synopsis of Homoeopathic Philosophy 1900Document21 pagesGibson Miller R - A Synopsis of Homoeopathic Philosophy 1900Rajesh Rajendran100% (2)
- An Improved Version of The Skin Chapter of Kent RepertoryDocument6 pagesAn Improved Version of The Skin Chapter of Kent RepertoryHomoeopathic PulseNo ratings yet
- Improper Lifestyles Lead to Pseudo-Chronic DiseasesDocument2 pagesImproper Lifestyles Lead to Pseudo-Chronic Diseasesthilothamai madheshwaranNo ratings yet
- D.K.M.M. Homoeopathic Medical College & Hospital, AurangabadDocument14 pagesD.K.M.M. Homoeopathic Medical College & Hospital, AurangabadShreyance Parakh100% (1)
- A Homeopathic Approach To Acute PharyngitisDocument7 pagesA Homeopathic Approach To Acute PharyngitisNadeem KhanNo ratings yet
- The Efficacy of Homoeopathic Simillimum in Treating Atopic Bronchial Asthma (IgEDocument14 pagesThe Efficacy of Homoeopathic Simillimum in Treating Atopic Bronchial Asthma (IgEAraafathNo ratings yet
- Homeopathy and ImmunityDocument57 pagesHomeopathy and ImmunityForam Patel100% (2)
- 3Document60 pages3muni100% (2)
- Borland PDFDocument9 pagesBorland PDFkamalNo ratings yet
- PANJAB UNIVERSITY BHMS SYLLABUSDocument74 pagesPANJAB UNIVERSITY BHMS SYLLABUSprince19000% (1)
- Doctor Vijyakar View On Corona (Homeopathy)Document6 pagesDoctor Vijyakar View On Corona (Homeopathy)drmanishmisraNo ratings yet
- Acne Study Assesses Role of Individualized HomeopathyDocument11 pagesAcne Study Assesses Role of Individualized Homeopathyshivam tiwari100% (1)
- The Brain Fag Syndrome and HomoeopathyDocument8 pagesThe Brain Fag Syndrome and HomoeopathyDr. Rajneesh Kumar Sharma MD HomNo ratings yet
- A Thesis On Homoeopathic Management of GoutDocument3 pagesA Thesis On Homoeopathic Management of GouthirenNo ratings yet
- Eczema - Final Thesis Edited 22.8.09Document152 pagesEczema - Final Thesis Edited 22.8.09579Rishikesh SavardekarNo ratings yet
- My Experience With Kali Brom in A Case of Polycystic Ovarian SyndromeDocument6 pagesMy Experience With Kali Brom in A Case of Polycystic Ovarian SyndromeHomoeopathic Pulse100% (1)
- 149 Aphorism of HomeopathyDocument2 pages149 Aphorism of HomeopathyRaveendra MungaraNo ratings yet
- Homoeopathic PosologyDocument56 pagesHomoeopathic Posologysubhro kanti duttaNo ratings yet
- My Experience With Homoeopathic Concordance Repertory in A Case of Nipple DischargeDocument4 pagesMy Experience With Homoeopathic Concordance Repertory in A Case of Nipple DischargeHomoeopathic Pulse100% (1)
- PROSPECTS AND LIMITATIONS OF HOMOEOPATHY AS A HEALTH CARE SYSTEMDocument43 pagesPROSPECTS AND LIMITATIONS OF HOMOEOPATHY AS A HEALTH CARE SYSTEMDr.bhagyaNo ratings yet
- Thuja As An IntercurrentDocument2 pagesThuja As An Intercurrentmikembad100% (1)
- Chitra Goyal Thesis Starting PagesDocument8 pagesChitra Goyal Thesis Starting PagesramanNo ratings yet
- Paper On Brain Tumor Data PDFDocument5 pagesPaper On Brain Tumor Data PDFBarbara SarterNo ratings yet
- A Case of Lateral Rectus Palsy by DR Sunil KannadaDocument5 pagesA Case of Lateral Rectus Palsy by DR Sunil KannadaHomoeopathic Pulse100% (1)
- Collapse - Margaret Lucy Tyler - HomeopathyBooks - in PDFDocument4 pagesCollapse - Margaret Lucy Tyler - HomeopathyBooks - in PDFMd Jahirul IslamNo ratings yet
- DISSERTATIonDocument101 pagesDISSERTATIonSukhada NimbhorkarNo ratings yet
- Homoeopathy in A Case of Palmo-Plantar Psoriasis: A Case ReportDocument5 pagesHomoeopathy in A Case of Palmo-Plantar Psoriasis: A Case ReportHomoeopathic PulseNo ratings yet
- Life History of Dr.J.T. KentDocument13 pagesLife History of Dr.J.T. KentPrathibha MadikiNo ratings yet
- Sahya Part 3Document26 pagesSahya Part 3Homeopathy TorrentsNo ratings yet
- My Experience in A Case of Haemorrhoids: Prescribing On Alternating Symptoms by DR Shelly AroraDocument5 pagesMy Experience in A Case of Haemorrhoids: Prescribing On Alternating Symptoms by DR Shelly AroraHomoeopathic Pulse100% (1)
- Aggravation in Homeopathy - COMPLETE Information About Aggravation in Homeopathy - Katja SchuettDocument3 pagesAggravation in Homeopathy - COMPLETE Information About Aggravation in Homeopathy - Katja SchuettMd Mohebbullah ChowdhuryNo ratings yet
- Value of Diffrent Kind of SymptomsDocument3 pagesValue of Diffrent Kind of SymptomsNavita SharmaNo ratings yet
- Aethusa CynapiumDocument4 pagesAethusa CynapiumnitkolNo ratings yet
- Fire FlyDocument10 pagesFire FlyMuralidaran SelvarajNo ratings yet
- Asthma and HomoeopathyDocument4 pagesAsthma and HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (1)
- A Case of Hemorrhagic Ovarian Cyst Treated With HomoeopathyDocument4 pagesA Case of Hemorrhagic Ovarian Cyst Treated With HomoeopathyHomoeopathic PulseNo ratings yet
- Scope and Limitations of Homoeopathic Materia MedicaDocument21 pagesScope and Limitations of Homoeopathic Materia Medicadrsabirmomin75% (8)
- Cazuri A.P PDFDocument453 pagesCazuri A.P PDFmihaipopescu0No ratings yet
- A Case of Paediatric CholelithiasisDocument4 pagesA Case of Paediatric CholelithiasisHomoeopathic PulseNo ratings yet
- COPD Study on Risk Factors and Right Heart FailureDocument100 pagesCOPD Study on Risk Factors and Right Heart FailureVimal NishadNo ratings yet
- Appendix of OrganonDocument70 pagesAppendix of OrganonSharyKrishna100% (1)
- Kent's 12 Observations on the Action of Homeopathic RemediesDocument3 pagesKent's 12 Observations on the Action of Homeopathic RemediesIndhumathiNo ratings yet
- Hering Guiding SymptomsDocument10 pagesHering Guiding SymptomsDr. Pankhuri Misra100% (1)
- Homoeopathy and MigraineDocument4 pagesHomoeopathy and MigraineEditor IJTSRDNo ratings yet
- Did Not Nor Did He Merely Read MyDocument13 pagesDid Not Nor Did He Merely Read Myअनुरूपम स्वामीNo ratings yet
- FR Muller-HMC-PGSynopsis (2007-08)Document30 pagesFR Muller-HMC-PGSynopsis (2007-08)mapati66No ratings yet
- Role of Homeopathy in Management of GERDDocument10 pagesRole of Homeopathy in Management of GERDEditor IJTSRDNo ratings yet
- An Effective Homoeopathic Management of Cases of Haemorrhoids Based On Synthesis RepertoryDocument2 pagesAn Effective Homoeopathic Management of Cases of Haemorrhoids Based On Synthesis RepertoryKamal PatidarNo ratings yet
- Homeopathy InfertilityDocument3 pagesHomeopathy Infertilitytakne_007No ratings yet
- Burnett Rediscovered: Clinical Strategies of the Great Homeopath for Modern Practice – Line of Action of Remedies – Organ Remedies – Pathological Similimum – VaccinosisFrom EverandBurnett Rediscovered: Clinical Strategies of the Great Homeopath for Modern Practice – Line of Action of Remedies – Organ Remedies – Pathological Similimum – VaccinosisNo ratings yet
- Order Regarding Enhancement of Age of Superannuation of AYUSH Doctors To 65 YearsDocument1 pageOrder Regarding Enhancement of Age of Superannuation of AYUSH Doctors To 65 YearsHomoeopathic PulseNo ratings yet
- Founder's Day Celebration in DR B R Sur Homeopathic Medical College & Research CentreDocument2 pagesFounder's Day Celebration in DR B R Sur Homeopathic Medical College & Research CentreHomoeopathic PulseNo ratings yet
- A Case of Hemorrhagic Ovarian Cyst Treated With HomoeopathyDocument4 pagesA Case of Hemorrhagic Ovarian Cyst Treated With HomoeopathyHomoeopathic PulseNo ratings yet
- Review of Rheumatology and Homoeopathic Management (Part-1: General Principles)Document20 pagesReview of Rheumatology and Homoeopathic Management (Part-1: General Principles)Homoeopathic Pulse100% (1)
- A Case of Common Warts Treated With HomoeopathyDocument4 pagesA Case of Common Warts Treated With HomoeopathyHomoeopathic PulseNo ratings yet
- Value of Observations in Homoeopathic PracticeDocument6 pagesValue of Observations in Homoeopathic PracticeHomoeopathic Pulse100% (2)
- A Case of Warts Treated With Thuja OccidentalisDocument4 pagesA Case of Warts Treated With Thuja OccidentalisHomoeopathic PulseNo ratings yet
- A Report On ROTP of GDMOs Held On 10th January 2018Document7 pagesA Report On ROTP of GDMOs Held On 10th January 2018Homoeopathic PulseNo ratings yet
- Solution For Crossword of E-Newsletter 'Homoeopathic Pulse' Vol. XIIDocument2 pagesSolution For Crossword of E-Newsletter 'Homoeopathic Pulse' Vol. XIIHomoeopathic PulseNo ratings yet
- Maganum AceticumDocument12 pagesMaganum AceticumHomoeopathic Pulse100% (1)
- Sudoku On Kent's RepertoryDocument3 pagesSudoku On Kent's RepertoryHomoeopathic PulseNo ratings yet
- Understanding Manganum Aceticum Through Hahnemann's Materia Medica PuraDocument12 pagesUnderstanding Manganum Aceticum Through Hahnemann's Materia Medica PuraHomoeopathic Pulse100% (1)
- Development of Medical Expertise and Clinical Decision Making - A Cognitive ApproachDocument4 pagesDevelopment of Medical Expertise and Clinical Decision Making - A Cognitive ApproachHomoeopathic PulseNo ratings yet
- Exclusive Interview With Prof. V. K. CHAUHANDocument5 pagesExclusive Interview With Prof. V. K. CHAUHANHomoeopathic PulseNo ratings yet
- A Case of PsoriasisDocument7 pagesA Case of PsoriasisHomoeopathic PulseNo ratings yet
- Topic of Discussion: "Can The Success Rate of Homoeopathy Be Improved by Relying On Minimum Syndrome of Symptoms As Understanding Every Individual and Individual Case Is A Mystery?"Document6 pagesTopic of Discussion: "Can The Success Rate of Homoeopathy Be Improved by Relying On Minimum Syndrome of Symptoms As Understanding Every Individual and Individual Case Is A Mystery?"Homoeopathic Pulse100% (1)
- Topic of Discussion: Can Psychological Evaluation of The Patient Be Helpful in Treating His Physical Ailments?Document7 pagesTopic of Discussion: Can Psychological Evaluation of The Patient Be Helpful in Treating His Physical Ailments?Homoeopathic PulseNo ratings yet
- Report On Superannuation of DR Sudhir SharmaDocument2 pagesReport On Superannuation of DR Sudhir SharmaHomoeopathic PulseNo ratings yet
- Fundamentals of Rheumatoid Arthritis and Various Homoeopathic Trials in Patients of Rheumatoid Arthritis: An UpdateDocument6 pagesFundamentals of Rheumatoid Arthritis and Various Homoeopathic Trials in Patients of Rheumatoid Arthritis: An UpdateHomoeopathic PulseNo ratings yet
- RPOC and Homoeopathy - A Practical StudyDocument4 pagesRPOC and Homoeopathy - A Practical StudyHomoeopathic Pulse100% (2)
- An Approach To A Case of PCOS/PCOD Through Homoeopathic Medicine ThyroidinumDocument13 pagesAn Approach To A Case of PCOS/PCOD Through Homoeopathic Medicine ThyroidinumHomoeopathic Pulse100% (1)
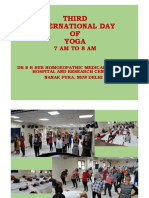
- Celebration of International Day of Yoga at Dr. B. R. Sur Homoeopathic Medical College, Hospital and Research CentreDocument14 pagesCelebration of International Day of Yoga at Dr. B. R. Sur Homoeopathic Medical College, Hospital and Research CentreHomoeopathic PulseNo ratings yet
- Exciting Germany VisitDocument9 pagesExciting Germany VisitHomoeopathic PulseNo ratings yet
- A Case of Warts (Verruca Vulgaris)Document7 pagesA Case of Warts (Verruca Vulgaris)Homoeopathic PulseNo ratings yet
- A Case of Warts Cured Through HomoeopathyDocument3 pagesA Case of Warts Cured Through HomoeopathyHomoeopathic PulseNo ratings yet
- Homoeopathy in Daily LifeDocument1 pageHomoeopathy in Daily LifeHomoeopathic PulseNo ratings yet
- Exclusive Interview With Dr. N. C. ChatterjeeDocument5 pagesExclusive Interview With Dr. N. C. ChatterjeeHomoeopathic Pulse100% (1)
- Research Study On Effectiveness of Homoeopathic Medicines in The Treatment of Alopecia AreataDocument3 pagesResearch Study On Effectiveness of Homoeopathic Medicines in The Treatment of Alopecia AreataHomoeopathic PulseNo ratings yet
- Solution For Crossword of E-Newsletter 'Homoeopathic Pulse' Vol. XIDocument2 pagesSolution For Crossword of E-Newsletter 'Homoeopathic Pulse' Vol. XIHomoeopathic PulseNo ratings yet
- Case Study On Observation and Newborn CareDocument38 pagesCase Study On Observation and Newborn CarePiyush Dutta100% (2)
- IBD MedicationDocument19 pagesIBD MedicationTheghanNo ratings yet
- Chapter II-Vocabulary ExerciseDocument3 pagesChapter II-Vocabulary ExerciseJessica KarinaNo ratings yet
- Col, Major Among 5 Martyred While Rescuing Hostages in J&KDocument14 pagesCol, Major Among 5 Martyred While Rescuing Hostages in J&KAshisNo ratings yet
- The Decline and Fall of Pax Americana, by DesertDocument200 pagesThe Decline and Fall of Pax Americana, by DesertDHOBO0% (1)
- Nursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationDocument10 pagesNursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationmalindaNo ratings yet
- Comp ReviewDocument99 pagesComp ReviewTHAO DANGNo ratings yet
- Ingrown Nail RemovalDocument28 pagesIngrown Nail RemovaljaphetnwapiNo ratings yet
- Slides 6 - ObturationDocument22 pagesSlides 6 - Obturationبراءة أحمد السلاماتNo ratings yet
- Couser Signifying Bodies - ExtractDocument79 pagesCouser Signifying Bodies - ExtractMarceloNo ratings yet
- 1.4.2 Making VaccinesDocument21 pages1.4.2 Making VaccinesVikas Viki0% (1)
- Heart Disease Course PDALongDocument84 pagesHeart Disease Course PDALongArpanpatelNo ratings yet
- Managing Feline Renal Disease: Proper Care Can Help Cats Live LongerDocument7 pagesManaging Feline Renal Disease: Proper Care Can Help Cats Live LongerIme PrezimeNo ratings yet
- Epidemiology SlidesDocument30 pagesEpidemiology SlidesHongMingNo ratings yet
- Osha - Ergonomics - The Study of WorkDocument14 pagesOsha - Ergonomics - The Study of Workhj100% (2)
- Bill Gates Human Chip 060606 - COVID, 19 Corona VirusDocument132 pagesBill Gates Human Chip 060606 - COVID, 19 Corona VirusTheFreeSchool90% (10)
- Hendra - EKGDocument34 pagesHendra - EKGRINANo ratings yet
- CucumberDocument25 pagesCucumberDa Nie LNo ratings yet
- Protein and Amino Acid MetabolismDocument52 pagesProtein and Amino Acid MetabolismRisky OpponentNo ratings yet
- Cardiovascular Embryology StagesDocument109 pagesCardiovascular Embryology StagesBir Singh100% (1)
- Benefits of ChocolateDocument13 pagesBenefits of ChocolateMohd Idris MohiuddinNo ratings yet
- Pom Maker The Ultimate Yarn Guide For Pompom MakingDocument20 pagesPom Maker The Ultimate Yarn Guide For Pompom MakingMaciek PikułaNo ratings yet
- Abortion, Anc, and CS: Focus+ Lecture SeriesDocument24 pagesAbortion, Anc, and CS: Focus+ Lecture SeriesTianah davisNo ratings yet
- Influenza: CausesDocument2 pagesInfluenza: CausesMaui ShihtzuNo ratings yet
- Double Unders MasteryDocument13 pagesDouble Unders MasterySebastian Hurtado100% (2)
- Primer: Gastro-Oesophageal Reflux DiseaseDocument23 pagesPrimer: Gastro-Oesophageal Reflux Diseasejcacia17No ratings yet