Professional Documents
Culture Documents
Rasio Neuro Pati
Uploaded by
Bramantyo DwiputraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rasio Neuro Pati
Uploaded by
Bramantyo DwiputraCopyright:
Available Formats
Volume 2, Issue 4, July 2008 Diabetes Technology Society
Journal of Diabetes Science and Technology
NEUROLOGICAL AND MICROVASCULAR FUNCTION
A Pocket-size Device to Detect Autonomic Neuropathy
Niels Ejskjaer, M.D., Ph.D.,1 Jesper Fleischer, M.Sc., BME,2 Jacob Fleischer, M.D.,3 Poul Erik Jacobsen, M.D.,4 Per Logstrup Poulsen, M.D., DMSci,1 Hans Nygaard, DMSci5
Abstract
Background:
Diabetic autonomic neuropathy (DAN) is a very frequent complication in the diabetic population (type 1 and type 2 diabetes), and patients may suffer debilitating symptoms from various organ systems. In the less symptomatic and even in the asymptomatic condition it severely impacts health. Testing for DAN is currently time-consuming and costly due to the technical setups available today, therefore the examination may not be offered regularly. The purpose of this study was to evaluate the clinical performance of a pocket-size device for detecting DAN by measuring heart rate variability (HRV).
Method:
Ten healthy young males and eight type 1 diabetes patients suffering symptomatic DAN were selected. The standardized spectral analysis equipment VariaPulse TF3 (Sima Media, Olumouc, Czechoslovakia) was used as a reference method for evaluating a prototype of the pocket-size device according to a specified protocol. HRV, inhalation/exhalation ratio (E:I) (deep breathing test), and 30:15 ratio (response going from lying to standing) were measured using both methods. Statistical calculations were performed.
Results:
The correlation between the two devices was R 2 = 0.98 and R 2 = 0.81 when 30:15 ratio and E:I were measured, respectively. Bland-Altman plots showed suitable agreement between the two devices, substantiated by 95% limits of agreement of the differences of 0.014 and 0.033 when 30:15 ratio and E:I were measured, respectively.
Conclusions:
The pocket-size device was fully interchangeable with the hitherto-used, research-based setup. It proved highly suitable for ambulatory testing of autonomic nervous function and may facilitate screening for DAN according to Danish and international recommendations.
J Diabetes Sci Technol 2008;2(4):692-696
Author Affiliations: 1Aarhus University Hospital, Department of Medicine M (Diabetes & Endocrinology) and Clinical Research Units, Aarhus University Hospital, Aarhus, Denmark, 2Medicus Engineering Ltd, The Engineering College of Aarhus, Aarhus, Denmark, 3Soendersoe General Practice, Soendersoe, Denmark, 4Department of Endocrinology, Aarhus University Hospital, Aalborg, Denmark, 5Center of Biomedical Engineering, The Engineering College of Aarhus, Aarhus, Denmark Abbreviations: (DAN) diabetic autonomic neuropathy, (DSP) digital signal processor, (E:I) inhalation/exhalation ratio, (ECG) electrocardiogram, (HRV) heart rate variability, (SD) standard deviation Keywords: autonomic neuropathy, cardiac, complications, diabetes, neuropathy, risk stratification Corresponding Author: Niels Ejskjaer, M.D., Ph.D., Aarhus University Hospital, Department of Medicine M (Diabetes & Endocrinology) and Clinical Research Units, Aarhus University Hospital, Denmark, email address niels.ejskjaer@as.aaa.dk 692
A Pocket-size Device to Detect Autonomic Neuropathy
Ejskjaer
eart rate variability (HRV) measures are an important means of determining cardiac autonomic function.1 Detecting and measuring autonomic dysfunction in the diabetic population is of particular interest and importance. First of all, it may identify patients at risk of developing late complications of diabetes, some of which may be threatening to quality of life and general health. This may in turn enable earlier intervention and treatment for the individual patient.2 Diminished HRV is associated with an increased risk of coronary heart disease and death, and it is hypothesized that low HRV is indicative of poor general health.3 Of particular clinic interest within the diabetic population has been the sudden death in bed syndrome which has been connected to diabetic autonomic neuropathy (DAN).4 It has been shown that low heart rate variability is a risk factor for sudden cardiac death in type 2 diabetes.5 HRV measures are important diagnostic tools for the physician in reaching a correct diagnosis and determining whether autonomic dysfunction plays a role in the patients symptoms. In spite of the importance of determining DAN, testing has rarely been available in hospitals and outpatient settings, and then primarily for research use. Possible explanations for this may be that the apparatus available has been both very time- and cost-consuming to use and of dimensions not allowing bedside testing. These are major obstacles to general testing of the diabetic populations, as is recommended,2,3 and the introduction of the pocket-size device described in this article may offer solutions to overcome these barriers.
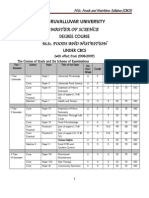
right hands on the two separate metal electrodes, and the device records an electrocardiogram (ECG) signal from which the heart rate and heart rate variability are calculated and shown in the display. An onboard graphical user interface guides the user through the standard tests to assess autonomic function. The patients were instructed to follow the graphical elements on the display. In the deep breathing [inhalation/exhalation ratio (E:I)] test, the graphical user interface visualizes the breathing pattern with a continuously moving bar and a short text message. When the bar moves up, the text Breathe in appears, and when the bar moves down the display shows the text Breathe out. Table 1. Subject Characteristics
Parameters Number of subjects Age (years)* Systolic/diastolic (mm Hg)* Heart Rate (beats/min)* * Mean standard deviation Control 10 34 4 129/79 12/10 56 9 DAN patients 8 43 12 141/91 20/17 82 11
Therefore, the purpose of this study was to evaluate the clinical performance of a pocket-size prototype device for detecting DAN by measuring HRV.
A bedside screening device warrants a user-friendly instrument that does not require substantial time for preparation and data analysis. The present prototype device was optimized for easy ad-hoc bedside examination requiring no preparation before use. For example, the integrated metal electrodes were specially designed for dry operation, and therefore need no gel. The device is based on two-electrode ECG recordings measured by two hand electrodes, and is powered by two 1.5-v AAA batteries to secure mobility and patient safety. The signal processing was performed automatically by a digital signal processor (DSP), where the discrete heartbeats were detected using a correlation algorithm adapting to individual R wave shapes to account for biological variation. Ectopic heart beats were removed automatically by digital filtering. The correlation algorithm is an optimized version of an earlier clinically tested device showing no significant systematic error of the detecting software compared with standard ECG devices. Correlation between the methods was R 2 = 1.00 and R 2 = 0.99 when measuring heart rate and the time domain HRV parameter, root mean square successive difference, respectively.6 A Preliminary test on the MITBIH Database indicates a high precision.
www.journalofdst.org
Materials and Methods
The clinical evaluation of the new device was performed on 10 healthy volunteers and 8 type 1 diabetes patients suffering symptomatic DAN, using recordings from VariaPulse TF3 (Sima Media, Olumouc, Czechoslovakia) as reference (Table 1). All type 1 diabetes patients were recruited from the neuropathy clinic in the department of medicine. All demonstrated two or more of the following symptoms of autonomic dysfunction: gustatory sweating, postural hypotension, diabetic gastroparesis, diabetic diarrhea, or neurogenic bladder. The pocket-size prototype device and clinical setup is shown in Figure 1a. The volunteer places his left and
J Diabetes Sci Technol Vol 2, Issue 4, July 2008
693
A Pocket-size Device to Detect Autonomic Neuropathy
Ejskjaer
For logistical and practical reasons, measurements with the two setups were not performed simultaneously. It was not possible to synchronize the two devices, which of course may lead to differences in the recorded data caused by the time difference between measurements. However, testing was performed under identical
circumstances by the same personnel, with measurement followed immediately by the next.
one
To show that the recorded differences were not a systematic error of the prototype device, we made a control measurement with the VariaPulse TF3 immediately after each recording with the prototype device.
Results
The correlations were first visualized in a scatter plot (Figure 2) and then calculated using the Pearson R 2 test and the mean difference between the methods. A high degree of correlation between the two methods is evident, with Pearson R 2 and mean difference values shown in Table 2 .
Figure 1. The prototype device. (a) The user places her hands on the two electrodes, and heart rate and heart rate variability are measured and shown in the display. The onboard user interface guides the user through the tests, in this case, the deep breathing test. (b) Shows ambulatory testing.
Figure 2. Prototype device and stationary equipment, with line of equality.
www.journalofdst.org
J Diabetes Sci Technol Vol 2, Issue 4, July 2008
694
A Pocket-size Device to Detect Autonomic Neuropathy
Ejskjaer
Note that Figures 24 have different scales for the A plot compared to the B plot because of the great difference in the recorded data between the control group and the diabetic group. The high correlation between the two devices indicates that HRV measurements by the pocket-size device and the stationary VariaPulse TF3 device are highly correlated, but not necessarily in agreement.7,8 Bland-Altman plots Table 2. Pearson R 2 and Mean Difference
Control Group R2 30:15 ratio E:I 0.92 0.81 Mean difference -0.031 -0.033 Patients With DAN R2 0.98 0.81 Mean difference 0.003 0.001
were applied to examine the agreement between the two methods. Figure 3 and Figure 4 depict a high level of agreement between the novel device and VariaPulse TF3. This is substantiated by 95% limits of agreement [1.96 standard deviation (SD)] of the difference showed in Table 3. The limits of agreement between the two devices are 0.14, indicating that 95% of the difference in E:I was Table 3. Limit of agreement
Control Group 1.96SD 30:15 ratio E:I 0.17 0.14 Patients With DAN 1.96SD 0.014 0.033
Figure 3. E:I test: difference of average of prototype device and stationary equipment, with mean and 95% limits of agreement.
Figure 4. 30:15 test: difference of average of prototype device and stationary equipment, with mean and 95% limits of agreement (6 patients only; 2 failed due to amputation/poor health).
J Diabetes Sci Technol Vol 2, Issue 4, July 2008
695
www.journalofdst.org
A Pocket-size Device to Detect Autonomic Neuropathy
Ejskjaer
between 0.107 and -0.173 for the healthy control group with a mean and standard deviation of 1.37 0.15. When measuring E:I two times in a row with the VariaPulse TF3 (with a 1-minute break between the measurements), the limits of agreement were 0.2, indicating a difference in E:I between -0.14 and 0.27 for the same healthy control group. The limits of agreement between the two devices in the group of DAN patients with a response going from lying to standing (30:15 ratio) measured in the range of 1.05 0.04 were 0.014, indicating that 95% of the difference in the 30:15 ratio was between 0.01 and -0.017 for this group. These results indicate a good agreement between the two methods.
for point-of-care screening for diabetic autonomic dysfunction and may facilitate screening according to Danish and international recommendations.
Acknowledgements: The authors would like to thank Medicus Engineering Ltd, Aarhus, Denmark, for funding the development of the present prototype. Biotechnician Merete Moeller at the Clinical Research Department of Department of Medicine M, Aarhus University Hospital, is thanked for valuable assistance. Volunteers and patients are likewise warmly thanked for their time and cooperation. Funding: Equipment was made available by Medicus Engineering Ltd, Aarhus, Denmark. Disclosure: Jesper Fleischer is co-founder of Medicus Engineering Ltd, Aarhus, Denmark. References: 1. Ewing DJ, Martyn CN, Young RJ, Clarke BF. The value of cardiovascular autonomic function tests: 10 years experience in diabetes. Diabetes Care 1985;8(5):491-8. 2. Vinik AI, Erbas T. Recognizing and treating diabetic autonomic neuropathy. Cleve Clin J Med. 2001;68(11):928-30, 932, 934-44. 3. Dekker JM, Crow RS, Folsom AR, Hannan PJ, Liao D, Swenne CA, Schouten EG. Low heart rate variability in a 2-minute rhythm strip predicts risk of coronary heart disease and mortality from several causes: the ARIC Study. Atherosclerosis Risk In Communities. Circulation. 2000;102(11):1239-44. 4. Vinik AI, Maser RE, Mitchell BD, Freeman R. Diabetic autonomic neuropathy. Diabetes Care. 2003;26(5):1553-79. 5. Kataoka M, Ito C, Sasaki H, Yamane K, Kohno N. Low heart rate variability is a risk factor for sudden cardiac death in type 2 diabetes. Diabetes Res Clin Pract. 2004;64(1):51-8. 6. Kristiansen NK, Fleischer J, Jensen MS, Andersen KS, Nygaard H. Design and evaluation of a handheld impedance plethysmograph for measuring heart rate variability. Med Biol Eng Comput. 2005;43(4):516-21. 7. Bland J.M, Altman, DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1(8476):307-10. 8. Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet 1995;346(8982):1085-7.
Discussion
Traditionally, DAN screening devices require manual data analysis and attachment of electrodes or chest belt to the patient beforehand and removal afterward, which prolongs the examination unnecessarily, resulting in increased time consumption and cost. To overcome these obstacles to regular testing, we have examined a new pocket-size device. With only a short introduction to the device, and especially the graphical and textual information on the display, the patients were able to perform the tests correctly. We admit that only two measures of HRV (E:I and 30:15 ratio) have been tested and not the Valsalva maneuver. Ideally, all three tests should be performed in a much broader investigation in the diabetic population. The new version of the device is able to measure the Valsalva maneuver, and results will be published accordingly. In statistical terms, we have shown that the minor time lapse between testing one apparatus and the other is of no significance. Furthermore, we have shown that the tested pocket-size device is fully interchangeable with the well-known stationary setups when used for clinical examinations, both in practical and statistical terms.
Conclusion
A pocket-size prototype device for estimating cardiac autonomic function by measuring HRV was compared to stationary equipment used for diabetic autonomic function testing in a pilot investigation with a limited number of patients in our department. A statistically significant degree of correlation and agreement between measurements using the two setups was found, suggesting that this new pocket-size device is suitable
J Diabetes Sci Technol Vol 2, Issue 4, July 2008
696
www.journalofdst.org
You might also like
- Pink Panther - Diabetes Management - Chapter 1Document6 pagesPink Panther - Diabetes Management - Chapter 1jennmoyerNo ratings yet
- Sanjeevini CombinationsDocument22 pagesSanjeevini Combinationsikonoso100% (1)
- Closing The Quality Gap-A Critical Analysis of Quality Improvement StrategiesDocument206 pagesClosing The Quality Gap-A Critical Analysis of Quality Improvement Strategiesturbina155No ratings yet
- Traditional Chinese Medicine PDFDocument32 pagesTraditional Chinese Medicine PDFGg KNo ratings yet
- Manila Health Programs Promote Maternal, Child HealthDocument5 pagesManila Health Programs Promote Maternal, Child Healthana dizonNo ratings yet
- Family Care PlanDocument5 pagesFamily Care Planjay5ar5jamorabon5torNo ratings yet
- AMC MCQ Exam 2 Questions & Answer KeyDocument38 pagesAMC MCQ Exam 2 Questions & Answer KeyVasile Rusnac100% (4)
- M.sc. Foods and NutritionDocument43 pagesM.sc. Foods and NutritionGeetha Arivazhagan0% (1)
- Benefits of Carrot JuiceDocument0 pagesBenefits of Carrot JuiceeQualizerNo ratings yet
- Chronic Axonal PolyneuropathyDocument19 pagesChronic Axonal PolyneuropathyzhoujNo ratings yet
- Pnle July 2013 DX Test (Np3) III ANSWER PRINTDocument29 pagesPnle July 2013 DX Test (Np3) III ANSWER PRINTPaul EspinosaNo ratings yet
- 1 s2.0 S1078588412006612 Main PDFDocument8 pages1 s2.0 S1078588412006612 Main PDFKenny AmbarwatiNo ratings yet
- 1 s2.0 S1532046420302768 MainDocument10 pages1 s2.0 S1532046420302768 MainDenzo NaldaNo ratings yet
- Tarvainen EMBC2013 Hyperglycaemia HRVDocument5 pagesTarvainen EMBC2013 Hyperglycaemia HRVsurbhi pareekNo ratings yet
- Jurnal 16 - An Internet-Based Tool For Pediatric Cardiac Disease Diagnosis Using Intelligent PhonocardiographyDocument5 pagesJurnal 16 - An Internet-Based Tool For Pediatric Cardiac Disease Diagnosis Using Intelligent PhonocardiographyAngela Erti Suci RosariNo ratings yet
- Machine learning model predicts T2DM risk using HRV featuresDocument10 pagesMachine learning model predicts T2DM risk using HRV featuresSuzanaPetrovicNo ratings yet
- 123I-MIBG Cutoff Points for PDDocument8 pages123I-MIBG Cutoff Points for PDPUIGCOZARNo ratings yet
- Medicina: Diagnosis Accuracy of Carpal Tunnel Syndrome in Diabetic NeuropathyDocument10 pagesMedicina: Diagnosis Accuracy of Carpal Tunnel Syndrome in Diabetic NeuropathyalinaNo ratings yet
- 24 Rudrajit EtalDocument6 pages24 Rudrajit EtaleditorijmrhsNo ratings yet
- Paper Section 3 Draft1Document11 pagesPaper Section 3 Draft1api-568855135No ratings yet
- Hand-Carried Ultrasound Improves Cardiovascular ExamsDocument9 pagesHand-Carried Ultrasound Improves Cardiovascular ExamsAhmedaref EzrinNo ratings yet
- 3 .Validation of An Automated Algorithm in Cardiac Implantable Electronic Devices For The Diagnosis of Advanced Sleep Disordered Breathing in Heart FailureDocument10 pages3 .Validation of An Automated Algorithm in Cardiac Implantable Electronic Devices For The Diagnosis of Advanced Sleep Disordered Breathing in Heart FailureMS GraphicsNo ratings yet
- BioRadio - WirelessECG PDFDocument13 pagesBioRadio - WirelessECG PDFsastrakusumawijayaNo ratings yet
- Development of A Wearable Cardiac Monitoring System For Behavioral Neurocardiac Training: A Usability StudyDocument11 pagesDevelopment of A Wearable Cardiac Monitoring System For Behavioral Neurocardiac Training: A Usability StudyGabriella CsernákNo ratings yet
- Robust Classification of Cardiac Arrhythmia Using Machine LearningDocument9 pagesRobust Classification of Cardiac Arrhythmia Using Machine LearningIJRASETPublicationsNo ratings yet
- Echocardiography Thesis TopicsDocument4 pagesEchocardiography Thesis Topicsbsqw6cbt100% (1)
- Jer 206 BBBDocument31 pagesJer 206 BBBVina SalsabilaNo ratings yet
- Polar V800Document9 pagesPolar V800AdriánNo ratings yet
- Applications of Minimally Invasive Cardiac Output Monitors: Review Open AccessDocument9 pagesApplications of Minimally Invasive Cardiac Output Monitors: Review Open AccessGilbertLiemNo ratings yet
- International Journal of Medical Informatics: Zhe Wang, Lijuan Yao, Dongdong Li, Tong Ruan, Min Liu, Ju GaoDocument8 pagesInternational Journal of Medical Informatics: Zhe Wang, Lijuan Yao, Dongdong Li, Tong Ruan, Min Liu, Ju GaoMuzamilNo ratings yet
- Final DraftDocument10 pagesFinal Draftapi-569174359No ratings yet
- Automatic Measurements of Mitral Annular Plane Systolic Excursion and Velocities To Detect Left Ventricular DysfunctionDocument9 pagesAutomatic Measurements of Mitral Annular Plane Systolic Excursion and Velocities To Detect Left Ventricular DysfunctionMiguelNo ratings yet
- Cuff Less Continuous Non-Invasive Blood Pressure Measurement Using Pulse Transit Time MeasurementDocument6 pagesCuff Less Continuous Non-Invasive Blood Pressure Measurement Using Pulse Transit Time MeasurementTensing RodriguesNo ratings yet
- Tonometria PDFDocument9 pagesTonometria PDFAdán LópezNo ratings yet
- Sensors 19 04708Document34 pagesSensors 19 04708Dr. Md. Salah Uddin YusufNo ratings yet
- Automatic Diagnosis of The 12-Lead ECG Using A Deep Neural NetworkDocument9 pagesAutomatic Diagnosis of The 12-Lead ECG Using A Deep Neural NetworkHema VisvanathanNo ratings yet
- 2021 EUROPEAN SH GuidelinesDocument10 pages2021 EUROPEAN SH GuidelinesJohan Steven RamirezNo ratings yet
- Diagnostic and Prognostic Value of Plasma Volume Status at Emergency Department Admission in Dyspneic Patients Results From The PARADISE CohortDocument11 pagesDiagnostic and Prognostic Value of Plasma Volume Status at Emergency Department Admission in Dyspneic Patients Results From The PARADISE CohortsunhaolanNo ratings yet
- Which Is More Accurate in Measuring The Blood Pressure? A Digital or An Aneroid SphygmomanometerDocument4 pagesWhich Is More Accurate in Measuring The Blood Pressure? A Digital or An Aneroid SphygmomanometerSri YatiNo ratings yet
- Journal of Cardiovascular Magnetic ResonanceDocument13 pagesJournal of Cardiovascular Magnetic ResonanceKrombaNo ratings yet
- Eur J Echocardiogr 2007 Scardovi 30 6Document7 pagesEur J Echocardiogr 2007 Scardovi 30 6Eman SadikNo ratings yet
- Ijecet: International Journal of Electronics and Communication Engineering & Technology (Ijecet)Document7 pagesIjecet: International Journal of Electronics and Communication Engineering & Technology (Ijecet)IAEME PublicationNo ratings yet
- Vrijednost D-Dimer Testa U Dijagnostici Akutne Plućne TromboembolijeDocument6 pagesVrijednost D-Dimer Testa U Dijagnostici Akutne Plućne TromboembolijeIkre19No ratings yet
- Effect of manual therapy vs electrophysical modalities on 2PD in CTSDocument10 pagesEffect of manual therapy vs electrophysical modalities on 2PD in CTSTomBramboNo ratings yet
- IOT Based Wearable Health Monitoring for Pregnant WomenDocument5 pagesIOT Based Wearable Health Monitoring for Pregnant WomenPenrose LearningNo ratings yet
- Transthoracic Echocardiography For Cardiopulmonary Monitoring in Intensive Care (FATE)Document9 pagesTransthoracic Echocardiography For Cardiopulmonary Monitoring in Intensive Care (FATE)Anish H DaveNo ratings yet
- Abstract SetDocument55 pagesAbstract SetelfotsonNo ratings yet
- 1 s2.0 S0208521620300590 MainDocument8 pages1 s2.0 S0208521620300590 MainLucas Micael Gonçalves da SilvaNo ratings yet
- Valtier Et Al 1998Document7 pagesValtier Et Al 1998GilbertLiemNo ratings yet
- Wavelet Based Analysis of Doppler Ultrasonic Wrist-Pulse SignalsDocument5 pagesWavelet Based Analysis of Doppler Ultrasonic Wrist-Pulse SignalsDr Vaishali MathapatiNo ratings yet
- Jam's Final Papers in SaadDocument38 pagesJam's Final Papers in SaadMarinelle TumanguilNo ratings yet
- Ambulatory Blood Pressure Measurement: Brief ReviewDocument8 pagesAmbulatory Blood Pressure Measurement: Brief ReviewBalan AlexandraNo ratings yet
- Estimation of Arterial Stiffness by Using PPG Signal: A ReviewDocument4 pagesEstimation of Arterial Stiffness by Using PPG Signal: A ReviewseventhsensegroupNo ratings yet
- FabioDocument1 pageFabioapi-224000210No ratings yet
- BMC Family PracticeDocument8 pagesBMC Family PracticeVashish RamrechaNo ratings yet
- 2014 Cin CWenfeng Duan LVET0241Document5 pages2014 Cin CWenfeng Duan LVET0241nandaNo ratings yet
- 2014CinCWenfengDuanLVET0241 PDFDocument5 pages2014CinCWenfengDuanLVET0241 PDFnandaNo ratings yet
- HeartBeat Rate and Temperature Monitoring Device 1 EDITEDDocument57 pagesHeartBeat Rate and Temperature Monitoring Device 1 EDITEDFeddy Micheal FeddyNo ratings yet
- Jurnal Code Blue PDFDocument4 pagesJurnal Code Blue PDFAfi Adi KiranaNo ratings yet
- Optic Nerve Sheath Diameter Measured Sonographically As Non-Invasive Estimator of Intracranial Pressure: A Systematic Review and Meta-AnalysisDocument11 pagesOptic Nerve Sheath Diameter Measured Sonographically As Non-Invasive Estimator of Intracranial Pressure: A Systematic Review and Meta-AnalysisWander ValentimNo ratings yet
- Obtaining Accurate In-Office Blood Pressure Readings: Eview RticleDocument4 pagesObtaining Accurate In-Office Blood Pressure Readings: Eview RticleGaema MiripNo ratings yet
- 2019 A Clinically Evaluated Interferometric CW Radar Sys For Contactless Meas of Human Vital ParamsDocument19 pages2019 A Clinically Evaluated Interferometric CW Radar Sys For Contactless Meas of Human Vital Paramsshireyoung717No ratings yet
- ABEST FeaturesDocument92 pagesABEST FeatureselfotsonNo ratings yet
- 1 s2.0 S0933365722001129 MainDocument12 pages1 s2.0 S0933365722001129 MainNaila AshrafNo ratings yet
- Journal Pre-Proof: Computer Methods and Programs in BiomedicineDocument23 pagesJournal Pre-Proof: Computer Methods and Programs in Biomedicinepuneet5246No ratings yet
- Jing Zhou, Jing Li, Tiantian Ye and Yanrong ZengDocument20 pagesJing Zhou, Jing Li, Tiantian Ye and Yanrong ZengNeelma MisraNo ratings yet
- 10.1007@s11739 019 02196 ZDocument10 pages10.1007@s11739 019 02196 ZMaharani Sari NastitiNo ratings yet
- Medical Thermography: A Diagnostic Approach For Type 2 Diabetes Based On Non-Contact Infrared Thermal ImagingDocument9 pagesMedical Thermography: A Diagnostic Approach For Type 2 Diabetes Based On Non-Contact Infrared Thermal ImagingDilip KenNo ratings yet
- Neurology Cardiology Report AnushaDocument11 pagesNeurology Cardiology Report AnushaDanielNo ratings yet
- Journal Pre-Proof: Journal of Cardiac FailureDocument72 pagesJournal Pre-Proof: Journal of Cardiac Failure18ME045No ratings yet
- Non Parametric Analysis of VarianceDocument4 pagesNon Parametric Analysis of VarianceBramantyo DwiputraNo ratings yet
- Hiv Dan AidsDocument42 pagesHiv Dan AidsBramantyo DwiputraNo ratings yet
- HIV and AnesthesiDocument9 pagesHIV and AnesthesiBramantyo DwiputraNo ratings yet
- HIV and AnesthesiDocument9 pagesHIV and AnesthesiBramantyo DwiputraNo ratings yet
- Presentation 1 AnestesiDocument38 pagesPresentation 1 AnestesiBramantyo DwiputraNo ratings yet
- Flip Chart Lesson PlanDocument3 pagesFlip Chart Lesson Planapi-231156895No ratings yet
- Natural Medicines Used in The Traditional Chinese Medical System For Therapy of Diabetes MellitusDocument21 pagesNatural Medicines Used in The Traditional Chinese Medical System For Therapy of Diabetes MellitusparibashaiNo ratings yet
- Quit Smoking BrochureDocument21 pagesQuit Smoking BrochureDumitrita NegoitaNo ratings yet
- Non Communicable DiseasesDocument13 pagesNon Communicable Diseaseszzzsubedi100% (1)
- Health Unit Plan Disease UnitDocument68 pagesHealth Unit Plan Disease UnitKelly0% (1)
- HNF 42 Case StudyDocument25 pagesHNF 42 Case StudyDana SablanNo ratings yet
- English PresentationDocument24 pagesEnglish PresentationAnnaNo ratings yet
- Type 1 Diabetes Mellitus Clinical Presentation - History, Physical Examination, ComplicationsDocument6 pagesType 1 Diabetes Mellitus Clinical Presentation - History, Physical Examination, ComplicationsTrifosa Ika Septiana EryaniNo ratings yet
- Murraya Koenigii: An Updated ReviewDocument21 pagesMurraya Koenigii: An Updated Reviewinternational journal ayurvedic and herbal medicineNo ratings yet
- Deteksi Dini Kegawatdaruratan Maternal Dan Neonatal (RS Persada Medika Cikampek) PEBDocument10 pagesDeteksi Dini Kegawatdaruratan Maternal Dan Neonatal (RS Persada Medika Cikampek) PEBindra pradjaNo ratings yet
- End State Renal Final Case Study MNTDocument18 pagesEnd State Renal Final Case Study MNTapi-242547654No ratings yet
- Hemo Glucose TestDocument3 pagesHemo Glucose TestrocheNo ratings yet
- Non-Pharmacological Treatment Options inDocument9 pagesNon-Pharmacological Treatment Options inkemal ghazaliNo ratings yet
- Compare Coffee vs Green Tea CostsDocument15 pagesCompare Coffee vs Green Tea CostsBrenda Venitta LantuNo ratings yet
- Case Study On Lovely Professional UniversityDocument4 pagesCase Study On Lovely Professional UniversitySatish JhaNo ratings yet
- 1Document4 pages1Surendra SainiNo ratings yet
- New Guidelines For Potassium ReplacementDocument33 pagesNew Guidelines For Potassium ReplacementAnggry MambaitNo ratings yet
- 6 5 Nerves Hormones and HomeostasisDocument19 pages6 5 Nerves Hormones and Homeostasisapi-235355872No ratings yet
- Diabetic NephropathyDocument7 pagesDiabetic NephropathyPlot BUnniesNo ratings yet