Professional Documents
Culture Documents
HGO Aplicaciones Clinicas Jama
Uploaded by
Priscila Tobar Alcántar0 ratings0% found this document useful (0 votes)
28 views4 pagesAll advocate a hemoglobin a 1c level of less than 7%. Questions remain about the effect of all the oral agents and insulin on reducing macrovascular complications. Self-management training is effective in type 2 diabetes.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAll advocate a hemoglobin a 1c level of less than 7%. Questions remain about the effect of all the oral agents and insulin on reducing macrovascular complications. Self-management training is effective in type 2 diabetes.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
28 views4 pagesHGO Aplicaciones Clinicas Jama
Uploaded by
Priscila Tobar AlcántarAll advocate a hemoglobin a 1c level of less than 7%. Questions remain about the effect of all the oral agents and insulin on reducing macrovascular complications. Self-management training is effective in type 2 diabetes.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
SCIENTIFIC REVIEW CLINICIANS CORNER
AND CLINICAL APPLICATIONS
Oral Antihyperglycemic Therapy
for Type 2 Diabetes
Clinical Applications
Eric S. Holmboe, MD
S
EVERALCLINICALPRACTICEGUIDE-
lines for type 2 diabetes are now
available. All advocate a hemo-
globin A
1c
level of less than 7%,
and at least 1 organization has adopted
a target of 6.5%.
1-3
Despite the number
of agents tochoose from, Inzucchi
4
notes
that the only ones evaluated inrandom-
izedcontrolledtrials withregardtoclini-
cally important outcomes are insulin,
metformin, andthe sulfonylureas.
5-7
Two
important clinical trials have demon-
strated that more aggressive glycemic
control in type 2 diabetic patients re-
duced microvascular complications.
Questions remain about the effect of all
the oral agents and insulin on reducing
macrovascular complications.
6,7
Primary care physicians provide
much of the care for patients with type
2 diabetes.
8
Although this article dis-
cusses primarily drug treatment, edu-
cation on self-management, nutrition,
and exercise is essential to help pa-
tients achieve glycemic control. Self-
management training is effective in
type 2 diabetes and should be recom-
mended for all patients.
9
Recommendations for the use of oral
agents for each clinical situation are
basedonthe best evidence available and
accepted clinical guidelines. Informed
decision making about therapy, how-
ever, must involve the patient and in-
clude a clear explanationof therapeutic-
choice rationale, an assessment of his
or her understanding, preferences, and
barriers to care, and a discussion of the
risks and benefits of each therapy.
10-12
An active patient-physician partner-
ship facilitates treatment of this com-
plex, multifaceted disease.
13
The TABLE
provides a brief summary of the avail-
able oral agents and their relative costs.
The BOX provides additional re-
sources.
CLINICAL CONTEXT
Patient 1
Amoderately obese 49-year-oldwoman
(body mass index, 29 kg/m
2
) com-
plains of increased thirst, polyuria, and
fatigue. Her family history is pertinent
for diabetes in her mother and an older
brother. A random plasma glucose se-
rum test shows a level of 480 mg/dL
(26.6 mmol/L). Her serum electrolyte
and anion gap levels are normal.
At this visit, the patient meets Ameri-
canDiabetes Associationcriteria for hav-
ing diabetes.
14
Givenher symptoms and
highblood glucose level, the questionis
whether to start an oral agent or insulin
therapy. Guidelines are not prescrip-
tive regarding the choice of the initial
agent.
1-3,15
One consideration in decid-
ing whether toinitiate insulintherapy or
anoral agent is glucose toxicity.
16,17
High
Author Affiliations: Department of Medicine, Yale
University School of Medicine, NewHaven, Conn, and
Qualidigm (Connecticut Peer Review Organization),
Middletown, Conn.
Corresponding Author and Reprints: Eric S. Holm-
boe, MD, Yale Primary Care Residency Program, Wa-
terbury Hospital, 64 Robbins St, Waterbury, CT 06721
(e-mail: eholmboe@msn.comor eholmboe@wtbyhosp
.chime.org).
Scientific Review: Clinical Applications Section Editor:
Wendy Levinson, MD, Contributing Editor.
Oral agents are the mainstay of pharmacologic treatment for type 2 diabe-
tes, and physicians now have a number of agents to choose from. However,
more choices translate into more complex decision making. Many patients
with diabetes have associated comorbidities, and most diabetic patients will
require more than 1 agent to achieve good glycemic control. This article il-
lustrates several of the pharmacologic approaches to type 2 diabetes through
4 situations that use principles of evidence-based medicine. The scenarios
also highlight some of the difficulties in choosing the optimal pharmaco-
logic treatment regimen for individual patients. Physicians should also rec-
ognize that type 2 diabetes is a multisystemdisorder that requires multidis-
ciplinary care, including education and ongoing counseling for effective patient
self-management of the disease. Finally, patient preferences are a vital com-
ponent of informed decision making for pharmacologic treatment of diabetes.
JAMA. 2002;287:373-376 www.jama.com
See also pp 360 and 379.
2002 American Medical Association. All rights reserved. (Reprinted) JAMA, January 16, 2002Vol 287, No. 3 373
on October 10, 2007 www.jama.com Downloaded from
levels of glucose are toxic to pancreatic
beta cells, impairing insulinsecretionin
the face of relative insulindeficiency. Al-
thoughnot studiedina randomizedcon-
trolled trial, initial treatment with insu-
lin has been suggested to allow more
rapid control of plasma glucose, recov-
ery of beta cell function, and better sub-
sequent response to oral agents.
17,18
Ad-
ditionally, insulindosage canbe adjusted
quickly, facilitating more rapid control
of hyperglycemia and associated symp-
toms.
15-17
Once a stable target glucose
level has beenachieved, the patient may
be able to begin receiving an oral agent.
However, insulin therapy does require
immediate patient education on injec-
tion techniques, use of a home glucose
meter, and identification and treat-
ment of hypoglycemic reactions. If avail-
able locally, certifieddiabetes nurse edu-
cators can be particularly helpful in this
process. Deciding whether to start in-
sulin therapy also requires assessment
of the patients understanding and
wishes.
10
Whenthepatient isswitchedtoanoral
agent or an oral agent is used as initial
therapy, guidelines suggest that either
a sulfonylurea or metformin agent is
appropriate. However, given that this
patient is moderately obese, metformin
would be the recommended initial
agent.
4,7,15
It tends topromoteweight loss
andisequallyeffectiveinloweringhemo-
globin A
1c
compared with sulfonylurea
and thiazolidinedione (TZD) agents.
4
Givenher degree of hyperglycemia, this
patient mayeventuallyneed2oral agents
to achieve adequate control.
Patient 2
A 57-year-old man with type 2 diabe-
tes treated for 9 years is currently re-
ceiving glyburide at a dosage of 10
mg/d. His hemoglobin A
1c
level a week
ago was 8.5%. You suggest adding met-
formin, but the patient wonders why he
cannot increase his glyburide dose be-
cause his hemoglobin A
1c
level was al-
ways controlled well by this medica-
tion and he has been told that 10 mg is
only half the maximal dose.
Although daily doses of up to 20 mg
of glyburide and 40 mg of glipizide are
approved and can be used, data have
clearly shownthat, above 10to12mg/d,
the additional gain in glycemic control
is marginal.
19
Inaddition, the failure rate
of sulfonylurea therapy is 5%yearly, and
this patient has been receiving gly-
buride therapy for 9years.
4,6,7,15
Thus, in-
creasing his sulfonylurea dose is highly
unlikelytohelphimreachthe target level
of hemoglobin A
1c
. Likewise, switching
to another single oral agent suchas met-
formin, TZD, or meglitinide or another
nonsulfonylurea secretagogue is un-
likely to lead to adequate glycemic con-
trol, given the duration of his diabetes.
Therefore, addition of another agent
should be considered. The United
Kingdom Prospective Diabetes Study
(UKPDS) andother trials foundthat add-
ing metformin to sulfonylurea therapy
loweredhemoglobinA
1c
levels.
4,7,20,21
The
UKPDS, however, found an unex-
pected increase indiabetes-related mor-
tality with this combination, although
when all patients who were actually
treatedwithmetforminaccordingtopro-
tocol analysis were investigated, a 19%
reductionindiabetes-related end points
was observed.
7,22
Another optionis toadd
a TZD; this combinationhas also shown
substantial reductions inhemoglobinA
1c
levels.
4
Although no definite evidence
exists of severe hepatotoxicity withrosi-
glitazone and pioglitazone, frequent
monitoring of liver enzymes is still re-
quired because of troglitazones associa-
tion with hepatotoxicity.
Patient 3
A 55-year-old woman was diagnosed
with diabetes almost 10 years ago and is
Table. Summary of Available Oral Agents and Costs
Monthly
Retail Cost, $*
Comparative
Cost, $/d
Sulfonylureas
Micronase (glyburide), 5mg, ii bid #120 112 3-4
Diabeta (glyburide), 5 mg, ii bid #120 101 3-4
Generic glyburide, 5 mg, ii bid #120 52 2
Glynase (micronized glyburide), 6 mg, i bid #60 86 2-3
Generic micronized glyburide, 6mg, i bid #60 58 2
Glucotrol (glipizide), 10 mg, ii bid #120 111 3-4
Generic glipizide, 10 mg, ii bid #120 46 2
Glucotrol XL (glipizide GITS), 10 mg/d, ii #60 50 2
Amaryl (glimepiride), 4 mg/d, ii #60 60 2-3
Biguanides
Glucophage (metformin), 500 mg, ii bid #120 102 3-4
Glucophage XR (metformin, extended release),
500 mg/d, iiii #120
88 2-3
-Glucosidase inhibitors
Precose, 100 mg, i tid #90 78 2-3
Glyset, 50 mg, i tid #90 73 2-3
Thiazolidinediones
Avandia, 4 mg, i bid #60 175 4
Actos, 45 mg/d, i #30 169 4
Nonsulfonylurea secretagogues
Prandin (repaglinide), 2 mg, ii tid #180 165 4
Starlix (nateglinide), 120 mg, i tid #90 103 3-4
Fixed combinations
Glucovance (glyburide/metformin), 5 mg/500 mg, ii bid #120 105 3-4
Insulins (1 vial, 100 U)
Novolin or Humulin NPH 24 2
Lantus 44 2-3
Humalog 45 2-3
Humalog 75/25 46 2-3
*Cost is based on the mean of retail costs in 2001 at 3 New Haven County, Connecticut, national chain pharmacies
and is adapted from Inzucchis Yale Diabetes Center Facts and Guidelines 2001, available from Takeda Pharma-
ceuticals America; bid indicates 2 times daily; tid, 3 times daily; roman numerals, the number of tablets in each dose;
and numbers following a pound sign, the number of tablets in a months supply.
Add approximately $5 to $15 monthly for insulin syringes and alcohol wipes for 1 to 2 injections daily.
ORAL ANTIHYPERGLYCEMIC THERAPY FOR TYPE 2 DIABETES
374 JAMA, January 16, 2002Vol 287, No. 3 (Reprinted) 2002 American Medical Association. All rights reserved.
on October 10, 2007 www.jama.com Downloaded from
receiving 20 mg of glipizide daily and
1000 mg of metformin twice daily. Her
hemoglobinA
1c
level is 8.5%. She is ada-
mant about not starting insulin therapy
becauseshebelieves it signals thelast step
before dying from diabetes. What are
your options?
Before embarking on a discussion
about therapy, the physicianshouldfirst
acknowledge and discuss the patients
concerns about insulintherapy. Regard-
ing drug treatment, will any of the re-
maining available oral agents lower he-
moglobin A
1c
levels in this patient?
Because of its relative decreased effi-
cacy in lowering hemoglobin A
1c
levels,
acarbose would not be a good therapeu-
tic option.
4,23
The meglitinides are insu-
lin secretagogues and therefore would
not be effective in a patient already re-
ceiving a sulfonylurea agent.
4
The only
feasible additional oral agent to use
would be rosiglitazone or pioglitazone,
both of which are approved for use in
combinationwithmetforminor a sulfo-
nylurea agent. Arecent study foundthat
43% of patients receiving triple oral
therapy (sulfonylurea, metformin, and
troglitazone) achieveda target hemoglo-
binA
1c
value (8%) comparedwithonly
6% of patients taking the metformin-
sulfonylurea combination.
24
Regardless of approach, the maingoal
for this relatively young patient re-
mains optimal glycemic control with a
hemoglobin A
1c
level below6.5%. Insu-
lin therapy is another reasonable op-
tion and is less expensive than adding
a TZD(Table).
1,4,15
If rosiglitazone or pio-
glitazone is added, the full effect of the
TZDtherapy may not be apparent for 4
to 12 weeks, but a hemoglobin A
1c
level
should be assessed at 3 months. Al-
though this patient is resistant to start-
ing insulintherapy, better glycemic con-
trol through insulin therapy in the
UKPDS
6
and the Kumomato Trial
5
led
to a reduction in microvascular compli-
cations. If the target hemoglobinA
1c
level
is not attained with the addition of a
TZD, theninsulintherapy is the best op-
tion. Many patients will eventually re-
quire insulin therapy for adequate gly-
cemic control. In the UKPDS, for
example, approximately 10% of pa-
tients initially assigned to receive a sul-
fonylurea agent hadtostart receiving in-
sulin therapy during the trial.
6
Talking
tothe patient mayhelpher overcome her
reluctance to start insulin therapy.
25
Patient 4
A72-year-old man with a history of hy-
pertension, myocardial infarction, and
New York Heart Association class II
congestive heart failure comes to the
clinic for a routine follow-up visit. At
his last visit 6 months ago, his random
blood glucose level was 180 mg/dL
(10.0 mmol/L). He was not subse-
quently tested for a fasting blood glu-
cose level but was encouraged to lose
weight and maintain a proper diet. He
now complains of having had poly-
uria and constant thirst for the past 2
months. His randombloodglucose level
is tested in your office and is 260 mg/dL
(14.4 mmol/L). His creatinine level was
1.7 mg/dL (129.63 mol/L) 6 months
ago. The patient weighs 83.3 kg. He is
receiving spironolactone, furosemide
for his hypertension, and an angioten-
sin-converting enzyme inhibitor for
congestive heart failure. What are your
therapeutic options?
Although determining a fasting glu-
cose level and a baseline hemoglobin
A
1c
level will be helpful, the patient now
has symptomatic diabetes and war-
rants pharmacologic treatment. Al-
though it appears that diet did not con-
trol his blood glucose level, reinforcing
the importance of diet and lifestyle
shouldstill be attempted.
26
Evidence ex-
ists that suggests consulting a nutri-
tionist or diabetes educator improves
glycemic control.
27,28
Regarding drug therapy, there are sev-
eral important issues to consider for this
older diabetic patient. First, what should
the target hemoglobin A
1c
level be? No
Box. Resources for Primary Care Physicians and Patients
Guidelines
American Diabetes Association. Standards of medical care for patients with dia-
betes mellitus. Diabetes Care. 2001;24(suppl 1):S33-S43. Web site available at: http://
www.diabetes.org.
Institute for Clinical Systems Improvement (ICSI). Web site available at: http://
www.icsi.org. Printed copies can be obtained from ICSI, 800934th Ave S, Suite
1200, Bloomington, MN 55425.
American Association of Clinical Endocrinologists. Web site available at: http://
www.aace.com/clin/guides/diabetes.
All guidelines listed above are also available at: http://www.guideline.gov (Na-
tional Guideline Clearinghouse).
Organizations
American Diabetes Association, 1701 N Beauregard St, Alexandria, VA 22311.
Phone: (800) 842-6323. Information and educational brochures are available for
patients. The association has offices across the United States.
American Dietetic Association. Diabetes Care & Educational Practice Group,
216 W Jackson Blvd, Suite 800, Chicago, IL 60606. Phone: (800) 366-1655. Web
site available at: http://www.eatright.org. Good source for information about nu-
tritional therapy in diabetes.
Centers for Medicare and Medicaid Services (CMS). Web site available at: http://
www.hcfa.gov. The CMS concentrates on diabetes improvement efforts for Medi-
care patients. Quality of care programs for the CMS are managed across the United
States by peer-review organizations, all of which have educational material and
ongoing projects designed to help the primary care provider care for Medicare pa-
tients with type 2 diabetes.
Centers for Disease Control and Prevention. Web site available at: http://www
.cdc.gov/nccdphp/ddt/ddthome.htm.
National Diabetes Education Program. Web site available at: http://www.ndep
.nih.gov.
ORAL ANTIHYPERGLYCEMIC THERAPY FOR TYPE 2 DIABETES
2002 American Medical Association. All rights reserved. (Reprinted) JAMA, January 16, 2002Vol 287, No. 3 375
on October 10, 2007 www.jama.com Downloaded from
outcome data for elderly diabetics ex-
ist. However, several studies have found
that lower hemoglobin A
1c
levels are as-
sociated with lower costs for patients in
all age groups, especially those withcar-
diovascular disease,
29-31
and better con-
trol of diabetes improves the quality of
life for older diabetic patients.
32-34
Sec-
ond, what are the appropriate oral agents
for this patient?Givenhis underlyingcar-
diovascular disease, metforminwouldbe
anideal agent, but his history of conges-
tive heart failure andelevatedserumcre-
atinine levels are absolute contraindica-
tions. Remaining agents to lower blood
glucose levels are a sulfonylurea, a rapid-
acting secretagogue, or a TZD. A major
concernabout startingsulfonylureatreat-
ment in older patients is hypoglycemia
that canbe profound and prolonged be-
cause of the long half-life of the second-
generation agents. If a long-acting sul-
fonylurea is chosen, the lowest possible
starting dose (eg, 2.5 mg of glipizide)
should be initiated and the patient fully
educated about hypoglycemic reac-
tions andtreatment.
4,34
His mildrenal in-
sufficiency also places him at increased
risk for hypoglycemia. If hypoglycemia
is a major concern related to other un-
derlying health issues (eg, the patient is
at significant riskfor falls or lives alone),
a rapid-acting secretagogue taken with
meals may be safer because of its shorter
half-life.
4
The disadvantage is the fre-
quent dosing schedule required with
these agents. Acarbose couldbe tried, but
the magnitude of glucose-level reduc-
tion is less than that with other agents,
the adverse gastrointestinal effects may
bedifficult for this older patient withcon-
gestive heart failure, and again the drug
must be taken several times a day.
4
A
TZD may be prescribed but should be
usedonly cautiously inthis patient with
class II congestive heart failure. Be-
cause of their propensity to expand
plasma volume, TZDs are clearly con-
traindicatedfor patients withclass III and
IVcongestive heart failure. Therefore, for
this patient anoral agent may not be the
best treatment and in fact may increase
the risk of adverse events because of his
multiple comorbidities. Despite the mild
degree of hyperglycemia, insulinmay be
the best choice as an initial agent in this
patient. It has several advantages: flex-
ibility withregardtodose anddosing ad-
justments andmultiple preparations that
allow physicians to tailor a treatment
regimen that best meets the needs and
goals of the patient.
CONCLUSIONS
Decisions about treatment with oral
agents require a number of important
considerations, including drug efficacy
and adverse effects, strength of evi-
dence, patient preferences, cost, and ef-
fective use of nonpharmacologic thera-
pies such as diet and exercise. Patient
involvement inself-management is criti-
cal to successful glycemic control, and
all therapeutic choices must involve a
comprehensive dialogue and negotia-
tionbetweenpatient and physician. Or-
ganizations to obtain resources for car-
ing for diabetic patients are provided in
the Box. For the majority of patients, the
overarching goal is to lower the hemo-
globinA
1c
level toas close tonormal and
as safely as possible.
REFERENCES
1. American Diabetes Association. Standards of medi-
cal care for patients with diabetes mellitus. Diabetes
Care. 2001;24(suppl 1):S33-S43.
2. American Association of Clinical Endocrinologists.
The AACE medical guidelines for the management of
diabetes mellitus. Endocr Pract. 2000;6:1-5.
3. Management of Type 2 Diabetes Mellitus. Bloom-
ington, Minn: Institute for Clinical Systems Improve-
ment; 2000. ICSI guideline GOH07.
4. Inzucchi S. Oral antihyperglycemic therapy for type
2 diabetes: scientific review. JAMA. 2002;287:360-
372.
5. Ohkubo Y, Kishikawa H, Araki E, et al. Intensive
insulin therapy prevents the progression of diabetic
microvascular complications in Japanese patients with
non-insulin-dependent diabetes mellitus. Diabetes Res
Clin Pract. 1995;28:103-117.
6. UK Prospective Diabetes Study Group. Intensive
blood-glucose control with sulphonylureas or insulin
comparedwithconventional treatment andrisk of com-
plications in patients with type 2 diabetes (UKPDS 33).
Lancet. 1998;352:837-853.
7. UK Prospective Diabetes Study Group. Effect of in-
tensive blood-glucose control with metformin on com-
plications in overweight patients with type 2 diabe-
tes (UKPDS 34). Lancet. 1998;352:854-865.
8. Griffin S, Kinmonth AL. Systems for routine sur-
veillance for people with diabetes mellitus [Cochrane
Reviewon CD-ROM]. Oxford, England: Cochrane Li-
brary, Update Software; 2000;issue 4.
9. Norris SL, Engelgau MM, Venkat Narayan KMV.
Effectiveness of self-management training in type 2
diabetes. Diabetes Care. 2001;24:561-587.
10. Braddock CH, Edwards KA, Hasenberg NM, et al.
Informeddecisionmakinginoutpatient practice. JAMA.
1999;282:2313-2320.
11. Guyatt GH, Sackett DL, Cook DJ, for the Evidence-
Based Medicine Working Group. Users guides to the
medical literature, II: how to use an article about
therapy or prevention, B: what were the results and
will they help me in caring for my patients? JAMA.
1994;271:59-63.
12. Deber RB, Kraetschmer N, Irvine J. What role do
patients wish to play in treatment decision making?
Arch Intern Med. 1996;156:1414-1420.
13. Wagner EH, Davis C, Schaefer J, et al. A survey
of leading chronic disease management programs.
Managed Care Q. 1999;7:56-66.
14. Expert Committee on the Diagnosis and Classi-
ficationof Diabetes Mellitus. Report of the Expert Com-
mittee on the Diagnosis and Classification of Diabe-
tes Mellitus. Diabetes Care. 2001;24(suppl):S5-S20.
15. DeFronzo RA. Pharmacologic therapy for type 2
diabetes. Ann Intern Med. 1999;131:281-303.
16. Yki-Jarvinen H. Acute and chronic effects of hy-
perglycaemia on glucose metabolism. Diabet Med.
1997;14(suppl 3):S32-S37.
17. Rossetti L, Giaccari A, DeFronzo RA. Glucose tox-
icity. Diabetes Care. 1990;13:610-630.
18. Kayashima T, Yamaguchi K, Konno Y, Nani-
matsu H, Aragaki S, Shichiri M. Effects of early intro-
ductionof intensive insulintherapy onthe clinical course
in non-obese NIDDMpatients. Diabetes Res Clin Pract.
1995;28:119-125.
19. Stenman S, Melander A, Groop PH, Groop LC.
What is the benefit of increasing the sulfonylurea dose?
Ann Intern Med. 1993;118:169-172.
20. Hermann LS. Therapeutic comparison of metfor-
min and sulfonylurea, alone and in various combina-
tions. Diabetes Care. 1994;17:1100-1109.
21. Erle G, Lovise S, Stocchiero C, et al. A compari-
son of preconstituted, fixed combinations of low-
dose glyburide plus metformin versus high-dose gly-
buride alone in the treatment of type 2 diabetic
patients. Acta Diabetol. 1999;36:61-65.
22. Palumbo PJ. Editorial. Endocr Pract. 1998;4:428-
429.
23. Scheen AJ. Clinical efficacy of acarbose in diabe-
tes mellitus. Diabetes Metab. 1998;24:311-320.
24. Yale J-F, Valiquett TR, Ghazzi MN, et al. The effect
of a thiazolidinedione drug, troglitazone, on glyce-
mia in patients with type 2 diabetes mellitus poorly
controlled with sulfonylurea and metformin. Ann In-
tern Med. 2001;134:737-745.
25. Snoek FJ. Barriers to good glycemic control. Int J
Obes Relat Metab Disord. 2000;24(suppl):S12-S20.
26. Maazuca SA, Moorman NH, Wheeler ML, et al.
The diabetes education study. Diabetes Care. 1986;
9:1-10.
27. Peyrot M, Rubin RR. Modeling the effects of dia-
betes education on glycemic control. Diabetes Educ.
1994;20:143-148.
28. Franz MJ, Monk A, Barry B, et al. Effectiveness
of medical nutrition therapy provided by dietitians in
the management of non-insulin diabetes mellitus.
J Am Diet Assoc. 1995;95:1009-1017.
29. Gilmer TP, OConnor PJ, Manning WG, Rush WA.
The cost to health plans of poor glycemic control. Dia-
betes Care. 1997;20:1847-1853.
30. Wagner EH, Sandhu N, Newton KM, et al. Ef-
fects of glycemic control on healthcare costs and uti-
lization. JAMA. 2001;285:182-189.
31. Testa MA, Simonson DC. Health economic ben-
efits and quality of life during improved glycemic con-
trol in patients with type 2 diabetes mellitus. JAMA.
1998;280:1490-1496.
32. Wandell PE, Tovi J. The quality of life of elderly
diabetics. J Diabetes Complications. 2000;14:25-30.
33. Goddijn PP, Bilo HJ, Feskens EJ, et al. Longitudi-
nal study on glycemic control and quality of life in pa-
tients with type 2 diabetes mellitus referred for inten-
sive control. Diabet Med. 1999;16:23-30.
34. Jennings PE. Oral antihyperglycaemics: consid-
erati ons i n ol der pati ents wi th non-i nsul i n-
dependent diabetes mellitus. Drugs Aging. 1997;10:
323-331.
ORAL ANTIHYPERGLYCEMIC THERAPY FOR TYPE 2 DIABETES
376 JAMA, January 16, 2002Vol 287, No. 3 (Reprinted) 2002 American Medical Association. All rights reserved.
on October 10, 2007 www.jama.com Downloaded from
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The Predominantly Plant-Based Pregnancy GuideDocument179 pagesThe Predominantly Plant-Based Pregnancy GuidePriscila Tobar Alcántar100% (1)
- Hiper Hipoparatir NejmDocument13 pagesHiper Hipoparatir NejmPriscila Tobar AlcántarNo ratings yet
- Ajuste de Dosis de Medicamentos en Paciente RenalDocument46 pagesAjuste de Dosis de Medicamentos en Paciente RenalThelma Cantillo RochaNo ratings yet
- La Teta Cansada - Montserrat Reverte PDFDocument4 pagesLa Teta Cansada - Montserrat Reverte PDFIpNo ratings yet
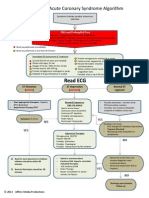
- ACS Algorithm DiagramDocument1 pageACS Algorithm DiagramPriscila Tobar Alcántar100% (1)
- Diabetic KetoacidosisDocument16 pagesDiabetic Ketoacidosisdrtpk100% (2)
- Breastfeeding Medicine Protocol on GalactogoguesDocument8 pagesBreastfeeding Medicine Protocol on GalactogoguespaulinaovNo ratings yet
- MayoClinProc Anemia in Adults A Contemporary Approach To DiagnosisDocument7 pagesMayoClinProc Anemia in Adults A Contemporary Approach To DiagnosisBarbarita Alvarado CamposNo ratings yet
- Acute Appendicitis in Adults ManagementDocument16 pagesAcute Appendicitis in Adults ManagementPriscila Tobar AlcántarNo ratings yet
- Myxedema AscitesDocument4 pagesMyxedema AscitesPriscila Tobar AlcántarNo ratings yet
- Acute Appendicitis in AdultsDocument20 pagesAcute Appendicitis in AdultsPriscila Tobar AlcántarNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- HCC GuidebookDocument153 pagesHCC Guidebookleadmonkeyboy100% (2)
- Deteksi Dini Kegawatdaruratan Maternal Dan Neonatal (RS Persada Medika Cikampek) PEBDocument10 pagesDeteksi Dini Kegawatdaruratan Maternal Dan Neonatal (RS Persada Medika Cikampek) PEBindra pradjaNo ratings yet
- Magic Wave July 2011 PDF 69Document19 pagesMagic Wave July 2011 PDF 69Budi TurmokoNo ratings yet
- Marketing Plan LKDFNDDocument3 pagesMarketing Plan LKDFNDapi-392259592No ratings yet
- Nutrition ManualDocument405 pagesNutrition ManualRaghavendra Prasad100% (1)
- Acanthosis NigricansDocument32 pagesAcanthosis NigricansZeliha TürksavulNo ratings yet
- Anatomia SufletuluiDocument1 pageAnatomia SufletuluiAlexandrina DeaşNo ratings yet
- Genetically Engineered Insulin and Its Pharmaceutical AnaloguesDocument11 pagesGenetically Engineered Insulin and Its Pharmaceutical AnaloguesNatália ZeninNo ratings yet
- DR Sibli PDFDocument19 pagesDR Sibli PDFIva Dewi Permata PhilyNo ratings yet
- Diabetes and Stroke RisksDocument26 pagesDiabetes and Stroke RisksPrecious SantayanaNo ratings yet
- Shoulder DystociaDocument13 pagesShoulder Dystociarolla_hiraNo ratings yet
- Risk Factors for PeriodontitisDocument174 pagesRisk Factors for PeriodontitisdevikaNo ratings yet
- National Geographic March 2016Document148 pagesNational Geographic March 2016Anonymous Azxx3Kp9No ratings yet
- Step 1 UworldDocument25 pagesStep 1 UworldKarl Abiaad100% (23)
- Dietary Management of Indian Vegetarian Diabetics: M. Viswanathan and V. MohanDocument2 pagesDietary Management of Indian Vegetarian Diabetics: M. Viswanathan and V. Mohanrockingtwo07No ratings yet
- Hemo Glucose TestDocument3 pagesHemo Glucose TestrocheNo ratings yet
- FIT UK Recommendations For Injection TechniqueDocument48 pagesFIT UK Recommendations For Injection TechniqueMadeleine OchianuNo ratings yet
- The UK Prospective Diabetes Study (UKPDS) : Clinical and Therapeutic Implications For Type 2 DiabetesDocument6 pagesThe UK Prospective Diabetes Study (UKPDS) : Clinical and Therapeutic Implications For Type 2 DiabetesLaila KurniaNo ratings yet
- AAHA Diabetes Guidelines - FinalDocument21 pagesAAHA Diabetes Guidelines - FinalKátia SouzaNo ratings yet
- Benefits of Carrot JuiceDocument0 pagesBenefits of Carrot JuiceeQualizerNo ratings yet
- Natural Medicines Used in The Traditional Chinese Medical System For Therapy of Diabetes MellitusDocument21 pagesNatural Medicines Used in The Traditional Chinese Medical System For Therapy of Diabetes MellitusparibashaiNo ratings yet
- International Nursing Conference Abstracts - AINEC 2018Document42 pagesInternational Nursing Conference Abstracts - AINEC 2018Rika Fatmadona100% (1)
- Insulin Therapy in Type 1 Diabetes UpdateDocument83 pagesInsulin Therapy in Type 1 Diabetes UpdateasupicuNo ratings yet
- Diabetic NephropathyDocument7 pagesDiabetic NephropathyPlot BUnniesNo ratings yet
- Form 4 - Graphic Stimuli and Short TextsDocument3 pagesForm 4 - Graphic Stimuli and Short TextsRupert Quentin William Kingston PNo ratings yet
- Change Management in ActionDocument28 pagesChange Management in Actionsikkim blossomsNo ratings yet
- Interactive Patient Case Management #1Document33 pagesInteractive Patient Case Management #1Luzman HizrianNo ratings yet
- 2015 March 11 Peanut ReviewDocument28 pages2015 March 11 Peanut ReviewEmmanuel AbonNo ratings yet
- Laboratory Tests To Evaluate Fluid StatusDocument52 pagesLaboratory Tests To Evaluate Fluid StatusLester Exconde Alfonso0% (1)
- Katie Humphrey-Freedom From PCOS-lulu - Com (2010)Document131 pagesKatie Humphrey-Freedom From PCOS-lulu - Com (2010)Patricia ReynosoNo ratings yet