Professional Documents
Culture Documents
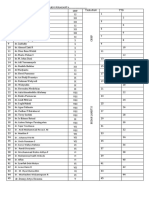
List Rik
Uploaded by
Ibnu YudistiroOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
List Rik
Uploaded by
Ibnu YudistiroCopyright:
Available Formats
Overview
Since its inception in 1849, commercial use of electricity has been one of the most potentially dangerous
commodities in our society. According to statistical data, 0.8-1% of accidental deaths are caused by an
electric injury, with approximately one quarter caused by natural lightning. Electric injury accounts for
1000 deaths each year in the United States, with a mortality rate of 3-15%.
[1, 2]
As the widespread use of electricity and injuries from it increase, all health professionals involved in burn
care must appreciate the physiologic and pathologic effects and management of electric current injury. As
either the current or its arc causes these injuries, an understanding of some fundamental laws of physics
is an essential prerequisite of proper management. This article describes the consequences of accidental
contact with commercial electric current and delineates principles involved in burn care.
For excellent patient education resources, visit eMedicineHealth's First Aid and Injuries Center. Also, see
eMedicineHealth's patient education articles Electric Shock and Thermal (Heat or Fire) Burns.
Physics of Electricity
Electricity is the flow of electrons from atom to atom.
[3, 4]
Movement of electrons is comparable to the way
water is passed along in a bucket brigade. Electrons, which comprise the current, are passed along from
atom to atom. Amperage is the term used for the rate of flow of electrons. Every time 6.242 x
10
15
electrons pass a given point in 1 second, 1 ampere of current has passed. The current is what can
kill or hurt a victim of an electric injury. One ampere is roughly equivalent to the amount of current flowing
through a lighted 100-watt light bulb.
In most materials, a number of electrons are free to move about at random until a driving force termed
voltage propels them to move in one direction. A large voltage exerts a greater force, which moves more
electrons through the wire at a given rate of time. Electric voltage of 380 volts or less is considered low
voltage and above 380 volts, high voltage. High voltage is generated at the power plant and is
transformed down to approximately 120 volts for most wall outlets in homes.
Resistance
Resistance of the human body has been likened to that of a leather bag filled with an electrolyte fluid, with
high resistance on the outside and lower inside.
[5]
Skin resistance also varies depending on moisture
content, thickness, and cleanliness. Resistance offered by the callused palm may reach 1,000,000
ohms/cm
2
, while the average resistance of dry normal skin is 5000 ohms/cm
2
. This resistance may
decrease to 1000 ohms/cm
2
if hands are wet. Skin resistance is encountered primarily in the stratum
corneum that serves as an insulator for the body. The voltage gradient in skin cannot be increased
indefinitely and breaks down at low voltages. Exposure of the skin to 50 volts for 6-7 seconds results in
blisters that have a considerably diminished resistance.
The dermis offers low resistance, as do almost all internal tissues except bone, which is a poor conductor
of electricity. Other factors that affect the flow of electrons are the nature and size of the substance
through which it passes. If the atomic structure of the material is such that the force of attraction between
its nucleus and outer electrons is small, little force is required to cause electron loss. These substances
(eg, copper, silver) in which electrons are loosely bound are termed conductors, because they readily
permit the flow of electrons. Materials such as porcelain and glass are composed of atoms that have
powerful bonds between their nuclei and the outer electrons. These materials are termed insulators
because electron flow is restricted.
Resistance is a measure of how difficult it is for electrons to pass through a material and is expressed in a
unit of measurement termed an ohm. The resistance offered to the flow of electricity by any material is
directly proportional to its length and inversely proportional to its cross-sectional area. Electricity is
transmitted by a high-voltage system, because it allows the same amount of energy to be carried at lower
current, which reduces electrical loss through leakage and heating. The relationship between current flow
(amperage), pressure (voltage), and resistance is described in Ohm's law, which states that the amount
of current flowing through a conductor is directly proportional to voltage and inversely related to
resistance.
Current (I) = Voltage (E)/Resistance (R)
Electrons set in motion by the current force (voltage) may collide with each other and generate heat. The
amount of heat developed by a conductor varies directly with its resistance. Power (watts) lost as a result
of the current's passage through a material provides a measure of the amount of heat generated and can
be determined by Joule's law.
Power (P) = Voltage (E) x Current (I)
Because E = I x R (resistance), the above equation becomes P = I(squared) R. Consequently, the heat
produced is proportional to the resistance and the square of the current. Commercial electric currents
usually are generated with a cyclic reversal of the direction of electric pressure (voltage). Pressure in the
line first pushes and then pulls electrons, resulting in alternating current. Frequency of current in hertz
(Hz) or cycles per second is the number of complete cycles of positive and negative pressure in 1
second. The usual wall outlet (120 volts) provides a current with 120 reversals of the direction of flow
occurring each second and is termed 60-cycle current. Frequency of alternating current can be increased
to a range of millions of cycles per second. In direct current, electron travel is always in the same
direction.
Alternating current
Alternating current has almost entirely superseded direct current, since it is cheaper and can be
transformed easily into any required voltage. Most machines in industry and appliances in the home use
alternating currents; therefore, workers and consumers are mainly at risk from this current. Direct current
usage is primarily restricted to the chemical and metallurgical industries, ships, streetcar systems, and
some underground train systems.
[6, 7]
Electric arc
Contact with high-voltage current may be associated with an arc or light flash.
[8]
An electric arc is formed
between two bodies of sufficiently different potential (high-voltage power source and the body, which is
grounded). The arc has an intense, pale-violet light and consists of ionized particles that are driven by the
voltage pressure between the two bodies and are present in the space between them. Temperature of the
ionized particles and immediately surrounding gases of the arc can be as high as 4000C (7232F) and
can melt bone and volatilize metal. As a general guide, arcing amounts to several centimeters for each
10,000 volts. Burns occur where portions of the arc strike the patient. The electric arc remains the cause
of most high-voltage electrical burn injuries. Because of its high frequency, the electric arc has become
the basis for many standard safety precautions.
Flash burns are caused by head from a nearby electric arc that can have temperatures of 5000C. These
hot flashes can pass over the surface of the body, usually resulting in superficial partial-thickness burns.
Flash burns have no internal electrical component.
Effects of electricity on the body
Effects of electricity on the body are determined by 7 factors: (1) type of current, (2) amount of current, (3)
pathway of current, (4) duration of contact, (5) area of contact, (6) resistance of the body, and (7)
voltage.
[9]
Low-voltage electric currents that pass through the body have well-defined physiologic effects
that are usually reversible. For a 1-second contact time, a current of 1 milliampere (mA) is the threshold of
perception, a current of 10-15 mA causes sustained muscular contraction, a current of 50-100 mA results
in respiratory paralysis and ventricular fibrillation, and a current of more than 1000 mA leads to sustained
myocardial contractions.
Humans are sensitive to very small electric currents because of their highly developed nervous system.
The tongue is the most sensitive part of the body. Using pure direct current and 60-cycle alternating
current, the first sensations are those of taste, which are detected at 45 microamperes. When subjected
to 60-cycle alternating current, the threshold of perception in the hands of men and women, which is
usually a tingling sensation, is approximately 1.1 mA. Using pure direct current applied to hands, the first
sensations are those of warmth in contrast to tingling, detected at 5.2 mA.
Skin offers greater resistance to direct current than alternating current, thus 3-4 times more direct current
is required to produce the same biologic effect elicited by alternating current. With increasing alternating
current, sensations of tingling give way to contractions of muscles. The magnitude of the muscular
contractions enhances as the current is increased. Finally, a level of alternating current is reached for
which the subject cannot release the grasp of the conductor. The maximum current a person can tolerate
when holding a conductor in one hand and still let go of the conductor using the muscles directly
stimulated by the current is termed the "let-go" current. This tetanizing effect on voluntary muscles is most
pronounced in the frequency range of 15-150 Hz.
Such strong muscular reactions may cause fractures and/or dislocations. Numerous reports of
bilateral scapular fractures and shoulder dislocations and fractures in electric accidents attest to this
occurrence. As the frequency increases above 150 Hz, the potential for this sustained contraction is
lessened. At frequencies from 0.5-1 megacycle, these high-frequency currents do not elicit sustained
contractions of the skeletal muscles. For 60-cycle alternating current, the let-go threshold for men and
women is 15.87 mA and 10.5 mA, respectively. The lower value for women may result from their
generally somewhat poorer muscular development compared to men.
Electrical accidents involving power frequency (50-60 Hz) and a relatively low voltage (150 V/cm)
occasionally can result in massive trauma to the victim. Skeletal muscle and peripheral nerve tissue are
especially susceptible to injury. Historically, Joule heating, or heating by electrical current, was viewed as
the only mechanism of tissue damage in electrical trauma. Yet in some instances, Joule heating does not
adequately describe the pattern of injury observed distant to the sites of contact with the electrical source.
These victims exhibit minimal external signs of thermal damage to the skin, while demonstrating
extensive muscle and nerve injury.
Recently, electroporation of skeletal muscle and nerve cells was suggested as an additional mechanism
of injury in electrical burns. This mechanism is different from Joule heating, even though it is influenced
by temperature. It is the enlargement of cellular-membrane molecular-scale defects that results when
electrical forces drive polar water molecules into such defects. Experimental studies have documented
that electroporation effects can mediate significant skeletal muscle necrosis without visible thermal
changes.
High-voltage accidents
The national electric code defines high-voltage exposure as greater than 600 volts. In the medical
literature, high-voltage exposure is judged as greater than 1,000 volts. In high-voltage accidents, the
victim usually does not continue to grasp the conductor. Often, he or she is thrown away from the electric
circuit, which leads to traumatic injuries (eg, fracture, brain hemorrhage). The infrequency with which
sustained muscular contractions occur with high-voltage injury apparently occurs because the circuit is
completed by arcing before the victim touches the contact. Currents that cause subjects to "freeze" to the
circuit despite their struggle to be free are frightening, painful, and hard to endure, even for a short time.
Turning off power source
Consequently, a witness of the accident must turn off the power source as soon as possible. If this is not
possible, the victim must be disengaged from the electric current. Wearing lineman's gloves, trained
electricians must separate the victim from the circuit by a specially insulated pole. Looping a polydacron
rope around the injured patient is another method of pulling him or her from the electric power source.
Ideally, the first responder should stand on a dry surface during the rescue.
Muscular contractions
Tests using gradually increasing amounts of direct current produce sensations of internal heating rather
than severe muscular contractions; however, sudden changes in the magnitude of direct current produce
powerful muscular contractions. At the instant of interruption of the direct current, the subject occasionally
falls back a considerable distance; the impact of the fall may cause a fracture. As the alternating current
strength increases above 20 mA, a sustained contraction of muscles of respiration of the chest occurs.
Normal respiration returns after the current has been turned off, provided that the duration of current flow
is less than 4 minutes. If sustained contractions last longer than this time interval, death from asphyxiation
occurs, unless the current is stopped and mouth-to-mouth ventilation on the breathless patient is started.
The pathway of current flow, involved in tetanic contractions of the muscles of respiration, is usually arm
to arm or arm to leg and does not pass through the respiratory center located in the medulla of the
brainstem. This center is injured in executions in the electric chair, leading to permanent respiratory
arrest.
Treatment at the scene
When current flow increases above 30-40 mA, ventricular fibrillation may be induced. Numerous factors
can influence the magnitude of electric current required to produce ventricular fibrillation.
[10, 11, 12, 13]
Factors
found to be of primary importance are duration of current flow and body weight. The threshold for
ventricular fibrillation is inversely proportional to the square root of the shock duration and directly
proportional to body weight.
[14]
When the heart is exposed to currents of increasing strength, its susceptibility to fibrillation first increases
and then decreases with even stronger currents. At relatively high currents (1-5 amps), the likelihood of
ventricular fibrillation is negligible with the heart in sustained contraction. If this high current is terminated
soon after electric shock, the heart reverts to normal sinus rhythm. In cardiac defibrillation, these same
high currents are applied to the chest to depolarize the entire heart.
If disconnecting the victim from the electric circuit does not restore pulses, the first responder must
start cardiopulmonary resuscitation to restore breathing and circulation. Ideally, when they arrive at the
scene of the accident, paramedics will continue this resuscitation. Field intervention should include
advanced life support treatments delivered under the direction of a physician at the hospital base station
using telemetered communication. Telemetered monitoring of these patients is recommended throughout
transport to the advanced life support hospital facility.
These life-threatening consequences of low-voltage electric burns usually occur without any lesions of the
skin at entrance and exit points of the current. An absence of local lesions indicates that the surface area
of contact (current density) is large and that the heat is insufficient to produce a thermal injury; however,
the smaller the surface area of the contact, the greater the density of the current and the more energy is
transformed into heat that can cause local burn injury.
Low-Voltage Electric Burns
Low-voltage electric burns almost exclusively involve either the hands or oral cavity.
[15]
In either injury,
hospitalization is recommended to treat the local burn injury and monitor for systemic sequelae. The most
common cause of low-voltage electric burns of the hand is contact with an extension cord where the
insulating material has worn off either from wear or misuse. Most of these patients are children aged 5
years or younger. A low-voltage burn of the hand usually consists of a small deep burn that may involve
vessels, tendons, and nerves. These burns involve a small area in the hand, yet they may be severe
enough to require amputation of a finger.
Initial treatment of hand burn wound
The hand burn wound is first cleansed with poloxamer 188 and then treated with poloxamer 188 gel
impregnated with polymyxin (10,000 U/g), nystatin (4000 U/g), and nitrofurantoin (0.3%) twice daily.
Immobilize the patient's hand in a splint and maintain it in an elevated position above his or her heart. At
48-72 hours after injury, a time in which acute edema has subsided, patients with full-thickness burns are
taken to the operating room for debridement of devitalized tissue and coverage with viable tissue.
Surgical treatment
Surgical treatment varies with the severity of the injury. If the injury involves only skin loss, coverage is
accomplished by autogenous skin grafts. If bone, tendon, or joint is exposed, pedicle flaps accomplish
coverage. This coverage prevents the development of septic necrosis of these specialized structures, a
normal consequence of conservative treatment; however, when the electric injury results in damage to
the skin, tendon, nerves, and all blood vessels, amputation of the devitalized portion of the finger is
necessary.
Oral cavity damage
Low-voltage electricity also can damage the oral cavity, leaving a permanent scar. These injuries occur
most frequently in those aged 1-2 years and generally (60%) in boys. Most of these children are injured
by sucking an extension cord socket (53.7%). Biting an electrical cord accounts for 29.9% of these burns
and sucking an electric outlet, 1.8%.
Two types of low-voltage electric burns of the lips and mouth occur. The most common type occurs when
an electric arc is formed between 2 wires of opposite polarity and passes external to the body surface via
the child's electrolyte-rich saliva. Heat generated may be greater than 1371C (2500F), resulting in
severe destruction of the mouth and contiguous tissue. Low-voltage electricity also can cause a contact
burn when current enters the mouth and passes throughout the body, exiting through a ground source
(eg, wet diaper touching a metal pipe). Contact electrical burns can cause death from ventricular
fibrillation; fortunately, this type of burn is uncommon.
A 5% incidence of cardiac and/or respiratory arrest occurs in patients with electric burns of the oral cavity.
Initially, the center of the wound resulting from an oral cavity burn is grayish-white and depressed,
surrounded by a slightly elevated margin. Histologically, the central portion of the wound exhibits protein
coagulation, fat liquefaction, and necrosis of collagen. A narrow zone of hyperemic tissue surrounds this
central area and fades into adjacent tissue.
Electric burns of the oral cavity do not disturb the arterial system beyond the margin of central necrosis,
but almost all veins are occluded or thrombosed for some distance beyond the burn. Immediately after
injury, tissue is soft to palpation and painless from sensory neural damage. Within a few hours, intense
swelling appears in the surrounding tissues. As these burned tissues become more protuberant because
of developing edema, labial competence decreases, making control of saliva difficult.
Healing of oral cavity
Edema subsides from 5-12 days after injury, when demarcation of nonviable tissue becomes apparent.
Over the next 2 weeks, nonviable tissue separates from viable tissue. As devitalized tissue sloughs,
bleeding from the labial artery may complicate its separation. Necrotic tissue soon replaces granulation
tissue, and wound repair occurs by epithelial migration, collagen synthesis, and contraction. This healing
distorts the appearance of the tissue considerably, and induration of the wound occurs for 3-5 months
before spontaneous softening takes place.
Sites of involvement
Electric burns of the oral cavity can involve the lip, tongue, mucous membranes, and underlying
bone.
[15]
The most frequent site of involvement is the upper and lower lips with the intervening
commissure. This injury to the lip may be associated with damage to the orbicularis oris muscle as well as
mucous membranes. As muscles heal, microstomia may develop, and repair of the injured mucous
membranes may result in labial, alveolar, and tongue adhesions. Obliteration of the buccal sulcus may
cause drooling. Injury to the tongue is common (26%) but usually not severe; however, adhesions can
develop, resulting in ankyloglossia, which impairs speech.
Severity of bony injury
Severity of bony injury from a low-voltage electric burn may vary considerably. Injury may be isolated to a
single tooth or involve many orofacial structures. Composite dysplasia involving both dentine and enamel
of a tooth may be evident. The injured tooth has a vital pulp, a shorter root than crown, and a wrinkled,
pitted, brownish labial surface. Abnormal growth of the orofacial structures causes dental changes, such
as crossbite, crowding, and retrusion of the bite. Severity of electric burns of the mouth can be
categorized into 3 groups: minor, moderate, and severe.
1. Minor injury involves less than one third of either the upper and lower lip without commissure
injury or less than one sixth of both lips with commissure injury.
2. Moderate injury affects more than one third of either lip without commissure injury or more than
one sixth of each lip with commissure injury. Moderate injuries are limited to skin around the lips
with minimal mucosal loss and do not involve the buccal sulcus.
3. Severe injury includes a significant loss of skin and muscle and mucosal involvement of buccal
sulcus.
Treatment of oral cavity electric burns
Cleanse an electric burn wound of the oral cavity with poloxamer 188 and then treat with a petroleum
base antibiotic ointment 4 times a day. Usually, the application of arm splints is advisable to keep the
child's hands away from his or her mouth. Administer feedings through a catheter bulb syringe to limit
trauma to the injured area.
Tetanus immunoprophylaxis is mandatory for patients with a tetanus-prone wound.
[16]
Systemic antibiotic
therapy has no apparent therapeutic benefit. Delayed hemorrhage from the labial artery is noted in as
many as 24% of patients. Bleeding can occur at any time from the day of injury to 221 days later. In most
cases, bleeding can be controlled easily with manual pressure; however, ligation of the bleeding vessel is
occasionally required. When these patients are discharged from the hospital, instruct their parents on how
to manage delayed bleeding by direct application of pressure.
Definitive treatment of electric burns
Definitive treatment of electric burns of the lips and mouth remains controversial.
[15]
Four different
treatment plans have been proposed to either prevent or correct the deformity. Immediate excision within
12 hours after injury has been recommended to shorten the period of wound repair and to permit
restoration with minimal reconstructive procedures. Delayed primary reconstruction, 4-7 days after injury
when the extent of tissue necrosis is known, has also been suggested. Delayed reconstruction following
complete healing of the wound is another approach. Finally, immediate postburn splinting to avoid
surgical reconstruction has also been advocated.
Consensus on fundamental principles
Definitive care of electric burns of the oral cavity remains controversial, yet consensus has been reached
on several fundamental principles. Without treatment, the injury heals with an almost invisible scar in a
considerable number of patients (20%). Most surgeons also agree that delineating the extent of damage
soon after injury is difficult and that early excision may sacrifice normal tissue. Finally, immediate
prosthetic splinting reduces the need to reconstruct the oral cavity after the injury.
On the basis of these principles, immediate treatment of electric burns of the oral cavity should include
splinting of the mouth after acute edema resolves, often 5-12 days after injury. Splinting should continue
until the scar softens and loses its contractile potential, which usually takes 6-12 months. Surgical
revision should then be performed to correct residual deformity.
Adequate function and aesthetic appearance
Prosthetic treatment of electric burns of the oral cavity attempts to provide physical resistance to
contraction of the injured tissue. Maintain symmetric width of the oral stoma to attain adequate functional
and aesthetic appearance of the injured mouth. Position each commissure laterally equidistant to the
midline of the lips, and maintain the orbicularis oris muscle at a 2-point fixation. This prosthetic treatment
can be accomplished either intraorally or extraorally, depending on the patient's dentition and ability to
cooperate. Because these patients are often aged only 1-2 years, parents must participate and cooperate
in the treatment plan.
Perform intraoral commissure splinting using a fixed, semifixed, or removable appliance. Intraoral
prostheses have posts at the oral commissures that apply static traction to the injured healing tissue.
Bilateral posts oppose the sphincterlike action of the orbicularis oris muscle as well as the forces of
wound contraction. Unfortunately, many children with electric burns of the oral cavity are not referred to
regional burn centers soon after their injury and do not benefit from these prostheses. Without these
appliances, the burn wound is allowed to heal by contraction, and the contracting scar often causes
severe deformities. In such cases, final reconstruction is best achieved after the scars are allowed to
soften, usually 6-12 months after the injury. Reconstructive procedures undertaken when the scars are
hypertrophic tend to produce additional hypertrophic scarring.
Two types of deformity
Two principal types of deformity that result from oral cavity electric burns are those that are limited to the
corner of the mouth and those that involve loss of a section of lower lip. When the corner of the lip is
destroyed, parts of the upper and lower lips adhere and interfere with full opening of the mouth. The
corner of the mouth can be reconstructed by separating the adherent portions of the upper and lower lips
and excising the scar. In most cases, skin loss is negligible and only mucous membrane is required to
establish the normal outline of the mouth.
Restoring the mucous membrane
One of two procedures can be used to restore the mucous membrane, depending on the amount of
mucosa missing at the vermilion border. If the raw areas of the corners of the upper and lower lips are
shorter than 1.5 cm, use an advancing flap from adjacent mucous membrane. More extensive loss
requires transfer of mucous membrane flaps from the cheek.
Tongue flaps also have been used to restore the commissure defect. A laterally or anteriorly based
tongue flap taken from the ventral surface of the tongue is preferable to avoid placing gustatory papillae
on the lips. However, tongue flaps have several disadvantages. Tongue tissue often is too bulky and
retains its papillary appearance. Furthermore, the junction at the vermilion border may be indistinct, and
a color disparity may exist between the lips and flap in patients with dark skin tones. If the median
section of the lip mucous membrane is lost, the lip retracts and adheres to the alveolar process.
Adhesions of the lower lip must be divided. Either a skin graft or a local mucous membrane flap covers
the resulting defect.
V-Y advancement procedure: Because skin grafts tend to contract significantly, use normal mucous
membrane from the bordering regions, if possible. A V-Y advancement procedure can be used to
advance the mucous membrane to replace the deficiency. In this procedure, first excise the scar to
allow the lip to assume its normal position. Then make an incision along the inner surface of the lip
close to the alveolar processes. The buccal incision is extended toward the molar region and then
vertically over the mucous membrane of the cheek. The resulting 2 rectangular-shaped flaps are then
sutured together to form a V-Y advancement flap. The raw area on the alveolar process is covered with
a split-thickness skin graft that enhances the depth of the buccal sulcus.
Other procedures: Various procedures have been described to repair median losses of muscle and skin
of the lower lip.
o A triangular wedge excision or the Hagedorn rectangular flap technique can repair small-to-moderate
losses.
o A step bilateral rectangular flap advancement is another approach that utilizes the line of the chin
crease to mask the scar.
o The Stein procedure, use of an Abb flap from the central portion of the upper lip, or modified Stein
operation that rotates flaps from each side of the philtrum to restore contour to the lower lip are not
recommended because they result in noticeable deformity of the upper lip.
Postpone surgery on the lower lip until the patient is aged at least 9 years, by which time permanent
lower incisors have erupted and alveolar bone growth is not significantly influenced by the tightness of the
lower lip. Surgery performed earlier results in a tight lower lip and either overbite occlusion or
retrognathism from pressure on the growing mandible or lower anterior dentition. The earliest indication of
these impending dental problems is forward protrusion of the upper lip beyond the reconstructed lower lip.
Later, crowding or lingual deviation of lower deciduous teeth becomes evident. If these problems develop,
orthodontic appliances are necessary to hold teeth in proper relationship.
Prevention
Prevention remains the best treatment of low-voltage electric burns. Educate parents regarding potential
safety hazards and the need for close supervision of their children; this is important to decrease the
incidence of childhood electric injuries. Use the following guidelines:
1. Use extension cords on a limited and temporary basis only.
2. Replace damaged electrical cords.
3. Place plastic nonconductive dummy plugs in unused outlets.
4. Do not use electric appliances near water, and keep them out of children's reach.
5. Supervise children closely, especially when electric toys are in use. Such toys should bear the
Underwriters' Laboratories label of safety, and damaged toys should be repaired or discarded.
High-Voltage Electric Burns
Burns due to contact with high-voltage electric circuits conform to 2 general types.
Burns from an electric arc
In burns from an electric arc, the current courses external to the body from the contact point to the
ground.
[8]
Circumscribed burns occur where the portions of the arc contact the patient. These contact
points may be multiple, single, or diffuse and vary in their depths. The most common contact points for
the current are the hands and skull, while the most common ground areas are the heels. Entry points on
the flexor surfaces often produce "kissing" entry lesions, resulting from severe tetanic muscle contractions
and causing extensive tissue damage. The most common of these lesions is the circumscribed deep
wound on the volar surface of the forearm in association with contact wounds of the palm. A flame may
complicate this burn injury if the flashes of an arc ignite the victim's clothing.
Burns from an electric current
The other burn injury is from an electric current that passes between the power source and the anatomic
point of contact (entrance wound), and between the patient (exit wound) and the grounding mechanism,
causing hidden destruction of deeper tissues. Such electrically conductive burns are simply thermal
injuries occurring when the electric energy is converted to thermal energy. The extent of the electric burn
is related to the magnitude, frequency, and duration of the current flow and the volume and resistance of
the tissue.
Resistance
Resistance of living tissue changes as the current flows. Skin represents an initial barrier to flow of current
and serves as insulation to the deeper tissues. Once an electric current contacts skin, the amperage rises
slowly, followed by an abrupt and rapid climb. This change in flow coincides with a progressive decline in
skin resistance. Once this skin resistance breaks down, current enters the underlying tissue whose
internal tissue resistance, with the exception of bone, is negligible to current flow. Within seconds, electric
current in tissue peaks and then falls precipitously to zero. Current ceases to flow when the heat-
producing tissue carbonization (eschar) volatilizes tissue fluid. Termination of current flow is signaled by
the appearance of an arc or flash.
Current pathways
Low-voltage current generally follows the path of least resistance (ie, nerves, blood vessels), yet high-
voltage current takes a direct path between entrance and ground. The volume of soft tissue through
which current flows behaves as a single uniform conductor, thus is a more important determinant of tissue
injury than the internal resistance of the individual tissues. Current is concentrated at its entrance to the
body, then diverges centrally, and finally converges before exiting. Consequently, the most severe
damage to the tissue occurs at the sites of contact, which are commonly referred to as the entrance and
exit wounds.
Entry and exit wounds
High-voltage electric entry wounds are charred, centrally depressed, and leathery in appearance, while
exit wounds are more likely to "explode" as the charge exits. High-voltage electrical burns often leave a
black metallic coating on the skin that is mistaken for eschar, from vaporization of the metal contacts and
electroplating of the conductive skin surface. Cleansing of the coating usually reveals only superficial skin
injury. Electric current chooses the shortest path between the contact points and involves the vital
structures in its pathway. Fatalities are high (nearly 60%) in hand-to-hand current passages and are
considerably lower (20%) in hand-to-foot current passages. Severity of damage to the tissue is greatest
around the contact sites.
Consequently, anatomic locations of the contact sites are critical determinants of injury. Most of this
underlying tissue damage, especially muscle, occurs at the time of initial insult and does not appear to be
progressive. Microscopic studies of electric burns demonstrate that this initial destruction of tissues is not
uniform. Areas of total thermal destruction are mixed with apparently viable tissue. Between the entrance
and exit points of the electric current, widespread anatomic damage and destruction may be seen. An
electric current can injure almost every organ system.
Complications
Sequelae peculiar to this type of injury are important determinants in the choice of therapy. Various
complications related to the damage to the various organ systems are now clearly identifiable.
Characteristic entry and exit wounds in extremities usually signal local destruction of deeper tissues, the
magnitude of which often cannot be predicted.
Bone has a high resistance, thus readily transforms current to heat production, which may result in
periosteal necrosis or even melting of the calcium phosphate matrix.
This injured underlying tissue has several consequences.
Necrosis of the entire limb is the most serious complication, necessitating amputation usually within 2-3
days after injury.
More commonly, the extent of underlying tissue injury involves a portion of the superficial and deep
muscles of one or more compartments. Vessels within these electrically injured tissues exhibit
increased vascular permeability.
[17]
This permeability change allows extravasation of fluids into the
wounds, resulting in a reduction in intravascular volume that must be corrected by an intravenous (IV)
infusion of Ringer lactate solution without glucose.
Treatment
The quantity of fluid sequestered in the injured tissue usually cannot be estimated using skin surface
measurement, because the magnitude of damage to the underlying tissue often is grossly
underestimated. Consequently, titrate the quantity of fluid administration to maintain an adequate urinary
output.
In contrast to flame injury, completion of fluid resuscitation can be predicted by the patient's hematocrit
and plasma volume. When extracellular fluid is restored, the hematocrit and plasma volume returns to
normal, if significant hemolysis has not occurred.
In acute electric injuries in the adult with underlying devitalized tissue, administer Ringer lactate solution
without glucose at a rate sufficient to maintain a urinary output of 50-100 mL/h.
In the presence of hemochromogens in the urine, the rate of fluid infused must be sufficient to maintain a
minimum urinary output of 100 mL/h. This rate and volume of fluid administration is continued until the
urine is free of pigment. Alkalization of the urine by adding sodium bicarbonate to the IV fluid increases
the solubility and clearance rate of myoglobin in the urine.
Transfusions are unnecessary during the first 24 hours unless multiple escharotomies and/or
fasciotomies result in significant blood loss. An almost immediate loss of intravascular fluid into an
electrically burned extremity results in considerable swelling of the muscle lying within a relatively inelastic
fascial compartment.
[18]
Such intense swelling of the injured muscle may cause noticeable changes in the
circumference of the extremity. More frequently, fascial investments may limit the swelling to such a
degree that minimal external enlargement of the limb occurs.
Postinjury physiologic events
Within a few hours after injury, rising interstitial pressure of the compartment exceeds the capillary
perfusion pressure, resulting in muscle ischemia. Consequences of this reduced perfusion are a further
increase in capillary permeability and extravasation of intravascular fluid, enhancing the interstitial
pressure of the compartment. After 6-8 hours of ischemia, muscle damage is irreversible. This vicious
cycle must be interrupted by fasciotomies, which limit ischemic injury to the muscle.
Muscle necrosis within a compartment has potentially severe systemic sequelae. It enhances local
vascular permeability with extravasation of intravascular fluids into the injured site with resultant
hypovolemia. Absorbed pigment from the damaged muscle cells and, to a lesser amount, hemoglobin
from injured red blood cells are released into the circulation soon after burn injury and expose the kidney
to significant pigment loads. This absorption of pigments into the intravascular space may lead to acute
renal failure. The mechanism of acute myoglobinuric renal failure is obstruction of the collecting system in
association with renal cortical ischemia.
Various modalities have been measured to elucidate the extent of muscle damage. The presence of
myoglobin is always associated with underlying devitalized muscle, yet not all muscle damage is
associated with myoglobinuria. Moreover, the presence of myoglobinuria does not identify either the
extent or location of damaged or dead muscle.
Laboratory studies
Laboratory studies, such as elevation of serum enzymes, serum glutamic-oxaloacetic transaminase, or
glutamic-pyruvic transaminase, are nonspecific, and levels are often elevated with only a cutaneous burn.
Numerous procedures have been cited as valuable aids in the diagnosis of the extent and location of
devitalized muscle. Escharotomies and fasciotomies are useful methods to identify and explore areas
suspicious of containing devitalized tissue. These exploratory incisions permit assessment of the extent of
muscle injury by visual and microscopic surveillance.
Microscopy as a guide to primary excision is the most accurate diagnostic procedure for muscle viability.
In this method, frozen section histology is used to determine muscle damage. Because muscle cross
striations may be preserved in dead or dying muscle, morphology of the muscle cell nuclei is the best
indicator of viability. Muscle containing clumped nuclear chromatin or poor staining with hematoxylin
indicates myonecrosis and should be excised.
Diagnostic tests
Early exploration of the burn wound remains the criterion standard for determining the severity of injury. If
no detectable viability of an electrically injured extremity is observed, amputation is mandatory because it
dramatically reduces life-threatening myoglobinuria.
MRI
MRI can be used to detect edema of the torso and extremities if the patient is medically stable enough
to tolerate an imaging procedure.
[19]
Tissue edema is a manifestation of cell membrane damage that
begins to accumulate minutes after electric injury from increased vascular permeability and
extravasation of intracellular contents.
The presence of edema on MRI can direct attention to areas with substantial muscle cell damage.
These edematous areas are at risk forcompartment syndrome and compression neuropathies, and
compartment pressures should be measured.
Compartment pressures exceeding 30 mm Hg compromise fluid and gas exchange between the blood
and tissue and necessitate fasciotomy. The only reliable indicator of compartment pressures is a direct
intramuscular pressure measurement. Digital pressure manometers are available for larger
compartments. For smaller compartments, such as the hand or foot, manometers may cause infection
of the perimuscular fluid, resulting in iatrogenic compartment syndrome. Absence of edema on MRI
indicates either that the muscle is not injured or that severe heat exposure caused intravascular
thrombosis with loss of muscle perfusion.
Nuclear medicine studies
No consistent correlation exists between MRI data and tissue survival or clinical outcome; therefore,
nuclear medicine studies are a useful adjunct to MRI.
[20, 21]
Technetium Tc 99m stannous pyrophosphate
(99m Tc-PYP) muscle scan is a sensitive and reliable diagnostic tool to define the extent and location of
muscle injury. This test can be performed in most hospitals with a nuclear medicine department. An
isotope is infused intravenously, and the scan is performed 2 hours later. Several characteristic
scintigraphic imaging patterns indicate muscle damage. An increased cellular uptake of 99m Tc-PYP
(hot spot) identifies an area of muscle damage consisting of 20-80% viable muscle, which should be
followed clinically.
Conversely, areas with no uptake of this radioactive material (cold spot) are devoid of blood supply and
obviously necrotic. Variations of this can occur, with a central cold spot surrounded by a perfused but
injured area of muscle. Uneven distribution of muscle necrosis characteristic of high-voltage electric
injuries is confirmed by this technique. This early identification of injured muscle by muscle scan is
helpful in planning the operative approach and predicting the approximate level of debridement and/or
amputation required. The short half-life (6 h) of 99m Tc-PYP allows this study to be repeated in 24
hours if extension of the injury is possible.
The major drawback to this technique is that the scan is excessively sensitive and may occasionally
incorrectly identify areas of muscle injury. These false-positive tests appear related to the developing
edema that occurs in the first 24 hours.
A newer isotope, technetium Tc 99m methoxy-isobutyl-isonitrile, shows decreased uptake in electrically
injured tissues and better sensitivity in localization of muscle injury.
Newer strategies to detect muscle injury include measurement of tissue electrical impedance. Electrical
resistance of electrically injured muscle decreases in proportion to the amount of cell membrane lysis.
Neurologic Complications
Neurologic complications are the most common complications of electric injury.
[22, 23, 24]
Both acute and
delayed central and peripheral nervous system sequelae have been described. Approximately 70% of
patients were rendered unconscious in high-voltage electric injures, including all those in whom the
current passed through the head and several patients in whom the current had not traversed the head. All
unconscious patients, except those fatally injured, recovered within a few hours, most in 5-10 minutes.
Transient agitation and confusion were seen in a few patients. With regard to their social rehabilitation, a
follow-up study detected some mild changes in personality and mental capacity. Less-frequent
complications of intracerebral injury include hemiplegia, aphasia, striatal symptoms, epilepsy, headaches,
and memory and concentration deficits.
Peripheral nerve injury
Peripheral nerve injury may be involved by direct injury at the site of entrance or exit or in polyneuritic
syndrome involving nerves far removed from the points of contact.
[23]
Typical symptoms include numbness
(anesthesia) and "pins and needles" sensation (paresthesia). Loss of function in a peripheral nerve is
usually transient, and complete recovery may be expected if the nerve is not involved in local tissue
injury; however, permanent damage to peripheral nerves in electric injuries is limited to the area of local
tissue contact.
Median, ulnar, and radial nerves have the highest incidence of persistent dysfunction. Heat released by
current flow causes total or partial loss of nerve function. In deep burns involving nerve trunks, prognosis
for recovery is unfavorable. In these severe injuries, usually total loss of nerve function occurs. Whenever
a nerve deficit is discovered, perform surgical exploration to exclude contributing factors, such as the
compartmental syndrome. A late cause of reversible peripheral nerve injury may be secondary to
heterotopic bone formation, which most often occurs at the elbow, resulting in ulnar nerve dysfunction.
Acute and delayed spinal cord injuries have been described distal to the site of electric contact. Such
injuries have occurred following contact with electric currents whose voltages varied from 75-75,000 volts.
Characteristically, no neurologic deficit was noted immediately after the accident. Symptoms and signs
did not develop until days to 2 years following injury, when total quadriplegia or hemiplegia may occur.
Signs are variable and may include ascending paralysis,amyotrophic lateral sclerosis, or transverse
myelitis. Motor deficits occur more frequently than sensory loss. This syndrome was first termed spinal
atrophic paralysis. In patients with electric spinal cord injuries, neurologic recovery is unusual.
Experimental studies demonstrated that electric injury may cause perivascular hemorrhage,
demyelinization, reactive gliosis, and neuronal death in the spinal cord in animals. Such neuronal damage
was produced in animals with minimal damage to the skin or structures outside the spinal cord. Results of
experimental studies parallel the clinical findings of extensive neurologic injury to patients with mild
cutaneous injury. Delayed appearance of the spinal cord injury has not been explained experimentally. It
may represent direct injury either to the neurons or the vascular supply of the spinal cord.
Cardiovascular and Pulmonary Complications
High-voltage electric current can produce a wide variety of different cardiac injuries and usually consists
of rhythm and conduction disturbances.
[25, 26, 27]
Cardiac arrest either from asystole or ventricular fibrillation
often presents in electrical injuries. The most common electrocardiographic abnormalities following high-
voltage electric injuries are sinus tachycardia and nonspecific ST-T segment alterations, which frequently
persist for several weeks following injury. Atrial fibrillation also has been reported following contact with
high-voltage electric wires. In most of these instances, rhythm reversed spontaneously or after
administration of either quinidine or digitalis.
Disturbances in the heart conduction system have rarely been reported in high-voltage electric accidents.
In one patient, a partial intraventricular conduction block persisted for 10 days. A nodal rhythm was
observed in another patient for a 24-hour period, after which it disappeared. Although these findings imply
myocardial or conduction system injury, the necessary extensive surgical procedures performed during
treatment of the burn injury were not associated with detectable cardiac complications.
Myocardial infarction, substantiated by cardiac enzyme studies, is an uncommon complication of high-
voltage electric injuries. Electric burns of the anterior chest may cause direct thermal injury to the
myocardium with perforation that must be closed during cardiopulmonary bypass. Using telemetered
monitoring, paramedics should be the first to detect evidence of cardiac injury at the scene of injury. An
electrocardiogram is usually repeated on arrival in the emergency department. Institute cardiac
monitoring when the patient is hospitalized.
Cardiac enzymes
Cardiac isoenzymes have questionable diagnostic value in electric injuries. A high creatine
phosphokinase (CPK) MM fraction is consistent with skeletal muscle damage, yet a significantly elevated
CPK-MB fraction may not indicate cardiac damage.
[28]
Recent studies show that skeletal muscle cells
contain up to 20-25% CPK-MB fraction, suggesting that electrical damage to skeletal muscle rather than
cardiac muscle may account for an elevated CPK-MB fraction. Ignoring this finding may lead to an
incorrect diagnosis of myocardial infarction.
In the presence of cardiac injury, lactic dehydrogenase (LDH) fractionation reveals that LDH-1 rises more
than LDH-2, and the LDH-1/LDH-2 ratio exceeds unity. Because LDH-2 exceeds LDH-1 in normal serum,
this reversed or "flipped" LDH pattern is present in most acute myocardial infarctions.
Vascular damage
Vascular lesions dominate the clinical presentation of many electric burns.
[29]
When current passes through
large vessels at its entrance or exit points, it may cause a pronounced inflammatory reaction as well as
small areas of vascular wall necrosis. The latter may lead to immediate or delayed rupture of the vessel.
Current flowing through larger vessels that are located beyond the entrance and exit points of the current
may damage the vessel, precipitating the development of mural thrombi, yet vessels usually remain
patent. Flow through these larger vessels dissipates heat and limits damage to their walls. In smaller
vessels, this heat injury results in vessel thrombosis.
Small nutrient vessels, like those in muscle, are very susceptible to thrombosis when exposed to high
temperature. Pathologic examination of the electrically injured tissue confirms the presence of small
arterial and microarterial thrombosis. Because arteriography is capable of identifying only arterial lesions
in large and medium vessels, it has limited clinical usefulness in acute electric injuries. This loss of blood
supply to muscle may be progressive, occurring over the first 1-3 months after injury. Such changes may
account for the progressive muscle fibrosis and flexion contractures that occur frequently after this injury.
Acute pulmonary complications
Acute pulmonary complications are limited to pleural damage resulting in effusions and lobular
pneumonitis directly adjacent to the entrance and exit wounds and are usually evident by the end of the
first week.
[30]
A closed tube thoracostomy may be necessary to remove a pleural effusion and typically
prevents reaccumulation. Pulmonary infection may result from systemic infection or from inhalation injury.
Abdominal, Bone, Joint, Eye, and Systemic Complications
Abdominal complications
A wide spectrum of abdominal visceral complications has been reported following high-voltage electrical
injury.
[31, 32, 33, 34]
These injuries result either from direct injuries to intra-abdominal structures from the
contact points over the abdomen or are a result of current passing through the abdominal viscera from
more distant entrance and exit wounds. In treating high-voltage electric accidents, anticipate the entire
spectrum of anatomic and pathologic alterations to the abdominal viscera.
Nausea and vomiting are the most common abdominal symptoms, seen in up to 25% of patients.
Numerous different GI complications have been reported following high-voltage electric injury.
Nonspecific adynamic ileus occurs in approximately 25% of patients. Usually a transient finding,
adynamic ileus may be a manifestation of a more serious underlying GI injury.
Stress ulceration (Curling ulcer) is probably one of the most serious complications (3%). With this
potential for stress ulceration, treatment of patients with high-voltage electric injuries with antacids and
histamine H2-receptor antagonists is prudent.
When either the entrance or exit wound is the abdominal wall, localized destruction of the abdominal wall
occurs with direct injuries to the underlying intra-abdominal structures, including small and large
intestines, bladder, or liver. High-voltage electric burns whose entrance and exit points do not contact the
abdominal wall may also result in injury to the intra-abdominal contents (eg, gallbladder, intestine). In the
latter case, the initial symptoms of underlying injury to the viscera may be slight and not appreciated until
2-3 weeks after injury.
Pancreatic injury is a rare complication of high-voltage electric current. Hyperamylasemia with prolonged
ileus has been encountered in several patients who responded favorably to medical management. A
pseudodiabetic state occurred toward the end of the first week after the accident in other patients. Marked
hyperglycemia and mild ketosis were treated with small amounts of insulin. After recovery, glucose
tolerance curves of these patients returned to normal. After abdominal surgery in patients with high-
voltage electric burns, the complication rate was alarming. Repair of bowel anastomoses is associated
with a high incidence of leakage, which has been attributed to the surgeon's inability to accurately
determine the extent and depth of damage to the intestine. Therefore, lesions of the small intestine
should be resected with wide margins.
Treatment of electric injuries of colon
Electric injuries of the colon seem best treated by wide resection and colostomy or exteriorization of the
injured segment.
[35]
When multiple superficial lesions are scattered over the bowel, a "second-look"
operation at 2-5 days may be advisable in instances where areas of injury with questionable viability are
not resected. Distribution of intravenously injected fluorescein dye may prove helpful in demarcating
devascularized intestine. Early staining of the injured bowel with fluorescein is evidence of tissue viability.
At times, active bleeding from the cut ends of the transected bowel may be present, indicating tissue
viability. Wound disruption following emergency abdominal surgery in burn patients is frequently noted.
On limited occasions when stainless steel wire was not used for fascial closure, wound complications
frequently have been encountered. On the basis of this experience, close abdominal wounds in burn
patients with stainless steel sutures, usually retention sutures, placed through all muscle and fascial
layers of the abdominal wall.
Long-term follow-up care of patients who had recovered from a high-voltage electric injury revealed a
high incidence of GI complications. Approximately three fourths of patients had recurrent dysfunction of
the GI tract within 12-18 months after injury. No discernible cause for the abdominal complaints was
found in most patients, while cholelithiasis was detected in approximately 8%.
Bone lesions
In high-voltage accidents in which the current enters near bony tissue, lesions of the bone are
common.
[36]
High resistance of bone to the passage of electric current results in periosteal necrosis and
melting of the calcium phosphate matrix. The resulting destruction is often difficult to diagnose at the time
of initial debridement. Stripping of the devitalized periosteum and obtaining early soft tissue coverage
limits the magnitude of bony injury.
Despite this aggressive therapy, small sites of bony sequestrum often form sinus tracts 1-8 months after
closure. After excision of the sequestra, wound closure is usually accomplished without infection. In
accidents where high-voltage current passed through the head, the injury was mainly confined to the
scalp and skull. Current was usually dissipated in the skin, galea, and outer table, sparing the brain from
direct cerebral injury. This explained the surprising fact that severe cerebral complications were rare in
such accidents.
With the progress of microvascular free-tissue transplantation in recent decades, free flaps have come
into use in the reconstruction of high-voltage electrical burn injuries. Free-flap coverage is mainly used for
upper limb reconstruction, primarily for purposes of forearm reconstruction.
Scalp burns
Scalp burns can be classified according to the depth of burn into the following 4 specific groups: (1) burns
without direct bone involvement; (2) burns with direct bone involvement (outer table only or both tables);
(3) burns involving dura mater; and (4) burns involving the brain.
[37]
Depth of the burn injury has
considerable influence on treatment. When the injury is confined to full-thickness destruction of the scalp,
closure is accomplished with split-thickness skin grafts. If the burn injury is localized to a small region,
local flaps can be employed to resurface the defect. When bone death is involved in burn injury, treating
these patients becomes considerably more difficult.
Treatment of scalp burns
Problems center around achieving complete skin cover without the development of infection. Two
treatments are available for patients with burns of the scalp that involve the underlying bones. One
technique is to remove all dead bone, closing the defect by grafting; the other is to close the wound with a
skin flap without excision of devitalized bone. There are several different approaches to remove dead
bone. The most conservative one is to leave the bone exposed for an undetermined time, usually weeks
or months. Eventually, nonviable bone sloughs or is removed as a sequestrum; the defect is then closed
either with a skin graft or flap, depending on the availability of local tissue. Holes can be drilled into the
skull to permit ingrowth of granulation tissue from a viable diploic cavity to accelerate sequestration.
Areas of bone between the holes tend to sequestrate slowly and delay stable skin cover.
Another technique is to remove the outer table completely. Wounds in these patients reportedly heal
twice as fast as those treated by the multiple burr hole technique. More recently, surgeons have believed
that these approaches to burn injuries of the scalp that involved bone removal were not warranted. They
demonstrated that the prolonged course of debridement, sequestrectomy, and subsequent reconstruction
can be bypassed effectively with a single, early definitive procedure that included primary excision of the
skin eschar followed by rotational flap coverage without removal of devitalized bone. The electrically
injured skull acted as an in situ bone graft. In the absence of a local flap, a free flap may prove an
important alternative method of wound coverage.
Currently, coverage of devitalized bone by a well-vascularized flap allows regeneration of bone. Several
clinical reports have documented the successful centripetal regrowth of bone following coverage with a
vascularized flap.
Joint injuries
Because the victim does not continue to grasp the conductor in high-voltage electric injuries, fractures
usually result from the patient falling from the electric current.
[36]
Powerful tetanic skeletal muscle
contractions have caused long bone fractures, cervical spinal fractures, and joint dislocations. Anterior
and posterior shoulder dislocations from tetanic spasm of the rotator cuff muscles have occurred during
electric injuries.
When overlying skin involvement is associated with the fracture, skeletal traction is preferred over internal
fixation to reduce the chance of bone infection. Heterotopic ossification of soft tissues is a common
consequence of commercial electric injury. This process occurs at joints, other synovial surfaces such as
bursa and nerve sheaths, and the end of amputation stumps. This ossification results from tissue injury,
constant shear forces between bone and surrounding tissues, and a systemic inflammatory response.
Upper and lower extremity burns
The loss of an arm or leg is one of the most devastating consequences of a burn injury. Reported rates of
amputation as a result of high-voltage electric burn injury range from 32-60%. Deep thermal burns
complicated by extensive soft tissue necrosis or invasive infection may produce nonsalvageable
extremities. Advances in reconstructive surgery have resulted in decreased amputation rates after
electrical burn injuries. Traditionally, amputation after burn trauma has been related primarily to high-
voltage electric injury. These amputations may be isolated to a major extremity or to digits, hands, or feet.
Sauerbier et al demonstrated that burn and high-voltage injuries are distinct entities that require custom-
tailored reconstructive solutions for limb salvage. Even if the surgeon's flap fails during the first 6 weeks,
remember that this type of coverage is the only alternative to amputation in select cases. As the versatility
and variability of free flaps have significantly increased during recent years, so have indications for free
tissue transplantation in burn reconstruction expanded. The progress of free tissue microvascular
transplantation in recent decades has led to the increasing use of free flaps for reconstruction in patients
with electrical burns. The flaps have reached a high level of surgical sophistication to include fascial flaps,
pre-expanded flaps, and composite tissue flaps, as well as multiple flap transplantations in the same
patient.
Eye injuries
Electric injuries to the eye occur chiefly when current enters the body through the patient's head.
[38]
The
lenses of both eyes can be equally affected, or one can be more affected than the other. A wide range of
voltages, from 220-50,000 volts, results in a cataract in 6% of electric injuries. Time of onset of the
symptoms ranges from 3 weeks to 2 years. Lesions of the cornea, fundus, and optic nerve, without
alteration of the lens, have also been reported.
Systemic complications
Severe potassium deficiency is an unexplained manifestation of high-voltage electric injury. This problem
was identified in patients with normal renal function who were eating well 2-4 weeks after injury. In such
patients, respiratory arrest and severe cardiac arrhythmias may lead to the diagnosis. Systemic
manifestations of electric current injury are not apparent in high-voltage electric burns that result only from
intense heat of the electric arc. Surface burns of varying size and depth result from this injury without
hidden destruction of deeper tissues. Occasionally, the arc ignites the patient's clothing, resulting in a
flame burn that further damages the skin.
Psychosocial complications
The psychosocial complications following electrical burns have been evaluated through a cross-sectional
survey of electrical burn patients using 3 outcome tools: the Burn Specific Health Scale, the Coping with
Burns Questionnaire, and the Pain Patient Profile. Patients surveyed more than 5 years from injury
showed improvement in their physical health. Optimism was the most commonly used coping strategy for
these patients. However, significant levels of emotional distress were encountered in all patients; anxiety
was more common in patients with high-voltage electrical injuries. Recognizing that electrical burn
patients may have a limited ability to return to work and an overall poor quality of life is important.
Emotional distress is the dominant feature that influences long-term outcome in these patients.
Pregnant patients
Electrical or lightning injury carries the additional risk of complications to a pregnant mother or her
fetus.
[39]
Because of the small number of cases reported, the actual risks are unknown. Reports of fetal
mortality vary widely, ranging from as high as 73% to as low as 15% after electrical injury and about 50%
after a lightning strike. Whether fetal mortality is due to primary electrical injury of the fetus or due to the
injury to the pregnant mother is not clear.
Safety Laws and Accident Prevention
Deaths from electric shock accidents
Almost 1200 people died from electric shock accidents associated with consumer products during a 3-
year period (1975-1977). Of these, electrocution by outdoor television and CB radio base station
antennas accounted for 355 deaths. Most electrocutions could have been prevented if consumers
understood the dangers and followed safety precautions. Most deaths linked with outdoor antennas
occurred when the device contacted an overhead power line while the victim was putting up or taking
down the antenna.
Consumer alerts
In an attempt to alert consumers to the danger of electrocution, the Consumer Product Safety
Commission (CPSC) now requires manufacturers and importers to include warning labels and installation
instructions with all outdoor TV and CB base station antennas and masts or other devices intended to
support these antennas. This regulation applies to all such products manufactured, imported, packaged,
or sold by the manufacturer or importer after September 26, 1978.
Similar incidents occur with ladders, especially metal ladders, when the user fails to observe a nearby
power line. Many ladder manufacturers are now labeling their products on a voluntary basis to alert
consumers to the possible electrocution hazard. In 1988, the CPSC conducted a human factor analysis of
reports of in-depth investigations to assess the electrocution hazard associated with the use of aluminum
ladders near power lines. This analysis was based on relating relevant victim characteristics, product
characteristics, and environmental factors that may have contributed to the electric injuries. Analysis
revealed that while some of the victims were unaware of the electrocution hazard, a number of victims
were aware of the electrocution hazard and either lost control of the ladders near power lines or
misjudged the clearance distance between the power lines and the ladders.
Further study of the in-depth investigations revealed that the human visual system has limited ability to
estimate the clearance necessary to avoid contacting power lines; therefore, carrying the ladder in its
extended position and misjudging the significant instability of the ladder resulted in victims inadvertently
contacting the high wires or losing control of the ladder. Unusually severe consequences from such
accidents led NIOSH (National Institute for Occupational Safety and Health) to recommend greater safety
precautions. NIOSH required employers and workers to comply with Occupational Safety and Health
Association (OSHA) regulations prohibiting the use of portable metal ladders for electrical work or in
locations where they may contact electrical conductors (Code of Federal Regulation, 1988).
NIOSH also suggested that arrangements be made with the power company to de-energize the lines or to
cover the lines with insulating line hoses or blankets. Furthermore, employers were encouraged to
provide workers with training in emergency medical procedures, such as cardiopulmonary resuscitation,
because fatalities may be prevented by prompt medical care. CPSC recommended changing the
American National Standards Institute's (ANSI) warning sticker that now appears on ladders to a more
descriptive sticker, including the type of hazard, the result of ignoring the warning, and how to avoid the
hazard. CPSC also suggested that approaches aimed at reducing this type of electrocution hazard that
do not rely solely upon people taking some action may be more effective.
Preventing electric burns
One solution is to place a fiberglass link in all new ladders, thereby providing isolation so that electricity
does not have a path to the ground. This type of ladder is already in use by some power-line companies.
An alternative solution is to cover the top half sliding section of extension ladders with an insulating,
nonconducting material such as heavy Teflon. This suggestion has been used successfully in the
installation of roof top antennae.
In 1989, the Commonwealth of Virginia created the Overhead High Voltage Line Safety Act to promote
the safety and protection of anyone working around overhead power lines. This law applies to individuals
and businesses whose work requires close proximity to overhead power lines, excluding cable television
and telephone companies. It specifies limits for working safely near overhead power lines and requires a
safe work area when those limits cannot be maintained to perform the necessary work. This law states
that no mechanized equipment can be operated within 10 feet of a power line within the range of 600-
50,000 volts, and a person cannot come within 6 feet. When working within these limits, the worker must
notify the power company, which will then turn off or relocate the line or make specific recommendations
regarding equipment.
Special protective apparel should be worn by employees who have to work near high-voltage lines,
including helmets, rubber gloves and sleeves, and goggles. According to OSHA, employees working near
high-voltage lines should wear class B helmets (as defined by ANSI) that are designed to withstand
20,000 volts of alternating current at a frequency of 60 Hz for a total of 3 minutes. In addition, these
helmets should resist burn-through at 30,000 volts.
High-voltage wires are prone to occasional discharges or arcs of electricity that can damage the corneal
epithelium. This protective eyewear prevents such an injury. In Washington, irrigation pipes (IP) used by
farmers are the most common source of fatal human contact with high-voltage electric lines. Groups such
as public utility companies and cooperative extension services have recognized the dangers of IP
electrocution and have advised caution when IPs are handled near electric lines. All agencies and groups
(including state and county health departments, utility companies, agriculture extension services, school
districts, civic associations, and agricultural workers groups) in rural areas irrigated with metal pipes are
encouraged to remind agricultural workers of the life-threatening hazard of IP electrocution.
Scientific basis for selecting gloves
Rubber insulating gloves are necessary for manipulation of high-voltage wires and for protection against
burn injury.
[40]
Class 2 gloves, as defined by the American Society for Testing and Materials, provide
protection at 20,000 volts. Class 4 gloves provide protection at 40,000 volts and should be worn by those
working near and with high-voltage wires. Tinted protective eyewear also should be worn. Despite
expensive regulatory and safety program efforts, electrical hazards still represent an important
occupational health and safety issue for workers in the electric utility industry.
Once the electrical current has been disconnected, the emergency medical technicians and paramedics
responding to an electrical injury situation should wear emergency medical examination gloves with a
glove hole leakage rate of 1% rather than examination gloves used in the hospital, which have a glove
hole leakage rate of 4% (as required by the Food and Drug Administration [FDA]).
[41]
Smoke Evacuation During Electrosurgery Procedures
Electrosurgical techniques have been used in hospitals for more than a century. Electrosurgery in the
operating room may be associated with smoke that contains the same airborne contaminants as laser
smoke. This plume contains toxic gases and vapors, such as benzene, hydrogen cyanide, formaldehyde,
and dead and living cellular material, including blood and viruses. The contaminants have an unpleasant
odor, may cause visibility problems at the surgical site, and may produce upper respiratory tract and eye
irritation. The contaminants have mutagenic and carcinogenic potential.
The National Institute of Safety and Health recommends the use of smoke evacuation systems. A smoke
evacuator and an ultra-low particulate air filter should be used when large amounts of smoke or plume
can be generated in the operative procedure. This filter can remove 99.9999% of the bacteria, dust,
pollen, mold, and particles with a size of 120 nanometers or larger from the air.
[42]
1. Haberal MA. An eleven-year survey of electrical burn injuries. J Burn Care Rehabil. Jan-Feb
1995;16(1):43-8. [Medline].
2. Hulsbergen-Kruger S, Pitzler D, Partecke BD. [High voltage accidents, characteristics and
treatment].Unfallchirurg. Apr 1995;98(4):218-23. [Medline].
3. Dalziel CF. Effects of electric shock on man. IRE Trans Med Electron. 1956;5:44-62.
4. Dalziel CF. The threshold of perception currents. Elec Eng. 1954;73:625-630.
5. Rai J, Jeschke MG, Barrow RE, Herndon DN. Electrical injuries: a 30-year review. J Trauma. May
1999;46(5):933-6. [Medline].
6. Casini V. Overview of electrical hazards. In:. Worker deaths by electrocution: A summary of
NIOSH surveillance and investigative findings. 98-131. NIOSH: Department of Health & Human
Services; 1998. 5-8.
7. Cooper MA. Electrical and lightning injuries. Emerg Med Clin North Am. Aug 1984;2(3):489-
501. [Medline].
8. Fish RM. Electric injury, part I: treatment priorities, subtle diagnostic factors, and burns. J Emerg
Med. Nov-Dec 1999;17(6):977-83. [Medline].
9. Koumbourlis AC. Electrical injuries. Crit Care Med. Nov 2002;30(11 Suppl):S424-30. [Medline].
10. Housinger TA, Green L, Shahangian S, Saffle JR, Warden GD. A prospective study of myocardial
damage in electrical injuries. J Trauma. Feb 1985;25(2):122-4. [Medline].
11. Diamond TH, Twomey A, Myburgh DP. High-voltage electrical injury. A case report and review of
the literature. S Afr Med J. Feb 27 1982;61(9):318-21. [Medline].
12. Ku CS, Lin SL, Hsu TL, Wang SP, Chang MS. Myocardial damage associated with electrical
injury. Am Heart J. Sep 1989;118(3):621-4. [Medline].
13. Carleton SC. Cardiac problems associated with electrical injury. Cardiol Clin. May
1995;13(2):263-6.[Medline].
14. Chandra NC, Siu CO, Munster AM. Clinical predictors of myocardial damage after high voltage
electrical injury. Crit Care Med. Mar 1990;18(3):293-7. [Medline].
15. Nichter LS, Morgan RF, Bryant CA, Haines PC, Bacchetta CA, Edlich RF. Electric burns of the
oral cavity.Compr Ther. Apr 1985;11(4):65-71. [Medline].
16. Edlich RF, Hill LG, Mahler CA, Cox MJ, Becker DG, Horowitz JH, et al. Management and
prevention of tetanus. J Long Term Eff Med Implants. 2003;13(3):139-54. [Medline].
17. Hunt JL, McManus WF, Haney WP, Pruitt BA Jr. Vascular lesions in acute electric injuries. J
Trauma. Jun 1974;14(6):461-73. [Medline].
18. Mann R, Gibran N, Engrav L, Heimbach D. Is immediate decompression of high voltage electrical
injuries to the upper extremity always necessary?. J Trauma. Apr 1996;40(4):584-7; discussion
587-9. [Medline].
19. Nettelblad H, Thuomas KA, Sjoberg F. Magnetic resonance imaging: a new diagnostic aid in the
care of high-voltage electrical burns. Burns. Mar 1996;22(2):117-9. [Medline].
20. Hammond J, Ward CG. The use of Technietium-99 pyrophosphate scanning in management of
high voltage electrical injuries. Am Surg. 1994;60(11):886-8.
21. Affleck DG, Edelman L, Morris SE, Saffle JR. Assessment of tissue viability in complex extremity
injuries: utility of the pyrophosphate nuclear scan. J Trauma. Feb 2001;50(2):263-9. [Medline].
22. Cherington M. Central nervous system complications of lightning and electrical injuries. Semin
Neurol. Sep 1995;15(3):233-40. [Medline].
23. Wilbourn AJ. Peripheral nerve disorders in electrical and lightning injuries. Semin Neurol. Sep
1995;15(3):241-55. [Medline].
24. Varghese G, Mani MM, Redford JB. Spinal cord injuries following electrical accidents. Paraplegia.
Jun 1986;24(3):159-66. [Medline].
25. Guinard JP, Chiolero R, Buchser E, Delaloye-Bischof A, Payot M, Grbic A, et al. Myocardial injury
after electrical burns: short and long term study. Scand J Plast Reconstr Surg Hand Surg.
1987;21(3):301-2.[Medline].
26. Chilbert MA, Swiontek T, Myklebust JB, Prieto TE, Sances A Jr, Leffingwell C, et al. Fibrillation
induced at powerline current levels. IEEE Trans Biomed Eng. Aug 1989;36(8):864-9. [Medline].
27. Hammond J, Ward CG. Myocardial damage and electrical injuries: significance of early elevation
of CPK-MB isoenzymes. South Med J. Apr 1986;79(4):414-6. [Medline].
28. McBride JW, Labrosse KR, McCoy HG, Ahrenholz DH, Solem LD, Goldenberg IF. Is serum
creatine kinase-MB in electrically injured patients predictive of myocardial injury?. JAMA. Feb 14
1986;255(6):764-8. [Medline].
29. Chuang SS, Yu CC. Delayed obturator artery rupture: a complication of high-voltage electrical
injury.Burns. Jun 2003;29(4):395-8. [Medline].
30. Grnfeld JP, Kleinknecht D, Moreau JF, Kamoun P, Sabto J, Garcia-Torres R, et al. Permanent
hypertension after renal homotransplantation in man. Clin Sci Mol Med. May 1975;48(5):391-
403. [Medline].
31. Newsome TW, Curreri PW, Eurenius K. Visceral injuries: an unusual complication of an electrical
burn.Arch Surg. Sep 1972;105(3):494-7. [Medline].
32. Sinha JK, Roy SK. Perforation of the caecum caused by an electrical burn. Br J Plast Surg. Apr
1976;29(2):179-81. [Medline].
33. Haberal M, Ucar N, Bayraktar U, Oner Z, Bilgin N. Visceral injuries, wound infection and sepsis
following electrical injuries. Burns. Mar 1996;22(2):158-61. [Medline].
34. Honda T, Yamamoto Y, Mizuno M, Mitsusada M, Nakazawa H, Sasaki K, et al. Successful
treatment of a case of electrical burn with visceral injury and full-thickness loss of the abdominal
wall. Burns. Sep 2000;26(6):587-92. [Medline].
35. Rijhwani A, Sunil I. Colonic fistula complicating electric burns--a case report. J Pediatr Surg. Aug
2003;38(8):1232-3. [Medline].
36. ten Duis HJ. Acute electrical burns. Semin Neurol. Dec 1995;15(4):381-6. [Medline].
37. Wright HR, Drake DB, Gear AJL, Wheeler JC, Edlich RF. Industrial high-voltage electrical burn of
the skull, a preventable injury. J Emerg Med. 1997;15(3):345-9. [Medline].
38. Reddy SC. Electric cataract: a case report and the view of the literature. Eur J Ophthalmol.
1999;9(2):134-8. [Medline].
39. Jaffe R, Fejgin M, Ben Aderet N. Fetal death in early pregnancy due to electric current. Acta
Obstet Gynecol Scand. 1986;65(3):283. [Medline].
40. American Society for Testing and Materials. Specification for rubber insulating gloves. ASTM
D120-87 [database online]. New York: American Society for Testing and Materials; 1987.
Updated 1987.
41. Edlich RF, Winters KL, Martin ML, Long Iii WB, Werner CL, Gubler KD. Scientific basis for the
selection of emergency medical examination gloves for emergency medical technicians,
paramedics, firefighters, and emergency department personnel. An update. J Long Term Eff Med
Implants. 2005;15(2):161-83.[Medline].
42. Ogg M. Smoke evacuation during electrosurgery procedures. AORN J. Nov 2009;90(5):751-
2. [Medline].
43. Edlich RF, Long WB 3rd, Gubler KD, et al. Citizen's Petition to Food and Drug Administration to
ban cornstarch powder on medical gloves: Maltese cross birefringence. Am J Emerg Med. Feb
2009;27(2):227-35. [Medline].
44. Edlich RF, Wind TC, Heather CL, Thacker JG. Reliability and performance of innovative surgical
double-glove hole puncture indication systems. J Long Term Eff Med Implants. 2003;13(2):69-
83. [Medline].
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Boy Scouts Notes: First AidDocument10 pagesBoy Scouts Notes: First Aidscoutingresources100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Neurogenic Shock: Understanding the Hemodynamic ResponseDocument7 pagesNeurogenic Shock: Understanding the Hemodynamic Responseyayayaniza100% (1)
- Pathophysiology of Burn InjuryDocument46 pagesPathophysiology of Burn InjuryIyanAsiana100% (1)
- TraumaDocument10 pagesTraumaNur Liyana Ahmad ZakiNo ratings yet
- Pediatric EmergenciesDocument47 pagesPediatric EmergenciesahmedNo ratings yet
- Renr Review Ras Practice Test 32Document22 pagesRenr Review Ras Practice Test 32Simone PhillipNo ratings yet
- ABSEN CC NewDocument3 pagesABSEN CC NewIbnu YudistiroNo ratings yet
- Diefenbeck Et Al-2013-International Wound JournalDocument5 pagesDiefenbeck Et Al-2013-International Wound JournalIbnu YudistiroNo ratings yet
- Logbook Agustus 2018Document4 pagesLogbook Agustus 2018Ibnu YudistiroNo ratings yet
- Anterolateral ApproachDocument3 pagesAnterolateral ApproachHanifNo ratings yet
- Quick DashDocument1 pageQuick DashIbnu YudistiroNo ratings yet
- Quick DashDocument1 pageQuick DashIbnu YudistiroNo ratings yet
- Quickdash Scoring System: The Quickdash Outcome Measure: Scoring E-Tool For Use by CliniciansDocument1 pageQuickdash Scoring System: The Quickdash Outcome Measure: Scoring E-Tool For Use by CliniciansOvidiu RusuNo ratings yet
- Quick DashDocument1 pageQuick DashIbnu YudistiroNo ratings yet
- Vol06 b3 14-17p PDFDocument4 pagesVol06 b3 14-17p PDFIbnu YudistiroNo ratings yet
- Hypertensive Emergency: Indonesian Society of HypertensionDocument29 pagesHypertensive Emergency: Indonesian Society of HypertensionRizky Saraswati IndraputriNo ratings yet
- Chapter Contents: 8. Maternal ResuscitationDocument10 pagesChapter Contents: 8. Maternal ResuscitationChristine Notoningtiyas SantosoNo ratings yet
- Chapter Contents: 8. Maternal ResuscitationDocument10 pagesChapter Contents: 8. Maternal ResuscitationChristine Notoningtiyas SantosoNo ratings yet
- ComprehensiveDocument4 pagesComprehensiveDeekshitha Turaka0% (1)
- Method Statement: (Continuous Flight Auger)Document15 pagesMethod Statement: (Continuous Flight Auger)sawkariqbal100% (1)
- Safety 2016Document64 pagesSafety 2016jackdrejeNo ratings yet
- Kunci Jawaban Lks Uas Ganjil Bahasa Inggris Kelas 12 2023-2024Document7 pagesKunci Jawaban Lks Uas Ganjil Bahasa Inggris Kelas 12 2023-2024Reno AdityaNo ratings yet
- Built-In Oven HBA63B2.1B: (En) Instruction ManualDocument28 pagesBuilt-In Oven HBA63B2.1B: (En) Instruction Manuals bNo ratings yet
- Basic First AidDocument27 pagesBasic First AidPisethSaoNo ratings yet
- BURNDocument5 pagesBURNLara TechiesNo ratings yet
- Incident Report Form: RPSG-IMS-F-24 Accident and Investigation Form 5ADocument2 pagesIncident Report Form: RPSG-IMS-F-24 Accident and Investigation Form 5ARocky BisNo ratings yet
- Wa0126.Document91 pagesWa0126.Sebes Ignacio Villa MayoNo ratings yet
- ETAT Ethiopia Manual For Participants May 20 2014 PRINTDocument184 pagesETAT Ethiopia Manual For Participants May 20 2014 PRINTNadik83% (6)
- Brain Dump NUR 213 FINALDocument37 pagesBrain Dump NUR 213 FINALkelsey jackson100% (1)
- Sample Case StudyDocument23 pagesSample Case StudyDELFIN, Kristalyn JaneNo ratings yet
- Burn Types, Causes, Classification and TreatmentDocument10 pagesBurn Types, Causes, Classification and TreatmentSonny Dizon PareñasNo ratings yet
- A) First Degree Burns (Superficial Burns)Document4 pagesA) First Degree Burns (Superficial Burns)Art Christian RamosNo ratings yet
- 3700 User Manual 2010Document76 pages3700 User Manual 2010Mariana DariiNo ratings yet
- Vaser Assisted High Definition LiposuctionDocument11 pagesVaser Assisted High Definition LiposuctiondcgNo ratings yet
- StudentsDocument756 pagesStudentsxxx xNo ratings yet
- Committee On Trauma Presents: Thermal InjuriesDocument35 pagesCommittee On Trauma Presents: Thermal InjuriesAlfina Aulia RizkiNo ratings yet
- Takara MicroMist OPDocument20 pagesTakara MicroMist OPNazihCosmeticsNo ratings yet
- Burn ManagementDocument19 pagesBurn ManagementKavimathy SukumaranNo ratings yet
- First Aid PamphletDocument14 pagesFirst Aid PamphletAriane Yhanna CastillonNo ratings yet
- Basic First Aid Procedures for EmergenciesDocument4 pagesBasic First Aid Procedures for EmergenciesSoyPedroNo ratings yet
- Isbi Practice Guidelines For Burn Care, Part 2: SciencedirectDocument90 pagesIsbi Practice Guidelines For Burn Care, Part 2: SciencedirectDella pinkaNo ratings yet
- Gano Massage Oil - English - Malaysia - v2Document13 pagesGano Massage Oil - English - Malaysia - v2bigjebatNo ratings yet