Professional Documents
Culture Documents
Gero Nursing
Uploaded by
Rodelen Maraño0 ratings0% found this document useful (0 votes)
32 views34 pagesfafsdgdfgdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentfafsdgdfgdf
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
32 views34 pagesGero Nursing
Uploaded by
Rodelen Marañofafsdgdfgdf
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 34
Dementia
Progressive, degenerative brain dysfunction, including
deterioration in memory, concentration, language skills,
visuospatial skills, and reasoning
Progressive forgetfulness, memory loss, and loss of
other cognitive function
Interferes with a persons daily functioning
Not considered a normal part of aging
Dementia: Background
4 million older adults have some form of dementia
How is dementia different from depression and
delirium?
Slower onset
Progressive, not variable
Irreversible
Different causes
Lowest MMSE
Risk Factors for Dementia
Age
Family history
Genetic factors
Head trauma
Vascular disease
Infections
Other modifiable factors
Maintain ideal body weight
Exercise
Avoid smoking
Control hyperlipidemia and hypertension
Exercising the brain with lifelong cognitive activity may help
lower the risk of dementia
Causes of Dementia
Drugs
Environmental
Metabolic
Eyes/Ears sensory deprivation
Nutrition
Trauma/Tumor
Infections
Alcohol abuse or intoxication
Assessing for Dementia
Mini-COG
A reliable and valid instrument used to screen for
cognitive impairment consisting of 3-item recall test
and a clock-drawing test (CDT)
It is evidence-based, easy to administer, and not too
taxing for patient or provider
Is a screening test, doesnt provide diagnosis
CLOCK DRAWING TEST
Types of Dementia
Alzheimers #1
Vascular
Parkinsons
Lewy body
Frontal lobe dementia
Lose inhibition and executive functioning skills earlier than
AD
Normal pressure hydrocephalus
Rare but partially reversible with surgery
Acute onset of a triad of symptoms
slowed cognitive processes, gait disturbances, UI
Alzheimers Disease (AD)
The most common type of dementia seen in
older adults
Advanced age is the single most significant risk
factor
Estimated 5.2 million Americans affected in
2008
5 million over age 65
Estimated to reach 7.7 million in 2030
Projected 11 16 million by 2050
Alzheimers Disease (AD)
May live from 3 20 years or more after
diagnosis
Seventy percent of people with AD live at home
until the latest stages, being cared for mainly by
family members (Alzheimers Association, 2005
Costs $61 billion annually
Expected to exceed $163 billion/yr by 2050
Characterized by progressive memory loss
Average life span of 8 years after dx
Alzheimers Disease (AD)
Two types of abnormal lesions in the brains of
individuals with Alzheimer's disease:
Plaques
Neurofibrillary tangles
Definitive diagnosis is still through biopsy
Dx: early dx is important to maximize function
and QOL as long as possible
Diagnosing Alzheimers
Memory impairment alone doesnt indicate AD
Requires one of the following features
Impaired executive function
Aphasia word finding difficulties
Apraxia cannot carry out motor skills
Agnosia cannot name familiar object
Must rule out delirium, depression, other CNS
disorders, medication side effects, and other medical
conditions first!
Diagnosing Alzheimers (contd)
H & P
Review of medications
Laboratory testing
Neuropsychological screening/testing
Mini Mental Status Exam (MMSE) no longer available in
public domain
Mini-Cog
Imaging
PET scan to rule out dementia
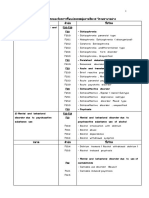
Medications for Dementia
Medications slow progression but do not stop decline
over time
Cholinesterase Inhibitors (CEIs)
donepezil (Aricept)
rivastigmine (Exelon)
galantamine (Razadyne)
N-methyl-D-aspartate (NMDA) Receptor Antagonist
memantine (Namenda) approved for moderate to late stage
Anticholinergics can worsen cognitive function
AD: Warning Signs
Ten warning signs of Alzheimers Disease
Memory loss
Difficulty performing familiar tasks
Problems with language
Disorientation to time and place
Poor or decreased judgment
Problems with abstract thinking
Misplacing things
Changes in mood or behavior
Changes in personality
Loss of initiative
AD: Treatment
Medications (Aricept, Namenda) may help slow
progress but does not change disease course
Symptom management
Behavior
Safety
Nutrition
Hygiene
As dementia progresses, likely to be institutionalized
Support for family/caregiver
Support groups
Respite
Be aware of caregiver strain
Other Types of Dementias
Vascular dementia results from multiple
cerebral infarctions
more rapid and more predictable than AD
risk factors: HTN, hyperlipidemia, history of stroke,
smoking
Lewy body dementia presence of Lewy body
substance in cerebral cortex many
gerontologists consider this the same type of
dementia as AD
Other Types of Dementias
Creutzfeld-Jacob disease (Mad Cow)
Rare brain disorder
Rapid onset and progression
Slow virus
Familial tendency
Destruction of neurons in cortex
Symptoms more varied than AD
Death with 1 year
Other Types of Dementias
Parkinsons disease
Small percentage of those with dementia are this
type
Degeneration of neurons due to lack of
neurotransmitter, Dopamine
Delirium: Background
Also called acute confusion
Occurs in 22- 38% of older patients in the
hospital
Occurs in as many as 40% of long-term care
residents
Associated with increased length of stays in the
hospital and higher mortality rates
Delirium: Background
Altered level of consciousness
Temporary
Reversible
Many treatable causes
Need to distinguish delirium, depression, and
dementia
Delirium
Treatment of delirium requires the diagnosis
and treatment of the underlying physiological
problem while using pharmacologic and non-
pharmacologic interventions to maintain patient
safety and return the patient to the pre-delirium
state (Mauk, pg. 445).
Delirium: Potential causes
Fluid and electrolyte
imbalances
Infection
CHF
Medications
Pain
Impaired cardiac or
respiratory function
Emotional stress
Unfamiliar surroundings
Malnutrition
Anemia
Dehydration
Alcoholism
Hypoxia
Causes of Delirium
Drugs
Electrolytes
Liver failure
Infection
Renal failure
Impaction
UTI or urinary retention
Metastasis
Delirium: Signs/Symptoms
Sudden onset
Disorientation to time and place
Altered attention
Impaired memory
Mood swings
Poor judgment
Altered LOC
Decreased MMSE score (less than depression, but
more than dementia)
Delirium: Treatment
Detect promptly by good H & P
MMSE, GDS and CAM are good assessment
tools
CBC, Lytes, LFTs, Renal function, Serum
calcium and glucose, UA, CXR, EKG, O2 Sat
For all Older Adults with
Cognitive Impairment
Maintain privacy and dignity
Realize their value as a unique individual
Maintain independence for as long as possible
Minimize restraints find other answers to
address wandering
Continue human contact and environmental
stimulation Repetition
Delirium
Acute confusion
Four basic features
Acute onset or fluctuating course
Inattention
Disorganized thinking
Altered level of consciousness
Primary treatment is to eliminate the cause
Delusion of theft and phantom intruder
Potential Causes of Delirium
Inadequate or inappropriate
pain control
Medications (including new
or change in dose)
Fecal impaction
Infection/fever
Injury/severe illness
Electrolyte imbalance
(glucose, Na+)
Dehydration
Change in surroundings
Hypoxia
Age
Male gender
Cognitive impairment
(dementia)
Hypotension
Malnutrition
Depression
Alcoholism
Restraints
Multiple IVs, lines, tubes
Assessing for Delirium
Delirium is often unrecognized by clinicians
Hence patients should be assessed frequently using a
standardized tool to facilitate prompt identification and
management of delirium and underlying etiology
Confusion Assessment Method (CAM)
Sensitivity of 94-100%
Specificity of 89-95%
CAM The Short Version
1. Acute Onset
Is there evidence of an acute change in mental status
from baseline?
2. Inattention
Does the patient have difficulty focusing attention;
easily distractible; have difficulty keeping track of
what is being said?
Does this behavior fluctuate; come and go or
increase and decrease in severity?
3. Disorganized thinking
Is the patients thinking disorganized or incoherent, such as
rambling or irrelevant conversation, unclear or illogical flow
of ideas, or unpredictable switching from subject to subject?
4. Altered level of consciousness
Overall, how would you rate this patients level of
consciousness?
Alert = normal
Vigilant = hyper-alert, overly sensitive to environmental stimuli,
startled very easily
Lethargic = drowsy, easily aroused
Stupor = difficult to arouse
Coma = unarousable
Uncertain
CAM Continued
Should assess patient on admission and during
each shift
Engage pt. in conversation for about one
minute. Ask:
What brought you to the hospital?
How are you feeling now?
Delirium is identified only if there is evidence of
features 1 and 2, and either 3 or 4 (or both)
Nursing Interventions/Strategies
Use general strategies (as appear in next slides)
Address specific issues/behaviors
Wandering
Aggression
Restlessness
Agitation
Physical comfort
Pain
You might also like
- Funda BulletsDocument13 pagesFunda BulletsCin DyNo ratings yet
- Comprehensive Examination: Trinity University of AsiaDocument1 pageComprehensive Examination: Trinity University of AsiaRodelen MarañoNo ratings yet
- Background of The StudyDocument4 pagesBackground of The StudyRodelen MarañoNo ratings yet
- MERCI retrieval removes brain clot less than 40Document1 pageMERCI retrieval removes brain clot less than 40Roel MarañoNo ratings yet
- Effective Airway ClearanceDocument2 pagesEffective Airway ClearanceRodelen MarañoNo ratings yet
- Appendicitis Is A Medical Emergency Characterized by Inflammation of The AppendixDocument1 pageAppendicitis Is A Medical Emergency Characterized by Inflammation of The AppendixRodelen MarañoNo ratings yet
- Systemic Lupus Erythematosus: Pathogenesis and Clinical FeaturesDocument30 pagesSystemic Lupus Erythematosus: Pathogenesis and Clinical FeaturesOrion JohnNo ratings yet
- CA - Amniotic Fluid EmbolismDocument13 pagesCA - Amniotic Fluid EmbolismRodelen Maraño100% (2)
- MERCI retrieval removes brain clot less than 40Document1 pageMERCI retrieval removes brain clot less than 40Roel MarañoNo ratings yet
- PHY101L Physics 1 Lab SyllabusDocument2 pagesPHY101L Physics 1 Lab SyllabusRodelen MarañoNo ratings yet
- Anatomy of Appendix HahahahaDocument1 pageAnatomy of Appendix HahahahaRodelen MarañoNo ratings yet
- Activated CharcoalDocument4 pagesActivated CharcoalRodelen MarañoNo ratings yet
- Gavin, M. L. (2011) : Hughes, F. P. (1999) General Characteristics of The AdolescentDocument1 pageGavin, M. L. (2011) : Hughes, F. P. (1999) General Characteristics of The AdolescentRodelen MarañoNo ratings yet
- 11background of The StudybfvutyfcgcDocument1 page11background of The StudybfvutyfcgcRodelen MarañoNo ratings yet
- Diagnostic Examination Ultrasonography: ResultDocument1 pageDiagnostic Examination Ultrasonography: ResultRodelen MarañoNo ratings yet
- Somewhere Only We KnowDocument4 pagesSomewhere Only We KnowRodelen MarañoNo ratings yet
- First AidDocument10 pagesFirst AidRodelen MarañoNo ratings yet
- What Is GangreneDocument12 pagesWhat Is GangreneRodelen MarañoNo ratings yet
- Informatics KoreaDocument40 pagesInformatics KoreaRodelen MarañoNo ratings yet
- Case Presentation: Ascariasis: Mrs. Lailanie Evangelista DotimasDocument10 pagesCase Presentation: Ascariasis: Mrs. Lailanie Evangelista DotimasRodelen MarañoNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- African American FactsheetDocument4 pagesAfrican American Factsheetঅমিত ভট্টাচার্যNo ratings yet
- Self Efficacy ModelDocument2 pagesSelf Efficacy ModelTrisha Daphney LimNo ratings yet
- Understanding Consciousness and Sleep Through Cognitive PsychologyDocument50 pagesUnderstanding Consciousness and Sleep Through Cognitive PsychologyMonicaNo ratings yet
- Overcome Speech Anxiety in 4 StepsDocument16 pagesOvercome Speech Anxiety in 4 StepsSerc YablaNo ratings yet
- Icd 10Document4 pagesIcd 10ÜnŶäÜnClubEverydayNo ratings yet
- Hilderley BettcherDocument10 pagesHilderley Bettcherapi-162509150No ratings yet
- Insights and Perception of The Senior High School Students Grade 11 Department of Holy Cross College of Carigara On DepressionDocument27 pagesInsights and Perception of The Senior High School Students Grade 11 Department of Holy Cross College of Carigara On DepressionAnnie MustaphaNo ratings yet
- PSYCHIATRYDocument6 pagesPSYCHIATRYRahaf Bin ManieNo ratings yet
- BS 4th Semester 2019Document328 pagesBS 4th Semester 2019Umair ShabbirNo ratings yet
- Generalized Anxiety Disorder: Timothy A. Brown Tracy A. O'Leary David H. BarlowDocument55 pagesGeneralized Anxiety Disorder: Timothy A. Brown Tracy A. O'Leary David H. BarlowCamila JoaoNo ratings yet
- Evidence-Based Cognitive Hypnotherapy For DepressionDocument19 pagesEvidence-Based Cognitive Hypnotherapy For DepressionEva JacintoNo ratings yet
- Classifying of Children's Cooperative Behavior: Pedodontics Lec. 3Document8 pagesClassifying of Children's Cooperative Behavior: Pedodontics Lec. 3Haider F YehyaNo ratings yet
- Eye Complaint QuestionnaireDocument2 pagesEye Complaint QuestionnairePande Bagus WidyantaraNo ratings yet
- The Art of Influencing PeopleDocument53 pagesThe Art of Influencing PeopleGiyan PratiwiNo ratings yet
- Benefit Speech TherapyDocument4 pagesBenefit Speech TherapyMoewardi KmkkNo ratings yet
- Literature Review of StressDocument3 pagesLiterature Review of StressLê Thùy TrangNo ratings yet
- OB Study Guide on History, Elements, Approaches & BenefitsDocument28 pagesOB Study Guide on History, Elements, Approaches & Benefitsfrance marie annNo ratings yet
- Personality Adaptations Further ClarifiedDocument5 pagesPersonality Adaptations Further ClarifiedAngela Hernandez CordobaNo ratings yet
- Etiology of Anxiety Disorders PDFDocument2 pagesEtiology of Anxiety Disorders PDFCourtneyNo ratings yet
- Parkinson Disease and Dementia: Understanding the LinkDocument45 pagesParkinson Disease and Dementia: Understanding the LinkraniNo ratings yet
- AITSA Internet Addiction ResearchDocument7 pagesAITSA Internet Addiction ResearchJayson PizonNo ratings yet
- Unit-1 Introduction To CounsellingDocument14 pagesUnit-1 Introduction To CounsellingAaquib Zaved100% (1)
- Assignment 3 Carl JungDocument7 pagesAssignment 3 Carl JungKendrew SujideNo ratings yet
- How To Read A Text Using PsychoanalysisDocument1 pageHow To Read A Text Using PsychoanalysisScholar Winterflame100% (1)
- The Alternative Genre Project AssignmentDocument3 pagesThe Alternative Genre Project Assignmentapi-533980796No ratings yet
- Diamond 2013 Executive Functions PDFDocument39 pagesDiamond 2013 Executive Functions PDFGustav RSR100% (1)
- Reference Pyromania DSM VDocument7 pagesReference Pyromania DSM VFadli AmaliNo ratings yet
- Reflection - Edupsy 204 - Abnormal PsychologyDocument1 pageReflection - Edupsy 204 - Abnormal PsychologyJEFFREY VILLANGCANo ratings yet
- Cluster ADocument4 pagesCluster ANobody but youNo ratings yet
- Anger ManagementDocument11 pagesAnger ManagementSakhawat Hossain ShawonNo ratings yet