Professional Documents
Culture Documents
GOLD AtAGlance 2014 Jun11
Uploaded by
Devi Eliani ChandraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
GOLD AtAGlance 2014 Jun11
Uploaded by
Devi Eliani ChandraCopyright:
Available Formats
At-A-Glance Outpatient
Management Reference
for Chronic Obstructive
Pulmonary Disease (COPD)
At-A-Glance Outpatient
Management Reference
for Chronic Obstructive
Pulmonary Disease (COPD)
BASED ON THE GLOBAL STRATEGY FOR DIAGNOSIS,
MANAGEMENT AND PREVENTION OF COPD
GLOBAL INITIATIVE FOR CHRONIC OBSTRUCTIVE LUNG DISEASE (GOLD)
UPDATED 2014
Please refer to the GOLD Report (updated 2014) at www.goldcopd.org
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
-
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
DIAGNOSING COPD
A diagnosis of COPD should be considered in any individual who has
dyspnea, chronic cough or sputum production, and a history of exposure
to risk factors for the disease, especially cigarette smoking.
Consider COPD, and perform spirometry, if any of these indicators
are present in an individual over age 40. These indicators are not
diagnostic themselves, but the presence of multiple key indicators
increases the probability of a diagnosis of COPD. Spirometry is
required to establish a diagnosis of COPD.
Dyspnea that is: Progressive (worsens over time).
Characteristically worse with exercise.
Persistent.
Chronic cough: May be intermittent and may be unproductive.
Chronic sputum production:
Any pattern of chronic sputum production may
indicate COPD.
History of exposure to risk factors:
Tobacco smoke (including popular local preparations).
Smoke from home cooking and heating fuels.
Occupational dusts and chemicals.
Family history of COPD
Table 1. Key Indicators for Considering a Diagnosis of COPD
Spirometry is required to make a clinical diagnosis of COPD; the presence of
a postbronchodilator FEV
1
/FVC < 0.70 conrms the presence of persistent
airow limitation and thus of COPD. All health care workers who care for
COPD patients should have access to spirometry.
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
-
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
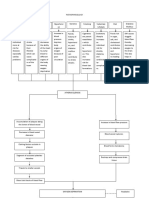
ASSESSMENT OF COPD
The goals of COPD assessment are to determine the severity of the disease, its
impact on patients health status, and the risk of future events (exacerbations,
hospital admissions, death) in order to guide therapy. Assess the following
aspects of the disease separately:
Symptoms
Degree of airow limitation (using spirometry)
Risk of exacerbations
Comorbidities
Assess Symptoms: Validated questionnaires such as the COPD Assessment
Test (CAT) or the Clinical COPD Questionnaire (CCQ) are recommended
for a comprehensive assessment of symptoms. The modied British
Medical Research Council (mMRC) scale provides only an assessment of
breathlessness.
Assess Degree of Airow Limitation Using Spirometry: Table 2 provides the
classication of airow limitation severity in COPD.
Assess Risk of Exacerbations: An exacerbation of COPD is dened as an acute
event characterized by a worsening of the patients respiratory symptoms that
is beyond normal day-to-day variations and leads to a change in medication.
The best predictor of having frequent exacerbations (2 or more per year) is
a history of previous treated events; the risk of exacerbations also increases
as airow limitation worsens. Hospitalization for a COPD exacerbation is
associated with a poor prognosis with increased risk of death.
Table 2. Classication of Severity of Airow Limitation in COPD
(Based on Post-Bronchodilator FEV
1
)
In patients with FEV1/FVC < 0.70:
GOLD 1: Mild FEV
1
80% predicted
GOLD 2: Moderate 50% FEV
1
< 80% predicted
GOLD 3: Severe 30% FEV
1
< 50% predicted
GOLD 4: Very Severe FEV
1
< 30% predicted
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
-
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
Assess Comorbidities: Cardiovascular diseases, osteoporosis, depression
and anxiety, skeletal muscle dysfunction, metabolic syndrome, and lung
cancer among other diseases occur frequently in COPD patients. These
comorbid conditions may inuence mortality and hospitalizations, and
should be looked for routinely and treated appropriately.
Combined Assessement of COPD: Table 3 provides a rubric for combining
these assessments to improve management of COPD.
Symptoms:
Less Symptoms (mMRC 0-1 or CAT < 10): patient is (A) or (C)
More Symptoms (mMRC 2 or CAT 10): patient is (B) or (D)
Airow Limitation:
Low Risk (GOLD 1 or 2): patient is (A) or (B)
High Risk (GOLD 3 or 4): patient is (C) or (D)
Exacerbations:
Low Risk: 1 per year and no hospitalization for exacerbation: patient is (A) or (B)
High Risk: 2 per year or 1 with hospitalization: patient is (C) or (D)
Table 3. Combined Assessment of COPD
When assessing risk, choose the highest risk according to GOLD grade or exacerbation history.
(One or more hospitalizations for COPD exacerbations should be considered high risk.)
Patient Characteristic
Spirometric
Classification
Exacerbations per year CAT mMRC
A
Low Risk
Less Symptoms
GOLD 1-2 1 < 10 0-1
B
Low Risk
More Symptoms
GOLD 1-2 1 10 2
C
High Risk
Less Symptoms
GOLD 3-4 2 < 10 0-1
D
High Risk
More Symptoms
GOLD 3-4 2 10 2
(C) (D)
(A) (B)
R
i
s
k
(
E
x
a
c
r
b
a
t
i
o
n
H
i
s
t
o
r
y
)
R
i
s
k
(
G
o
l
d
C
l
a
s
s
i
c
a
t
i
o
n
o
f
A
i
r
o
w
L
i
m
i
t
a
t
i
o
n
)
Symptoms
Breathlessness
CAT < 10 CAT 10
mMRC 0-1 mMRC 2
4
3
2
1
2
or
1 leading
to hospital
admission
1 (not leading
to hospital
admission)
0
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
-
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
Once COPD has been diagnosed, effective management should be based on an
individualized assessment of current symptoms and future risks:
Relieve symptoms
Improve exercise tolerance
Improve health status
and
Prevent disease progression
Prevent and treat exacerbations
Reduce mortality
These goals should be reached with minimal side effects from treatment, a particular
challenge in COPD patients because they commonly have comorbidities that also
need to be carefully identied and treated.
Bronchodilators Recommendations:
For both beta
2
-agonists and anticholinergics, long-acting formulations are
preferred over short-acting formulations.
The combined use of short- or long-acting beta
2
-agonists and anticholinergics
may be considered if symptoms are not improved with single agents.
Based on efcacy and side effects, inhaled bronchodilators are preferred
over oral bronchodilators.
Based on evidence of relatively low efcacy and greater side effects,
treatment with theophylline is not recommended unless other bronchodilators
are not available or unaffordable for long-term treatment.
Corticosteroids and Phosphodiesterase-4 Inhibitors Recommendations
There is no evidence to recommend a short-term therapeutic trial with oral
corticosteroids in patients with COPD to identify those who will respond to
inhaled corticosteroids or other medications.
Long-term treatment with inhaled corticosteroids is recommended for
patients with severe and very severe airow limitation and for patients with
frequent exacerbations that are not adequately controlled by long-acting
bronchodilators.
Long-term monotherapy with oral corticosteroids is not recommended in
COPD.
Long-term monotherapy with inhaled corticosteroids is not recommended
in COPD because it is less effective than the combination of inhaled
corticosteroids with long-acting beta2-agonists.
Long-term treatment containing inhaled corticosteroids should not be
prescribed outside their indications, due to the risk of pneumonia and the
possibility of a slightly increased risk of fractures following long-term-term
exposure.
The phosphodiesterase-4 inhibitor roumilast may also be used to reduce
exacerbations for patients with chronic bronchitis, severe and very severe
airow limitation, and frequent exacerbations that are not adequately
controlled by long-acting bronchodilators.
MANAGEMENT OF STABLE COPD
REDUCE SYMPTOMS
REDUCE RISK
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
-
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
*
M
e
d
i
c
a
t
i
o
n
s
i
n
e
a
c
h
b
o
x
a
r
e
m
e
n
t
i
o
n
e
d
i
n
a
l
p
h
a
b
e
t
i
c
a
l
o
r
d
e
r
a
n
d
t
h
e
r
e
f
o
r
e
n
o
t
n
e
c
e
s
s
a
r
i
l
y
i
n
o
r
d
e
r
o
f
p
r
e
f
e
r
e
n
c
e
.
*
*
M
e
d
i
c
a
t
i
o
n
s
i
n
t
h
i
s
c
o
l
u
m
n
c
a
n
b
e
u
s
e
d
a
l
o
n
e
o
r
i
n
c
o
m
b
i
n
a
t
i
o
n
w
i
t
h
o
t
h
e
r
o
p
t
i
o
n
s
i
n
t
h
e
F
i
r
s
t
a
n
d
A
l
t
e
r
n
a
t
i
v
e
C
h
o
i
c
e
c
o
l
u
m
n
s
G
l
o
s
s
a
r
y
:
S
A
:
s
h
o
r
t
-
a
c
t
i
n
g
L
A
:
l
o
n
g
-
a
c
t
i
n
g
I
C
S
:
i
n
h
a
l
e
d
c
o
r
t
i
c
o
s
t
e
r
o
i
d
P
D
E
-
4
:
p
h
o
s
p
h
o
d
i
e
s
t
e
r
a
s
e
-
4
p
r
n
:
w
h
e
n
n
e
c
e
s
s
a
r
y
T
a
b
l
e
4
:
P
h
a
r
m
a
c
o
l
o
g
i
c
T
h
e
r
a
p
y
f
o
r
S
t
a
b
l
e
C
O
P
D
*
P
a
t
i
e
n
t
G
r
o
u
p
R
E
C
O
M
M
E
N
D
E
D
F
I
R
S
T
C
H
O
I
C
E
A
L
T
E
R
N
A
T
I
V
E
C
H
O
I
C
E
O
T
H
E
R
P
O
S
S
I
B
L
E
T
R
E
A
T
M
E
N
T
S
*
*
A
S
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
p
r
n
o
r
S
A
b
e
t
a
2
-
a
g
o
n
i
s
t
p
r
n
L
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
o
r
L
A
b
e
t
a
2
-
a
g
o
n
i
s
t
o
r
S
A
b
e
t
a
2
-
a
g
o
n
i
s
t
a
n
d
S
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
T
h
e
o
p
h
y
l
l
i
n
e
B
L
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
o
r
L
A
b
e
t
a
2
-
a
g
o
n
i
s
t
L
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
a
n
d
L
A
b
e
t
a
2
-
a
g
o
n
i
s
t
S
A
b
e
t
a
2
-
a
g
o
n
i
s
t
a
n
d
/
o
r
S
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
T
h
e
o
p
h
y
l
l
i
n
e
C
I
C
S
+
L
A
b
e
t
a
2
-
a
g
o
n
i
s
t
o
r
L
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
L
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
a
n
d
L
A
b
e
t
a
2
-
a
g
o
n
i
s
t
o
r
L
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
a
n
d
P
D
E
-
4
I
n
h
i
b
i
t
o
r
o
r
L
A
b
e
t
a
2
-
a
g
o
n
i
s
t
a
n
d
P
D
E
-
4
I
n
h
i
b
i
t
o
r
S
A
b
e
t
a
2
-
a
g
o
n
i
s
t
a
n
d
/
o
r
S
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
T
h
e
o
p
h
y
l
l
i
n
e
D
I
C
S
+
L
A
b
e
t
a
2
-
a
g
o
n
i
s
t
a
n
d
/
o
r
L
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
I
C
S
+
L
A
b
e
t
a
2
-
a
g
o
n
i
s
t
a
n
d
L
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
o
r
I
C
S
+
L
A
b
e
t
a
2
-
a
g
o
n
i
s
t
a
n
d
P
D
E
-
4
i
n
h
i
b
i
t
o
r
o
r
L
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
a
n
d
L
A
b
e
t
a
2
-
a
g
o
n
i
s
t
o
r
L
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
a
n
d
P
D
E
-
4
i
n
h
i
b
i
t
o
r
C
a
r
b
o
c
y
s
t
e
i
n
e
S
A
b
e
t
a
2
-
a
g
o
n
i
s
t
a
n
d
/
o
r
S
A
a
n
t
i
c
h
o
l
i
n
e
r
g
i
c
T
h
e
o
p
h
y
l
l
i
n
e
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
-
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
Table 5. Formulations and Typical Doses of COPD Medications*
Drug
Inhaler (g)
Solution for
Nebulizer
(mg/ml)
Oral
Vials for
Injection (mg)
Duration
of Action
(hours)
Beta
2
-agonists
Short-acting
Fenoterol 100-200 (MDI) 1 0.05% (Syrup) 4-6
Levalbuterol 45-90 (MDI) 0.21, 0.42 6-8
Salbutamol (albuterol) 100, 200 (MDI & DPI) 5
5 mg (Pill),
0.024%(Syrup)
0.1, 0.5 4-6
Terbutaline 400, 500 (DPI) 2.5, 5 mg (Pill) 4-6
Long-acting
Formoterol 4.5-12 (MDI & DPI) 0.01
12
Arformoterol 0.0075 12
Indacaterol 75-300 (DPI) 24
Salmeterol 25-50 (MDI & DPI) 12
Tulobuterol 2 mg (transdermal) 24
Anticholinergics
Short-acting
Ipratropium bromide 20, 40 (MDI) 0.25-0.5 6-8
Oxitropium bromide 100 (MDI) 1.5 7-9
Long-acting
Aclidinium bromide 322 (DPI) 12
Glycopyrronium bromide 44 (DPI) 24
Tiotropium 18 (DPI), 5 (SMI) 24
Combination short-acting beta
2
-agonists plus anticholinergic in one inhaler
Fenoterol/Ipratropium 200/80 (MDI) 1.25/0.5 6-8
Salbutamol/Ipratropium 100/20 (SMI) 6-8
Combination long-acting beta
2
-agonist plus anticholinergic in one inhaler
Indacaterol/
glycopyrronium
85/43 (DPI) 24
Vilanterol/umeclidinium 25/62.5 (DPI) 24
Methylxanthines
Aminophylline 200-600 mg (Pill) 240
Variable, up
to 24
Theophylline (SR) 100-600 mg (Pill)
Variable, up
to 24
Inhaled corticosteroids
Beclomethasone 50-400 (MDI & DPI) 0.2-0.4
Budesonide 100, 200, 400 (DPI) 0.20. 0.25, 0.5
Fluticasone 50-500 (MDI & DPI)
Combination long-acting beta
2
-agonists plus corticosteroids in one inhaler
Formoterol/Budesonide
4.5/160 (MDI)
9/320 (DPI)
Formoterol/mometasone 10/200, 10/400 (MDI)
Salmeterol/Fluticasone
50/100, 250, 500 (DPI)
25/50, 125, 250 (MDI)
Vilanterol/Fluticasone
furoate
25/100 (DPI)
Systemic corticosteroids
Prednisone 5-60 mg (Pill)
Methyl-prednisolone 4, 8, 16 mg (Pill)
Phosphodiesterase-4 inhibitors
Roflumilast 500 mcg (Pill) 24
MDI=metered dose inhaler; DPI=dry powder inhaler; SMI=soft mist inhaler
*Not all formulations are available in all countries; in some countries, other formulations may be available.
Formoterol nebulized solution is based on the unit dose vial containing 20 mcg in a volume of 2.0 ml
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
-
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
GOLD 2014 source documents are at www.goldcopd.org
Global Initiative for Chronic Obstructive Lung Disease
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
-
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
You might also like
- Be Bold With GOLD - An Update From The Late 2011: Where Do The Staging and Handling Go From Here?Document39 pagesBe Bold With GOLD - An Update From The Late 2011: Where Do The Staging and Handling Go From Here?sintinNo ratings yet
- GOLD 2011 Guideline SummaryDocument25 pagesGOLD 2011 Guideline SummaryebramnainggolanNo ratings yet
- COPD Guide: Diagnosis, Assessment, TreatmentDocument34 pagesCOPD Guide: Diagnosis, Assessment, TreatmentFa9v 1No ratings yet
- COPD NEW GuidelinesDocument45 pagesCOPD NEW GuidelinesMuhammad HaneefNo ratings yet
- Copd - 2 Penting 13Document14 pagesCopd - 2 Penting 13Rahmat MuliaNo ratings yet
- Gold and Gina Guideline For Copd and AsthmaDocument56 pagesGold and Gina Guideline For Copd and AsthmaSomnath Das GuptaNo ratings yet
- COPD Clinical Management Review Provides GuidanceDocument11 pagesCOPD Clinical Management Review Provides GuidanceAlejandro Kanito Alvarez SNo ratings yet
- 2019 Copd OutpatientsDocument61 pages2019 Copd OutpatientsArshamNo ratings yet
- Stable COPDDocument42 pagesStable COPDFandi ApriyanNo ratings yet
- COPDDocument38 pagesCOPDMuhammad SulfikarNo ratings yet
- 006 COPD - Lecture StudentsDocument52 pages006 COPD - Lecture Studentszyz6639No ratings yet
- Case Presentation On Copd - Shaik NazmaDocument29 pagesCase Presentation On Copd - Shaik NazmaDeepikaNo ratings yet
- Key Points on Diagnosing and Assessing Severity of COPDDocument12 pagesKey Points on Diagnosing and Assessing Severity of COPDfallenczarNo ratings yet
- Chronic Obstructive Pulmonary Disease (COPD) : Assistant Sukhonos NDocument17 pagesChronic Obstructive Pulmonary Disease (COPD) : Assistant Sukhonos NRayan Rayan darwishNo ratings yet
- COPD2019Document9 pagesCOPD2019ClintonNo ratings yet
- COPD Exacerbations - Clinical Manifestations and Evaluation - UpToDateDocument20 pagesCOPD Exacerbations - Clinical Manifestations and Evaluation - UpToDateJúlia PompeuNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument30 pagesChronic Obstructive Pulmonary DiseaseAnam MirNo ratings yet
- COPD Updated Guidelines and Newer TherapiesDocument90 pagesCOPD Updated Guidelines and Newer TherapiesVlad Constantin100% (1)
- COPD Student Lec DR Atef Alkarn 6-2022Document42 pagesCOPD Student Lec DR Atef Alkarn 6-2022mohamed albnaNo ratings yet
- Copd (Chronic Obstructive Pulmonary Disease) : GOLD, 2015Document11 pagesCopd (Chronic Obstructive Pulmonary Disease) : GOLD, 2015ratubalqisanasaNo ratings yet
- Management of COPDDocument21 pagesManagement of COPDikrimahsbNo ratings yet
- COPD Assessment and ManagementDocument161 pagesCOPD Assessment and ManagementClarisse Nicole TanNo ratings yet
- Jover Reflection PaperDocument2 pagesJover Reflection PaperGwen Myles JoverNo ratings yet
- GOLD PocketGuide 2011 Jan18Document32 pagesGOLD PocketGuide 2011 Jan18Teresa ChangNo ratings yet
- Recentadvancesinthe Managementofacute Exacerbationsofchronic ObstructivepulmonarydiseaseDocument16 pagesRecentadvancesinthe Managementofacute Exacerbationsofchronic Obstructivepulmonarydiseaseadek07No ratings yet
- 2020 REPORT: Global Strategy For The Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary DiseaseDocument53 pages2020 REPORT: Global Strategy For The Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary DiseaseManoj GhimireNo ratings yet
- Chronic Obstructive Pulmonary Disease Study (COPDDocument12 pagesChronic Obstructive Pulmonary Disease Study (COPDHamid RazaNo ratings yet
- CopdDocument5 pagesCopdapi-719803017No ratings yet
- Abnormal Lung Physiology Through Spirometry: A Comprehensive Overview of COPDDocument12 pagesAbnormal Lung Physiology Through Spirometry: A Comprehensive Overview of COPDK.Sathvik. AcharyaNo ratings yet
- EBM COPD Dan Gagal Napas - EditDocument57 pagesEBM COPD Dan Gagal Napas - EditNiarti Ulan Sari SiarnuNo ratings yet
- Chronic Obstructive Pulmonary Disease: Saja QuzmarDocument28 pagesChronic Obstructive Pulmonary Disease: Saja Quzmarkolakav107No ratings yet
- Gold Copd 2013 GuidelinesDocument3 pagesGold Copd 2013 GuidelinesMatthewNo ratings yet
- Chronic Obstructive Pulmonary Disease: Laily Hidayati, S.Kep., NS., M.KepDocument55 pagesChronic Obstructive Pulmonary Disease: Laily Hidayati, S.Kep., NS., M.KepGlory Stefanny NorotumilenaNo ratings yet
- COPD Case StudyDocument22 pagesCOPD Case StudyAnonymous HNTNhspNo ratings yet
- Anaesthesia and CopdDocument7 pagesAnaesthesia and CopdAshish PandeyNo ratings yet
- Onbrez June 2014Document32 pagesOnbrez June 2014NateStephBarnardNo ratings yet
- Diskusi Topik 2 (PPOK) - Nafisa Zulpa Elhapidi - 406202067Document59 pagesDiskusi Topik 2 (PPOK) - Nafisa Zulpa Elhapidi - 406202067nafisa zulfaelNo ratings yet
- 05 j.1532-5415.2007.01332.x EPOC PDFDocument7 pages05 j.1532-5415.2007.01332.x EPOC PDFAlejandroNo ratings yet
- COPD3Document77 pagesCOPD3mohammedNo ratings yet
- COPDDocument11 pagesCOPDSherree HayesNo ratings yet
- Bio-Ethical Issue and 3 ArticlesDocument7 pagesBio-Ethical Issue and 3 ArticlesSittie Nashieva A. UsmanNo ratings yet
- Gold Copd 2017Document4 pagesGold Copd 2017ChrisNo ratings yet
- "A Study ON Chronic Obstructive Pulmonary Diseases": Ananta Institute of Medical Sciences and ResearchDocument13 pages"A Study ON Chronic Obstructive Pulmonary Diseases": Ananta Institute of Medical Sciences and ResearchHamid RazaNo ratings yet
- Key Learning Points - GOLD COPD 2020 Report - Key Learning Points - Guidelines in PracticeDocument12 pagesKey Learning Points - GOLD COPD 2020 Report - Key Learning Points - Guidelines in PracticeHJ GNo ratings yet
- Analysis of Sputum Markers in The Evaluation of Lung Inflammation and Functional Impairment in Symptomatic Smokers and COPD PatientsDocument10 pagesAnalysis of Sputum Markers in The Evaluation of Lung Inflammation and Functional Impairment in Symptomatic Smokers and COPD PatientsAndreea MoalesNo ratings yet
- Copd Case StudyDocument6 pagesCopd Case StudyChrischia Yvonne GualbertoNo ratings yet
- Copd in Primary CareDocument27 pagesCopd in Primary CarerobyalfNo ratings yet
- COPD Guide Covers Causes, Symptoms, DiagnosisDocument5 pagesCOPD Guide Covers Causes, Symptoms, DiagnosisElvando SimatupangNo ratings yet
- COPD Risk Factors & Spirometry StagingDocument38 pagesCOPD Risk Factors & Spirometry StagingKudingLimMingYaoNo ratings yet
- Topic Related Activity Format-COPDDocument27 pagesTopic Related Activity Format-COPDLiza M. KharroubiNo ratings yet
- COPDDocument11 pagesCOPDBahaa Shaaban67% (3)
- Gold 2019Document43 pagesGold 2019Hayatillah Natasya100% (1)
- Chronic Obstructive Pulmonary Disease: Continuing Education ActivityDocument11 pagesChronic Obstructive Pulmonary Disease: Continuing Education ActivityBBD BBDNo ratings yet
- PpokDocument6 pagesPpokSatria UtomoNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument28 pagesChronic Obstructive Pulmonary DiseaseZhe Kang LimNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument23 pagesChronic Obstructive Pulmonary DiseaseLe RobertNo ratings yet
- Demystifying COVID-19: Understanding the Disease, Its Diagnosis. and TreatmentFrom EverandDemystifying COVID-19: Understanding the Disease, Its Diagnosis. and TreatmentNo ratings yet
- Manajemen Ulkus Kaki Diabetik PDFDocument28 pagesManajemen Ulkus Kaki Diabetik PDFCaca IchamioNo ratings yet
- Tere Liye - HujanDocument17 pagesTere Liye - HujanSesilia Sri Yanti GaddyNo ratings yet
- Kegawatdaruratan Diabetes Melitus: Terapi Insulin IntravenaDocument27 pagesKegawatdaruratan Diabetes Melitus: Terapi Insulin IntravenaSesilia Sri Yanti GaddyNo ratings yet
- Vertigo Blok15Document23 pagesVertigo Blok15Mul YaniNo ratings yet
- Sat-Asatkaryavada in DiseaseDocument7 pagesSat-Asatkaryavada in DiseaseSamhitha Ayurvedic ChennaiNo ratings yet
- Brain Implant Victims - MCRAISDocument11 pagesBrain Implant Victims - MCRAISProjekt_-stop-tortureNo ratings yet
- 1536106348Document144 pages1536106348Saman SarKoNo ratings yet
- Genetic Polymorphism of Cyp2d6Document23 pagesGenetic Polymorphism of Cyp2d6Oscar Velasco0% (1)
- Swami Paramarthananda's Talks on Self-KnowledgeDocument332 pagesSwami Paramarthananda's Talks on Self-Knowledgemuralipmd100% (1)
- Pathophysiology Tia VS CvaDocument6 pagesPathophysiology Tia VS CvaRobby Nur Zam ZamNo ratings yet
- Child Health Course: Amref Directorate of Learning SystemsDocument25 pagesChild Health Course: Amref Directorate of Learning SystemsEirehc Eam Aiboro SamorNo ratings yet
- BONE Level 2-BDocument60 pagesBONE Level 2-Bjefri banjarnahorNo ratings yet
- Informed Consent TimetableDocument11 pagesInformed Consent TimetableAkita C.No ratings yet
- Risk Management in Medical LaboratoriesDocument32 pagesRisk Management in Medical Laboratoriesapanisile14142No ratings yet
- Med school memes that are medically funnyDocument1 pageMed school memes that are medically funnylostinparadise0331No ratings yet
- Akshita Country EditedDocument41 pagesAkshita Country EditedniranjanNo ratings yet
- Shatavari (Asparagus Racemosus), Jivanti (Leptadenia Reticulata) and Methi (Trigonella Foenum-Graecum) : The Herbal Galactogogues For RuminantsDocument7 pagesShatavari (Asparagus Racemosus), Jivanti (Leptadenia Reticulata) and Methi (Trigonella Foenum-Graecum) : The Herbal Galactogogues For RuminantsSanjay C. ParmarNo ratings yet
- Datex-Ohmeda Aespire 7900 - Maintenance and Troubleshooting PDFDocument118 pagesDatex-Ohmeda Aespire 7900 - Maintenance and Troubleshooting PDFJosé Morales Echenique100% (1)
- Minutes Prac Meeting 26 29 October 2020 - enDocument80 pagesMinutes Prac Meeting 26 29 October 2020 - enAmany HagageNo ratings yet
- Classification of Endodontic FlapsDocument23 pagesClassification of Endodontic FlapsDilu DavisNo ratings yet
- Annotated BibliographyDocument3 pagesAnnotated Bibliographyicemocha6910% (1)
- Estevan Jimenez Patient Clinical Report ForDocument7 pagesEstevan Jimenez Patient Clinical Report ForIsrael MelloNo ratings yet
- Modern Wound Care Practical Aspects of Non Interventional Topical Treatment of Patients With Chronic WoundsDocument14 pagesModern Wound Care Practical Aspects of Non Interventional Topical Treatment of Patients With Chronic WoundsDauz ArashNo ratings yet
- The Endocrine Pancreas: Regulation of Carbohydrate MetabolismDocument61 pagesThe Endocrine Pancreas: Regulation of Carbohydrate MetabolismFatima OngNo ratings yet
- Risk of Ovarian Cancer Algorithm (ROCA) Using Serial CA 125Document9 pagesRisk of Ovarian Cancer Algorithm (ROCA) Using Serial CA 125primadian atnaryanNo ratings yet
- Occlusion: DR - Inas Abdul SattarDocument33 pagesOcclusion: DR - Inas Abdul SattarKhanh NguyễnNo ratings yet
- Medicine, Coptic.: Chronological Table of Ostraca and Papyri Dealing With MedicineDocument7 pagesMedicine, Coptic.: Chronological Table of Ostraca and Papyri Dealing With MedicinePaula VeigaNo ratings yet
- Low Fat Diet PlanDocument2 pagesLow Fat Diet Planmelissa_glancNo ratings yet
- Effectiveness of Planned Teaching Programme On The Knowledge of Endotracheal Suctioning Among Staff Nurses Working in IcuDocument6 pagesEffectiveness of Planned Teaching Programme On The Knowledge of Endotracheal Suctioning Among Staff Nurses Working in IcuRizwan KhanNo ratings yet
- Health and its failure: Causes, Types, and Prevention of DiseasesDocument9 pagesHealth and its failure: Causes, Types, and Prevention of DiseasesAbhimanyu BahreeNo ratings yet
- Medical ReceptionistDocument4 pagesMedical ReceptionistM LubisNo ratings yet
- Latihan Un Bahasa Inggris 2018: The Following Text Is For Questions 1 and 2Document9 pagesLatihan Un Bahasa Inggris 2018: The Following Text Is For Questions 1 and 2AWDNo ratings yet
- Oral Physio FinalDocument34 pagesOral Physio FinaldraggarwalNo ratings yet
- Aplicación FacialDocument28 pagesAplicación FacialJuan Esteban GómezNo ratings yet