Professional Documents
Culture Documents
Traumatic Brain Injury
Uploaded by
Lharra Cagulada-PostranoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Traumatic Brain Injury
Uploaded by
Lharra Cagulada-PostranoCopyright:
Available Formats
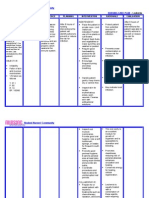
Traumatic Brain Injury
Source http://nursingcrib.com/nursing-notes-reviewer/medical-surgical-
nursing/traumatic-brain-injury/
Also known as head injury.
Is the disruption of normal brain function due to trauma-related injury resulting in compromised
neurologic function resulting in focal or diffuse symptoms.
Motor vehicle accidents are the most common etiology of injury.
Etiology And Pathophysiology
Types of Traumatic Brain Injury
Concussion transient interruption in brain activity; no constructural injury noted on radiographics.
Cerebral contusion bruising of brain with associated swelling.
Intracerebral hematoma bleeding into the brain tissue commonly associated with edema.
Epidural hematoma blood between the inner table of the skull and dura.
Subdural hematoma blood between the dura and arachnoid caused by bleeding commonly associated
with additional brain injury.
Diffuse axonal injury axonal tears within the white matter of the brain.
Assessment
Disturbance in level of consciousness from slightly drowsy to unconscious.
Headache, vertigo, agitation, and restlessness.
Cerebrospinal fluid leakage at ears and nose, which may indicate skull fracture.
Contusions about eyes and ears indicating skull fractures.
Irregular respirations
Cognitive deficit
Pupillary abnormality
Sudden onset of neurologic deficits
Otorrhea indicating posterior fossa skull fracture
Rhinorrhea indicating anterior fossa skul fracture.
Nursing Diagnosis
Risk for injury related to complications of head injury.
Acute pain related to altered brain or skull tissue.
Diagnostic Evaluation
CT identifies and localizes lesions, cerebral edema, and bleeding.
Skull and cervical spine X-ray identify fracture and displacement.
Complete blood count, coagulation profile, electrolyte levels, serum osmolarity, arterial blood gases,
and other laboratory tests monitor for complications.
Neuropsychological test during rehabilitation phase determine cognitive deficits.
Nursing Interventions
Maintain ICP monitoring, as indicated, and report abnormalities.
Maintain patent airway; assist with intubation and ventilatory assistance is needed.
Turn the patient every 2 hours and encourage coughing and deep breathing.
Apply firm pressure over puncture site for subdural trap, and observe for drainage and dressing.
Suction the patient as needed.
Institute measures to prevent increased ICP or other neurovascular compromise.
Feed the patient as soon as possible after a head injury and administer histamine-2 blockers to prevent
gastric ulceration and hemorrhage from gastric acid hypersecretion.
If the patient is unable to swallow, provide enteral feedings after bowel sounds have returned.
Elevate the head of the bed after feedings, and check residuals to prevent aspiration.
Monitor respiratory rate, depth, and pattern of respirations.
Complications
Infections
Increased intracranial pressure
Posttraumatic seizure disorder
Permanent neurologic deficits
Persistent sympathetic storming
SIADH
Death
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Special Test For All JointsDocument42 pagesSpecial Test For All JointsVinothini Adaikkalasamy91% (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Nursing Care Plan LeukemiaDocument2 pagesNursing Care Plan Leukemiaderic87% (30)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- NCLEX Nursing Exam Cram SheetDocument9 pagesNCLEX Nursing Exam Cram SheetJodie OrangeNo ratings yet
- Concept of SafetyDocument3 pagesConcept of SafetyDave100% (1)
- Disaster Management and Nurses RoleDocument27 pagesDisaster Management and Nurses RolePrincess Louise ViceralNo ratings yet
- Iii. Nursing Care PlansDocument13 pagesIii. Nursing Care PlansLharra Cagulada-Postrano100% (1)
- Clinical Diagnosis and Management of Ocular TraumaDocument372 pagesClinical Diagnosis and Management of Ocular TraumaMatías PierottiNo ratings yet
- HAZARD AND INCIDENT REPORTDocument2 pagesHAZARD AND INCIDENT REPORTAnku Kingsley Etornam100% (1)
- Exceeds Standards Meets Standards Below Standards Possible Points Score 5 3 2 5Document1 pageExceeds Standards Meets Standards Below Standards Possible Points Score 5 3 2 5Lharra Cagulada-PostranoNo ratings yet
- Case Study AnalysisDocument1 pageCase Study AnalysisLharra Cagulada-PostranoNo ratings yet
- Rubric: Video Project On The Routes of Medication AdministrationDocument2 pagesRubric: Video Project On The Routes of Medication AdministrationLharra Cagulada-PostranoNo ratings yet
- Ra 9173Document14 pagesRa 9173Lharra Cagulada-PostranoNo ratings yet
- Community Organizing: Ensuring Health in The Hands of The PeopleDocument22 pagesCommunity Organizing: Ensuring Health in The Hands of The PeopleLharra Cagulada-Postrano100% (2)
- Nursing Law and EthicsDocument14 pagesNursing Law and Ethicsaleth joyce cubacub96% (25)
- QUIZDocument16 pagesQUIZLharra Cagulada-PostranoNo ratings yet
- Flush - 1655 19% No Toilet - 21 0%Document5 pagesFlush - 1655 19% No Toilet - 21 0%Lharra Cagulada-PostranoNo ratings yet
- Filariasis Control ProgramDocument17 pagesFilariasis Control ProgramLharra Cagulada-PostranoNo ratings yet
- Rubric: Video ProjectDocument2 pagesRubric: Video ProjectLharra Cagulada-PostranoNo ratings yet
- Table of ContentsDocument9 pagesTable of ContentsLharra Cagulada-PostranoNo ratings yet
- Improper Delegation Case StudyDocument31 pagesImproper Delegation Case StudyLharra Cagulada-PostranoNo ratings yet
- Normal ValuesDocument5 pagesNormal ValuesPeter Lucky TurianoNo ratings yet
- Spot MapDocument1 pageSpot MapLharra Cagulada-PostranoNo ratings yet
- Preeclampsia, Severe, UncontrolledDocument22 pagesPreeclampsia, Severe, UncontrolledLharra Cagulada-PostranoNo ratings yet
- DOCTORs OrderDocument2 pagesDOCTORs OrderLharra Cagulada-Postrano100% (1)
- Student Leaders Attend Third Philippine I TransformDocument1 pageStudent Leaders Attend Third Philippine I TransformLharra Cagulada-PostranoNo ratings yet
- Traumatic Brain InjuryDocument3 pagesTraumatic Brain InjuryLharra Cagulada-PostranoNo ratings yet
- Case Study ResearchDocument5 pagesCase Study ResearchLharra Cagulada-PostranoNo ratings yet
- Family Coping Index..Document3 pagesFamily Coping Index..Lharra Cagulada-PostranoNo ratings yet
- Research Methods Books Held in MIRCDocument4 pagesResearch Methods Books Held in MIRCMauton WhenuNo ratings yet
- Pathophysio (Hemophilia)Document2 pagesPathophysio (Hemophilia)Lharra Cagulada-PostranoNo ratings yet
- Theoretical FrameworkDocument12 pagesTheoretical FrameworkLharra Cagulada-Postrano100% (1)
- Emergency JournalsDocument20 pagesEmergency JournalsLharra Cagulada-PostranoNo ratings yet
- Political System Ppt. (Final)Document40 pagesPolitical System Ppt. (Final)Lharra Cagulada-PostranoNo ratings yet
- Downward Movement - Left Hand Only: (Figure 3-7Document20 pagesDownward Movement - Left Hand Only: (Figure 3-7mamun31No ratings yet
- Femoral Neck FractureDocument28 pagesFemoral Neck FractureayuegpNo ratings yet
- FlipCutter A Pin That Changes Arthroscopic Tunnel Drilling Forever...Document12 pagesFlipCutter A Pin That Changes Arthroscopic Tunnel Drilling Forever...andrelbportoNo ratings yet
- Acutepain PneumoniaDocument3 pagesAcutepain PneumoniaJoy SalvadorNo ratings yet
- Locked in SyndromeDocument52 pagesLocked in SyndromeFarrukh Ali KhanNo ratings yet
- The Vanishing Throne: Book Two of The Falconer Trilogy (Excerpt)Document24 pagesThe Vanishing Throne: Book Two of The Falconer Trilogy (Excerpt)ChronicleBooks0% (1)
- ww11701 Hunter - The - Reckoning + Vampire - The - Masquerade - Fiction - Predator - Prey - Book 2 - Judge PDFDocument288 pagesww11701 Hunter - The - Reckoning + Vampire - The - Masquerade - Fiction - Predator - Prey - Book 2 - Judge PDFPawel Vlad LatoNo ratings yet
- Cartilage LectureDocument31 pagesCartilage LecturemalyaaNo ratings yet
- Understanding Child Abuse: Causes, Signs, SolutionsDocument7 pagesUnderstanding Child Abuse: Causes, Signs, Solutionsdew23No ratings yet
- VIPower: VIPer22A Dual Output Reference Board 90 To 264 VAC Input, 10W OutputDocument20 pagesVIPower: VIPer22A Dual Output Reference Board 90 To 264 VAC Input, 10W OutputLullaby summerNo ratings yet
- Volume 1 Issue 1 Page 1-5 Morphometric Study of The Pedicles of Dried Adult Human Lumbar VertebraeDocument5 pagesVolume 1 Issue 1 Page 1-5 Morphometric Study of The Pedicles of Dried Adult Human Lumbar VertebraeEditorsNo ratings yet
- Chapter 13: Support Surfaces and Special Beds Perry Et Al.: Clinical Nursing Skills & Techniques, 9th Edition Multiple ChoiceDocument11 pagesChapter 13: Support Surfaces and Special Beds Perry Et Al.: Clinical Nursing Skills & Techniques, 9th Edition Multiple ChoiceComfort YaaNo ratings yet
- Quiz OlpcDocument4 pagesQuiz OlpcAdriane TornoNo ratings yet
- War Essay 2Document12 pagesWar Essay 2api-280869491No ratings yet
- 6 - Nutrition in Surgical PatientsDocument12 pages6 - Nutrition in Surgical PatientsAnonymous WjMMmcm1gNo ratings yet
- Traction (Orthopedics)Document2 pagesTraction (Orthopedics)Sunil PatelNo ratings yet
- 12 - Sps. Flores v. Sps. Pineda, G.R. No. 158996, Nov. 14, 2008 PDFDocument1 page12 - Sps. Flores v. Sps. Pineda, G.R. No. 158996, Nov. 14, 2008 PDFVia Rhidda ImperialNo ratings yet
- Joint Pain - ApproachDocument32 pagesJoint Pain - ApproachHassan Bin AjmalNo ratings yet
- Kinesiology For Occupational Therapy-32-50Document19 pagesKinesiology For Occupational Therapy-32-50birjuNo ratings yet
- Lifern’s Anatomy: Limbs & TrunkDocument161 pagesLifern’s Anatomy: Limbs & TrunkPauline MakahamadzeNo ratings yet
- Retrograde Urethrography Examination in Penile Fracture: Case ReportDocument3 pagesRetrograde Urethrography Examination in Penile Fracture: Case Reportsofia ayu lestariNo ratings yet
- CBLM - LO#3 Clean Public Areas, Facilities & Equipment"Document48 pagesCBLM - LO#3 Clean Public Areas, Facilities & Equipment"Buena Jaro80% (25)
- 45 Web BK, Karate JutsuDocument71 pages45 Web BK, Karate Jutsudiamond68100% (5)
- Yogasana Seq 1.0Document90 pagesYogasana Seq 1.0deesahNo ratings yet
- BandagingDocument6 pagesBandagingwinkerbellNo ratings yet
- Acknowledging help for a first aid projectDocument9 pagesAcknowledging help for a first aid projectAshish Goel100% (1)