Professional Documents
Culture Documents
Recurrent Henoch SCH Nlein Purpura in Children.6
Uploaded by
gaatgaatOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Recurrent Henoch SCH Nlein Purpura in Children.6
Uploaded by
gaatgaatCopyright:
Available Formats
ORIGINAL ARTICLES
Recurrent Henoch-Schonlein Purpura in Children
Dario Prais, MD, Jacob Amir, MD, and Moshe Nussinovitch, MD
Background: Henoch-Schonlein purpura (HSP), also known as
anaphylactoid purpura is a clinically recognizable systemic disorder
occurring in children, mainly from ages 3 to 10 years.
Objectives: To describe the clinical, epidemiological, and laboratory findings in a group of patients with recurrent HSP, admitted to
a tertiary pediatric center.
Methods: Retrospective analysis of medical records of patients
hospitalized due to HSP between 1969 and 2004.
Results: Two hundred sixty children (56.7% males) were hospitalized due to HSP, 7 (2.7%) more than once. There were no statistically significant differences in demographic or clinical characteristics between the patients with 1 event of HSP and patients with
recurrence. Mean age of the subgroup with recurrence was 3.67
years (10 months to 7.4 years) at the first episode, and 5.03 years
(2.210 years) at the second one, with a mean lag period of 13.5
2.8 months (range 226). The duration of the recurrent clinical
symptoms ranged from 9 to 30 days, and in 72% of those patients,
resolution took more than 14 days.
Conclusion: In our inpatient population, no clinical or laboratory
characteristics were found to be predictive of recurrence; the second
episode was longer than the first and the lag period between the 2
episodes was substantially longer than previously reported. Hospital
admissions for recurrent HSP are not common. Nevertheless, a good
prognosis was the rule of our admitted patients.
Key Words: vasculitis, anaphylactoid, recurrence, prognosis,
Henoch-Schonlein
(J Clin Rheumatol 2007;13: 2528)
enoch-Schonlein purpura (HSP), also known as anaphylactoid purpura is a clinically recognizable systemic
disorder occurring in children, mainly from ages 3 to 10 years
and in young adults.1 It is characterized by a distinctive
purpuric rash distributed symmetrically over the buttocks and
lower extremities, but sometimes involving the upper extremities, trunk, and face. Systemic symptoms and signs include
edema (particularly in the younger age group),2 joint involvement (arthralgia or arthritis), gastrointestinal manifestations
From the Department of Pediatrics C, Schneider Childrens Medical Center
of Israel, Petah Tiqva and Sackler Faculty of Medicine, Tel Aviv
University, Tel Aviv, Israel.
Reprints: D. Prais, MD, Department of Pediatrics C, Schneider Childrens
Medical Center of Israel, 49202 Petah Tiqva, Israel. E-mail: dariop@
clalit.org.il
Copyright 2007 by Lippincott Williams & Wilkins
ISSN: 1076-1608/07/1301-0025
DOI: 10.1097/01.rhu.0000255692.46165.19
(abdominal pain, blood diarrhea), and renal damage (hematuria, nephritis). In rare cases, there may be central nervous
system, scrotal, pulmonary, or cardiac complications. Diagnosis is usually made clinically. Skin biopsy, which typically
shows leukocytoclastic vasculitis, is generally unnecessary.
The underlying pathologic process of HSP is an immunecomplex-mediated inflammation of the small vessels.3 The
site, extent, and severity of vessel involvement in the individual patient determine the clinical picture. Although the
nature of the immunologic reaction is unclear, the frequent
reports of upper respiratory tract infection or streptococcal
pharyngitis preceding the onset of symptoms suggest a hypersensitivity phenomenon.
There are several reports in the literature of long-term,
recurrent HSP. Most concern the recurrence of renal impairment. Full-blown recurrent HSP, with the characteristic clinical presentation including the distinctive purpuric rash, has
been described in only a few cases.4 Its incidence in the
pediatric population is unknown.
The aim of the present study was to report the clinical,
epidemiological, and laboratory findings of patients with
recurrent HSP admitted to a tertiary pediatric center during
the past 30 years.
PATIENTS AND METHODS
The medical records of all children discharged from our
tertiary pediatric medical center with a diagnosis of HSP from
1969 to 2004 were analyzed. The diagnosis was confirmed by
clinical, laboratory, and in some cases, pathology studies.
Inclusion criteria were presence of nonthrombocytopenic palpable purpura with or without systemic involvement, characteristic purpuric rash, and absence of any other disease or
medication known to cause purpura. Since the diagnosis of
HSP is mainly clinical, patients who did not undergo skin
biopsy were not excluded; however, patients had to fulfill the
American College of Rheumatologys criteria for diagnosis
of HSP.5 Demographic data associated clinical manifestations, and laboratory, radiologic, and pathologic findings
were summarized.
Patients diagnosed more than once with HSP were
classified as having recurrent HSP. The inclusion criteria for
this subgroup were the same as for all patients with HSP, in
addition to the reappearance of the characteristic purpuric
rash (with or without associated symptoms), following a
previous complete remission. The medical records of the
patients with recurrent disease were rechecked to determine
that diagnosis was confirmed. The patients were followed in
the outpatient clinic or by telephone. Data were analyzed for
JCR: Journal of Clinical Rheumatology Volume 13, Number 1, February 2007
25
JCR: Journal of Clinical Rheumatology Volume 13, Number 1, February 2007
Prais et al
statistical significance with the Fisher exact test and Student
t test.
On long-term follow-up (at least 2 years), no further
recurrent episodes were reported, and no complications or
persistent symptoms were found.
RESULTS
During the study period, 260 children were hospitalized
with HSP; 56.7% males and 43.3% females; mean age at
presentation was 5.7 2.6 years (range 114.8 years). Mean
duration of the skin involvement was 11.5 days (range 327
days); 12% of patients showed skin involvement for more
than 15 days. Systemic involvement was arthritis and arthralgia in 68%, abdominal pain in 59%, hematuria or proteinuria
in 35%, and impaired renal function or acute renal failure in
3%. Documented evidence of a previous bacterial or viral
infection was found in 12% of patients; 8 patients had
positive antistreptolysin O test (of the 193 patients tested,
4%). Immune-globulin A levels were elevated in 2 of the 6
examined patients.
Recurrent HSP
Seven of the 260 patients were hospitalized more than
once for HSP (2.7%). Their clinical and epidemiological
characteristics are presented in Table 1. There were no
statistically significant differences between the entire patient
group and the recurrence subgroup in sex or age distribution,
clinical presentation, systemic involvement, duration of
symptoms, and need for medical treatment during the first
episode (P 0.1, data not shown). All patients reported a
nonspecific viral illness during the month before presentation.
Forty-three percent of the recurrence subgroup were
male. Mean age at the first episode was 3.67 2.08 years
(range 10 months to 7.4 years); at the second episode, 5.03
2.6 years (range 2.210 years). Mean lag period between the
2 episodes was 13.5 2.8 months (range 226 months).
During the second episode, all patients had the characteristic cutaneous involvement and abdominal pain of differing severity at various stages of the disease. Arthralgia was
noted in 5/7, hematuria in 3/7, proteinuria in 2/7, bloody
stools and vomiting in 1 patient each. Laboratory studies
were not diagnostic: mean leukocyte count was 9800 800
cells/mm3 (range 8300 12,200); C-reactive protein level,
erythrocyte sedimentation rate, immunoglobulin levels, and
coagulation test were within normal range. Normal findings
were found on urinalysis, except for 2 cases of microhematuria and mild proteinuria (150 mg/24 hours), and on stool
examination for occult blood, except for 1 case of overt
bloody diarrhea. No cases of severe renal impairment were
seen. Other serological tests (antinuclear antibody, antineutrophilic cytoplasmic antibody, anticardiolipin) were negative. Antistreptolysin O was positive in 1 child.
Because of the recurrent nature of the episodes and the
need to confirm the diagnosis, skin biopsy was performed in
5 patients. All showed leukocytoclastic vasculitis. Immunoglobulin A deposits were present in 4 patients, and C3
deposits in 1. Corticosteroid treatment (2 mg/kg/d) was prescribed in 2 patients: 1 with bloody diarrhea and the other
with severe abdominal pain.
The duration of the clinical symptoms ranged from 9 to
30 days (mean 17.85 days); in 72% of the patients, resolution
took 15 days or more.
26
DISCUSSION
HSP, the most common acute vasculitis affecting children, is usually clinically diagnosed on the basis of the classic
triad of nonthrombocytopenic purpura, abdominal symptoms
(Henoch), and joint complaints (Schonlein). Full-blown
recurrent HSP, with the characteristic clinical presentation including the distinctive purpuric rash, was previously
reported,4 but the incidence in the pediatric population remains
unknown.
We describe 7 cases of recurrent HSP requiring rehospitalization in our pediatric population. All patients had the
characteristic purpuric rash and abdominal pain. Arthralgia,
renal involvement, and gastrointestinal bleeding were less
frequent. Full recovery was the rule, with no sequelae.
Most of the few published reports of recurring HSP
cases described unusual or atypical presentations, such as
Wiskott-Aldrich syndrome in an 8-year-old boy6; abnormally long intervals between onset of abdominal pain and
skin rash (24 weeks) in a 7-year-old boy7; tube-ovarian
abscesses in a 15-year-old girl8; recurrent testicular swelling
and orchitis in a 4-year-old boy.9 Nathawani et al4 described
5 patients with recurrent HSP, including 2 children: a 16year-old who experienced the second episode 7 years after the
first, and a 3-year-old with a recurrent episode of nephritis
following a throat infection.
Recurrence of HSP commonly occurs within 23
months of the primary episode. The incidence may be higher
than expected, since some cases of recurrence may be misdiagnosed as part of a prolonged course of primary HSP.
Saulsbury1 reported a 33% incidence of recurrence, defined
as reappearance of the characteristic rash or other symptoms
following resolution of the disease for at least 2 weeks. In 16
of their patients (48%), recurrence occurred during the first
month, and only 2 had a recurrence beyond 4 months.
Similarly, Trapani et al reported a recurrence of purpura in
35% of patients, occurring within 12 months after the acute
phase of the disease.10 When comparing this to our data, it
must be emphasized that we included only rehospitalized
patients.
In general, the recurrent episode tended to mimic the
original one. Our population is unique in 2 aspects: the lag
period between the 2 episodes of HSP was substantially
longer than in other reports (mean 13.5 2.8 months), and
the second episode (especially the skin rash) tended to be
longer than the first. However, in our series, similar to
previous studies, there were no significant differences in the
clinical presentation between the first and second episodes.
The incidence of systemic involvement was also comparable.
There were also no significant differences in the clinical
presentation of the first episode between the entire group of
patients and the subgroup with recurrent HSP. Thus, no
specific characteristics of the first episode could be identified
that would predict patients at risk for recurrences. As in other
2007 Lippincott Williams & Wilkins
2007 Lippincott Williams & Wilkins
F
M
M
3
4
5
3.67*
2.08
2.6
3.5
7.4
2.5
0.8
Age
(yr)
Streptococcal
pharyngitis
Viral
Viral
Viral
Previous
Infection
Arthritis
AP, renal
AP, renal,
arthritis
AP, renal,
arthritis
AP
AP
AP, renal,
arthritis
Systemic
Symptoms
AP, abdominal pain; URTI, upper respiratory tract infection.
*P 0.005 between 1st and 2nd episode.
Mean
SD
Sex
Patient
No.
9.14*
4.1
13
12
5
7
15
Duration
Symptoms (d)
First Episode
No
Yes
No
Yes
Yes
No
No
Skin
Biopsy
Supportive
Steroids
Supportive
Supportive
Steroids
Supportive
Supportive
Treatment
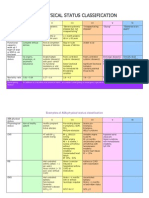
TABLE 1. Clinical and Epidemiological Characteristics of Patients with Recurrent HSP
5.03*
2.6
5.5
2.8
5
10
3.75
2.2
Age
(yr)
Pharyngitis
Viral
Viral
URTI
Viral
URTI
Previous
Infection
AP, hematuria
AP, arthralgia
AP, arthritis,
proteinuria,
bloody stools
AP, arthralgia,
microhematuria
Arthralgia,
microhematuria,
proteinuria
AP
AP, arthritis
Systemic
Symptoms
17.85*
7.7
20
9
24
30
18
15
Duration
Symptoms (d)
Second Episode
No
Yes
No
Yes
Yes
Yes
Yes
Skin
Biopsy
Supportive
Supportive
Supportive
Supportive
Steroids
Steroids
Supportive
Treatment
JCR: Journal of Clinical Rheumatology Volume 13, Number 1, February 2007
Recurrent Henoch-Schonlein Purpura in Children
27
JCR: Journal of Clinical Rheumatology Volume 13, Number 1, February 2007
Prais et al
studies, our patients, including those with recurrent diseases,
had a good prognosis.1,7,9,10
Our lower incidence of recurrence compared with previous reports may be explained by the longer lag period
between episodes in our population. Another explanation
may be that our sample was limited to patients hospitalized in
a tertiary pediatric medical center.
This report should shed further light on the rarely
reported clinical and epidemiological characteristics of recurrent HSP needing hospitalization. Recurrent cases of HSP
may be more common than reported, but most are treated in
an outpatient setting. In our inpatient population, no clinical
or laboratory characteristics were found to be predictive of
recurrence; the second episode was longer than the first one;
and the lag period between the 2 episodes was substantially
longer than previously reported.
REFERENCES
1. Saulsbury FT. Henoch-Schonlein purpura in children. Report of 100
patients and review of the literature. Medicine. 1999;78:395 409.
2. Nussinovitch M, Prais D, Finkelstein Y, et al. Cutaneous manifestations
28
3.
4.
5.
6.
7.
8.
9.
10.
of Henoch-Schonlein purpura in young children. Pediat Dermatol.
1998;5:426 428.
Kaufman RH, Hermann WA, Meyer CJL, et al. Circulating IgA immune
complexes in Henoch-Schonlein purpura. Am J Med. 1980;69:859 866.
Nathwani D, Laing R, Smith CC, et al. Recurrent post-infective HenochSchonlein syndrome: a genetic influence related to HLA B35? J Infect.
1992;25:205210.
Michel BA, Hunder GG, Bloch DA, et al. Hypersensitivity vasculitis and
Henoch-Schonlein purpura: a comparison between the 2 disorders.
J Rheumatol. 1992;19:721728.
Duzova A, Toaloglu R, Sanal O, et al. Henoch-Schonlein purpura in
Wiskott-Aldrich syndrome. Pediatr Nephrol. 2001;16:5000 5002.
Nathan K, Cunasekaran TS, Berman JH. Recurrent gastrointestinal
Henoch-Schoenlein purpura. J Clin Gastroenterol. 1999;29:86 89.
Pomeranz A, Korzets Z, Eliakim R, et al. Relapsing Henoch-Schonlein
purpura associated with a tubo-ovarian abscess due to Morganella
morganii. Am J Nephrol. 1997;17:471 473.
Hardoff D, Jaffe M, Front H. Recurrent episodes of testicular swelling
preceding Henoch-Schonlein purpura by 11 months. Eur J Pediatr.
1987;146:613 614.
Trapani S, Micheli A, Grisolia F, et al. Henoch Schonlein purpura in
childhood: epidemiological and clinical analysis of 150 cases over a 5
year period and review of literature. Semin Arthritis Rhem. 2005;35:
143153.
2007 Lippincott Williams & Wilkins
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Neonatal AKI PDFDocument13 pagesNeonatal AKI PDFgaatgaatNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Tugas Anestesi LODocument2 pagesTugas Anestesi LOgaatgaatNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- IntramuscularDocument4 pagesIntramusculargaatgaatNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hepatic Fibrosis and Cirrhosis: The (Myo) Fibroblastic Cell Subpopulations InvolvedDocument17 pagesHepatic Fibrosis and Cirrhosis: The (Myo) Fibroblastic Cell Subpopulations InvolvedgaatgaatNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Blood PressureDocument60 pagesBlood PressureEnerolisa ParedesNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- 1 s2.0 S0022347615003583 MainDocument8 pages1 s2.0 S0022347615003583 MainRully SuryonugrohoNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Jurnal Nutrisi Agatha FixDocument26 pagesJurnal Nutrisi Agatha FixgaatgaatNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- ReviewDocument13 pagesReviewgaatgaatNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Referat EbvDocument9 pagesReferat EbvgaatgaatNo ratings yet
- 9th EFCC HandbookDocument129 pages9th EFCC HandbookgaatgaatNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Preparing IV Infusions For Children 2.0Document17 pagesPreparing IV Infusions For Children 2.0gaatgaatNo ratings yet
- 2013 World Pneumonia Day InfographicDocument1 page2013 World Pneumonia Day InfographicgaatgaatNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Pelod 2Document14 pagesPelod 2gaatgaatNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Pediatric Heart FailureDocument11 pagesPediatric Heart Failuregaatgaat100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Pneumonia Diarrhea Disease Infographic 2012Document1 pagePneumonia Diarrhea Disease Infographic 2012gaatgaatNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Pediatrik Gawat Darurat Dosis Obat AAP PDFDocument20 pagesPediatrik Gawat Darurat Dosis Obat AAP PDFuzumakienggaNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- HIV and Infant Feeding Counseling Tools - Reference GuideDocument97 pagesHIV and Infant Feeding Counseling Tools - Reference Guideerkalem100% (1)
- 2013 World Pneumonia Day InfographicDocument1 page2013 World Pneumonia Day InfographicgaatgaatNo ratings yet
- Asa ClassDocument3 pagesAsa ClassPriska Gusti Wulandari67% (3)
- Amazing Grace (Lyrics and History)Document8 pagesAmazing Grace (Lyrics and History)gaatgaatNo ratings yet
- Abbreiation Resep.Document6 pagesAbbreiation Resep.gaatgaatNo ratings yet
- Amebiasis CRDocument3 pagesAmebiasis CRgaatgaatNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- CeftriaxoneDocument2 pagesCeftriaxonegaatgaatNo ratings yet
- Hazard Identification Risk Assessment Risk ControlDocument3 pagesHazard Identification Risk Assessment Risk Controle cubeNo ratings yet
- Psychoeducational and Family Therapy in Relapse PreventionDocument4 pagesPsychoeducational and Family Therapy in Relapse PreventionEdson HilárioNo ratings yet
- Methodology Tapping Methodology of WaterlineDocument15 pagesMethodology Tapping Methodology of WaterlineBryNo ratings yet
- DSM 5Document35 pagesDSM 5Hemant KumarNo ratings yet
- OPD Network ListDocument354 pagesOPD Network ListSHAIKH ABDUL AZIZ salim bashaNo ratings yet
- The Doctor-Patient Relationship and Interviewing TechniquesDocument50 pagesThe Doctor-Patient Relationship and Interviewing TechniquesPranay KumarNo ratings yet
- Table : Number of Population, Hospitals and Beds in All Over JordanDocument8 pagesTable : Number of Population, Hospitals and Beds in All Over JordanjNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- TIVA Part I - Pharmacokinetic Principles and Methods of Delivery PDFDocument56 pagesTIVA Part I - Pharmacokinetic Principles and Methods of Delivery PDFMaria José RecheNo ratings yet
- Prevention Strategies For Periodontal Disease - Chapter 16Document10 pagesPrevention Strategies For Periodontal Disease - Chapter 16Daniah MNo ratings yet
- NCP Gastric CancerDocument7 pagesNCP Gastric CancerAnonymous XvwKtnSrMR100% (4)
- Prepositions of Time ExplainedDocument18 pagesPrepositions of Time ExplainedyuèNo ratings yet
- Abbott Rabeprazole PM e PDFDocument45 pagesAbbott Rabeprazole PM e PDFdonobacaNo ratings yet
- Voyeuristic Disorder SymptomsDocument7 pagesVoyeuristic Disorder SymptomsgoyaNo ratings yet
- Curing Stage 4 Cancer and Terminal Liver Disease with Alpha Lipoic AcidDocument14 pagesCuring Stage 4 Cancer and Terminal Liver Disease with Alpha Lipoic Acidguy777No ratings yet
- Complaints Handling: BDA AdviceDocument8 pagesComplaints Handling: BDA Advicedruzair007No ratings yet
- Topical Agents and Dressings For Local Burn Wound CareDocument25 pagesTopical Agents and Dressings For Local Burn Wound CareViresh Upase Roll No 130. / 8th termNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hahnemann Advance MethodDocument2 pagesHahnemann Advance MethodRehan AnisNo ratings yet
- Postpartum Health TeachingDocument8 pagesPostpartum Health TeachingMsOrange96% (24)
- How To Make An ELearning ModuleDocument22 pagesHow To Make An ELearning ModulePradeep RawatNo ratings yet
- Informed Consent and Release, Waiver, and Quitclaim: Know All Men by These PresentsDocument2 pagesInformed Consent and Release, Waiver, and Quitclaim: Know All Men by These PresentsRobee Camille Desabelle-SumatraNo ratings yet
- Common Assessment Framework FormDocument9 pagesCommon Assessment Framework FormparaypanNo ratings yet
- Spesifikasi Cardio 7Document2 pagesSpesifikasi Cardio 7Ali RidwanNo ratings yet
- Mine Ventilation FundamentalsDocument36 pagesMine Ventilation FundamentalsArihant JainNo ratings yet
- Posthumus 2021 Competition Nutrition Practices ofDocument13 pagesPosthumus 2021 Competition Nutrition Practices ofSyazmi MohdNo ratings yet
- GoalSettingWorkbookFinal PDFDocument21 pagesGoalSettingWorkbookFinal PDFDato KhutsishviliNo ratings yet
- E136Document4 pagesE136Subramanya RaoNo ratings yet
- Module 7 Health Insurance Types and ImportanceDocument10 pagesModule 7 Health Insurance Types and ImportanceKAH' CHISMISSNo ratings yet
- Behavorial Methods IIDocument18 pagesBehavorial Methods IImehak727No ratings yet
- الورقة الثالثة- القبالة-2Document4 pagesالورقة الثالثة- القبالة-2Habebt MusabNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)