Professional Documents
Culture Documents
Mental Health, Depression, and Anxiety in Patients On Maintenance Dialysis
Uploaded by
Try Febriani SiregarOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mental Health, Depression, and Anxiety in Patients On Maintenance Dialysis
Uploaded by
Try Febriani SiregarCopyright:
Available Formats
Dialysis
Review
Mental Health, Depression, and Anxiety in Patients on
Maintenance Dialysis
Usama Feroze,1,2 David Martin,3 Astrid Reina-Patton,3
Kamyar Kalantar-Zadeh,1,2,4 Joel D Kopple1,2,4
1Harold Simmons Center for
Chronic Disease Research and
Epidemiology, Los Angeles
Biomedical Research Institute
at Harbor-UCLA Medical
Center, Torrance, California,
USA
2Division of Nephrology and
Hypertension, Los Angeles
Biomedical Research Institute
at Harbor-UCLA Medical
Center, Torrance, California,
USA
3David Geffen School of
Medicine at UCLA and the
UCLA School of Public Health,
Los Angeles, California, USA
4Department of Psychiatry, Los
Angeles Biomedical Research
Institute at Harbor-UCLA
Medical Center, Torrance,
California, USA
Keywords. kidney failure,
depression, anxiety, dialysis
Depression and anxiety are among the most common comorbid
illnesses in people with end-stage renal disease (ESRD). Patients
with ESRD face many challenges which increase the likelihood that
they will develop depression or anxiety or worsen these conditions.
These include a general feeling of unwellness; specific symptoms
caused by ESRD or the patients treatment; major disruptions in
lifestyle; the need to comply with treatment regimens, including
dialysis schedules, diet prescription, and water restriction; ancillary
treatments and hospitalizations; and the fear of disability, morbidity,
and shortened lifespan. Depression has been studied extensively in
patients on maintenance dialysis, and much effort has been done to
validate the proper screening tools to diagnose depression and to
define the treatment options for patients on maintenance dialysis
with depression. Anxiety is less well studied in this population
of patients. Evidence indicates that anxiety is also common in
maintenance dialysis. More attention should be paid to measuring
the incidence and prevalence and developing methods of diagnosis
and treatment approaches for anxiety in patients with ESRD. In this
review, we attempted to underscore those aspects of depression
and anxiety that have not been investigated extensively, especially
with regard to anxiety. The interaction between racial/ethnic
characteristics of patients on maintenance dialysis with depression
and anxiety needs to be studied more extensively, in order to assess
better approaches to healthcare for these individuals.
IJKD 2010;4:173-80
www.ijkd.org
INTRODUCTION
End-stage renal disease (ESRD) is defined as kidney
failure sufficiently severe to require maintenance
dialysis or kidney transplantation to maintain health
or life. According to the United States Renal Data
System report in 2008, there were 485 000 patients
with ESRD in the United States, 61% of whom were
Caucasian; 31.7%, African-American; 14%, Hispanic;
4.5%, Asian; and 1.3%, Native American (1.5% had
no defined ethnicity).1 Like many chronic diseases,
ESRD may affect the psychological state of the
patients (Table 1). Psychiatric illness in patients with
ESRD has persistently intrigued healthcare workers
due to its effect on the morbidity and healthcare
costs in patients with ESRD. Levy introduced the
term psychonephrology, to refer to psychiatric
problems of people suffering from kidney disease, and
particularly those with kidney failure who undergo
maintenance dialysis or who are transplanted.2
Although there have been many estimates of the
actual prevalence of psychiatric illness in patients
with ESRD, these estimates may be erroneously
low, because patients often fail to seek mental
healthcare. Johnson and Dwyer reported that over
70% of patients on maintenance hemodialysis
who had symptoms of depression or anxiety and
described barriers to mental health treatment did
not recognize their symptoms or did not perceive
Iranian Journal of Kidney Diseases | Volume 4 | Number 3 | July 2010
173
Mental Health in Patients on DialysisFeroze et al
Table 1. Patient Challenges Upon Starting Maintenance Dialysis
Patient Challenges Upon Starting Maintenance Dialysis
Medical management of their end-stage renal disease (requires compliance to dialysis and medicinal intake)
Adjustment to dietary prescription and reduced fluid intake
Maintaining meaningful life roles regarding jobs, family, and friends
Coping with the anger, fear, anxiety, frustration, and sadness of having a chronic illness
Accepting the disruption of their activities
Confronting their own mortality and probable shortened life span
Acceptance of recurrent hospitalizations, placement and repair of vascular or peritoneal access, and the discomfort of dialysis and
other medical treatments
that they were in need of therapy for their mental
health condition.3 Dialysis physicians and nurses,
who are not psychiatrists, often fail to recognize such
symptoms, and physicians may pay less attention
to somatic complaints of psychiatric illnesses, and
therefore, leave these comorbidities undiagnosed.
In this review, we have tried to highlight those
aspects of depression and anxiety in patients with
ESRD which can be addressed to improve the life of
patients undergoing maintenance dialysis therapy.
EPIDEMIOLOGY
Depression: a Greater Focus of Attention
Much attention has been given to depression in
patients on maintenance dialysis during the past
3 decades. Considered to be the most common
psychiatric abnormality in patients with ESRD,4,5
depression has been studied extensively in these
individuals. The effect of depression on mortality,
suicide, and hospitalization has been studied recently,
and depression is established as an independent
risk factor for mortality and morbidity.6-9 Drayer
and colleagues found that patients with ESRD and
depression have 4.1 times the mortality rate of
patients with ESRD who do not have depression
(Figure 1).10 Lopes and coworkers suggested a higher
rate of withdrawal from maintenance dialysis in
patients who developed depression while on dialysis
than in those patients who were not depressed. These
investigators also found a higher risk of mortality
and hospitalization associated with depression.9
Einwohner and colleagues showed a similar increased
risk of morbidity and mortality in depressed patients
on maintenance peritoneal dialysis.11
Suicide is highly linked with a depressed state
of mind. 4,12 It accounts for a death rate of 0.2%
per 1000 dialysis patients-years at risk.13 Kurella
and colleagues also found a strong association
between alcohol dependence and hospitalization for
substance abuse and mental illness with subsequent
174
Figure 1. Survival possibilities for depressed and nondepressed
patients on hemodialysis patients. Adapted from Drayer and
colleagues.10
death by suicide.14 Patients with ESRD are often
poorly adherent to their medical regimens, and
Cukor and coworkers have reported depression
as an independent factor for nonadherence in
patients on maintenance dialysis.15
The prevalence rate for depression in patients
with ESRD is around 3 times that of the general
population. A national survey reported that the
prevalence rate for major depressive disorders in
the general population in the United States was
10.4% in Caucasians, 7.5% in African-Americans, and
8.0% in Mexican Americans.16 In contrast, Kutner
and colleagues and Cukor and associates reported
prevalence rates of 26.6% and 29% for depression,
respectively, in patients with ESRD.17,18 Heydayati
and colleagues demonstrated a point prevalence of
depression of 26% and of major depression of 17%
in patients on maintenance hemodialysis.19,20 Other
studies, taken together, report a wider range for the
prevalence of depression in patients with ESRD.7,20,21
Anxiety: an Often Overlooked Disturbance
Anxiety has been an understudied aspect of
Iranian Journal of Kidney Diseases | Volume 4 | Number 3 | July 2010
Mental Health in Patients on DialysisFeroze et al
psychiatric illness in patients on maintenance
dialysis. Most studies have focused on depression
in these individuals. The National Institute of
Mental Health defines an anxiety disorder as an
excessive, irrational dread of every day situations.
In the general population in the United States, the
prevalence rate of anxiety disorders is 18%, which
is tantamount to about 40 000 000 American adults
aged 18 or older having this disorder.22 Precise data
regarding the prevalence rate of anxiety disorders
among patients with ESRD are unknown, but Kutner
and colleagues,17 Taskapan and colleagues,23 and
Cukor and coworkers18 reported prevalence rates
of 45%, 30%, and 45.7%, respectively. A review
of 55 studies of the prevalence of symptoms of
anxiety in patients with ESRD by Murtagh and
coworkers found that 38% of patients with ESRD
(12% to 52%) have substantial anxiety.24
Because data are scarce regarding the prevalence
of anxiety, the exact nature of its effects on patients
with ESRD is also unknown. In the general
population in the United States, the prevalence rates
of social anxiety disorders over a 12-month period
were reported to be 4.5% in African-Americans
and 7.1% in Caucasians.25
Sareen and associates established anxiety
disorders as an independent risk factor for suicidal
behavior and showed strong associations between
the comorbidity of anxiety disorders and comorbid
physical conditions, poor quality of life, and
disability.26,27 Such associations have not been studied
in patients with ESRD suffering from anxiety.
One co-author of this review (JDK) has
personally observed that adult patients who are
well established on maintenance hemodialysis
therapy often describe higher anxiety levels during
many of their thrice-weekly dialysis sessions. The
prevalence of this problem is unknown. A possible
temporal relationship between dialysis treatments
and anxiety level was reported in 7 patients on
maintenance hemodialysis in 1978 by Bedell and
coworkers. 28 They reported that patients were
more anxious on hemodialysis days, and that the
intensity of their anxiety increased as their dialysis
treatment session proceeded.28 The small sample
size and the lack of characterization of the patients
were important limitations of this study.
Billington and coworkers reported that the degree
of hope in 103 patients on maintenance dialysis,
assessed from a self-report scale, correlated inversely
Figure 2. Correlation of hope with the quality of life in patients
with end-stage renal disease. Adapted from Billington and
colleagues (a cross-sectional study evaluating self-reported
measures from 103 patients on dialysis in 5 dialysis centers in
the Northwest United Kingdom).29 Hope was defined as an active
cognitive process of belief in ones capacity to produce goals, as
well as goal-directed determination/energy and a positive sense
of planning to meet goals. QOL indicates quality of life.
*P < .001
P < .05
with the degree of depression and anxiety and
positively with the disease effects, the burden of ESRD,
and the physical and mental quality of life (Figure 2).29
Race/Ethnicity and Its Association With
Depression and Anxiety
Racial effects on depression and anxiety have
been studied in the general population, and the
results have been conflicting. Brown and colleagues
showed no racial differences in the prevalence of
anxiety disorders and comorbid major depression
between African-Americans and Caucasians in the
general population.30 Himle and coworkers indicated
in their study that most anxiety disorders are more
prevalent among whites than African-Americans
and Caribbean blacks.25 Stephanie and colleagues
reported a higher prevalence rate of major depressive
disorders among whites than African-Americans and
Mexican-Americans.16 No study has been conducted
in patients with ESRD that clearly delineated racial
effects of African-Americans and Caucasians on
anxiety levels in patients on maintenance dialysis.
The studies of Cukor and coworkers and Kimmel
and colleagues consisted of 88.6% of the AfricanAmericans; thus, they may not have had an adequate
sample size to compare their findings to those of
nonAfrican-Americans.18,31,32
Weisbord and associates reported the only available
study on the association of race with depression in
patients on maintenance hemodialysis. They reported
that there were no racial differences in the prevalence
of depression between Caucasian and African-
Iranian Journal of Kidney Diseases | Volume 4 | Number 3 | July 2010
175
Mental Health in Patients on DialysisFeroze et al
American patients on maintenance hemodialysis.33
SCREENING
Validation of Practical Screening Tools
In the past decade, several questionnaires
have been used to screen for depression and
anxiety in patients with ESRD (Tables 2 and 3).
The Beck Depression Inventory has been studied
extensively, and its use has been validated to screen
for depression in patients with ESRD. 13,21,31,36 A
higher cutoff value has been proposed to diagnose
depression in patients on maintenance dialysis.19,21,37
The Hospital Anxiety and Depression Scale is
used as a screening tool for depression and anxiety
and has been validated in the general population.
A review by Bjelland and coworkers suggests that
it has good internal consistency and validity. 38
Loosman and associates validated its use to screen
depression in patients undergoing maintenance
dialysis,39 although Cukor and coworkers reported
that the Hospital Anxiety and Depression Scale does
not serve as an effective screening tool for anxiety
disorders in patients on dialysis.18 There is clearly
a need for more effective screening tools, especially
for anxiety, in patients on maintenance dialysis.
MANAGEMENT
In patients with ESRD, the symptoms of
depression or anxiety may be similar to those
that occur with kidney failure or uremia per se.
Therefore, the diagnosis and treatment of depression
and anxiety in these patients is often delayed
or missed altogether because the symptoms are
disguised by, or attributed to, uremia.12,13,36 This
is especially true for the symptoms of depression.
Insomnia is commonly reported in patients with
either depression or uremia,40 and drug-induced
symptoms (eg, from glucocorticoid medicines) may
also present in ways that overlap with the symptoms
of anxiety, depression, or uremia. A team approach
that includes psychologists, psychiatrists, or social
workers is generally needed in order to identify,
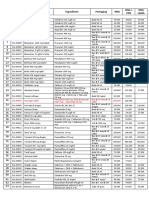
Table 2. Assessment Tools and Prevalence Rates Reported in 6 Recent Studies of Depression and Anxiety in Patients on Maintenance
Hemodialysis*
Author
Taskapan et al23
Weisbord et al33
Number of
Patients
40
160
Study Tools
HDRS
HARS
PRIME-MD
MMSE
SF-36
BDI
CDI
DSI
Prevalence Results
Depression, 30%
Anxiety, 35%
Additional Comments (Major
Recommendations of Article)
A negative correlation between interdialytic
weight gain and quality of life domains of
vitality and social function was found.
Depression, 27% (in both
races)
No racial differences were found in the
prevalence of depression. Spiritual/religious
belief in African-Americans seemed relevant
to their better quality of life and survival.
Cukor et al31
70
SCID
BDI
KDQOL-SF
YSQ
Depression, 20%
Anxiety, 27%
Aloneness and ineffectiveness were
hallmarks of the depressogenic changes that
were associated with end-stage renal disease
treatment.
Cukor et al32
50
SCID
BDI-2
KDQOL-SF
LESS
Depression, 42%
(depression on follow-up)
Anxiety, 33% of the
diagnosed patients from
the above study31 still had
an anxiety disorder
Level of depressive affect is a more powerful
predictor of depression 16 month later, than
other psychological measures, including
baseline depression diagnosis. It was a
follow-up study in which patients were again
interviewed after 16 months of their diagnosis.
Cukor et al18
70
Depression, 29%
Anxiety, 45.7%
Hedayati et al6
98
SCID
HADS
KDQOL-SF
SCID
BDI
CDI
CESD
It was a single-center study with population not
demographic representation of the United
States.
It was the first report on association between
depression and poor clinical outcome in
patients with end-stage renal disease.
Depression, 26.7%
*HDRS indicates Hamilton Depression Rating Scale; HARS, Hamilton Anxiety Rating Scale; PRIME-MD, Primary Care Evaluation of Mental
Disorders; MMSE, Mini Mental State Examination; SF-36, Short Form Health Survey 36; BDI, Beck Depression Inventory; CDI, Cognitive
Depression Index; DSI, Dialysis Symptom Index; SCID, Structured Clinical Interview for Diagnosis; KDQOL-SF, Kidney Disease Quality of LifeShort Form; YSQ, Youngs Schema Questionnaire; LESS, Life Events Stress Scale; HADS, Hospital Anxiety and Depression Scale; and CESD,
Center for Epidemiological Study of Depression.
176
Iranian Journal of Kidney Diseases | Volume 4 | Number 3 | July 2010
Mental Health in Patients on DialysisFeroze et al
Table 3. Assessment and Approach to Depressed Patients on Dialysis*
Intervention
Measures
Screening
Beck Depression Inventory
Asking 2 basic questions:
a. How much of the time have you felt so down in the dumps that nothing could cheer you up?
b. How much of the time have you felt downhearted and blue?
Referral
Treatment
Mental Health Professionals
Nonpharmacological therapy
a. Psychotherapy
b. Cognitive behavioral therapy
c. Exercise training programs
d. Treat Anxiety
e. Counseling and psychotherapy for family members, significant others and caregivers
f. Management of medical conditions that may contribute to depression, such as sleep deprivation, medicinal
intake, and syndromes causing pain or other physical discomfort
Pharmacological therapy
Electroconvulsive therapy
*Adapted from articles by Lopes and colleagues,9 Cohen and colleagues,34 and Hedayati and Finkelstein35
comprehensively diagnose, and treat these illnesses.
Pharmacological treatment, psychotherapy and
cognitive behavioral therapy have been the mainstay
for the treatment of depression and anxiety in the
general population (Table 3).41,42 Similar options
are available to treat the psychological disorders
in patients with ESRD.34 However, in patients with
ESRD, more consideration may need to be paid
to the appropriate doses of medicines to be used.
Failure to treat with appropriate psychotropic
medicines or underdosing of such medicines
appears to be common in patients with ESRD who
have depression. Hedayati and colleagues reported
that less than 50% of patients with ESRD who
were diagnosed with depression by the Structured
Clinical Interview for Diagnosis were receiving
antidepressants, and approximately 50% of whom
were receiving subtherapeutic doses. 19 Wartnick
and coworkers reported an even lower rate of
treatment for depression in patients commencing
maintenance dialysis therapy. 43 No studies are
available regarding the numbers of patients with
ESRD who receive treatment for anxiety disorders
or the appropriateness of the doses of psychotropic
medicines that are employed for these individuals.
Selective serotonin reuptake inhibitors are the
main category of medicines that are currently
used to treat depression in such patients, because
of their effectiveness and enhanced safety,
including their potential for reducing the risk of
orthostatic hypotension in patients on maintenance
hemodialysis.4 Blumenfield and associates studied
the effect of fluoxetine in patients on hemodialysis
and reported both effectiveness and safety in
these individuals. 44 Citalopram and sertraline
also have safe pharmacokinetics in patients with
ESRD, and hence, are often prescribed.45 Tricyclic
antidepressants and monoamine oxidase inhibitors
are other treatment options, but they have a higher
side effect profile which limits their use (Table 4).
Benzodiazepines, such as diazepam, have been
used to relieve acute episodes of panic and anxiety.
Generally, an adjustment of the drug dose for the
level of the glomerular filtration rate is not needed, as
they are metabolized in the liver. However, the dosing
of midazolam should be adjusted cautiously because
the conjugate of main metabolite of medazolam;
ie, alpha-hydroxymedazolam. causes prolonged
sedation in patients with kidney failure. 46,47
Buspirone, a partial serotonin agonist that acts on
the 5HT(1A) receptor, is often recommended over
benzodiazepines because of the greater incidence
of unfavorable side effects with benzodiazepines.48
There is an increase in the half-life of the parent
compound, buspirone and its active metabolite,
1-(2-pyrimidinyl)-piperazine, in kidney impairment,
especially in anuric patients on hemodialysis during
the interdialytic interval; thus, the dose of this
medication must be carefully titrated.49,50
Nonpharmacological treatment of these
disorders is an important component in the overall
treatment of the mental health of these patients.
Cognitive behavioral therapy has been shown to
improve symptoms of depression in patients on
maintenance dialysis.51,52 Exercise programs may
also be effective at reducing depressive symptoms
in these individuals.53,54
The psychological, social, economic, and emotional
Iranian Journal of Kidney Diseases | Volume 4 | Number 3 | July 2010
177
Mental Health in Patients on DialysisFeroze et al
Table 4. Commonly Used Psychotropic Medications in End-stage Renal Disease (ESRD)
Psychotropic
Medications
Selective serotonin
reuptake inhibitors
(fluoxetine,
citalopram,
paroxetine,
serteraline)
Serotoninnorepinephrine
reuptake inhibitors
(venlafaxine)
Important
Potential Side Effects
Considerations
Effects are usually Suicidal ideation,
seen in 6 weeks. bleeding, weight
gain, gastrointestinal
symptoms
Serum half-life
increases from 4
hours to 6 to 11
hours in patients
with ESRD.
Serotonin modulators Avoid use
(netazodone,
in cardiac
Trazodone)
patients due to
accumulation
of toxic
metabolites.
DopamineThey increase
risk of seizures
norepinephrine
due to toxicity of
reuptake inhibitors
(bupropion)
drug level and
accumulation
of active
metabolites.
Partial Serotonin
Serum half-life
5HT(1A)
in patients with
receptor agonists
ESRD is 1 to 5
(buspirone)
hours.
In normal adults,
serum half-life is
0.5 to 2.5 hours.
Tricyclics and
Avoid if possible
tetracyclics
given cardiac
(amitriptyline,
side Effects.
desipramine,
doxepin,
nortriptyline)
Benzodiazepines
(alprazolam,
lorazepam,
diazepam,
midazolam,
chlordiazepoxide)
Fluoxetine: not removed by
dialysis
Citalopram: not studied
Paroxetine: not studied
Sertraline: not removed by
dialysis
Accumulation of toxic
Not removed by Dialysis
metabolites, sexual
dysfunction, hypertension
Pharmacokinetics in Kidney
Impairment
Citalopram in severe impairment
(creatinine clearance < 20 mL/
min): Use with caution.
Paroxetine ( creatinine
clearance <30 mL/min): mean
plasma concentrations is about
4 times that seen in normal
function.
Decrease total daily dose by
50% given after completion of
dialysis.
Accumulation of toxic
rnetabolites, liver failure
(for nefazodone),
central nervous system
symptoms, hypotension
and cardiac arrhythmias
Hallucinations, insomnia,
agitation
Nefazodone: minimal
removal
Trazodon : no effect
Nefazodone: nonrenal
elimination of drug. Serum
half-life in ESRD: 3 to 5.8
hours.
Trazodone: no data available.
Not known
Use with caution and consider a
reduction in dosing frequency.
Dizziness, nausea,
headache, insomnia,
tremor, and seizure on
withdrawal
Not removed by dialysis
Usually 25% to 50% dose
reduction is advised to prevent
hypotension.
Central nervous
Amitryptyline: not removed
system symptoms,
by hemodialysis
anticholinergic effects,
Desipramine: not removed
QTc prolongation, cardiac by hemodialysis or CAPD
arrhythmia, orthostatic
Doxepin : not removed by
hypotension
hemodialysis or CAPD
Nortryptyline: not removed
by hemodialysis or CAPD
This group is used Delusion, hallucination,
Alprazolam: minimal
Alprazolam and diazepam:
with care due to
prolonged sedation
removal
increased free fraction of
high rate of side
Lorazepam: Not removed
plasma protein bound drug in
effects.
by hemodialysis
ESRD. Minimal differences in
Diazepam : Not removed by dialysis-dependent patients is
hemodialysis
seen.
Midazolam: not known.
Lorazepam: manufacturer does
not recommend use in ESRD.
stresses of living with ESRD often are overwhelming
or nearly so for the patients and their family or
close associates. These factors, coupled with the
extra physical workload that ESRD often brings
to family and friends, can be major contributors to
depression and anxiety in these individuals. Social
support is also an integral way of providing better
healthcare for patients with ESRD. Integration
of psychological and material support for better
178
Effect of Dialysis
healthcare of the patient is the essence of the social
support system. Social support has been shown to
have an improved end result in a variety of chronic
illnesses.55,56 Symister and Friend reported that social
support decreased depression by improving the
self-esteem of the patients with ESRD, which led to
an increased degree of optimism in these patients.56
A continuous care model, a native model for the
Iranian society, was used by Rahimi and colleagues,57
Iranian Journal of Kidney Diseases | Volume 4 | Number 3 | July 2010
Mental Health in Patients on DialysisFeroze et al
which appeared to make a significant difference in
the levels of depression and anxiety of patients on
maintenance hemodialysis. This model was based
on the principle that continuous care requires an
integration of the orientation, sensitization, control,
and evaluation of the disease process. It also lays
stress on the dynamic relationship among the
healthcare team and the patients and their family.57
CONCLUSIONS
Depression as a comorbid illness in patients
with ESRD has been more extensively studied. Less
attention has been paid to anxiety, and hence, the
information in the medical literature is sparser with
regard to information on practical anxiety screening
tools, the potential effects of race/ethnicity on
anxiety, and the preferred methods of treatment
of anxiety in patients with ESRD. The psychiatric
burden experienced by patients with ESRD may
have profound effects on their quality of life and
response to treatment. Such patients often develop
depressive or anxiety disorders in response to these
stresses, and of course, they may develop ESRD with
underlying psychiatric illnesses that may not be
directly related to kidney disease or kidney failure.
The management plan for medical treatment as well
as for possible psychotherapy of patients with ESRD
should take these issues into consideration.
as a correlate of hospitalizations in patients receiving
long-term hemodialysis. Am J Kidney Dis. 2005;46:642-9.
8. Kimmel PL, Peterson RA, Weihs KL, et al. Multiple
measurements of depression predict mortality in a
longitudinal study of chronic hemodialysis outpatients.
Kidney Int. 2000;57:2093-8.
9. Lopes AA, Bragg J, Young E, et al. Depression as
a predictor of mortality and hospitalization among
hemodialysis patients in the United States and Europe.
Kidney Int. 2002;62:199-207.
10. Drayer RA, Piraino B, Reynolds CF, 3rd, et al.
Characteristics of depression in hemodialysis patients:
symptoms, quality of life and mortality risk. Gen Hosp
Psychiatry. 2006;28:306-12.
11. Einwohner R, Bernardini J, Fried L, Piraino B. The effect
of depressive symptoms on survival in peritoneal dialysis
patients. Perit Dial Int. 2004;24:256-63.
12. Kimmel PL. Depression in patients with chronic renal
disease: what we know and what we need to know. J
Psychosom Res. 2002;53:951-6.
13. Kimmel PL, Peterson RA. Depression in end-stage renal
disease patients treated with hemodialysis: tools, correlates,
outcomes, and needs. Semin Dial. 2005;18:91-7.
14. Kurella M, Kimmel PL, Young BS, Chertow GM. Suicide in
the United States end-stage renal disease program. J Am
Soc Nephrol. 2005;16:774-81
15. Cukor D, Rosenthal DS, Jindal RM, Brown CD, Kimmel
PL. Depression is an important contributor to low
medication adherence in hemodialyzed patients and
transplant recipients. Kidney Int. 2009;75:1223-9.
16. Riolo SA, Nguyen TA, Greden JF, King CA. Prevalence
of depression by race/ethnicity: findings from the National
Health and Nutrition Examination Survey III. Am J Public
Health. 2005;95:998-1000.
CONFLICT OF INTEREST
None declared.
17. Kutner NG, Fair PL, Kutner MH. Assessing depression
and anxiety in chronic dialysis patients. J Psychosom Res.
1985;29:23-31.
REFERENCES
18. Cukor D, Coplan J, Brown C, et al. Anxiety disorders in
adults treated by hemodialysis: a single-center study. Am
J Kidney Dis. 2008;52:128-36.
1. Collins AJ, Foley RN, Herzog C, et al. United States Renal
Data System 2008 Annual Data Report. Am J Kidney Dis.
2009;53:S1-374.
2. Levy NB. What is psychonephrology? J Nephrol. 2008;21
Suppl 13:S51-3.
3. Johnson S, Dwyer A. Patient perceived barriers to
treatment of depression and anxiety in hemodialysis
patients. Clin Nephrol. 2008;69:201-6.
4. Kimmel PL. Psychosocial factors in dialysis patients.
Kidney Int. 2001;59:1599-613.
5. Kimmel PL, Weihs K, Peterson RA. Survival in
hemodialysis patients: the role of depression. J Am Soc
Nephrol. 1993;4:12-27.
6. Hedayati SS, Bosworth HB, Briley LP, et al. Death or
hospitalization of patients on chronic hemodialysis
is associated with a physician-based diagnosis of
depression. Kidney Int. 2008;74:930-6.
7. Hedayati SS, Grambow SC, Szczech LA, Stechuchak KM,
Allen AS, Bosworth HB. Physician-diagnosed depression
19. Hedayati SS, Bosworth HB, Kuchibhatla M, Kimmel PL,
Szczech LA. The predictive value of self-report scales
compared with physician diagnosis of depression in
hemodialysis patients. Kidney Int. 2006;69:1662-8.
20. Hinrichsen GA, Lieberman JA, Pollack S, Steinberg H.
Depression in hemodialysis patients. Psychosomatics.
1989;30:284-9.
21. Craven JL, Rodin GM, Littlefield C. The Beck Depression
Inventory as a screening device for major depression in renal
dialysis patients. Int J Psychiatry Med. 1988;18:365-74.
22. Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters
EE. Prevalence, severity, and comorbidity of 12-month
DSM-IV disorders in the National Comorbidity Survey
Replication. Arch Gen Psychiatry. 2005;62:617-27.
23. Taskapan H, Ates F, Kaya B, et al. Psychiatric disorders
and large interdialytic weight gain in patients on chronic
haemodialysis. Nephrology (Carlton). 2005;10:15-20.
24. Murtagh FE, Addington-Hall J, Higginson IJ. The prevalence
of symptoms in end-stage renal disease: a systematic
Iranian Journal of Kidney Diseases | Volume 4 | Number 3 | July 2010
179
Mental Health in Patients on DialysisFeroze et al
review. Adv Chronic Kidney Dis. 2007;14:82-99.
J Med. 2005;353:1819-34.
25. Himle JA, Baser RE, Taylor RJ, Campbell RD, Jackson
JS. Anxiety disorders among African Americans, blacks of
Caribbean descent, and non-Hispanic whites in the United
States. J Anxiety Disord. 2009;23:578-90.
26. Sareen J, Cox BJ, Afifi TO, et al. Anxiety disorders
and risk for suicidal ideation and suicide attempts: a
population-based longitudinal study of adults. Arch Gen
Psychiatry. 2005;62:1249-57.
27. Sareen J, Jacobi F, Cox BJ, Belik SL, Clara I, Stein MB.
Disability and poor quality of life associated with comorbid
anxiety disorders and physical conditions. Arch Intern
Med. 2006;166:2109-16.
28. Bedell JR, Kilpatrick DG, Robinson J, Gilbert G, Miller
WC. Anxiety during hemodialysis sessions: discrepant
evaluations of patients and nurses. J Am Assoc Nephrol
Nurses Tech. 1978;5:72-6.
29. Billington E, Simpson J, Unwin J, Bray D, Giles D. Does
hope predict adjustment to end-stage renal failure and
consequent dialysis? Br J Health Psychol. 2008;13:683-99.
30. Brown C, Shear MK, Schulberg HC, Madonia MJ. Anxiety
disorders among African-American and white primary
medical care patients. Psychiatr Serv. 1999;50:407-9.
31. Cukor D, Coplan J, Brown C, et al. Depression and
anxiety in urban hemodialysis patients. Clin J Am Soc
Nephrol. 2007;2:484-90.
32. Cukor D, Coplan J, Brown C, Peterson RA, Kimmel PL.
Course of depression and anxiety diagnosis in patients
treated with hemodialysis: a 16-month follow-up. Clin J
Am Soc Nephrol. 2008;3:1752-8.
33. Weisbord SD, Fried LF, Unruh ML, et al. Associations
of race with depression and symptoms in patients on
maintenance haemodialysis. Nephrol Dial Transplant.
2007;22:203-8.
34. Cohen SD, Norris L, Acquaviva K, Peterson RA, Kimmel
PL. Screening, diagnosis, and treatment of depression
in patients with end-stage renal disease. Clin J Am Soc
Nephrol. 2007;2:1332-42.
35. Hedayati SS, Finkelstein FO. Epidemiology, diagnosis,
and management of depression in patients with CKD. Am
J Kidney Dis. 2009;54:741-52.
36. Cukor D, Peterson RA, Cohen SD, Kimmel PL.
Depression in end-stage renal disease hemodialysis
patients. Nat Clin Pract Nephrol. 2006;2:678-87.
37. Watnick S, Wang PL, Demadura T, Ganzini L. Validation
of 2 depression screening tools in dialysis patients. Am J
Kidney Dis. 2005;46:919-24.
38. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity
of the Hospital Anxiety and Depression Scale. An updated
literature review. J Psychosom Res. 2002;52:69-77.
39. Loosman WL, Siegert CE, Korzec A, Honig A. Validity of
the Hospital Anxiety and Depression Scale and the Beck
Depression Inventory for use in end-stage renal disease
patients. Br J Clin Psychol. 2009.
40. Parker KP. Sleep and dialysis: a research-based review of
the literature. Anna J. 1997;24:626-39; quiz 40-1.
41. Whooley MA, Simon GE. Managing depression in medical
outpatients. N Engl J Med. 2000;343:1942-50.
42. Mann JJ. The medical management of depression. N Engl
180
43. Watnick S, Kirwin P, Mahnensmith R, Concato J. The
prevalence and treatment of depression among patients
starting dialysis. Am J Kidney Dis. 2003;41:105-10.
44. Blumenfield M, Levy NB, Spinowitz B, et al. Fluoxetine
in depressed patients on dialysis. Int J Psychiatry Med.
1997;27:71-80.
45. Cohen LM, Tessier EG, Germain MJ, Levy NB. Update
on psychotropic medication use in renal disease.
Psychosomatics. 2004;45:34-48.
46. Wagner BK, OHara DA. Pharmacokinetics and
pharmacodynamics of sedatives and analgesics in
the treatment of agitated critically ill patients. Clin
Pharmacokinet. 1997;33:426-53.
47. Bauer TM, Ritz R, Haberthur C, et al. Prolonged sedation
due to accumulation of conjugated metabolites of
midazolam. Lancet. 1995;346:145-7.
48. Rickels K, Rynn M. Pharmacotherapy of generalized
anxiety disorder. J Clin Psychiatry. 2002;63 Suppl 14:9-16.
49. Mahmood I, Sahajwalla C. Clinical pharmacokinetics and
pharmacodynamics of buspirone, an anxiolytic drug. Clin
Pharmacokinet. 1999;36:277-87.
50. Caccia S, Vigano GL, Mingardi G, et al. Clinical
pharmacokinetics of oral buspirone in patients with impaired
renal function. Clin Pharmacokinet. 1988;14:171-7.
51. Cukor D. Use of CBT to treat depression among patients
on hemodialysis. Psychiatr Serv. 2007;58:711-2.
52. Duarte PS, Miyazaki MC, Blay SL, Sesso R. Cognitivebehavioral group therapy is an effective treatment for
major depression in hemodialysis patients. Kidney Int.
2009;76:414-21.
53. Levendoglu F, Altintepe L, Okudan N, et al. A twelve week
exercise program improves the psychological status,
quality of life and work capacity in hemodialysis patients. J
Nephrol. 2004;17:826-32.
54. Ouzouni S, Kouidi E, Sioulis A, Grekas D, Deligiannis A.
Effects of intradialytic exercise training on health-related
quality of life indices in haemodialysis patients. Clin
Rehabil. 2009;23:53-63.
55. House JS, Landis KR, Umberson D. Social relationships
and health. Science. 1988;241:540-5.
56. Symister P, Friend R. The influence of social support
and problematic support on optimism and depression in
chronic illness: a prospective study evaluating self-esteem
as a mediator. Health Psychol. 2003;22:123-9.
57. Rahimi A, Ahmadi F, Gholyaf M. The effects of Continuous
Care Model on depression, anxiety, and stress in patients
on hemodialysis. Nephrol Nurs J. 2008;35:39-43.
Correspondance to:
Joel D Kopple, MD
Los Angeles Biomedical Research Institute at Harbor-UCLA
Medical Center, 1124 West Carson St, C1-Annex, Torrance, CA
90502, USA
Tel: +1 310 222 3891
Fax: +1 310 782 1837
E-mail: jkopple@labiomed.org
Received April 2010
Iranian Journal of Kidney Diseases | Volume 4 | Number 3 | July 2010
You might also like
- The Impact of Emotional Support in Managing Cardiovascular Diseases Among Hispanic and Non -Hispanic Menopausal Women Aged 55 to 84 YearsFrom EverandThe Impact of Emotional Support in Managing Cardiovascular Diseases Among Hispanic and Non -Hispanic Menopausal Women Aged 55 to 84 YearsNo ratings yet
- Crit Care Nurse 2014 Chapa 14 25Document12 pagesCrit Care Nurse 2014 Chapa 14 25Ferdy LainsamputtyNo ratings yet
- Alzheimer’s Disease: A Physician’s Guide to Practical ManagementFrom EverandAlzheimer’s Disease: A Physician’s Guide to Practical ManagementRalph W. RichterNo ratings yet
- Gender Differences in the Pathogenesis and Management of Heart DiseaseFrom EverandGender Differences in the Pathogenesis and Management of Heart DiseaseNo ratings yet
- Bipolar MedicationDocument5 pagesBipolar MedicationindarNo ratings yet
- Depressive Symptoms and Dietary Adherence in Patients With End-Stage Renal DiseaseDocument10 pagesDepressive Symptoms and Dietary Adherence in Patients With End-Stage Renal Diseasebasti_aka_slimNo ratings yet
- Hypertension in High Risk African Americans: Current Concepts, Evidence-based Therapeutics and Future ConsiderationsFrom EverandHypertension in High Risk African Americans: Current Concepts, Evidence-based Therapeutics and Future ConsiderationsNo ratings yet
- Psychological Aspects in Chronic Renal Failure: Review RticleDocument10 pagesPsychological Aspects in Chronic Renal Failure: Review RticleTry Febriani SiregarNo ratings yet
- Delirium in The Intensive Care Unit: ReviewDocument9 pagesDelirium in The Intensive Care Unit: ReviewCristopher Castro RdNo ratings yet
- Mazujnms v2n2p29 enDocument7 pagesMazujnms v2n2p29 enDoc RuthNo ratings yet
- Blood Works: An Owner's Guide: What Every Person Needs to Know BEFORE They Are a PatientFrom EverandBlood Works: An Owner's Guide: What Every Person Needs to Know BEFORE They Are a PatientRating: 5 out of 5 stars5/5 (1)
- Nihms 1021376 PDFDocument15 pagesNihms 1021376 PDFBasilio Papuico RomeroNo ratings yet
- Geriatric Depression: Stephen C. Cooke and Melissa L. TuckerDocument13 pagesGeriatric Depression: Stephen C. Cooke and Melissa L. TuckerDini indrianyNo ratings yet
- National Nutrition and Health Sur Vey (Nnhes) : Atherosclerosis - Related Diseases and Risk FactorsDocument11 pagesNational Nutrition and Health Sur Vey (Nnhes) : Atherosclerosis - Related Diseases and Risk FactorsGene Alfonso BanawaNo ratings yet
- Quality of Life and Depression in CKD: Improving Hope and HealthDocument4 pagesQuality of Life and Depression in CKD: Improving Hope and HealthDani ursNo ratings yet
- Delirium: Acute Brain Dysfunction in the Critically IllFrom EverandDelirium: Acute Brain Dysfunction in the Critically IllChristopher G. HughesNo ratings yet
- UncertaintyDocument16 pagesUncertaintymaya permata sariNo ratings yet
- Komorbid 1Document15 pagesKomorbid 1ErioRakiharaNo ratings yet
- Dual - Diagnosis - Alcoholism - and - Co - Morbid PDFDocument15 pagesDual - Diagnosis - Alcoholism - and - Co - Morbid PDFalexandra mariaNo ratings yet
- Factors Associated With Depression and Anxiety of Hospitalized Patients With Heart FailureDocument10 pagesFactors Associated With Depression and Anxiety of Hospitalized Patients With Heart FailureineNo ratings yet
- Cardiorenal Syndrome in Heart FailureFrom EverandCardiorenal Syndrome in Heart FailureW. H. Wilson TangNo ratings yet
- Depresi CKD 2Document4 pagesDepresi CKD 2sufaNo ratings yet
- 11 Health-Related Quality of Life and Depression ArtritisDocument10 pages11 Health-Related Quality of Life and Depression ArtritisSilvia OliveraNo ratings yet
- The Prevalence of Diabetic Retinopathy and Associated Risk Factors Among Sioux IndiansDocument3 pagesThe Prevalence of Diabetic Retinopathy and Associated Risk Factors Among Sioux IndiansTrx AntraxNo ratings yet
- Depression and Increased Mortality in Diabetes: Unexpected Causes of DeathDocument8 pagesDepression and Increased Mortality in Diabetes: Unexpected Causes of DeathAna LemesNo ratings yet
- 1830 PDF PDFDocument5 pages1830 PDF PDFDexter BluesNo ratings yet
- Experiences of Adolescents Living with Type 1 Diabetes Mellitus whilst Negotiating with the Society: Submitted as part of the MSc degree in diabetes University of Surrey, Roehampton, 2003From EverandExperiences of Adolescents Living with Type 1 Diabetes Mellitus whilst Negotiating with the Society: Submitted as part of the MSc degree in diabetes University of Surrey, Roehampton, 2003No ratings yet
- Rethinking Diabetes: Entanglements with Trauma, Poverty, and HIVFrom EverandRethinking Diabetes: Entanglements with Trauma, Poverty, and HIVNo ratings yet
- Anxiety and Depression in Patients With Coronary Heart Disease: A Study in A Tertiary HospitalDocument6 pagesAnxiety and Depression in Patients With Coronary Heart Disease: A Study in A Tertiary Hospitalcindyaperthy22No ratings yet
- When Lightning Strikes: An Illustrated Guide To Stroke Prevention And Re coveryFrom EverandWhen Lightning Strikes: An Illustrated Guide To Stroke Prevention And Re coveryNo ratings yet
- Iraqi JMSDocument5 pagesIraqi JMSsarhang talebaniNo ratings yet
- Heart Failure With Comorbid Dementia Association With Clinical CharacteristicsDocument7 pagesHeart Failure With Comorbid Dementia Association With Clinical Characteristicsagar agarNo ratings yet
- The Association Between Insomnia and Cardiovascular DiseasesDocument8 pagesThe Association Between Insomnia and Cardiovascular Diseasesnouval_iqbalNo ratings yet
- 2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in Ca1Document17 pages2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in Ca1Angie OvandoNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 12: NeurologyFrom EverandComplementary and Alternative Medical Lab Testing Part 12: NeurologyNo ratings yet
- Symptom Clusters in Men and Women With Heart Failure and Their Impact On Cardiac Eventyfree SurvivalDocument10 pagesSymptom Clusters in Men and Women With Heart Failure and Their Impact On Cardiac Eventyfree Survivalabraham rumayaraNo ratings yet
- Killer Diseases, Modern-Day Epidemics: Keys to Stopping Heart Disease, Diabetes, Cancer, and Obesity in Their TracksFrom EverandKiller Diseases, Modern-Day Epidemics: Keys to Stopping Heart Disease, Diabetes, Cancer, and Obesity in Their TracksNo ratings yet
- Depresi Dan Kualiti Hidup Kesihatan Pesakit Buah Pinggang TahapakhirDocument14 pagesDepresi Dan Kualiti Hidup Kesihatan Pesakit Buah Pinggang Tahapakhire-BANGINo ratings yet
- Depression and Anxiety in Hemodialysis PatientsDocument5 pagesDepression and Anxiety in Hemodialysis PatientsIJAR JOURNALNo ratings yet
- Fatigue in A Cohort of Geriatric Patients With and Without Parkinson's DiseaseDocument5 pagesFatigue in A Cohort of Geriatric Patients With and Without Parkinson's DiseaseOcisa ZakiahNo ratings yet
- PsihiatrieDocument43 pagesPsihiatrieAdina OlteanuNo ratings yet
- ASCP Corner Increased Risk of Cerebrovascular Adverse Events and Death in Elderly Demented PatienDocument1 pageASCP Corner Increased Risk of Cerebrovascular Adverse Events and Death in Elderly Demented PatienSantosh KumarNo ratings yet
- The Expert Guide to Beating Heart Disease: What You Absolutely Must KnowFrom EverandThe Expert Guide to Beating Heart Disease: What You Absolutely Must KnowNo ratings yet
- Erectile Dysfunction and Comorbid Diseases, Androgen Deficiency, and Diminished Libido in MenDocument7 pagesErectile Dysfunction and Comorbid Diseases, Androgen Deficiency, and Diminished Libido in MenAfif Al FatihNo ratings yet
- Manual of Outpatient CardiologyFrom EverandManual of Outpatient CardiologyJohn D. BisognanoNo ratings yet
- Fast Facts: Psychosis in Parkinson's Disease: Finding the right therapeutic balanceFrom EverandFast Facts: Psychosis in Parkinson's Disease: Finding the right therapeutic balanceNo ratings yet
- Cardiac Failure Explained: Understanding the Symptoms, Signs, Medical Tests, and Management of a Failing HeartFrom EverandCardiac Failure Explained: Understanding the Symptoms, Signs, Medical Tests, and Management of a Failing HeartNo ratings yet
- Anxiety PaperDocument3 pagesAnxiety Paperapril2001100% (2)
- PIIS0002934311002920 CGHDocument10 pagesPIIS0002934311002920 CGHJulianda Dini HalimNo ratings yet
- Prevalence of Depression Among Patients With Multiple Sclerosis in Erbil CityDocument10 pagesPrevalence of Depression Among Patients With Multiple Sclerosis in Erbil Citysarhang talebaniNo ratings yet
- Mitchell Et All 2011 Prevalence Depression Anxiety Oncoligical HaematologicalDocument15 pagesMitchell Et All 2011 Prevalence Depression Anxiety Oncoligical HaematologicalGuillermoNo ratings yet
- Back To Psychopharmacology - The Fourth Generation of ProgressDocument6 pagesBack To Psychopharmacology - The Fourth Generation of ProgressJose ValentinNo ratings yet
- Evaluation of Depression and Suicidal Patients in The Emergency RoomDocument15 pagesEvaluation of Depression and Suicidal Patients in The Emergency RoomjuanpbagurNo ratings yet
- NIH Public Access: Frailty and Depression in Older Adults: A High-Risk Clinical PopulationDocument21 pagesNIH Public Access: Frailty and Depression in Older Adults: A High-Risk Clinical PopulationBasilio Papuico RomeroNo ratings yet
- JournalsDocument11 pagesJournalsrachmaniabudiatiNo ratings yet
- ESCALA de Somnolencia de Epworth en Un Centro de Salud FamiliarDocument10 pagesESCALA de Somnolencia de Epworth en Un Centro de Salud FamiliarEnith VilelaNo ratings yet
- A Review of Bipolar Disorder Among Adults PDFDocument13 pagesA Review of Bipolar Disorder Among Adults PDFNadyaNo ratings yet
- Determining Quality of Life and Sleep in Hemodialysis PatientsDocument5 pagesDetermining Quality of Life and Sleep in Hemodialysis PatientsTry Febriani SiregarNo ratings yet
- QoL CKD - Cruz Et AlDocument5 pagesQoL CKD - Cruz Et AlTry Febriani SiregarNo ratings yet
- AhmedDocument6 pagesAhmedTry Febriani SiregarNo ratings yet
- Psychological Aspects in Chronic Renal Failure: Review RticleDocument10 pagesPsychological Aspects in Chronic Renal Failure: Review RticleTry Febriani SiregarNo ratings yet
- "If You Want To Go Fast, Go Alone. If You Want To Go Far, GoDocument1 page"If You Want To Go Fast, Go Alone. If You Want To Go Far, GoTry Febriani SiregarNo ratings yet
- Gambaran Tingkat Depresi Pada Pasien Gagal Ginjal KronikDocument19 pagesGambaran Tingkat Depresi Pada Pasien Gagal Ginjal KronikGupiesNo ratings yet
- Pediatric Acute Respiratory Distress SyndromeDocument2 pagesPediatric Acute Respiratory Distress SyndromeTry Febriani SiregarNo ratings yet
- TaeyangDocument9 pagesTaeyangTry Febriani SiregarNo ratings yet
- PartingDocument3 pagesPartingTry Febriani SiregarNo ratings yet
- Until It's GoneDocument5 pagesUntil It's GoneTry Febriani SiregarNo ratings yet
- Sakurai MinamiDocument11 pagesSakurai MinamiTry Febriani SiregarNo ratings yet
- Arashi Ni Shiyagare With GacktDocument1 pageArashi Ni Shiyagare With GacktTry Febriani SiregarNo ratings yet
- Last Flower - RadioheadDocument2 pagesLast Flower - RadioheadTry Febriani SiregarNo ratings yet
- NIJIIRIDocument1 pageNIJIIRITry Febriani SiregarNo ratings yet
- Best DoramaDocument1 pageBest DoramaTry Febriani SiregarNo ratings yet
- On The SubwayDocument2 pagesOn The SubwayTry Febriani SiregarNo ratings yet
- MaterialDocument3 pagesMaterialTry Febriani SiregarNo ratings yet
- Yoon Jong Shin Collaboration WDocument5 pagesYoon Jong Shin Collaboration WTry Febriani SiregarNo ratings yet
- 2NE1Document6 pages2NE1Try Febriani SiregarNo ratings yet
- What Is An Inevitable AbortionDocument1 pageWhat Is An Inevitable AbortionTry Febriani SiregarNo ratings yet
- 200Document4 pages200Try Febriani SiregarNo ratings yet
- MeltedDocument2 pagesMeltedTry Febriani SiregarNo ratings yet
- Skenario F Blok 23 Tahun 2014Document9 pagesSkenario F Blok 23 Tahun 2014Try Febriani SiregarNo ratings yet
- Winner CoverDocument4 pagesWinner CoverTry Febriani SiregarNo ratings yet
- Bom and HayiDocument3 pagesBom and HayiTry Febriani SiregarNo ratings yet
- WINNER's Cover of YB's "Flying Butterfly"!: EnglishDocument4 pagesWINNER's Cover of YB's "Flying Butterfly"!: EnglishTry Febriani SiregarNo ratings yet
- LordeDocument6 pagesLordeTry Febriani SiregarNo ratings yet
- Complications of RDS: o o o oDocument1 pageComplications of RDS: o o o oTry Febriani SiregarNo ratings yet
- Winner CoverDocument4 pagesWinner CoverTry Febriani SiregarNo ratings yet
- Understanding Nursing Research - Burns Chapter 1Document11 pagesUnderstanding Nursing Research - Burns Chapter 1sylphlike5100% (1)
- Cognitive Therapy From The Inside, James Bennett-LevyDocument16 pagesCognitive Therapy From The Inside, James Bennett-Levysusie cabrillanaNo ratings yet
- Spine Lumbar Low Back Core ExercisesDocument2 pagesSpine Lumbar Low Back Core Exercisessmnabeel100% (1)
- Word HNPDocument14 pagesWord HNPALan ButukNo ratings yet
- Checklist: Aspiration/Aspiration PneumoniaDocument3 pagesChecklist: Aspiration/Aspiration PneumoniaWienaIbunyaKevinNo ratings yet
- Cognitive Behavioral TherapyDocument5 pagesCognitive Behavioral Therapynosheen murtazaNo ratings yet
- 50 State Survey - Scope - 07.2015Document85 pages50 State Survey - Scope - 07.2015Anonymous kdBDppigENo ratings yet
- Graviola - Secret Cancer CureDocument10 pagesGraviola - Secret Cancer CureRegina E.H.Ariel100% (3)
- Restraints AssignmentDocument6 pagesRestraints Assignmentapi-284091020100% (1)
- Cardiorenal SyndromeDocument21 pagesCardiorenal SyndromeAndy McCulloughNo ratings yet
- ENLS V4.0 ICH Manuscript FINAL PDFDocument15 pagesENLS V4.0 ICH Manuscript FINAL PDFkoko komarudinNo ratings yet
- AIDS and PeriodontiumDocument25 pagesAIDS and PeriodontiumKarthik Krishna M100% (1)
- Laser IsmDocument13 pagesLaser Ismapi-266989440No ratings yet
- Respiratory Physiology AnswersDocument4 pagesRespiratory Physiology AnswersRamya100% (3)
- Marketing I - Price ListDocument3 pagesMarketing I - Price ListthimotiusNo ratings yet
- Diagnose of Submandibular Abscess PDFDocument13 pagesDiagnose of Submandibular Abscess PDFElvitrianaNo ratings yet
- HEMATOCHEZIADocument26 pagesHEMATOCHEZIAAlvin HartantoNo ratings yet
- Child PPT Conference MineDocument28 pagesChild PPT Conference MineSeerat FatimaNo ratings yet
- JAM2Document80 pagesJAM2Nicoleta Florentina GhencianNo ratings yet
- Aaron Beck: Psychology BiographiesDocument3 pagesAaron Beck: Psychology BiographiesNiniNo ratings yet
- About Company: Its Balance SheetDocument14 pagesAbout Company: Its Balance SheetVeekeshGuptaNo ratings yet
- Drugs That Require Frequent MonitoringDocument22 pagesDrugs That Require Frequent MonitoringNader Smadi100% (7)
- Class 1 Introduction To Clinical PharmacologyDocument33 pagesClass 1 Introduction To Clinical Pharmacologymustafa 1No ratings yet
- Implicit Memory and MetacognitionDocument22 pagesImplicit Memory and MetacognitionMonica SanduleanuNo ratings yet
- 1.D/D of Intraconal Mass 2.D/D of Leucocoria 3.U/S & CT Findings of RB 4.how Will You Manage That CaseDocument15 pages1.D/D of Intraconal Mass 2.D/D of Leucocoria 3.U/S & CT Findings of RB 4.how Will You Manage That CaseMuhammad SharjeelNo ratings yet
- TommatisDocument9 pagesTommatisAldo PrietoNo ratings yet
- Providing Oral CareDocument54 pagesProviding Oral CareErcel ArellanoNo ratings yet
- Daftar Harga ObatDocument2 pagesDaftar Harga ObatHadi SetiawanNo ratings yet
- Asthma PDFDocument2 pagesAsthma PDFtriwantiNo ratings yet
- First Steps in REBT - Windy DrydenDocument44 pagesFirst Steps in REBT - Windy DrydenStefan Alexandru100% (4)