Professional Documents
Culture Documents
Berkemeyer 2009
Uploaded by
Dianne Faye ManabatCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Berkemeyer 2009
Uploaded by
Dianne Faye ManabatCopyright:
Available Formats
Medical Hypotheses 73 (2009) 347356
Contents lists available at ScienceDirect
Medical Hypotheses
journal homepage: www.elsevier.com/locate/mehy
Acidbase balance and weight gain: Are there crucial links via protein
and organic acids in understanding obesity?
Shoma Berkemeyer *
Ruhr-Universitt-Bochum, Klinik fr Altersmedizin und Frhrehabilitation, Studienbro, Room 23, Widumerstr. 8, 44627 Herne, Germany
a r t i c l e
i n f o
Article history:
Received 9 September 2008
Accepted 12 September 2008
s u m m a r y
Obesity is associated with ever increasing social costs posing a general public health challenge. The most
obvious reason for obesity, given healthy body functioning, is a positive calorie balance. This article
delves into the lesser studied realm of the relationship of weight gain, in particular adipose tissue gain,
with increased hydrogen ion concentration, taking protein and organic acids as important caveats in this
discussion. The review opens the topic with the contradictory result of various studies reporting a positive relationship between chronic metabolic acidosis and weight loss. It goes to explain a process of
weight gain, primarily adipose tissue gain, on acidogenic diets. Insufficient dietary protein could lead
to muscle loss, and individual organic acids might indicate if there is any fatty acid oxidation or accumulation of hydrogen ion. The solution to the acid accumulation is discussed not in protein limitation but an
increase in the consumption of vegetables and fruits. Finally, this review article based on studies published puts forward a physiological basis including a hypothesis to explain the possible link between
hydrogen ion concentration and weight gain. This link could possibly explain the development of diseases
and aging partially, and warrants research.
! 2009 Elsevier Ltd. All rights reserved.
Introduction
Obesity is a known risk factor for diseases, such as, diabetes,
insulin resistance, cardiovascular diseases, and hypertension. The
number of people with obesity is increasing [1]. Obesity is also observed in childhood and adolescence [2,3]. Likewise, the number of
people with diseases such as, diabetes, insulin resistance, cardiovascular diseases, and hypertension are also increasing with earlier
disease onsets [46]. These trends have translated into increasing
public health concerns with greater efforts towards strategies for
their prevention.
The most obvious reason for weight gain, in the absence of diseases or malfunctions, is a positive energy balance. The Western
diet [7], a diet rich in calories, acid load, sodium salt, and glycemic
index but poor in fibers [810], is a foremost example of the modern
day dietary practice. Western diets health and disease consequences are currently under scientific investigation, primarily over
an unfavorable acidbase balance (ABB) [826]. This Western diet
is, however, not only characterized by high acid load but also calorie, so that, ABB and obesity could be related. This review focuses
and updates the current level of knowledge on the relationship of
ABB and weight gain or weight loss (WG or WL). It builds on the
caveats of protein consumption and organic acids on Western diets
to elucidate the relationship between ABB and WG or WL. Finally, it
* Tel.: +49 2323 4992622; fax: +49 2323 4992621.
E-mail address: shoma.berkemeyer@ruhr-uni-bochum.de
0306-9877/$ - see front matter ! 2009 Elsevier Ltd. All rights reserved.
doi:10.1016/j.mehy.2008.09.059
puts forward a hypothesis which might be a crucial link in understanding obesity warranting scientific investigation.
Section Weight gain or weight loss on chronic metabolic acidosis? of the review begins with the discussion on the reported WL on
chronic metabolic acidosis. Section Weight gain on acidogenic
diets updates on the association of acidogenic diets and WG. Protein and organic acids are important confounders in the understanding of ABB and WL or WG. Sections The protein conundrum
and The organic acid conundrum addresses to these issues. Finally,
section A culmination of acidosis and weight gain, given the caveats of protein and organic acids, from published literature brings
together the entire concept of WG and/or WL and ABB, via Western
diet, by putting forward a hypothesis as well. Studies are reported
that support the concept of WG via fat increase and the blood
hydrogen ion concentration or protons (H+). For this study, H+ has
been defined as a generalization to mean the total acid load, barring
section A culmination of acidosis and weight gain, given the caveats of protein and organic acids, from published literature and Table 1, where blood H+ is used to denote the blood free hydrogen ion
concentration.
Weight gain or weight loss on chronic metabolic acidosis?
Blood pH is highly regulated [27] and maintained within the narrow normal range of 7.367.44. Thus, when the blood pH dips below
the clinical normal, it would have been well preceded by various
body compensatory and adjustment processes, which ultimately
348
S. Berkemeyer / Medical Hypotheses 73 (2009) 347356
Table 1
Synopsis of cellular studies on the relationship of obesity and cellular pH.
Author
Year
Journal
Disease
Conclusion
Positive association
Kaloyianni et al.
2001
Cell Phyiol Biochem
IR, Ob
NHE increases Na influx into cell by H+ efflux out of cell
Obese have lower cellular pH
Konstantinou-Tegou
et al.
2001
Mol Cell Endocrinol
Ob
Increase in adipose tissue perhaps linked to cardiovascular complications of Ob
Obese have lower cellular pH
Koren et al.
Aviv
Resnick
1997
1992
1992
Diabetologia
J Am Soc Nephrol
Am J Med
NIDDM
IR, HT, NIDDM
Ob, NIDDM,
HT
Increased cellular acidity might result in proteinuria
Increased NHE activity associated with increased free Ca in cells
Increased NHE activity associated with increased free Ca but lower Mg in cells
Resnick et al.
1991
Hypertension
Ob, NIDDM,
HT
Increased NHE activity not only increase cellular Na but also Ca, but lowers Mg
HT is associated with lower cellular pH
Negative association
Treuth et al.
2001
Ob
Family history of obesity does not change skeletal muscle energetics or cellular pH
Ghigo et al.
1994
Int J Obes Relat Metab
Disord
Eur J Clin Invest
Ob, DM2, HT
Increased NHE activity (increased cytosolic Na and higher alkaline pH) in HT but not DM2
or Ob
Abbreviations: IR, insulin resistance; HT, hypertension; Ob, obesity; NIDDM, non insulin dependent diabetes mellitus; DM2, diabetes mellitus type 2; H+, proton; NHE, sodium
hydrogen (H+) exchanger; Ca, calcium; Mg, magnesium, P(i)/PCr, intracellular phosphate to phosphocreatine ratio; pH(i), cellular pH.
could not avert the decline. That is to say, a blood pH change (opposed to fluctuations) is a long-term, slow change. A blood pH constantly at the lower end of the normal range has been termed latent
acidosis [28]. A blood pH constantly at or below 7.35 is clinically defined as chronic metabolic acidosis, which is known as a stress situation for the body [29].
Undernutrition, associated with WL, is characterized by accompanying metabolic acidosis. A classical example of undernutrition
is protein calorie malnutrition (PCM) per se or secondary to chronic
renal diseases (CRD) [2934]. It is known that starvation diets induce endogenous ketosis [35]. Patients of childhood epilepsy are
prescribed a ketogenic diet, which is known to slow weight gain
[36]. To generalize: undernutrition, e.g., PCM, CRD, starvation,
etc., is widely reported to be associated with acidosis, evenso this
result is not without contradiction. A review by Kalantar-Zadeh
et al. [32] elucidates the contradiction succinctly. Evidence from
metabolic studies suggest that metabolic acidosis is related to
WL through increased protein catabolism, which in turn is due to
increased activity of adenosine triphosphate (ATP)-dependent
ubiquitin-proteasome and ketoacid dehydrogenase. In contrast,
epidemiologic studies (on maintenance dialysis patients) suggest
that lower blood pH is associated with improved status of PCM.
In other words low blood pH is associated with WG. Finally, interventional studies yielded inconsistent results. To recapitulate,
there is the concept of WL on chronic metabolic acidosis, which
is not without contradiction as studies have also indicated WG,
or maintenance, on chronic metabolic acidosis. A statement of causality appears pertinent to the issue. Metabolic studies show
undernourishment leads to WL and metabolic acidosis due to catabolic stress [29]. The metabolic acidosis observed in affected population groups in epidemiological studies does not let infer
causality.
The concept of metabolic acidosis leading to low WG is perhaps
best documented in pediatric studies on preterm or low birth
weight term infants [17,3741]. This infant group requires greater
protein intake for catch-up growth, which is usually provided by
fortified human milk or formula milk. Studies have put forward
that the high protein intake of formula milk promotes the development of metabolic acidosis, which promotes WL instead of WG.
Hence, these studies suggest an alkali supplementation along with
formula milk to neutralize the excess H+ and promote growth.
Studies have also reported WG in infants on higher protein diets
[4244]. The protein supplement is thought to engender positive
protein balance through anabolic effects via growth hormone,
insulin-like growth factor I, carnitine and steroids [33]. These
above results introduce the protein conundrum, i.e., is protein
harmful or beneficial in terms of ABB, and this will be taken up
in the section Weight gain on acidogenic diets.
Like in the case of CRD, cases of low birth weight and preterm
infants are a group that are already affected by less than optimal
growth. Thus, therapy effects of protein diets in undernourished
people to achieve optimal growth and/or development with the
accompanying metabolic acidosis can be regarded in a slightly different light as excess protein and/or calorie consumption and a
metabolic acidosis thereof due to a diet of plenty. Finally, chronic
metabolic acidosis associated WL might be a characterization of
undernutrition, rather than the acidosis, since acidosis can be also
related to WG.
Weight gain on acidogenic diets
It is necessary to distinguish between the body endogenous
chronic metabolic acidosis and an acidogenic diet, since the two
terms are not synonymous [45]. An acidogenic diet is associated
with the increased probability to raise the bodys H+ load [7], if
the various compensatory and adjustment processes are exhausted. Chronic metabolic acidosis, however, is the condition,
when the development has gone as far, signaling a disequilibrium
in the ABB. It remains to be evaluated whether an increase in H+,
neither captured by a blood pH decline nor compensated via the
renal or the respiratory route, but, e.g., stored in cells instead, is
a welcome development in itself. Table 1 is a synopsis of cellular
studies showing the relationship of obesity to cellular pH along
with the convergence of ill-conditions of hypertension, diabetes,
and insulin resistance.
The first five studies in Table 1 shows that the concurrence of
obesity, hypertension, insulin resistance have been related to the
same underlying cellular basis, i.e., a generalized defect in cell
ion handling, specifically the sodium hydrogen exchangers (NHE).
NHE allows the exchange of intracellular proton with extracellular
sodium, with one study reporting hypertension to be associated
with lower cellular pH, i.e., less sodium influx into the cell [46].
A lower cytosolic pH has been observed by some study groups in
obese subjects [47,48] with a study reporting that it could lead
to protein loss in urine [49]. The latter study supports the concept
349
S. Berkemeyer / Medical Hypotheses 73 (2009) 347356
of muscle loss in metabolic acidosis due to endogenous protein
catabolism [32]. Obese individuals had lower cytosolic free magnesium with higher free calcium compared to normal individuals
[46,50,51] supporting an ionic hypothesis in diseases development, explaining the concurrence of obesity, hypertension, and
insulin resistance. An ionic base is central to ABB [14,22,45]. Thus,
this ionic base could be a common pathway linking ABB with the
development of obesity, hypertension, insulin resistance, partially
explaining the development of diseases on consumption of acidogenic diets due to a longer term disequilibrium H+, indirectly, the
anions and cations.
Epidemiological studies on the relationship of H+ and WG are
few. Three studies on patients with renal stones reported an inverse relationship between measures of WG (BMI or weight) and
the urine pH [5254] (Table 4), so that as H+ is higher there should
be greater weight (WG). An experimental study on otherwise
healthy but obese subjects [55] reported that on a protein-free diet,
obese individuals excreted more H+ in the urine than could be accounted for by oxidation of sulfur to sulfate. Sulfur from protein is
a chief contributor to the bodys acid load [45]. In other words,
there is a loss of endogenous protein, i.e., muscle mass, even so
the subjects are obese on protein deficient diets. That is, in total
there is WG (obesity), even so there is WL as far as muscle mass
(endogenous protein loss) is concerned. This corroborates the reported WL on undernutrition [32].
Another clinical study reported the acidbase responses to a
hypoenergetic protein and a hypoenergetic glucose diet, in obese
individuals [56]. The protein diet resulted in mild acidosis, greater
excretion of urinary ammonium and urea nitrogen, and ketosis but
with better nitrogen balance compared to the glucose diet. A subsequent fast resulted in greater acidosis in the glucose meal group
than in the protein group. This suggests, long-term consumption of
calorie reduced, protein-poor diets would possibly result in poor
nitrogen balance (nitrogen and weight loss to that extent) with
development of acidosis, even so in total obese.
Clinical studies have reported a greater loss of magnesium on
acidogenic diets [55,57] and a fall in blood pH in response to acidogenic diets [58]. Observational studies on community dwelling
healthy young adults and healthy elderly corroborate the loss of
magnesium with higher dietary acid loads [59] and that urine pH
is inversely associated with BMI (WG) and directly with muscle
mass [60].
To generalize, cellular studies report obese people had lower
cellular pH compared to normal weight (Table 1). Results reported
by Frassetto et al. [58] let infer a somewhat causal role of Western
diet in the blood pH decline in healthy people. The remaining body
of studies indicate that the Western diets are associated with lower
pH and obesity. It is hence appropriate to reconsider the core biochemicalphysiological dynamics of this relationship.
Undernutrition implies emaciation and general tissue loss, muscles and fat, to provide endogenous sources of energy. In undernutrition the muscle loss would also partly supply ammonia, to buffer
and excrete the acid load [58], a sizable amount being also the organic ketoacids. The body would use fat stores and have a higher
rate of beta oxidation. These processes would lead to general tissue
loss (WL), with accompanying metabolic acidosis as reported in the
section Weight gain or weight loss on chronic metabolic acidosis?.
Acidogenic diet is a dietary pattern subsequent to civilization
process, i.e., a change from hunters and food-gatherers to agriculturalists to industrialization, and post-industrialization [7].
Thus, Western diet is a dietary concept of nutrition in plenty.
The combination of high acid and high energy consumption on
Western diet supports development of acidosis with time (age)
and down-regulation of fatty acid oxidation since the diet is energy rich (glucose preferred energy substrate). A certain amount
of muscle protein loss, as endogenous ammonia buffer, could
Western diet
Acidosis
(latent &/ metabolic)
(volatile &/ fixed acid
Ill-conditions
Diseases
Aging
Fig. 1. The straight line hypothesis of diet, acidosis, and aging.
accompany the process to neutralize the acid load, acerbated on
protein deficient diet. It could be for such reasons that Jourdan
et al. [55] reported that obese people on protein-free diets excreted greater amounts of H+ as could be accounted by dietary intake of sulfur (protein) [55]. That is, if there is insufficient dietary
protein intake there will be muscle loss, irrespective of whether
the person is obese or underweight, hence a poor nitrogen balance [56]. If diet is additionally characterized by high energy
intake, as in Western diets, it implies only a concomitant accumulation of fat mass (WG), at a loss of endogenous muscle protein
(WL). In fact, the ratio of fat to muscle mass might increase over
time. So, a relatively healthy person on Western diet would run
the risk of losing muscle relative to fatty tissue; possibly becoming relatively obese in the longer run, which would be acerbated
on a low to no protein diet. If a sub-clinical latent metabolic acidosis would set in, the dietary life-style dependent acidosis itself
would further support the latent acidosis, since before a complete
recovery or adjustment can occur the next food intake would take
place. In the longer run, this could lead to a metabolic acidosis but
a metabolic acidosis of plenty (Fig. 1), which would be different
from the metabolic acidosis of undernutrition. Both routes to acidosis implies body stress, and hence a certain amount of stress related catabolic processes [29,32], i.e., muscle breakdown. The over
or malnutrition related acidosis, when unchecked, can be visible
as disease complications (hypertension, diabetes, cardiovascular
diseases) with time (age), which has been termed as the cascade
effect [22].
The protein conundrum
A discussion of the dietary protein emerges somewhat central
to the understanding of the concept of WG or WL in relation to acid
load. It is well-known that the dietary proteins are one the chief
sources of the dietary acid load [45], especially in the form of
methionine and cysteine. Methionine and cysteine are some of
the few amino acids containing sulfur, the sulfur contributing to
the dietary nonvolatile, fixed acid load [45]. This has been a reason
to recommend animal protein limited diets [16], in order to control
the dietary source of acids [26]. The strong sulfuric acid, when in
excess of body requirements, requires to be excreted, one of the
many reasons why CRD patients are also recommended protein
limited diets.
A protein duality in acidbase studies has been reported [61].
Protein increases the total acid load but also allows the kidneys
to increase their net acid excretion capacity (NAEC), so that the
body can excrete the excess H+. This is a normal body compensatory process. Cysteine (a hydrophobic amino acid with a sulfhydryl
group) is found in most protein sources but in very small quantities. Usually, therefore, it requires to be synthesized in the liver
from methionine, an essential amino acid. Rich sources of methionine are meats, fishes, cottage cheese, to name the important. The
very cysteine that contributes to the non-volatile acid load is also
the rate-limiting step in the production of glutathione, the most
common intracellular antioxidant, protecting cells from oxidative
stress and cell death [6264]. Animal studies show that an ade-
350
S. Berkemeyer / Medical Hypotheses 73 (2009) 347356
quacy of the dietary sulfur amino acids determines the extent to
which antioxidant defenses are maintained during inflammation
[65]. This could exactly be a means to maintain a healthy aging
process, since aging is associated with net altered gene expression
leading possibly to a net higher production of reactive oxygen species (ROS) with time [66,67]. In fact, gerontology studies prescribe
a consumption of adequate amounts of dietary protein from high
quality sources as an important means to slow down or treat sarcopenia [68]. Interestingly, elderly compared to younger subjects
had a depressed response to stimulation of muscle protein synthesis following administration of mixed meals due to a decreased
ability to respond to anabolic stimuli, such as insulin. Likewise,
the anabolic effect of amino acids seems blunted on low protein
doses [69]. To summate, proteins are the building blocks of the
body and while ad lib over-consumption, as with all excesses,
would have deleterious consequences, it still does not gainsay an
adequate requirement of it at all ages.
Taking another example of wasting in HIV/AIDs, which is characterized by loss of cysteine, methionine, and carnitine, it is known
that the carnitine is synthesized from cysteine and lysine. Carnitine
is normally found in high levels in muscles and is responsible for
the transport of long-chain fatty acids into mitochondria for beta
oxidation. Thus, a dearth of cysteine or in general high quality
proteins could mean a reduction in the amount of glutathione antioxidant, and possible accumulation of adipose tissue, which a low
to no protein intake, quantity and quality, would only acerbate.
Regulated protein consumption, including high quality red meats,
would help maintain carnitine and glutathione levels. A third
example would be in maintenance of the bone-protein-collagenmatrix [70,71]; even so excessive consumption of the non-neutralized dietary proteins could result in bone calcium leaching
[11,12,19,23,24,72]. The lack of adequate concomitant consumption of alkalis (vegetables and fruits, base supplements), rather
than the protein, is probably responsible for the leaching [73],
which is characteristic of Western diet [7,26,58,74]. This reduction
in alkali consumption is possibly what needs rectification [19]
rather than decreasing protein consumption.
Western diet
The organic acid conundrum
It has been recently shown that healthy people had a more-orless constant total organic acid excretion on mixed diets once body
surface area was factored out [75]. The reasons for such an observation are not very well understood. Organic acid excretion is partially diet-dependent, as already successfully demonstrated [45].
Thus, the formula for endogenous total organic acid production
[45] (Eq. (1)), often extrapolated for organic acid excretion, shows
it to be a function of dietary intakes of acids (excluding sulfur),
termed as the dietary unmeasured anion:
OAdiet 32:9 0:15 $ Dietary unmeasured anions
where,
Dietary unmeasured anions Na K Ca2 Mg2
&
& Cl 1:8PO4
Empirically it is well-proven that with higher dietary ingestion
of acids there is higher urinary excretion of it as well, i.e., the net
acid excretion (NAE) is higher. NAE is directly measured in urine
by summing up titratable acidity and ammonium, and subtracting
the bicarbonate. A measurement of total organic acids excretion in
healthy people commenced principally because, apart from sulfur
and phosphates, it was identified as the third most important component of the bodys NAE [45]. Thus, with higher dietary intakes of
acids, the NAE is also higher. It is possibly for such reasons that it is
understood that the excretion of sulfur, phosphates, and total organic acids is also higher. This is supported by the fact that the dietary intake dependent excretion of each of these components
cannot be disregarded. But while this might hold good for sulfur
and phosphates, there is reason to believe that this is physiologically not completely the case for organic acids, as supported by
the empirical finding of a largely constant total organic acid excretion in health, having accounted for body size [75].
The body endogenous production of organic acids, either due to
metabolism of dietary intakes and/or endogenous metabolic processes, is rather difficult to estimate due to the ready conversion
Lactic acid increases,
most of lactate converted
into CO 2, some to fat and
glycogen
Respiratory alkalosis
Cell lactic acid produced
Mild proton retention
CO2 increases, hypercapnia
Mild cellular
acidity at normal
blood pH
Respiratory acidosis
Activation of hypoxic /
hypercapnic
chemoreflex
Mild inhibition of
mitochondrial energy
production
Hyperventilation,
(Obesity increased
hyperventilation)
Some pyruvate
accumulation
O2 increases
Fig. 2. The lactic acid trap.
Next Western meal
ingestion
Cell pH decrease a bit more
than the ph of the last cycle
Only regular consumption of
vegetables and fruits or alkali
dosage to get out of trap
S. Berkemeyer / Medical Hypotheses 73 (2009) 347356
of organic acids into carbon-dioxide and water and vice-versa. Organic acids, which are volatile acids, remain in a constant state of
flux in the body endogenous condition. Traditionally, individual organic acids are measured in urine in order to diagnose certain disease conditions, such as the inborn errors of metabolism, or
poisonings. The constant state of flux of endogenous organic acid
production renders the estimation of it with pitfalls. Yet in spite
the OAdiet is rather a reasonable estimate of total organic acid production (extrapolated for excretion) on net acid diets [75]. However, on net alkaline diets, OAdiet (Eq. (1)) predicts a negative
organic acid production, which might be physiologically not
tenable.
The organic keto acids
The keto acids are one the major endogenous organic acids. In
the 1980s there was a row of experiments conducted by Chalmers
et al. [76] which went to show that in relatively healthy subjects
the total organic acid excretion hardly varies. Another independent
study reported that the production of keto acids increases in subjects who ingested alkalis, specifically, sodium bicarbonate [77].
This implies if the body has a greater intake of dietary net alkalis,
the body produces more organic keto acids of purely endogenous
origin. Thus, a relative constancy in organic acid excretion having
accounted for body size is possible even on net alkaline diets
[75]. The study by Hood et al. [77] reported that in conditions of
351
moderate acid load there was a reduction in organic keto acid production of endogenous origin. Thus, with acid ingestion it seems
that the body down-regulates endogenous production of organic
keto acids and would in preference excrete the exogenous, dietary
organic acids, thereby maintaining a relatively constant net organic
acid excretion, once corrected for body surface area. To that extent
OAdiet would then exaggerate the dietary alkalinity when calculating the net endogenous acid production [45], on net alkaline diets.
The other available formula (Eq. (2)) for total organic acids is
based on anthropometry (OAanthro) [75] and it estimates the total
organic acid excretion. In the process it avoids the pitfalls of estimating the endogenous production of organic acids, in that, it
never estimates it, but thereby provides a means to show that
the total organic acid excretion is largely a constant, having accounted body surface area:
OAanthro body surface area $ 41=1:73
where, 41 is the median daily organic acid anions excretion (mEq/d)
at an average body surface area of 1.73 m2 for healthy subjects.
The increase in endogenous keto acid production on alkaline
diets [77] so that the total organic acids remain largely a constant
[75] indicates a step-up in fatty acid oxidation on alkaline diets via
beta-oxidation. This could go some way to explain the weight
maintenance to WL on net alkaline diets; often higher vegetables
and fruits consumption compared to net acid diets, e.g., Western
diets. This suggests why possibly Western diets in the longer run
Table 2
A synopsis of relationship of hydrogen ion with weight gain in obese in comparison to normal controls.
Author
Year
Journal
Treatment
Conclusion
Epidemiological
Harper et al.
2002
Diabetes
Six weeks of 900 kcal meal
Proton leak correlate with weight loss success
Clinical
Gougeon et al.
1992
Am J Clin Nutr
Two very low calorie diet, with isocaloric
high and low quality proteins
Perhaps insufficient exogenous protein intake results in loss of muscle
tissue in obese
Gougeon-Reyburn et al.
1991
Am J Med Sci
Neutral to alkali intervention in
ketoacidosis (induced by very low energy
protein diets)
Excretion of magnesium associated with acidosis
Urinary acid load decrease with alkali supplementation
Gougeon-Reyburn et al.
1989
Am J Clin Nutr
Two hypoenergetic diets, one protein other
glucose
Second intervention: a fast following the
above diets
Dietary protein is net acid producing but also prevents the body from
going into negative nitrogen balance
Hood et al.
1988
Metabolism
Methionine, like ammonium chloride, results less endogenous ketoacid
excretion
Jakober et al.
1983
Hood et al.
1982
J Endocrinol
Invest
Am J Physiol
Intervention (methionine, ammonium
chloride, and sodium chloride) in
hypocaloric ketogenic fast
Exercise after prolonged starvation
Jourdan et al.
1980
Sonka et al.
Sodium bicarbonate and ammonium
chloride intervention after fasting
Prolonged starvation changes basal values of metabolites and hormones
but not their exercise induced shifts compared to normal
With increase in acid production less endogenous ketoacids are excreted
so that systemic acidbase status can exert feedback controls
Am J Clin Nutr
Metabolic unit for 63 days with differing
protein and calorie liquid formula diets
Increased loss of calcium and magnesium on acidogenic diets
Perhaps, both, protein intake and protein free diets increase acid excretion
1978
Endokrinolgoie
Administration of sodium bicarbonate
Fasting led to lipoylsis even in obese
The acidosis due to fasting can be corrected with intake of alkalies
Bray et al.
1977
Metabolism
Varying levels of exercise
Maybe overweight leads to hyperventilation
Overweight people seem to run the risk of developing insulin resistance
with higher blood pressures
Lack of enough growth hormone in overweight which could lead to lower
level of growth hormone functions
Goeschke et al.
1976
Res Exp Med
(Berl)
Four to six days of fasting
Lean women probably require higher alkali intake than their men
counterpart when fasting
Sapir et al.
1975
Metabolism
Total starvation
Possibly a constant organic acid excretion
Conservation of ketone bodies minimizes body protein loss, and prevents
large urinary losses of cations during prolonged starvation since
ammonium becomes the major cation excreted
Sapir et al.
1972
J Clin Invest
Consumption of minute quantities of
carbohydrate during prolonged starvation
Carbohydrate ingestion in starvation has nitrogen sparing effects by
reducing urinary ammonium excretion
The urinary ammonium excretion is possibly an indicator of tissue loss
352
S. Berkemeyer / Medical Hypotheses 73 (2009) 347356
could indirectly promote WG. A direct promotion of WG would be
simply due to the high energy intakes on Western diet as discussed
in the section Weight gain on acidogenic diets. Section Weight
gain on acidogenic diets also reported the study by Jourdan et al.
[55] which shows that inspite of obesity (WG) there was concomitant muscle loss (endogenous protein loss). This was explained as
relative obesity on Western diet in the section The protein
conundrum. The dynamics of this relative obesity could be further
linked to the hitherto not discussed organic lactic acid, and its production on Western diets.
The organic lactic acids
Lactic acid is another important endogenous organic acid. An
animal study reported that kidney and liver mitochondria, isolated
from acidotic murine models had lower mitochondrial energy production (MEP), than controls [78]. A human study reported an inhibition of the MEP in methylmalonic aciduria [79]. These studies
support a decline in MEP due to acidosis, hinting at inhibition of
the tricarboxy acid cycle (TCA), though not glycolysis. This implies
a collection of the organic pyruvic acid (pyruvate); normally referred to as incomplete carbohydrate metabolism. Pyruvate accumulation would lead to increased levels of the organic lactic acid
(lactate), not associated with physical exercise. All tissues can produce lactate under anaerobic conditions (hypoxia) but tissues with
active glycolysis, e.g., muscles, brain, skin, red cells, gut, produce
excess lactate due to the interchangeability of pyruvate and lactate,
i.e., lactic acid production even in the presence of oxygen. Prolonged consumption of the Western diet could lead to a certain degree of lactacidosis, not measurable in renal NAE, which could
inhibit MEP. Lactic acid being a volatile organic acid can be exhaled
via respiratory compensation. However, if there is hyperventilation, e.g., in stress situations, then the body would continue to be
exposed to organic lactic acid with no recovery.
Hyperventilation leads to respiratory alkalosis. The stickiness of
haemoglobin for oxygen increases, resulting in less oxygen being
released into cells. To counteract the alkalosis, cells begin to produce lactic acid, which lead to tiring and aching muscles. In our
example, there was already a high lactic acid production, from glycolysis which never entered the TCA cycle. This could be compen-
Table 3
A synopsis of relationship of hydrogen ion with weight gain in normal, disease free people.
Author
Year
Journal
Treatment
Conclusion
Prospective
Yancy et al.
2007
Eur J Clin Nutr
Low-carbohydrate ketogenic diet
Low-fat diet
Healthy people on ketogenic/low fat diet do not show
significant metabolic derangements
Clinical
Roef et al.
2003
Four hours cycle exercise, then either sodium lactate or sodium
bicarbonate infusion
Gluconeogeneis can be used to sustain blood glucose
after overnight fast if lactate available
Miyamura et al.
1998
Am J Physiol
Endocrinol
Metab
Jpn J Phyiol
Exercise till exhaustion
Within normal weight, weight increase is associated
with low levels of dopamine
Lin et al.
1997
Am J Physiol
Four received sodium chloride infusion (acid)
Acid ingestion in fasting leads largely to potassium
conservation
Base ingestion in fasting leads to potassium excretion
Brengger et al.
1997
Am J Physiol
Ammonium chloride intervention
Vittone et al.
1997
Metabolism
Growth hormone releasing hormone (GHRH) as nightly doses
Rankin et al.
1996
Kundu et al.
1991
Med Sci Sport
Exerc
Clin Chem
Hypoenergetic diets followed by either high or moderate
carbohydrate diets
Subjects on restricted calorie weight loss programs
Mitchell et al.
1990
Am J Med Sci
Exercise to exhaustion performed under intervention of no infusion
(control), sodium bicarbonate and sodium chloride
Greenhaff et al.
1988
Dominguez et al.
1976
Eur J Appl
Physiol Occup
Phyisol
J Clin
Endocinol
Metab
Two exercise episodes after two 4-day isoenergetic diet intervention
of low carbohydrate, high fat and protein or high carbohydrate, low
fat and protein diets
Dietary phosphate restriction
Sutton et al.
1976
Clin Sci Mol
Med
Ergometer exercise at 33%, 66% and 90% of VO2 max with ammonium
chloride, sodium bicarbonate, and calcium carbonate intervention
Possibly lactacidosis is compensated via respiratory
route in health
Metabolic acidosis is less associated with anaerobic
lactic acid production
Beneficial effects of exercise and alkali intake possibly
via increases in GH
Stinbaugh et al.
1975
Metabolism
Systemic alkalization with either sodium lactate or sodium
bicarbonate
Alkalization of system in fasting induced ketosis
results in no change in net acid excretion, even so the
total number of free protons excreted increases
Observational
Remer et al.
2007
Eur J Clin Nutr
As body fat is higher urinary pH is lower
As body muscle mass is higher urinary pH is also
higher
Rouslin
1983
J Biol Chem
The proton load can inhibit mitochondrial energy
production
Five received sodium bicarbonate infusion (alkali)
Metabolic acidosis might decrease thyroid hormones
and their functions
Optimizing GHRH might attenuate some effects of
aging on skeletal muscles
High carbohydrate group recovered performance and
moderate did not after exercise in health
Fat loss better determined by blood or breath ketone
bodies production and not urinary ketonic (organic)
acids excretion
In health, alkalization possibly improves exercise
endurance with less glucose exhaustion and greater
anaerobic respiration
Blood pH is tightly regulated
Dietary phosphate deficiency (associated with dietary
protein intake) can lead to hypercalciuria and
negative calcium balance in women but not men
S. Berkemeyer / Medical Hypotheses 73 (2009) 347356
sated via respiratory route. If, however, there is hyperventilation, it
would result in lactic acid to be expired out temporarily, only to be
produced again in the cells, in response to the hyperventilation.
Thus, lactacidosis would continue, within the range of what is
broadly classified healthy (no clinical symptoms), still not measurable as the renal NAE, latter which, would have a relatively constant organic acid excretion. If there is no or reduced respiratory
compensation, the next Western meal intake will only acerbate
the problem, possibly setting in a lactic acid trap, given no change
in dietary habits (Fig. 2). Apart from inefficient MEP and beta-oxidation, the inhibition of the TCA cycle due to acidosis, e.g., lactacidosis, would make electrons available for the production of ROS
instead [67]; certain amount of lactate could also be converted into
fat. Hence, a possibility of developing degenerative diseases in the
longer run, perhaps even a contribution to aging process cannot be
ruled out, as put forward in the straight line hypothesis of diet, acidosis, and aging (Fig. 1).
A culmination of acidosis and weight gain, given the caveats of
protein and organic acids, from published literature
Tables 24 list studies examining the relationship of the blood H+
concentration in obese (Table 2), in normal weight, disease free (Table 3), and in some patient-groups (Table 4), respectively. The success of WL in obese has been related to those who tend to respond
to dietary intervention and those who do not; the diet responsive
group reported to be successful in WL principally via the mechanism of proton leak [80]. Animal studies indicate that proton leak
accounts for 2025% of the resting metabolic rate (RMR) [81,82].
Muscle energy expenditure accounts for 20% of standard metabolic
rate, and proton leak is observed in muscle tissue and explains 20
25% of muscle tissues RMR; hence indirectly proton leak accounts
about 5% of the standard metabolic rate between diet responsive
and non-responsive group [80]. Harper and colleagues have further
proposed that only thyroid hormones seem to regulate the proton
leak [83,84]. Metabolic acidosis itself has been reported to decrease
353
thyroid hormones and hence their functions (nitrogen balance, protein synthesis, lean body mass, insulin-like growth factor I, cardiac
contraction, and renal acidification) [13]. Thus, a higher H+ could inhibit thyroid hormone function [13]. Thyroid hormone is also reported to regulate proton leak and indirectly heat production
[83,84] leading to lower resting metabolic rates, resulting in a obesity not responsive to dietary interventions [80].
A study on 12 animal species, including humans, reported that
H+ itself can inhibit mitochondrial energy production (MEP) [85]
(sections Weight gain on acidogenic diets and The organic acid
conundrum) explained via inhibition of TCA [78] and accumulation of lactic acid on Western diets. The latent acidosis on Western
diets could lead to lactacidosis when not efficiently or effectively
compensated via the respiratory route could imply a prolonged
exposure to acidosis (latent or metabolic). The inhibition of the
MEP due to acidosis could divert the electrons in the production
of ROS [67], possibly explaining disease development and aging
with time (age), as put forward in the straight-line hypothesis
(Fig. 1). This hypothesis is corroborated with the observation of
elevated ROS and cytokines in diabetics [86]. This lactate production cannot be confused with anaerobic lactate production which
is a normal body response to exercise [87,88], which, in health is
compensated by the respiratory route [89]. Section The organic
acid conundrum reviewed the H+ due to lactacidosis. This acidosis
could inhibit thyroid functioning and the proton leak making the
symptom of low heat production and lower MEP occur simultaneously (Fig. 3). The lower energy required for maintaining RMR
would partly adjust the lower MEP; i.e., the body would down-regulate its energy requirement as adjustment.
More importantly, overweight (WG) has been reported to lead
to hyperventilation [90]. This supports the straight-line hypothesis
(Fig. 1); that both calories and acids can be accumulated on Western diets, which could produce lactacidosis with concomitant less
endogenous ketoacid production, thus accumulate adipose tissue
with lower fatty acid oxidation (Fig. 3). Thus, there would be a tendency to become overweight with time (Figs. 1 and 3). The over-
Table 4
A synopsis of relationship of hydrogen ion with weight gain in various disease groups.
Author
Year
Epidemiological
Taylor et al.
2006
Siener et al.
2005
Maalouf
2004
et al.
Clinical
Tuma et al.
2005
Journal
Disease/treatment
Conclusion
Am J Kidney dis
J Urol
Kidney Int
Renal stones
Renal stones
Renal stones
Urinary pH inversely related to weight gain
Urinary pH inversely related to weight gain
Urinary pH inversely related to weight gain
Diabetes mellitus II
Obesity and diabetes mellitus II are associated with loss of skeletal muscle
Treatment for acute respiratory failure for 6
8 months
Diabetic ketoacidosis (DKA), with and
without obesity with controls
Possibly the development of respiratory acidosis in patients with acute
respiratory failure
DKA associated with elevated proinflammatory cytokines, reactive oxygen
species and cardiovascular factors in absence of obvious infection or
cardiovascular pathology
Neutralized protein intake, i.e., correction of acidosis, is beneficial for protein
turnover
BaHammam
et al.
Stentz et al.
2005
J Chromatogr B:
Anal Technol
Biomed Life Sci
Respir Med
2004
Diabetes
Graham
et al.
1997
Kidney Int
Kopple et al.
1995
Kidney Int
Reaich et al.
1995
Am J Physiol
CRF/Leucine infusion, before and after
correction of acidosis with bicarbonate
Reaich et al.
1993
Am J Physiol
CRF/First: Leucine intervention
Second: Sodium bicarbonate intervention
Third: Sodium chloride intervention
The more acid neutralized protein supplement resulted in less endogenous
protein loss, lower exogenous protein required for tissue building/
maintenance with least amount of protein used for energy production, hence
lower catabolic rates
Nery et al.
1983
Chest
Chronic obstructive pulmonary disease
(COPD) and mitral valve disease/exercise
intervention
Compromised oxygen delivery to muscles in mitral valve disease
COPD group unable to increase ventilatory gas exchange sufficiently to match
the exercise induced carbon-dioxide production
Chronic renal failure (CRF)/Leucine infusion,
before and after correction of acidosis with
bicarbonate
CRF/Dialysate substituted with amino acids
Amino acid intervention might improve protein malnutrition in chronic renal
disease patients ingesting low protein intakes
Acidosis contributes to the insulin resistance in chronic renal failure but does
not affect the action of insulin on protein degradation
354
S. Berkemeyer / Medical Hypotheses 73 (2009) 347356
Metabolic / latent acidosis
Less thyroid hormone
(IGF-I, GH)
Less
IGF-I
High calorie
intake from
Western diet
Less proton
leak
Reduced
thermogenesis
Lower
anabolic
processes
If obese, not
responsive to
diet therapy
Decreased
heart
contraction,
decreased
renal
acidifying
property
Lower
nitrogen
balance and
protein
synthesis
Cardiovascular
disease
Muscle protein
breakdown, if
no/less protein
intake
Inhibition of
mitochondrial
energy
production
Lactacidosis
hyperventilation
Electrons
converted
to ROS
Lower endogenous
ketoacid production
net fat deposition
OBESITY
Lactic acid
trap /
Acidosis
worsens
Aging
Fig. 3. Possible pathology of diet-dependent latent or metabolic acidosis.
weight in itself could also support the hyperventilation [90], which
with no change in dietary habits would lead to a repetitive cycle of
mild lactacidosis, perhaps a lactic acid trap (Fig. 2), initially not visible as diseases, but with (age) (Figs. 1 and 3). This is supported by,
that overweight (WG) is associated with diabetes mellitus II, insulin resistance and/or higher blood pressures, and chronic renal failure [9092], skeletal muscle loss [92] lower growth hormone
functions [90], low dopamine [93], and increase in proton excretion [20,53,54,60].
It becomes important to state that this overweight (WG) would
be principally due to an increase in adipose tissue. The above processes elucidate that there would be less fatty acid breakdown and
a tendency of greater fat synthesis, indirectly due to acidosis, directly due to the calories (sections The protein conundrum and
The organic acid conundrum). Thus, WG requires differentiating
the WG into fat mass gain or muscle mass gain. Loss of non-dietary
nitrogen has been associated to increases in the H+ load [94,95]. A
protein deficient diet would intensify the loss of muscle protein on
acidogenic diets (section The protein conundrum). This suggest
that what is required is not a protein-deficient diet but a balanced
diet providing both high quality proteins with high intake of alkalies (vegetables and fruits, base supplements) so that the acid anions of the protein intake get neutralized [19]. There are studies
that mention the benefit of acid load neutralized diets [96,97]
which was associated with lower skeletal mass catabolism and improved protein turnover. Thus, Western diets could lead to the
development of selectively deficient nutrition; e.g., deficient vegetables and fruits intakes, with or without protein intake deficiency,
but also in micronutrients, vitamins, and minerals, even so there is
concomitant energy overnutrition, leading to loss of muscle mass
but adding to the adipose tissue (relative obesity). This with no
change in dietary habits, in the long run (age), can promote overweight to obesity, with or without diseases.
Conclusion
This review suggests:
' Undernutrition is characterized by general emaciation, whereas
overnutrition, such as on Western diets, is characterized with
relative obesity, leading to long-term increase in fat mass but
less of muscle mass.
' Both under and overnutrition are conditions of catabolic stress
for the body and related to the risk of developing H+ retention.
' The loss of muscle mass is acerbated on a protein deficient diet,
even so protein adds to the acid load of the body.
' The correction of acidosis warrants urgent increased consumption of vegetables and fruits and/or alkali supplements. A regular
consumption of these would prevent the acidosis from setting
in, in the first place and should be vigorously targeted as a
health objective.
' Concomitant to food practices, breathing dynamics are just as
important, i.e., not only diet but also breathing is important in
ABB. Ignoring any of the two, diet or breathing, could lead to disease complications and/or aging through concomitant net
increases in adipose tissue and ROS.
The review puts forward that what we eat and how we
breathe are two important cornerstones in ABB maintenance,
which might affect general health, disease etiology, and aging as
put forward in the straight-line hypothesis. Support for the
straight-line hypothesis can be partially drawn from published literature though urgently warranting targeted studies in this
direction.
References
[1] Hyde R. Europe battles with obesity. Lancet 2008;371:21601.
[2] Nicklas TA, Hayes D. Position of the American Dietetic Association: nutrition
guidance for healthy children ages 2 to 11 years. J Am Diet Assoc
2008;108:103844. 10467.
[3] Plotnikoff RC, Lightfoot P, Spinola C, Predy G, Barrett L. A framework for
addressing the global obesity epidemic locally: the Child Health Ecological
Surveillance System (CHESS). Prev Chronic Dis 2008;5:A95.
[4] Buckland G, Salas-Savado J, Roure E, Bull M, Serra-Majem L.
Sociodemographic risk factors associated with metabolic syndrome in a
Mediterranean population. Public Health Nutr 2008 [Epub ahead of print].
[5] Rosso D, Campagna S, Di Stefano F, Romano G, Maugeri D, Maggi S, et al.
Prevalence of diabetes mellitus in a sample of the elderly population of the city
of Catania. Arch Gerontol Geriatr 1998;27:22335.
[6] Winter Y, Rohrmann S, Linseisen J, Lanczik O, Ringleb PA, Hebebrand J, et al.
Contribution of obesity and abdominal fat mass to risk of stroke and transient
ischemic attacks. Stroke 2008 [Epub ahead of print].
[7] Cordain L, Eaton SB, Sebastian A, Mann N, Lindeberg S, Watkins BA, et al.
Origins and evolution of the Western diet: health implications for the 21st
century. Am J Clin Nutr 2005;81:34154.
[8] Frassetto LA, Morris Jr RC, Sebastian A. Dietary sodium chloride intake
independently predicts the degree of hyperchloremic metabolic acidosis in
healthy humans consuming a net acid-producing diet. Am J Physiol Renal
Physiol 2007;293:F5215.
S. Berkemeyer / Medical Hypotheses 73 (2009) 347356
[9] Kurtz I, Nguyen MK. Evolving concepts in the quantitative analysis of the
determinants of the plasma water sodium concentration and the
pathophysiology and treatment of the dysnatremias. Kidney Int
2005;68:198293.
[10] Nguyen MK, Kurtz I. New insights into the pathophysiology of the
dysnatremias: a quantitative analysis. Am J Physiol Renal Physiol
2004;287:F17280.
[11] Brandao-Burch A, Utting JC, Orriss IR, Arnett TR. Acidosis inhibits bone
formation by osteoblasts in vitro by preventing mineralization. Calcif Tissue
Int 2005;77:16774.
[12] Tucker KL, Chen H, Hannan MT, Cupples LA, Wilson PW, Felson D, et al. Bone
mineral density and dietary patterns in older adults: the Framingham
Osteoporosis Study. Am J Clin Nutr 2002;76:24552.
[13] Brungger M, Hulter HN, Krapf R. Effect of chronic metabolic acidosis on thyroid
hormone homeostasis in humans. Am J Physiol 1997;272:F64853.
[14] Sebastian A, Frassetto LA, Sellmeyer DE, Merriam RL, Morris Jr RC. Estimation
of the net acid load of the diet of ancestral preagricultural Homo sapiens and
their hominid ancestors. Am J Clin Nutr 2002;76:130816.
[15] Arnett TR. Extracellular pH regulates bone cell function. J Nutr
2008;138:415S8S.
[16] Sellmeyer DE, Stone KL, Sebastian A, Cummings SR. A high ratio of dietary
animal to vegetable protein increases the rate of bone loss and the risk of
fracture in postmenopausal women. Study of Osteoporotic Fractures Research
Group. Am J Clin Nutr 2001;73:11822.
[17] Manz F, Diekmann L, Kalhoff H, Stock GJ, Kunz C. Low renal net acid excretion.
High calciuria and biochemical signs of sodium deficiency in low-birth-weight
infants fed a new low-phosphorus formula. Acta Paediatr 1992;81:96973.
[18] Maalouf NM, Cameron MA, Moe OW, Adams-Huet B, Sakhaee K. Low urine pH:
a novel feature of the metabolic syndrome. Clin J Am Soc Nephrol
2007;2:8838.
[19] Maurer M, Riesen W, Muser J, Hulter HN, Krapf R. Neutralization of Western
diet inhibits bone resorption independently of K intake and reduces cortisol
secretion in humans. Am J Physiol Renal Physiol 2003;284:F3240.
[20] Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of
kidney stones. JAMA 2005;293:45562.
[21] Jehle S, Zanetti A, Muser J, Hulter HN, Krapf R. Partial neutralization of the
acidogenic Western diet with potassium citrate increases bone mass in
postmenopausal women with osteopenia. J Am Soc Nephrol 2006;17:321322.
[22] Berkemeyer S. Dietary and renal acid loads across various age-groups. PhD
thesis, Landwirtschaftliche Fakultt vol. PhD, Rheinische Friedrich-WilhelmsUniversitt, Bonn; 2008. p. 139.
[23] Arnett T. Regulation of bone cell function by acidbase balance. Proc Nutr Soc
2003;62:51120.
[24] Krieger NS, Frick KK, LaPlante Strutz K, Michalenka A, Bushinsky DA.
Regulation of COX-2 mediates acid-induced bone calcium efflux in vitro. J
Bone Miner Res 2007;22:90717.
[25] Kraut JA, Kurtz I. Use of base in the treatment of acute severe organic acidosis
by nephrologists and critical care physicians: results of an online survey. Clin
Exp Nephrol 2006;10:1117.
[26] Frassetto LA, Todd KM, Morris Jr RC, Sebastian A. Worldwide incidence of hip
fracture in elderly women: relation to consumption of animal and vegetable
foods. J Gerontol A: Biol Sci Med Sci 2000;55:M58592.
[27] Greenhaff PL, Gleeson M, Maughan RJ. The effects of diet on muscle pH and
metabolism during high intensity exercise. Eur J Appl Physiol Occup Physiol
1988;57:5319.
[28] Vormann J, Goedeke T. Latent acidosis: acidity as a cause for chronic diseases
[Latente Azidose: bersuerung als Ursache chronischer Erkrankungen].
Schewiz Zschr Ganszheits Medizin 2002;2:906.
[29] Paisley RB, Angers M, Frenk S. Plasma cortisol levels in malnourished children
with and without superimposed acute stress. Arch Dis Child 1973;48:7146.
[30] Bohe J, Rennie MJ. Muscle protein metabolism during hemodialysis. J Ren Nutr
2006;16:316.
[31] De Luca F. Impaired growth plate chondrogenesis in children with chronic
illnesses. Pediatr Res 2006;59:6259.
[32] Kalantar-Zadeh K, Mehrotra R, Fouque D, Kopple JD. Metabolic acidosis and
malnutritioninflammation complex syndrome in chronic renal failure. Semin
Dial 2004;17:45565.
[33] Mehrotra R, Kopple JD. Protein and energy nutrition among adult patients
treated with chronic peritoneal dialysis. Adv Ren Replace Ther
2003;10:194212.
[34] Guarnieri G, Antonione R, Biolo G. Mechanisms of malnutrition in uremia. J
Ren Nutr 2003;13:1537.
[35] Cahill Jr GF. Starvation in man. Clin Endocrinol Metab 1976;5:397415.
[36] Thio LL, Erbayat-Altay E, Rensing N, Yamada KA. Leptin contributes to slower
weight gain in juvenile rodents on a ketogenic diet. Pediatr Res
2006;60:4137.
[37] Kalhoff H, Manz F, Diekmann L, Kunz C. Decreased growth rate of low-birthweight infants with prolonged maximum renal acid stimulation. Acta Paediatr
1993;82:5227.
[38] Kalhoff H, Manz F, Kiwull P, Kiwull-Schone H. Food mineral composition and
acidbase balance in preterm infants. Eur J Nutr 2007;46:18895.
[39] Bines J, Francis D, Hill D. Reducing parenteral requirement in children with
short bowel syndrome: impact of an amino acid-based complete infant
formula. J Pediatr Gastroenterol Nutr 1998;26:1238.
[40] Fok TF, So LY, Lee NN, Leung RK, Wong W, Cheung KL, et al. Late metabolic
acidosis and poor weight gain in moderately pre-term babies fed with a
[41]
[42]
[43]
[44]
[45]
[46]
[47]
[48]
[49]
[50]
[51]
[52]
[53]
[54]
[55]
[56]
[57]
[58]
[59]
[60]
[61]
[62]
[63]
[64]
[65]
[66]
[67]
[68]
[69]
[70]
355
casein-predominant formula: a continuing need for caution. Ann Trop Paediatr
1989;9:2437.
Jadhav P, Parimi PS, Kalhan SC. Parenteral amino acid and metabolic acidosis in
premature infants. J Parenter Enteral Nutr 2007;31:27883.
Moro GE, Minoli I, Fulconis F, Clementi M, Raiha NC. Growth and metabolic
responses in low-birth-weight infants fed human milk fortified with human
milk protein or with a bovine milk protein preparation. J Pediatr Gastroenterol
Nutr 1991;13:1504.
Boehm G, Gedlu E, Muller DM, Beyreiss K, Raiha NC. Relationship between urea
and ammonium excretion in the urine of very-low-birth-weight infants
appropriate for gestational age. Biomed Biochim Acta 1990;49:6974.
Porcelli Jr PJ, Sisk PM. Increased parenteral amino acid administration to
extremely low-birth-weight infants during early postnatal life. J Pediatr
Gastroenterol Nutr 2002;34:1749.
Kleinman JG, Lemann JJ. Acid production. In: Kleeman CR, Maxwell MH, Narins
RG, editors. Clinical disorders of fluid and electrolyte metabolism, vols. 159
173. New York: McGraw Hill; 1987.
Resnick LM, Gupta RK, Bhargava KK, Gruenspan H, Alderman MH, Laragh JH.
Cellular ions in hypertension, diabetes, and obesity. A nuclear magnetic
resonance spectroscopic study. Hypertension 1991;17:9517.
Kaloyianni M, Bourikas D, Koliakos G. The effect of insulin on Na+H+ antiport
activity of obese and normal subjects erythrocytes. Cell Physiol Biochem
2001;11:2538.
Konstantinou-Tegou A, Kaloyianni M, Bourikas D, Koliakos G. The effect of
leptin on Na(+)H(+) antiport (NHE 1) activity of obese and normal subjects
erythrocytes. Mol Cell Endocrinol 2001;183:118.
Koren W, Koldanov R, Pronin VS, Postnov IY, Peleg E, Rosenthal T, et al.
Amiloride-sensitive Na+/H+ exchange in erythrocytes of patients with NIDDM:
a prospective study. Diabetologia 1997;40:3026.
Aviv A. The roles of cell Ca2+, protein kinase C and the Na(+)H(+) antiport in
the development of hypertension and insulin resistance. J Am Soc Nephrol
1992;3:104963.
Resnick LM. Cellular calcium and magnesium metabolism in the
pathophysiology and treatment of hypertension and related metabolic
disorders. Am J Med 1992;93:11S20S.
Taylor EN, Curhan GC. Body size and 24-hour urine composition. Am J Kidney
Dis 2006;48:90515.
Maalouf NM, Sakhaee K, Parks JH, Coe FL, Adams-Huet B, Pak CY. Association of
urinary pH with body weight in nephrolithiasis. Kidney Int 2004;65:14225.
Siener R, Glatz S, Nicolay C, Hesse A. The role of overweight and obesity in
calcium oxalate stone formation. Obes Res 2004;12:10613.
Jourdan M, Glock C, Margen S, Bradfield RB. Sulphate, acidbase, and mineral
balances of obese women during weight loss. Am J Clin Nutr 1980;33:23643.
Gougeon-Reyburn R, Leiter LA, Yale JF, Marliss EB. Comparison of daily diets
containing 400 kcal (1.67 MJ) of either protein or glucose, and their effects on
the response to subsequent total fasting in obese subjects. Am J Clin Nutr
1989;50:74658.
Gougeon-Reyburn R, Lariviere F, Marliss EB. Effects of bicarbonate
supplementation on urinary mineral excretion during very low energy diets.
Am J Med Sci 1991;302:6774.
Frassetto LA, Morris Jr RC, Sebastian A. Effect of age on blood acidbase
composition in adult humans: role of age-related renal functional decline. Am
J Physiol 1996;271:F111422.
Rylander R, Remer T, Berkemeyer S, Vormann J. Acidbase status affects renal
magnesium losses in healthy, elderly persons. J Nutr 2006;136:23747.
Remer T, Berkemeyer S, Rylander R, Vormann J. Muscularity and adiposity in
addition to net acid excretion as predictors of 24-h urinary pH in young adults
and elderly. Eur J Clin Nutr 2007;61:6059.
Berkemeyer S, Vormann J, Gunther A, Rylander R, Frassetto L, Remer T. Renal
net acid excretion capacity is comparable in prepubescence, adolescence and
young adulthood but is reduced with aging. J Am Geriatr Soc 2008;56:14428.
Canals S, Casarejos MJ, De Bernardo S, Rodriguez-Martin E, Mena MA.
Glutathione depletion switches nitric oxide neurotrophic effects to cell
death in midbrain cultures: implications for Parkinsons disease. J
Neurochem 2001;79:118395.
Pocernich CB, La Fontaine M, Butterfield DA. In vivo glutathione elevation
protects against hydroxyl free radical-induced protein oxidation in rat brain.
Neurochem Int 2000;36:18591.
Schulz JB, Lindenau J, Seyfried J, Dichgans J. Glutathione, oxidative stress and
neurodegeneration. Eur J Biochem 2000;267:490411.
Hunter EA, Grimble RF. Cysteine and methionine supplementation modulate
the effect of tumor necrosis factor alpha on protein synthesis, glutathione and
zinc concentration of liver and lung in rats fed a low protein diet. J Nutr
1994;124:231928.
Lanza IR, Befroy DE, Kent-Braun JA. Age-related changes in ATP-producing
pathways in human skeletal muscle in vivo. J Appl Physiol 2005;99:
173644.
Wallace DC. A mitochondrial paradigm for degenerative diseases and ageing.
Novartis Found Symp 2001;235:24763. discussion 2636.
Campbell WW, Leidy HJ. Dietary protein and resistance training effects on
muscle and body composition in older persons. J Am Coll Nutr
2007;26:696S703S.
Timmerman KL, Volpi E. Amino acid metabolism and regulatory effects in
aging. Curr Opin Clin Nutr Metab Care 2008;11:459.
Martin TJ. Protein nutrition as therapy for a genetic disorder of bone? Cell
Metab 2006;4:41920.
356
S. Berkemeyer / Medical Hypotheses 73 (2009) 347356
[71] Bonjour JP. Dietary protein: an essential nutrient for bone health. J Am Coll
Nutr 2005;24:526S36S.
[72] Alexy U, Remer T, Manz F, Neu CM, Schoenau E. Long-term protein intake and
dietary potential renal acid load are associated with bone modeling and
remodeling at the proximal radius in healthy children. Am J Clin Nutr
2005;82:110714.
[73] Heaney RP, Layman DK. Amount and type of protein influences bone health.
Am J Clin Nutr 2008;87:1567S70S.
[74] Frassetto LA, Morris Jr RC, Sellmeyer DE, Sebastian A. Adverse effects of sodium
chloride on bone in the aging human population resulting from habitual
consumption of typical American diets. J Nutr 2008;138:419S22S.
[75] Berkemeyer S, Remer T. Anthropometrics provide a better estimate of urinary
organic acid anion excretion than a dietary mineral intake-based estimate in
children, adolescents, and young adults. J Nutr 2006;136:12038.
[76] Chalmers RA, Healy MJ, Lawson AM, Hart JT, Watts RW. Urinary organic acids
in man. III. Quantitative ranges and patterns of excretion in a normal
population. Clin Chem 1976;22:12928.
[77] Hood VL, Tannen RL. Protection of acidbase balance by pH regulation of acid
production. N Engl J Med 1998;339:81926.
[78] Bento LM, Fagian MM, Vercesi AE, Gontijo JA. Effects of NH4Cl-induced
systemic metabolic acidosis on kidney mitochondrial coupling and calcium
transport in rats. Nephrol Dial Transplant 2007;22:281723.
[79] Morath MA, Okun JG, Muller IB, Sauer SW, Horster F, Hoffmann GF, et al.
Neurodegeneration and chronic renal failure in methylmalonic aciduriaa
pathophysiological approach. J Inherit Metab Dis 2007.
[80] Harper ME, Dent R, Monemdjou S, Bezaire V, Van Wyck L, Wells G, et al.
Decreased mitochondrial proton leak and reduced expression of uncoupling
protein 3 in skeletal muscle of obese diet-resistant women. Diabetes
2002;51:245966.
[81] Rolfe DF, Newman JM, Buckingham JA, Clark MG, Brand MD. Contribution of
mitochondrial proton leak to respiration rate in working skeletal muscle and
liver and to SMR. Am J Physiol 1999;276:C6929.
[82] Porter RK, Brand MD. Body mass dependence of H+ leak in mitochondria and
its relevance to metabolic rate. Nature 1993;362:62830.
[83] Hafner RP, Nobes CD, McGown AD, Brand MD. Altered relationship between
protonmotive force and respiration in non-phosphorylating liver mitochondria
isolated from rats of different thyroid hormone status. Eur J Biochem
1988;178:5118.
[84] Harper ME, Brand MD. The quantitative contributions of mitochondrial proton
leak and ATP turnover reactions to the changed respiration rates of
[85]
[86]
[87]
[88]
[89]
[90]
[91]
[92]
[93]
[94]
[95]
[96]
[97]
hepatocytes from rats of different thyroid status. J Biol Chem
1993;268:1485060.
Rouslin W. Protonic inhibition of the mitochondrial oligomycin-sensitive
adenosine 50 -triphosphatase in ischemic and autolyzing cardiac muscle.
Possible mechanism for the mitigation of ATP hydrolysis under
nonenergizing conditions. J Biol Chem 1983;258:965761.
Stentz FB, Umpierrez GE, Cuervo R, Kitabchi AE. Proinflammatory cytokines,
markers of cardiovascular risks, oxidative stress, and lipid peroxidation in
patients with hyperglycemic crises. Diabetes 2004;53:207986.
Rankin JW, Ocel JV, Craft LL. Effect of weight loss and refeeding diet
composition on anaerobic performance in wrestlers. Med Sci Sport Exerc
1996;28:12929.
Roef MJ, De Meer K, Kalhan SC, Straver H, Berger R, Reijngoud DJ.
Gluconeogenesis in humans with induced hyperlactatemia during lowintensity exercise. Am J Physiol Endocrinol Metab 2003;284:E116271.
Sutton JR, Jones NL, Toews CJ. Growth hormone secretion in acidbase
alterations at rest and during exercise. Clin Sci Mol Med 1976;50:2417.
Bray GA, Whipp BJ, Koyal SN, Wasserman K. Some respiratory and metabolic
effects of exercise in moderately obese men. Metabolism 1977;26:40312.
Reaich D, Graham KA, Channon SM, Hetherington C, Scrimgeour CM,
Wilkinson R, et al. Insulin-mediated changes in PD and glucose uptake after
correction of acidosis in humans with CRF. Am J Physiol 1995;268:E1216.
Tuma P, Samcova E, Balinova P. Determination of 3-methylhistidine and 1methylhistidine in untreated urine samples by capillary electrophoresis. J
Chromatogr B: Anal Technol Biomed Life Sci 2005;821:539.
Miyamura M, Ishida K, Itoh H, Ohkuwa T. Relationship between maximal
pulmonary ventilation and arterialized venous blood potassium and dopamine
concentrations obtained at exhaustion in man. Jpn J Physiol 1998;48:1723.
Kopple JD, Bernard D, Messana J, Swartz R, Bergstrom J, Lindholm B, et al.
Treatment of malnourished CAPD patients with an amino acid based dialysate.
Kidney Int 1995;47:114857.
Sapir DG, Owen OE. Renal conservation of ketone bodies during starvation.
Metabolism 1975;24:2333.
Graham KA, Reaich D, Channon SM, Downie S, Gilmour E, Passlick-Deetjen J,
et al. Correction of acidosis in CAPD decreases whole body protein
degradation. Kidney Int 1996;49:1396400.
Reaich D, Channon SM, Scrimgeour CM, Daley SE, Wilkinson R, Goodship TH.
Correction of acidosis in humans with CRF decreases protein degradation and
amino acid oxidation. Am J Physiol 1993;265:E2305.
You might also like
- Mukabang Hamzy Korea 2Document1 pageMukabang Hamzy Korea 2Dianne Faye ManabatNo ratings yet
- Lemon Vine - Google SearchDocument1 pageLemon Vine - Google SearchDianne Faye ManabatNo ratings yet
- Goodcatch Humanity II 902MS Medium + Medium Light Spinning Casting Rod Fishing Buddy GoodcatchDocument1 pageGoodcatch Humanity II 902MS Medium + Medium Light Spinning Casting Rod Fishing Buddy GoodcatchDianne Faye ManabatNo ratings yet
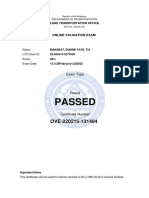
- LTO ExamDocument1 pageLTO ExamDianne Faye ManabatNo ratings yet
- Pone 0161211 s003Document70 pagesPone 0161211 s003Dianne Faye ManabatNo ratings yet
- FWD Proximate Analysis of Phil Buffalo MilkDocument2 pagesFWD Proximate Analysis of Phil Buffalo MilkDianne Faye ManabatNo ratings yet
- Josephine Landscape Design Post Offers Grotto and Waterfall ConstructionDocument1 pageJosephine Landscape Design Post Offers Grotto and Waterfall ConstructionDianne Faye ManabatNo ratings yet
- Safari - Apr 4, 2021 at 4:46 PMDocument1 pageSafari - Apr 4, 2021 at 4:46 PMDianne Faye ManabatNo ratings yet
- Facebook 3Document1 pageFacebook 3Dianne Faye ManabatNo ratings yet
- Casa Balario An Exclusive Bali-Inspired Resort in Tanay, RizalDocument1 pageCasa Balario An Exclusive Bali-Inspired Resort in Tanay, RizalDianne Faye ManabatNo ratings yet
- 6R's Eatery SectionDocument1 page6R's Eatery SectionDianne Faye ManabatNo ratings yet
- Returnlabel: To Lazada Warehouse: FromDocument1 pageReturnlabel: To Lazada Warehouse: FromDianne Faye ManabatNo ratings yet
- 20 Sep 2019Document1 page20 Sep 2019Jay JohnNo ratings yet
- Prior Notice Confirmation: Submitted For Your Records OnlyDocument1 pagePrior Notice Confirmation: Submitted For Your Records OnlyMarlon Martinez CNo ratings yet
- Pone 0161211 s003Document70 pagesPone 0161211 s003Dianne Faye ManabatNo ratings yet
- Edge 1997Document12 pagesEdge 1997Dianne Faye ManabatNo ratings yet
- Authorization Letter - PDF - Signed Using Adobe Fill & SignDocument1 pageAuthorization Letter - PDF - Signed Using Adobe Fill & SignDianne Faye ManabatNo ratings yet
- Figure S1Document1 pageFigure S1JorgeMelloFeiraNo ratings yet
- Amylase EnzymeDocument6 pagesAmylase EnzymeDianne Faye ManabatNo ratings yet
- Pone 0161211 s003Document70 pagesPone 0161211 s003Dianne Faye ManabatNo ratings yet
- Lecture 2 Feed Comp Proximate AnalysisDocument6 pagesLecture 2 Feed Comp Proximate AnalysisDianne Faye ManabatNo ratings yet
- Nqaa010 Supplement FileDocument5 pagesNqaa010 Supplement FileDianne Faye ManabatNo ratings yet
- The Human Milk Oligosaccharides Are Not Affected by Pasteurization and Freeze-DryingDocument8 pagesThe Human Milk Oligosaccharides Are Not Affected by Pasteurization and Freeze-DryingDianne Faye ManabatNo ratings yet
- Laboratory PrelabDocument6 pagesLaboratory PrelabDianne Faye ManabatNo ratings yet
- Selective Extraction of Phospholipids From Egg YolkDocument3 pagesSelective Extraction of Phospholipids From Egg YolkDianne Faye ManabatNo ratings yet
- Starvation Induced Metabolic Alterations - Biochemistry For Medics - Clinical CasesDocument6 pagesStarvation Induced Metabolic Alterations - Biochemistry For Medics - Clinical CasesDianne Faye ManabatNo ratings yet
- Chick, 1913Document19 pagesChick, 1913Dianne Faye ManabatNo ratings yet
- Mcgarry, 1972Document10 pagesMcgarry, 1972Dianne Faye ManabatNo ratings yet
- Gambar Obesitas Menyebabkan DislipidemiaDocument40 pagesGambar Obesitas Menyebabkan DislipidemiaAldy RinaldiNo ratings yet
- J. Nutr.-2005-Kalm-1347-52Document6 pagesJ. Nutr.-2005-Kalm-1347-52Dianne Faye ManabatNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Safe Work in Confined Spaces: Confined Spaces Regulations 1997 Approved Code of Practice, Regulations and GuidanceDocument44 pagesSafe Work in Confined Spaces: Confined Spaces Regulations 1997 Approved Code of Practice, Regulations and GuidanceantonpeleleNo ratings yet
- THS625 Bond Strength Fixtures: All Specifications Subject To Change Without Prior Notice Page 1 of 2Document2 pagesTHS625 Bond Strength Fixtures: All Specifications Subject To Change Without Prior Notice Page 1 of 2Ninh TranNo ratings yet
- Series 500Document4 pagesSeries 500Nilton GarcíaNo ratings yet
- Pts Painting 2017Document67 pagesPts Painting 2017Faiz IshakNo ratings yet
- Siemens Fire ProtectionDocument5 pagesSiemens Fire ProtectionMohd A IshakNo ratings yet
- Chapter 03 SlidesDocument55 pagesChapter 03 SlidesHaneshNo ratings yet
- Aluminum Sulfate GHSDocument9 pagesAluminum Sulfate GHSJean Carla RosarioNo ratings yet
- Full Lectures ChemistryDocument85 pagesFull Lectures ChemistrySaja AliNo ratings yet
- Multiple Choice Questions in PharmacologyDocument65 pagesMultiple Choice Questions in PharmacologyLokesh MahataNo ratings yet
- College of Medical Technology Center For Medical and Allied Health ScienceDocument15 pagesCollege of Medical Technology Center For Medical and Allied Health ScienceGlomelyn Rose Ortiz TañedoNo ratings yet
- Amoled DisplaysDocument5 pagesAmoled DisplaysChaithanya MannepalliNo ratings yet
- Curcumin Derivatives PreparationDocument10 pagesCurcumin Derivatives PreparationGuru DevNo ratings yet
- 509 - F 250 BODYFIBER - TdsDocument1 page509 - F 250 BODYFIBER - TdsИван ПетровNo ratings yet
- Instruments Used in Bacteriology LabDocument1 pageInstruments Used in Bacteriology LabJiro Anderson EscañaNo ratings yet
- Physics 2nd Year Full BookDocument3 pagesPhysics 2nd Year Full BookAsif Rasheed RajputNo ratings yet
- IJCS Insights on ancient medical chemistryDocument4 pagesIJCS Insights on ancient medical chemistryCuriosityShopNo ratings yet
- FLUENT 6.1 Features: General Modeling CapabilitiesDocument9 pagesFLUENT 6.1 Features: General Modeling CapabilitiestktdNo ratings yet
- En LNG Air Products MCR Coil Wound Heat Exchangers PDFDocument10 pagesEn LNG Air Products MCR Coil Wound Heat Exchangers PDFJoan Andrey Bolaños CruzNo ratings yet
- Demo PPT Scie 7Document18 pagesDemo PPT Scie 7Tricia RodriguezNo ratings yet
- Chemistry of Oil, Fats, and Wax ProcessingDocument22 pagesChemistry of Oil, Fats, and Wax ProcessingGaboniumNo ratings yet
- Syllabus For Admission TestDocument2 pagesSyllabus For Admission TestSyed Moinul HoqueNo ratings yet
- Deposition of Zinc - Zinc Phosphate Composite Coatings On Steel by Cathodic Electrochemical Treatment-1Document13 pagesDeposition of Zinc - Zinc Phosphate Composite Coatings On Steel by Cathodic Electrochemical Treatment-1mirosekNo ratings yet
- Lecture 1 NotesDocument46 pagesLecture 1 NotesIncNo ratings yet
- Emergency Response and Spill ControlDocument5 pagesEmergency Response and Spill ControlbaluchakpNo ratings yet
- Estimate Casein in Milk SamplesDocument17 pagesEstimate Casein in Milk SamplesYuvraj SinghNo ratings yet
- Troubleshooting For Increased PressureDocument5 pagesTroubleshooting For Increased PressureMubarak PatelNo ratings yet
- Illness Biomagnetism TreatmentDocument3 pagesIllness Biomagnetism TreatmentSilvia Arias100% (2)
- Emf KrohneDocument69 pagesEmf KrohneMaria Fernanda FS100% (1)
- Literature ReviewDocument4 pagesLiterature Reviewsiddeshkorgaonkar42No ratings yet
- All QA 1Document16 pagesAll QA 1dhyaneshchaudhari25No ratings yet