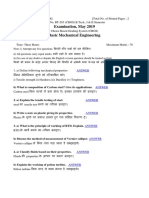
Professional Documents
Culture Documents
Closed Circuit-Low Flow PDF
Uploaded by
jsagayOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Closed Circuit-Low Flow PDF
Uploaded by
jsagayCopyright:
Available Formats
SS-1 HEALTH TELEMATICS AND TELEMEDICINE: TECHNOLOGY, METHODOLOGY AND MANAGEMENT ASPECTS
CLOSED-CIRCUIT LOW-FLOW ANESTHESIA: MODELLISTIC
APPROACH TO REAL TIME CONTROL, AND DICOM-BASED
ARCHIVING IN THE MEDARCNET TELEMEDICINE SYSTEM
S. Radin*, E. Romano**, P. Bosazzi*, P. Inchingolo*
* University of Trieste, Dipartimento di Elettrotecnica, Elettronica ed Informatica, Trieste, Italy
** Maggiore Hospital, Unit of Anesthesia and Reanimation, Az. Osp. Trieste, Trieste, Italy
radin@deei.units.it, ezio.romano@aots.sanita.fvg.it, bosazzi, inchingolo@deei.units.it
shunt. Moreover, this model does not include the
breathing system part of the circuit, but only the patient,
and it works only for a 70-kg, 40-year-old standard
anesthetized man.
Lerou and colleagues, in 1991 [3], included the
breathing system in the model, and permitted to
calculate all the physiologic data using only three
simple external measures of the patient: age, weight and
height. This model is therefore usable not only for the
standard man, but has a too simple representation of
the lungs (two compartments) and of the breathing
system (one compartment).
Mapleson, in 1998 [4], introduced a multicompartmental breathing system, a three-compartmental
lung, and suggested a sequence of fresh-gas flows and
anesthetic concentrations which permits to reach in a
short time whatever predefined concentration of
anesthetic in the end-tidal expired gas. However, also
this model works only with the standard man.
All these models were rewritten in our labs using
Matlab and Simulink, in order to have a homogenous
representation and to allow a comparison. From this
study we concluded that a new model is needed to
accurately simulate the closed-circuit low-flow
anesthesia for any patient.
The integration of clinical data is very important for
all hospitals. Since the Hospital Informative System
appeared, the need of integrating and organizing all data
acquired from various devices in a complete and
integrated clinical record was felt. However some
technological limitations of the devices and the
complexity and amount of data to be managed slowed
the development of a centralized system, leading to
many little departmental systems. Moreover, in the past
there was not an adequate standard to allow to integrate
all data coming from all different biomedical devices.
In the last years however, some standards were
introduced, advanced enough to face the problem of
data management and integration. An example is the
DICOM (Digital Imaging and Communications in
Medicine) standard [5], which can manage all clinical
data, from images to patients personal data, from
biomedical signals represented by curves to single
values (like the results of a blood exam).
The DPACS (Data and Picture Archiving and
Abstract: Literature recently proposed a new
anesthesia scheme which, based on a precise
theoretical model, promises to reach in a short time
any predefined concentration of anesthetic in the
alveolar gas through the use of fixed fresh-gas flows
and anesthetic concentrations maintained for
predefined time intervals. The first part of this work
is based on a study of the evolution of the theoretical
models concerning anesthesia, to evaluate their
benefits and lacks. After this, a new model is built,
based on the data obtained through the application
of the new anesthesia scheme to a population of non
selected patients submitted to various types of
surgery. Based on this new model, a real time control
is proposed, which permits to have a fast induction
and to save the 63% of anesthetic in relation to an
open circuit anesthesia. All the acquired data have
been archived in standard format (DICOM 3.0) in
the DPACS-MedArcNet telemedicine system. An
integration with the DPACS system was achieved, in
order to expand this system from radiology to all
clinical activities. This was made through the
development of specific applications and through
some necessary modifications to the DPACS
software. For the first time curves in the DPACS
system were archived, which means to archive the
values of each curve point, and not the image of the
curve. This is very important because the physician
can manage the real data, not a representation of
them.
Introduction
The closed-circuit low-flow anesthesia is an
anesthetic technique which recycles the anesthetic that
is not absorbed by the patient: the expired anesthetic is
reinserted in the breathing system by mixing it with that
coming out from the vaporizer.
Mapleson, in 1973 [1-2], introduced the circulation
time in the conventional compartmental models,
showing that the absence of that time causes some
systematic errors. This model was however very simple,
and had only one compartment to represent the lungs,
while for a good representation we need at least three
compartments: alveoli, parallel dead space and central
IFMBE Proceedings
MEDICON 2001, 12-15 June 2001, Pula, Croatia
Part I
135
SS-1 HEALTH TELEMATICS AND TELEMEDICINE: TECHNOLOGY, METHODOLOGY AND MANAGEMENT ASPECTS
Communication System) project [6-7], which started
with the goal of substituting the old PACS of the
Cattinara Hospital in Trieste, realizes an open system
for the archiving, communicating and remote consulting
of clinical images and data.
The DPACS system, realized by the Dipartimento
di Elettrotecnica, Elettrotecnica ed Informatica (DEEI)
together with the Radiology Institute of the University
of Trieste and the Azienda Ospedaliera O.R. of Trieste
(AOTS), is currently used to archive and consult all the
exams of the hospital, while the system is growing to
integrate the other two hospitals of Trieste, the
Maggiore Hospital and the Burlo Children Hospital.
This work deals with the DPACS integration of the
Anesthesia and Reanimation Unit of the Maggiore
Hospital of the AOTS, that started with the archiving of
anesthesia data acquired during an operation. The
acquired data are 11 curves, which are: end-tidal and
first-input anesthetic concentration, inspired and expired
oxygen, carbon dioxide and gas flow, oxygen saturation,
pulse, and respiratory frequency. These curves have a
point every 10 seconds for each of them.
This work was primarily made in the Health
Telematics Laboratory of the DEEI, with the
collaboration of physicians from the Anesthesia and
Reanimation Unit of the Maggiore Hospital.
anesthesia curve, the Study Information Entity
represents the operation, and the Series Information
Entity represents the anesthesia.
The application used to query the DPACS archive,
called DPACS Workstation, which already could
visualize images and patients personal data, was
modified to allow the visualization of the curves.
Results
The Mapleson model of 1998 is thought to simulate
the anesthetized standard man: 40 years old, 70 kg of
weight, 1 m and 80 cm tall, ventilated with a 5 l/min
flow with a respiratory frequency of 10 per minute. It is
than obvious that the sequences proposed by Mapleson
(Figure 2) will not be accurate for every patient.
Materials and Methods
All data were acquired through the Datex-Ohmeda
Capnomac Ultima, a respiration and ventilation monitor
equipped with a pulse oxymeter.
Figure 2: the sequences of Mapleson for isoflurane
However, the sequences of Mapleson were followed
exactly, with the only change of calculating the MAC
(Minimum Alveolar Concentration), using the age of the
patient, through the following formula [8]:
MAC = a*10bx
Figure 1: screen-shots of the acquiring-archiving
application
This device gives out a numeric string of all
measured data every 10 seconds through a 25-pin serial
port.
All these data were acquired on a personal computer
through a specifically developed application (Figure 1),
which creates 11 files in DICOM format using the
Curve Information Object Definition of the standard
and sends them to the DPACS archive. It seems
adequate to use the Curve Information Object
Definition, which represents graphs that can be
specified as a series of interconnected points. For an
136
Part I
Where a is the MAC at 40 years of age (it is 1.17% for
isoflurane, the anesthetic used in this study), b = -0.0027
and x = patients age less 40.
The application of the sequences of Mapleson as
they are to 20 non selected patients submitted to
various types of surgery, anesthetized with isoflurane,
brought an unavoidable error, so that the target of 1
MAC for the end-tidal expired concentration of
anesthetic was not, averagely, reached. In figure 3 all
the acquired data (one datum every 10 seconds for each
patient for the first 20 minutes of anesthesia) and the
average and standard deviation are shown. A
concentration of 0.750.10 MAC is reached rapidly (1.5
minutes) and maintained almost constant for the rest of
the acquisition time.
The relative error obtained applying the sequences
of Mapleson as they are is then -2510%. This
IFMBE Proceedings
MEDICON 2001, 12-15 June 2001, Pula, Croatia
SS-1 HEALTH TELEMATICS AND TELEMEDICINE: TECHNOLOGY, METHODOLOGY AND MANAGEMENT ASPECTS
personalization needed by the model to match each
single patient. This last modification brings the relative
error to +15%.
The goodness of this result makes possible to
simulate a real-time control of the fresh-gas flow and of
the anesthetic concentration of the vaporizer.
As suggested by Mapleson, it is opportune to first
lower the fresh-gas flow, and then, once a minimum
value is reached, to lower the anesthetic concentration
of the vaporizer.
The real-time control is a proportional-integral
feedback which calculates, for every step, the fresh-gas
flow through the following relation:
happens because none of the 20 patients had
characteristics similar to those of the standard man.
In order to obtain a better representation of the
various patients, all the physiological parameters of the
patient part of the Mapleson model were calculated
from the three external measures that Lerou and
colleagues used in their work in 1991. Moreover, the
modification of ventilation and respiratory frequency
from the standard values has been introduced directly
in the model of Mapleson.
Qfgf = 30*Ep + 0.005*Ei
Where Ep is the proportional error and Ei is the integral
error. The values obtained from this relation are
saturated by a maximum value equal to the 95% of the
alveolar ventilation and by a minimum value equal to 1
l/min, which is a safety value to assure the oxygen
consumption to the patient. Once this minimum value is
reached, the real-time control starts to lower the
anesthetic concentration of the vaporizer through the
following relation:
Pvap = 3 MAC + 0.5*Ep + 0.00005*Ei
Figure 3: all acquired data for end-tidal anesthetic
concentration, average and standard deviation
The value obtained from this relation is saturated by a
maximum value equal to 3 MAC. Figure 5 shows the
simulation of the real-time control to reach the MAC95
(which is the MAC multiplied for 1.3) for the same
patient of figure 4.
These modifications on the model of Mapleson
allow to reduce the relative error to -139%. In figure 4
the curves of first-input anesthetic concentration
(FiAA), end-tidal anesthetic concentration (EtAA),
EtAA/FiAA and the relative error of the EtAA, are
shown for one of the patients. The dashed lines are
related to the results of the computer simulation of the
modified model of Mapleson.
Figure 5: simulation of the real-time control
Figure 4: measured and simulated
concentration curves and relative error
The use of the real-time control can better the use of
the anesthetic. The computer simulation shows that, for
a two-hours operation, the use of a closed-circuit lowflow anesthesia, aided by the real-time feedback control,
the anesthetic consumption is 63% lower than using an
open-circuit anesthesia (Figure 6).
The real-time control has the great advantage, in
relation to the sequences of Mapleson, to be
independent from the subjective variations of the
physiological parameters of the patients.
anesthetic
A further modification was made to the model of
Mapleson: the cardiac output was not considered
constant, and it was calculated for each calculation step
in relation to the value of EtAA/FiAA. This
modification is made to consider every other
IFMBE Proceedings
MEDICON 2001, 12-15 June 2001, Pula, Croatia
Part I
137
SS-1 HEALTH TELEMATICS AND TELEMEDICINE: TECHNOLOGY, METHODOLOGY AND MANAGEMENT ASPECTS
The integration with the DPACS-MedArcNet system
was achieved through an application specifically
developed, which permits 1) to insert patients personal
data (those useful for anesthesia), 2) to automatically
acquire the data coming from the Datex-Ohmeda
Capnomac Ultima via serial port, 3) to visualize the
real-time curves of end-tidal and first-input anesthetic
concentration in order to see the time variations of these
parameters and to test if the target value is reached and
maintained and 4) at the end of the operation to create
11 files in DICOM format using the Curve Information
Object Definition of the standard. The same application
is used to send the data to the DPACS archive, so as to
integrate the clinical record of the patient.
The lacks of previous models were overtook by two
modifications to the model of Mapleson of 1998. The
first modification is to use the relations of Lerou and
colleagues of 1991 to calculate some physiological
parameters, and the second is to use the EtAA/FiAA to
calculate, for every step, the cardiac output, which is not
constant during operations.
Based on this model, a real-time control is proposed,
in order to lower anesthetic consumption by a better use
of it in a closed-circuit low-flow anesthesia. Anyhow,
this real-time control must be experimented.
Archiving all data of an operation in the DPACSMedArcNet telemedicine system is very useful to have a
vision of the going of the operation on every instant of
it. It is also useful to have all data from a patient
(radiographies, nuclear medicine images, anesthesia
curves, etc.) available all together, to facilitate the
physician to elaborate a precise diagnosis. A possible
development for this program is to acquire data from all
the instruments used during an operation, and also from
those used in reanimation.
The reanimation data are very useful to archive
because a lot of statistics are made on them. All these
statistics are now handmade, and the physician looses
much time; computer aided statistics are desirable.
Acknowledgments
Figure 6: liquid isoflurane consumption
Discussion
The last modified model seem to be a good
representation of every patient, independently from the
subjectivity of the physiological data, and also includes
the breathing system, through a multi-compartmental
model.
The good results were reached through the
modification of the cardiac output relation, using it as a
sum of all subjective differences between patients, but
also to explain the great negative average relative error,
which seems to be related to a wrong estimation of the
cardiac output. Probably, the cardiac output is the real
difference between the model and the reality between
patients. Although it doubtless is not the only
physiological parameter changing between patients, in
this study it is considered to be the most important
parameter to change, and the good results obtained seem
to give reason to this hypothesis.
It is obvious that the real-time control is only a
theoretical model, and that an experimentation should
be made before its application. Anyway, an automatic
real-time control could be really useful in clinical
application, giving a significant help to the anesthetist.
The acquired data are not exhaustive to have a
complete vision of the going of the operation, so the
acquisition program should gather information from
more than one instrument. These added data are also
useful to further refine the model and to credit more the
hypothesis discussed before.
138
Conclusions
Part I
Work supported by University of Trieste and by the Ministry
of the University and the Scientific and Technologic Research,
Italy, National Projects Cofin2000 n. MM09163913 and
"GARR-B - Regional Networks Strengthening".
References
[1] MAPLESON WW. (1973): Circulation-time models of the
uptake of inhaled anaesthetics and data for quantifying
them, British Journal of Anaesthesia, 45, pp. 319-34
[2] MAPLESON WW. (1978): Circulation-time models of the
uptake of inhaled anaesthetics and data for quantifying
them (Correction), British Journal of Anaesthesia, 50, p.
731
[3] LEROU JGC, DIRKSEN R, BENEKEN KOLMER HH, BOOIJ
LHDJ. (1991): A system model for closed-circuit
inhalation
anesthesia
I.
Computer
study,
Anesthesiology, 75, pp. 345-55
[4] MAPLESON WW. (1998): The theoretical ideal fresh-gas
flow sequence at the start of low-flow anaesthesia,
Anaesthesia, 53, pp. 264-72
[5] NATIONAL ELECTRICAL MANUFACTURERS ASSOCIATION
(2000): Digital imaging and communications in medicine
(DICOM):
Version
3.0,
(National
Electrical
Manufacturers Association, Rosslyn)
[6] FIORAVANTI F, INCHINGOLO P, VALENZIN G, DALLA PALMA
L. (1997): The DPACS project at the University of
Trieste, Medical Informatics, 22-4, pp. 301-14
[7] INCHINGOLO, P. (1998): Lintegrazione PACS, RIS e HIS.
Lezione magistrale, Relazioni Congresso Nazionale
ANMDO, Gubbio, Italy, 1998, pp. 16-22
[8] MAPLESON WW. (1996): Effect of age on MAC in
humans: a meta-analysis, British Journal of Anaesthesia,
76, pp. 179-85
IFMBE Proceedings
MEDICON 2001, 12-15 June 2001, Pula, Croatia
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hell On Earth Reloaded AdventureDocument16 pagesHell On Earth Reloaded AdventureKurt Garwood100% (1)
- Wiki SpeedDocument5 pagesWiki Speedprashanthfeb90100% (1)
- Resume Michal SzalonekDocument2 pagesResume Michal Szalonekszalonek4330No ratings yet
- GMP SIMATIC WinCC V15 en en-US PDFDocument216 pagesGMP SIMATIC WinCC V15 en en-US PDFsybaritzNo ratings yet
- English Language 4EA0/KEAO Paper 1 exemplarsDocument2 pagesEnglish Language 4EA0/KEAO Paper 1 exemplarsBooksNo ratings yet
- The History of AstronomyDocument3 pagesThe History of AstronomyAguilon Layto WendyNo ratings yet
- A Study On Employee Personality in Nature Capsules Ltd. in PondicherryDocument19 pagesA Study On Employee Personality in Nature Capsules Ltd. in PondicherryCHEIF EDITORNo ratings yet
- Increasing Seismic Safety by CombiningDocument386 pagesIncreasing Seismic Safety by CombiningIvan Hadi SantosoNo ratings yet
- Deutsche Bank Human Resources Report 2017Document57 pagesDeutsche Bank Human Resources Report 2017YamNo ratings yet
- Endcarriage - KZL-S 315Document116 pagesEndcarriage - KZL-S 315Josip Nuno CoricNo ratings yet
- Logic A4Document1,218 pagesLogic A4Alpheios Alpha100% (1)
- Tools of Data CollectionDocument36 pagesTools of Data CollectionJmarie Calumba100% (1)
- African American Women's LanguageDocument30 pagesAfrican American Women's LanguageRatih Santi MianawatiNo ratings yet
- September 2022 A - 035011Document127 pagesSeptember 2022 A - 035011EDMIL REBOLLOSNo ratings yet
- Public Service InnovationDocument112 pagesPublic Service InnovationresearchrepublicNo ratings yet
- IB Source AnalysisDocument8 pagesIB Source AnalysisRita LimNo ratings yet
- Itp 8Document5 pagesItp 8Arung IdNo ratings yet
- Using Sales and Operations PlanningDocument136 pagesUsing Sales and Operations PlanningJose Lara100% (1)
- Final QuestionDocument5 pagesFinal QuestionrahulNo ratings yet
- How To Be Happy All The Time - NLP AnchorsDocument9 pagesHow To Be Happy All The Time - NLP Anchorsmramakrishna919No ratings yet
- Surface Treatment of Flexible PavementDocument36 pagesSurface Treatment of Flexible PavementUsman Ahmad0% (1)
- Android Caputre CameraDocument7 pagesAndroid Caputre CameraSagarraj WangdareNo ratings yet
- An Alarming National Trend - False Rape AllegationsDocument7 pagesAn Alarming National Trend - False Rape Allegationsdesbest100% (1)
- SaaS Marketing Automation Playbook TeaserDocument19 pagesSaaS Marketing Automation Playbook TeaserValery FenskeNo ratings yet
- Seance 1 Introduction To DystopiaDocument32 pagesSeance 1 Introduction To DystopiaHanane AmadouNo ratings yet
- Data Encryption DecryptionDocument60 pagesData Encryption DecryptionMohit Sharma100% (2)
- Beno K Pradekso - Solusi247 - In40aiDocument36 pagesBeno K Pradekso - Solusi247 - In40aiMuhammad HattaNo ratings yet
- Ignou Assignment 2018 BA III YearDocument6 pagesIgnou Assignment 2018 BA III YearTelika RamuNo ratings yet
- BT 203 Basic Mechanical Engineering May 2019 PDFDocument2 pagesBT 203 Basic Mechanical Engineering May 2019 PDFKunta PatleNo ratings yet
- Total Productive MaintenanceDocument41 pagesTotal Productive Maintenancejeff090288No ratings yet