Professional Documents
Culture Documents
Pharmacology - A Summary of Common Conditions
Uploaded by
Jeremy YangOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharmacology - A Summary of Common Conditions
Uploaded by
Jeremy YangCopyright:
Available Formats
Pharmacology Notes
Medical Rotation - 2015
PHARMACOLGY NOTES
ROTATION B
MEDICAL
2015
Ron Castelino- 10-12 MCQs in end of year exams
Question hint: What is used for HTN in pregnancy.
Pharmacology Notes
Medical Rotation - 2015
Contents
Contents............................................................................................2
Angina...............................................................................................3
Congestive Heart Failure....................................................................6
Acute Heart Failure............................................................................................. 8
Acute Coronary Syndrome..................................................................9
Hypertension...................................................................................13
Arrhythmias.....................................................................................18
Asthma............................................................................................23
Antimicrobial Therapy......................................................................26
COPD...............................................................................................31
Dyslipidemia....................................................................................34
Diabetes Mellitus.............................................................................36
Pharmacology Notes
Medical Rotation - 2015
Angina
-
Presentation of Central Chest Tightness of Heaviness- brought on by
exertion, alleviated by rest. Etiology Atherosclerosis > anaemia
Stable vs Unstable Vs Variant (Prinzmetal)
o S w\ exertion - goes away with rest/GTN
o U at rest- not often relieved with GTN
o V Vasospasm of the Coronary Arteries. Relieved by Nitraterandom presentation (not rest/exertional) pattern... typical in
AM- 1st line therapy blood supply.
Principles of Mgmt
-
Modify Risk Factors smoking, exercise, BMI, HTN, DM
Drug therapy Rationale -Symptom relief and Prevent MI
1. Chest Pain relief- Short Acting Nitrate
2. blocker or if contraindicated Ca2+-Channel Blockers, Long Acting
Nitrates-Inotropic (O2 demand)3. Statin- Independent of Cholesterol Profile to CVD risk
4. Consider Other Antianginals- Ivabradine, Nicorandil, Perhexiline
Class
Short Acting
Nitrates
Name
Glyceryl Trinitrate GTN
Long Acting
Nitrates
Isosorbide dinitrate
Isosorbide
mononitrate
Blockers
Atenolol*
Propranolol*
Carvedilol*
Bisoprolol
Notes
Sublingual (to
bypass liver
metabolism) 1 minute
to effect lasts <30
mins
Relieve or prevent
chest pain
Also available in a
transdermal patch.
30 minutes to effectlast 10-12 hours
Prophylactic before
exercise
Oral Prevents angina
in patients with
frequent symptoms.
30minute to work
Cleared Renally
Consider in Patients
with HF and reduced
ejection fracture
Consider in Patients
3
Pharmacology Notes
Medical Rotation - 2015
Metoprolol
Labetalol
Nebivolol
Oxprenolol
Pindolol
Calcium Channel
Blockers
Amlodipine
Clevidipine
Diltiazem
Felodipine
Lercanidipine
Nifedipine
Nimodipine
Verapamil
Antianginal
Nicorandil
Ivabradine
Perhexiline
with HF and reduced
ejection fracture
Consider in Patients
with HF and reduced
ejection fracture
Pregnancy
Avoid Have intrinsic
sympathomimetic
activity less effective
and no evidence of
MI risk.
Arterial vasodilator
variant angina.
Negative Inotropic
effect- combine with
blockers cautiously. (
AV conduction).
Extended release oral
form- arterial
vasodilator
May worsen angina at
start of therapy. Reflex
tachycardia w\
cessation.
Dont combine with
blocker- severe
bradycardia and heart
block.
Contraindicated in
patients with systolic
HF
Controlled release
used in stable angina.
Produces venous and
arterial dilation via
Nitrate and K+
channels in smooth
muscle. improves
myocardial O2 balance.
HR at the SA node,
improves exercise
tolerance
Changes myocyte
4
Pharmacology Notes
Medical Rotation - 2015
metabolism improving
O2 demand and
utilisation. Antiischaemic effects via
long-chain fatty acid
metabolism.
Hepatotoxicity
Notes
-
1 Selective agents are preferred Atenolol, Metoprolol (w\ HF),
Propranolol.
Nitrates can cause reflex tachycardia- blockers prevent this
when used in combined therapy.
Vasospastic angina- blockers contraindicated exacerbate
symptoms when -mediated vasoconstriction is unopposed by mediated vasodilation.
Short acting dihydropyridines should be avoided in CAD = MI
mortality.
Non-dihydropyridines can worsen HF due to negative inotropic
effect.
Remember- Nitrates contraindicated in ICP and hypovolemia.
Pharmacology Notes
Medical Rotation - 2015
Congestive Heart Failure
-Cardiac Output is inadequate for the bodys requirements.
Systolic Vs Diastolic Failure.
-
Systolic Failure- inability of the ventricles to contract normally =
CO Ejection Fracture is <40% - Etiology IHD, MI, Cardiomyopathy
(non-ischaemic idiopathic dilated) or (less common are druginduced, peripartum, inflammatory, alcoholic, HIV-related
cardiomyopathy).
Diastolic Failure inability for the ventricles to relax, filling,
filling pressures, Ejection Fracture is >50%- Etiology Constrictive
pericarditis, tamponade, restrictive cardiomyopathy, hypertension,
IHD.
o Note: Usually Systolic and Diastolic failures co-exist.
Left Ventricular Vs Right Ventricular independently or together as
congestive cardiac failure.
-
Left Ventricular Pulmonary Congestion Signs: Cheyne-Stokes
respiration, wheeze (cardiac asthma, see below), crackles,
pulmonary oedema, pleural effusion Symptoms: Dyspnoea,
exercise tolerance (SOBOE), fatigue, orthopnea, PND, nocturnal
cough w\ pink frothy sputum, nocturia, cold extremities, weight loss
and muscle atrophy.
Right Ventricular Systemic Congestion Caused by LVF, Pulmonary
Stenosis and Lung Disease. Signs: Peripheral oedema, ascites,
facial engorgement, pulsations in the neck and face (w\ tricuspid
regurgitation), raised JVP, hepatomegaly, epistaxis Symptoms:
nausea, bloating, anorexia, abdominal pain and constipation.
New York Heart Association Classification
-
Class
Class
hill)
Class
Class
1- no symptoms
2- slight dyspnoea w\ exertion- (climbing stairs, walking up
3- Moderate dyspnoea w\ walking one flight of stairs
4- Severe dyspnoea, unable to perform physical activity.
Principles of Mgmt
Alter lifestyle factors Smoking cessation, Na+ in diet, weight loss.
Treat underlining cause e.g. dysrhythmias, valvular disease.
Treat exacerbating factors anaemia, thyroid disease (thyrotoxicosis,
myxoedema), infection, HTN, cor pulmonale, obesity, glomerulonephritis,
pregnancy, nutritional deficiencies.
Avoid exacerbating factors6
Pharmacology Notes
o
o
o
o
o
Medical Rotation - 2015
Na+/ H2O retention NSAIDS, glitazones, corticosteroids,
androgens)
Ve Inotropes- Verapamil (CCA), itraconazole
Cardiotoxins- cytotoxics, cocaine, amphetamines, alcohol,
ergot alkaloids, pergolide
Bradycardia inducing- cholinergic drugs, anticholinesterases
Others vasodilators, moxonidine, decongestants, TNFantagonists
Prevention- Influenza and Pneumococcal Vaccination
Drug Therapy- rationale symptom relief, improve exercise tolerance
and QoL, mortality Think: ABCD
1. Ace Inhibitor
2. Beta Blocker
3. Cardiac Glycoside
o Digoxin in patients with AF
o Spironolactone in patients w\o AF
4. Diuretic (symptom control)
Class
Ace Inhibitor
ARBs
Beta Blocker
Cardiac Glycosides
Name
Captopril
Enalapril
Fosinopril
Lisinopril
Perindopril
Quinapril
Cadesartan
Valsartan
Bisoprolol
Carvediolol
Metoprolol XL
Nebivolol
Digoxin
Notes
Recommended for all CHF
with LVEF <40%
- Preload and
afterload, improve S
& S with SOBOE
and QoL
- Slows disease
progression,
hospitalisation rates
survival
C/I renal artery
stenosis
Only these two indicated for
HF in aus
Titrate slowly
May exacerbate initially
bradycardia and
hypotension.
Digoxin in patients w\ AF
-dose with renal
impairment
Adverse effects/toxicity
nausea, vomiting, anorexia,
blurred/ halo vision, ectopic
beats
****Not for diastolic HF****
7
Pharmacology Notes
Medical Rotation - 2015
Diuretic
Spironolactone
Eplerenone
Diuretic- symtrom
relieving
Hydrochlorothiazi
de
Chorthialidone
Ivabradine
(aldosterone antagonists)
Spironolactone w\out AF* in
addition, for patients who
remain symptomatic
despite ACE-I and diuretic.
Thiazides urine volume
by 10%
Consider adding Ivabradine
to optimal standard
treatment (including betablocker) in patients with
continuing symptoms of
moderate-to-severe heart
failure (left ventricular
ejection fraction (LVEF)
<35%) if in sinus rhythm
and heart rate >77
beats/minute
ARBS for patients with Kinin-mediated adverse effect (cough) with ACEIs
Acute Heart Failure
1. Airway Stability and Oxygenation
2. BP and COa. Inotropic support- dopamine, dobutamine
b. Diuretic IV frusemide
c. Vasodilator IV GTN/ nitroprusside
3. Relieve congestive symptoms
4. Manage Complications- arrhythmias, acid-base imbalance
Notes:
Cardiac Asthma- Congestion of the bronchial mucosa.
Pharmacology Notes
Medical Rotation - 2015
Acute Coronary Syndrome
The initial working diagnosis of a patient presenting with Chest pain is
ACS.
-
Working Diagnosis: ST-segment elevation MI Vs Non-ST segment
elevation ACS
- Evaluation of ECG and biomarkers
- Final Diagnosis: STEMI, Vs non-STEMI, Vs Unstable angina
Principles of Mgmt
Reperfuse the ischaemic myocardium
Minimise Infarct Size
Relieve symptoms
Prevent complications
STEMI example
Acute Care -000 emergency
-
Reperfusion therapy (antiplatelet).
o 300mg chewable/dissolvable aspirin 300mg (loading dose, if
aspiring not already taken)
o + Either
300mg Clopidogrel orally (600mg is PCI).
OR
60mg Prasugrel orally in patients >60kg, <75y.o
OR
180mg ticagrelor orally
If known hypersensitive to 1 of the above 3, avoid
ALL as known cross-reactivity.
Cannulate- large gauge needle
IV morphine- for pain and venodilatory effect
Oxygen therapy
GTN- if ongoing chest pain.
Notify emergency/cardiology of incoming patient.
12 lead ECG
o ST elevation of >2mm on chest leads V1-3, >1mm in two
contaginous leads, or presumed new LBBB
Anterior Wall Ischemia V2-4
Anteroseptal Ischemia V1-3
Apical or Lateral Ischemia V4-6
Inferior Wall Ischemia II, III, aVF
Posterior Wall Ischemia, depression in V1-2 w\ upright T
waves. Plus, ST elevation in posterior leads V7-9
Pharmacology Notes
Medical Rotation - 2015
Blood Tests
o Cardiac Enzymes
Troponin Most cardiac specific marker, but NOT MI
specific- initial reading asap. 8 hours detect most MI, 12
hours all.
CK-MB- Normalises in 3-4 days therefore the preferred
marker in re-infarction.
LD lactate dehydrogenase
Myoglobin
o FBC
o Serum Creatinine and Electrolytes
o Blood Glucose Levels
o UEC
o LFT
Interventions- Reperfusion therapy to restore blood flow to viable
myocardium.
-
Fibrinolytic therapy- pharmaceutical- within 30minutes of medical
intervention (especially if known PCI unavailable). Dissolution of clot
via
o Pharmacotherapy
Fibrin selective- IV Tenecteplase, Alteplase, OR,
Reteplase
Non-fibrin selective - Streptokinase
Absolute contraindications**- need transfer to
appropriate facility for PCI
Risk of bleeding active or diathesis, Suspected aortic
dissection, INR>2-3 (on anticoagulant therapy)
Risk of intercranial haemorrhage stroke w\in 3/12,
known mets or 1, vascular lesion.
o Relative Contraindications
Pregnancy
Active Peptic Ulcer
o Adjuvant therapy
antithrombin therapy risk of re-occlusion- DVT, PE
Enoxaparin or unfractionated heparin
Percutaneous Coronary Intervention-transluminal coronary
balloon angioplasty and stenting. - mechanical intervention- within
90-120 minutes of medical intervention
o Adjuvant therapy.
Antiplatelet
Heparin OR bivalirudin
10
Pharmacology Notes
Medical Rotation - 2015
Optional additional platelet glycoprotein IIb/IIIa inhibitor
(NSTEACS)
o Types of Stent
Drug-eluting Stent - Used more in practice- is dependent
on patient compliance with dual antiplatelet therapy.
Bare Metal Stent
Coronary Artery Bypass Grafting
o w\ CBP (cardiopulmonary by pass)
o & To operate on still heart- fibrillate, hypothermia or
Cardioplegia (with K+ rich solution)
o Median Sternotomy, Conduit (saphenous vein, radial artery)
anastomosed to coronary artery beyond lesion and ascending
aorta. OR Left internal thoracic artery (LITA) to LAD
(maintains original pathway from left subclavian).
Risks death, stroke, sternotomy bleed or tamponade,
infection, AF, renal failure.
NOTES:
PCI implies Stenting, angiography is imaging technique not intervention
If presentation of patient is >12 hours after onset of symptoms, MI may be
complete.
Reperfusion (fibrinolytic) should be considered w\
o Continuing ischemia (persistent pain).
o Viable myocardium (preservation of R waves in infarct leads)
o Major complications (cardiogenic shock).
11
Pharmacology Notes
Medical Rotation - 2015
In addition
-
+ Nitrates
blockers within 24hours for HR and BP stabilising
Calcium Channel Blockers
ACE-Is
Secondary Prevention
-
Antiplatelet therapy
Beta-blockers
SL NTG
ACE-I/ARB
Warfarin
Spironolactone
Statin
? Fish Oils- we dont obtain therapeutic dose from current capsules.
Lifestyle Changes
12
Pharmacology Notes
Medical Rotation - 2015
Hypertension
Isolated systolic hypertension- from atherosclerosis of the large arteries.
Accelerated Phase (malignant) Hypertension- rapid BP leading to
vascular damage.
-
Systolic >200mg, diastolic >130mg
Bilateral retinal haemorrhage
Papilledema (swelling of optic disc). ** marker of malignant HTN
of ICP
Essential Hypertension- unknown cause
Secondary Hypertension
-
Renal- intrinsic renal disease- Glomerulonephritis, polyarteritis
nodosa, chronic pyelonephritis, systemic sclerosis, polycystic kidney.
Renovascular disease- atheromatous
Endocrine- Cushings, Conns Syndrome, pheochromocytoma,
acromegaly, hyperparathyroidism
Other- Pregnancy, Coarctation (congenital narrowing), Steroids.
Principles of Mgmt
Treat underlying cause- renal disease, alcoholism
Identify and Treat other CVD risk factors- dyslipidemia, obesity, smoking,
alcohol, diabetes.
Remove Secondary causes NSAIDs,
Drugs therapy- rationale -Reduce Premature Cardiovascular morbidity
and mortality. microvascular disease of the brain, kidney and retina.
Attempt to reach recommended targets.
For uncomplicated hypertension
1. ACE Inhibitor (or ARB)
13
Pharmacology Notes
Medical Rotation - 2015
2. Dihydropyridine CCB
3. Thiazide Diuretic (low dose)
With inadequate response add additional therapy instead of dose.
dose will more likely cause adverse effects. Preferred combinations 1 +
(2 or 3,) OR (2+3).
If BP remains elevated consider
o
o
o
o
o
o
o
Compliance
High sodium diet (try lowering)
Secondary hypertension (including drug induced)
Volume overload- chronic kidney disease
Sleep apnoea
Alcohol/recreational drug use
White coat
1. Ace inhibitors are first line, contraindicated in pregnancy
-
Most
o
S/E:
o
o
o
o
ACE-Is have similar features,
Exception Captopril: Short half-life- rarely used.
Cough
Hypokalaemia
Hypotension
Angioedema rare but serious
Can occur at any time during treatment
One occurrence is contraindication for future use of all
ACE-Is and ARBs
With Impaired Renal Function:
o First line drug for kidney disease with hypertension
o Dose may need to be adjusted
o GFR monitoring
If it decreases more than 25% from baseline cease ACEIs
+
o K should not exceed 6
Monitor: Kidney function, potassium, cough, angioedema
ARBs
-
Most ARBs have similar features, except losartan, which has risk
of side effects and hepatotoxicity.
2. Calcium channel blockers
-
Dihydropyridines act peripherally as vasodilators, and are used in
uncomplicated HTN
o Nifidipine has a short half life, but a slow-release form can be
used
14
Pharmacology Notes
Medical Rotation - 2015
o Nifidipines immediate release form has a high rate of reflex
tachycardia as a side effect shouldnt be used in anyone who
has angina (can worsen symptoms or precipitate MI).
o Amlodipine is most commonly used
-
Side effects:
o Peripheral oedema. This is diuretic resistant, as it is a result of
fluid redistribution, rather than fluid overload, only goes away
w\ treatment cessation.
o Hypotension
o Headache (especially early in treatment), goes away w\ time
o Reflex tachycardia
Notes:
Diltiazem and verapamil are centrally acting not used in uncomplicated
HTN
Only Nifedipine can be used in pregnancy.
3. Thiazide Diuretics
-
Only used as First line treatment in those over 65
o It is associated with new onset diabetes
Good evidence for treating Isolated systolic HTN
Peripheral resistance, - at low dose cause vasodilation
o Hydrochlorothiazide
12.5-25mg is an anti HTN dose
25mg is diuretic dose
Other diuretics are not used unless fluid overload issues.
Use in impaired renal function- When creatinine clearance <25,
thiazides will have no diuretic effect, but can still be used at a low
dose for their vasodilatory effects
Side Effects
o Electrolyte disturbances ( common at low dose)
o Precipitation of gout (competes w\ uric acid for excretion at
kidneys)
o Glucose intolerance- new onset diabetes
15
Pharmacology Notes
Medical Rotation - 2015
16
Pharmacology Notes
Medical Rotation - 2015
*** blockers are no longer first line therapy in isolate systolic HTN
because of association with new onset diabetes. It is acceptable to
continue use in elderly on long term use.
Labetalol can be used in pregnancy, others are contraindicated
Used in complicated hypertension in patients with IHD:
-
Do not use pindolol or oxprenolol these have intrinsic
sympathomimetic activity and may precipitate MI
Side effects:
o Cold extremities
o Bronchoconstriction
o Sexual dysfunction
o Nightmares and insomnia (metoprolol and propranolol)
Other drugs that may be used:
-
Alpha agonists:
Methyldopa used first-line in pregnancy, as it has the most
evidence for safety, but otherwise rarely used
Potassium sparing diuretics- If patient is hypokalemic on other
diuretics
17
Pharmacology Notes
Medical Rotation - 2015
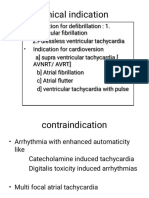
Arrhythmias
Disturbance of the cardiac rhythm.
Drug Therapy-Rationale
-
Prevent sudden cardiac death.
Prevent recurrence of life-threatening arrhythmias.
Restore haemodynamic stability.
Restore sinus rhythm.
Control ventricular rate in AF (without restoring sinus rhythm).
Provide symptom relief.
Atrial Fibrillation
Irregular atrial rhythm 300bpm, AV node responds intermittentlyirregular ventricular rate. CO: 20% because filling/co-ordination.
Pulse: Irregular Irregular, Auscultation: Varying intensity of 1st heart sound.
Classification:
-
Recurrent- occurs more than once
Lone - <60yrs w\ no evidence of cardiopulmonary disease.
Valvular- w\ rheumatic valve disease or prosthesis.
Paroxysmal- 7 days, spontaneous return to Sinus Rhythm
Persistent- > 7 days requires Cardioversion or Pharmacological
Mgmt
Permanent- >1yr
Thromboembolic risk
-
Virchows Triad
o Disorganised Flow
o Hypercoagulability
o Endothelial Dysfunction
Principles of Mgmt
Treat underlying cause: HF, IHD, HTN, PE, Mitral Valve disease,
Pneumonia, Hyperthyroidism, caffeine, alcohol, post op, K+, and Mg2+
Non-pharmacological therapies:
-
Carotid sinus massage- vagal stimulation - HR = Good for SVT
Direct cardioversion (Af/Aflutter, VT/VF, highly successful - 80-90%)
Cardiac pacing (permanent pacemakers, for bradycardia, AV block),
Radiofrequency or surgical ablation (localised foci, SVT, AF, Aflutter)
- Multiple ablations may be required.
18
Pharmacology Notes
Medical Rotation - 2015
Cardioversion
Pharmacological
Advantages
- No need for sedation
- Potential to enhance
subsequent electrical
cardioversion
Disadvantages
- Continuous medical
supervision
- Proarrhythmia
- Thromboembolic
- Lo success rate for
longstanding AF
Electrical
Advantages
- Success Rate >90%
Disadvantages
- Needs sedation
- Skin burn
- Proarrhythmia
- Thromboembolic
- Potential interference of
other medical devices
Rate Vs Rhythm Control
19
Pharmacology Notes
Medical Rotation - 2015
Rate Control
Target Range HR 60-80bom resting, 90-115 w\ exercise
Drug Therapy
To obtain and maintain ventricular rate control:
-
blockers- Atenolol, Metoprolol
CCB Diltiazem/Verapamil (Non-dihydropyridines)
Digitalis- Digoxin
Class III antiarrhythmic Amiodarone
o When other methods ineffective.
Rhythm Control
Conversion the Sinus Rhythm
-
More successful in recent onset AF, L atrium normal size.
o Avoid in elderly asymptomatic chronic AF
Drug Therapy
-
Amiodarone
Flecainide
Thromboembolic Risk treatment
Electroversion w\ no evidence of thrombus
-
Subcutaneous Enoxaparin, risk of thrombus post stunning
Three weeks of anticoagulant therapy in patient w\ Thrombus prior to
electroversion
-
Sub Cut- Dalteparin OR
SC Enoxaparin
IV Unfractionated Heparin
Longterm
-
Aspirin OR
Warfarin (Valvular AF) OR
Dabigatran
20
Pharmacology Notes
Medical Rotation - 2015
Post Cardioversion Rhythm maintenance
-
Flecainide OR
Sotalol OR
Amiodarone
Acute AF w\ very ill patients / haemodynamically unstable
-
O2
U&E
Emergency Cardioversion within 48hrs (amiodarone if unavailable).
Anti-coagulation therapy - LMWH
Ventricular Rate control
o 1st line Verapamil OR Bisoprolol
o 2nd line Digoxin OR Amiodarone.
Notes:
Limitations of warfarin; slow onset of action, individual variability,
food/drug interactions etc require regular monitoring and dosage
adjustment
Newer anticoagulants (faster onset of action, fewer drug/food interactions,
lower bleed risk etc)
-
Xa inhibitors; rivaroxaban (direct/specific competitive Xa inhibitor,
not inferior to warfarin with similar adverse events), apixiban (better
than aspirin in AF who could not take warfarin with reduced
stroke/embolism)
IIa inhibitor; dabigatran (direct thrombin inhibitor)
Ventricular arrhythmias;
-
VT; Clinical features if >30secs (lignocaine/amiodarone/sotalol,
cardioversion, radio frequency/ablation)
VF; Sudden loss of consciousness, no BP, no pulse, cyanosis, death
3-5minutes
Torsades de pointes; VT with QT prolongation, prolonged can lead to
VT and death (lignocaine,
21
Pharmacology Notes
Medical Rotation - 2015
Sinus bradycardia; caused by increased vagal tone, hypothermia,
hypothyroidism, BB, CaCB, digoxin, amiodarone (treated with atropine)
Reminder
-
Class
Class
Class
Class
Class
Class
Class
1a- Na+ channel blocker- disopyramide
1b- Na+ channel blocker-lignocaine
1c- Na+ channel blocker-flecainide
2- sympathetic blockers- B-blockers
3- potassium channel blockers- amiodarone, sotalol
4- Ca channel blockers- verapamil, diltiazem
5- Other- adenosine, digoxin
Secondary to Heart Failure
All arrhythmias are more frequent in patients with heart failure.
-
Atrial Tachyarrhythmias
o Atrial Fibrillation
o Atrial Flutter
Atrial enlargement = atrial stretch (proarrhythmic
mechanism).
Ventricular Tachyarrhythmias
Principles of antiarrhythmic therapy in Heart Failure
-
Avoid K+ depletion from diuretic therapy- Use K+ sparring agents.
Avoid Mg+ depletion from diuretic therapy
Use ACE-I in all patients at maximum dose tolerated.
Use blockers
Avoid long-term use of cardiac stimulants ( agonists, or MilrinonePDE-I) because of their proven proarrhythmic quality.
Avoid Class I arrhythmics (proarrhythmic quality).
22
Pharmacology Notes
Medical Rotation - 2015
Asthma
Chronic Obstructive Respiratory Illness. Difficulties in exhaling airresulting in wheeze and hyperinflation.
Airway narrowing via Type 1 hypersensitivity (IgG): Remember has an
acute phase and latent phase (2-24hr later).
-
Bronchial muscle contraction w\ smooth muscle and basement
membrane hypertrophy results in narrowed bronchial lumen.
Mucosal swelling- mediated by mast cell and basophil
degranulation-eosinophil mediated asthma, results in
submucosal oedema and epithelial desquamation.
Increased mucus production. goblet cell hyperplasia and mucous
plugging.
Status Asthmaticus- acute exacerbation of repetitive attacks of asthma.
Remains unresponsive to initial treatment w\ bronchodilators.
Diagnosis- observe obstructive respiratory pattern w\ spirometry.
FEV1/FVC, (ratio) + RV w\ usually a 15% Fev1 following 2 agonists
or steroid therapy.
Principles of Mgmt
Encourage self-management to increase compliance
Identify and Avoid Precipitant- Common = dust mite, pollen, moulds,
domestic pets, drugs ( blockers, NSAIDs, Aspirin), exercise.
Lifestyle factors smoking
Re-enforce good inhaler technique
Consider Influenza and pneumococcal vaccination. Consider
desensitisation for allergens
Drug Therapy- Rationale- Symptom control and relief, prevent
exacerbation, improve and maintain lung function and QoL.
Adults:
1. SABA for symptom relief
o SABA only if sympt. <2 times in a month + no flare up in a
year
o w\ low dose Inhaled Corticosteroids when above is not the
case.
2. Low-dose ICS + LABA for maintenance try use fixed-dose
combination inhaler
o SABA for symptom relief.
3. Medium dose ICS + LABA
23
Pharmacology Notes
Medical Rotation - 2015
o SABA for symptom relief, though not required if using
Budesonide.
4. High Dose ICS + Laba
o SABA for symptom relief,
SABA = relievers every 20 minutes until effective, + 1-4hrly if
symptoms persist
-
Salbutamol
Terbutaline
S/E tremor, tachycardia and headache. SEVERE- high dose =
hypokalemia, Lactic acidosis with IV due to resp. compensation.
LABA= maintenance
-
Eformoterol- twice daily,
o Budesonide (ICS) = (Symbicort)
o Fluticasone (ICS)
Salmeterol- twice daily
o Fluticasone (= SERETIDE)
Vilanterol- once daily (This LABA is always coupled with one of the
following)
o Fluticosone
o Umeclidinum (anticholinergic)
ICS=preventer
-
Beclomestasone diproprionate
Budesonide
Ciclesonide
Fluticasone
S/E
o Dysphonia time to recover
o Candida- rinse mouth to prevent
o Adrenal suppression dose related. Always do a 3 mth
review
NOTE: long term use of corticosteroid can lead to Cataracts (posterior
subcapsular) and Osteoporosis.
Leukotriene Receptor Antagonists- has effect on both the acute and
chronic phase of asthma.
-
Montelukast- 2yrs
Indications
24
Pharmacology Notes
Medical Rotation - 2015
Preventer
o Day/night symptoms
o Exercise induced bronchoconstriction
Treatment of aspirin-sensitive asthma patient
As add on therapy to ICS where LABAs are not tolerated or control is
inadequate.
Consider ketamine in intubated asthmatic patients
Children
1-2yrs
1. SABA
2. Cromoglycate or Nedocromil for persistent asthma
3. Consider low dose ICS if symptoms disrupt sleep or no response for
cromone after 2-4 weeks.
>2yrs
1. SABA symptom control
2. Add montelukast for frequent intermittent or mild persistent asthma
3. Add low dose ICS for persistent asthma stop after 3mths if control is
good, esp. if >6yrs
At > 6yrs
4. Change montelukast to low dose ICS- or increase dose if already using.
Cromoglycate (cromone) 3-4 times a day
-
Inhibits inflammatory mediator release from mast cells
S/E- nasal congestion
Montelukast
-
Inhibits cysteinyl leukotriene receptor; antagonises airway smooth muscle
contraction and inflammation caused by leukotrienes.
S/E headache and nasal congestion. Potential hyperreactivity.
Dermatologic and psychiatric rare by note worthy. REVIEW-REPEAT
dispensing.
C AND M can be used in patients with intolerable dysphonia induced by ICS
25
Pharmacology Notes
Medical Rotation - 2015
26
Pharmacology Notes
Medical Rotation - 2015
Antimicrobial Therapy
Consider:
-
Organisms Identity
Organisms Susceptibility
o Bacteriostatic arrests growth and replication, limiting spread
o Bactericidal- kills the bacteria
Site of infection
o Remember Lipid soluble to penetrate BBB,
o low molecular weight can penetrate BBB
o high Protein content will not pass into CSF
Patient Factors
o Immune System
o Renal Dysfunction elimination
o Hepatic Dysfunction
o Poor perfusion- circulation to areas of infection
effectiveness of therapy.
o Age
o Pregnancy- Cross Placenta,
CONTRAINDICATION: Aminoglycosides
o Lactation
o Presence of foreign body
o Hx of Allergy/Adverse reactions
Safety of the Agent
Cost of the Therapy
Route of Administation
o Oral- mild infections
o IV for serious
Types of Antimicrobial Therapy
Penicillin
Bactericidal- cell lysis and death- interfere w\ bacteria cell wall
peptidoglycan synthesis when bound to penicillin-binding proteins. C/I- hx
of allery.
-
Amoxycillian
o Extended spectrum
o Rash- widespread erythematous maculopapular rash is
common.
o Indication
Exacerbation of chronic bronchitis, community-acquired
pneumonia
Acute bacterial otitis media, sinusitis
Gonococcal infection
27
Pharmacology Notes
Medical Rotation - 2015
Epididymo-orchitis, acute prostatitis, acute
pyelonephritis, UTI
Non-surgical prophylaxis of endocarditis
Acute cholecystitis, peritonitis, eradication
Amoxycillin w\ Clavulanic Acid = Augmentin
o Active against Beta-Lactamase
o Indication
Hospital-acquired pneumonia
Epididymo-orchitis (urinary tract source)
PID (not sexually acquired)
UTI
Bites and clenched fist injuries
Otitis media (unresponsive to amoxycillin)
Acute bacterial sinusitis (unresponsive to amoxycillin)
Acute cholecystitis (after IV treatment)
Melioidosis
Ampicillin
o Extended spectrum
o Indications
Exacerbation of chronic bronchitis, community-acquired
pneumonia
Gonococcal infection, UTI
Non-surgical prophylaxis of endocarditis
Acute cholecystitis, peritonitis, epididymo-orchitis, acute
pyelonephritis, acute prostatitis
Benzathine penicillin
o Narrow Spectrum
o Prevention of Rheumatic fever
Benzylpenicillin
o Narrow Spectrum
o Indication
Bacterial endocarditis
Meningitis
Aspiration pneumonia, lung abscess
Community-acquired pneumonia
Syphilis
Septicaemia in children
Dicloxacillin
o Narrow Spectrum (stable to beta-lactamases)
o Indications
Staphylococcal skin infections including folliculitis, boils,
carbuncles, bullous impetigo, mastitis, crush injuries,
stab wounds, infected scabies
Pneumonia
Osteomyelitis, septic arthritis
Flucloxacillin
o Narrow Spectrum (stable to beta-lactamases)
28
Pharmacology Notes
Medical Rotation - 2015
o Indications
Staphylococcal skin infections including folliculitis, boils,
carbuncles, bullous impetigo, mastitis, crush injuries,
stab wounds, infected scabies
Pneumonia
Osteomyelitis, septic arthritis
Septicaemia
Empirical treatment for endocarditis
Surgical prophylaxis
Note C/I for flucloxacillin and Dicloxacillin= Cholestatic hepatitis, risk
>55yrs, female and course > 2 weeks.
-
Phenoxymethylpenicillin (Penicilllin V)
o 60-70% absorbed orally.
o Limited to Staph and Strep
o Indications
S. pyogenes tonsillitis, pharyngitis or skin infections
Prevention of rheumatic fever
Moderate-to-severe gingivitis (with metronidazole)
Ticarcillin w\ Clavulanic Acid
o Toxicity Impaired platelet function/
o Indications
Mixed (aerobic and anaerobic) infections, especially if P.
aeruginosa is involved
Febrile neutropenia
Notes:
Jarisch-Herxheimer reaction
Fever, chills, headache, hypotension and flare-up of lesions lasting for 12
24 hours (due to release of pyrogens from the organisms) can occur
shortly after starting to treat syphilis and other spirochete infections;
prednisolone may be used to minimise likelihood of reaction in
cardiovascular syphilis or neurosyphilis where this can be dangerous
Aminoglycosides
For treatment of serious gram-negative intestinal infections and sepsis
Inhibit protein synthesis by irreversibly binding to the 30S ribosomal
subunit and causing cell membrane damage. Concentration-dependent
bactericidal effect.
Adverse Effect- Serious and dose-related
-
Ototoxicity
Nephrotoxicity
Transient Myasthenic Syndrome
29
Pharmacology Notes
Medical Rotation - 2015
May result in respiratory depression; can usually be reversed with
prompt administration of IV calcium gluconate; the effect of neostigmine
is variable.
-
Amikacin
o Indications
Treatment of infections caused by organisms resistant to
other aminoglycosides
Mycobacterial infections
Gentamicin
o IM/IV
o Indications
Empirical treatment for <48 hours of serious Gramnegative infections
Serious systemic enterococcal infections (with betalactams or vancomycin)
Serious infections due to sensitive organisms that are
resistant to other antibacterials
Surgical prophylaxis
P. aeruginosa infections, including cystic fibrosis,
bronchiectasis (inhalation)
Brucellosis
Eye infections
Tobramycin
Cephalosporins
-
First generation; Cephalexin, cephazolin, cephalotin (strep, UTI)
Second generation; cefaclor and cefuroxime (alternative to
amoxycilin - otitis media, sinusitis, gonococcal), cefoxitin
(prophylaxis of GI procedures, non-tuberculosis mycobacterium,
clostridium)
Third generation; cefotaxime and ceftriaxone (in combination with
other Abx - meningitis, peritonitis, pneumonia, cholecystitis),
ceftazidime (pseudomanas),
Fourth generation; cefeprime (broad spectrum activity of all
cephalosporins, used for sepsis, pseudomonas and cephalosporin
resistant infections)
S/E Those with anaphylactic reaction to penicillins should not have
cephalosporins
Monobactams - Aztreonam; (gram ves - pseudomonas)
Carbapenems
-
Imipenem, doripenem, ertapenem, meropenem (resistant staph,
pneumococcus, H influenza pseudomonas)
S/E Neurotoxicity, nausea and vomiting
INHIBIT PROTEIN SYNTHESIS
30
Pharmacology Notes
Medical Rotation - 2015
Macrolides
-
Azithromycin (chlamydia), clarithromycin, roxithromycin,
erythromycin (respiratory tract infections)
S/E Nausea, vomiting, diarrhoea, prolonged QT (CYP450 inhibition)
Aminoglycosides
-
Gentamycin, streptomycin, tobramycin, amikacin (severe gram ve
infections of GI and sepsis)
S/E ototoxicity (nausea, vomiting, vertigo, hearing loss, tinnitus),
nephrotoxicity (also cleared by kidneys so can be difficult cycle),
neuromuscular blockade
Tetracycline
-
Doxycycline, minocycline, tetracycline, demeclocycline (RTI, acne,
malaria prophylaxis)
S/E nausea, vomiting, diarrhoea, epigastric burning,
photosensitivity, tooth discolouration (impair absorption of Ca, zinc,
iron, Mg, Zn, antacids)
INHIBIT BACTERIAL DNA SYNTHESIS
Nitroimidazoles
-
Metronidazole, tinidazole (anaerobic bacterial and parasitic
infections)
S/E nausea, vomiting, diarrhoea, metallic taste (interacts with
alcohol and warfarin)
Quinolones
-
Ciprofloxacin, norfloxacin, ofloxacin (other agents
ineffective/contraindicated UTIs, joint/bone infections, prostatitis)
S/E Can cause tendon damage, arthropath in children (avoid in
epilepsy, CNS and myasthenia gravis)
Glycopeptides
-
Vancomycin, teicoplanin (MRSA, MRSE, clostridium defficile,
endocarditis/surgical prophlaxis)
S/E Nephrotoxicity, ototoxicity, red man syndrome, allergic reactions
Mixed infections
-
Synergistic effects of antimicrobial combinations
o Lactam + Aminoglycosides
Multi therapy to minimise the development of drug resistance
o Tuberculosis treatment: Isoniazid, rifampicin, ethambutol and
pyrazinamide
31
Pharmacology Notes
Medical Rotation - 2015
32
Pharmacology Notes
Medical Rotation - 2015
COPD
Progressive Obstruction of the Airways with little to No reversibility.
Term inclusive of
-
Emphysema- enlarged air spaces distal to terminal bronchioles with
alveolar wall destruction. Loss of elasticity, Poor gas exchange.
Chronic Bronchitis- cough and sputum production 3/12 for 2
successive years.
Classic profile: >35yr smoker or exposed to air pollutants. Chronic
Dyspnoea and Sputum Production. Minimal diurnal variation.
Pink Puffer- alveolar ventilation, near normal PaO2 and low PaCO2,
breathless but not cyanosed, can progress to type 1 respiratory failure
Blue Bloater- alveolar ventilation with a low PaO2 and high PaCO2.
Cyanosed, not breathless, can develop cor pulmonale. Respiratory centre
not sensitive to CO2- dependent on hypoxic drive to maintain resp ***
caution should be taken with O2 therapy.
Common clinical presentations: Chronic Cough, Dyspnoea, SOBOE,
Sputum, Cyanosis of mucus membranes, Barrel chest (hyperinflation),
RR at rest, shallow breathing, pursed lips, use of accessory respiratory
muscles, tripod brace position.
Complications:
-
Acute exacerbations
Polycythaemia
Respiratory Failure
Cor Pulmonale w\ Oedema and JVP
Pneumothorax (ruptured bullae)
Lung Ca.
Principles of Mgmt - COPDX
Confirm Diagnosis
o FEV1: FVC ratio post bronchodilator <0.7, no reversibility with
bronchodilator.
Optimise Function
Prevent Deterioration
o Smoking cessation, influvax, pneumovax, O2 therapy,
mucolytics, ICS
Develop support network and self-mgmt
33
Pharmacology Notes
Medical Rotation - 2015
o Pulmonary rehabilitation, multidisciplinary care, enable
responsibly for self-management
Manage Exacerbations
o Inhaled bronchodilators, systemic corticosteroids
(prednisolone, side effects mood disorders, insomnia,
dysphagia, dyspepsia, long term - osteoporosis, DM), positive
pressure ventilation, treat infections (Amoxycilin, doxycycline)
, O2 therapy
Drug Therapy- rationale- Symptom relief, exercise tolerance, Prevent
or Tx exacerbations and complications
1. SABA Salbutamol, Terbutaline Anticholinergic Ipratropium
bromide
34
Pharmacology Notes
Medical Rotation - 2015
o Symptom relief and improved exercise function
o Choice dependent on patient preference, response and S/E
experienced.
2. LABA OR LAMA
LAMA; triotropium (reduce exacerbations and hospitalisations as
well as reductions in coughing wheezing and dyspnoea. Adverse
events antimuscarinic e.g. dry mouth, urinary retention, shouldnt
use with other muscarinics as increases adverse effects. Perhaps
o LABA; salmetarol, efermeterol - MDI (reduces exacerbations, no
increase in mortality used in combination in asthma but can be
used solitary in COPD, can cause tremors, palpitations
o Theophylline; oral, less effective than previous two
ICS for moderate/severe COPD with frequent exacerbations
o Long term systematic CS not recommended
o No known benefit, no difference in mortality with ICS vs LABA
o Only approved ICS fluticasone
o ICS less risk than systemic steroids but still dangerous
o
diabetes
o ICS LABA combs improve QOL and FEV1
Mucolytics
o Acetylcysteine - Improves cough, sputum and wellbeing
Notes:
Definition revisit
Type I Resp failure: hypoxia w\ normal or low PaCO2. V/Q mismatch
-
E.g. Pneumonia, Pulmonary Oedema, PE, Asthma, Emphysema,
Pulmonary Fibrosis, ARDS.
Type II Resp Failure: hypoxia w\ hypercapnia, caused by alveloar
hypoventilartion w\ or w\o V\Q mismatch.
-
E.g.
o Pulmonary Disease- COPD, pneumonia, obstructive sleep
apnoea, end-stage pulmonary fibrosis, Asthma.
o Reduced Respiratory Drive- sedative drugs, CNS tumour,
trauma
o Neuromuscular disease- cervical cord lesions, diaphragmatic
paralysis, myasthenia gravis, Guillain-Barre syndrome.
o Thoracic Wall disease- kyphoscoliosis.
Hypoxia- Dyspnoea, restlessness, agitation, confusiojn, central cyanosis
-
Long term- polycythaemia ( RBC), pulmonary hypertension, cor
pulmonale
Hypercapnia- Headache, peripheral vasodilation, tachycardia, bounding
pulse, asterixis, papilledema, confusion, drowsiness, death.
35
Pharmacology Notes
Medical Rotation - 2015
Dyslipidemia
Principles of Mgmt
1. Lifestyle Changes
2. Measure lipids 4-6 weeks during titration
Drug use progression of atherosclerosis, survival, MI/ CVA risk.
Prevent pancreatitis due to hypertriglyceridemia, premature
cardiovascular mortality.
1. In hypercholesterolemia
o Statins- LDL of 30-50%
o Bile-acid binding resins- LDL 15-25%
o Nicotinic acid poorly tolerates
o Ezetimibe- for patients who cant tolerate statins, v good
when combined w/ statin instead of incr dose of statin and
incr risk adverse s/e, new, no clinical evidence
o Fibrates- less for LDL- better for TG
2. In hypertriglyceridemia
o Fibrates Gemfibrozil, Fenofibrate- S/E : rhabdomyolysis,
potentiate anticoags (monitor warfarin, aspirin, clopidogrel)
o Nicotinic Acid
o Fish Oil decrease CVD risk and choles,- 1000mg capsules but
active ingredient is 300mg only (needs to be 1500mg),- no
evidence for lowered choles w/ only 300-600mg
Statins: HMG-CoA reductase inhibitors
Start therapy in everyone post cardiovascular event, independent of blood
levels, because of antiinflammatory and plaque stabilising effects.
-
Rosuvastatin- most potent, Cleared via kidney
Atorvastatin
Simvastatin- interactions, risk of muscle S/E
Fluvastatin (less interactions)
Pravastatin
Do not exceed 40mg
Take at night to Cholesterol synthesis
-
Indications
o dyslipidaemia,
o hypercholesterolemia
o post MI (high risk of CAD)
Side effects
o rhabdomyolysis,
o hepatotoxicity (monitor liver function), - 3x upper normal limit
o myopathy and myalgia
36
Pharmacology Notes
Medical Rotation - 2015
o association w\ NODM
Fibrates
-
Fenofibrate,
Gemfibrozil
Effective against TG
-
Increased risk of side effects when combined with statins (e.g.
rhabdomyolysis)
No heart disease improvement while statins do
Cleared renally- C/I AKI
Ezetimide
-
Decreases cholesterol absorption in small intestine, not a primary
agent, not much evidence
Cholestyramine
-
Bile acid sequesterant, preventing enterohepatic recycling,
increasing cholesterol output
Causes GI upset, flatulence, abdo pain, also need to spacing
Reduces LDL
Nicotinic acid
-
GPCR binding and up regulation inhibits lipolysis
Not widely used, GI upset, flushing
Effective against TGs
37
Pharmacology Notes
Medical Rotation - 2015
Diabetes Mellitus
Metabolic disorder characterised by chronic elevated blood glucose levels
w\ metabolism disturbances.
Type 1
-
Autoimmune destruction of pancreatic cells
Abrupt onset. Medical emergency.
Diagnostic marker- Anti GAD
Type 2 DM
-
Peripheral resistance to insulin
Inadequate secretory response by pancreatic cells.
Principles of Mgmt
Lifestyle Changes
Consider
-
Glucose
Lipids
Blood Pressure
Drug therapy-rationale Symptom control (Polydipsia, Polyuria), Control
of Blood Glucose Conc. Prevent and Treat complications (neuropathy,
nephropathy, and retinopathy), macrovascular events (early stable
control)
Generally, treatment targets are:
-
Fasting blood glucose, 48 mmol/L
Postprandial blood glucose, 610 mmol/L
Glycated haemoglobin concentration (HbA1c), 53 mmol/mol (7%).
Low-dose aspirin in patients with cardiovascular disease
ACE inhibitor (or, if intolerant, a sartan) to delay progression of renal
disease in patients with microalbuminuria or proteinuria (including
normotensive patients)
Oral Therapy
1. Metformin
o + Sulfonylurea (most common) OR
o DPP-4 inhibitor OR
o GLP-1 agonist
Can add Sulfonylurea plus one of other therapies above
or below (of the 4):
Acarbose OR
38
Pharmacology Notes
Medical Rotation - 2015
Thialidinediones
o Esp. when avoiding insulin therapy.
2. Basal Insulin
o w\ continued Metformin, w\o sulfonylurea
o Consider ceasing noninsulin therapy based on:
Risk of hypoglycaemia
Complexity of regimen
TGA combination recommendations.
3. Continue Metformin insulin therapy (by dose of regimen BB)
o Again consider ceasing non-insulin therapy based on above
criteria.
Biguanide- Metformin
-
Decreases hepatic glucose production and increases peripheral
utilisation of glucose
Reduces insulin requirements in obese patients and assists in
control of weight gain
Renally cleared
No risk of hypos as monotherapy
S/E Nausea, vomiting, anorexia, diarrhoea, may assist with weight
loss, lactic acidosis (anorexia, nausea vomiting, abdominal pain,
cramps, malaise and weight loss), also avoid contrast media
Secretalogogues
Sulfonylureas- Glipizide, Glicazide, Glimepiride, Glibenclamide
-
pancreatic insulin secretion
Glipizide and Gliclazide preferred in renal impairment- all require
dosage adjustment.
S/E hypoglycaemia, weight gain
Stopped w\ the commencement of Insulin therapy.
Glitazones/Thiazolidinediones- Piaglitazone, rosiglitazone
-
Reserve for patients unable to take other antidiabetics
ineffective in up to 30% of patients
insulin sensitivity in peripheral tissues.
hepatic glucose output
Assist sensitisation to insulin, effective in insulin resistance
S/E peripheral oedema (worsened by HF), CV events, increase bone
fractures, bladder cancer
Incretin therapies;
Appear to improve glycaemic control when combined with insulin
-
Incretin enhancer (DPP-4 inhibitors) Alogliptin, linagliptin,
saxagliptin, sitagliptin vildagliptin
39
Pharmacology Notes
Medical Rotation - 2015
o Increase concentration of GLP1 and GIP, resulting in glucose
dependant insulin secretion and glucagon suppression.
o No weight gain or hypos
Incretin mimimics (GLP1 agonists), Exenatide, liraglutide,
lixisenatide
S/E nausea, vomiting, can aid with weight loss
Acarbose- Alpha-Glycosidase Inhibitor, breakdown of complex CHO in
GIT, absorption
-
poorly tolerated due to GI effects
limited role
Insulin therapy endogenous insulin
-
greater risk of hypoglycaemia and weight gain than sulfonylureas
when generalised allergic reactions occur, switching to another
insulin or desensitisation may be necessary
local reactions often disappear spontaneously
SC injections are usually given in the abdomen (fastest rate of
absorption and onset of action)
Regimens:
-
Split-Mixed
Basal-Bolus
- SM
Two injections per day
- 2/3rd in morning
- 1/3rd in evening
Adv Simple and convenient w\
risk of hypos
D/Adv flexibility, cannot miss
meals.
BB
4 injections per day
- 3 short acting insulin before
meals
- 1 night time long acting
insulin
Adv: flexibility, better BSL control
D/Adv: more BSL requires, fails to
cover snacks, risk of hypos.
Insulin Types
-
Ultra-short acting Aspart (NovoRapid), Glulisine (Apidra), Lispro
(Humalog)
Short acting Actrapid
Long Acting- Glargine
Complications:
Acute complication: DKA w\ type 1 diabetes
Clinical Picture:
40
Pharmacology Notes
Medical Rotation - 2015
Acidemia (blood pH <7.3
Hyperglycaemia
Ketonaemia
Principles of Mgmt
Correct fluid loss
Correct hyperglycaemia and supress ketones
Correct electrolyte disturbances *** Potassium
Resolution of acid/base balance
Treat concurrent conditions
Drug therapy rationale
1. Fluid
2. BSLs
3. Potassium
Acute complication Hyperglycaemic Hyperosmolar state
-
Insidiously Develops (days to weeks) via
o hepatic glucose production
o peripheral glucose utilisation
Results in osmotic diuresis substantial fluid loss and
hyperosmolarity
Patient has dehydration/hypotension, tachycardia, tachypnoea
weakness and leg cramps, focal neurological symptoms and seizures.
Principle of Mgmt
circulatory volume and tissue perfusion
1L in 1hr first 2 hours, 2L in 4hr. Change to 5% dextrose when BLS
<15mmolL-1Gradual serum glucose and plasma osmolarity
Insulin infusion. Stop orals
Correct electrolyte imbalance
Treatment of precipitating cause
Infection (cellulitis, pneumonia, sepsis, UTI)
Coexisting disease (AMI, CVA, Cushings RF)
Drugs (Chemotherapeutic, glucocorticoids, diuretics, ethanol)
Prophylactic LMWH, consider full anticoagulation if serum osmolarity
exceeds 350mmolL-1
41
Pharmacology Notes
Medical Rotation - 2015
42
Pharmacology Notes
Medical Rotation - 2015
Drugs that increase blood glucose
43
Pharmacology Notes
Medical Rotation - 2015
For chronic complication of diabetes: remember KNIVES
Kidneys, Nerves, Infection, Vasculature, Eyes, Skin
Counselling
Drinking alcohol decreases your blood glucose. It can also mask warning
symptoms of hypoglycaemia (low blood glucose). Avoid binge drinking and
have something to eat when you drink alcohol.
Make sure that you, and your friends and family, know how to recognise
and treat hypoglycaemia; ask your doctor or diabetes educator if you are
unsure.
Insulin is injected under the skin (subcutaneous injection) usually in the
abdomen, or less commonly in the thigh, upper arm or buttock. Pinch the
skin to reduce the chance of injecting into a blood vessel. Rotate injection
sites in the same general area to prevent damage to the fat and tissues
under the skin (called lipodystrophy).
Use short-acting insulin 30 minutes before meals. Use ultra-short-acting
insulin immediately before or soon after meals when necessary.
44
Pharmacology Notes
Medical Rotation - 2015
Before using insulin, allow it to stand at room temperature for about 30
minutes (cold insulin may be more painful to inject).
Gently rotate vials and cartridges of cloudy insulin in hands before use to
ensure it is evenly mixed (it should look white and uniformly cloudy).
When mixing insulins, draw up short-acting insulin into the syringe first to
avoid contaminating the vial with long-acting insulin. Do not mix insulin
glargine with other insulins.
45
Pharmacology Notes
Medical Rotation - 2015
NOTES
___________________________
46
Pharmacology Notes
Medical Rotation - 2015
NOTES
___________________________
47
Pharmacology Notes
Medical Rotation - 2015
NOTES
___________________________
48
Pharmacology Notes
Medical Rotation - 2015
NOTES
___________________________
49
Pharmacology Notes
Medical Rotation - 2015
50
You might also like
- Congestive Heart Failure ReportDocument6 pagesCongestive Heart Failure ReportSunshine_Bacla_4275100% (1)
- HYPERTENSIONDocument5 pagesHYPERTENSIONRajesh RamanNo ratings yet
- 10-11 Treatment of HypertensionDocument11 pages10-11 Treatment of HypertensionHanif GandohNo ratings yet
- Congestive Heart Failure: CardiacDocument36 pagesCongestive Heart Failure: CardiacHUZAIFA YAMAANNo ratings yet
- Antihypertensive Pharmacologic Agents: Nr33 K Burger, Msed, MSN, RN, CneDocument28 pagesAntihypertensive Pharmacologic Agents: Nr33 K Burger, Msed, MSN, RN, CneLopez JoeNo ratings yet
- Pedal EdemaDocument45 pagesPedal Edemafirdaushassan2112No ratings yet
- Anti Arrhythmic DrugsDocument91 pagesAnti Arrhythmic DrugsAlex beharuNo ratings yet
- Pharmacology Cardiovascular DrugsDocument120 pagesPharmacology Cardiovascular DrugsDareRaymond100% (1)
- Cardiotronic MedicationsDocument13 pagesCardiotronic MedicationsTee WoodNo ratings yet
- Treating Heart Failure: Current Guidelines for Pharmacological ManagementDocument11 pagesTreating Heart Failure: Current Guidelines for Pharmacological ManagementKareem SaeedNo ratings yet
- Pharmacotherapy of Congestive Heart Failure (CHF)Document163 pagesPharmacotherapy of Congestive Heart Failure (CHF)Aditya rathoreNo ratings yet
- Cad CommerDocument2 pagesCad CommerWhatDoYouSeriesNo ratings yet
- Cardiovascular Agent: Prof. Clement Belvis RN, RM, MPHDocument86 pagesCardiovascular Agent: Prof. Clement Belvis RN, RM, MPHEimhie Lee CasiNo ratings yet
- Drug Presentation On Anti-Hypertensive: All India Institute of Medical and Science New Delhi 2021-2022Document12 pagesDrug Presentation On Anti-Hypertensive: All India Institute of Medical and Science New Delhi 2021-2022Priya SinghNo ratings yet
- Drugs For Congestive Heart FailureDocument46 pagesDrugs For Congestive Heart Failuresultan khabeeb100% (1)
- Cardio Lab MedsDocument11 pagesCardio Lab MedsDianne Erika MeguinesNo ratings yet
- Management of Heart Failure: OutlineDocument27 pagesManagement of Heart Failure: OutlineBoetik AlifiaNo ratings yet
- CHF Drugs Guide: Key Medications for Treating Congestive Heart FailureDocument21 pagesCHF Drugs Guide: Key Medications for Treating Congestive Heart Failuremohsen mirdamadiNo ratings yet
- Antihypertensive & Antianginal DrugsDocument5 pagesAntihypertensive & Antianginal Drugsdomememe1No ratings yet
- Drugs for Hypertension 2023 (1)Document19 pagesDrugs for Hypertension 2023 (1)aguilarjanicaNo ratings yet
- Pharmacology Chapter 42 zp-1-3Document42 pagesPharmacology Chapter 42 zp-1-3sho bartNo ratings yet
- 1 Antihypertensive DrugsDocument14 pages1 Antihypertensive DrugsReda SoNo ratings yet
- Cardiac Drugs PowerpointDocument17 pagesCardiac Drugs PowerpointsiratelNo ratings yet
- Congestive Cardiac Failure (1)Document27 pagesCongestive Cardiac Failure (1)Krupasagar Pn PalegarNo ratings yet
- ACE Inhibitors: Medications To Control Blood PressureDocument3 pagesACE Inhibitors: Medications To Control Blood PressurekNo ratings yet
- Pharmacology: Unit VIIIDocument92 pagesPharmacology: Unit VIIIChristian Laraya AlayonNo ratings yet
- Hypertension: 1-Hypertension Is Defined As (BP)Document37 pagesHypertension: 1-Hypertension Is Defined As (BP)hussein alnasryNo ratings yet
- Drug StudyDocument28 pagesDrug StudyJheryck SabadaoNo ratings yet
- CARDIAC-MEDICATION-LECTUREDocument23 pagesCARDIAC-MEDICATION-LECTUREilikeedsheeranNo ratings yet
- Cardiac Drugs PowerpointDocument17 pagesCardiac Drugs PowerpointNoci M. FrenkNo ratings yet
- Merged 1 PDFDocument305 pagesMerged 1 PDFAhmed KurdiNo ratings yet
- Update: Review and Update On Inotropes and VasopressorsDocument9 pagesUpdate: Review and Update On Inotropes and VasopressorsMaryam JamilahNo ratings yet
- Antihypertensive DrugsDocument52 pagesAntihypertensive Drugsapi-224264169No ratings yet
- Drugs Used in HF IIDocument40 pagesDrugs Used in HF IIJamal LudinNo ratings yet
- CHF Simulation PreparationDocument5 pagesCHF Simulation Preparation5Dragoon5No ratings yet
- Heart Failure New SlidesDocument41 pagesHeart Failure New SlidesjawadNo ratings yet
- 11A Drugs Acting On The Cardiovascular SystemDocument85 pages11A Drugs Acting On The Cardiovascular SystemJaps De la CruzNo ratings yet
- 5 HypertensionDocument8 pages5 Hypertensioniraqeana100100No ratings yet
- Hypertension (HTN or HT), Also Known As High Blood Pressure (HBP), Is ADocument4 pagesHypertension (HTN or HT), Also Known As High Blood Pressure (HBP), Is AReynaKatNo ratings yet
- Cardiovascular Drugs and Blood Pressure RegulationDocument4 pagesCardiovascular Drugs and Blood Pressure RegulationReynaKatNo ratings yet
- Acute Heart FailureDocument18 pagesAcute Heart FailureGeorge GeorgeNo ratings yet
- Anti-Arrhythmic Agents For Pharmacy PDFDocument41 pagesAnti-Arrhythmic Agents For Pharmacy PDFKelvinTMaikanaNo ratings yet
- Cardiac Drugs HypertensionDocument5 pagesCardiac Drugs HypertensionEciOwnsMeNo ratings yet
- HypertensionDocument10 pagesHypertensionaa zzNo ratings yet
- Clinical Pharmacy 2023-2024 Lectures - 2Document104 pagesClinical Pharmacy 2023-2024 Lectures - 2ameerjawad150No ratings yet
- Lecture 1 antihypertensionSDSDocument7 pagesLecture 1 antihypertensionSDSSara AbbasNo ratings yet
- Cardiovascular Agents: Florianne E. Adlawan, R.NDocument31 pagesCardiovascular Agents: Florianne E. Adlawan, R.NadlawanflorianneNo ratings yet
- Lec 2 Heart Failure, Angina and Arryth2Document19 pagesLec 2 Heart Failure, Angina and Arryth2Adel AlomarNo ratings yet
- Cardiotonic DrugsDocument67 pagesCardiotonic DrugsLady Mae Ramos100% (1)
- Antianginal Drugs: Roger Joseph Ii R. Jecino, M.DDocument31 pagesAntianginal Drugs: Roger Joseph Ii R. Jecino, M.DFranz Earl Niño AlbesaNo ratings yet
- Heart Failure Drug Treatment GuideDocument45 pagesHeart Failure Drug Treatment GuideJoshua ObrienNo ratings yet
- Cardiovascular SystemDocument4 pagesCardiovascular SystemRegineCuasSulibNo ratings yet
- Cardiac Medications: Mildred YarboroughDocument51 pagesCardiac Medications: Mildred YarboroughQueennitaNo ratings yet
- Heart FailureDocument30 pagesHeart FailureYopih YohanesNo ratings yet
- DBP: Diastolic Blood Pressure SBP: Systolic Blood PressureDocument7 pagesDBP: Diastolic Blood Pressure SBP: Systolic Blood PressureM. JoyceNo ratings yet
- Cardiovascular Endocrinology and Metabolism: Theory and Practice of Cardiometabolic MedicineFrom EverandCardiovascular Endocrinology and Metabolism: Theory and Practice of Cardiometabolic MedicineAndrew J. KrentzNo ratings yet
- Hepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Eating Disorder Admission GuideDocument14 pagesEating Disorder Admission GuideJeremy Yang100% (1)
- Beethoven Pathetique Sonata AnalysisDocument3 pagesBeethoven Pathetique Sonata AnalysisJeremy YangNo ratings yet
- OSCE Shoulder ExaminationDocument6 pagesOSCE Shoulder ExaminationJeremy YangNo ratings yet
- Atrial Fibrillation Management PDFDocument3 pagesAtrial Fibrillation Management PDFJeremy YangNo ratings yet
- OSCE Station 1 Diabetic LL ExamDocument5 pagesOSCE Station 1 Diabetic LL ExamJeremy YangNo ratings yet
- Atrial Fibrillation Management PDFDocument3 pagesAtrial Fibrillation Management PDFJeremy YangNo ratings yet
- Scale Practice TableDocument1 pageScale Practice TableJeremy YangNo ratings yet
- Iacta 2011 Janak Mehta Award Winning PresentationDocument56 pagesIacta 2011 Janak Mehta Award Winning PresentationDr.Sandeep Kumar KarNo ratings yet
- Almostadoctor - co.Uk-Summary of ECG AbnormalitiesDocument8 pagesAlmostadoctor - co.Uk-Summary of ECG AbnormalitiesAnu SharmaNo ratings yet
- Simultaneous Atrial and Ventricular Pacing During Narrow Complex Tachycardia - The Janus Response. Which One Is True?Document5 pagesSimultaneous Atrial and Ventricular Pacing During Narrow Complex Tachycardia - The Janus Response. Which One Is True?Sahil HasanNo ratings yet
- ECG in Emergency Room, HowDocument43 pagesECG in Emergency Room, HowFabian Fabiansyah100% (1)
- ALTERATION/ ABNORMAL FINDINGS IN PULSEDocument7 pagesALTERATION/ ABNORMAL FINDINGS IN PULSEShalabh JoharyNo ratings yet
- ECG Rhythm InterpretationDocument21 pagesECG Rhythm Interpretationvanstar7100% (1)
- Rhythm Description Schematic Diagram Egc Characteristics Sample TraceDocument6 pagesRhythm Description Schematic Diagram Egc Characteristics Sample TraceJhenne Kyle Ko Dee100% (1)
- ArrhythmiasDocument29 pagesArrhythmiasVijay GadagiNo ratings yet
- Paroxysmal Supraventricular Tachycardia: Pathophysiology, Diagnosis, and ManagementDocument8 pagesParoxysmal Supraventricular Tachycardia: Pathophysiology, Diagnosis, and ManagementLaurensia Sherly SusiloNo ratings yet
- Ecg For AnkiDocument3 pagesEcg For AnkijNo ratings yet
- Emp SyncopeDocument20 pagesEmp SyncopeWilmer JimenezNo ratings yet
- Nurs 603 Assignment 1 Objective Tests Design and Considerations Final For SubmissionDocument13 pagesNurs 603 Assignment 1 Objective Tests Design and Considerations Final For Submissionapi-323169345No ratings yet
- Basic EKG RefresherDocument210 pagesBasic EKG RefresherAaron D. Phoenix100% (6)
- Ventricular Arrhythmias EP Overview MedtronicDocument44 pagesVentricular Arrhythmias EP Overview Medtronicinu_upNo ratings yet
- Important Causes of Sudden Cardiac DeathDocument2 pagesImportant Causes of Sudden Cardiac DeathTausif AbbasNo ratings yet
- KKH Baby Bear Book 2010 2nd EditionDocument305 pagesKKH Baby Bear Book 2010 2nd EditionErnest Ho100% (4)
- Drug StudyDocument9 pagesDrug StudyChristine PunsalanNo ratings yet
- A. Bayés de Luna (Auth.) Textbook of Clinical EDocument520 pagesA. Bayés de Luna (Auth.) Textbook of Clinical ETAUFAN RACHIMNo ratings yet
- Intepretasi EKG (DR Eka)Document93 pagesIntepretasi EKG (DR Eka)Danil Anugrah JayaNo ratings yet
- Chapter 12Document28 pagesChapter 12Muhammad AmirNo ratings yet
- From: Rapid Interpretation of EKG'sDocument14 pagesFrom: Rapid Interpretation of EKG'sLucija Kljaić100% (1)
- Clinical Indication Def.Document11 pagesClinical Indication Def.Anish H DaveNo ratings yet
- Medicine in The Pagan Arab StatesDocument134 pagesMedicine in The Pagan Arab StatesQurratu QolbiNo ratings yet
- ACLS Tachycardia Algorithm For Managing Stable TachycardiaDocument4 pagesACLS Tachycardia Algorithm For Managing Stable TachycardiaizkalotlNo ratings yet
- Heart Block PPT by SibaDocument36 pagesHeart Block PPT by Sibaritumitu_ritumitu100% (1)
- ECG With DR Samson-1.Document10 pagesECG With DR Samson-1.Ebuwa AmadasunNo ratings yet
- AbbreviationDocument35 pagesAbbreviationroxy0709No ratings yet
- WPW SyndromeDocument6 pagesWPW SyndromeAlvin Wijaya RustamNo ratings yet
- A Simplified ECG GuideDocument4 pagesA Simplified ECG Guidejalan_z96% (25)
- Supraventricular Tachycardia - Life in The Fast Lane ECG LibraryDocument29 pagesSupraventricular Tachycardia - Life in The Fast Lane ECG LibraryYehuda Agus SantosoNo ratings yet