Professional Documents
Culture Documents
Bullshit
Uploaded by
Umar FarooqOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bullshit
Uploaded by
Umar FarooqCopyright:
Available Formats
British Journal of Urology (1998), 81, 253256
Transversely tubularized ileal segments for the MitrofanoV
or Malone antegrade colonic enema procedures:
the Monti principle
I.D . SUGARMAN, P .S. MALONE, T .R. T ERRY* and M. A. KOYLE
Department of Paediatric Urology, Wessex Department of Paediatric Surgery, Southampton General Hospital, *Department of
Urology, Leicester General Hospital, UK and Department of Pediatric Urology, The Childrens Hospital, Denver, Colorado, USA
Objective To assess the use of a transverse tubularized
segment(s) of ileum in the MitrofanoC or Malone
antegrade colonic enema (MACE) procedures.
Patients and methods Eleven patients in three centres
underwent the formation of a continent conduit to
bowel (MACE, eight patients) and/or bladder
(MitrofanoC, four) using either a single segment of
transverse tubularized ileum (10 patients) or two
segments of ileum anastomosed and tubularized into
a single conduit (two).
Introduction
The treatment of urinary and faecal incontinence has
improved dramatically over the last two decades, after
the introduction of the MitrofanoC principle and the
Malone antegrade colonic enema (MACE) procedure,
respectively [1,2]. For both of these procedures, the
appendix is the favoured catheterizable conduit but
problems arise when the appendix is absent or both
procedures are performed simultaneously [3]. Therefore,
diCerent conduits have been devised using tapered ileum,
caecal flaps, tubularized colon, gastric tubes, ureter,
fallopian tube, detrusor muscle, prepuce and button
devices [411].
Recently, Monti et al. described an experimental technique of transversely tubularizing a short segment of
ileum, converting a 2 cm segment into a 7 cm tube
which could then be reimplanted following the
MitrofanoC principle [12]. It was also shown that two
segments could be anastomosed to create a 14 cm tube.
We have adapted this technique to clinical practice and
present the preliminary results.
Patients and methods
Eleven patients (450 years old) in three centres underwent the formation of a transverse ileal tube conduit.
Accepted for publication 15 October 1997
1998 British Journal of Urology
Results Within a follow-up of 8 weeks to 6 months, all
conduits were continent and catheterized easily. One
stomal stenosis required a revision procedure.
Conclusion This method for forming a continent catheterizing conduit, based on the MitrofanoC principle,
appears to be eCective and is recommended in cases
where the appendix cannot be used or where a second
conduit is required.
Keywords Incontinence, conduit, MitrofanoC principle
Nine had spina bifida and two had high anorectal
malformations. The conduit was used for the MACE
procedure in eight and MitrofanoC in four (patient no. 10
had a Monti conduit for both bowel and bladder). Seven
patients had a combined MACE and bladder reconstruction with a MitrofanoC, three had an isolated MACE and
one an isolated MitrofanoC. In nine patients a singlesegment tube was constructed and in two a composite
tube, using two segments of ileum; their details are
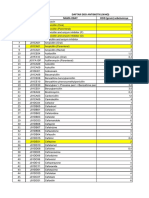
shown in Table 1.
Technique
One or two ileal segments 2 cm long are isolated (Fig. 1).
The ileum is divided longitudinally either on the antimesenteric border or eccentric to it, to produce a 7 cm ileal
flap from each segment, with the valvulae conniventes
now running in the longitudinal axis (Fig. 2). The bowel
is then tubularized over a 12 F catheter producing ends
free of mesentery to facilitate the creation of an antireflux
tunnel, and an exit through the abdominal wall (Fig. 3).
When two segments are used they are anastomosed at
their mesenteric ends to produce a 14 cm conduit
(Fig. 4). For those patients undergoing a MACE procedure, the conduit is implanted into a 45 cm submucosal tunnel along a taenia. For the MitrofanoC, a standard
submucosal tunnel into the bladder was used. All conduits were brought out onto the abdominal wall, incorporating either a V skin flap or multiple flaps (VZQ) [13].
253
32
14
SB
SB
SB
SB
HAR
SB
SB
SB
HAR
SB
SB
Diagnosis
6 months
5 months
4 months
8 weeks
6 months
6 months
6 months
6 months
6 months
6 months
8 weeks
Follow-up
S
S
MACE caecum
MitrofanoC
bladder
Single/double
ileal segment
MitrofanoC
bladder +
MitrofanoC
bladder
MACE
caecum
MitrofanoC
bladder
MACE
A colon
MACE
A colon
MACE
A colon
MACE
T colon
MACE
A colon
MACE
T colon
Conduit
Appendix MACE
Ileocystoplasty
Pippe-Salle UL
Appendix MACE
Ileocystoplasty
Pippe-Salle UL
Ileocystoplasty
None
Appendix MitrofanoC
Pippe-Salle UL
Appendix MitrofanoC
Ileocystoplasty
Pippe-Salle UL
None
Bladder neck closure
Ileocystoplasty
Appendix MitrofanoC
None
Bladder neck closure
Colocystoplasty
Appendix MitrofanoC
None
Other procedure
at same operation
Umbilical
MitrofanoC stoma
revised
MACE stoma Easy
Easy
Easy
Easy
Easy
Easy
Easy
Easy
Minimal ACE
stomal stenosis
Minimal ACE
stomal stenosis
Easy
Catheterization
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Continent
SB, spina bifida. HAR, high anorectal malformation. T, transverse. A, ascending. D, double. S, single. UL, urethral lengthening. F-C, faecally clean. U-D, urinary-dry.
50
11
11
11
17
10
15
Age
(years)
Patient
Table 1 Patients details, procedure, complications, follow-up and outcome
UD
FC
FC
UD
UD
FC
FC
UD
UD
FC
UD
FC
UD
FC
FC
UD
FC
FC
Outcome
254
I. D. SU GAR MAN et al.
1998 British Journal of Urology 81, 253256
C ONTINENT C AT HETER IZI NG CONDUI T B ASED ON T HE M ITR OFANOF F PRINC IPLE
1a
255
1b
Fig. 1. a. A single 2 cm ileal segment and b, two 2 cm ileal segments.
Fig. 2. Detubularized ileal segment 7 cm long; note the longitudinal
axis of the valvulae conniventes.
Fig. 4. A double-segment 14 cm conduit.
did so easily; the remaining two had slight diBculty in
catheterizing their ACEs, but neither catheterized the
stoma on the other days, as advised. They have since
done so and their diBculty resolved. Of the four patients
with a MitrofanoC, all are dry and have normal upper
tracts on ultrasonography. Three catheterized easily and
one patient underwent a revision procedure for an
umbilical stomal stenosis.
Discussion
Fig. 3. Seven centimetre tubularized conduit; note the free ends.
Results
The follow-up ranged from 8 weeks to 6 months
(Table 1). Six of the eight patients with the MACE
catheterized daily and two on alternate days; all the
conduits were continent. The six who catheterized daily
1998 British Journal of Urology 81, 253256
The MitrofanoC and MACE procedures have proved to
be useful for patients with urinary and faecal incontinence to become both dry and clean. If the appendix is
not available or, as is often the case, more than one
catheterizable stoma is necessary, another conduit is
required. In a few patients it is possible to split the
appendix to form the two conduits and results with this
are encouraging. Koyle et al. reported 14 patients in
whom this procedure was performed, with complete
success and minimal problems [14].
Longitudinal tubularized ileal conduits have been
256
I. D. SU GAR MAN et al.
described but revision rates of up to 30% have been
reported [4,7]. Most problems relate to catheterizing the
channel, as it will be at right-angles to the valvulae
conniventes. Tubularized caecal or colonic flaps fare little
better [10]. Gastric tube conduits are well described but
the problems of skin excoriation, with the possible
requirement for long-term H2-antagonist medication,
make this procedure less attractive [8,15].
Non-gastro-intestinal conduits are also fully described;
Woodhouse and MacNeily reviewed their experience
with ureter, fallopian tube and detrusor flaps [5].
Although the continence rate was 83% in these patients,
the revision rate was >40%, compared with 24% when
the appendix was used. For the ureter to be used
transuretero-ureterostomy is necessary, with its possible
complications [16]. Duckett and Lofti found that ureteric
conduits caused more discomfort than other conduits
and recommended that they were not used [6]. For a
detrusor tube, the bladder needs to have a high capacity
and be thin-walled, and the fallopian tube conduit
required revision in all three cases described by
Woodhouse and MacNeily [5]. The use of the prepuce
for continent vesicostomy was described by Krstic [9]
and in a subsequent study of eight patients, complete
success was reported [17]. However, if the patient is
female or a circumcised male, this conduit is unavailable.
Another restriction with this technique is that the position of the stoma is restricted to the lower abdomen.
Because of these problems, there is an obvious need
for a better conduit to replace the appendix when it is
absent or used for another channel. Although the followup of the present patients is short, the Monti principle
may well prove to be the ideal alternative to the appendix. It is created easily using a short segment of an
abundant tissue, producing a good calibre tube with
minimal loss of bowel length, and it configures the
valvulae conniventes in the longitudinal axis of the
conduit, facilitating easier catheterization. It can be
extended to 14 cm long, rendering the technique possible
even in very obese patients. The ends of the conduit are
free of mesentery, facilitating the creation of an antireflux
tunnel and the exit through the abdominal wall. As the
conduit is on a mobile mesentery, there is no restriction
on siting the abdominal wall stoma.
6
7
9
10
11
12
13
14
15
16
17
and the antegrade continence enema procedure. Br J Urol
1995; 75: 3869
Squire R, Keily EM, Carr B, Ransley PG, DuCy PG. The
clinical application of the Malone Antegrade Colonic
Enema. J Pediatr Surg 1993; 28: 10125
Woodhouse CRJ, MacNeily AE. The MitrofanoC principle:
expanding upon a versatile technique. Br J Urol 1994;
74: 44753
Duckett JW, Lotfi AH. Appendicovesicostomy (and variations) in bladder reconstruction. J Urol 1993; 149: 5679
Figueroa TE, Sabogal L, Helal M, Lockhart JL. The tapered
and reimplanted small bowel as a variation of the MitrofanoC
procedure: preliminary results. J Urol 1994; 152: 735
Gosalbez R, Padron OF, Singla AK et al. The gastric
augment single pedicle tube catheterizable stoma: a useful
adjunct to reconstruction of the urinary tract. J Urol 1994;
152: 20057
Krstic ZD. Preputial continent vesicostomy: Preliminary
report of a new technique. J Urol 1995; 154: 11601
Keily EM, Ade-Ajayi N, Wheeler RA. Caecal flap conduit
for antegrade continence enema. Br J Surg 1994; 81: 1215
Fukunga K, Kimura K, Lawrence JP, Soper RT, Phearman
LA. Button device for antegrade enema in the treatment of
incontinence and constipation. J Pediatr Surg 1996; 31:
10389
Monti PR, Lara RC, Dutra MA, Rezende de Carvalho J. New
techniques for construction of eCerent conduits based on
the MitrofanoC principle. Urology 1997; 49: 1125
Kajbafzadeh AM, DuCy PG, Carr D, Ransley PG. One
hundred MitrofanoC stomas reviewed: A comparison of
techniques. British Association of Urological Surgeons
Annual Meeting. 2022 June 1995 Brighton. A119
Koyle MA, Waxman SW, Duque M et al. Applications and
modifications of the Malone antegrade continence enema
(MACE) with coincidental urinary tract reconstruction
the dual role of the appendix. European Surgeons of
Paediatric Urology 8th Annual Meeting. 35 April 1997
Rome. A069: 24
Birhle R, Klee LW, Adams MC, Foster RS. Early clinical
experience with the transverse colon-gastric tube continent
urinary reservoir. J Urol 1991; 146: 7513
Hendren WH, Hensle TW, Transureteroureterostomy.
Experience with 75 cases. J Urol 1980; 123: 82633
Krstic ZD. Preputial continent vesicostomy. A new technique. Our two and a half year experience. European
Surgeons of Paediatric Urology 8th Annual Meeting.
35 April 1997 Rome. A067: 23
Authors
References
1 MitrofanoC P. Cystostomie continente trans-appendiculare
dans le traitment des vessies neurologiques. Chir Pediatr
1980; 21: 297305
2 Malone PS, Ransley PG, Keily EM. Preliminary report: the
antegrade continence enema. Lancet 1990; 336: 12178
3 Roberts JP, Moon S, Malone PS. Treatment of neuropathic
urinary and faecal incontinence with synchronous bladder
I.D. Sugarman, FRCS(Ed), Specialist Registrar in Paediatric
Surgery.
P.S. Malone, MCh, FRCS(I), Consultant Paediatric Urologist.
T.R. Terry, MS, FRCS, Consultant Urologist.
M.A. Koyle MD, FAAP, FACS, Consultant Paediatric Urologist.
Correspondence: Mr P.S. Malone, Department of Paediatric
Urology, Wessex Department of Paediatric Surgery,
Southampton General Hospital, Tremona Road, Southampton
SO16 6YD, UK.
1998 British Journal of Urology 81, 253256
You might also like
- PAKISTAN CUSTOMS TARIFF 2014-15Document348 pagesPAKISTAN CUSTOMS TARIFF 2014-15AliChana1No ratings yet
- 2167190Document20 pages2167190Umar FarooqNo ratings yet
- Force 30 Valleylab ManualDocument16 pagesForce 30 Valleylab ManualUmar FarooqNo ratings yet
- A Systematic Review of Graft Augmentation Urethroplasty Techniques For The Treatment of Anterior Urethral StricturesDocument18 pagesA Systematic Review of Graft Augmentation Urethroplasty Techniques For The Treatment of Anterior Urethral StricturesUmar FarooqNo ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- AmputationsDocument30 pagesAmputationsUmar FarooqNo ratings yet
- Apr 02 14Document59 pagesApr 02 14Umar FarooqNo ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Intramuscular CKLDocument2 pagesIntramuscular CKLapi-310181843No ratings yet
- Bio OssDocument4 pagesBio OssVizi AdrianNo ratings yet
- SinusitisDocument12 pagesSinusitis05-NH-HU-KEVIN JULIO HUAYLLANE SOLISNo ratings yet
- DescargaDocument173 pagesDescargaAlexander León PuelloNo ratings yet
- Solvalitt Aluminium - MSDSDocument11 pagesSolvalitt Aluminium - MSDSLITOGENT 893No ratings yet
- 2010 STEPS Report BangladeshDocument176 pages2010 STEPS Report Bangladeshfatehatun noorNo ratings yet
- ACWA MBR presents Submerged Membrane Bioreactors using the Kubota MembraneDocument48 pagesACWA MBR presents Submerged Membrane Bioreactors using the Kubota Membranecharles samsonNo ratings yet
- Prostho IV-Slides 2 - Assessment of The Edentulous PatientDocument60 pagesProstho IV-Slides 2 - Assessment of The Edentulous Patientبراءة أحمد السلاماتNo ratings yet
- Clean The Pressure Sore by Irrigating The WoundDocument3 pagesClean The Pressure Sore by Irrigating The WounddeardestinyNo ratings yet
- NarrativeDocument10 pagesNarrativesaikrish36No ratings yet
- Stugeron® TabletsDocument3 pagesStugeron® TabletsmahgadNo ratings yet
- Social and Emotional Well Being Framework 2004-2009Document79 pagesSocial and Emotional Well Being Framework 2004-2009MikeJacksonNo ratings yet
- Acellular MatricesDocument16 pagesAcellular MatricesElo MediavillaNo ratings yet
- Ganga Action PlanDocument18 pagesGanga Action PlanAjithEdathootNo ratings yet
- Chad ScoreDocument5 pagesChad ScoreakochaNo ratings yet
- Burn WoundDocument68 pagesBurn WoundjrefkyNo ratings yet
- Acetabular Labral Tears and Hip Scope Rehab Webinar HandoutDocument20 pagesAcetabular Labral Tears and Hip Scope Rehab Webinar Handoutgemichan26No ratings yet
- Sodium Valproate Uses, DosageDocument2 pagesSodium Valproate Uses, DosageKhairul KhairulNo ratings yet
- 3 2.Msds Shell GTL Sarawax Sx50v1915072016gbDocument18 pages3 2.Msds Shell GTL Sarawax Sx50v1915072016gbArturo BLANCAS MARTINEZNo ratings yet
- Amen ADD QuestionnaireDocument3 pagesAmen ADD QuestionnaireReeshabhdev GauttamNo ratings yet
- DAFTAR ATC DDD ANTIBIOTIK WHO 2018 AbcDocument12 pagesDAFTAR ATC DDD ANTIBIOTIK WHO 2018 AbcMahezha DhewaNo ratings yet
- Listening and Reading Comprehension TestDocument12 pagesListening and Reading Comprehension TestPrimaIstianaNo ratings yet
- Brochure Rev04Document2 pagesBrochure Rev04nickj702No ratings yet
- PsychoanalysisDocument30 pagesPsychoanalysisjaydokNo ratings yet
- Drugs For Epilepsy: Subgroup 6Document31 pagesDrugs For Epilepsy: Subgroup 6Kwadwo Sarpong JnrNo ratings yet
- Case Presentation Ji Castante, Leah SDocument17 pagesCase Presentation Ji Castante, Leah SLeah CastanteNo ratings yet
- Effectiveness of Micronutrients and Physiotherapy in The Management of Oral Submucous Fibrosis PDFDocument5 pagesEffectiveness of Micronutrients and Physiotherapy in The Management of Oral Submucous Fibrosis PDFNia LieantoNo ratings yet
- ANSI/ASHRAE/ASHE Standard 170-2008 Tables for Filter Efficiencies and Design ParametersDocument4 pagesANSI/ASHRAE/ASHE Standard 170-2008 Tables for Filter Efficiencies and Design ParametersPradeep SukumaranNo ratings yet
- Cholestasis: Dr. Darmadi SPPD, FinasimDocument20 pagesCholestasis: Dr. Darmadi SPPD, FinasimTiens MonisaNo ratings yet
- Reflective QuestionsDocument2 pagesReflective Questionsayne joulceNo ratings yet