Professional Documents
Culture Documents
21 - Thyroid Function Tests
Uploaded by
hamadadodo7Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
21 - Thyroid Function Tests
Uploaded by
hamadadodo7Copyright:
Available Formats
21 Thyroid Function Tests
Management of thyroid disorders based on:
Accurate diagnosis
History
o
o
PE
o
Signs and symptoms
Accurate interpretation of laboratory results
Primary Hypothyroidism
Most frequently caused by chronic autoimmune
thyroiditis (Hashimotos thyroiditis)
Affects elderly and women over 40 years
Other causes
Thyroidectomy
131
Radioactive iodine ( I) therapy
Anti-thyroid agents
Head and neck irradiation
Medications
Congenital defects
Subclinical hypothyroidism (mild thyroid failure)
May be asymptomatic
Non-specific symptoms
Depression
o
o
Cognitive dysfunction
o
Weight gain
o
Fatigue
Alterations in lipid metabolism
o
o
Abnormalities in cardiac, GI, or
reproductive dysfunction
Diagnostics
American Thyroid Association recommends
thyroid stimulating hormone (TSH)
determination at 35 years and every 5 years
thereafter
TSH + FT4 = Primary hypothyroidism
(TSH 0.45 4.12 mlu/L)
TSH + (N) FT4 = Subclinical hypothyroidism +
TPOab (Thyroperoxidase Ab)
(N) TSH + FT4 = Secondary hypothyroidism or a
hypothalamic pituitary disorder
(N) or TSH + FT4 = TSH-secreting pituitary tumor or
thyroid hormone resistance
Symptomatology
History of autoimmune disease
History of Graves disease treatment/ thyroid
surgery
Family history of thyroid disease
History of heat/ neck irradiation
Depression/dementia/lithium treatment
Increased cholesterol
Increased CPK
Increased Na > 130 mg/L
Infertility/irregular menses
Cardiomegaly/ bradycardia/ low voltage ECG/
pericardial effusion
Alopecia/ coarse or thinning hair/ vitiligo
Cold intolerance/ fatigue/ hoarse voice
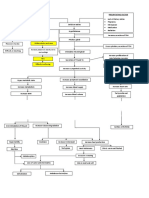
Suspect hypothyroidism
Measures TSH
TSH
> 4.12 mlu/L
TSH = 0.45 4.12 mlu/L
TSH
< 0.45 mlu/L
Patient
euthyroid
Measure FT4
Refer to
hyperthyroidism
algorithm
FT4
TSH-secreting pituitary tumor or thyroid
hormone resistance
(N) FT4
Test TPOab
Patient hypothyroid
FT4
Patient hypothyroid
Management
Thyroid hormone replacement therapy:
Levothyroxine sodium (1.6 ug/kg/d)
Goal of therapy:
o
Restore patient to euthyroid state
o
(N) TSH
Overdosage causes:
o
Decreased bone density
Accelerated bone turnover
o
o
Alterations in liver enzymes,
tachycardia and CV changes
Replacement therapy: lifetime
Hyperthyroidism
Thyrotoxicosis: excess thyroid hormone
o
Toxic diffuse goiter (Graves disease)
o
Toxic multinodular goiter
o
Toxic adenoma
o
Thyroiditis (painful, subacute, or silent)
Associated with:
o
Excessive pituitary TSH production
o
Trophoblastic tumor
o
Excessive ingestion of iodine or thyroid
hormone
Diagnosis
TSH + FT4
TSH + (N) FT4 + (N) FT3
TSH + FT3 + (N) FT4
TSH + FT4
=
=
=
=
Hyperthyroidism
Subclinical hyperthyroidism
T3 toxicosis
TSH secreting pituitary tumor
of familial thyroid hormone
resistance
TSH + (N) FT4 + FT3 = Euthyroid sick syndrome
rainwater@mymelody.com || 1st semester, AY 2011-2012
Goiter
Suspect hypothyroidism
Measures TSH
TSH
> 4.12 mlu/L
Hypothyroid
algorithm
TSH =
0.45 - 4.12 mlu/L
TSH
< 0.45 mlu/L
Patient
euthyroid
Measure FT4
FT4
Hyperthyroid
(N) FT4
Investigate pituitary disease
FT4
Subclinical hyperthyroidism
Symptomatology
History of autoimmune disease
History of Graves disease treatment/ thyroid
surgery
Family history of thyroid disease
Excessive iodine exposure (contrast
dyes/medications)
Goiter/ exophthalmos/ pretibial myxedema
Atrial fibrillation/ palpitations/ tremor
Depression/ dementia
Unexplained weight loss/ hyperdefecation
Vitiligo/ alopecia/ coarse thinning hair
Heat intolerance/ sweating
Management
131
Radioactive Iodine (I ) Therapy
o
Treatment of choice for Graves
disease
Recurrent hyperthyroidism after
o
antithyroid therapy
o
Toxic multinodular gland
Toxic adenoma
o
Thyroiditis (painful, subacute or silent) should
131
not be treated with (I ) but requires
symptomatic therapy (-blockade)
Goal of therapy
o
To destroy thyroid tissue (followed by
fibrosis and atrophy which leads to
thyroid failure)
o
(N) TSH
131
Complications of I therapy: hypothyroidism
Antithyroid Drugs
o
Propylthiouracil preferred in severe
or life-threatening hyperthyroidism)
(thyroid storm); inhibits conversion of
T4 to T3
o
Methimazole for patients who will
131
subsequently undergo I therapy
o
50-80% recurrence of hyperthyroidism
following withdrawal of antithyroid
drugs
Enlargement of the thyroid gland
Diffuse
o
o
Nodular
Clinically exhibits
Hypothyroidism
o
o
Hyperthyroidism
Solitary Thyroid Nodule
Occurs in 4-7% of the general population
More common in women than in men
History of head/neck irradiation is a major risk
factor
Classification
o
Benign (colloid or follicular adenomas)
o
Suspicious
o
Malignant
FNAB principal diagnostic tool
Surgical excision depends on:
o
Tumor size
o
Location
o
Presence of lymph nodes
Thyroid scan:
o
Hot (hyperfunctioning)
o
Cold (hypofunctioning): higher
probability of being malignant and
managed with surgery
Post-Partum Thyroiditis (PPT)
Transient thyroiditis developing hypothyroidism
or hyperthyroidism in postpartum women who
were euthyroid during pregnancy
Occurs in 5-8% of women
Occurs in 25% of women with DMI
Autoimmune disorder, hence increased TPO Ab
Levothyroxine sodium therapy used as
replacement therapy
25% of women with PPT develop permanent
primary hypothyroidism
At high risk of recurrence following subsequent
pregnancies
Additional Reading:
Henrys metabolism and other factors affecting thyroid
function tests (p. 339)
rainwater@mymelody.com || 1st semester, AY 2011-2012
You might also like
- Preview of Knowing Ourselves What Does The Body Want To Tell Us With DiseasesDocument20 pagesPreview of Knowing Ourselves What Does The Body Want To Tell Us With Diseasesamita2009 saini60% (5)
- Mksap NotesDocument43 pagesMksap NotesDenny Hong100% (5)
- History Taking Cheat SheetDocument1 pageHistory Taking Cheat SheetLaura ForsythNo ratings yet
- Test Banks For Contemporary Clinical Immunology and SerologyDocument1 pageTest Banks For Contemporary Clinical Immunology and Serologyhamadadodo7No ratings yet
- Test Banks For Basic and Applied Concepts of Blood Banking and Transfusion PracticesDocument1 pageTest Banks For Basic and Applied Concepts of Blood Banking and Transfusion Practiceshamadadodo7No ratings yet
- Ely. Delirium SlidesDocument51 pagesEly. Delirium SlidesParvathy R NairNo ratings yet
- Pat 2 Medsurg1Document20 pagesPat 2 Medsurg1api-300849832No ratings yet
- Hypothyroidism Detection and TreatmentDocument4 pagesHypothyroidism Detection and TreatmentJoseph De Joya100% (1)
- Low thyroid hormone levels and hypothyroidism in Hazel CDocument5 pagesLow thyroid hormone levels and hypothyroidism in Hazel CRegine Mae EncinadaNo ratings yet
- Drug Management of Thyroid DiseaseDocument22 pagesDrug Management of Thyroid DiseaseHassan.shehri100% (6)
- Grave'S Disease: Farida Ulfa 1510211057Document11 pagesGrave'S Disease: Farida Ulfa 1510211057farida ulfaNo ratings yet
- Thyroid DisordersDocument67 pagesThyroid DisordersMA 09No ratings yet
- Pleural EffusionDocument35 pagesPleural Effusionkhikmatul mu'jizahNo ratings yet
- Hyperthyroidism History TakingDocument11 pagesHyperthyroidism History TakingmokkailinNo ratings yet
- Thyroid PathophysiologyDocument7 pagesThyroid PathophysiologyS RiarNo ratings yet
- Pituitary Gland: The Hormones and Their Function Presented By: Gufran Bulbul Rono Ciit IslamabadDocument16 pagesPituitary Gland: The Hormones and Their Function Presented By: Gufran Bulbul Rono Ciit IslamabadGufran Gb RonoNo ratings yet
- Therapeutics: Thyroid DisordersDocument24 pagesTherapeutics: Thyroid DisordersSharas FarhadNo ratings yet
- TB TreatmentDocument58 pagesTB TreatmentNdayisaba CorneilleNo ratings yet
- CholeraDocument5 pagesCholerabishnu011978No ratings yet
- Pa Tho Physiology of ParkinsonDocument2 pagesPa Tho Physiology of Parkinsoncuriosity_killsNo ratings yet
- Radio PharmaceuticalsDocument48 pagesRadio PharmaceuticalsKris Joy EbonNo ratings yet
- Sheehan SyndromeDocument6 pagesSheehan SyndromeArvie TagnongNo ratings yet
- Grave's Disease2.Document42 pagesGrave's Disease2.safeer kNo ratings yet
- Case PresDocument57 pagesCase PresJobelle Fernandez-SantosNo ratings yet
- Hyperthyroidism: A Practical Approach To Diagnosis and ManagementDocument70 pagesHyperthyroidism: A Practical Approach To Diagnosis and ManagementMutiara Manuella TambaNo ratings yet
- Cushings SyndromeDocument9 pagesCushings SyndromeMavra Imtiaz100% (1)
- Oral Revalida Im Cases Dec. 12 and 13 2020Document16 pagesOral Revalida Im Cases Dec. 12 and 13 2020Bea Y. Bas-ongNo ratings yet
- Addison's DiseaseDocument9 pagesAddison's Diseaseash ashNo ratings yet
- LA Myxoma Case PresentationDocument34 pagesLA Myxoma Case PresentationWiwik Puji LestariNo ratings yet
- Depression: Understanding the Leading Mental Health ConditionDocument38 pagesDepression: Understanding the Leading Mental Health Conditiondrmsupriya091159No ratings yet
- PresentationDocument11 pagesPresentationShravan TuragaNo ratings yet
- OsteoarthritisDocument15 pagesOsteoarthritisMichael BanksNo ratings yet
- Rheumatoid ArthritisDocument14 pagesRheumatoid ArthritisLorebell100% (5)
- Acute Appendicitis Diagnosis and ManagementDocument57 pagesAcute Appendicitis Diagnosis and ManagementYS NateNo ratings yet
- GoitreDocument6 pagesGoitreJohn Vladimir A. BulagsayNo ratings yet
- MR Elamin ShockDocument70 pagesMR Elamin ShockMohammed Abd AlgadirNo ratings yet
- Preoperative Assessment of Diabetic PatientsDocument2 pagesPreoperative Assessment of Diabetic PatientsShilpa Pradhan100% (1)
- Hypertension: Department of Internal MedicineDocument58 pagesHypertension: Department of Internal MedicineLouije MombzNo ratings yet
- Heart Failure With Preserved Ejection FractionDocument19 pagesHeart Failure With Preserved Ejection Fractioncosmin balanNo ratings yet
- Thyroid Emergencies: Abrar AlharbiDocument35 pagesThyroid Emergencies: Abrar AlharbiabrarNo ratings yet
- Hyporeninemic HypoaldosteronismDocument12 pagesHyporeninemic HypoaldosteronismCésar Augusto Sánchez SolisNo ratings yet
- Review Notes for Diabetes Mellitus Types, Pathophysiology, Complications & ManagementDocument8 pagesReview Notes for Diabetes Mellitus Types, Pathophysiology, Complications & ManagementEditha LucasNo ratings yet
- AGE AND DRUG DISPOSITION FACTORSDocument35 pagesAGE AND DRUG DISPOSITION FACTORSMalueth AnguiNo ratings yet
- DIABETIC COMA - Clinical Features and ManagementDocument54 pagesDIABETIC COMA - Clinical Features and ManagementRitesh SinghNo ratings yet
- NCM116 Addison DiseaseDocument20 pagesNCM116 Addison DiseaseSofia MikaelaNo ratings yet
- Amniotic Fluid Embolism Clinical Presentation ReviewDocument29 pagesAmniotic Fluid Embolism Clinical Presentation ReviewArun Kumar Gupta100% (1)
- Osteogenesis ImperfectaDocument27 pagesOsteogenesis Imperfectacode212No ratings yet
- Causes and Symptoms of Nontoxic GoiterDocument17 pagesCauses and Symptoms of Nontoxic Goiterabigaille chua100% (1)
- Journal - Alzheimer DiseaseDocument1 pageJournal - Alzheimer DiseaseTriLightNo ratings yet
- Myocardial InfarctionDocument25 pagesMyocardial Infarctionfam111222No ratings yet
- Case 7 ResultsDocument14 pagesCase 7 ResultsRegia putri ellandaNo ratings yet
- Hyperlipidemia Guide: Causes, Symptoms and TreatmentDocument17 pagesHyperlipidemia Guide: Causes, Symptoms and Treatmentbent alfay7a2No ratings yet
- Assess Patients HolisticallyDocument18 pagesAssess Patients HolisticallySavita Hanamsagar100% (1)
- Hyperthyroidism Causes, Symptoms, Diagnosis and TreatmentDocument40 pagesHyperthyroidism Causes, Symptoms, Diagnosis and TreatmentEmmanuelNo ratings yet
- Bronchial AsthmaDocument54 pagesBronchial AsthmaSehar162100% (2)
- Quiz 1Document3 pagesQuiz 1Micah Magallano100% (1)
- Graves DseDocument5 pagesGraves DseHester Marie SimpiaNo ratings yet
- New Thyroid PDFDocument4 pagesNew Thyroid PDFCrystal Gayle Nario SabadoNo ratings yet
- Management of Thyroid DisordersDocument53 pagesManagement of Thyroid DisordersAnityo S AthmadjaNo ratings yet
- Pathophysiology of Malaria: How Parasite Infection Affects the BodyDocument20 pagesPathophysiology of Malaria: How Parasite Infection Affects the Bodymelia100% (1)
- Adrenal DisordersDocument29 pagesAdrenal DisordersSuliman Garalleh100% (1)
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Distillation and DeionizerDocument26 pagesDistillation and Deionizerhamadadodo7No ratings yet
- Bur EtteDocument9 pagesBur Ettehamadadodo7No ratings yet
- Clinical PathologyDocument2 pagesClinical Pathologyhamadadodo7No ratings yet
- Use of Water BathDocument1 pageUse of Water Bathhamadadodo7No ratings yet
- BeakerDocument10 pagesBeakerhamadadodo7No ratings yet
- Chloride Test in WaterDocument4 pagesChloride Test in Waterhamadadodo7No ratings yet
- DecontaminationDocument9 pagesDecontaminationhamadadodo7No ratings yet
- Dis in Fact AntsDocument19 pagesDis in Fact Antshamadadodo7No ratings yet
- Deter GantsDocument8 pagesDeter Gantshamadadodo7No ratings yet
- Laboratory SafetyDocument18 pagesLaboratory Safetyhamadadodo7No ratings yet
- Conical Elernmeyer FlaskDocument10 pagesConical Elernmeyer Flaskhamadadodo7No ratings yet
- BalancesDocument28 pagesBalanceshamadadodo7No ratings yet
- Correct Use of A CentrifugeDocument1 pageCorrect Use of A Centrifugehamadadodo7No ratings yet
- Cleaning Lab GlasswareDocument19 pagesCleaning Lab Glasswarehamadadodo7No ratings yet
- Centrifuge: (January 2009)Document11 pagesCentrifuge: (January 2009)hamadadodo7No ratings yet
- Care and maintenance of autoclave for sterilizationDocument1 pageCare and maintenance of autoclave for sterilizationhamadadodo7No ratings yet
- Test Banks For Clinical Hematology and Fundamentals of HemostasisDocument1 pageTest Banks For Clinical Hematology and Fundamentals of Hemostasishamadadodo7No ratings yet
- Auto ClaveDocument12 pagesAuto Clavehamadadodo7No ratings yet
- Test Banks For Clinical Chemistry - A Laboratory PerspectiveDocument1 pageTest Banks For Clinical Chemistry - A Laboratory Perspectivehamadadodo7No ratings yet
- Boro Cili CateDocument9 pagesBoro Cili Catehamadadodo7No ratings yet
- Textbook of Diagnostic Microbiology 4th Edition Test BanksDocument1 pageTextbook of Diagnostic Microbiology 4th Edition Test Bankshamadadodo70% (1)
- 24 - Transfusion MedicineDocument3 pages24 - Transfusion Medicinehamadadodo7No ratings yet
- 24 - Blood Transfusion ReactionsDocument3 pages24 - Blood Transfusion Reactionshamadadodo7No ratings yet
- 23 - Introduction To ImmunopathologyDocument4 pages23 - Introduction To Immunopathologyhamadadodo7No ratings yet
- 22 - ImmunohematologyDocument6 pages22 - Immunohematologyhamadadodo7No ratings yet
- 18 - Flow Cytometry and Introduction To Molecular PathologyDocument11 pages18 - Flow Cytometry and Introduction To Molecular Pathologyhamadadodo7No ratings yet
- 20 - Tumor MarkersDocument2 pages20 - Tumor Markershamadadodo7No ratings yet
- Pediatric EndrocinologyDocument453 pagesPediatric Endrocinologyrayx323100% (1)
- ENDO SamsonDocument12 pagesENDO SamsonMuhammad BilalNo ratings yet
- ThyroidectomyDocument5 pagesThyroidectomyJennelyn LumbreNo ratings yet
- Journal AnalysisDocument2 pagesJournal AnalysisJust yor Regular CavegirlNo ratings yet
- ConclusionDocument2 pagesConclusionanzarNo ratings yet
- Thyroid Pregnancy ATA 2017 v2b 101017-021022Document11 pagesThyroid Pregnancy ATA 2017 v2b 101017-021022luismcanalNo ratings yet
- The Lympho Glandular and Intugmentary System: Presenter: Abdurke Dido - Physician (MD) May 22,2011Document62 pagesThe Lympho Glandular and Intugmentary System: Presenter: Abdurke Dido - Physician (MD) May 22,2011Worku KifleNo ratings yet
- Diagnosis and Treatment Hot NoduleDocument4 pagesDiagnosis and Treatment Hot NoduleGame overNo ratings yet
- Yoga Notes For Serious StudentsDocument10 pagesYoga Notes For Serious StudentsDr Srinivasan Nenmeli -KNo ratings yet
- Serie de Casos Ejemplo PDFDocument6 pagesSerie de Casos Ejemplo PDFGodoy GoNo ratings yet
- Autoimmunity Reviews: R. Tozzoli, M. Bagnasco, D. Giavarina, N. BizzaroDocument7 pagesAutoimmunity Reviews: R. Tozzoli, M. Bagnasco, D. Giavarina, N. BizzaroMohamed KhalidNo ratings yet
- Graves Disease and Hyperthyroidism Causes 60% of CasesDocument6 pagesGraves Disease and Hyperthyroidism Causes 60% of CasesLeitavia D.No ratings yet
- What Is GravesDocument3 pagesWhat Is GravesSynoyk AnunciacionNo ratings yet
- Medical School Lecture Notes: Cardiovascular, Pulmonary, GI, Renal, Neuro, and MoreDocument1 pageMedical School Lecture Notes: Cardiovascular, Pulmonary, GI, Renal, Neuro, and MoreGabriella RosinaNo ratings yet
- Endocrine Glands PathologyDocument8 pagesEndocrine Glands Pathologychrisp7No ratings yet
- Vijaya Diagnostic Lab Report AnalysisDocument5 pagesVijaya Diagnostic Lab Report AnalysisP Nagaraju RajuNo ratings yet
- MCQs on skin flaps, burns, trauma and thyroid disordersDocument9 pagesMCQs on skin flaps, burns, trauma and thyroid disordersFarrukh Ali Khan0% (1)
- HyperthyroidismDocument6 pagesHyperthyroidismNader Smadi100% (2)
- Instruments Leads - Hyderabad - ApDocument13 pagesInstruments Leads - Hyderabad - Apprasanth gNo ratings yet
- Thyroid GlandDocument30 pagesThyroid GlandahmedkomranNo ratings yet
- Approach To A Patient With "Solitary Thyroid Nodule" (STN)Document6 pagesApproach To A Patient With "Solitary Thyroid Nodule" (STN)Jacob Alexander MarpaungNo ratings yet
- Nodular Nontoxic Goiter: Causes, Risks, SymptomsDocument4 pagesNodular Nontoxic Goiter: Causes, Risks, SymptomsEjay Jacob RicamaraNo ratings yet
- LAB REPORT REVEALS THYROID AND PREGNANCY HORMONE LEVELSDocument2 pagesLAB REPORT REVEALS THYROID AND PREGNANCY HORMONE LEVELSSnju BjajNo ratings yet
- Multinodular Goiter: Dr.V.V.Subrahmanyam Professor of Surgery Narayana Medical College & HospitalDocument34 pagesMultinodular Goiter: Dr.V.V.Subrahmanyam Professor of Surgery Narayana Medical College & HospitalPraveen Chandra GanjiNo ratings yet
- HY Endocrine UsmleDocument22 pagesHY Endocrine UsmleNakhal JararNo ratings yet
- Choosing Wisely Master ListDocument92 pagesChoosing Wisely Master ListrobertojosesanNo ratings yet
- Thyroid Gland 2021Document28 pagesThyroid Gland 2021Dr. Ali100% (1)