Professional Documents
Culture Documents
Ajopht 1975 Bos
Uploaded by
remotmCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ajopht 1975 Bos
Uploaded by
remotmCopyright:
Available Formats
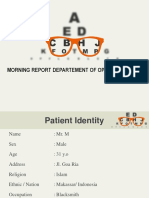
AMERICAN JOURNAL OF OPHTHALMOLOGY
VOLUME
80
OCTOBER, 1975
NUMBER
ACUTE MACULAR NEURORETINOPATHY
PIERRE J.
M.
BOS,
M.D.
Amsterdam, The Netherlands
AND
AUGUST F.
DEUTMAN,
M.D.
Rotterdam, The Netherlands
Recently we observed four women with a
peculiar acute macular affection, characterized by slight depression of visual acuity and
nararentral scotomas correfip"ti"g w i t n
dark-reddish, wpHgp-sriappfl jrrfrarptinal lesin^g rw^ntinff tr> trip fnvpa.
We performed electroretinography and
electro-oculography in two patients.2 All patients underwent general physical examination and laboratory tests.
CASE REPORTS
Case 1A 29-year-old white woman had noticed
black dots and scotomas in both central visual
fields since April 15, 1971. The onset of the complaints was sudden. She was first seen on April 20,
1971, when corrected visual acuity in both eyes
was 20/20.
Ophthalmologic examination showed no abnormalities outside the macular regions. There were
irregular reflexes and dark, brown-reddish flecks in
the right macula; some had a triangular configuration with the sharp point of the triangle directed
toward the fovea (Fig. 1, left). Some polymorphic
spots were present elsewhere in the macula. In her
left eye (Fig. 1, right), she demonstrated similar
irregular reflexes and some dark red-brownish dots,
like those in her right eye.
Biomicroscopy revealed that these spots were not
located in the pigment epithelium but in the more
superficial retinal structures. Fluorescein angiography was normal (Fig. 2). Kinetic perimetry
showed that the peripheral boundaries of the visual
fields were intact, while static perimetry demonstrated dense scotomas in the 2- to 5-degree area of
both eyes and a slight decrease in central light sensitivity (Fig. 3).
There were no systemic complaints. In her youth
the patient had had a splenectomy because of familial thrombocytopenia, but otherwise she had a noncontributory medical history. She was taking the
oral contraceptive lynestrenol (Lyndiol).
No subjective changes were observed during follow-up and static visual fields were unchanged. The
From the Department of Ophthalmology, Univer- fundus changes were visible, although the lesions
sity of Amsterdam (Dr. Bos), and the Eye Hospital, were less obvious.
Erasmus, University of Rotterdam (Dr. Deutman),
Case 2A 33-year-old white woman noticed a
The Netherlands.
scotoma in her left eye of sudden onset on Sept. 18,
Reprint requests to A. F. Deutman, M.D., De- 1972. Her right eye was completely normal. She
partment of Ophthalmology, University of Nij- had not been ill before the ocular complaints. She
megen, Nijmegen, The Netherlands.
had been using lynestrenol for eight years.
573
The macular pigment epithelium appeared
normal and the retinal vessels did not show
gross abnormalities. The optic disk was unaffected and there were no nerve fiber defects. Visual recovery, when present, progressed slowly over many months.
Since no similar disease process is known
to us, we called this entity acute macular
neuroretinopathy (neuroepitheliopathy)1 because of the acute onset and the localization
of the lesions in the more superficial retinal
layers at the macula.
Two patients were seen in the Amsterdam
Eye Clinic, one patient was seen in the
Rotterdam Eye Hospital, and the fourth was
examined at both hospitals.
Routine ophthalmoscopic examination,
fundus photography, andfluoresceinangiography were done in all patients. The photographic methods have been described.2 Kinetic visual fields were recorded with the
Goldmann perimeter and static perimetry
with the Tubinger perimeter.
574
AMERICAN JOURNAL OF OPHTHALMOLOGY
OCTOBER, 1975
Fig. 1 (Bos and Deutman). Case 1. Right macula (left) and left macula (right) showing darkish
wedge-shaped and irregular flecks, localized in the neuroretina.
Fig. 2 (Bos and Deutman). Case 1. Fluorescein
angiography of the right macula showing a normal
fluorescence pattern in the arteriovenous phase.
Two days after the onset of symptoms, she had
normal central vision in both eyes. There was a
dark brown-reddish spot in the macular region of
the left eye close to the fovea (Fig. 4, left). Other-
wise her eyes were normal.
Fluorescein angiography revealed some questionably dilated perimacular capillaries (Fig. 4, right).
There was, however, no leakage of dye recorded in
the late stages of the angiogram, such as seen in
cystoid macular edema.3
Meticulous static perimetry revealed a scotoma in
the 1- to 3-degree area from the center of the left
eye (Fig. S). This scotoma was not as dense as
the scotoma recorded in Case 1.
The patient was last seen in October 1973, when
the symptoms were unaltered. Careful ophthalmoscopy showed a faint discoloration located where
the dark spot was seen originally. Static perimetry
still showed a scotoma that had decreased slightly
in depth (Fig. 6).
Case 3A 24-year-old white woman noticed disturbance of her central vision after visiting a game
reserve where she had had a bout of enteritis. She
claimed she had not been looking at the sun.
On March 2, 1972, she was seen in the Amsterdam University Clinic. Visual acuity in both eyes
was 20/20. Ophthalmologic examination was normal outside the macular regions, which had a
swollen glossy appearance with increased reflexes
and vague, darkish red, wedge-shaped lesions around
the center of the macula. The lesions pointed toward
the fovea with a butterfly-shaped appearance (Fig.
7
>Fluorescein angiography revealed no abnormali-
Fig. 3 (Bos and Deutman). Case 1. Static perimetry (top and bottom) performed with the Tiibinger perimeter showing slightly decreased light sensitivity centrally and paracentrally in the right eye (top) and
dense paracentral scotomas in the left eye (bottom). These scotomas were also seen with kinetic perimetry
(center) in the left eye.
AMERICAN JOURNAL OF OPHTHALMOLOGY
576
OCTOBER, 1975
Fig. 4 (Bos and Deutman). Case 2, left eye. Macula showing one darkish, wedge-shaped dot superonasally to the fovea. Fluorescein angiography of this macula (right) showed no clear abnormalities.
There is only questionable dilatation of some of the perimacular capillaries.
40
30
210
35
25
20
15
~1
;
^
1I v> ST \
~S
-'"
f*^
JI
10
32
10
05
Fig. 5 (Bos and Deutman). Case
2, left eye. September 1972. There
is a dense, well-delineated, paracentral scotoma corresponding to the
side of the ophthalmoscopically
visible dot. This scotoma was recorded with the Tubinger perimeter
after painstaking care in static
perimetry.
I
1 1 1 11 1 1 11 1 1 1'111 1111
20
10
0'
1 1 1 11111
3 0"
I I I I I I I 1 1 1 1.' ML
20
SO4"'
10
IM
40
30:
2)0
35
1
30
3,2
310
20
15
32
10
I I 1 1 1111 1 1 1 1 1 1 1l l 1 1.IL>'
3 0*
10
20
1 III
I 11 l M i l
10'
IP
1 III
20 *
1,111
320
^000
Fig. 6 (Bos and Deutman). Case
2, left eye. May 1973. Left macula
showing some remnants of the paracentral scotoma shown in Figure 5.
VOL. 80, NO. 4
ACUTE MACULAR NEURORETINOPATHY
577
Fig. 7 (Bos and Deutman). Case 3. March 2, 1972. Right macula (left) and left macula (right) demonstrating wedge-shaped lesions not unlike the shape of a butterfly. However, these lesions are localized
more superficially in the retina than in butterfly-shaped pigment dystrophy and they are not pigmented.
ties (Fig. 8). Static perimetry, however, showed a
paracentral scotoma for maximal luminance above
the center in the right eye (Fig. 9). No scotoma
was seen in the left eye.
On March 29, she was seen at the Rotterdam
Eye Hospital. Visual acuity in both eyes was 20/20.
The Amsler grid test showed three small scotomas,
two temporal to the fixation point in the left eye.
Ophthalmologic examination revealed abnormalities
at the macula that appeared swollen and glossy,
with increased reflexes and vague, darkish red,
wedge-shaped lesions around the center of the
macula. The lesions pointed toward the fovea with
a butterfly-like appearance. The ophthalmoscopically
abnormal areas appeared to correspond almost completely with the scotomas demonstrated on the
Amsler grid.
On April 4, 1973, there was little subjective
change (Fig. 10). Electroretinography and electrooculography were performed and appeared to be
completely normal. The electroretinogram (ERG)
responses were normal. Scotopic and photopic a
and b waves were well above the lower limits of
normal. The electro-oculogram (EOG) showed a
normal light/dark ratio of 2.74 in the right eye and
2.85 in the left eye.
There were no systemic complaints. This patient
was taking the oral contraceptive norgestrel
(Eugynon).
In October 1973, there were no subjective
changes. The same characteristic fimdus changes
were observed, although they were more faint.
Angiography was performed, and was normal. Perimetric details were the same as in March 1972
(Fig. 9).
Case 4A 32-year-old white woman noticed
scotomas in both eyes during a bout of influenza
and high fever in the middle of December 1972.
When seen on Jan. 2, 1973, visual acuity was R.E.:
20/25, and L.E.: 20/66. Visual acuity in the left
eye had always been slightly worse than in her
right eye, probably due to amblyopia.
On Jan. 9, her visual acuity was unchanged. The
Amsler test demonstrated a paracentral scotoma on
the temporal side of the fixation point in the right
eye and a rather large scotoma temporal to the
center in the left eye. Both macular areas appeared
Fig. 8 (Bos and Deutman). Case 3. Fluorescein
angiogram of the right macula revealing no abnormalities in the arteriovenous phase.
578
AMERICAN JOURNAL OF OPHTHALMOLOGY
OCTOBER, 1975
Fig. 9 (Bos and Deutman). Case 3, right eye. Absolute paracentral scotoma in the
45- to 225-degree axis with kinetic perimetry (top) and static perimetry (bottom).
edematous with increased reflexes. There was one
dark-reddish, triangular zone in the right macula,
just nasal to the foveola (Fig. 11, left), and at
least three wedge-shaped darkish-red lesions pointing to the center in the left eye (Fig. 11, right).
The nerve fiber layer was more pronounced nasal
to the center. Otherwise the ocular examination
showed no pathologic findings. Vessels, disk, and
retinal periphery were normal in both eyes and the
media were clear.
Fluorescein angiography demonstrated an intact
retinal pigment epithelium. There were some ques-
tionably dilated perimacular capillaries above the
fovea (Fig. 12, top left), but there were no fluorescein leaks (Fig. 12, top right and bottom left).
With the Goldmann contact lens, the retinal
swelling appeared to be localized to the inner
portion of the sensory retina. The patient was hospitalized on Jan. 16, when vision had not improved.
A general physical and laboratory examination revealed a slightly abnormal glucose tolerance test.
There was no glycosuria. She had hypercholesterolemia (9.9 mM/1; normal, 6.4 mM/1). She had
used contraceptives for many years. The patient
VOL. 80, NO. 4
ACUTE MACULAR NEURORETINOPATHY
579
Fig. 10 (Bos and Deutman). Case 3. April 4, 1973. Right macula (left) and left macula (right) with
the wedge-shaped paracentral dots that are more visible in tht right eye than in the left eye.
received one tablet of xanthinol niacinate (Complamine), twice daily, carbon dioxide inhalation,
clofibrate capsules, and a diet. A neurologic examination, including x-ray films of the sella turcica,
was normal.
On Jan. 18, central visual fields showed a small
paracentral scotoma on the superotemporal side of
the fixation (Fig. 13). On Jan. 29, visual fields were
unchanged, but by May 11, there was a small but
definite decrease in the size and depth of the scotomas (Fig. 14).
Electroretinograms performed on J a a 17, with
diffuse and macular stimulation, were normal. The
visually evoked cortical potentials were also normal.
On May 4, visual acuity was R.E.: 20/25, and
L.E.: 20/50. Subjectively there was not much
change, although the left eye had improved slightly.
On June 27, visual acuity was R.E.: 20/22, and
L.E.: 20/40. She complained of seeing flecks close
to the center in the right eye and paracentral and
temporal flecks in the left eye. The maculae appeared swollen although the swelling had subsided.
Fig. 11 (Bos and Deutman). Case 4. Acute macular neuroretinopathy. Clearly visible darkish wedgeshaped lesions are in the superficial part of the retina. In the left eye (right), these lesions are doverleaf
shaped and the nerve fiber layer demonstrates an increased visibility.
580
AMERICAN JOURNAL OF OPHTHALMOLOGY
OCTOBER, 1975
Fig. 12 (Bos and Deutman). Case 4. Fluorescein
angiography of the left macula (top) shows questionably dilated perimacular capillaries on top oi
the macula. However, there is no sign of fluorescein
leakage in the late phases of angiography. Bottorr
left, The right macula also has a normal fluorescence pattern.
On Nov. 19, visual acuity was R.E.: 20/20, and
L.E.: 20/33. The paracentral scotomas were present
and caused considerable disability.
DISCUSSION
This disease appears to be a distinct entity
that, to our knowledge, was described only in
a short communication.1
It is different from the many clinical diseases affecting the central f undus, recognized
in recent years and differentiated from one
another based on the nature of the disease
and the accompanying morphologic changes.
Central serous choroidopathy4 is one such
entity that is well known but poorly understood. It is probably caused by dilation anc
profusely leaking capillaries of the centra
choriocapillaris.
Acute posterior multifocal placoid pig
ment epitheliopathy is another of these enti
ties.5 Although some authors 5 think this dis
ease process is due to pigment epithelia
disease, there are arguments in favor of ;
primary affection of the choriocapillaris.
In both diseases the morphologic change
occurring in the pigment epithelium ar
probably secondary.
The changes in acute retinal pigment epi
VOL. 80, NO. 4
ACUTE MACULAR NEURORETINOPATHY
581
theliitis7*8 appear to be nearly completely
restricted to the pigment epithelium and this
disease has a more favorable course, leading
to complete recovery in six to ten weeks.
There are no cells in the vitreous body or in
the anterior chamber. A viral inflammation
probably causes this self-limiting condition.
Serpiginous (geographic) choroiditis1'9
presents lesions at different stages of evolution. In early lesions there is a definite pale
swelling of the pigment epithelium while
older lesions demonstrate atrophy of the
pigment epithelium and choriocapillaris surrounded by an edematous retinal zone. This
inflammatory disease is characterized by
relentless progression, presents in patients
in their fourth decade and, in our experience,
responds well to corticosteroids.
The so-called presumed histoplasmic choroiditis represents a distinct clinical entity
Fig. 13 (Bos and Deutman). Case 4. January
1973. Central visual fields demonstrating dense
paracentral scotomas on the superonasal side of the
center. Top, right eye; bottom, left eye.
Fig. 14 (Bos and Deutman). Case 4. May 1973.
Central visual fields demonstrating some improvement. The scotomas are slightly smaller and less
dense than in January 1973. Top, right eye; bottom,
left eye.
582
AMERICAN JOURNAL OF OPHTHALMOLOGY
Fig. IS (Bos and Deutman). Case 4. Wedgeshaped lesions, shaped not unlike the lesion in acute
macular neuroretinopathy, in a patient with intraretinal hemorrhages due to hypertensive retinopathy.
affecting adults, characterized by subretinal
neovascularization at the fovea. We saw this
ocular syndrome in patients without evidence
of previous infection by Histoplasma capsulatum.1
The disease we present appears to be localized to the more superficial retinal layers,
shown well on binocular slit-lamp examination, while fluorescein angiography displayed
no choroidal or retinal pigment epithelial
abnormalities. The retinal vessels do not
show definite abnormalities and do not leak
fluorescein. The nerve fiber layer is not
obviously affected since no nerve fiber layer
defects were disclosed even after extensive
perimetric examination.
There was no diffuse retinal disturbance
since, in those patients tested, the ERGs and
EOGs were normal. Static perimetry demonstrated a well-localized paracentral retinal
disease with dense scotomas. The lesions
were located predominantly on the nasal
side of the fovea. The wedge-shaped lesions
were shaped not unlike certain intraretinal
hemorrhages (Fig. 15) and, therefore, may
be localized at the same level in the neuroretina.
OCTOBER, 197S
As in all macular diseases without striking
ophthalmoscopic changes, optic neuropathy
has to be differentiated. However, there are
no macular changes in optic neuropathy and
partial or complete optic atrophy occurs in
time. The visual fields and the macular
changes together with the normal appearance
of the optic disk indicated macular pathology
in all four cases. In Case 4, optic nerve
pathology was excluded by normal, visually
evoked cortical potentials and by a normal
neurologic examination.
AddendumRecently
one
of
us
(PJ.M.B.) examined a 30-year-old white
woman who developed acute macular neuroretinopathy a few weeks after an influenzalike disease. Visual acuity was R.E.: 20/20,
and L.E.: 20/100. The maculae showed
wedge-shaped lesions in the superficial retinal
layers (Fig. 16). Paracentral scotomas were
elicited. Color vision was normal. After a
few weeks visual acuity was 20/20 in both
eyes. However, four months after the visual
symptoms started, she still had paracentral
scotomas. No systemic abnormalities were
found. This patient used the oral contraceptive ethinyl estradiol (Neogynon).
Another patient, a 23-year-old white man
who developed visual problems in his right
eye after a bout of influenza, presented with
a mild form of acute macular neuroepitheliopathy. Visual acuity was R.E.: 20/25,
W L.E.: 20/20. Nasally to the right fovea
there was a darkish dot in the superficial
retinal layers (Fig. 17). Fluorescein angiography did not show any abnormality. Color
vision was also normal. Perimetry, however,
demonstrated a small and dense visual field
defect at the site of the ophthalmoscopically
visual lesion. The left eye was completely
normal. The macular picture did not change
during two months of observation.
SUMMARY
An unrecognized acute macular affection
occurred in four women, 24 to 35 years
old, using oral contraceptives who com-
VOL. 80, NO. 4
ACUTE MACULAR NEURORETINOPATHY
plained of a sudden decrease of visual acuity
or paracentral scotomas.
Three patients had bilateral lesions and one
patient had unilateral lesions. These lesions
consisted of darkish brown-red, wedgeshaped dots in the macula pointing to the
fovea. These dots were located mostly on the
nasal side of the macula.
Biomicroscopy showed these lesions were
located in the superficial layers of the retina.
Fig. 17 (Bos and Deutman). A small darkish dot
on the nasal side of the right fovea corresponding
with a deep paracentral scotoma as the only manifestation of acute macular neuroretinopathy.
The retinal vessels, pigment epithelium, and
optic disk showed no distinct pathologic
features. Fluorescein angiography, performed repeatedly, showed some questionably dilated perimacular capillaries without
leakage in two cases.
Static perimetry delineated dense paracentral scotomas. Recovery was slow or
absent, confirmed by perimetric observation.
Ophthalmoscopic, fluorescein angiography,
and perimetric details excluded an affection
of the pigment epithelium, the nerve fiber
layer, and the optic disk. Since the affection
appears to be localized superficially in the
retina, we called this specific entity acute
macular neuroretinopathy.
ACKNOWLEDGMENTS
H. H. A. H6tte, M.D., and R. A. Crone, Ph.D.,
referred Case 3, and H. E. Henkes, Ph.D., referred
Case 4.
REFERENCES
Fig. 16 (Bos and Deutman). Right and left macula (top and bottom, respectively) of a 30-year-old
white woman shows the typical superficial wedgeshaped lesions of acute macular neuroretinopathy.
The wedges point to the center of the fovea.
1. Deutman, A. F.: Fluorescein angiography in
macular diseases. In Henkes, H. E. (ed.) : Photography, Electro-Ophthalmology and EchoOphthalmology in Ophthalmic Practice, vol. 3. The
Hague, W. Junk, 1973, pp. 208-209.
2.
: The Hereditary Dystrophies of the
Posterior Pole of the Eye, thesis. Assen, The
Netherlands, Van Gorcum and Co., 1971.
584
AMERICAN JOURNAL OF OPHTHALMOLOGY
3. Gass, J. D. M., and Norton, E. W. D.:
Cystoid macular edema and papilledema following
cataract extraction. Arch. Ophthalmol. 76:646,
1966.
4. Gass, J. D. M.: Pathogenesis of disciform detachment of the neuroepithelium. 1. General concepts and classification. Am. J. Ophthalmol. 63:573,
1967.
5.
: Acute posterior multifocal placoid
pigment epitheliopathy. Arch. Ophthalmol. 80:177,
1968.
OCTOBER, 1975
6. Deutman, A. F., Oosterhuis, J. A., Boen-Tan,
T. N., and Aan de Kerk, A. L.: Acute posterior
multifocal placoid pigment epitheliopathy. Br. J.
Ophthalmol. 56:863, 1972.
7. Krill, A. E., and Deutman, A. F.: Acute
retinal pigment epitheliitis. Am. J. Ophthalmol.
74:193, 1972.
8. Deutman, A. F.: Acute retinal pigment
epitheliitis. Am. J. Ophthalmol. 78:571, 1974.
9. Schlaegel, T. F., Jr.: Essentials of Uveitis.
London, Churchill, 1969, pp. 101-103.
OPHTHALMIC MINIATURE
He had only one good eye. The left distinguished only light and shade.
But the good eye was dark-bright, full of observation through the overhanging hair of the brow as in some breeds of dog. For his height he had
a small face. The combination made him conspicuous.
Saul Bellow, Mister Sammler's Planet
New York, Viking Press, 1970
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Arch Ophthalmol 1991 YannuzziDocument6 pagesArch Ophthalmol 1991 YannuzziremotmNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Choroidal Granulomas in Sistemic SarcoidosisDocument8 pagesChoroidal Granulomas in Sistemic SarcoidosisremotmNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Arch Ophthalmol 2011 YehDocument4 pagesArch Ophthalmol 2011 YehremotmNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Am J Ophthalmol 2015 SridharDocument12 pagesAm J Ophthalmol 2015 SridharremotmNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Brief Reports Out - 2001Document39 pagesBrief Reports Out - 2001remotmNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Ajopht 1977 RushDocument5 pagesAjopht 1977 RushremotmNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Am J Ophthalmol 2014 YuDocument13 pagesAm J Ophthalmol 2014 YuremotmNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Am J Ophthalmol 2015 DansinganiDocument5 pagesAm J Ophthalmol 2015 DansinganiremotmNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Am J Ophthalmol 2015 ChenDocument10 pagesAm J Ophthalmol 2015 ChenremotmNo ratings yet
- Acta Ophthalmol Scand 2000 Feigl-1Document4 pagesActa Ophthalmol Scand 2000 Feigl-1remotmNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Am J Ophthalmol 2014 Rahimy-3Document10 pagesAm J Ophthalmol 2014 Rahimy-3remotmNo ratings yet
- An Analysis of Lesion Size and Location in Newly Diagnosed CyDocument7 pagesAn Analysis of Lesion Size and Location in Newly Diagnosed CyremotmNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- AJOPHT 1978 PriluckDocument4 pagesAJOPHT 1978 PriluckremotmNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Squisis MacularDocument8 pagesSquisis MacularremotmNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Brief Reports Fev - .2001pdfDocument30 pagesBrief Reports Fev - .2001pdfremotmNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- AntioxidantDocument8 pagesAntioxidantremotmNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Reducing Wrong IOL Implantation in Cataract CareDocument5 pagesReducing Wrong IOL Implantation in Cataract CareremotmNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Randomized, Double-Masked Trial of Topical Ketorolac VersusDocument6 pagesA Randomized, Double-Masked Trial of Topical Ketorolac VersusremotmNo ratings yet
- Katarak Penyebab KebutaanDocument96 pagesKatarak Penyebab KebutaanIhsan HaidarNo ratings yet
- Artigo01 10 - 3928 - 1081597X - 20120921 - 07Document11 pagesArtigo01 10 - 3928 - 1081597X - 20120921 - 07remotmNo ratings yet
- Acute Multifocal Placoid Pigment EpitheliopathyDocument8 pagesAcute Multifocal Placoid Pigment EpitheliopathyremotmNo ratings yet
- Artigo 02 1-S2.0-S0161642012003545-MainDocument6 pagesArtigo 02 1-S2.0-S0161642012003545-MainremotmNo ratings yet
- Oral Mifepristone For Chronic Central Serous.26Document9 pagesOral Mifepristone For Chronic Central Serous.26remotmNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Spaide PDFDocument11 pagesSpaide PDFremotmNo ratings yet
- Low Vision - AidsDocument209 pagesLow Vision - AidsDudi50% (2)
- Contrast Sensitivity For Human Eye SystemDocument10 pagesContrast Sensitivity For Human Eye SystemNandagopal SivakumarNo ratings yet
- Application PDFDocument6 pagesApplication PDFRohit ChandrasekharNo ratings yet
- Bates Method How Does It WorkDocument4 pagesBates Method How Does It WorkIvan MedićNo ratings yet
- Vision Requirements SNT-TC-1ADocument1 pageVision Requirements SNT-TC-1ARameez Farouk100% (1)
- The Effects of Visual Training On VisionDocument6 pagesThe Effects of Visual Training On VisionEvelyn SepulvedaNo ratings yet
- PRESBYOPIA May 2014Document93 pagesPRESBYOPIA May 2014Tonpitonpi Ton PiNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Visual AcuityDocument16 pagesVisual AcuityjoshulyNo ratings yet
- Titmus 2s Aparato de Revisin de La VistaDocument3 pagesTitmus 2s Aparato de Revisin de La VistaJavier LagunaNo ratings yet
- Physical Assessment Health Assessment: Light Palpation TYPES OF PALPATIONDocument22 pagesPhysical Assessment Health Assessment: Light Palpation TYPES OF PALPATIONLore Anne Mhae SantosNo ratings yet
- Introduction To Penetrant TestingDocument61 pagesIntroduction To Penetrant TestingjerryceppyNo ratings yet
- Printable Snellen Eye ChartDocument1 pagePrintable Snellen Eye ChartRoger ArcNo ratings yet
- The Neurological ExaminationDocument28 pagesThe Neurological ExaminationpremaNo ratings yet
- Renewal STCW Certificates Endorsements PDFDocument25 pagesRenewal STCW Certificates Endorsements PDFVioleta BautuNo ratings yet
- Low Vision AidsDocument209 pagesLow Vision Aidssabeeha kausarNo ratings yet
- Logmar Bailey-Lovie ChartDocument14 pagesLogmar Bailey-Lovie ChartristaniatauhidNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- CataractDocument17 pagesCataractrhopmaeNo ratings yet
- Measuring Reading PerformanceDocument9 pagesMeasuring Reading PerformanceRishabh DevNo ratings yet
- Optics and Refraction For PodcastDocument74 pagesOptics and Refraction For PodcastWaleedAhmadNo ratings yet
- RS Sayang Rakyat - CORPALDocument11 pagesRS Sayang Rakyat - CORPALNurbaitil Atiq TamiiNo ratings yet
- Etec 500 ResearchproposalfinalDocument13 pagesEtec 500 Researchproposalfinalapi-336460760No ratings yet
- Waiver Guide US Navy2010Document325 pagesWaiver Guide US Navy2010Ridy Ishvara PNo ratings yet
- NIDEK ARK560a User ManualDocument6 pagesNIDEK ARK560a User Manualc_887338806No ratings yet
- Ms Penta NotesDocument84 pagesMs Penta Notesshenric16No ratings yet
- Binocular Vision: Rahul Bhola, MDDocument17 pagesBinocular Vision: Rahul Bhola, MDRonny AvatarNo ratings yet
- Blue Collar Billing CodingDocument18 pagesBlue Collar Billing CodingShell VenkatNo ratings yet
- 06 Bin Ocula BalanceDocument9 pages06 Bin Ocula BalanceReuben GuzmánNo ratings yet
- Semi Elliptical Head Specs PDFDocument2 pagesSemi Elliptical Head Specs PDFJ.SIVIRANo ratings yet
- Neuro Exam ReviewDocument6 pagesNeuro Exam ReviewDianne Flores100% (2)
- Simulation in ophthalmology: Detecting malingering and conversionDocument9 pagesSimulation in ophthalmology: Detecting malingering and conversionYeremias EdwinNo ratings yet