Professional Documents
Culture Documents
Efficacy Comparison of Cetirizine and Loratadine For
Uploaded by
Rully Febri AnggoroCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Efficacy Comparison of Cetirizine and Loratadine For
Uploaded by
Rully Febri AnggoroCopyright:
Available Formats
Efficacy Comparison Of Cetirizine And Loratadine
For
Allergic Rhinitis In Children
Abstract
Background
Allergic rhinitis represents a global health problem
affecting 10% to more than 40% of the population worldwide.
Several studies in recent years have described the efficacy of secondgeneration antihistamines in younger children. It is not well established
whether cetirizine is more effective than loratadine in reducing symptoms
of allergic rhinitis.
Objective
The objective of this study was to compare the efficacy of loratadine with
cetirizine for treatment of allergic rhinitis. Methods We conducted a
randomized, double-blind, controlled trial of 100 children, aged 13 to 16
years, from October to November 2009 at two junior high schools in
Medan. Group I received 10 mg of cetirizine and group II received 10 mg
of loratadine, each once daily in the morning for 14 days. Drug efficacy
was assessed by changes from baseline symptom scores and evaluation
of therapeutic responses after 3 days, 7 days and 14 days of treatment.
Results
The efficacy of cetirizine compared to that of loratadine was not
statistically significant in diminishing nasal symptoms after 3 days, 7 days
and 14 days of treatment (P 0.40, P 0.07, and P 0.057, respectively).
Evaluation of side effects, however, revealed significantly fewer
headaches in the cetirizine group after
3 days and 7 days of treatment (P 0.01 and P 0.03, respectively) than in
the loratidine group. In addition, the loratadine group had significantly
more instances of palpitations after 7 days of treatment (P 0.04)
compared to the cetirizine group.
Conclusion There was no significant difference in cetirizine and loratadine
treatment effectiveness on allergic rhinitis. However, loratadine was found
to cause more headaches and palpitations than cetirizine.
Allergic rhinitis (AR) is a global health problem, affecting 10% to
more than
40% of the population worldwide.
Symptomatic allergic rhinitis reduces quality of life and may
contribute to impairment of psychological well-being and cognitive
function.
Antihistamines are the pharmacologic corner - stone of treatment
for allergic rhinitis. The comparative effects of second generation antihistamines, cetirizine and loratadine, among younger patients have not
been well documented. Cetirizine and loratadine are antagonists to the
histamine H1 receptor and their metabolism may lead to sedative.
and cardiotoxic effects. Thus, more research on these drugs is needed.
Loratadine is 98% metabolized in the liver and excreted by the
kidneys, while cetirizine metabolism does not involve the liver, though it is
mostly excreted by the kidneys. However, Bucks et al found that
cetirizine is six times more potent than loratadine, thus a higher dose of
loratadine is often required to achieve a similar result. Other second
generation antihistamines, such as terfenadine and astemizole, also had
similar effects compared to cetirizine, but these drugs are metabolized
rapidly in the liver and have cardiotoxic effects. The purpose of this
study was to compare the efficacy of cetirizine and loratadine for
treatment of allergic rhinitis in children.
Methods
We conducted a randomized, double-blind, controlled trial from
October to November 2009 at two junior high schools in Medan. Data were
collected by questionnaire. Patients were enrolled in the study if they had
symptoms of allergic rhinitis (runny nose, sneezing, nasal stuffiness, eye
itchiness, eye redness, sleep disturbance, impaired cognitive functioning,
or school absence) and were atopic. We included children aged 13 to 16
years, who were diagnosed with allergic rhinitis that was confirmed by
nasal examination. To evaluate severity of the disease, we used a rhinitis
allergic scoring system : 0 evident symptoms, 1 mild symptoms not
interfering with daily activities and or sleep, 2 moderate symptoms
somewhat interfering with daily activities and or sleep, and 3 severe
symptoms with major.
interference in daily activities and/or sleep. We excluded subjects with a
history of documented asthma, sinusitis, common cold, otitis media,
nasal anatomic abnormalites, known idiosyncratic reactions to cetirizine or
loratadine, corticosteroid use within two weeks of the first test dose, oral
or topical decongestant and antihistamine use within 24 hours of the first
test dose, and those who refused to consume the drug.
Patients were divided into two groups by simple randomization
using random tables. Group I received 10 mg cetirizine and group II
received 10 mg loratadine, with each medication taken once a day orally
for 14 days. We evaluated the patients at visit 1 for screening, after 3
days (visit 2), after 7 days (visit 3) and after 14 days (visit 4) of treatment.
Subjects were not allowed to consume other antihistamines or
corticosteroids during treatment period.
Treatment efficacy was assessed by changes from baseline
symptom scores and side effects were assessed after therapeutic
response at 3 days, 7 days, and 14 days of treatment. Symptoms were
observed and physical examination was performed at each visit. This
study was approved by the Ethics Committee of the Medical School
University of North Sumatera.
Chi- square test was performed to analyze treatment efficacy and
side effects. Differences were considered significant if P< 0.05. We used
SPSS version 15 for data processing. Our study was an intention to treat
analysis.
Result
We screened 475 students, of which 150 suffered from allergic rhinitis.
Fifty of these students were excluded for the following reasons: 40
students were aged below 13 years, 5 students refused to participate, and
5 students were already taking antihistamines. The remaining 100
students were randomized into two groups of 50, each of whom received
treatment with 10 mg loratadine or 10 mg cetirizine (Figure 1).
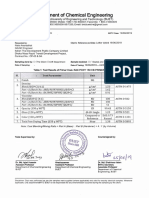
Subjects' characteristics are shown in Table 1.
The mean age in the cetirizine group was 13.40 years while in that
of the loratadine group was 13.38 years. There were 34 females in the
cetirizine group (68%) and 29 in the loratadine group (58%). At the first
visit, 21 students in the cetirizine group had a moderate allergic rhinitis
score while 29 students had a severe score. In the loratadine group, 16
had moderate and 34 had severe scores. The majority of subjects (63%)
had severe allergic rhinitis scores at baseline.
Table 2 shows scores of allergic rhinitis at days 3, 7, and 14 of
treatment. On days 3 and 7, there were decreased symptoms of rhinitis in
both groups, but there was no statistically significant difference between
the two groups (P 0.40 for day 3 and P 0.07 for day 7).
On day 14, the majority of subjects in both groups were free from
symptoms, but difference in the two groups was also not statistically
significant (P 0.057).
Table 3 reports the observation of symptoms after 3, 7, and 14
days of treatment. There was improvement in symptoms in each group,
but there were no statistically significant differences between the two
groups.
Table 4 shows the incidence of side effects after 3, 7, and 14 days
of treatment. There were significant differences between the two groups
after 3 days and 7 days of treatment. Headaches were more frequently
present in the loratadine group compared to the cetirizine group (day 3, P
0.01 and day 7, P 0.03). In addition, at 7 days, we observed more
palpitations in the loratadine group than in the cetirizine group (P 0.04).
You might also like
- (ENGLISH) Perbandingan Khasiat Cetirizine Dan LoratadinDocument9 pages(ENGLISH) Perbandingan Khasiat Cetirizine Dan Loratadinintan nabilah pratiwiNo ratings yet
- Efficacy of Cetirizine vs Loratadine for Allergic Rhinitis in Children (39Document9 pagesEfficacy of Cetirizine vs Loratadine for Allergic Rhinitis in Children (39intan nabilah pratiwiNo ratings yet
- MizolastineDocument6 pagesMizolastineSemeen Samreen100% (1)
- The Efficiency and Safety of Olopatadine Against Rupatadine in Chronic Urticaria of Idiopathic Origin: A Comparative StudyDocument6 pagesThe Efficiency and Safety of Olopatadine Against Rupatadine in Chronic Urticaria of Idiopathic Origin: A Comparative StudyArezoo JamNo ratings yet
- Antipsychotics in ProdromeDocument3 pagesAntipsychotics in ProdromeTejus Murthy A GNo ratings yet
- 201105loratadine and Desloratadine Use in ChildrenDocument4 pages201105loratadine and Desloratadine Use in ChildrenGavril Diana AlexandraNo ratings yet
- Clinical Comparison of The Efficacy of Spirulina Platensis and Cetirizine For Treatment of Allergic RhinitisDocument6 pagesClinical Comparison of The Efficacy of Spirulina Platensis and Cetirizine For Treatment of Allergic RhinitisfelitaNo ratings yet
- Pediatric Theophylline StudyDocument1 pagePediatric Theophylline StudyElaine M. GeorgeNo ratings yet
- Intranasal Corticosteroids Benefit Acute SinusitisDocument9 pagesIntranasal Corticosteroids Benefit Acute Sinusitisindry_purnamasari0% (1)
- Efficacy and Safety of Azelastine and Levocetirizine in Allergic RhinitisDocument5 pagesEfficacy and Safety of Azelastine and Levocetirizine in Allergic RhinitisRiskaaNo ratings yet
- Aerius Syrup PIDocument9 pagesAerius Syrup PITerrence LiNo ratings yet
- Hearing Loss in Patients Using Isotretinoin: Is It A Side Effect or Due To Hyperlipidemia?Document5 pagesHearing Loss in Patients Using Isotretinoin: Is It A Side Effect or Due To Hyperlipidemia?Ajshe ÇekanNo ratings yet
- Epidemiology and Drug Allergy Results in Children Investigated in Allergy Unit of A Tertiary-Care Paediatric Hospital SettingDocument13 pagesEpidemiology and Drug Allergy Results in Children Investigated in Allergy Unit of A Tertiary-Care Paediatric Hospital SettingOliva Hernández Carla MailynNo ratings yet
- Controlled Trial Lansoprazole For Children With Poorly Controlled Asthma: A RandomizedDocument4 pagesControlled Trial Lansoprazole For Children With Poorly Controlled Asthma: A RandomizedJames HollandNo ratings yet
- Genetic EngineeringDocument4 pagesGenetic EngineeringSanam BangashNo ratings yet
- Mild Persistent Asthma JournalDocument6 pagesMild Persistent Asthma JournalMohammed Ramzy GhifariNo ratings yet
- Ajp.161.10.1837 2Document11 pagesAjp.161.10.1837 2HKANo ratings yet
- Comparison of Depression, Anxiety and Life Quality in Acne Vulgaris Patients Who Were Treated With Either Isotretinoin or Topical AgentsDocument6 pagesComparison of Depression, Anxiety and Life Quality in Acne Vulgaris Patients Who Were Treated With Either Isotretinoin or Topical AgentsFii Fathayati PutriNo ratings yet
- Methotrexate For Treatment of Atopic Dermatitis in Children and AdolescentsDocument5 pagesMethotrexate For Treatment of Atopic Dermatitis in Children and AdolescentsYossy VesriNo ratings yet
- Comparison of Loratadine and Cetirizine in Perennial Allergic RhinitisDocument5 pagesComparison of Loratadine and Cetirizine in Perennial Allergic RhinitisRiskaaNo ratings yet
- Comparative Study To Assess Clinical Efficacy of Leukotriene Receptor Antagonists and Antihistamines in The Treatment of Allergic RhinitisDocument8 pagesComparative Study To Assess Clinical Efficacy of Leukotriene Receptor Antagonists and Antihistamines in The Treatment of Allergic Rhinitisika safitriNo ratings yet
- Case Study3Document9 pagesCase Study3tviacrucisNo ratings yet
- Loratadine vs Cetirizine for Somnolence and MotivationDocument10 pagesLoratadine vs Cetirizine for Somnolence and MotivationJericho ImmanuelaNo ratings yet
- DocumentDocument5 pagesDocumentAnonymous V7hQNxplXNo ratings yet
- Effect of Oral Vitamin E On Atopic DermatitisDocument4 pagesEffect of Oral Vitamin E On Atopic DermatitisYusufTaqwaMuladiNo ratings yet
- Quality of Life in Patients With Persistent Allergic Rhinitis Treated With Montelukast Alone or in Combination With Levocetirizine or DesloratadineDocument7 pagesQuality of Life in Patients With Persistent Allergic Rhinitis Treated With Montelukast Alone or in Combination With Levocetirizine or DesloratadineNurani AtikasariNo ratings yet
- Assessment of Synthetic Glucocorticoids in Asthmatic SputumDocument3 pagesAssessment of Synthetic Glucocorticoids in Asthmatic SputumDewiRahmatikaNo ratings yet
- Milk Oral Immunotherapy Is Effective in School-Aged ChildrenDocument6 pagesMilk Oral Immunotherapy Is Effective in School-Aged ChildrenAnry UmarNo ratings yet
- Levotiroxina Brigitte NygaardDocument6 pagesLevotiroxina Brigitte NygaardAntonio SanchezNo ratings yet
- Group 5 Pubmed Accepted Results PDFDocument683 pagesGroup 5 Pubmed Accepted Results PDFDnyanesh LimayeNo ratings yet
- Intranasal corticosteroids relieve sinusitis symptomsDocument9 pagesIntranasal corticosteroids relieve sinusitis symptomsagustinadianasariaguNo ratings yet
- Jurnal Referat 10Document6 pagesJurnal Referat 10Ferdy BahasuanNo ratings yet
- Olanzapine For The Prevention of Chemotherapy-Induced Nausea and VomitingDocument9 pagesOlanzapine For The Prevention of Chemotherapy-Induced Nausea and VomitingAdina NeagoeNo ratings yet
- Efficacy of Nebulised Epinephrine Versus Salbutamol in Hospitalised Children With BronchiolitisDocument4 pagesEfficacy of Nebulised Epinephrine Versus Salbutamol in Hospitalised Children With BronchiolitisFiaz medicoNo ratings yet
- Out (9) Jurnal KulkelDocument8 pagesOut (9) Jurnal KulkelFelisiana KasmanNo ratings yet
- Glenmark Remo+Teneli MS D1 (17082021)Document13 pagesGlenmark Remo+Teneli MS D1 (17082021)Bhavani KirthiNo ratings yet
- Clinical Profile of Severe Cutaneous Drug EruptionsDocument4 pagesClinical Profile of Severe Cutaneous Drug EruptionsAndriHernadiNo ratings yet
- Paediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva SusantiDocument6 pagesPaediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva SusantiharnizaNo ratings yet
- OiutDocument11 pagesOiutPrasetiyo WilliamNo ratings yet
- Intranasal Corticosteroids for Acute Sinusitis SymptomsDocument9 pagesIntranasal Corticosteroids for Acute Sinusitis SymptomsBudi KhangNo ratings yet
- Clozapine Alone Versus Clozapine and Risperidone With Refractory SchizophreniaDocument11 pagesClozapine Alone Versus Clozapine and Risperidone With Refractory SchizophreniawardahNo ratings yet
- Pi is 1081120622006536Document11 pagesPi is 1081120622006536Niken KuncorowatiNo ratings yet
- Paediatric TB Treatment LandscapeDocument11 pagesPaediatric TB Treatment Landscapegiant nitaNo ratings yet
- Efficacy of Topical Retinoic Acid Compared With Topical Triamcinolone Acetonide in The Treatment of Oral Lichen PlanusDocument6 pagesEfficacy of Topical Retinoic Acid Compared With Topical Triamcinolone Acetonide in The Treatment of Oral Lichen PlanusPorcupine TreeNo ratings yet
- 2ARandomizedControlledVol24No2 3june Sep2006P97Document7 pages2ARandomizedControlledVol24No2 3june Sep2006P97I Made AryanaNo ratings yet
- Jufe 3 10.30Document38 pagesJufe 3 10.30LíaNo ratings yet
- Two Cases of Recurrent ADIH in ChildrenDocument6 pagesTwo Cases of Recurrent ADIH in ChildrenTry Ahmad MirzaNo ratings yet
- 10 1111@jcpt 13177Document8 pages10 1111@jcpt 13177opanocayNo ratings yet
- Childhood Nephrotic Syndrome in TurkeyDocument4 pagesChildhood Nephrotic Syndrome in TurkeyDrago BakovicNo ratings yet
- Off-Label Prescribing For Allergic Diseases in Pre-School ChildrenDocument6 pagesOff-Label Prescribing For Allergic Diseases in Pre-School ChildrenrizkaNo ratings yet
- Association of Food and Drug Allergy With Anti-Tuberculosis Drug Related Hepatitis or Skin Reactions: A Case Control StudyDocument6 pagesAssociation of Food and Drug Allergy With Anti-Tuberculosis Drug Related Hepatitis or Skin Reactions: A Case Control StudyPutri YingNo ratings yet
- Allergen Immunotherapy Expert ExchangeDocument4 pagesAllergen Immunotherapy Expert ExchangeAnna LiachenkoNo ratings yet
- Ijerph 12 10984 v2Document11 pagesIjerph 12 10984 v2Nurjanah PutriNo ratings yet
- Open Study On Ef Cacy and Tolerability of Cipro Oxacin XR Compared With Cipro Oxacin BID in The Treatment of Typhoid FeverDocument5 pagesOpen Study On Ef Cacy and Tolerability of Cipro Oxacin XR Compared With Cipro Oxacin BID in The Treatment of Typhoid FeverLia Devi AnisaNo ratings yet
- Journal 2 Steven Hartanto Kurniawan - A Comparative Study To Assess The Efficacy of Fluticasone and Mometasone in Allergic RhinitisDocument5 pagesJournal 2 Steven Hartanto Kurniawan - A Comparative Study To Assess The Efficacy of Fluticasone and Mometasone in Allergic Rhinitissteven hkNo ratings yet
- Drug Hypersensitivity17211Document6 pagesDrug Hypersensitivity17211sanasharNo ratings yet
- Journal ClubDocument63 pagesJournal Clubdrkadiyala2No ratings yet
- General Practice: Are Antibiotics Indicated As Initial Treatment For Children With Acute Otitis Media? A Meta-AnalysisDocument5 pagesGeneral Practice: Are Antibiotics Indicated As Initial Treatment For Children With Acute Otitis Media? A Meta-AnalysisJuan Carlos Aguayo RomeroNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 13: DermatologyFrom EverandComplementary and Alternative Medical Lab Testing Part 13: DermatologyRating: 5 out of 5 stars5/5 (4)
- Sari Gunawan, Skm. Msi: Admen UKPDocument1 pageSari Gunawan, Skm. Msi: Admen UKPRully Febri AnggoroNo ratings yet
- Icd X (10) Ruang Kb/Kia Puskesmas Ri Penengahan 2019Document1 pageIcd X (10) Ruang Kb/Kia Puskesmas Ri Penengahan 2019Rully Febri AnggoroNo ratings yet
- Raphael Guzman PublikationslisteDocument14 pagesRaphael Guzman PublikationslisteRully Febri AnggoroNo ratings yet
- Konjungtivitis Ringan EnglishDocument4 pagesKonjungtivitis Ringan EnglishRully Febri AnggoroNo ratings yet
- Accjurnal PDFDocument10 pagesAccjurnal PDFRully Febri AnggoroNo ratings yet
- BlefaritisDocument7 pagesBlefaritisRully Febri Anggoro100% (1)
- AnemiaDocument3 pagesAnemiaRully Febri AnggoroNo ratings yet
- Accjurnal PDFDocument10 pagesAccjurnal PDFRully Febri AnggoroNo ratings yet
- Blefaritis ENGLISHDocument6 pagesBlefaritis ENGLISHRully Febri AnggoroNo ratings yet
- BlefaritisDocument7 pagesBlefaritisRully Febri Anggoro100% (1)
- Jurnal MetoclorpamideDocument6 pagesJurnal MetoclorpamideRully Febri AnggoroNo ratings yet
- Konjungtivitis AlergicDocument5 pagesKonjungtivitis AlergicRully Febri AnggoroNo ratings yet
- LicenseDocument1 pageLicenseEmiliano PachecoNo ratings yet
- BanquoDocument29 pagesBanquoTree LeavesNo ratings yet
- (ENGLISH) Early Initiation of Breastfeeding at Dustira HospitalDocument6 pages(ENGLISH) Early Initiation of Breastfeeding at Dustira HospitalRully Febri AnggoroNo ratings yet
- AutismDocument3 pagesAutismRully Febri AnggoroNo ratings yet
- Ketorolac vs. TramadolDocument5 pagesKetorolac vs. TramadolRully Febri AnggoroNo ratings yet
- Farmakoterapi Tuberculosis TBCDocument30 pagesFarmakoterapi Tuberculosis TBCRizal PrasetyaNo ratings yet
- Hotel Design Planning and DevelopmentDocument30 pagesHotel Design Planning and DevelopmentTio Yogatma Yudha14% (7)
- The Bloodless GospelDocument7 pagesThe Bloodless GospelKJVNo ratings yet
- Little Book of Effective WritingDocument44 pagesLittle Book of Effective Writingshalashvili100% (1)
- JR Hydraulic Eng. Waterways Bed Protection Incomat BelfastDocument2 pagesJR Hydraulic Eng. Waterways Bed Protection Incomat Belfastpablopadawan1No ratings yet
- The Life and Works of Jose RizalDocument20 pagesThe Life and Works of Jose RizalBemtot Blanquig100% (1)
- E PortfolioDocument76 pagesE PortfolioMAGALLON ANDREWNo ratings yet
- WA Beretta M92FS Parts ListDocument2 pagesWA Beretta M92FS Parts ListDenis Deki NehezNo ratings yet
- OROLO & W. D. GannDocument56 pagesOROLO & W. D. GannGaurav Garg100% (1)
- Overview for Report Designers in 40 CharactersDocument21 pagesOverview for Report Designers in 40 CharacterskashishNo ratings yet
- Understand Azure Event HubsDocument12 pagesUnderstand Azure Event HubselisaNo ratings yet
- Where On Earth Can Go Next?: AppleDocument100 pagesWhere On Earth Can Go Next?: Applepetrushevski_designeNo ratings yet
- AJK Newslet-1Document28 pagesAJK Newslet-1Syed Raza Ali RazaNo ratings yet
- Ipo Exam Revised SyllabusDocument1 pageIpo Exam Revised Syllabusজ্যোতিৰ্ময় বসুমতাৰীNo ratings yet
- Arduino Nano based K1EL Winkeyer compatible CW contest keyerDocument35 pagesArduino Nano based K1EL Winkeyer compatible CW contest keyerSreejith SreedharanNo ratings yet
- Critique On A Film Director's Approach To Managing CreativityDocument2 pagesCritique On A Film Director's Approach To Managing CreativityDax GaffudNo ratings yet
- Drypro832 PreInstallGude 0921YH220B 070627 FixDocument23 pagesDrypro832 PreInstallGude 0921YH220B 070627 FixRicardoNo ratings yet
- Trove Research Carbon Credit Demand Supply and Prices 1 June 2021Document51 pagesTrove Research Carbon Credit Demand Supply and Prices 1 June 2021Ceren ArkancanNo ratings yet
- Marksmanship: Subject: III. Definition of TermsDocument16 pagesMarksmanship: Subject: III. Definition of TermsAmber EbayaNo ratings yet
- Khaton Prayer BookDocument47 pagesKhaton Prayer BookKarma TsheringNo ratings yet
- The Rich Hues of Purple Murex DyeDocument44 pagesThe Rich Hues of Purple Murex DyeYiğit KılıçNo ratings yet
- Compare and Contrast High School and College EssayDocument6 pagesCompare and Contrast High School and College Essayafibkyielxfbab100% (1)
- Zhihua Yao - Dignaga and The 4 Types of Perception (JIP 04)Document24 pagesZhihua Yao - Dignaga and The 4 Types of Perception (JIP 04)Carlos Caicedo-Russi100% (1)
- The Polynesians: Task1: ReadingDocument10 pagesThe Polynesians: Task1: ReadingHəşim MəmmədovNo ratings yet
- EE-434 Power Electronics: Engr. Dr. Hadeed Ahmed SherDocument23 pagesEE-434 Power Electronics: Engr. Dr. Hadeed Ahmed SherMirza Azhar HaseebNo ratings yet
- Turbine 1st Stage Nozzle - DPTDocument15 pagesTurbine 1st Stage Nozzle - DPTAnonymous gWKgdUBNo ratings yet
- Class 9th Chemistry Unit#4 Structure of MoleculesDocument8 pagesClass 9th Chemistry Unit#4 Structure of MoleculesIrfanullahNo ratings yet
- Rakpoxy 150 HB PrimerDocument1 pageRakpoxy 150 HB Primernate anantathatNo ratings yet
- StsDocument10 pagesStsSamonte, KimNo ratings yet
- Mechanical Questions & AnswersDocument161 pagesMechanical Questions & AnswersTobaNo ratings yet
- Mba Project GuidelinesDocument8 pagesMba Project GuidelinesKrishnamohan VaddadiNo ratings yet