Professional Documents
Culture Documents
Review: Cardio Vascular Complication of Diabetes Mellitus
Uploaded by
novia khairulbariaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Review: Cardio Vascular Complication of Diabetes Mellitus
Uploaded by
novia khairulbariaCopyright:
Available Formats
Journal of Applied Pharmaceutical Science 01 (04); 2011: 01-06
ISSN: 2231-3354
Received: 01-06-2011
Revised on: 04-06-2011
Accepted: 10-06-2011
Review: Cardio vascular complication of Diabetes
Mellitus
Chintan A. Patel, Nimish L Pathak, Nayana Bhatt, Bhavna Marya,
Mahendra Gavania and Hardik Trivedi
ABSTRACT
Chintan A. Patel, Nimish L pathak,
Nayana Bhatt, Bhavna Marya,
Mahendra Gavania and Hardik trivedi
Department of Pharmacology,
C.U.Shah College of Pharmacy and
Research,
Wadhwan-Surendranagar, ,India.
Now day diabetes is very common world wild disease. Basically two type of diabetes:
Type-I and Type-II. Various short term complications like diabetec ketoacidosis, hyperosmolar
nonketotic coma and hypoglycemia and long term complication like diabetec neuropathy,
diabetec retinopathy, diabetec nepheropathy, diabetec microangiopathy, heart disease and stroke
occur due to diabetes mellitus. Cardiovascular complication mainly occurs by either increase of
glucose by activation of protein kinase, rennin angeotensin system, advance glycation endproduct theory i.e. AGE-RAGE or by metabolic syndrome and insulin resistance mechanism
which precipitates obesity, physical inactivity and genetic susceptibility. Insulin secretion is
decreases with advancing age which may be accelerate by genetic factor. Insulin resistance led
to onset of Type-II diabetes mellitus and is commonly associated with other cardio vascular risk
factors like dysbetalipidema, hypertension and prothombic factor. Evaluation of these major risk
factors is very necessary. Predisposing risk factors are body weight and fat distribution in the
body, physical activity and family history. Detection of clinical and sub clinical cardiovascular
disease in diabetic patient. Evaluation of factor such as a stress testing for coronary heart
disease, non-invasive evaluation of cardiac function, evaluation of autonomic dysfunction,
detection of sub clinical cardio vascular disease and it treated by changing life style or by using
insulin matrix.
Key words: Complications, Mechanism, Various systems play role in this mechanism,
Management, insulate matrix.
INTRODUCTION
Diabetes Mellitus
Diabetes mellitus is a disorder in which the body is unable to metabolize carbohydrates
properly. The disease is characterized by excessive amounts of sugar in the blood and urine;
inadequate production and/or utilization of insulin; and by thirst, hunger and loss of weight (Rang
et al., 1999).
*For Correspondence:
Chintan A Patel
Email:
chintan.pharma.2007@gmail.com
Complications of Diabetes Mellitus
Diabetic complications are of two types, they are short term complication and long term
complication. Short term complications are like diabetic ketoacidosis, hyperosmolar non ketotic
coma and hypoglycemia (Charles et al., 2010; Goodman et al., 2006). Long term complications are
like diabetic nephropathy, diabetic retinopathy, diabetic micro angiopathy, diabetic neuropathy,
heart disease stroke and Arteriosclerosis. Prevalence of diabetes mellitus is much higher in Asian
countries then European countries. One fourth to one half of patients with diabetes develop cardio
vascular complication. An approximately 58.9% to 77.8% of all diabetics will develop evidence of
cardio vascular complication. There are different types of cardio vascular complications in
Journal of Applied Pharmaceutical Science 01 (04); 2011: 01-06
in diabetics are Atherosclerotic chronic heart disease, diabetic
cardiomyopathy, stroke and renal disease.
Mechanism Involved In Cardiovascular Complication
Increase of glucose
Glucose is the main cause for micro vascular
complications of diabetes like retinopathy, nephropathy and
neuropathy. The negative role of hyperglycemia on endothelial
functions and pathological changes occurring in diabetes is well
established. There are four major molecular signaling mechanisms
activated by hyperglycemia in endothelial cells (Imenta et al.,
1995). These include,
1.
2.
3.
4.
Activation of PKC
Increased hexosamine pathway flux
Increased advanced glycation end product formation and
Increased polyol pathway flux.
Most cardiovascular risk factors are affected directly by
an acute increase of glycemia in individuals with diabetes and are
modified in the postprandial phase. LDL oxidation in diabetes is
related to metabolic control (Tsai et al., 1994) and it has been
shown in type 2 diabetic patients that after meals, LDL oxidation
increases (Tsai et al., 1994) and that this phenomenon is in strict
relationship with the degree of hyperglycemia (Enkins et al., 1996).
Endothelial function is altered early in diabetes. It has been
demonstrated that in diabetic subjects, the vasodilating response to
stimuli is diminished and that this anomaly is related to glycemic
control (Diwadkar et al., 1999). In vivo studies have demonstrated
that hyperglycemic spikes induce, in both diabetic and normal
subjects, an endothelial dysfunction (Ceriello et al., 1999).
postprandial hyperglycemia (Marfella et al., 1995). The possible
role of hyperglycemia in the activation of blood coagulation has
previously been reviewed (Kawano et al., 1999). It emerges that
acute glycemic variations are matched with a series of alterations
of coagulation that are likely to cause a thrombosis. This tendency
is documented by studies demonstrating that when hyperglycemia
is induced, a shortening of the fibrinogen half-life (Giugliano et al.,
1997) and an increase in fibrinopeptide A (Shige et al., 1999;
Ceriello et al., 1993), in fragments of prothrombin (Jones et al.,
1979), in factor VII (Jones et al., 1985) and in platelet aggregation
(Ceriello et al., 1989) can be found in both normal and diabetic
subjects. These data indicate that during experimental
hyperglycemia, the coagulation is activated. It is interesting that it
already has been documented that in diabetic subjects, postprandial
hyperglycemia causes an overproduction of thrombin (Ceriello et
al., 1995). This phenomenon is strictly dependent on the glycemic
levels reached (Ceriello et al., 1995). Adhesion molecules regulate
the interaction between endothelium and leukocytes (Ceriello et al.,
1988). They participate in the process of atherogenesis because
their greater expression would imply an increase in the adhesion of
leukocytes (monocytes in particular) to the endothelium (Sakamoto
et al., 2000). It is well known that this is considered one of the
early stages of the process leading to atheromatous lesion. Among
the various proadhesive molecules, intracellular adhesion molecule
(ICAM)-1 has received particular interest. Increase in the
circulating form of this molecule has been demonstrated in subjects
with vascular disease (Ceriello et al., 1996) and with diabetes, with
or without vascular disease (Ruosladti et al., 1991; Lopes-Virella et
al., 1992). These increases have been considered the indication of
the activation of the atherogenic process. The soluble form of
ICAM-1 is stored in the cells and can be quickly expressed outside
them as a consequence of various stimuli. It has been demonstrated
that acute hyperglycemia in both normal and diabetic subjects is a
sufficient stimulus for the circulating level of ICAM-1 to increase,
thus activating one of the first stages of the atherogenic process
(Blann et al., 1994; Cominacini et al., 1995). The concept of
atherosclerosis as an inflammatory disease even in diabetes is now
well established (Ceriello et al., 1996). Studies support the
evidence that an acute hyperglycemia during a hyperglycemic
clamp (Ceriello et al., 1998) or in the postprandial state (Marfella
et al., 2000) can increase the production of plasma interleukin- 6,
tumor necrosis factor-, and interleukin-18 which can causes
various diabetic complication including cardio vascular disease.
Various systems play role in this mechanism
Fig 1.1: Described mechanism involved in cardio vascular complication.
This effect of hyperglycemia is probably linked with a
reduced production/bioavailability of nitric oxide (NO), since
hyperglycemia-induced endothelial dysfunction is counterbalanced
by arginine (Jorgensen et al., 1998). Furthermore, it is very
interesting that a rapid decrease of flow-mediated vasodilation has
been shown in the postprandial phase in type 2 diabetic patients
and that the decrease correlated inversely with the magnitude of
Renin angiotensin Aldosterone system
Aldosterone is a steroid hormone that is primarily
produced in the zona glomerulosa, the outer layer of the adrenal
cortex. Classical effects of aldosterone are to promote sodium
retention and potassium loss by the kidney, although it exerts
similar but lesser effects on the colon, sweat and salivary glands.
The three principal factors that regulate aldosterone secretion are
Ang II, ACTH and potassium. Changes in aldosterone secretion in
response to changes in volume status or alteration in salt intake are
Journal of Applied Pharmaceutical Science 01 (04); 2011: 01-06
mediated primarily by Ang II. Most patients with type 2 diabetes
have normal Ang II regulation of aldosterone and normal
circulating level of this hormone (Sowers et al., 1995). However, in
diabetic patients with dysautonomia, usually associated with longstanding diabetes, there may be impaired conversion of the
precursor of renin, prorenin, to renin by the diabetic kidney
(Sowers et al., 2001). Hypertension in diabetes is characterized by
reduced nitric oxide (NO)-mediated vasorelaxation, reduced
baroreflex sensitivity and enhanced sympathetic activity and
abnormalities that are promoted by aldosterone (Sowers et al.,
2001; Sacco et al., 2003; Rocha et al., 1999).
Protein kinase c (pkc)
Fig 1.4: Described overview of PKC-dependent activation and induction of eNOS
and vascular NAD(P)H oxidase (Farlane et al., 2003).
Fig 1.2: Described effects of aldosterone on the brain, heart and kidney.
Aldosterone appears to have effects on the brain, the
heart, vasculature and kidneys that lead to elevated blood pressure.
These changes include enhanced sympathetic nervous system
activity, reduced vascular compliance and endothelial-derived
vasorelaxation, increases in volume expansion, reduced serum
potassium and increases in left ventricular mass and cardiac output
(Duprez et al., 2000; The Lancet, 2000). Aldosterone antagonists
have been shown to substantially reduce blood pressure in patients
as well as in animal models with hypertension (Yee et al., 1998).
Aldosterone antagonists also appear to have considerable potential
in treating the diabetic patient with hypertension. There are data in
the stroke-prone spontaneously hypertensive rats (SHRSP),
suggesting that aldosterone antagonists may also reduce strokes.
Aldosterone and hypertension in diabetic patients
Hypertension in diabetes is characterized by reduced nitric
oxide (NO)-mediated vasorelaxation, reduced baroreflex sensitivity
and enhanced sympathetic activity and abnormalities that are
promoted by aldosterone.
Fig 1.3: Described management of cardio vascular complication
Glucose and free fatty acids stimulates PKC. PKC
through IRS-1 stimulate phosphorylation and NAD(P)H oxidase
(Griendling et al., 2000). Angiotensin II increases NAD(P)H
oxidase gene expression. Vascular cells express several catalytic
subunit isoforms, including nox2.The reactive oxygen species
theory in the diabetic state, the generation of ROS is enhanced
through the processes of glucose autoxidation, polyol pathway,
prostanoid synthesis and protein glycation (Lassegue et al., 2003;
Baynes et al., 1991). Hyperglycemia also attenuates anti-oxidative
mechanisms (Giugliano et al., 1996). ROS formed in the diabetes
associated autoxidation processes are superoxide anions, the
hydroxyl radicals and hydrogen peroxides. ROS cause lipid
peroxidation and damage proteins by chemical modifications
through cross-linking and fragmentation. Therefore, oxidative
stress has been considered to contribute to the pathological
processes of diabetic complications (Lassegue et al., 2003;
Giugliano et al., 1996).
The advanced glycation end-product theory
The glycation process, otherwise known as the Maillard
reaction, is divided into three key stages: the early reactions
resulting in the formation of base products, the rearrangements of
these chemical groups and the final reactions forming the classical
Maillard browning products or now known as AGEs (Wolff et al.,
1991). The role of AGE in vascular disease was first identified by
their ability to cross-link proteins of the vascular wall leading to
the thickening of vessels and leakage from the vasculature (Baynes
et al., 1991). Glycation of many structural and intracellular proteins
occurs through covalent and cross-linking modifications by
glucose, which may change protein conformation and permanently
impair their functions (Singh et al., 2001; Bierhaus et al., 1998).
AGEs can also alter cellular functions by binding to their receptors,
such as the receptor for AGEs (RAGE) or other receptors,
including the macrophage scavenger receptor, p60, p90 and
galectin-3. RAGE is a trasmembrane protein that belongs to the
immunoglobulin family. Upon binding to AGE-modified proteins;
RAGE initiates multiple cascades of cellular signalling pathways,
including p44/42 MAPK and PKCs, and further disrupts cellular
homeostasis.
Age-rage and diabetic complications:
It is well established that other organ systems are
strikingly susceptible to injury and dysfunction in chronic
hyperglycemia. As discussed above, human diabetic kidneys
display increased AGEs and increased expression of RAGE.
Journal of Applied Pharmaceutical Science 01 (04); 2011: 01-06
Although strictly an association, studies in animal models
suggest that blockade of the receptor is beneficial in murine
diabetes and nephropathy. Specifically, we have shown that RAGE
blockade provides benefit in diabetes-associated nephropathy in
db/db mice (Odetti et al., 1998).
Metabolic Syndrome and there are many influences that contribute
to the presence of both these disorders in the body. In essence, our
environment and lifestyles have evolved too rapidly for our bodies
to keep pace (Muller et al., 1996). We are still genetically "wired"
to thrive on the entrenched habits of our ancestors, who consumed
different, nutrient-rich foods and a diet low in carbohydrates, as
well as sustaining greater levels of movement and exercise
(Dechenes et al., 1998; Humphriss et al., 1997).
Fig 1.5: Described advanced glycation end product-receptor for advanced glycation
end products (AGE-RAGE) and a vicious cycle of cellular perturbation and tissue
injury: implications for diabetic complications.
In addition, the administration of stz triggered
albuminuria and mesangial expansion in wildtype mice; these
processes were significantly suppressed in diabetic homozygous
RAGE null mice. Consistent with findings in human diabetes, in
the mouse kidney in diabetes, podocytes were the principal RAGEexpressing cells. Intensive studies are underway to elucidate the
precise link between AGE, RAGE, and podocytes in diabetic and,
perhaps, other nephropathies, especially those characterized by
heightened oxidative stress. In other studies, the role of RAGE
blockade in the neuropathy of diabetes has been tested. Based on
the hypothesis that the activation of NF-kB was a key and critical
RAGE dependent contributing factor to the development of
diabetic nephropathy, diabetes was induced with stz in transgenic
mice in which the expression of globin transgene was under
control of an NF-kB dependent promoter. In the sciatic nerve,
diabetes was associated with 20-fold increase in the induction of globin transcripts (which was reduced strikingly with intense
insulin therapy to reduce hyperglycemia, and, thus, AGE
generation). This was inhibited fully by pretreatment of the
diabetic mice with sRAGE (Thornalley et al., 1998). To further
dissect the role of RAGE, we rendered wild-type mice and
homozygous RAGE null mice diabetic with stz. After 6 months,
mice were killed. Although sciatic nerve demonstrated increased
expression of IL-6 and activated NF-kB in the peripheral nerve of
wild-type mice, there was no up-regulation of either IL-6 or NF-kB
activation in RAGE null mice. The hot plate test was performed to
test for thermonocieception after 3 months of stz diabetes.
Treatment with sRAGE for 3 weeks completely restored pain
perception and corrected the latency time. In RAGE null mice
rendered diabetic with stz, compared to wild-type mice with
diabetes,
a
significant
protection
against
impaired
thermonocieception was observed.
Metabolic syndrome and insulin resistance
Metabolic Syndrome is a collection of risk factors that
substantially increase your chances of causing damage to your
cardiovascular system, which can lead to a heart attack or stroke
(Chisholm et al., 1997).Insulin Resistance is an underlying cause of
Fig 1.6: Describe the relationship between metabolic syndrome, insulin resistance,
hyperinsulinemia and hyperglycemia.
Some people may also have a genetic predisposition to
Insulin Resistance, while others develop the condition through high
stress and unhealthy lifestyles (Hopkins et al., 1996). Over time,
the above factors have damaged the complex ability of the body's
cells to properly utilize insulin to convert glucose to energy. This
process creates Insulin Resistance, which can cause Metabolic
Syndrome.
Fig 1.7: Describe normal cell and insulin resistant cell
The body draws its energy from a complex metabolic
process whereby food is first converted into glucose in the
bloodstream. The glucose then passes through the walls of your
cells via insulin to be converted into essential energy. Insulin
Resistance, however, desensitizes the cell wall to insulin, resulting
in most of the glucose being unable to enter and be converted into
energy. The unused glucose remains in the blood stream which
carries it to the liver. Once there, it is converted into fat and
distributed around the body via the blood stream. This process can
lead to weight gain. Insulin Resistance also causes excess levels
of insulin because the latter hormone is not being used properly.
The resulting imbalance of glucose and insulin can lay the
groundwork for Metabolic Syndrome as well as a variety of other
disorders, including Pre- and Type 2 Diabetes, plus PCOS
(Polycystic Ovarian Syndrome) - a leading cause of menstrual
irregularity and female infertility.
Journal of Applied Pharmaceutical Science 01 (04); 2011: 01-06
Management of cardio vascular complication
Evidence from randomized controlled studies is lacking,
the American Diabetes Association Consensus Development
Conference on the Diagnosis of Coronary Heart Disease in People
with Diabetes has recommended that patients with an established
coronary heart disease (CHD) history or who have had a prior
cardiac event warrant cardiac testing for risk stratification. Further,
in patients without a prior history of an event or symptoms strongly
suggesting CHD, testing for CHD is warranted in patients with the
following.
1. Typical or atypical cardiac symptoms;
2. Resting electrocardiogram suggestive of ischemia or infarction;
3. Peripheral or carotid occlusive arterial disease;
4. Sedentary lifestyle, age 35 years, and plans to begin a vigorous
exercise program (Wendt et al., 2003);
5. In addition to diabetes, two or more cardiac risk factors (total
cholesterol 3240 mg/dl, LDL cholesterol 160 mg/dl, or HDL
cholesterol <35 mg/dl; blood pressure >140/90 mmHg; smoking;
family history or premature CHD; positive microalbuminuria test).
Cardiac testing might consist of exercise stress testing, stress
perfusion imaging, stress echocardiography or catheterization. The
type of testing and need for referral to a cardiologist depend on the
severity of underlying or suspected coronary artery disease. At
present, there is no single pharmaceutical drug that can reverse the
symptoms of Metabolic Syndrome. We feel a complete system of
elements is needed to treat a major factor in causing this condition,
namely Insulin Resistance.
The Insulite Matrix
The Insulite matrix System is the first scientificallyformulated plan to address the underlying cause of Insulin
Resistance and reverse its symptoms. The Insulite System supports
your body's ability to balance glucose and insulin levels, thus
helping you lose weight, which is crucial for reversing Insulin
Resistance and Metabolic Syndrome.
1.
2.
3.
Insulin Resistance can cause hyperinsulinemia, an excess of
insulin in the blood stream and a symptom of Metabolic
Syndrome. This latter condition may result in higher levels of
LDL "bad" cholesterol that could damage the cardiovascular
system and lead to a heart attack or stroke. Reversing Insulin
Resistance is an important factor in heart disease prevention.
Insulin Resistance heightens the risk of Metabolic Syndrome
sufferers becoming Pre-Diabetic which, if neglected, can lead
to Type 2 Diabetes - an increased risk factor for
Cardiovascular Disease. Insulin Resistance can also cause high
blood pressure or hypertension, another risk factor for heart
problems.
Type 2 Diabetes can only be managed for the rest of a
Diabetic's life in the vast majority of cases and may require
daily injections of insulin. Just by itself, Type 2 Diabetes is a
seriously increased risk factor for blindness, kidney disease
and the need for amputation.
4.
Researchers have long known that people who are overweight
and suffer from Type 2 Diabetes are at greater risk of
developing Alzheimers disease and other types of dementia.
Men with Metabolic Syndrome run a greater risk of
developing prostate cancer. Because there is no single solution for
Insulin Resistance and Metabolic Syndrome you might want to
consider a multi-faceted approach. We feel that whats required to
address the issues presented by these syndromes is a complete
systematic approach, which includes nutraceuticals (vitamins,
herbs and minerals that are disease specific), a realistic exercise
program combined with nutritional guidance, advice on combating
carbohydrate addiction and a support network that will help you
change unhealthy lifestyle choices that could lead to weight loss
(Farlane et al., 2003).
REFERENCE
Baynes JW: Role of oxidative stress in development of
complications in diabetes. Diabetes. 1991; 40: 405412.
Blann AD and Collum CN: Circulating endothelial
cell/leukocyte adhesion molecules in atherosclerosis. Thromb Haemostas.
1994; 72: 151154.
Charles R and Robert E: Insulin and oral drug for diabetes
mellitus; Modern pharmacology in clinical application. 2010: 2(6); 763776.
Ceriello A, Bortolotti N, Motz E, Pieri C, Marra M, Tonutti L,
Lizzio S, Feletto F, Catone B and Taboga C:Meal-induced oxidative stress
and low density lipoprotein oxidation in diabetes, the possible role of
hyperglycemia. Metabolism. 1999: 48; 15031508.
Ceriello A, Giugliano D, Quatraro A, Dello Russo P, Marchi E
and Torella R: Hyperglycemia may determine fibrinopeptide A plasma
level increase in humans. Metabolism. 1989: 38; 11621163.
Ceriello A, Giacomello R, Stel G, Motz E, Taboga C, Tonutti L,
Pirisi M, Falleti E and Bartoli E: Hyperglycemia-induced thrombin
formation in diabetes; the possible role of the oxidative stress. Diabetes
1995: 44; .924 928.
Ceriello A, Giugliano D, Quatraro A, Dello Russo P and Torella
R: Blood glucose may condition factor VII levels in diabetic and normal
subjects. Diabetologia 1988: 31; 889891.
Ceriello A, Taboga C, Tonutti L, Giacomello R, Stel G, Motz E
and Pirisi M: Pos meal coagulation activation in diabetes mellitus; the
effect of acarbose. Diabetologia 1996: 39; 469473.
Ceriello A, Falleti E, Bortolotti N, Motz E, Cavarape A, Russo
A, Gonano F and Bartoli E: Increased circulating ICAM-1 levels in type-2
diabetic patients; the possible role of metabolic control and oxidative
stress. Metabolism 1996 : 45; 498 501.
Ceriello A, Falleti E, Motz E, Taboga C, Tonutti L, Ezsol Z,
Gonano F and Bartoli E: Hyperglycemia-induced circulating ICAM-1
increase in diabetes mellitus; the possible role of oxidative stress. Horm
Metab Res 1998: 30; 146 149.
Chisholm DJ, Campbell LV, Kraegen EW: Pathogenesis of the
insulin resistance syndrome (syndrome X). Clin Exp Pharmacol Physiol.
1997: 24;782784.
Cominacini L, Fratta Pasini A, Garbin U, Davoli A, De Santis A,
Campagnola M, Rigoni A, Zenti MG, Moghetti P and Lo Cascio V:
Elevated levels of soluble E-selectin in patients with IDDM and NIDDM;
relation to metabolic control. Diabetologia 1995: 38;11221124.
Dechenes CJ, Verchere CB, Andrikopoulos S, Kahn SE: Human
aging is associated with parallel reductions in insulin and amylin release.
Am J physiol 1998: 275;E785E791.
Diwadkar VA, Anderson JW, Bridges SR, Gowri MS and
Oelgten PR: Postprandial low density lipoproteins in type 2 diabetes are
oxidized more extensively than fasting diabetes and control samples, Proc
Soc Exp Biol Med 1999: 222;178 184.
Journal of Applied Pharmaceutical Science 01 (04); 2011: 01-06
Duprez D, De Buyzere M, Rietzschel ER and Clement DL:
Aldosterone andvascular damage; Curr Hypertens Rep 2000: 2;327334.
Enkins AJ, Klein RL, Chassereau CN, Hermayer KL and LopesVirella MF: LDL from patients with well-controlled IDDM is not more
susceptible to in vitro oxidation. 1996: 45;762767.
Farlane Mc and Sowers: Cardiovascular Endocrinology. J Clin
Endocrinol Metab, February 2003: 88(2); 516523.
Giugliano D: Circulating adhesion molecules in humans; role of
hyperglycemia and hyperinsulinemia. Circulation 2000: 101;22472251.
Giugliano D, Ceriello A and Paolisso G: Oxidative stress and
diabetic vascular complications. Diabetes Care 1996: 19; 257267.
Giugliano D, Marfella R, Coppola L, Verrazzo G, Acampora R,
Giunta R, Nappo F, Lucarelli C and DOnofrio F: Vascular effects of acute
hyperglycemia in humans are reversed by L-arginine; evidence for reduced
availability of nitric oxide during hyperglycemia.1997; 95: 17831790.
Goodman and Gilman: Pharmacological basis of therapeutics;
keto acid, 11thed, mcgraw-hill medical publishing division. (2006)1699.
Griendling KK, Sorescu D and Ushio-Fukai M: NAD(P)H
oxidase; role in cardiovascular biology and disease. Circ Res 2000:
86;494 501.
Hopkins PN, Hunt SC, Wu LL, Williams GH and Williams:
Hypertension dyslipidemia and insulin resistance; links in a chain or
spokes on a wheel? Curr Opin Lipidol. 1996: 7; 241253.
Hudson Barry I, Hofmann Marion A, Bucciarelli Loredana,
Wendt Thoralf, Moser Bernhard, Lu Yan, Qu Wu, Stern David M,
DAgati Vivette, Yan Shi Du, Yan Shi Fang,Grant Peter J and Ann Marie
Schmidt: Glycation and diabetes; The RAGE connection. Circ. Res. 1998:
37;586600.
Humphriss DB, Stewart MW, Berrish TS, Barriocanal LA,
Trajano LR, Ashworth LA, Brown MD, Miller M, PJ Avery, Alberti KG
and Walker M: Multiple metabolic abnormalities in normal glucose
tolerant relatives of NIDDM families. Diabetologia 1997: 40;1185
1190.
Imenta W, Korytkowski M, Mitrakou A., Jenssen T, YkiJarvinen H, Evron W, Dailey G and Gerich G: Pancreatic beta-cell
dysfunction as the primary genetic lesion in NIDDM; evidence from
studies in normal glucose-tolerant individuals with a first-degree NIDDM
relative. JAMA 1995: 273; 18551861.
Jones RL and Peterson CM: Reduced fibrinogen survival in
diabetes mellitus a reversible phenomenon. J Clin Invest 1979: 63;485
493.
Jones RL: Fibrinopeptide-A in diabetes mellitus, relation to
levels of blood glucose, fibrinogen disappearance and hemodynamic
changes. (1985) 836843.
Jorgensen RG, Russo L, Mattioli L and Moore WV: Early
detection of vascular dysfunction in type I diabetes. 1988: 37;292296.
Kawano H, Motoyama T, Hirashima O, Hirai N, Miyao Y,
Sakamoto T, Kugiyama K, Ogawa H and Yasue H: Hyperglycemia rapidly
suppresses flow-mediated endothelium-dependent vasodilation of brachial
artery. J Am Coll Cardiol 1999: 34; 146 154.
Lassegue B and Clempus RE: Vascular NAD(P)H oxidases;
specific features; expression; regulation. Am J Physiol Regul Integr Comp
Physiol 2003: 285; R277-R297.
Lopes-Virella MF and Virella G: Immune mechanism of
atherosclerosis in diabetes mellitus. Diabetes 1992: 41;86-91.
Marfella R, Verrazzo G, Acampora R, La Marca C, Giunta R,
Lucarelli C, Paolisso G, Ceriello A and Giugliano D: Glutathione reverses
systemic hemodynamic changes by acute hyperglycemia in healthy
subjects. Am J Physiol 268; 1995: E 1167E1173.
Muller DC, Elahi D, Tobin JD and Andres R: The effect of age
on insulin; resistance ;secretion; Semin Nephrol 1996: 16; 289-298.
Odetti P, Aragno I, Garibaldi S, Valentini S, Pronzato MA and
Rolandi R: A scanning forces microscope study; Gerontology; Role of
advanced glycation endproducts in aging collagen.1998: 187191.
Rang HP, Dale MM, Moore JM and Ritter PK : The endocrine
pancreas and the control of blood glucose, 5th ed, Livingston publication,
London. 1999:380-393.
Rocha R, Chander PN, Zuckerman A and Stier CT: Role of
aldosterone inrenal vascular injury in stroke-prone hypertensive rats.
Hypertension 1999: 33;232237.
Ruosladti E and Integrins J: Glucemia posprandial y riesgo
cardiovascular. Clin Invest 1991: 187; 15.
Sacco RL: Reducing the risk of stroke in diabetes; what have we
leant that is new? Diabetes Obes Metab 4(Suppl 1); (2002) S27S34.
Sakamoto T, Ogawa H, Kawano H, Hirai N, Miyamoto S,
Takazoe K, Soejima H, Kugiyama K, Yoshimura M and Yasu H: Rapid
change of platelet aggregability in acute hyperglycemia. Detection by a
novel laser-light scattering method. Thromb Haemos 2000: 83(3); 475-9.
Shige H, Ishikawa T, Suzukawa M, Ito T, Nakajima K, Higashi
K, Ayaori M, Tabata S, Ohsuzu F and Nakamura H: Endotheliumdependent flow-mediated vasodilation in the postprandial state in type 2
diabetes mellitus. Am J Cardiol 1999: 84(10);127- 4 A9.
Sowers JR and Epstein M: Diabetes mellitus and associated
hypertension; vascular disease and nephropathy. An update Hypertension
1995: 26;869879.
Sowers JR, Epstein M and Frohlich ED: Diabetes; hypertension
and cardiovascular disease. An update. Hypertension 2001: 37; 1051059.
The Lancet: Effects of ramipril on cardiovascular and
microvascular outcomes in people with diabetes mellitus; results of the
HOPE study and MICRO-HOPE substudy; Heart Outcomes Prevention
Evaluation Study Investigators 2000: 355; 253259.
Thornalley PJ: Cell activation by glycated proteins; AGE
receptors; receptor recognition factors and functional classification of
AGEs. Cell Mol. Biol 1998: 44; 10131023.
Tsai EC, Hirsch IB, Brunzell JD and Chait A: Reduced plasma
peroxyl radical trapping capacity and increased susceptibility of LDL to
oxidation in poorly controlled IDDM. 1994: 43;1010 1014.
Wendt TM, Tanji N, Guo J, Kislinger TR, Qu W, Lu Y,
Bucciarelli LG, Rong LL, Moser B and Markowitz GS: RAGE drives the
development of glomerulosclerosis and implicates podocyte activation in
the pathogenesis of diabetic nephropathy. Am. J. Pathol 2003: 162; 1123
1137.
Wolff SP, Jiang ZY and Hunt JV: Protein glycation; oxidative
stress in diabetes mellitus and ageing, Free Radic. Biol. Med. 1991: 10;
339352.
Yee KM and Struthers AD: Aldosterone blunts the baroreflex
response in man; Clin Sci (Lond) 1998: 95; 687692.
You might also like
- Vq40de Service ManualDocument257 pagesVq40de Service Manualjaumegus100% (4)
- Partnership Digest Obillos Vs CIRDocument2 pagesPartnership Digest Obillos Vs CIRJeff Cadiogan Obar100% (9)
- Type 2 Diabetes MellitusDocument19 pagesType 2 Diabetes MellitusFelipe Senn Guerrero100% (2)
- Hypokalemia - Consequences, Causes, and CorrectionDocument10 pagesHypokalemia - Consequences, Causes, and CorrectionWawan BwNo ratings yet
- New Microsoft Word DocumentDocument6 pagesNew Microsoft Word DocumentKawther El-FikyNo ratings yet
- Therapy of Diabetes Mellitus Using Experimental Animal ModelsDocument8 pagesTherapy of Diabetes Mellitus Using Experimental Animal ModelsRajesh KumarNo ratings yet
- Current&TX DNDocument25 pagesCurrent&TX DNdharmaNo ratings yet
- InTech-Animal Models For Study of Diabetes Mellitus PDFDocument26 pagesInTech-Animal Models For Study of Diabetes Mellitus PDFArinda Rani AstutiNo ratings yet
- Ravi Kumar PHD TheisisDocument100 pagesRavi Kumar PHD TheisissujithradeviNo ratings yet
- Definition of Diabetes Mellitus (DM)Document12 pagesDefinition of Diabetes Mellitus (DM)Romarc Owen CorpuzNo ratings yet
- Dia Care 2009 Kitabchi 1335 43crisis HiperglicemicasDocument9 pagesDia Care 2009 Kitabchi 1335 43crisis HiperglicemicassstdocNo ratings yet
- Guideline ADA 2010 in Hyperglicemia CrisisDocument9 pagesGuideline ADA 2010 in Hyperglicemia CrisisAissyiyah Nur An NisaNo ratings yet
- Diabetes and Hypertension Physiopathology and Therapeutics: Journal of Human Hypertension May 2000Document7 pagesDiabetes and Hypertension Physiopathology and Therapeutics: Journal of Human Hypertension May 2000chandra9000No ratings yet
- R VI W Li9'Ery1LqeDocument28 pagesR VI W Li9'Ery1LqeV.Bastin JeromeNo ratings yet
- Hyperglycemic CrisisDocument9 pagesHyperglycemic CrisisRoberto López MataNo ratings yet
- CHF Secondary To COPD and DM Type 2Document3 pagesCHF Secondary To COPD and DM Type 2Ma Regina Ocio PatanaNo ratings yet
- IGAN Danuyanti 1207 1215Document9 pagesIGAN Danuyanti 1207 1215felia liandaNo ratings yet
- Diabetes Dan HipertrofiDocument10 pagesDiabetes Dan HipertrofiHanif FakhruddinNo ratings yet
- Cardiac Autonomic Neuropathy in Diabetes: A Clinical PerspectiveDocument8 pagesCardiac Autonomic Neuropathy in Diabetes: A Clinical PerspectiveHandriee Oka DiputeraNo ratings yet
- Hyperglycemic Crise1Document146 pagesHyperglycemic Crise1Vincent ReyesNo ratings yet
- Type 2 Diabetes MellitusDocument24 pagesType 2 Diabetes Mellitusdr. M.F. Romdhoni100% (1)
- Diabetes Mellitus Is A Group of Metabolic Diseases Characterized byDocument67 pagesDiabetes Mellitus Is A Group of Metabolic Diseases Characterized byBivek TimalsinaNo ratings yet
- Diabetes and Its Effect On Wound Healing 20910Document12 pagesDiabetes and Its Effect On Wound Healing 20910DesyPratiwiWidjajanaNo ratings yet
- Review of Literature On Diabetes, Self-Care, Quality of Life, and Psychosocial IssuesDocument8 pagesReview of Literature On Diabetes, Self-Care, Quality of Life, and Psychosocial IssuesGitaq Tri YatmaNo ratings yet
- Management of Diabetic Ketoacidosis in AdultsDocument4 pagesManagement of Diabetic Ketoacidosis in AdultsRusida LiyaniNo ratings yet
- Diabetes Mellitus Type 2Document19 pagesDiabetes Mellitus Type 2Ann MaraeNo ratings yet
- IvonneDocument2 pagesIvonneivone_0812No ratings yet
- English Assignment Journal: Created By: Amalina Nur Fadhilah P1337420217061 IibDocument3 pagesEnglish Assignment Journal: Created By: Amalina Nur Fadhilah P1337420217061 IibAmalina Nur FadhilahNo ratings yet
- 6article PDFDocument12 pages6article PDFMillenium AyurvedaNo ratings yet
- Diabetes and Herbal Medicines: Edwin Jarald, Siddaheswar Balakrishnan Joshi Dharam Chandra JainDocument10 pagesDiabetes and Herbal Medicines: Edwin Jarald, Siddaheswar Balakrishnan Joshi Dharam Chandra JainrawanNo ratings yet
- Running Header: A Review of Type 2 Diabetes 1 A Review of Type 2 Diabetes Camille Shepherd Utah Valley UniversityDocument15 pagesRunning Header: A Review of Type 2 Diabetes 1 A Review of Type 2 Diabetes Camille Shepherd Utah Valley Universityapi-520722163No ratings yet
- Management of Diabetic Ketoacidosis.4Document7 pagesManagement of Diabetic Ketoacidosis.4boomNo ratings yet
- Research ProposalDocument9 pagesResearch ProposalAbiola IbrahimNo ratings yet
- Understanding DM and Kidney DiseaseDocument7 pagesUnderstanding DM and Kidney DiseasegitaNo ratings yet
- Eid2019 Article NewInsightsIntoTheMechanismsOf PDFDocument11 pagesEid2019 Article NewInsightsIntoTheMechanismsOf PDFStella UrdinolaNo ratings yet
- Management of HT in DNDocument23 pagesManagement of HT in DNyosefsugiNo ratings yet
- Kimmelstiel-Wilson Syndrome BDocument13 pagesKimmelstiel-Wilson Syndrome BRanela Kwinkee Pastor SalazarNo ratings yet
- Metabolic Syndrome As A Predictor of Type 2 Diabetes, and Its Clinical Interpretations and UsefulnessDocument10 pagesMetabolic Syndrome As A Predictor of Type 2 Diabetes, and Its Clinical Interpretations and UsefulnessChiranjeeviNo ratings yet
- Diabetes Emergencia Umpierrez 2016Document11 pagesDiabetes Emergencia Umpierrez 2016Nathalie GandoNo ratings yet
- Management of Diabetes and Hyperglycemia in Hospitalized Patients Endotext NCBI BookshelfDocument21 pagesManagement of Diabetes and Hyperglycemia in Hospitalized Patients Endotext NCBI Bookshelfhenry hernandezNo ratings yet
- Cetoacidosis Diabética y Estado Hiperosmolar.Document25 pagesCetoacidosis Diabética y Estado Hiperosmolar.Eduardo HernándezNo ratings yet
- The Role of Epigenetics in The Pathology of Diabetic ComplicationsDocument12 pagesThe Role of Epigenetics in The Pathology of Diabetic ComplicationsSyamsu Akbar KhairillahNo ratings yet
- Diabetes Mellitus IIDocument20 pagesDiabetes Mellitus IIMa R Dy100% (1)
- DiabetesDocument10 pagesDiabetesPoore IreneNo ratings yet
- Uji Terong UnguDocument8 pagesUji Terong Ungumuna warohNo ratings yet
- Review Article: Refeeding Syndrome: A Literature ReviewDocument7 pagesReview Article: Refeeding Syndrome: A Literature ReviewJames Cojab SacalNo ratings yet
- Korelasi Kadar Kolesterol Dengan Kejadian Diabetes Mellitus Tipe 2 Pada Laki-LakiDocument6 pagesKorelasi Kadar Kolesterol Dengan Kejadian Diabetes Mellitus Tipe 2 Pada Laki-LakiRengganis PutriNo ratings yet
- Diabetes Mellitus Type 2Document16 pagesDiabetes Mellitus Type 2Roland Jireh MarananNo ratings yet
- Diabetes Case StudyDocument6 pagesDiabetes Case StudyDavid DeegbeNo ratings yet
- Perspectives in Diabetes: Postprandial Hyperglycemia and Diabetes ComplicationsDocument7 pagesPerspectives in Diabetes: Postprandial Hyperglycemia and Diabetes ComplicationsHania Asmarani RahmanitaNo ratings yet
- Grp.10 DiabetesDocument15 pagesGrp.10 DiabetesVanessa JanneNo ratings yet
- Diabetes: Introduction and History of The Diabetes MellitusDocument6 pagesDiabetes: Introduction and History of The Diabetes Mellitusثہيہودور'ۦ شہوأنہﮩٰۧٛۗ ﮩٰۧٛNo ratings yet
- Diabetes and Cardiovascular Disease: Story of DiscoveryDocument5 pagesDiabetes and Cardiovascular Disease: Story of DiscoveryMahesh DmNo ratings yet
- Can Hypoglicemic EpisodesDocument6 pagesCan Hypoglicemic EpisodesRizki NovNo ratings yet
- Jrip 2 73Document8 pagesJrip 2 73devyNo ratings yet
- Uric Acid, The Metabolic Syndrome, and Renal DiseaseDocument4 pagesUric Acid, The Metabolic Syndrome, and Renal DiseaseraynanthaNo ratings yet
- Diabetic Ketoacidosis in Toddler With A Diaper RashDocument4 pagesDiabetic Ketoacidosis in Toddler With A Diaper RashKarl Angelo MontanoNo ratings yet
- VERNILLO Et Al PDFDocument8 pagesVERNILLO Et Al PDFJardelSantosNo ratings yet
- Discover The Best Exercises For Overall Health & Longevity - Based On The Teachings Of Dr. Andrew Huberman: The Ultimate Workout Guide For Lifelong Well-BeingFrom EverandDiscover The Best Exercises For Overall Health & Longevity - Based On The Teachings Of Dr. Andrew Huberman: The Ultimate Workout Guide For Lifelong Well-BeingNo ratings yet
- Diabetes Mellitus and Oral Health: An Interprofessional ApproachFrom EverandDiabetes Mellitus and Oral Health: An Interprofessional ApproachNo ratings yet
- 53-62 Barki S Et Al PDFDocument10 pages53-62 Barki S Et Al PDFnovia khairulbariaNo ratings yet
- Diabetes Mellitus Nair PDFDocument5 pagesDiabetes Mellitus Nair PDFWeng RamojalNo ratings yet
- Iaat14i12p644 PDFDocument8 pagesIaat14i12p644 PDFnovia khairulbariaNo ratings yet
- Contoh Karakteristik SosialekonomiDocument10 pagesContoh Karakteristik Sosialekonominovia khairulbariaNo ratings yet
- Krisis Ekonomi Terhadap Kesehatan PDFDocument8 pagesKrisis Ekonomi Terhadap Kesehatan PDFnovia khairulbariaNo ratings yet
- Diabetes Mellitus A Devastating Metabolic Disorder PDFDocument7 pagesDiabetes Mellitus A Devastating Metabolic Disorder PDFsshmitaaNo ratings yet
- The Quality of Ambulatory Care Delivered To Children in The United StatesDocument9 pagesThe Quality of Ambulatory Care Delivered To Children in The United Statesnovia khairulbariaNo ratings yet
- Cochlear Implants For Children With Severe-to-Profound Hearing LossDocument8 pagesCochlear Implants For Children With Severe-to-Profound Hearing Lossnovia khairulbariaNo ratings yet
- ATLSDocument92 pagesATLSRendi MuflihNo ratings yet
- Cochlear Implants For Children With Severe-to-Profound Hearing LossDocument8 pagesCochlear Implants For Children With Severe-to-Profound Hearing Lossnovia khairulbariaNo ratings yet
- Hipoglikemia PDFDocument12 pagesHipoglikemia PDFVhiny ChaNo ratings yet
- Nej Mic M 1002094Document1 pageNej Mic M 1002094novia khairulbariaNo ratings yet
- The Quality of Ambulatory Care Delivered To Children in The United StatesDocument9 pagesThe Quality of Ambulatory Care Delivered To Children in The United Statesnovia khairulbariaNo ratings yet
- J. Antimicrob. Chemother. 2011 Xu 1687 95Document9 pagesJ. Antimicrob. Chemother. 2011 Xu 1687 95novia khairulbariaNo ratings yet
- Nej Me 1309006Document3 pagesNej Me 1309006novia khairulbariaNo ratings yet
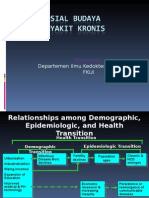
- Aspek Sosial BudayaDocument33 pagesAspek Sosial Budayanovia khairulbariaNo ratings yet
- Biaya Pengobatan Terhadap MDR PDFDocument10 pagesBiaya Pengobatan Terhadap MDR PDFnovia khairulbariaNo ratings yet
- Emergency and Disaster Risk ManagementDocument43 pagesEmergency and Disaster Risk Managementnovia khairulbariaNo ratings yet
- Emergency Care in Fammed Practice PDFDocument25 pagesEmergency Care in Fammed Practice PDFnovia khairulbariaNo ratings yet
- Hipoglikemia PDFDocument12 pagesHipoglikemia PDFVhiny ChaNo ratings yet
- Aspek Sosial BudayaDocument33 pagesAspek Sosial Budayanovia khairulbariaNo ratings yet
- Emergency and Disaster Risk ManagementDocument43 pagesEmergency and Disaster Risk Managementnovia khairulbariaNo ratings yet
- Aspek Sosial BudayaDocument33 pagesAspek Sosial Budayanovia khairulbariaNo ratings yet
- Presentation Damage Control in Thoracic SurgeryDocument44 pagesPresentation Damage Control in Thoracic Surgerynovia khairulbariaNo ratings yet
- Club FootDocument23 pagesClub FootBernard Santoso0% (2)
- Hipoglikemia PDFDocument12 pagesHipoglikemia PDFVhiny ChaNo ratings yet
- Jurnal1 PDFDocument12 pagesJurnal1 PDFnovia khairulbariaNo ratings yet
- Deteksi Dini KPDDocument52 pagesDeteksi Dini KPDMima Fatimah LuthfieNo ratings yet
- Clubfoot PresentationDocument74 pagesClubfoot Presentationnovia khairulbaria100% (2)
- Ethical Hacking IdDocument24 pagesEthical Hacking IdSilvester Dian Handy PermanaNo ratings yet
- Final SEC Judgment As To Defendant Michael Brauser 3.6.20Document14 pagesFinal SEC Judgment As To Defendant Michael Brauser 3.6.20Teri BuhlNo ratings yet
- Clinical Skills TrainingDocument12 pagesClinical Skills TrainingSri Wahyuni SahirNo ratings yet
- B-GL-385-009 Short Range Anti-Armour Weapon (Medium)Document171 pagesB-GL-385-009 Short Range Anti-Armour Weapon (Medium)Jared A. Lang100% (1)
- Actron Vismin ReportDocument19 pagesActron Vismin ReportSirhc OyagNo ratings yet
- Land CrabDocument8 pagesLand CrabGisela Tuk'uchNo ratings yet
- 4039-Texto Del Artículo-12948-3-10-20211123Document14 pages4039-Texto Del Artículo-12948-3-10-20211123Ricardo ApazaNo ratings yet
- Reference GuideDocument88 pagesReference GuideAnonymous Qm0zbNk100% (1)
- Ships Near A Rocky Coast With Awaiting Landing PartyDocument2 pagesShips Near A Rocky Coast With Awaiting Landing PartyFouaAj1 FouaAj1No ratings yet
- Creating A Research Space (C.A.R.S.) ModelDocument5 pagesCreating A Research Space (C.A.R.S.) ModelNazwa MustikaNo ratings yet
- ES Parent Bulletin Vol#19 2012 May 25Document13 pagesES Parent Bulletin Vol#19 2012 May 25International School ManilaNo ratings yet
- Investment Analysis and Portfolio Management: Frank K. Reilly & Keith C. BrownDocument113 pagesInvestment Analysis and Portfolio Management: Frank K. Reilly & Keith C. BrownWhy you want to knowNo ratings yet
- JEE Mains Paper 1 (12 Apr 2019 Shift 2) EnglishDocument131 pagesJEE Mains Paper 1 (12 Apr 2019 Shift 2) EnglishRudraksha KushwahaNo ratings yet
- Formato MultimodalDocument1 pageFormato MultimodalcelsoNo ratings yet
- Music Production EngineeringDocument1 pageMusic Production EngineeringSteffano RebolledoNo ratings yet
- Handbook of Storage Tank Systems: Codes, Regulations, and DesignsDocument4 pagesHandbook of Storage Tank Systems: Codes, Regulations, and DesignsAndi RachmanNo ratings yet
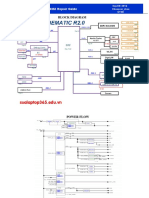
- Asus x453Document5 pagesAsus x453Rhiry Ntuh AthryNo ratings yet
- 2.ed - Eng6 - q1 - Mod3 - Make Connections Between Information Viewed and Personal ExpiriencesDocument32 pages2.ed - Eng6 - q1 - Mod3 - Make Connections Between Information Viewed and Personal ExpiriencesToni Marie Atienza Besa100% (3)
- Entrepreneurship - PPTX Version 1 - Copy (Autosaved) (Autosaved) (Autosaved) (Autosaved)Document211 pagesEntrepreneurship - PPTX Version 1 - Copy (Autosaved) (Autosaved) (Autosaved) (Autosaved)Leona Alicpala67% (3)
- Documentos de ExportaçãoDocument17 pagesDocumentos de ExportaçãoZineNo ratings yet
- Brain Injury Patients Have A Place To Be Themselves: WHY WHYDocument24 pagesBrain Injury Patients Have A Place To Be Themselves: WHY WHYDonna S. SeayNo ratings yet
- Advanced Herd Health Management, Sanitation and HygieneDocument28 pagesAdvanced Herd Health Management, Sanitation and Hygienejane entunaNo ratings yet
- NCP - Impaired Urinary EliminationDocument3 pagesNCP - Impaired Urinary EliminationFretzgine Lou ManuelNo ratings yet
- Auditing Principles and Practices-IDocument8 pagesAuditing Principles and Practices-IMoti BekeleNo ratings yet
- PCM Cables: What Is PCM Cable? Why PCM Cables? Application?Document14 pagesPCM Cables: What Is PCM Cable? Why PCM Cables? Application?sidd_mgrNo ratings yet
- Investigation Data FormDocument1 pageInvestigation Data Formnildin danaNo ratings yet
- Worksheet in Bio 102: Microbiology and Parasitology (WEEK 17)Document3 pagesWorksheet in Bio 102: Microbiology and Parasitology (WEEK 17)DELOS SANTOS JESSIECAHNo ratings yet
- Work Sample 2 - Eoc and CrucibleDocument35 pagesWork Sample 2 - Eoc and Crucibleapi-259791703No ratings yet