Professional Documents
Culture Documents
Diabetic Emergencies PDF
Uploaded by
Juan C. Salazar PajaresOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diabetic Emergencies PDF
Uploaded by
Juan C. Salazar PajaresCopyright:
Available Formats
REVIEWS
Diabetic emergencies ketoacidosis,
hyperglycaemic hyperosmolar state
and hypoglycaemia
Guillermo Umpierrez1 and Mary Korytkowski2
Abstract | Diabetic ketoacidosis (DKA), hyperglycaemic hyperosmolar state (HHS) and
hypoglycaemia are serious complications of diabetes mellitus that require prompt recognition,
diagnosis and treatment. DKA and HHS are characterized by insulinopaenia and severe
hyperglycaemia; clinically, these two conditions differ only by the degree of dehydration and the
severity of metabolic acidosis. The overall mortality recorded among children and adults with
DKA is <1%. Mortality among patients with HHS is ~10fold higher than that associated
withDKA. The prognosis and outcome of patients with DKA or HHS are determined by the
severity of dehydration, the presence of comorbidities and age >60years. The estimated annual
cost of hospital treatment for patients experiencing hyperglycaemic crises in the USA exceeds
US$2billion. Hypoglycaemia is a frequent and serious adverse effect of antidiabetic therapy that
is associated with both immediate and delayed adverse clinical outcomes, as well as increased
economic costs. Inpatients who develop hypoglycaemia are likely to experience a long duration
of hospital stay and increased mortality. This Review describes the clinical presentation,
precipitating causes, diagnosis and acute management of these diabetic emergencies, including
a discussion of practical strategies for their prevention.
Diabetic ketoacidosis (DKA), hyperglycaemic hyper HHS4,11, a rate that is ~10fold higher than that reported
osmolar state (HHS) and hypoglycaemia are frequent for DKA4,12. Similarly, hypoglycaemia is associated with
and serious complications arising among patients twofold to threefold increased mortality, particularly as
with type1 diabetes mellitus (T1DM) and type2 dia age increases and among patients who have a history
betes mellitus (T2DM). In the USA, ~145,000 cases of severe hypoglycaemic episodes13. Several studies
of DKA occur each year 1,2. The rate of hospitalization have reported that mortality in hyperglycaemic states
for HHS is lower, accounting for <1% of all diabetes- is not caused by metabolic disarray but rather reflects
related admissions3,4. The frequency of emergency room the precipitating factor 14,15. In the case of hypoglycae
visits for hypoglycaemia is similar to that reported for mia, inhospital mortality is reported as being more fre
severe hyperglycaemia1,5. Among hospitalized individu quentamong patients with spontaneous hypoglycaemia
als,hypoglycaemia is a frequent complication of ongoing than among those with insulin-induced or iatrogenic
1
Division of Endocrinology treatment for hyperglycaemia, with a reported incidence hypoglycaemia; however, these claims have been dis
and Metabolism, Emory of 528% in intensive care unit (ICU) trials (depending puted1619. Treatment of diabetic emergencies represents
University School of Medicine,
49 Jesse Hill Jr Drive,
on the intensity of glycaemic control)6, and 133% in a substantial economic burden. For example, in the
Atlanta, Georgia 30303, USA non-ICU trials using subcutaneous insulin therapy 7,8. USA, the average cost of managing DKA is US$17,500
2
Division of Endocrinology DKA, HHS and hypoglycaemia are associated with per patient, which represents a total annual hospital cost
and Metabolism, University substantial morbidity and mortality, as well as high of $2.4billion1. Similarly, hypoglycaemia is associated
of Pittsburgh, 3601
healthcare costs. DKA is the leading cause of mortality with immediate and delayed adverse clinical outcomes,
FifthAvenue, Suite 560,
Pittsburgh, Pennsylvania among children and young adults with T1DM, account as well as an increase in economic costs2022.
15213, USA. ing for ~50% of all deaths in this population9. The over This Review describes the clinical presentation, pre
Correspondence to G.U. all DKA mortality recorded in the USA is <1%1,2, but a cipitating causes, diagnosis and acute management of
geumpie@emory.edu higher rate is reported among patients aged >60years DKA, HHS and hypoglycaemia, including a discussion
doi:10.1038/nrendo.2016.15 and individuals with concomitant life-threatening of practical approaches to prevent the onset of these
Published online 19 Feb 2016 illnesses1,2,9,10. Death occurs in 516% of patients with diabetic emergencies.
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 1
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Key points insulin or other antidiabetic medications and the presence
of concomitant illnesses, such as cerebrovascular events,
Diabetic ketoacidosis (DKA) and hyperglycaemic hyperosmolar state (HHS) are myocardial infarction and trauma14,26.
serious acute metabolic complications of diabetes mellitus, representing points along
a spectrum of hyperglycaemic emergencies caused by poor glycaemic control Pathophysiology
DKA comprises hyperglycaemia, hyperketonaemia and metabolic acidosis; diagnostic Both DKA and HHS result from absolute or relative
criteria for HHS include a plasma glucose level >33.3mmol/l, serum osmolality insulin deficiency in association with increased circulat
>320mmol/kg and no appreciable metabolic acidosis and ketonaemia
ing levels of glucagon and other counter-regulatory hor
Management objectives for DKA and HHS include restoration of circulatory volume mones (catecholamines, cortisol and growth hormone),
and tissue perfusion; correction of hyperglycaemia, ketogenesis and electrolyte
all of which oppose the action of any residual circulating
imbalance; and identification and treatment of the precipitating event
insulin14,26. This hormonal milieu promotes increased
Hypoglycaemia is defined as a blood glucose level <3.9mmol/l in both the inpatient
hepatic glucose production, decreased peripheral insulin
and outpatient settings
sensitivity and hyperglycaemia.
Severe hypoglycaemic events can negate the beneficial effects of intensive glycaemic
Severe insulin deficiency correlates with increased
management strategies that target near normoglycaemia among patients with
diabetes mellitus
activity of the hormone-sensitive lipase in adipose tis
sue, which in turn leads to the breakdown of triglycer
Patient and family education regarding the signs and symptoms of hypoglycaemia, as
ides into glycerol and high circulating levels of free fatty
well as the methods available for treatment, can effectively reduce the risk of severe
hypoglycaemic episodes acids27. In the liver, free fatty acids are oxidized to ketone
bodies, a process predominantly stimulated by glucagon28.
Increased concentrations of glucagon lower hepatic lev
DKA and HHS els of malonyl coenzymeA (CoA), the first rate-limiting
Precipitating causes enzyme in denovo fatty acid synthesis. Decreased levelsof
DKA. TABLE1 outlines the most common precipitating malonyl-CoA then stimulate the rate-limiting enzyme
causes of DKA worldwide, as determined by epidemio of ketogenesis (carnitine Opalmitoyltransferase1, liver
logical studies. In the USA and other developed nations, isoform (CPT1L)), which promotes transesterification
the most frequently reported precipitating causes are of fatty acyl carnitine and oxidation of free fatty acids to
poor adherence to insulin therapy, infection and newly ketone bodies (acetoacetate and hydroxybutyrate)29.
diagnosed diabetes mellitus. By contrast, infections and Thus, production of ketone bodies is accelerated as a
poor access to care are the most prevalent precipitating result of increased fatty acyl CoA and CPT1L activ
causes in developing nations. ity 29,30. In addition, metabolism and clearance of ketone
Drugs that affect carbohydrate metabolism, such as bodies are decreased in states of DKA. Ketone bodies are
corticosteroids, sympathomimetics and atypical anti strong acids that, when present at high levels, can cause
psychotics, might also precipitate the development of metabolic acidosis. Both hyperglycaemia and high levels
DKA1,14,23. In addition, an association has been reported of ketone bodies cause osmotic diuresis, which leads to
between the use of sodiumglucose cotransporter2 hypovolaemia and decreased glomerular filtration rate,
(SGLT2) inhibitors (a class of oral antidiabetic agents the latter of which further aggravates hyperglycaemia14.
that decrease concentrations of plasma glucose by inhib Patients with HHS are also insulin-deficient; however,
iting proximal tubular reabsorption in the kidney) and they exhibit higher insulin concentrations (demonstrated
the development of DKA among patients with T1DM by basal and stimulated Cpeptide levels) than do patients
andT2DM24,25. with DKA26,31. Furthermore, patients with HHS have lower
concentrations of free fatty acids, cortisol, growth hormone
HHS. HHS is the initial manifestation of diabetes mellitus and glucagon than do patients with DKA31. The slower
in 717% of patients; however, this complication is more onset of HHS (several days) versus DKA (<12days)
often reported in the setting of previously diagnosed dia results in more severe manifestations of hyperglycaemia,
betes mellitus14,26. Infection is the major precipitating cause dehydration and plasma hyperosmolality, all of which
in 3060% of patients with HHS, followed by omission of correlate with impaired levels of consciousness26.
Table 1 | Precipitating causes of diabetic ketoacidosis
Precipitating cause Australia115 Brazil116 China117 Indonesia118 Korea119 Nigeria120 Spain121 Syria122 Taiwan123 USA15,23
New diagnosis of 5.7 12.2 NR 3.3 NR NR 12.8 NR 18.2 17.223.8
diabetes mellitus, %
Infection, % 28.6 25.0 39.2 58.3 25.3 32.5 33.2 47.8 31.7 14.016.0
Poor adherence 40.0 39.0 24.0 13.3 32.7 27.5 30.7 23.5 27.7 41.059.6
totreatment, %
Other, % 25.7 15.0 10.9 17.1 11.2 4.8 23.3 7.8 6.2 9.718.0
Unknown, % NA 8.8 25.9 8.0 30.8 34.6 NA 20.9 16.2 3.04.2
NA, not applicable; NR, not reported.
2 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Diagnosis HHS. The diagnostic criteria for HHS include a plasma
A diagnosis of DKA or HHS should be suspected in glucose level >33.3mmol/l, an effective serum osmolality
every ill patient with hyperglycaemia. >320mmol/kg and the absence of appreciable metabolic
acidosis and ketonaemia1 (TABLE2). By contrast to the
DKA. Patients with DKA usually present within hours original formula used to estimate total serum osmolality
to days of developing polyuria, polydipsia and weight (2[Na]+[Glucose]/18+[BUN]/2.8, where [Glucose] and
loss. Nausea, vomiting and abdominal pain are detected [BUN] are measured in mg/dl)4,37, some reports and con
in 4075% of cases32. Physical examination reveals signs sensus guidelines have recommended the use of effective
of dehydration, changes in mental status, hypothermia serum osmolality (2[measured Na+ in mEq/l)]+[glu
and the scent of acetone on the patients breath. A deep cose in mmol]), not taking urea into consideration, as
laboured breathing pattern (Kussmaul respirations) is it is distributed equally in all body compartments and
observed among patients with severe metabolic acidosis. its accumulation does not induce an osmotic gradient
As outlined in TABLE2, DKA comprises a triad of across cell membranes1,14. Symptoms of encephalopathy
hyperglycaemia, hyperketonaemia and metabolic aci are usually present when serum sodium levels exceed
dosis. The condition can be classified as mild, moderate 160mmol/l and when the calculated effective osmolality
or severe, depending on the extent of metabolic acido is >320mmol/kg 15. Estimates suggest that ~2030%
sis and alterations in the sensorium or mental obtun of patients who present with HHS exhibit increased
dation. The key diagnostic criterion is an elevation in anion gap metabolic acidosis as the result of concom
the serum concentration of ketone bodies. Although itant ketoacidosis, either alone or in combination with
the majority of patients with DKA present with plasma increased serum levels of lactate.
glucose levels >16.7mmol/l, some patients exhibit only
mild elevations in plasma glucose levels (termed eugly Management at presentation
caemic DKA) after withholding or decreasing the dose Considerable variability exists in the presentation of
of insulin in the context of reduced food intake or illness. patients with DKA and HHS. FIGURE 1 outlines the
Euglycaemic DKA is also observed during pregnancy, treatment algorithm for DKA and HHS recommended
among patients with impaired gluconeogenesis owing to in the 2009 American Diabetes Association consensus
alcohol abuse or liver failure, and among patients treated statement 1. Management objectives include restoration
with SGLT2 inhibitors15,25,33. Thus, plasma glucose levels of circulatory volume and tissue perfusion, cessation of
do not determine the severity ofDKA. ketogenesis, correction of electrolyte imbalances and
Confirmation of increased ketone body production resolution of hyperglycaemia. Many patients with DKA
is performed using either the nitroprusside reaction or can be safely managed in intermediate care units unless
direct measurement of hydroxybutyrate14. The nitro they present with severe alteration of mental status or
prusside reaction provides a semiquantitative estimation with critical illnesses (for example, myocardial infarc
of acetoacetate and acetone levels in the plasma or urine, tion, gastrointestinal bleeding or sepsis) that require
but does not detect the presence of hydroxybutyrate, treatment in the ICU. The decision as to where affected
which is the predominant ketone body among patients individuals are treated is often based on the availabil
with DKA34. Although more expensive than evalua ity of adequate nursing personnel to carefully monitor
tion of urinary ketone bodies, direct measurement of the patient and to manage the insulin and intravenous
hydroxybutyrate either via a laboratory service or fluid administration required for successful resolution
through use of a pointofcare metre is the preferred of DKA. Owing to increased risk of mortality and the
option to diagnose ketoacidosis (3mmol/l), as well as presence of comorbidities, most patients with HHS are
to follow the patients response to treatment 15,35,36. treated in theICU.
Table 2 | Diagnostic criteria for diabetic ketoacidosis and hyperglycaemic hyperosmolarstate
Measure DKA HSS
Mild Moderate Severe
Plasma glucose level, mmol/l 13.9 13.9 13.9 33.3
Arterial or venous pH 7.257.30 7.007.24 <7.00 >7.30
Bicarbonate level, mmol/l 1518 1014 <10 >15
Urine or blood acetoacetate Positive Positive Positive Negative or
(nitroprusside reaction) lowpositive
Urine or blood hydroxybutyrate, mmol/l >3 >3 >3 <3
Effective serum osmolality, mmol/kg* Variable Variable Variable >320
Anion gap, mmol/l >10 >12 >12 <12
Alteration in sensorium Alert Alert or drowsy Stupor or coma Stupor or coma
Coexistence of DKA and HHS is reported in up to 30% of cases. *Defined as 2[measured Na+ (mEq/l)]+[glucose (mmol)].
Abbreviations: DKA, diabetic ketoacidosis; HHS, hyperglycaemic hyperosmolar state. 2009 American Diabetes Association.
From Diabetes Care, Vol. 32, 2009; 13351343. Modified by permission of The American Diabetes Association.
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 3
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
IV uids Insulin Potassium
Administer 0.9% NaCl IV route SC route If serum K+ is <3.3 mmol/l
at 5001,000 ml/h hold insulin and give
during the rst 12 h 1020 mmol/h of KCl
until serum K+ 3.3 mmol/l
0.1 U/kg 0.2 U/kg
IV bolus SC bolus
Evaluate corrected serum Na+
If serum K+ is >5.0 mmol/l
0.1 U/kg/h 0.2 U/kg do not give K+ but check
High Normal Low serum K+ every 2 h
IV insulin SC every
infusion 2h
0.45% NaCl 0.9% NaCl
at 250500 ml/h at 250500 ml/h
depending on depending on Check serum or capillary glucose If serum K+ is <5.0 mmol/l
state of hydration state of hydration every 12 h add 2040 mmol of KCl in
When glucose reaches ~11.113.9 mmol/l: each litre of IV uid to keep
reduce insulin to 0.1 U/kg SC every 2 h serum K+ at 45 mmol/l
to maintain glucose at 8.311.1 mmol/l
until resolution of ketoacidosis
When plasma or capillary glucose
reaches ~11.113.9 mmol/l
Change to 5% dextrose with 0.45% Transition to SC insulin when the patient is alert and can eat
NaCl until resolution of ketoacidosis* Identify and treat precipitating cause
Figure 1 | Protocol for management of adult patients with diabetic ketoacidosis and hyperglycaemic
Nature Reviews | hyperosmolar
Endocrinology
state recommended by the ADA. Treatment includes the administration of intravenous fluids to correct dehydration and
restore tissue perfusion, insulin administration to correct hyperglycaemia and increased lipolysis and ketogenesis,
andelectrolyte replacement. *Defined as a blood glucose level <13.9mmol/l, bicarbonate level >18mmol/l and arterial
orvenous pH >7.3. ADA, American Diabetes Association; IV, intravenous; SC, subcutaneous. 2009 American Diabetes
Association. From Diabetes Care, Vol. 32, 2009; 13351343. Modified by permission of The American Diabetes Association.
Fluids. Replacement of lost fluids is the critical first step Most treatment algorithms recommend adminis
in the management of both DKA and HHS38. The esti tration of an intravenous bolus dose of 0.1U/kg, fol
mated water deficit is ~100ml/kg of body weight among lowed by continuous intravenous infusion of 0.1U/kg/h
patients with DKA14 and ~100200ml/kg among patients (510U/h)1. The necessity of the initial bolus has been
with HHS26,39. The water deficit is estimated as follows: called into question by one study that demonstrated no
water deficit=(0.6)(body weight in kg)(1[corrected differences in outcomes or hypoglycaemia risk among a
sodium/140])14. Fluid therapy restores intravascular group of 157 patients who either did or did not receive
volume and renal perfusion and reduces the level of an initial insulin bolus40. Several studies have shown that
counter-regulatory hormones and hyperglycaemia. insulin administration and force hydration results in a
Isotonic saline is infused at a rate of 5001000ml/h fairly predictable decrease in plasma glucose concentra
during the first 24h, followed by the infusion of 0.9% tion at a rate of 3.66.9mmol/l/h15,41,42. The insulin rate
saline at 250500ml/h or 0.45% saline, depending on the should be decreased to 0.05U/kg/h and dextrose should
serum sodium concentration and the state of hydration14 be added to the intravenous fluids when the plasma
(BOX1). Once the plasma glucose level reaches ~11.1 glucose concentration reaches ~11.113.9mmol/l. The
13.9mosm/l, replacement fluids should contain 510% of insulin infusion rate should be adjusted to maintain a
dextrose to allow continued insulin administration until plasma glucose level of 8.311.1mmol/l until ketoacido
ketonaemia is controlled, while avoiding hypoglycaemia1. sis is resolved, as evidenced by normalization of venous
pH and anion gap. Insulin infusion should be continued
Insulin. Following the initiation of intravenous fluids, among patients with HHS until mental obtundation and
insulin administration is the next essential step in restor the hyperosmolar state are corrected.
ing cellular metabolism, reducing hepatic gluconeogen The use of subcutaneous rapid-acting insulin ana
esis and suppressing lipolysis and ketogenesis38. Insulin logues (lispro 4345 or aspart 46), administered every
administration by the intravenous, intramuscular or 12h, is as effective as the use of intravenous regular
subcutaneous routes is safe and effective for correcting human insulin among patients with uncomplicated
DKA (FIG.1). Continuous intravenous infusion of reg mildtomoderate DKA. After an initial bolus subcutane
ular human insulin is the treatment of choice among ous dose of 0.20.3U/kg, the administration of lispro or
critically ill patients and those with a reduced level of aspart (subcutaneous doses of 0.1U/kg/h or 0.2U/kg/2h)
consciousness (mentally obtunded). elicits a similar decline in glucose concentration as those
4 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Box 1 | Treatment of hyperglycaemic crises 45mmol/l1 (FIG.1). The administration of 2040mmolof
potassium per litre of fluids is sufficient for most patients;
Intravenous fluids however, lower doses are required for patients with acute
10002000ml 0.9% NaCl over 12h for prompt recovery of hypotension and/or or chronic renal failure. Among patients with serum
hypoperfusion. Switch to 0.9% saline or 0.45% saline at 250500ml/h depending upon potassium levels <3.3mmol/l, replacement should begin
serum sodium concentration. When plasma glucose level ~11.1mmol, change to
at a rate of 1020mmol/h and insulin therapy should be
dextrose in 5% saline.
delayed until the potassium level rises above 3.3mmol/l
Insulin to prevent worsening of hypokalaemia1.
Regular human insulin intravenous bolus of 0.1U/kg followed by continuous insulin
infusion at 0.1U/kg/h. When glucose level 13.9mmol/l, reduce insulin rate to
Bicarbonate. Bicarbonate infusion is rarely required in
0.05U/kg/h. Thereafter, adjust rate to maintain glucose level ~11.1mmol/l.
Subcutaneous rapid-acting insulin analogues might be an alternative to intravenous
the management of DKA. Indeed, the results of a sys
insulin in patients with mildtomoderate DKA. tematic review of 12 randomized clinical studies on
the efficacy of bicarbonate therapy in the treatment of
Potassium
severe acidaemia in DKA reported that administration
Serum potassium level >5.0mmol/l (no supplement is required); 45mmol/l (add
20mmol potassium chloride to replacement fluid); 34mmol/l (add 40mmol to
of bicarbonate offers no advantage in improving either
replacement fluid); <3mmol/l (add 1020mmol/h per hour until serum potassium level outcome or the rate of recovery of hyperglycaemia and
>3mmol/l, then add 40mmol to replacement fluid). ketoacidosis49. Bicarbonate therapy also has the poten
tial to increase the risk of hypokalaemia and cerebral
Bicarbonate
oedema1. Nevertheless, clinical guidelines recommend
Not routinely recommended. If pH <6.9, consider 50mmol/l in 500ml of 0.45% saline
over 1h until pH increases to 7.0. Do not give bicarbonate if pH 7.0. the administration of 50100mmol of sodium bicarbo
nate as an isotonic solution (in 200ml of water) among
Laboratory evaluation patients with a venous pH of 6.9 (REF.1). Patients with
Initial evaluation should include blood count; plasma glucose; serum electrolytes, urea
DKA and a venous pH >7.0 and patients with HHS
nitrogen, creatinine, serum or urine ketone bodies, osmolality; venous or arterial pH;
and urinalysis. During therapy, measure capillary glucose every 12h. Measure serum should not receive bicarbonate therapy.
electrolytes, blood glucose, urea nitrogen, creatinine and venous pH every 4h.
Phosphate. Phosphate repletion is almost never required
Transition to subcutaneous insulin
in the management of DKA as mild degrees of hypophos
Continue insulin infusion until resolution of ketoacidosis. To prevent recurrence of
ketoacidosis or rebound hyperglycaemia, continue intravenous insulin for 24h after
phataemia usually self-correct once the patient has
subcutaneous insulin is given. For patients treated with insulin before admission, restart resumed eating. The need for repletion is limited to
previous insulin regimen and adjust dosage as needed. For patients with newly patients with evidence of respiratory or cardiac distress
diagnosed diabetes mellitus, start total daily insulin dose at 0.6U/kg/day. Consider who have serum phosphate levels <0.32mmol/l. Studies
multi-dose insulin given as basal and prandial regimen. have failed to show any beneficial effect of phosphate
replacement on clinical outcome50,51. Furthermore,
aggressive phosphate therapy can be potentially hazard
achieved using the intravenous route. Once glucose ous, as indicated in case reports of children with DKA
levels reach ~13.8mmol/l, the dose of subcutaneous who developed hypocalcaemia secondary to intravenous
insulin should be reduced by half and continued at the phosphate administration52,53.
same interval until DKA resolves. Intramuscular admin
istration of insulin is also effective in the treatment of Management after resolution of DKA and HHS
DKA41,47; however, this route tends to be more painful Criteria for resolution of DKA include a plasma glucose
than subcutaneous injection and might increase the risk level <13.8mmol/l, serum bicarbonate level 18mmol/l,
of bleeding among patients receiving anticoagulation normalization of the anion gap and venous or arterial
therapy. The use of rapid-acting subcutaneous insulin pH 7.3 (REFS1,14). The resolution of HHS is indicated
analogues is not recommended for patients with severe by an effective serum osmolality <310mmol/kg and a
hypotension or those with severe DKA or HHS. No pro plasma glucose level 13.8mmol/l in a patient who has
spective randomized studies have yet compared the sub recovered mental alertness1,14.
cutaneous infusion of rapid-acting insulin analogues with The half-life of intravenous regular human insulin is
the intravenous infusion of regular human insulin among <10min; if the infusion is interrupted suddenly, patients
patients admitted to theICU. might be at risk of ketoacidosis relapse and/or rebound
hyperglycaemia. Therefore, insulin infusion should be
Potassium. Patients with DKA and HHS have a total-body continued for 24h after subcutaneous insulin is started.
potassium deficit of ~35mmol/kg 48. Despite this deficit, Transition to subcutaneous insulin should be consid
the serum potassium level measured on hospital admis ered when the patient is alert and able to tolerate food by
sion is frequently within the normal range or even elevated mouth. Patients with confirmed diabetes mellitus who
owing to the shift of intracellular potassium to the extra were treated with subcutaneous insulin before hospital
cellular compartment in the setting of hypertonicity, insu admission can resume their previous insulin regimen.
lin deficiency and acidosis. Insulin therapy lowers serum Newly diagnosed patients or adult patients who have not
potassium levels by promoting the movement of potas previously received insulin can be started at a total dose
sium back into the intracellular compartment. Potassium of 0.50.7U/kg/d1. The use of a basal bolus regimen with
replacement should, therefore, be started when the insulin analogues is preferred over the use of intermediate-
serum concentration is <5.0mmol/l to maintain a level of acting insulin (neutral protamine Hagedorn; NPH) and
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 5
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
regular human insulin1,54. A randomized study compared Hypoglycaemia
the safety and efficacy of insulin analogues and regular Hypoglycaemia is the most frequent and serious adverse
human insulin during the transition from intravenous effect of antidiabetic therapy. This complication represents
to subcutaneous administration among patients with a major barrier to achieving desired levels of glycaemic
DKA42. No differences were detected in mean daily glu control in both outpatient and inpatient settings62.
cose levels; however, 41% of patients treated with NPH
or regular human insulin had an increased rate of hypo Precipitating causes
glycaemia versus 15% in those treated with once-daily Severe hypoglycaemia occurs in ~3040% of patients
glargine or glulisine beforemeals. with T1DM and ~1030% of patients with insulin-
To avoid rebound hyperglycaemia following acute treated T2DM each year 6366. Numerous patients experi
management of DKA, one study administered the ence more than one hypoglycaemic event annually. The
long-acting insulin analogue glargine at a dose of frequency of mild hypoglycaemia is difficult to quan
0.25U/kg within 12h of initiation of intravenous insulin tify as many of these events go unreported because the
infusions. The incidence of rebound hyperglycaemia was affected individual quickly treats them. In a study based
lower in the group receiving glargine than in the control on self-report, 216 of 418 (51%) patients with T1DM
group (no glargine; 94% versus 33%; P<0.001) and there or T2DM who responded to a questionnaire reported
was no increased risk of hypoglycaemia among patients experiencing a mild hypoglycaemic event in the past
who received the insulin analogue55. year 67. The investigators did not describe these mild
events owing to concerns that some represented anxiety
Prevention of hyperglycaemic crises about hypoglycaemia rather than a true hypoglycaemic
Many cases of DKA can be avoided by improved out event. When given the definition for severe hypoglycae
patient treatment and followup programmes, as well as mia as events requiring third-party assistance, 26 of 92
by the implementation of initiatives to engage patients (28%) patients with T1DM and 55 of 326 (17%) patients
with diabetes mellitus in self-management education with T2DM reported experiencing one or more events
and adherence to self-care56,57. in the past year 67. Although this study had the limitations
The frequency of hospitalizations for DKA was associated with self-reported survey data, the estimates
reduced following diabetes education programmes, are consistent with other reports64,65.
improved followup care and access to medical advice58. A study that analysed data from two large national
Patients should be instructed on how to adjust their surveys found that hypoglycaemia accounted for more
insulin dosage during illness, emphasizing that insulin than 97,000 visits to the emergency room each year,
should never be discontinued. Patients also need to be one-third of which required hospitalization5. Insulin
informed on how to contact their healthcare providers therapy and insulin secretogogues were identified as
and how to maintain adequate fluid intake in the setting the medications most frequently associated with hypo
of hyperglycaemia14. Providing patients with T1DM with glycaemia. Sulfonylureas and insulin were reported as
instructions on the use of home monitoring of blood the agents most frequently associated with emergency
ketone body levels during illness and the management of room admissions, particularly among patients aged
persistent hyperglycaemia could enable early recognition >80years. This subgroup was fivefold more likely to
of impending ketoacidosis. require hospitalization than patients aged <80years.
The FDA and European Medicines Agency have both In a study of patients with T1DM or T2DM who
issued statements warning that treatment with SGLT2 were hospitalized at one of 29 academic medical cen
inhibitors might be associated with an increased risk of tres, 1218% of all admissions were associated with at
DKA59,60. The exact prevalence of DKA among patients least one episode of hypoglycaemia, defined as a glucose
receiving these drugs is unknown but SGLT2 inhibitors value <3.3mmol/l68. Severe hypoglycaemia, defined as a
seem to primarily affect individuals with T1DM25,61. The glucose value <2.2mmol/l, occurred in <5% of admis
estimated incidence of DKA among patients with T2DM sions7,68,69. A study comparing glycaemic data among ICU
who are receiving various SGLT2 inhibitors is 0.10.8 per patients in the pre-NICE-SUGAR (Normoglycaemia
1,000 patient-years61. Most cases of DKA occur among in Intensive Care EvaluationSurvival Using Glucose
patients with a concomitant precipitating cause (for Algorithm Regulation) versus the post-NICE-SUGAR
example, surgery, alcohol abuse, insulin-pump mal trial era observed that 7.2% and 5.9% of patient-days
function and poor adherence to insulin treatment)25,61. were associated with glucose values <3.9mmol/l, and
Increased awareness among healthcare professionals, as 0.9% and 0.7% with values <2.2mmol/l, respectively 70.
well as patient education, might facilitate early detection In the hospital setting, hypoglycaemia can occur
of DKA during SGLT2inhibitor treatment or even pre among patients with or without a history of diabetes
vent development of this diabetic emergency. Potential mellitus, as well as among those who either are or are
strategies include routine monitoring of blood and urine not receiving glucose-lowering therapies. Spontaneous
ketone bodies during acute illness, periods of starvation, hypoglycaemia has been defined as events that occur
and in the presence of hyperglycaemia. Until more infor in the absence of any glucose-lowering therapies. This
mation is available, the use of SGLT2 inhibitors should be complication might be observed among patients with
avoided during severe illness, major surgical procedures dementia, severe illness, sepsis, end-stage renal disease,
and when ketone bodies are detected despite increases cancer, or liver disease, and serves as an indicator of
in insulindose. illness severity and mortality risk16,17.
6 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Contributing factors to iatrogenic hypoglycaemia Box 2 | Factors contributing to hypoglycaemia
include age >65years, underlying renal or hepatic insuf
ficiency, long duration of diabetes mellitus, presence of Insufficient patient education
other diabetic complications, intensive glycaemic control, Medications (insulin, sulfonylureas, glinides, quinolones)
counter-regulatory hormone deficiencies, variability in Aggressive treatment protocols targeting
food intake, errors in insulin dosing, and a history of normoglycaemia
hypoglycaemia events5,21,71 (BOX2). In the hospital setting, Poor coordination of insulin administration and
use of correction insulin for bedtime hyperglycaemia fooddelivery
contributes to the risk of overnight hypoglycaemia72. Abrupt changes in nutritional intake
Abrupt discontinuation of parenteral or enteral
Diagnosis nutrition among insulin-treated patients
Several different glycaemic values have been used to Decline in renal or hepatic function
define hypoglycaemia in inpatient and outpatient set Severe illness
tings; however, the definition used by the American Tapering of steroid doses without appropriate
Diabetes Association and the Endocrine Society is any reductions in insulin
plasma glucose level <3.9mmol/l73. This value is approx Inappropriate insulin dosing
imately equivalent to the lower limit of the normal range
Counter-regulatory hormone deficiencies
for postabsorptive plasma glucose concentrations and
Impaired awareness of hypoglycaemia
represents the glycaemic threshold for activation of
glucose counter-regulatory systems among nondiabetic Dementia
individuals74,75. This definition also encompasses pub Age >65years
lished values that use venous, capillary or interstitial Sepsis
glucose levels and so provides a margin of safety when
blood glucose levels are measured with home glucose
metres or continuous glucose monitoring devices, which Questions regarding the contribution of hypogly
have variable correlation with laboratory glucosevalues. caemia to adverse cardiovascular outcomes were raised
Mild hypoglycaemia is defined as any plasma glu following publication of large clinical trials that demon
cose level 3.9mmol/l that can be self-treated. The strated no reductions in cardiovascular disease events
occurrence of a mild hypoglycaemic event does not among intensively treated patients with T2DM8891. In
usually require a visit to the emergency room; however, each of these studies, the occurrence of severe hypo
recurrent mild hypoglycaemic events increase the risk glycaemia was more frequent among the intensively
of severe hypoglycaemia, which is defined as the need treated participants (twofold to threefold) than the con
for assistance from another person to take corrective ventionally treated participants, a situation that might
action73. Severe hypoglycaemic events account for the have hampered the ability to recognize any benefit of
majority of visits to the emergency room and subsequent improved levels of glycaemic control. Severe hypoglycae
hospital admissions5. Impaired awareness of hypogly mia was associated not only with an increased incidence
caemia refers to the reduced ability of the affected indi of macrovascular events and deaths from cardiovascular
vidual to recognize a decline in glucose levels before disease but also with microvascular events and non-
the onset of neuroglycopaenic symptoms20,62,64,75. In the cardiovascular mortality 90. Whether these adverse out
hospital setting, severe hypoglycaemia has been defined comes were a direct result of hypoglycaemia, or a marker
as any plasma glucose level <2.2mmol/l, independent of underlying vulnerability, has not been established.
of altered sensorium7678. The rationale for the differ In one study, a group of patients with T2DM who
ent definitions of severe hypoglycaemia in the inpatient either had concomitant cardiovascular disease or
setting reflects the fact that hospitalized patients might whowere are at high risk of cardiovascular disease
have an impaired ability to detect or report usual were assessed using continuous electrocardiography
hypoglycaemic symptoms. Holtermonitoring in conjunction with a continuous
glucose monitoring system able to detect hypoglycae
Adverse effects mia to a level of 1.1mmol/l80. Nocturnal hypoglycaemia
Hypoglycaemia is associated with both immediate and was associated with lower glucose values, which per
delayed adverse clinical outcomes2022. Acute adverse sisted for a longer duration, than those observed with
outcomes include seizures, arrhythmias, alterations in daytime hypoglycaemia. Bradycardia, atrial arrhythmia
the level of consciousness and cardiovascular events and ventricular ectopy were more prevalent during noc
(myocardial infarction and stroke)20,62,7981. Severe out turnal (but not daytime) hypoglycaemia when compared
comes, such as brain damage and death, have also been with euglycaemia. Both daytime and nocturnal hypo
observed, usually in the setting of unrecognized severe glycaemia were associated with increased ventricular
hypoglycaemia of long duration13,62,8284. Similar to what is ectopy, which manifested primarily as an increase in
observed with hyperglycaemia, hypoglycaemia increases ventricular premature beats, with a greater increase
levels of pro-inflammatory cytokines, markers of lipid occurring during nocturnal episodes80 (FIG.2). These
peroxidation, reactive oxygen species and leukocytosis85. cardiac abnormalities are similar to those observed
Recurrent episodes of severe hypoglycaemia can increase among patients with T1DM during hypoglycaemia92.
risk of cardiovascular disease and death81,86,87. Hyperglycaemia (defined as a glucose level 15mmol/l)
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 7
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
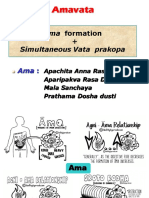
Continuous interstitial glucose and electrocardiogram monitoring with increased risk of death, although a definitive cause-
and-effect relationship could not be established. In one
Hypoglycaemia Hyperglycaemia
IG 3.5 mmol/l IG 15 mmol/l retrospective cohort study of >4,000 patients with con
firmed diabetes mellitus who were admitted to general
medical wards, both early mortality (in hospital) and late
Day Night Day Night mortality (at 1year after discharge) were higher among
VPB Transient HR VPB No arrhythmia patients who had experienced at least one hypoglycaemic
episode than those who hadnot 22.
Prolonged QTC Bradycardia Hypoglycaemic events exert adverse consequences
Atrial ectopy other than increasing cardiovascular morbidity and mor
tality. Deterioration in cognitive function, increased risk
VPB
of falls, decreased health-related quality of life, increased
Prolonged QTC absenteeism from work, decreased work productivity
and fear of hypoglycaemia have all been reported with
Figure 2 | Differential effects of daytime versus night time hypoglycaemia on deterioration in overall glycaemic control67,94,95.
Nature Reviews | Endocrinology
cardiovascular risk. Nocturnal hypoglycaemia is associated with more cardiac
arrhythmias than what is observed during daytime hypoglycaemia. Hyperglycaemia Management
wasassociated with an increased risk for VPB during the day but not overnight. HR, Clinicians must provide patients and their family with
heartrate; IG, interstitial glucose; QTc, cardiac repolarization interval; VPB, ventricular information on how to recognize and treat both mild
premature beats.
and severe hypoglycaemic events when theyoccur.
In both outpatient and inpatient settings, mild hypo
glycaemic events can be treated by oral administration of
was not associated with atrial arrhythmias or complex rapidly absorbed carbohydrate, glucose tablets or glucose
ventricular arrhythmias at any time of the day; however, gel (BOX3). Mild events can be readily treated in the out
the risk of ventricular arrhythmias was similar to that patient setting using the socalled rule of 15. This rule
observed with daytime hypoglycaemia80. recommends consuming 15g of carbohydrate; allowing
Blood pressure elevations (>180/120mmHg), 15min for absorption of nutrients and return of plasma
hypokalaemia and prolonged QT intervals on electro glucose to levels within the normal range; and repeat
cardiography, were observed in a study of 414 visits to ingglucose measurement after another 15min. Some
an emergency department for severe hypoglycaemia hypoglycaemic episodes can require 30g of carbo
(defined as the inability of the patient to self-treat)83. hydrate to restore normoglycaemia. In the inpatient set
Mean nadir plasma glucose levels were similar among ting, the introduction of nurse-directed hypoglycaemia
the 88 patients with T1DM and the 326 with T2DM (1.8 treatment protocols guide oral administration of 1530g
and 1.7mmol/l, respectively); however, cardiovascu of rapidly absorbed carbohydrate for the immediate
lar disease events and death were observed only in the treatment of any glucose level <3.9mmol/l96,97. Some
population withT2DM. institutions have incorporated hypoglycaemic treatment
Together, the findings of these studies provide evi regimens into computerized or standardized order sets
dence that hypoglycaemia contributes to cardiovascu that guide the prescribing of scheduled basal, bolus and
lar morbidity and mortality through several potential correction insulin therapy 98101.
mechanisms, such as increased sympathetic nervous Severe hypoglycaemic events that are associated with
system activation, catecholamine excess and abnormal changes in the level of consciousness require third-party
cardiac repolarization with the development of atrial assistance. All insulin-treated patients should, therefore,
and cardiac arrhythmias91,93. Other proposed mecha be provided with a glucagon kit and their family mem
nisms include increased thrombogenesis, inflamma bers, friends and coworkers educated in its use in the
tion, vasoconstriction and impaired cardiac autonomic event of severe hypoglycaemia.
function, all of which can contribute to ischaemia among In the inpatient setting, severe hypoglycaemic epi
susceptible individuals91,93. sodes among patients who are either not awake or una
The occurrence of hypoglycaemic events in the ble to ingest oral nutrition require the administration
inpatient setting has also been associated with adverse of intravenous solutions that contain dextrose. The
outcomes. Several studies have reported that sponta specific dose of oral or intravenous glucose administra
neous, but not insulin-mediated or iatrogenic, hypo tion required to resolve hypoglycaemia while avoiding
glycaemia contributes to morbidity and mortality among rebound hyperglycaemia is not clearly defined. In one
hospitalized patients16,17. By contrast, other studies have study, 54 patients experiencing hypoglycaemia associ
reported that insulin-mediated hypoglycaemia is asso ated with a decline in mental status were randomly
ciated with increased morbidity and mortality 18,19,62. In assigned to receive a 10% or 25% solution of dextrose,
one study, insulin-treated patients experiencing hypo administered in 5g aliquots of 50ml or 5ml, respec
glycaemia (glucose levels <2.8mmol/l) had a lower death tively. Doses were repeated at 1min intervals until the
rate than patients with spontaneous hypoglycaemia buta patient either regained consciousness or the maximum
higher death rate than those receiving insulin without dose of 25g was administered. Despite similar pre
a hypoglycaemic event 18. In the NICE-SUGAR study 19, treatment glucose levels, the group receiving the 10%
moderate and severe hypoglycaemias were associated dextrose solution required a median total dose of 10g,
8 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Box 3 | Prevention of hypoglycaemia in hospitalized patients Among patients with severe hypoglycaemia owing to
impaired awareness, implementation of glycaemic goals
Use of rational goal-directed insulin therapy with weight-based dosing strategies that scrupulously target avoidance of low blood glucose
Modification of insulin dosing for glucose values <5.5mmol/l levels can help restore hypoglycaemia awareness and so
Administration of dextrose-containing solutions in the event of unanticipated reduce the risk of future events64,110,111. A meta-analysis
discontinuation of enteral or parenteral nutrition among insulin-treated patients of studies that targeted interventions to restore aware
Modification of bedtime correction insulin dosing ness of hypoglycaemia symptoms and so reduce risk of
Avoid use of sulfonylureas among high-risk patients (age >65years; estimated severe hypoglycaemia among patients with T1DM con
glomerular filtration rate <45ml/min; those receiving basal insulin) cluded that patient education programmes in concert
with avoidance of intensive glycaemic targets might be
an effectiveapproach111.
whereas the group receiving the 25% dextrose solution Modification of pharmacological strategies for glycae
required a dose of 25g 102. No between-group differences mic control can also effectively reduce the frequency and
were observed in the time to resolution of mental sta severity of hypoglycaemic events. Among insulin-treated
tus changes (8min); however, post-treatment glucose patients with either T1DM of T2DM, switching to
levels were lowest among patients receiving the 10% long-acting or short-acting insulin analogues can reduce
dextrosesolution. the risk of hypoglycaemic events111. Although insu
Subcutaneous or intramuscular administration of lin analogues are more expensive than regular human
glucagon (1mg) provides an effective option for treat insulin preparations, they are particularly useful among
ment in cases where intravenous access is not immedi patients identified at high risk of hypoglycaemia74,112. For
ately available (for example, patients who are mentally patients already using insulin-analogue therapy, continu
obtunded or unable to take oral supplementation). ous subcutaneous insulin infusions, provided either alone
However, glucagon therapy is not recommended for or in combination with continuous glucose monitoring
glycogen-depleted patients, such as those with heavy devices, can reduce hypoglycaemia risk113.
alcohol use or following high levels of exercise (for For inpatients with diabetes mellitus or newly rec
example, after completing a marathon race)103. Questions ognized hyperglycaemia who are receiving glucose-
have been raised regarding the need to pretreat patients lowering therapies, glycaemic targets have been modi
with a history of heavy alcohol use or severe nutritional fied from earlier recommendations of 4.46.1mmol/l to
deficiencies with thiamine before intravenous admin 5.510.0mmol/l. This range avoids the adverse effects of
istration of glucose. This recommendation is based on uncontrolled hyperglycaemia while minimizing the risk
concern for precipitating Wernicke encephalopathy, a of hypoglycaemia7678. Modification of glucose-lowering
neurological disorder associated with delirium, oculo medications is recommended when the plasma glucose
motor dysfunction and ataxia that can be iatrogenically level declines to <5.5mmol/l7678. Weight-based insu
precipitated by glucose loading among patients with lin dosing strategies using 0.40.5U/kg/day as a total
thiamine deficiency 104. In the setting of hypoglycaemia, dailydose for basal bolus or 0.200.25U/kg/day for
correction of blood glucose is recommended as the ini basal plus insulin regimens have been demonstrated to
tial treatment, followed by early administration of intra improve glycaemic control among hospitalized patients
venous thiamine among patients suspected as being at with T2DM when compared to sliding scale insulin regi
risk of Wernicke encephalopathy 104. mens, but also increase the percentage of patients experi
Sulfonylurea-associated hypoglycaemia can be encing hypoglycaemia7,69. Reducing the total insulin dose
prolonged and severe, particularly among patients to 0.10.2U/kg/day is preferable for patients at increased
with underlying renal insufficiency 105. Use of oral risk of hypoglycaemia114. These patients include individu
and parenteral glucose administration has the poten als with lean body habitus, age >65years, renal or hepatic
tial to aggravate hypoglycaemia among patients with insufficiency, or a history of severe hypoglycaemic events.
sulfonylurea-associated hypoglycaemia as these drugs In one study, patients with T2DM and a low estimated
mediate glucose-stimulated insulin secretion. Use of glomerular filtration rate were randomly assigned to
short-acting octreotide (5075g administered subcu basal bolus insulin therapy with either glargine or glulis
taneously or intravenously) can inhibit insulin secretion ine (0.25 or 0.50U/kg/day)114. The incidence of hypogly
acutely, which negates the need for repeated doses of oral caemia among patients receiving the 0.25U/kg/day dose
or intravenous glucose while waiting for the effects of the was approximately half of that seen with the higher dose,
sulfonylurea todissipate106. without causing additional hyperglycaemic episodes.
Prevention Conclusions
Most hypoglycaemic episodes can be either prevented or DKA, HHS and hypoglycaemia are commonly encoun
limited to mild events. All patients treated with insulin or tered medical emergencies among patients with dia
an insulin secretogogue in the outpatient setting require betes mellitus. DKA and HHS are most likely to develop
education about the risk, symptoms and treatment of hypo in the outpatient setting, prompting hospital admission,
glycaemia107 (BOX3). Educational interventions that focus whereas hypoglycaemia is a frequent complication
on glucose-awareness training have substantially reduced of glucose-lowering therapy in both outpatient and
the frequency and severity of hypoglycaemic events, often inpatient settings. For patients with DKA and HHS,
without any deterioration in glycaemic control74,75,108,109. appropriate administration of intravenous fluids and
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 9
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
insulin, with attention to associated fluid and elec hypoglycaemia treatment protocols that guide immedi
trolyte disorders, can effectively and rapidly resolve ate therapy before notifying the treating physician can
the metabolic dysregulation. Hypoglycaemia also effectively offset deterioration of a mild hypoglycae
requires immediate recognition and aggressive man mic event to a severe episode with associated adverse
agement. Tailoring glycaemic goals and individualizing sequelae. Following acute management and restoration
glucose-lowering therapies according to age, presence of physiological glucose levels, DKA, HHS and hypo
of comorbidities and individual risk of hypoglycae glycaemia all require identification of the precipitat
mia, can also contribute to a lowered risk of severe ing cause to prevent these potentially life-threatening
hypoglycaemic events. In the hospital, nurse-directed diabetic complications fromrecurring.
1. Kitabchi,A.E., Umpierrez,G.E., Miles,J.M. & employees with diabetes. J.Occup. Environ. Med. 47, 42. Umpierrez,G.E. etal. Insulin analogs versus human
Fisher,J.N. Hyperglycemic crises in adult patients with 447452 (2005). insulin in the treatment of patients with diabetic
diabetes. Diabetes Care 32, 13351343 (2009). 22. Turchin,A. etal. Hypoglycemia and clinical outcomes in ketoacidosis: a randomized controlled trial. Diabetes
2. Centers for DiseaseControl and Prevention. Diabetes patients with diabetes hospitalized in the general ward. Care 32, 11641169 (2009).
data & trends. [online], http://www.cdc.gov/nchs/fastats/ Diabetes Care 32, 11531157 (2009). 43. Umpierrez,G.E. etal. Efficacy of subcutaneous insulin
inpatient-surgery.htm (2015). 23. Randall,L. etal. Recurrent diabetic ketoacidosis in lispro versus continuous intravenous regular insulin
3. Fishbein,H.A. & Palumbo,P.J. in Diabetes in America inner-city minority patients: behavioral, socioeconomic, forthe treatment of patients with diabetic ketoacidosis.
2nd edn Ch. 13 283291 (National Institutes of Health, and psychosocial factors. Diabetes Care 34, 18911896 Am. J.Med. 117, 291296 (2004).
1995). (2011). 44. Ersoz,H.O. etal. Subcutaneous lispro and intravenous
4. Pasquel,F.J. & Umpierrez,G.E. Hyperosmolar 24. Taylor,S.I., Blau,J.E. & Rother,K.I. SGLT2 inhibitors regular insulin treatments are equally effective and safe
hyperglycemic state: a historic review of the clinical may predispose to ketoacidosis. J.Clin. Endocrinol. for the treatment of mild and moderate diabetic
presentation, diagnosis, and treatment. Diabetes Care Metab. 100, 28492852 (2015). ketoacidosis in adult patients. Int. J.Clin. Pract. 60,
37, 31243131 (2014). 25. Peters,A.L. etal. Euglycemic diabetic ketoacidosis: 429433 (2006).
5. Geller,A.I. etal. National estimates of insulin-related apotential complication of treatment with sodium- 45. Karoli,R., Fatima,J., Salman,T., Sandhu,S. &
hypoglycemia and errors leading to emergency glucose cotransporter2 inhibition. Diabetes Care 38, Shankar,R. Managing diabetic ketoacidosis in non-
department visits and hospitalizations. JAMA Int. Med. 16871693 (2015). intensive care unit setting: role of insulin analogs.
174, 678686 (2014). 26. Ennis,E.D., Stahl,E.J. & Kreisberg,R.A. The IndianJ.Pharmacol. 43, 398401 (2011).
6. Krikorian,A., Ismail-Beigi,F. & Moghissi,E.S. hyperosmolar hyperglycemic syndrome. Diabetes Rev. 46. Umpierrez,G.E. etal. Subcutanbeous aspart insulin:
Comparisons of different insulin infusion protocols: a 2, 115126 (1994). asafe and cost effective treatment of diabetic
review of recent literature. Curr. Opin. Clin. Nutr. Metab. 27. Foster,D.W. & McGarry,J.D. The metabolic ketoacidosis. Diabetes 52 (Suppl.1), 584A (2003).
Care 13, 198204 (2010). derangements and treatment of diabetic ketoacidosis. 47. Sobngwi,E. etal. Evaluation of a simple management
7. Umpierrez,G.E. etal. Randomized study of basal-bolus N.Engl. J.Med. 309, 159169 (1983). protocol for hyperglycaemic crises using intramuscular
insulin therapy in the inpatient management of patients 28. McGarry,J.D. & Foster,D.W. Regulation of hepatic insulin in a resource-limited setting. Diabetes Metab.
with type2 diabetes (RABBIT2 trial). Diabetes Care 30, fatty acid oxidation and ketone body production. 35, 404409 (2009).
21812186 (2007). Ann.Rev. Biochem. 49, 395420 (1980). 48. Adrogue,H.J., Lederer,E.D., Suki,W.N. & Eknoyan,G.
8. Umpierrez,E. etal. Randomized study of basal bolus 29. McGarry,J.D., Woeltje,K.F., Kuwajima,M. & Determinants of plasma potassium levels in diabetic
insulin therapy in the inpatient management of patients Foster,D.W. Regulation of ketogenesis and the ketoacidosis. Med. (Baltimore) 65, 163172 (1986).
with type2 diabetes undergoing general surgery renaissance of carnitine palmitoyltransferase. Diabetes 49. Chua,H.R., Schneider,A. & Bellomo,R. Bicarbonate
(RABBIT2 surgery). Diabetes Care 34, 256261 Metab. Rev. 5, 271284 (1989). indiabetic ketoacidosis a systematic review.
(2011). 30. Reichard,G.A. Jr, Skutches,C.L., Hoeldtke,R.D. Ann.Intensive Care 1, 23 (2011).
9. Basu,A. etal. Persisting mortality in diabetic &Owen,O.E. Acetone metabolism in humans during 50. Fisher,J.N. & Kitabchi,A.E. A randomized study of
ketoacidosis. Diabet. Med. 10, 282284 (1993). diabetic ketoacidosis. Diabetes 35, 668674 (1986). phosphate therapy in the treatment of diabetic
10. Malone,M.L., Gennis,V. & Goodwin,J.S. 31. Gerich,J.E., Martin,M.M. & Recant,L. Clinical and ketoacidosis. J.Clin. Endocrinol. Metab. 57, 177180
Characteristics of diabetic ketoacidosis in older versus metabolic characteristics of hyperosmolar nonketotic (1983).
younger adults. J.Am. Geriatr. Soc. 40, 11001104 coma. Diabetes 20, 228238 (1971). 51. Wilson,H.K., Keuer,S.P., Lea,A.S. & Boyd,A.E. 3rd
(1992). 32. Umpierrez,G. & Freire,A.X. Abdominal pain in patients &Eknoyan,G. Phosphate therapy in diabetic
11. Bhowmick,S.K., Levens,K.L. & Rettig,K.R. with hyperglycemic crises. J.Crit. Care 17, 6367 ketoacidosis. Arch. Intern. Med. 142, 517520 (1982).
Hyperosmolar hyperglycemic crisis: an acute life- (2002). 52. Winter,R.J., Harris,C.J., Phillips,L.S. & Green, O. C.
threatening event in children and adolescents with 33. Guo,R.X., Yang,L.Z., Li,L.X. & Zhao,X.P. Diabetic Diabeticketoacidosis: induction of hypocalcemia and
type2 diabetes mellitus. Endocr. Pract. 11, 2329 ketoacidosis in pregnancy tends to occur at lower blood hypomagnesemia by phosphate therapy. Am. J.Med.
(2005). glucose levels: casecontrol study and a case report of 67, 897900 (1979).
12. Fadini,G.P. etal. Characteristics and outcomes of the euglycemic diabetic ketoacidosis in pregnancy. 53. White,N.H. Diabetic ketoacidosis in children.
hyperglycemic hyperosmolar non-ketotic syndrome in a J.Obstet. Gynaecol. Res. 34, 324330 (2008). Endocrinol. Metab. Clin. North Am. 29, 657682 (2000).
cohort of 51 consecutive cases at a single center. 34. Stephens,J.M., Sulway,M.J. & Watkins,P.J. 54. Savage,M.W. etal. Joint British Diabetes Societies
Diabetes Res. Clin. Pract. 94, 172179 (2011). Relationship of blood acetoacetate and guideline for the management of diabetic ketoacidosis.
13. McCoy,R.G. etal. Increased mortality of patients with 3hydroxybutyrate in diabetes. Diabetes 20, 485489 Diabet. Med. 28, 508515 (2011).
diabetes reporting severe hypoglycemia. Diabetes Care (1971). 55. Hsia,E. etal. Subcutaneous administration of glargine
35, 18971901 (2012). 35. Sheikh-Ali,M. etal. Can serum hydroxybutyrate be to diabetic patients receiving insulin infusion prevents
14. Kitabchi,A.E. etal. Management of hyperglycemic used to diagnose diabetic ketoacidosis? Diabetes Care rebound hyperglycemia. J.Clin. Endocrinol. Metab. 97,
crises in patients with diabetes. Diabetes Care 24, 31, 643647 (2008). 31323137 (2012).
131153 (2001). 36. Taboulet,P. etal. Urinary acetoacetate or capillary 56. Jefferies,C.A. etal. Preventing diabetic ketoacidosis.
15. Umpierrez,G.E., Kelly,J.P., Navarrete,J.E., hydroxybutyrate for the diagnosis of ketoacidosis in Pediatr. Clin. North Am. 62, 857871 (2012).
Casals,M.M. & Kitabchi,A.E. Hyperglycemic crises the emergency department setting. Eur. J.Emerg. Med. 57. Vanelli,M. etal. Effectiveness of a prevention program
inurban blacks. Arch. Intern. Med. 157, 669675 11, 251258 (2004). for diabetic ketoacidosis in children. An 8year study in
(1997). 37. Arieff,A.I. & Kleeman,C.R. Cerebral edema in diabetic schools and private practices. Diabetes Care 22, 79
16. Boucai,L., Southern,W.N. & Zonszein,J. Hypoglycemia- comas. II. Effects of hyperosmolality, hyperglycemia and (1999).
associated mortality is not drug-associated but linked to insulin in diabetic rabbits. J.Clin. Endocrinol. Metab. 58. Laffel,L. Sick-day management in type1 diabetes.
comorbidities. Am. J.Med. 124, 10281035 (2011). 38, 10571067 (1974). Endocrinol. Metab. Clin. North Am. 29, 707723
17. Kosiborod,M. etal. Relationship between spontaneous 38. Luzi,L., Barrett,E.J., Groop,L.C., Ferrannini,E. & (2000).
and iatrogenic hypoglycemia and mortality in patients DeFronzo,R.A. Metabolic effects of low-dose insulin 59. U.S. Food and Drug Administration. FDA Drug Safety
hospitalized with acute myocardial infarction. JAMA therapy on glucose metabolism in diabetic ketoacidosis. Communication: FDA warns that SGLT2 inhibitors for
301, 15561564 (2009). Diabetes 37, 14701477 (1988). diabetes may result in a serious condition of too much
18. Garg,R., Hurwitz,S., Turchin,A. & Trivedi,A. 39. CanadianDiabetes AssociationClinical acid in the blood. [online], http://www.fda.gov/Drugs/
Hypoglycemia, with or without insulin therapy, is PracticeGuidelines ExpertCommittee. Hyperglycemic DrugSafety/ucm446845.htm (2015).
associated with increased mortality among hospitalized emergencies in adults. Can. J.Diabetes 37, S72S76 60. EuropeanMedicines Agency. Review of diabetes
patients. Diabetes Care 36, 11071110 (2013). (2013). medicines called SGLT2 inhibitors started. Risk of
19. Finfer,S. etal. Hypoglycemia and risk of death in 40. Goyal,N., Miller,J.B., Sankey,S.S. & Mossallam,U. diabetic ketoacidosis to be examined. [online], http://
critically ill patients. N.Engl. J.Med. 367, 11081118 Utility of initial bolus insulin in the treatment of www.ema.europa.eu/docs/en_GB/document_library/
(2012). diabetic ketoacidosis. J.Emerg. Med. 38, 422427 Referrals_document/SGLT2_inhibitors__20/Procedure_
20. Carey,M., Boucai,L. & Zonszein,J. Impact of (2010). started/WC500187926.pdf (2015).
hypoglycemia in hospitalized patients. Curr. Diabetes 41. Kitabchi,A.E., Ayyagari,V. & Guerra,S.M. The efficacy 61. Erondu,N., Desai,M., Ways,K. & Meininger,G.
Rep. 13, 107113 (2013). of low-dose versus conventional therapy of insulin for Diabetic ketoacidosis and related events in the
21. Rhoads,G.G. etal. Contribution of hypoglycemia to treatment of diabetic ketoacidosis. Ann. Intern. Med. canagliflozin type2 diabetes clinical program.
medical care expenditures and short-term disability in 84, 633638 (1976). DiabetesCare 38, 16801686 (2015).
10 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
62. Cryer,P.E. Glycemic goals in diabetes: trade-off intheACCORD study. Diabetes Care 35, 409414 type1 diabetes: a prospective implementation study.
between glycemic control and iatrogenic hypoglycemia. (2012). Diabetologia 48, 19651970 (2005).
Diabetes 63, 21882195 (2014). 87. The AccordStudy Group. Long-term effects of intensive 110. Bott,S., Bott,U., Berger,M. & Muhlhauser,I.
63. Cryer,P. Hypoglycemia during therapy of diabetes. glucose lowering on cardiovascular outcomes. N.Engl. Intensified insulin therapy and the risk of severe
Endotext.org [online], http://www.endotext.org/ (2015). J.Med. 364, 818828 (2011). hypoglycaemia. Diabetologia 40, 926932 (1997).
64. Cryer,P.E. Hypoglycemia-associated autonomic failure 88. Miller,M.E. etal. The effects of baseline characteristics, 111. Yeoh,E., Choudhary,P., Nwokolo,M., Ayis,S. &
in diabetes: maladaptive, adaptive, or both? Diabetes glycaemia treatment approach, and glycated Amiel,S.A. Interventions that restore awareness of
64, 23222323 (2015). haemoglobin concentration on the risk of severe hypoglycemia in adults with type1 diabetes: a
65. Weinstock,R.S. etal. Severe hypoglycemia and hypoglycaemia: post hoc epidemiological analysis of the systematic review and meta-analysis. Diabetes Care 38,
diabetic ketoacidosis in adults with type 1 diabetes: ACCORD study. BMJ 340, b5444 (2010). 15921609 (2015).
results from the T1D Exchange clinic registry. J.Clin. 89. Boussageon,R. etal. Effect of intensive glucose lowering 112. Tylee,T. & Hirsch,I.B. Costs associated with using
Endocrinol. Metab. 98, 34113419 (2013). treatment on all cause mortality, cardiovascular death, different insulin preparations. JAMA 314, 665666
66. Miller,C.D. etal. Hypoglycemia in patients with type2 and microvascular events in type2 diabetes: meta- (2015).
diabetes mellitus. Arch. Intern. Med. 161, 16531659 analysis of randomised controlled trials. BMJ 343, 113. Bergenstal,R.M., Welsh,J.B. & Shin,J.J. Threshold
(2001). d4169 (2011). insulin-pump interruption to reduce hypoglycemia.
67. McCoy,R.G. etal. Self-report of hypoglycemia and 90. Zoungas,S. etal. Severe hypoglycemia and risks of N.Engl. J.Med. 369, 1474 (2013).
health-related quality of life in patients with type1 and vascular events and death. N.Engl. J.Med. 363, 114. Baldwin,D. etal. A randomized trial of two weight-
type2 diabetes. Endocr. Pract. 19, 792799 (2013). 14101418 (2010). based doses of insulin glargine and glulisine in
68. Wexler,D.J., Meigs,J.B., Cagliero,E., Nathan,D.M. 91. Fox,C.S. etal. Update on prevention of cardiovascular hospitalized subjects with type2 diabetes and renal
&Grant, R. W. Prevalenceof hyper- and hypoglycemia disease in adults with type2 diabetes mellitus in light of insufficiency. Diabetes Care 35, 19701974 (2012).
among inpatients with diabetes: a national survey of 44 recent evidence: a scientific statement from the 115. Thuzar,M., Malabu,U.H., Tisdell,B. & Sangla,K.S.
U.S. hospitals. Diabetes Care 30, 367369 (2007). American Heart Association and the American Diabetes Use of a standardised diabetic ketoacidosis
69. Umpierrez,G.E. etal. Randomized study comparing a Association. Diabetes Care 38, 17771803 (2015). management protocol improved clinical outcomes.
basal-bolus with a basal plus correction insulin regimen 92. Gill,G.V., Woodward,A., Casson,I.F. & Weston,P.J. Diabetes Res. Clin. Pract. 104, e8e11 (2014).
for the hospital management of medical and surgical Cardiac arrhythmia and nocturnal hypoglycaemia in 116. Weinert,L.S. etal. Precipitating factors of diabetic
patients with type2 diabetes: basal plus trial. Diabetes type1 diabetes the dead in bed syndrome revisited. ketoacidosis at a public hospital in a middle-income
Care 36, 21692174 (2013). Diabetologia 52, 4245 (2009). country. Diabetes Res. Clin. Pract. 96, 2934 (2012).
70. Lleva,R.R., Thomas,P., Bozzo,J.E., Hendrickson,K.C. 93. Desouza,C.V., Bolli,G.B. & Fonseca,V. Hypoglycemia, 117. Tan,H., Zhou,Y. & Yu,Y. Characteristics of diabetic
& Inzucchi,S.E. Using the glucometrics website to diabetes, and cardiovascular events. Diabetes Care 33, ketoacidosis in Chinese adults and adolescents a
benchmark ICU glucose control before and after 13891394 (2010). teaching hospital-based analysis. Diabetes Res. Clin.
theNICE-SUGAR study. J.Diabetes Sci. Technol. 8, 94. Amiel,S.A., Dixon,T., Mann,R. & Jameson,K. Pract. 97, 306312 (2012).
918922 (2014). Hypoglycaemia in type2 diabetes. Diabet. Med. 25, 118. Suwarto,S., Sutrisna,B., Waspadji,S. & Pohan,H.T.
71. Leese,G.P. etal. Frequency of severe hypoglycemia 245254 (2008). Predictors of five days mortality in diabetic ketoacidosis
requiring emergency treatment in type1 and type2 95. Feinkohl,I. etal. Severe hypoglycemia and cognitive patients: a prospective cohort study. Acta Med. Indones.
diabetes: a population-based study of health service decline in older people with type2 diabetes: the 46, 1823 (2014).
resource use. Diabetes Care 26, 11761180 (2003). Edinburgh type2 diabetes study. Diabetes Care 37, 119. Ko,S.H. etal. Clinical characteristics of diabetic
72. Kerry,C., Mitchell,S., Sharma,S., Scott,A. & 507515 (2014). ketoacidosis in Korea over the past two decades. Diabet.
Rayman,G. Diurnal temporal patterns of 96. DiNardo,M., Noschese,M., Korytkowski,M. & Med. 22, 466469 (2005).
hypoglycaemia in hospitalized people with diabetes Freeman,S. The medical emergency team and rapid 120. Edo,A.E. Clinical profile and outcomes of adult patients
may reveal potentially correctable factors. Diabet. Med. response system: finding, treating, and preventing with hyperglycemic emergencies managed at a tertiary
30, 14031406 (2013). hypoglycemia. Jt. Comm. J.Qual. Patient Saf. 32, care hospital in Nigeria. Niger. Med. J. 53, 121125
73. Seaquist,E.R. etal. Hypoglycemia and diabetes: 591595 (2006). (2012).
areport of a workgroup of the American Diabetes 97. Korytkowski,M., DiNardo,M., Donihi,A.C., Bigi,L. 121. Guisado-Vasco,P. etal. Clinical features, mortality,
Association and the Endocrine Society. J.Clin. &Devita,M. Evolution of a diabetes inpatient safety hospital admission, and length of stay of a cohort of
Endocrinol. Metab. 98, 18451859 (2013). committee. Endocr. Pract. 12 (Suppl.3), 9199 (2006). adult patients with diabetic ketoacidosis attending the
74. Seaquist,E.R. etal. Hypoglycemia and diabetes: 98. Umpierrez,G.E. etal. Management of hyperglycemia in emergency room of a tertiary hospital in Spain.
areport of a workgroup of the American Diabetes hospitalized patients in non-critical care setting: an Endocrinol. Nutr. 62, 277284 (2015).
Association and the Endocrine Society. Diabetes Care endocrine society clinical practice guideline. J.Clin. 122. Alourfi,Z. & Homsi,H. Precipitating factors, outcomes,
36, 13841395 (2013). Endocrinol. Metab. 97, 1638 (2012). and recurrence of diabetic ketoacidosis at a university
75. Cryer,P.E., Davis,S.N. & Shamoon,H. Hypoglycemia 99. Maynard,G., Lee,J., Phillips,G., Fink,E. & Renvall,M. hospital in Damascus. Avicenna J.Med. 5, 1115
in diabetes. Diabetes Care 26, 19021912 (2003). Improved inpatient use of basal insulin, reduced (2015).
76. Moghissi,E.S. etal. American Association of Clinical hypoglycemia, and improved glycemic control: effect of 123. Lin,S.F., Lin,J.D. & Huang,Y.Y. Diabetic ketoacidosis:
Endocrinologists and American Diabetes Association structured subcutaneous insulin orders and an insulin comparisons of patient characteristics, clinical
consensus statement on inpatient glycemic control. management algorithm. J.Hosp. Med. 4, 315 (2009). presentations and outcomes today and 20years ago.
Endocr. Pract. 15, 353369 (2009). 100. Noschese,M. etal. Effect of a diabetes order set on Chang Gung Med. J. 28, 2430 (2005).
77. Moghissi,E.S. etal. American Association of Clinical glycaemic management and control in the hospital.
Endocrinologists and American Diabetes Association Qual. Saf. Health Care 17, 464468 (2008). Acknowledgements
consensus statement on inpatient glycemic control. 101. Korytkowski,M., McDonnell,M.E., Umpierrez,G.E. & G.U. is supported in part by research grants from the
Diabetes Care 32, 11191131 (2009). Zonszein,J. Patient guide to managing hyperglycemia American Diabetes Association (114LLY36), Public Health
78. Umpierrez,G.E. etal. Management of hyperglycemia (high blood sugar) in the hospital. J.Clin. Endocrinol. Service grant UL1 RR025008 from the Clinical Translational
in hospitalized patients in non-critical care setting: Metab. 97, 27A28A (2012). Science Award Program (M01 RR00039), the NIH and the
anEndocrine Society Clinical Practice Guideline. J.Clin. 102. Moore,C. & Woollard,M. Dextrose 10% or 50% in National Center for Research Resources. M.K. is supported
Endocrinol. Metab. 97, 1638 (2012). thetreatment of hypoglycaemia out of hospital? in part by research grants from the NIH.
79. Hsu,P.F. etal. Association of clinical symptomatic Arandomised controlled trial. Emerg. Med. J. 22,
hypoglycemia with cardiovascular events and total 512515 (2005). Author contributions
mortality in type2 diabetes: a nationwide population- 103. Graveling,A.J. & Frier,B.M. Risks of marathon running G.U. and M.K. researched data for the article, made sub
based study. Diabetes Care 36, 894900 (2013). and hypoglycaemia in type1 diabetes. Diabet. Med. 27, stantial contributions to discussions about the content, wrote
80. Chow,E. etal. Risk of cardiac arrhythmias during 585588 (2010). thearticle and reviewed and/or edited the manuscript
hypoglycemia in patients with type2 diabetes and 104. Schabelman,E. & Kuo,D. Glucose before thiamine for beforesubmission.
cardiovascular risk. Diabetes 63, 17381747 (2014). Wernicke encephalopathy: a literature review. J.Emerg.
81. Goto,A., Arah,O.A., Goto,M., Terauchi,Y. & Noda,M. Med. 42, 488494 (2012). Competing interests statement
Severe hypoglycaemia and cardiovascular disease: 105. Deusenberry,C.M., Coley,K.C., Korytkowski,M.T. G.U. declares that he has received consulting fees or/and hon-
systematic review and meta-analysis with bias analysis. &Donihi,A.C. Hypoglycemia in hospitalized patients oraria for membership of advisory boards from Boehringer
BMJ 347, f4533 (2013). treated with sulfonylureas. Pharmacotherapy 32, Ingelheim, Glytec, Johnson and Johnson, Merck, Novo
82. Reno,C.M. etal. Severe hypoglycemia-induced lethal 613617 (2012). Nordisk and Sanofi, and that he has received unrestricted
cardiac arrhythmias are mediated by sympathoadrenal 106. Fleseriu,M., Skugor,M., Chinnappa,P. & Siraj,E.S. research support for inpatient studies (to Emory University
activation. Diabetes 62, 35703581 (2013). Successful treatment of sulfonylurea-induced prolonged School of Medicine) from Astra Zeneca, Boehringer
83. Tsujimoto,T. etal. Vital signs, QT prolongation, and hypoglycemia with use of octreotide. Endocr. Pract. 12, Ingelheim, Merck, Novo Nordisk and Sanofi. M.K. declares
newly diagnosed cardiovascular disease during severe 635640 (2006). no competing interests.
hypoglycemia in type1 and type2 diabetic patients. 107. Korytkowski,M.T. Diabetes and aging. Diabetes
Diabetes Care 37, 217225 (2014). Spectrum. 26, 34 (2013). Review criteria
84. Tanenberg,R.J., Newton,C.A. & Drake,A.J. 108. Little,S.A. etal. Recovery of hypoglycemia awareness in References were identified by searching the OVID MEDLINE
Confirmation of hypoglycemia in the deadinbed long-standing type1 diabetes: a multicenter 22 and PubMed databases (19462015) using the terms
syndrome, as captured by a retrospective continuous factorial randomized controlled trial comparing insulin type1 diabetes, type2 diabetes, diabetic ketoacidosis,
glucose monitoring system. Endocr. Pract. 16, 244248 pump with multiple daily injections and continuous with hyperglycaemia, hypoglycaemia, inpatient and sulfony-
(2010). conventional glucose self-monitoring (HypoCOMPaSS). lureas. English-language full-text manuscripts were selected
85. Razavi Nematollahi,L. etal. Proinflammatory cytokines Diabetes Care 37, 21142122 (2014). whenever possible. References were also identified through
in response to insulin-induced hypoglycemic stress in 109. Samann,A., Muhlhauser,I., Bender,R., Kloos,C. review of manuscripts selected using the search engines
healthy subjects. Metabolism 58, 443448 (2009). &Muller,U.A. Glycaemic control and severe described above, in addition to use of the Similar articles
86. Seaquist,E.R. etal. The impact of frequent hypoglycaemia following training in flexible, intensive and Cited by sidebars provided by PubMed. Several of the
andunrecognized hypoglycemia on mortality insulin therapy to enable dietary freedom in people with references were suggested by peer reviewers.
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 11
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
You might also like
- Place a chest tubeDocument83 pagesPlace a chest tubehwelpNo ratings yet
- DISTRIBUTIVE SHOCKDocument41 pagesDISTRIBUTIVE SHOCKFuzi HannyNo ratings yet
- Darkest HoursDocument45 pagesDarkest Hoursharlock87No ratings yet
- Penetrating Trauma ManagementDocument103 pagesPenetrating Trauma ManagementAlrexan B. MalatagNo ratings yet
- Diabetes For EMS ProvidersDocument58 pagesDiabetes For EMS ProvidersPaulhotvw67100% (2)
- Prehospital STEMI CareDocument39 pagesPrehospital STEMI Careapi-21568727No ratings yet
- Heat EmergenciesDocument3 pagesHeat EmergenciesScott KNo ratings yet
- Evangeline Poem PDFDocument2 pagesEvangeline Poem PDFZiadNo ratings yet
- Chapter 12 - Cardiovascular EmergenciesDocument47 pagesChapter 12 - Cardiovascular EmergenciesJunx TripoliNo ratings yet
- Medical EmergenciesDocument81 pagesMedical EmergenciesKreshnik HAJDARINo ratings yet
- Gastric Emergencies: Principles of Critical Care ModuleDocument32 pagesGastric Emergencies: Principles of Critical Care ModuleDeni AdriansyahNo ratings yet
- Vascular Responses to PathogensFrom EverandVascular Responses to PathogensFelicity N.E. GavinsNo ratings yet
- Thyroid EmergenciesDocument23 pagesThyroid EmergenciesHeron BayaninNo ratings yet
- List Ebook EpidemiologyDocument3 pagesList Ebook EpidemiologyarifNo ratings yet
- Exam 3 pathophysiology Cancer growth types and characteristicsDocument7 pagesExam 3 pathophysiology Cancer growth types and characteristicsmenickel3No ratings yet
- Fisdap Practice PatientDocument2 pagesFisdap Practice Patientapi-463830419No ratings yet
- Head Injury 1Document33 pagesHead Injury 1drvishal bhattNo ratings yet
- Muscle Skeletal Trauma For EMSDocument79 pagesMuscle Skeletal Trauma For EMSPaulhotvw67100% (4)
- Patient Assessment Model (PAMDocument18 pagesPatient Assessment Model (PAMMarian Ioan-LucianNo ratings yet
- "Get in My Belly": Abdominal EmergenciesDocument74 pages"Get in My Belly": Abdominal EmergenciesSherif Abou BakrNo ratings yet
- Respiratory PathophysDocument1 pageRespiratory PathophysTori IkeharaNo ratings yet
- Common Medical Emergencies: Jude D. Positos, RNDocument27 pagesCommon Medical Emergencies: Jude D. Positos, RNNenen PositosNo ratings yet
- Adult - SNS 2014 StudentDocument91 pagesAdult - SNS 2014 StudentJamie Lynn MorganNo ratings yet
- What Is Respiratory Alkalosis?Document3 pagesWhat Is Respiratory Alkalosis?Lorenn AdarnaNo ratings yet
- Hypertensive EmergenciesDocument49 pagesHypertensive EmergenciesSafa Abdualrahaman Ali HamadNo ratings yet
- KegawatdaruratanDocument164 pagesKegawatdaruratanmeida astriani gozaziNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- Drug Nomenclature Suffixes and PrefixesDocument6 pagesDrug Nomenclature Suffixes and PrefixesMariaNo ratings yet
- Acute Renal FailureDocument12 pagesAcute Renal FailureRifa Aprillia CahyaniNo ratings yet
- A. Cardio: Anatomy & Physiology - A. AnatomyDocument43 pagesA. Cardio: Anatomy & Physiology - A. AnatomyGloryJaneNo ratings yet
- Krisis HipertensiDocument12 pagesKrisis HipertensiDani NurseNo ratings yet
- West Visayas State University: Nursing ProcessDocument4 pagesWest Visayas State University: Nursing ProcessPhylum Chordata100% (1)
- Concept of Extreme Conditions: ShockDocument12 pagesConcept of Extreme Conditions: ShockAnonymous 8hJAATBNo ratings yet
- Pediatric 3 - Answers v1 (Wide)Document56 pagesPediatric 3 - Answers v1 (Wide)Humzala BashamNo ratings yet
- 1538 Exam 4 Cell Reg & GriefDocument35 pages1538 Exam 4 Cell Reg & GriefJade EdanoNo ratings yet
- Right Side EcgDocument4 pagesRight Side EcgDragos CirsteaNo ratings yet
- Respiratory Patho PhysDocument1 pageRespiratory Patho PhysTori IkeharaNo ratings yet
- Paramedic Exam Guide to Immunizations & Research MethodsDocument21 pagesParamedic Exam Guide to Immunizations & Research MethodsBarry GruenbaumNo ratings yet
- Multiple Sclerosis AANN-ARN-IOMSN-MS-Guideline - FINAL PDFDocument49 pagesMultiple Sclerosis AANN-ARN-IOMSN-MS-Guideline - FINAL PDFCyntia Theresia LumintangNo ratings yet
- Adult Bradycardia Algorithm: Identify and Treat Underlying CauseDocument1 pageAdult Bradycardia Algorithm: Identify and Treat Underlying CausenebrasNo ratings yet
- #9 Ie 8 PDFDocument8 pages#9 Ie 8 PDFOmar BasimNo ratings yet
- Critical Care 2012Document490 pagesCritical Care 2012Carlos PradoNo ratings yet
- HFandVADRoleDocument34 pagesHFandVADRoleJohnNo ratings yet
- Aorta DissectionDocument98 pagesAorta DissectionDian SukaryaNo ratings yet
- COPD GuideDocument69 pagesCOPD GuideEster Elisabeth WoworNo ratings yet
- PedsCases - Anaphylaxis Emergency TreatmentDocument5 pagesPedsCases - Anaphylaxis Emergency TreatmentSara Ilyas KhanNo ratings yet
- English in Urgent Care Medicine – Anglictina V Urgentní Medicíne: Textbook – UcebniceFrom EverandEnglish in Urgent Care Medicine – Anglictina V Urgentní Medicíne: Textbook – UcebniceNo ratings yet
- Drugs in Cardiac EnmergenciesDocument94 pagesDrugs in Cardiac EnmergenciesVijayan VelayudhanNo ratings yet
- Abdominal Pain DR - Shaesta.TabassumDocument45 pagesAbdominal Pain DR - Shaesta.TabassumAjay DherwaniNo ratings yet
- Brain InjuriesDocument46 pagesBrain Injuriesbasic100% (5)
- DR Romila Chimoriya Lecturer Department of Pediatrics: Acute Rheumatic FeverDocument27 pagesDR Romila Chimoriya Lecturer Department of Pediatrics: Acute Rheumatic FeverDhiraj PantNo ratings yet
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Shock, Sirs & ModsDocument37 pagesShock, Sirs & ModsambitioustamannaNo ratings yet
- Treatment of Resistant and Refractory HypertensionDocument21 pagesTreatment of Resistant and Refractory HypertensionLuis Rodriguez100% (1)
- Asphyxialconditions 120917062150 Phpapp02Document93 pagesAsphyxialconditions 120917062150 Phpapp02minaaminmaNo ratings yet
- Common Medication Classifications and Adverse/Side Effects: This Is Not An All Inclusive ListDocument2 pagesCommon Medication Classifications and Adverse/Side Effects: This Is Not An All Inclusive ListHashim Mushtasin RezaNo ratings yet
- Toxicology Tables PDFDocument23 pagesToxicology Tables PDFIssam HadiNo ratings yet
- Varices Esophagus PDFDocument7 pagesVarices Esophagus PDFDimas ErlanggaNo ratings yet
- Sindrome de Cobb - Ibrahim - 2021Document5 pagesSindrome de Cobb - Ibrahim - 2021Juan C. Salazar PajaresNo ratings yet
- Pituitary Incidentaloma Freda 2011Document11 pagesPituitary Incidentaloma Freda 2011Juan C. Salazar PajaresNo ratings yet
- Case 40-2021 - A 9-Year-Old - Enf - MoyamoyaDocument10 pagesCase 40-2021 - A 9-Year-Old - Enf - MoyamoyaJuan C. Salazar PajaresNo ratings yet
- Brain Tumors Children Cohen 2022Document10 pagesBrain Tumors Children Cohen 2022Juan C. Salazar PajaresNo ratings yet
- Hyperprolactinemia EsDocument16 pagesHyperprolactinemia Esswathi bsNo ratings yet
- A Clinical Practice Guideline For The Management of Acute Spinal Cord Injury - Introduction, Rationale, and ScopeDocument11 pagesA Clinical Practice Guideline For The Management of Acute Spinal Cord Injury - Introduction, Rationale, and ScopeOla OlaNo ratings yet
- Virus de Inmunodeficiencia Humana y Complicaciones Neurológicas - Pediatría (Santiago de Chile) 2 (1) Abr. 2005. Tab - LILACSDocument1 pageVirus de Inmunodeficiencia Humana y Complicaciones Neurológicas - Pediatría (Santiago de Chile) 2 (1) Abr. 2005. Tab - LILACSJuan C. Salazar PajaresNo ratings yet
- Pocket Neurology: Publication Year Edition Author/Editor Publisher Isbn Platform Product Type SpecialityDocument2 pagesPocket Neurology: Publication Year Edition Author/Editor Publisher Isbn Platform Product Type SpecialityJuan C. Salazar PajaresNo ratings yet
- Clasificación de Las Enfermedades CerebrovascularesDocument10 pagesClasificación de Las Enfermedades CerebrovascularesDavidemNo ratings yet
- Caso Encefalitis AmebiasisDocument2 pagesCaso Encefalitis AmebiasisJuan C. Salazar PajaresNo ratings yet
- Quiste Aracnoideo Espinal PDFDocument12 pagesQuiste Aracnoideo Espinal PDFJuan C. Salazar PajaresNo ratings yet
- 1 s2.0 S0022391302002998 MainDocument5 pages1 s2.0 S0022391302002998 MainManjeev GuragainNo ratings yet
- Crabtales 061Document20 pagesCrabtales 061Crab TalesNo ratings yet
- CaseDocument31 pagesCaseErnes PutraNo ratings yet
- Firstaid ModuleDocument143 pagesFirstaid Moduleretni wulandariNo ratings yet
- Range of Motion PresentationDocument27 pagesRange of Motion Presentationsathish100% (1)
- Breast LumpDocument2 pagesBreast Lumplentini@maltanet.netNo ratings yet
- Phobiasgalore1 2Document2 pagesPhobiasgalore1 2api-264827695No ratings yet
- Growth PredictionDocument101 pagesGrowth PredictionKristty Magallanes100% (1)
- Ngos in WayanadDocument51 pagesNgos in Wayanadnivia008No ratings yet
- All Models W ExplanationDocument63 pagesAll Models W Explanationpayal1407No ratings yet
- Ohi 2Document6 pagesOhi 2api-242024640No ratings yet
- Joint Disorders - Ay NewDocument46 pagesJoint Disorders - Ay NewPraisingson SyiemliehNo ratings yet
- CefepimeDocument2 pagesCefepimeMae Ann Bueno CastillonNo ratings yet
- Juvenile Sex Offenders A Complex PopulationDocument6 pagesJuvenile Sex Offenders A Complex PopulationRoberto GalleguillosNo ratings yet
- Music and MoodDocument5 pagesMusic and MoodNatalia TríasNo ratings yet
- Obama Mind ControlDocument68 pagesObama Mind Controlkdnkgljfg67% (3)
- BLS Adult Skills Checklist 2016Document2 pagesBLS Adult Skills Checklist 2016Wahyudi QorahmanNo ratings yet
- 2nd Brochure PDFDocument2 pages2nd Brochure PDFhappy855No ratings yet
- Introduction To Dental Anatomy: DR - Yad Raouf BDS, Efb, MrcsedDocument27 pagesIntroduction To Dental Anatomy: DR - Yad Raouf BDS, Efb, MrcsedRabarNo ratings yet
- 5105 - Achilles TendonDocument30 pages5105 - Achilles Tendonalbertina tebayNo ratings yet
- Youtsey Kristen Cover LetterDocument1 pageYoutsey Kristen Cover Letterapi-457850399No ratings yet
- Botox 2017 PDFDocument244 pagesBotox 2017 PDFDyah Ayu Putri Midiantari50% (2)
- Pain Myocardial: Review Treatment of in InfarctionDocument5 pagesPain Myocardial: Review Treatment of in InfarctionAlifah ChoNo ratings yet
- DetailsDocument21 pagesDetailskanthavelNo ratings yet
- DHI Score PDFDocument2 pagesDHI Score PDFAnonymous HNGH1oNo ratings yet
- MCPS Form For Annual Sports Physical Exam - (PPE) 2010 Edition Prepared by Am Academy of Ped, Am. Academy of Family Phys Et Al.Document5 pagesMCPS Form For Annual Sports Physical Exam - (PPE) 2010 Edition Prepared by Am Academy of Ped, Am. Academy of Family Phys Et Al.Concussion_MCPS_MdNo ratings yet
- Ergogenic Aids 1Document24 pagesErgogenic Aids 1unattractiveyouNo ratings yet
- (Doi 10.1016/j.ijpharm.2015.01.022) T. Loftsson - Excipient Pharmacokinetics and ProfilingDocument7 pages(Doi 10.1016/j.ijpharm.2015.01.022) T. Loftsson - Excipient Pharmacokinetics and ProfilingRia DeviNo ratings yet
- CLASS 1 - Image - Roles Revised June 260Document48 pagesCLASS 1 - Image - Roles Revised June 260Marie-Lynne L'orNo ratings yet
- Baker v. Dalkon Sheild, 156 F.3d 248, 1st Cir. (1998)Document10 pagesBaker v. Dalkon Sheild, 156 F.3d 248, 1st Cir. (1998)Scribd Government DocsNo ratings yet