Professional Documents
Culture Documents
Journal Hemophilia 3
Uploaded by
Sastra SinagaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Journal Hemophilia 3
Uploaded by
Sastra SinagaCopyright:
Available Formats
1p33-38.
QXD 10/12/2004 14:34 Page 33
RESEARCH
IN BRIEF
This pilot study is small and lacks the power to recommend changes in clinical practice. A
larger multi-centre study may be the solution.
The results from this study promise the possibility of reducing the need of using factor
replacement therapy on a minor traumatic procedure in people with haemophilia.
It gives the patients more freedom in determining their own treatment; reserve factor for
more severe bleeding situations; thus
avoiding the disadvantages of factor replacement therapy (high cost, development
factor antibodies and risks of blood product contamination).
Effectiveness in controlling haemorrhage after
dental scaling in people with haemophilia by
using tranexamic acid mouthwash
A. P. H. Lee,1 C. A. Boyle,2 G. F. Savidge3 and J. Fiske4
Aims To compare the effectiveness of tranexamic acid mouthwash Haemophilia is an inherited disorder of blood clotting with an
(TAMW) in controlling gingival haemorrhage after dental scaling with that incidence of 1 in 5,000 male births.1 There are two types
of using factor replacement therapy (FRT) prior to dental scaling in people haemophilia A characterised by a deficiency of clotting factor VIII
with haemophilia. (F VIII), and haemophilia B characterised by a deficiency of clot-
Design Double-blind cross-over randomised control trial. ting factor IX (F IX). Haemophilia A is the more common type,
Setting Dedicated hospital dental practice for patients with inherited accounting for approximately 85% of all cases of haemophilia.2
bleeding disorders. Despite a deficit of different clotting factors, types A and B have
Method Sixteen patients with haemophilia who required dental scaling identical clinical manifestations, screening test abnormalities, and
participated in this pilot study. The experimental treatment regime (ETR) X-linked genetic transmission. Specific factor assays are required
involved transfusing each patient with saline before scaling both quadrants to distinguish the two.1
on one side of the mouth followed by oral rinsing with TAMW four times The frequency and severity of bleeding experienced by a person
daily for up to eight days. The control regime (CR) involved giving each with haemophilia depends mainly on their plasma levels of F VIII
patient FRT before scaling the opposite side of the mouth followed by use or the F IX activity. The lower the factor levels are, the more severe
of a placebo TAMW. Each patient underwent both treatments in a random- the condition (Table 1). An individual with haemophilia does not
ised sequence. Both the operator and the patients were unaware of which bleed more profusely or faster than normal simply for longer.3
were the ETR and CR episodes. On both occasions the patient kept a log The main treatment options currently available to control bleeding
book of the rinsing regime and any post-operative bleeding. Additionally, a are: factor replacement therapy; release of endogenous factor
structured post-treatment telephone interview was conducted to assess stores; and clot stabilisation.4
the effectiveness and the patient acceptability of the ETR. Factor replacement therapy (FRT) is the main mode of treatment
Results Thirteen patients completed the study. No statistically significant for both haemophilia A and haemophilia B. The missing factor is
difference was found in gingival bleeding and mouthwashing frequencies given intravenously by the person with haemophilia, parents or
between the ETR and the CR (p > 0.05). Five patients reported no gingival experienced staff at hospitals.3 It is either prescribed regularly two or
bleeding with either the ETR or the CR. No patient, using either regime, three times a week on a prophylactic basis to prevent bleeds, or it is
required extra FRT due to gingival haemorrhage. All subjects found the administered on-demand as soon as a bleed starts. In many bleeding
ETR acceptable and easy and reported feeling safe in using TAMW alone to situations, FRT is the only effective treatment for people with
control gingival bleeding after dental scaling.
Conclusion TAMW use after dental scaling was as effective as using FRT
Table 1 Classification of haemophilia1
beforehand in controlling gingival haemorrhage for people with
% of F VIII or IX* Degree of Characteristics
haemophilia. haemophilia
1% or less Severe Frequent spontaneous bleeds. Coagulation
1Dental Officer, Community Dental Service for Camden and Islington Primary Care NHS screening tests always abnormal.
Trusts, London, 2Associate Specialist, Department of Sedation and Special Care Dentistry, >1 - 5% Moderate Few spontaneous bleeds. Bleeding after minor
Guys, Kings and St. Thomas Dental Institute, Kings College London, 3Professor of trauma. Prolonged partial thromboplastin
Coagulation Medicine, Haemophilia Reference Centre, St. Thomas Hospital, Guys, Kings time.
and St. Thomas NHS Trust, London, 4Senior Lecturer, Honorary Consultant in the >5 - 30%** Mild Bleed only after trauma or surgery. Coagulation
Department of Sedation and Special Care Dentistry, Guys, Kings and St. Thomas Dental screen tests may be low normal.
Institute, Kings College London. >30 - 50%** Very Mild May or may not bleed abnormally after major
*Correspondence to: Dr. Carole A. Boyle, Department of Sedation and Special Care trauma or surgery. Coagulation screen tests
Dentistry, GKT Dental Institute, 26/F Guys Tower, Guys Hospital, LONDON SE1 9RT
often normal.
Email: carole.boyle@kcl.ac.uk
*The activity of clotting factors is expressed in terms of units, defined as the activity
Refereed paper present in 1ml of fresh plasma from normal donors. The concentration of all clotting
Received 10.10.03; Accepted 26.01.04 factors in native plasma is thus 1U/ml or 100U/dl or 100% activity.
DOI: 10.1038/sj.bdj.4811955 **About one third of people with haemophilia have levels between 15% and 50%.
British Dental Journal 2005; 198: 3338
BRITISH DENTAL JOURNAL VOLUME 198 NO. 1 JANUARY 8 2005 33
1p33-38.QXD 07/12/2004 17:06 Page 34
RESEARCH
haemophilia. The development of recombinant factor replacement AIM
therapy (rFRT) has reduced the risk of blood borne infection. Whilst it As there is no randomised control study on the effectiveness of
has been postulated that recombinant F VIII might cause the forma- using TA mouthwash (TAMW) alone for haemorrhage control in
tion of more inhibitors than plasma F VIII products, there is no evi- people with haemophilia after dental scaling, the aims of this study
dence to support this concern and recombinent F VIII is the recom- were to:
mended treatment for haemophilia A.5 The main disadvantage is its
high cost. It has been estimated that for medication alone, the cost per a. Compare the effectiveness of TAMW, to control haemorrhage
bleeding episode for a child of 20 kg varies from 54 to 493 and that after dental scaling, with that of FRT prior to dental scaling
for an adult varies from 90 to 822.50 depending on the severity of using a double-blind cross-over randomised control trial.
the bleeding, and the purity, type and amount of F VIII used.6
Release of endogenous F VIII stores from endothelial cells to the b. Gauge patient acceptability of the use of TAMW alone.
blood stream7 can be stimulated by the use of the hormone desmo-
pressin (DDAVP). DDAVP can be used to increase plasma concen- METHOD
trations of F VIII in people with mild to moderate haemophilia A Design
for a short time.8 However, patients repeatedly treated with DDAVP This pilot study was a double-blind cross-over randomised con-
can become less responsive, probably because stores are exhaust- trolled trial. The patients underwent both the experimental and
ed,9 thus, limiting its use in the management of haemophilia. control treatment regimes in turn with at least a two-week
Clot stabilisation can be used to facilitate haemostasis and is interval, and the sequence was determined by a random table
achieved through the use of synthetic amino acid derivatives of provided by the statistician, thus accounting for the cross-over
lysine that have antifibrinolytic activity.10 One such product is and randomisation characteristics of this study. The procedures
tranexamic acid [4-(aminomethyl) cyclohexanecarboxylic acid]. It for the two dental appointments were similar except that oppo-
works by binding reversibly to plasminogen (preventing it from site sides of the mouth were scaled and different medications
forming plasmin) and preventing plasminogen binding to fibrin, used on each of the two appointments. During the study period,
thereby, halting fibrinolysis (Figure 1). Tranexamic acid (TA) has neither the patients nor the hygienist knew which regime the
been used in conjunction with other haemostatic measures to con- patients were receiving in order to achieve the effect of double-
trol bleeding in various medical and surgical situations including blindness. The staff of the Haemophilia Reference Centre at St.
oral bleeding in congenital and acquired coagulation disorders.12 Thomas Hospital, London and the researcher (AL), however,
It has some role in controlling haemorrhage in haemophilia. were not blinded in this study in case of emergencies.
Sindet-Pedersen has demonstrated that TA produces therapeutic
saliva concentrations by mouthrinsing with 10 ml of 5% TA aque- Sample selection
ous solution.14 TA in conjunction with FRT, in a non-blind study, Potential subjects were identified from the Haemophilia Refer-
has been shown to provide effective haemorrhage control after sub- ence Centre database. Patients were contacted and those fulfill-
gingival dental scaling in people with haemophilia.15 ing the non-dental inclusion criteria (Table 2) of the study were
The dental needs of people with haemophilia are high. A recent invited to participate. Once informed consent had been
study of people with inherited bleeding disorders attending a dental obtained, they underwent a thorough dental examination
service established specifically for their care showed that 50% of including a six point periodontal pocket charting and recording
people required scaling and polishing, 74% required restorative of any sites that bled on probing. Those participants who ful-
treatment, 30% needed extractions and 10% needed partial den- filled the dental inclusion criteria were assigned identification
tures. This outstanding dental treatment need was mainly due to numbers, to facilitate the organisation of the double blind trial,
anxiety related to dental treatment and focused on haemorrhage and given two dental appointments at least two weeks apart.
management.13
Tissue Lysine -binding
Plasminogen
plasminogen site
activator
Fibrin
-aminocaproic
acid or
Tissue Plasmin tranexamic acid
plasminogen
activator
Fibrin
Fig 1 Antifibrinolytic effect of tranexamic acid11
34 BRITISH DENTAL JOURNAL VOLUME 198 NO. 1 JANUARY 8 2005
1p33-38.QXD 07/12/2004 17:12 Page 35
RESEARCH
Table 2 Study inclusion / exclusion criteria
Non-dental inclusion criteria Dental inclusion criteria
1. Haemophilia A or B 1. Requires a dental scaling
2. Aged 16 or over 2. < 3 teeth difference between the left & right sides of mouth
3. Platelet counts >50 x 109/L 3. CPITN score of 2 or 3
4. No history of:
i. allergy to tranexamic mouthwash
ii. deep vein thrombosis
iii. renal impairment
iv. cardiac pacemaker
Non-dental exclusion criteria Dental exclusion criteria
1. Receiving ongoing prophylactic 1. Does not require a dental scaling
replacement therapy
2. History of acquired disturbances 2. > 3 teeth difference between the left & right sides of mouth
of colour vision
3. Taken aspirin or NSAI in the week 3. CPITN score of < 2
prior to/during the study period
Ethical approval Control treatment regime (CTR)
Ethical approval was granted from the Guys and St Thomas For the CTR, the patient was transfused pre-operatively with
Research Ethics Committee in July 2000, following changes to the active factor concentrate according to their type of haemophilia
patient information sheet and log book. (ie F VIII for patients with haemophilia A and F IX for patients
with haemophilia B) rather than with saline. Upper and lower
Drug licensing exemption quadrants of the other side of the mouth were scaled by the
Tranexamic acid is not covered for use as a mouthwash by the hygienist and the subject was given three 100 ml bottles of place-
existing pharmaceutical licence in the UK. Exemption was sought bo mouthwash (Table 4) for post-operative use. The instructions
and obtained from the Medicines Control Agency of the Depart- for inspection for bleeding, mouthwash use and data recording
ment of Health for this experimental use. were the same as for the ETR.
Experimental treatment regime (ETR) Safety measures
The ETR involved patients receiving placebo factor concentrate In the interests of safety and emergencies, there was a mecha-
(0.9% normal saline) by intravenous transfusion (administered by nism in place so that patients could find out from either the
the nurses at the Haemophilia Centre) no more than one hour prior Haemophilia Reference Centre or from the researcher (AL) which
to dental treatment. The scaling of both upper and lower quadrants regime they had been given. Additionally, patients were
of one side of the mouth was carried out by a dental hygienist. As informed that they could receive factor replacement therapy at
indicated in the dental inclusion criteria (Table 2), all the patients any time during the study if they thought the mouthwash was
had a CPITN of either 2 or 3, the gingival pockets scaled were ineffective or if bleeding occurred in other parts of their bodies.
between 3mm and 5mm deep. The hygienist was blinded in the Also, patients were at liberty to withdraw from the study at any
study and she was instructed to treat the patients as if they had point.
FRT prior to both scaling appointments. She was allowed to choose
the most appropriate method to perform the scaling, but she was
obliged to use the same method for the same patient. The study
participant was given three 100 ml bottles of active 5% TAMW
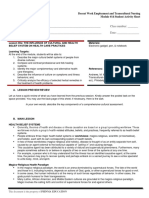
Day 1
(Table 3) for home use sufficient for eight days. The subject was
instructed to visually check for gingival bleeding four times per Yes No Forgotten
day, once after each of the three main meals and once before going
Morn
Morning
r ing Did you find bleeding gums?
to bed. If bleeding was noted, 10 ml of the mouthwash was to be
held in the mouth for 2 minutes and then expectorated. Patient Did you use the mouthwash?
bleeding and mouthwash-use data was recorded in a log book
(Figure 2) supplied by the researcher. The patients determined how
often and for how many days they needed to use the mouthwash. Did you find bleeding gums?
Noon
Table 3 Composition of active 5% tranexamic acid Did
id you use the mouthwash?
mouthwash
Tranexamic acid 500 g
Methyl hydroxybenzote (Nipagin M)* 15 g
Propyl hydroxybenzoate (Nipasol M)* 1.5 g Evening Did you find bleeding gums?
Distilled water (cold) 10 L
Did you use the mouthwash?
* Preservatives.
Table 4 Composition of placebo mouthwash Bedtime Did you find bleeding gums?
Methyl hydroxybenzoate (Nipagin M) 15 g
Propyl hydroxybenzoate (Nipasol M) 1.5 g Did you use the mouthwash?
Distilled water (cold) 10 L
Prepared by the Pharmacy Department, St Thomas' Hospital,
London Fig 2 Log book sample page
BRITISH DENTAL JOURNAL VOLUME 198 NO. 1 JANUARY 8 2005 35
1p33-38.QXD 07/12/2004 17:12 Page 36
RESEARCH
Collection of patient log books Additionally, no statistically significant differences were found
The patients were provided with a log book after each phase of the between the ETR and CTR for the overall use of the mouthwash.
study. They were requested to return their log books to the
researcher in the self-addressed envelopes provided once their data Patient assessment of acceptability of the ETR
recording was completed. Subjects who had not returned log A structured telephone interview was used to establish the
books by two weeks after their last dental scaling appointment patients experiences after each dental scaling appointment and to
were reminded by phone to do so. gauge acceptability of the ETR. After matching the random table
with the patients responses, it was found that there was a statisti-
Telephone interviews cally significant preference towards the ETR over the CTR (p = 0.04
Structured telephone interviews (Fig. 3) were carried out by one using Pearson Chi-square test for independence with test signifi-
researcher (AL) to record the subjects experiences after each den- cance predetermined at p = 0.05). Subjects were unable to accu-
tal scaling appointment and to assess the effectiveness and the rately assess which treatment regime had been used, and only one
patient acceptability of the ETR. person felt that his guesstimate of which regime he had under-
gone influenced his use of the mouthwash. Additionally, all
Data analysis patients found the mouthwash easy to use and 12 subjects (92%)
The data were collated and presented as absolute numbers and per- found its taste acceptable. One person found the taste of both the
centages. They were analysed using SPSS for Windows Release active and placebo mouthwashes unacceptably salty.
10.0.1, Stata Release 7 and StatXact 3. The differences in the oral
conditions between the patients left and right hand sides of the Patient assessment of safety of the ETR
mouth and the differences between the experimental and control One hundred per cent of participants reported that they would feel
treatment regimes were both analysed using the Wilcoxon signed safe receiving dental scaling when only using tranexamic acid
rank test with test significance predetermined at 0.05. mouthwash afterwards to control gingival bleeding. Five patients
(38.5%) felt that it was not safe to use nothing to control gingival
RESULTS bleeding after dental scaling. The remaining eight patients thought
Patient demography it was safe to do so.
All 16 participants in this study were male. The data of three sub-
jects were excluded from the analysis one person required FRT 1. Of the two scaling appointments, which one do you prefer?
for an elbow bleed during the study and two others failed to return
their log books despite reminders. Thirteen people (81%) complet- Appointment 1 Appointment 2 No difference
ed the study. Their mean age was 37.8 years with a range from 18
to 68. Eleven of them had haemophilia A and 2 had haemophilia B.
Among the haemophilia A patients, one had mild haemophilia, 3 2. On which occasion did you think you had the factor cover before the
had moderate and 7 had severe haemophilia. The 2 haemophilia B
patients both had severe haemophilia. scaling appointment?
The information obtained from both haemophilia A and B
Appointment 1 Appointment 2 Uncertain
patients was grouped together by their severity in this study.
Periodontal conditions
The percentages of the number of pockets > 3 mm between the left 3. Did it influence your behaviour of using the mouthwash?
and right hand sides of the mouth were compared for each patient
Yes No Uncertain
and then calculated among all the study participants using the
Wilcoxon signed rank test. The difference was not statistically signif-
icant (p = 0.56). Similarly, the percentages of bleeding sites on prob-
ing pre-operatively were compared for each patient. Adopting the 4. Did you think the mouthwash was easy to use?
Wilcoxon signed rank test, these differences were compared among Yes No
all subjects and no significant differences were found (p = 0.06).
Post-scaling haemorrhage
5. Did you think the taste of the mouthwash acceptable?
Five out of the 13 subjects (38.5%) who completed the study
reported no gingival bleeding with either the experimental or the Yes No
control treatment regimes.
No patients required extra factor replacement therapy due to
gingival haemorrhage with either the experimental or the control
6. Would you feel safe having a dental scaling without factor cover in
treatment conditions. Data analysis showed no significant differ-
ence for reported gingival bleeding between the ETR and the CTR advance and by using just the tranexamic acid mouthwash afterwards?
(p = 0.57, Wilcoxon signed-rank test with test significance prede-
termined at 0.05). Yes No Uncertain
Use of mouthwash
Data related to the use of mouthwash was analysed using the Wilcox- 7. Would you feel safe having a dental scaling with neither the factor cover
on signed-rank test with test significance predetermined at 0.05. No
significant differences were found for mouthwash use between the in advance nor the tranexamic acid mouthwash afterwards?
ETR and the CTR for the number of times the mouthwash was used to Yes No Uncertain
control bleeding (p = 0.51); the number of times the mouthwash was
electively not used when bleeding occurred (p = 0.32); and the num-
ber of times the mouthwash was used despite no bleeding (p = 0.62). Fig 3 Structured telephone interview
36 BRITISH DENTAL JOURNAL VOLUME 198 NO. 1 JANUARY 8 2005
1p33-38.QXD 07/12/2004 17:13 Page 37
RESEARCH
DISCUSSION management, in particular, are major factors.13,23 The concern of
Study design people with IBD that dentists may not have the knowledge and
This study is, to the authors knowledge, the first double-blind ran- experience to provide their treatment safely23 acts as a deterrent to
domised controlled trial on the effectiveness of TAMW in control- seeking care that, when they do attend, is compounded by dentists
ling gingival haemorrhage after dental scaling in people with lack of confidence in providing invasive treatment.23,24 The use of
haemophilia. The finding, that the use of TAMW after dental scal- TAMW in preference to FRT transfers the responsibility for haemo-
ing is as effective in controlling gingival bleeding as using FRT static management from the dentist to the patient. In so doing it
before dental scaling, is encouraging. provides the individual with control and removes/reduces any
However, it is difficult to overlook the fact that the number of anxiety about the operators understanding of the haemophilia
participants in this study is small (n = 13) and some statistics pro- management.
vided results that are difficult to interpret. For example, although it A further difficulty associated with FRT is that Factor VIII cover
was found that among all subjects there was no significant differ- has a comparatively short half-life (around 2 hours) necessitating
ence (p = 0.06) in the percentages of bleeding sites on probing pre- dental treatment to begin immediately following its administra-
operatively between the left and the right sides of each patient, the tion.13 This poses a problem for those people who do not adminis-
p-value is too close to the predetermined value 0.05. ter their own prophylactic factor and who have to travel from the
The rigorous study design and the appropriate data analysis go centre of administration to the dental surgery. The use of TAMW in
someway to compensate for the small sample size. Consideration preference to FRT allows this barrier to be overcome.
of appropriate data analysis for this size sample led to the use of Interestingly, five of the thirteen participants (38.5%) in the
non-parametric inference. This is a computationally intensive type current study reported no post-operative bleeding with either the
of analysis based on permutation techniques such that data are experimental or the control regimes suggesting that a proportion
repeatedly rearranged and the appropriate test statistic recalculat- of patients with haemophilia may not require any medication at all
ed to produce an exact sampling distribution and reduce the likeli- to control gingival bleeding after dental scaling. This makes
hood of chance results. TAMW ideal in that it can be used as needed post-operatively.
Difficulty in recruitment Feeling of safety
The difficulty in recruiting subjects to the study was due to a combi- All the patients in the current study related that they would feel safe
nation of factors. They included: the distance some people have to using the TAMW regime alone following dental scaling in the future.
travel to the Haemophilia Reference Centre (up to 200 miles round However, this feeling cannot be detached from the environment in
trip); mobility problems as a consequence of haemarthrosis; the which the treatment was delivered. All treatment was provided in a
desire to limit the number of episodes of haemostatic cover and thus dedicated dental unit for patients with IBD on the same site as the
a preference for full mouth scaling in one visit rather than in two; patients HRC and overseen by a dentist experienced in the dental
and a reticence to receive unnecessary FRT because of the fear of management of patients with IBD. A previous study23 found that,
contracting viral or other infections. This latter fear was inflamed by despite the increased autonomy associated with self-administration
a front page, newspaper article (reporting that NHS patients were of factor replacement, adults with IBD made little use of the general
treated with blood products from a man who died of vCJD) that dental practitioner service and preferred to receive dental treatment
appeared on a day when patients were being recruited to the study.16 in a hospital environment where they felt more secure.
The problem of recruitment to future studies could be overcome The current study has demonstrated that TAMW used post-oper-
by recognising the difficulties and by using a multi-centred atively is an effective regime for controlling gingival haemorrhage
approach. following dental scaling. The work of Forbes et al.17 and Sindet-Ped-
ersen and Stenbjerg18 suggests that the use of TAMW post-opera-
Use of FRT tively, rather than FRT pre-operatively, may also be suitable for
Until now FRT has remained the main method of controlling haemostatic control following tooth extraction. However, it is
haemorrhage in people with haemophilia A and B.19 Its use is not important to remember that haemophilia can still be a life threaten-
without concern. Not only is it very costly,6 but also its use (both ing condition and any haemostatic regime used for dental treatment
as plasma and recombinant factor concentrates) has been associ- that is not general practice should only be employed with the agree-
ated with the formation of inhibitors.20 This is a serious compli- ment and close support of the individuals haemophilia reference
cation that compromises haemostatic management as the centre.
inhibitors render the factor concentrates ineffective. The devel-
opment of inhibitors can occur at any time but the more often CONCLUSION
FRT is used the more likely they are to develop.20 Additionally, As the number of participants was small causing difficulties in inter-
the transmission of blood borne viruses (including HIV, Hepatitis preting some of the statistics, the authors cannot recommend a
A, B, C, G, parvovirus) has been associated with FRT.21 At present change in clinical practice based on the results of this study. Howev-
a small risk of plasma concentrates transmitting blood borne er, this pilot study has shown that the use of tranexamic acid mouth-
viruses still exists.5 Also, the production of factor concentrates is wash after dental scaling is well tolerated by patients and is as effec-
not constant due to the complex procedures involved. For exam- tive as using factor replacement therapy before dental scaling in
ple, from early 2001 there has been a worldwide shortage of controlling gingival bleeding for people with haemophilia. By
recombinant F VIII because Bayer suspended their product with adopting this treatment, it avoids the disadvantages of factor
the discovery of bacterial contamination in the production replacement therapy (high cost, development of factor antibodies,
process.22 Thus the attraction of finding alternative methods of and risk of blood product contamination). The authors thus recom-
haemorrhage control is evident. mend further studies in this area with a multi-centred approach to
overcome recruitment problems.
Barriers to dental care
This study was made possible by the financial assistance of the 2000 Shirley
The documented barriers to dental care,13,23 and the consequent Glasstone Hughes Memorial Prize Fund of the British Dental Research
unmet treatment needs,13 experienced by people with inherited Foundation. The authors also wish to thank the patients, Ms Muna Savage
bleeding disorders (IBD) such as haemophilia are multifactorial. (hygienist) and staff at both the Dental Clinic and the Haemophilia Reference
Centre at St Thomas Hospital for their involvement in this project.
Anxiety related to dental treatment, per se, and to haemostatic
BRITISH DENTAL JOURNAL VOLUME 198 NO. 1 JANUARY 8 2005 37
1p33-38.QXD 07/12/2004 17:16 Page 38
RESEARCH
1 Berry E, Hilgartner M, Mariani G, Sultan Y, Members of the Advisory Board, World 13 Fiske J, McGeoch R J, Savidge G F, Smith M P. The treatment needs of adults with
Federation of Hemophilia; Jones P (Ed); Kasper C and Peake I (Reviewers). inherited bleeding disorders. J Disabil Oral Health 2002; 3: 59-61.
Haemophilia: Facts for health care professionals. WHO. (WHO/HGN/WFH/EM/96.4) 14 Sindet-Pedersen S. Distribution of tranexamic acid to plasma and saliva after oral
1996. administration and mouth rinsing: a pharmacokinetic study. J Clin Pharmacol 1987;
2 Walter J, High K. Haemophilias. Encyclopedia of life sciences. Nature Publishing 27: 10051008.
Group. www.els.net 2001 [accessed on 4 July 2001]. 15 Sindet-Pedersen S, Stenbjerg S and Ingerslev J. Control of gingival hemorrhage in
3 Cowe A, Fuller S. Introduction to Haemophilia. 1999; hemophilic patients by inhibition of fibrinolysis with tranexamic acid. J Perio Res
www.haemophilia.org.uk/booklets.html [accessed on 23 May 2001]. 1998; 23: 72-74.
4 Cahill M R, Colvin B T. Haemophilia. Postgrad Med J 1997; 73: 201-206. 16 Race to find patients at risk of CJD. The Times. 30th January 2001; pp 1, 8.
5 Anthony D, Milne R. On-demand recombinant factor VIII for people with 17 Forbes C D, Barr R D, Reid G et al. Tranexamic acid in control of haemorrhage after
haemophilia A. Report to the Development and Evaluation Committee. 1997; 71. dental extraction in haemophilia and Christmas disease. Br Med J 1972; 2: 311-313.
6 United Kingdom Haemophilia Centre Directors Organisation Executive Committee. 18 Sindet-Pedersen S, Stenbjerg S. Effect of local antifibrinolytic treatment with
Guidelines on therapeutic products to treat Haemophilia and other hereditary tranexamic acid in hemophiliacs undergoing oral surgery. J Oral Maxillofac Surg
coagulation disorders. Haemophilia 1997; 3: 63-77. 1986; 44: 703-707.
7 Mannucci P M. Desmopressin (DDAVP) in the treatment of bleeding disorders: the 19 Minor P D. Are recombinant products really infection risk free? Haemophilia 2001; 7:
first twenty years. Haemophilia. 2000; 6(Suppl. 1): 60 - 67. 114-116.
8 Mannucci P M, Aberg M, Nilsson I M and Robertson B. Mechanism of plasminogen 20 Ehrenforth S, Kreuz W, Scharrer I, Linde R, Funk M, Gngr T, Krackhardt B, Kornhuber
activator and factor VIII increase after vasoactive drugs. Br J Haematol 1975; 30: 81-90. B. Incidence of development of factor VIII and factor IX inhibitors in haemophiliacs.
9 Mannucci P M, Bettega D, Cattaneo M. Patterns of development of tachyphylaxis in Lancet 1992; 339: 594-598.
patients with hemophilia and von Willebrand disease after repeated doses of 21 Jarvis L M, Davidson F, Hanley J P, Yap P L, Ludlam C A, Simmonds P. Infection with
desmopressin (DDAVP). Br J Haematol 1992; 82: 87. hepatitis G virus among recipients of plasma products. Lancet 1996; 348: 1352-1355.
10 Andersson I, Nilsson I M, Nilehn J E, Hedner U, Granstrand B, Melander B. 22 World Federation of Hemophilia. Factor VIII product shortage. Information Update (23
Experimental and clinical studies on AMCA, the antifibrinolytically active isomer of p- April 2001). www.wfh.org [accessed on 15 June 2001].
aminomethyl cyclohexane carboxylic acid. Scand J Haematol 1965; 2: 230-247. 23 Fiske J, Pitt Ford H E, Savidge G F, Smith M P. The expressed dental needs of patients
11 Astedt B. Clinical pharmacology of tranexamic acid. Scand J Gastroenterol 1987; 22 attending a Haemophilia Reference Centre. J Disabil Oral Health 2000; 1: 20-25.
(suppl 137): 22-25. 24 Roberts R E, McCory O F, Glasser J H et al. Dental care for handicapped children re-
12 Mannucci P M. Hemostatic drugs. N Engl J Med 1998; 339: 245-253. examined: II Dimensions of dental practice. J Public Health Dentistry 1978; 38: 136-147.
Fifty years ago
British Dental Journal, 21 December 1954
Scots wha hae!
The 75th Annual Conference of the B.D.A. will be held in Glasgow during the week beginning
July 4, 1955
The members of the West of Scotland Branch are the Scots wha hae the honour and the
privilege to let you know something of what they as hosts have to offer you during that week.
We ask you, first of all, to come to Glasgow, a friendly city of character and characters, and
hope to impress upon you during your visit that many of the less complimentary labels which
have described her bear no truth to her real identity, and we are hopeful that you will carry away
fond memories of Dear Old Glasgow Town
Br Dent J 1954
38 BRITISH DENTAL JOURNAL VOLUME 198 NO. 1 JANUARY 8 2005
You might also like
- Dental Management of Patients With HemophiliaDocument5 pagesDental Management of Patients With HemophiliaarjayNo ratings yet
- Discracia en TX DentalDocument24 pagesDiscracia en TX DentaliraizaNo ratings yet
- Fanc. AnemiaDocument8 pagesFanc. AnemiaLujainNo ratings yet
- 10.1007@s00784 014 1366 3Document10 pages10.1007@s00784 014 1366 3ammar slimanNo ratings yet
- jhm2616 AmDocument15 pagesjhm2616 Amkishore kumar meelNo ratings yet
- Fourth Stage HemostasisDocument9 pagesFourth Stage HemostasisAli MONo ratings yet
- Hemophilia A. Considerations For Dental Management of Pediatric PatientsDocument5 pagesHemophilia A. Considerations For Dental Management of Pediatric PatientsUlfa Yasmin ShahabNo ratings yet
- Reporte de 58 ExtraccionesDocument6 pagesReporte de 58 Extraccionesyisuskakaroto300No ratings yet
- DR - Syed Muhammad Ali Ms Oral and Maxillofacial Surgery (Resident) Under Supervision of Prof, DR - Syed Mahmood HaiderDocument22 pagesDR - Syed Muhammad Ali Ms Oral and Maxillofacial Surgery (Resident) Under Supervision of Prof, DR - Syed Mahmood Haiderكرار حيدر وهيبNo ratings yet
- Hemofilia C Dan DisfibrinogenemiaDocument6 pagesHemofilia C Dan DisfibrinogenemiaDavrina DavronNo ratings yet
- Haemophilia 1Document10 pagesHaemophilia 1mahadirrosNo ratings yet
- Bleeding Post ExtDocument2 pagesBleeding Post ExtNyitnyit Kunyit100% (1)
- BLT 09 320 PDFDocument16 pagesBLT 09 320 PDFFakhrur Rozy NasutionNo ratings yet
- Hemostasis 19-3-2012Document11 pagesHemostasis 19-3-2012Mateen ShukriNo ratings yet
- 2003 Purpura Trombocitopenica Idiopatica en AdultosDocument5 pages2003 Purpura Trombocitopenica Idiopatica en AdultosConrado Vera PinedaNo ratings yet
- Oral Care For Children With Leukaemia: SY Cho, AC Cheng, MCK ChengDocument6 pagesOral Care For Children With Leukaemia: SY Cho, AC Cheng, MCK Chengvefiisphepy83312No ratings yet
- Glanz MansDocument7 pagesGlanz Mansthroaty rhinoNo ratings yet
- Jurnalku OsccDocument4 pagesJurnalku OsccAndiOctafiantoNo ratings yet
- Secondary Disorders: Group 3Document33 pagesSecondary Disorders: Group 3Joseph VillamorNo ratings yet
- J Clin Apher 2020 Sep 17 Chuliber FaDocument8 pagesJ Clin Apher 2020 Sep 17 Chuliber FaFernando SousaNo ratings yet
- Nathwani 2019Document8 pagesNathwani 2019Marcelo Viejo RubioNo ratings yet
- Operativesplenectomy 0410 p129-133 PDFDocument5 pagesOperativesplenectomy 0410 p129-133 PDFAkbarHadityaNo ratings yet
- Dios1999 PDFDocument5 pagesDios1999 PDFGina MaulidaNo ratings yet
- Dental extractions protocol for HIV patientsDocument5 pagesDental extractions protocol for HIV patientsSaptiadi OktoraNo ratings yet
- Bloody Easy PDFDocument164 pagesBloody Easy PDFJenny JeongNo ratings yet
- 1 s2.0 S0140673603134058 MainDocument9 pages1 s2.0 S0140673603134058 MainΚωνσταντίνος ΤσίπηςNo ratings yet
- LEUKAEMIA AND ORTHDONTICS by AlmuzianDocument3 pagesLEUKAEMIA AND ORTHDONTICS by AlmuzianRahulLife'sNo ratings yet
- European Guidelines On Perioperative Venous.5Document12 pagesEuropean Guidelines On Perioperative Venous.5ionut.andruscaNo ratings yet
- Trombocytopenia in CaDocument7 pagesTrombocytopenia in CaanisaNo ratings yet
- Management of Bleeding in CancerDocument12 pagesManagement of Bleeding in CancerRoyan M. VarendraNo ratings yet
- HemophiliaDocument19 pagesHemophiliaAtiya HajjajNo ratings yet
- Inpatient Inherited Thrombophilia Testing: Choosing Wisely: Things We Do For No ReasonDocument4 pagesInpatient Inherited Thrombophilia Testing: Choosing Wisely: Things We Do For No Reasonkishore kumar meelNo ratings yet
- Dental Management of Hemophiliac ChildDocument6 pagesDental Management of Hemophiliac ChildMelisa RuthNo ratings yet
- Bleeding Rate After Tooth Extraction in Patients Under Oral Anticoagulant TherapyDocument6 pagesBleeding Rate After Tooth Extraction in Patients Under Oral Anticoagulant TherapyjhoselinNo ratings yet
- A Review of The Management of Childhood Immune Thrombo - Cytopenia - How Can We Provide An Evidence-Based ApproachDocument12 pagesA Review of The Management of Childhood Immune Thrombo - Cytopenia - How Can We Provide An Evidence-Based ApproachsolecitodelmarNo ratings yet
- A Rare Case of Factor X Deficiency AssociatedDocument16 pagesA Rare Case of Factor X Deficiency AssociatedRoss Mark PerandosNo ratings yet
- Buy The Book Mobile VersionsDocument4 pagesBuy The Book Mobile VersionsWafa AwadNo ratings yet
- Hemophilia: CPC Cram Like Hell NotesDocument9 pagesHemophilia: CPC Cram Like Hell NotesCitrusNo ratings yet
- 1-s2.0-S0278239117314350-mainDocument7 pages1-s2.0-S0278239117314350-mainCaio GonçalvesNo ratings yet
- Cancer PDFDocument9 pagesCancer PDFMihaela IonescuNo ratings yet
- 26 - 2 - 193 - Oral Surgery in Patients Undergoing Chemoradiation Therapy PDFDocument15 pages26 - 2 - 193 - Oral Surgery in Patients Undergoing Chemoradiation Therapy PDFTabishur RahmanNo ratings yet
- Oral Surgery in Patients Undergoing Chemoradiation TherapyDocument15 pagesOral Surgery in Patients Undergoing Chemoradiation TherapyTabishur RahmanNo ratings yet
- Complications and Management of Patients With Inherited Bleeding Disorders During Dental Extractions - A Systematic Literature ReviewDocument11 pagesComplications and Management of Patients With Inherited Bleeding Disorders During Dental Extractions - A Systematic Literature ReviewnatalyaNo ratings yet
- 14-Coagulation DisorderDocument51 pages14-Coagulation Disorderqjf7p2pstdNo ratings yet
- Hemostasis in Oral Surgery PDFDocument7 pagesHemostasis in Oral Surgery PDFBabalNo ratings yet
- Dental Care for Patients with Bleeding DisordersDocument8 pagesDental Care for Patients with Bleeding Disordersmamfm5No ratings yet
- Jurnal SistemikDocument3 pagesJurnal SistemikMariatun Zahro NasutionNo ratings yet
- Buy The Book Mobile VersionsDocument4 pagesBuy The Book Mobile VersionsWafa AwadNo ratings yet
- 1000 Laboratory Management of Haemolysed Samples Results of An RCPAQAP Survey - Ms Penny PetinosDocument37 pages1000 Laboratory Management of Haemolysed Samples Results of An RCPAQAP Survey - Ms Penny PetinosPAUL AVELINO CALLUPENo ratings yet
- Jurnal: Lila Esi Mustika, Amkg NIK: PK2013050Document11 pagesJurnal: Lila Esi Mustika, Amkg NIK: PK2013050lilaNo ratings yet
- Practice: Investigating An Incidental Finding of LymphopeniaDocument3 pagesPractice: Investigating An Incidental Finding of LymphopeniaramiroNo ratings yet
- 157 161 RadiotherapyDocument5 pages157 161 RadiotherapyEko SetiawanNo ratings yet
- MSM 27 359Document4 pagesMSM 27 359Tayta UmayuqNo ratings yet
- Management of Bleeding PDFDocument25 pagesManagement of Bleeding PDFGlory Owens AgbonkpoloNo ratings yet
- Oral Surgery in Liver Transplant Candidates: A Retrospective Study On Delayed Bleeding and Other ComplicationsDocument6 pagesOral Surgery in Liver Transplant Candidates: A Retrospective Study On Delayed Bleeding and Other Complicationsrahmawati isnaningrumNo ratings yet
- Int J of Urology - 2017 - Saluja - Venous Thromboembolism Prophylaxis in Urology A ReviewDocument5 pagesInt J of Urology - 2017 - Saluja - Venous Thromboembolism Prophylaxis in Urology A ReviewsofiaNo ratings yet
- Hematologic Disorders: JeffreyDocument582 pagesHematologic Disorders: JeffreyPalak GuptaNo ratings yet
- Assessment of Bleeding During Minor Oral Surgical Procedures and Extraction in Patients On Anticoagulant TherapyDocument11 pagesAssessment of Bleeding During Minor Oral Surgical Procedures and Extraction in Patients On Anticoagulant TherapyCindy Bernal MNo ratings yet
- Von Willebrand An Dental Rewport CasDocument4 pagesVon Willebrand An Dental Rewport CashospitalvitartedentalNo ratings yet
- Assesment Sex DisorderDocument13 pagesAssesment Sex DisorderSastra SinagaNo ratings yet
- Jurnal Kwalitatif 3Document17 pagesJurnal Kwalitatif 3Sastra SinagaNo ratings yet
- Assesment Sex DisorderDocument13 pagesAssesment Sex DisorderSastra SinagaNo ratings yet
- Pengembangan Format Pengkajian OremDocument20 pagesPengembangan Format Pengkajian OremMiftakhul KhoeryNo ratings yet
- Congenital Ovarian CystDocument4 pagesCongenital Ovarian CystSastra SinagaNo ratings yet
- Massage For CancerDocument5 pagesMassage For CancerSastra SinagaNo ratings yet
- Plebitis in NeonatusDocument7 pagesPlebitis in NeonatusSastra SinagaNo ratings yet
- Pengembangan Format Pengkajian OremDocument20 pagesPengembangan Format Pengkajian OremMiftakhul KhoeryNo ratings yet
- Phelibitis AlsoDocument5 pagesPhelibitis AlsoSastra SinagaNo ratings yet
- End-Of-life Decisions. Ethical PerspectiveDocument11 pagesEnd-Of-life Decisions. Ethical PerspectiveSastra SinagaNo ratings yet
- Akupuncture PainDocument7 pagesAkupuncture PainSastra SinagaNo ratings yet
- Selenium Nutrient For Hiv PDFDocument6 pagesSelenium Nutrient For Hiv PDFSastra SinagaNo ratings yet
- OK art-3A10.1186-2Fs12910-015-0001-4Document10 pagesOK art-3A10.1186-2Fs12910-015-0001-4Sastra SinagaNo ratings yet
- Hyperbaric For Autism 2Document15 pagesHyperbaric For Autism 2Sastra SinagaNo ratings yet
- Nutrition For HivDocument49 pagesNutrition For HivSastra SinagaNo ratings yet
- Therapy Bermain Journal PDFDocument16 pagesTherapy Bermain Journal PDFSastra SinagaNo ratings yet
- Hiv NutritionDocument79 pagesHiv NutritionSastra SinagaNo ratings yet
- Hyperbaric For Autism 2Document15 pagesHyperbaric For Autism 2Sastra SinagaNo ratings yet
- Nutrition 4 For HivDocument60 pagesNutrition 4 For HivSastra SinagaNo ratings yet
- Hyperbaric For Autism 2Document15 pagesHyperbaric For Autism 2Sastra SinagaNo ratings yet
- Disturbed Thought Process NCP Gallano May 22 2018Document3 pagesDisturbed Thought Process NCP Gallano May 22 2018Charles Mallari ValdezNo ratings yet
- Management of Medically Compromised PatientsDocument70 pagesManagement of Medically Compromised PatientsPriyanka WadhawanNo ratings yet
- Essay Catcher in The RyeDocument4 pagesEssay Catcher in The Ryeapi-256192196No ratings yet
- Pharmacokinetics of Intravenous FK027 in Healthy VolunteersDocument10 pagesPharmacokinetics of Intravenous FK027 in Healthy VolunteersKharisma Aditya Rasyid Tf'ersNo ratings yet
- CSP Core Standards 2005 0Document68 pagesCSP Core Standards 2005 0Irina MafteiNo ratings yet
- Protein TherapeuticsDocument14 pagesProtein TherapeuticsSumanth Kumar ReddyNo ratings yet
- Bobath Concept Effectiveness in Stroke RehabDocument15 pagesBobath Concept Effectiveness in Stroke RehabAfrizal BintangNo ratings yet
- Chest Physiotherapy in Mechanically Ventilated Children A ReviewDocument10 pagesChest Physiotherapy in Mechanically Ventilated Children A Reviewmrizki_1No ratings yet
- Dosage Cal ProblemsDocument13 pagesDosage Cal ProblemsNatalie DukesNo ratings yet
- Bronchitis: Kelompok IDocument14 pagesBronchitis: Kelompok ILinda Permata Sari100% (1)
- SAS #14 - Decent Work Employment - Transcultural NursingDocument9 pagesSAS #14 - Decent Work Employment - Transcultural NursingBless O DumagoNo ratings yet
- Sexual Development and OrientationDocument43 pagesSexual Development and OrientationSaqib AhmedNo ratings yet
- The Ashtavaidya Medical Tradition of KeralaDocument5 pagesThe Ashtavaidya Medical Tradition of Keralahari haraNo ratings yet
- Tumor MarkersDocument14 pagesTumor MarkersPatrick LizarondoNo ratings yet
- Dossier RPG EnglishDocument15 pagesDossier RPG EnglishtetevoNo ratings yet
- Current Concepts of Plyometric ExerciseDocument27 pagesCurrent Concepts of Plyometric ExerciseMustafid Alwi AlvaroNo ratings yet
- Goodman and Gilman39s Manual of Pharmacology and Therapeutics Latest EditionDocument3 pagesGoodman and Gilman39s Manual of Pharmacology and Therapeutics Latest EditionLinda0% (1)
- Chest Pain Investigation, Diagnosis and TreatmentDocument4 pagesChest Pain Investigation, Diagnosis and TreatmentHadsabsaNo ratings yet
- Vascular Diseases: Idar Mappangara Department of Cardiology Hasanuddin UniversityDocument31 pagesVascular Diseases: Idar Mappangara Department of Cardiology Hasanuddin Universitynurliah armandNo ratings yet
- Gastric Ulcer Nursing CareDocument6 pagesGastric Ulcer Nursing CareAesthea BondadNo ratings yet
- CaseDocument3 pagesCasebLessy_july16No ratings yet
- Biological PollutantsDocument25 pagesBiological PollutantsM.SohailNo ratings yet
- Fever in The Neurointensive Care UnitDocument9 pagesFever in The Neurointensive Care UnitDiayanti TentiNo ratings yet
- Insulin Degludec PDFDocument19 pagesInsulin Degludec PDFLilisNo ratings yet
- ACT For Psychosis Recovery A Practical Manual For Group-Based Interventions Using Acceptance and Commitment Therapy by Emma K. O'Donoghue Eric M.J. Morris Joseph E. Oliver Louise C. Johns Steven C. HaDocument286 pagesACT For Psychosis Recovery A Practical Manual For Group-Based Interventions Using Acceptance and Commitment Therapy by Emma K. O'Donoghue Eric M.J. Morris Joseph E. Oliver Louise C. Johns Steven C. HaHarriet Osakwe0% (1)
- Pityriasis AlbaDocument6 pagesPityriasis AlbaLee Eng SiangNo ratings yet
- Nick Franks - Chapter 14 Instruments and Codes FN v2 - Rev 3 For Radionic Journal 17.4.15Document19 pagesNick Franks - Chapter 14 Instruments and Codes FN v2 - Rev 3 For Radionic Journal 17.4.15evandrojsilvaNo ratings yet
- Evaluation of Psychiatric Disorders: Key ConceptsDocument12 pagesEvaluation of Psychiatric Disorders: Key ConceptsraniNo ratings yet
- Calgevax BSG Bugarska EngDocument10 pagesCalgevax BSG Bugarska EngAnonymous idBsC1No ratings yet
- Skin Hydrating and Whitening Effects of Vitamin C and Glutathione in Asian Skin Types - PRIME JournalDocument9 pagesSkin Hydrating and Whitening Effects of Vitamin C and Glutathione in Asian Skin Types - PRIME JournalNovia SaragihNo ratings yet