Professional Documents
Culture Documents
Oral Infections
Uploaded by
mirfanulhaqCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oral Infections
Uploaded by
mirfanulhaqCopyright:
Available Formats
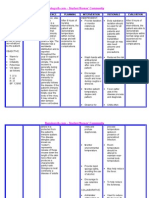
ORAL INFECTIONS
Viral infections
Herpes
Human Papilloma Viruses
Coxsackie
Paramyxoviruses
Retroviruses: HIV
Bacterial Infections
Dental caries
Periodontal disease
Pharyngitis and tonsillitis
Scarlet fever
Tuberculosis - Mycobacterium
Syphilis -Treponema pallidum
Actinomycosis Actinomyces
Gonorrhea Neisseria gonorrheae
Osteomyelitis - Staphylococcus
Fungal infections (Mycoses)
Candida albicans
Histoplasma capsulatum
Coccidioides
Blastomyces dermatitidis
Aspergillus
Zygomyces
CDE (Oral Pathology and Oral Medicine) 1 ORAL INFECTIONS
VIRAL INFECTIONS
Viruses consist of:
Single or double strand DNA or RNA
Protein coat (capsid)
Often with an Envelope.
Obligate intracellular parasites enters host cell in order to replicate.
3 most commonly encountered virus families in the oral cavity:
Herpes virus
Papovavirus (HPV)
Coxsackie virus (an Enterovirus).
DNA Viruses:
A. HUMAN HERPES VIRUS (HHV) GROUP:
1. HERPES SIMPLEX VIRUS
Double stranded DNA virus.
2 types: HSV-1 and HSV-2.
Lytic to human epithelial cells and latent in neural tissue.
Clinical features:
May penetrate intact mucous membrane, but requires breaks in skin.
Infects peripheral nerve, migrates to regional ganglion.
Primary infection, latency and recurrence occur.
99% of cases are sub-clinical in childhood.
Primary herpes: Acute herpetic gingivostomatitis.
1% of cases; severe symptoms.
Children 1 - 3 years; may occur in adults.
Incubation period 3 8 days.
Numerous small vesicles in various sites in mouth; vesicles rupture to form multiple
small shallow punctate ulcers with red halo.
Child is ill with fever, general malaise, myalgia, headache, regional lymphadenopathy,
excessive salivation, halitosis.
Self limiting; heals in 2 weeks.
Immunocompromised patients may develop a prolonged form.
Secondary herpes: Recurrent oral herpes simplex.
Presents as: a) herpes labialis (cold sores) or
b) recurrent intra-oral herpes palate or gingiva.
Seen in adults (approx 30%).
Predisposing factors: sunlight, fever, allergy, trauma, menstruation,
immunosuppression.
Herpes labialis:
Prodrome of burning and tenderness.
Intraepithelial blisters which burst, crust and heal in 10 -12 days.
Recurrent intra-oral herpes (uncommon):
Vesicles rupture early, form ulcers with red or white bases.
Heal in 10 to 12 days.
CDE (Oral Pathology and Oral Medicine) 2 ORAL INFECTIONS
Herpetic whitlow.
Primary or secondary infection localized to hands or fingers, acquired by direct contact
with active lesion.
Histopathology:
Keratinocytes show ballooning degeneration.
Nucleus: margination of chromatin, eosinophilic nuclear inclusions.
Multinucleate giant cells (syncytial epithelial cells).
Vesicles, which rupture and become erosions.
Diagnosis: Mostly on clinical presentation, but occasionally by Biopsy; Smear; Culture;
Fluorescent antibody or Immunohistochemistry; Serology.
Treatment:
Acyclovir, valacyclovir or penciclovir.
Topical (localised or recurrent lesions) or systemic.
2. VARICELLA-ZOSTER VIRUS (HHV3)
Similar to HSV.
Primary infection: Chicken pox.
Recurrent infection: herpes zoster or shingles.
Clinical features:
Chickenpox (Varicella):
90% of the adult population will contact the virus and harbour it in its latent form.
Generalized, usually itchy, maculo-papular rash of the skin.
Vesicles and pustules occur.
Malaise, fever, minor oral cavity lesions (vesicles/ulcers).
Herpes zoster (shingles):
Recurrent lesion. Affects 10 20% of the population
Common in elderly and immunocompromised.
Skin: unilateral linear vesicular rash outlining the cutaneous distribution of affected
peripheral nerves.
Trigeminal nerve: unilateral facial and oral lesions may develop.
Pain, paresthesia.
Potential for post-herpetic neuralgia.
Histopathology:
Virtually identical to HSV.
Acantholysis, Tzanck cells, with nuclear margination of chromatin and occasional multi-
nucleation.
Diagnosis:
History, clinical appearance (rash), (Smear, Culture, Serology).
Treatment:
Usually heals spontaneously within about 2 weeks for Chickenpox or 6 weeks for
Shingles.
Herpes zoster: Acyclovir or Valacyclovir. IV in severe cases.
CDE (Oral Pathology and Oral Medicine) 3 ORAL INFECTIONS
B. HUMAN PAPILLOMA VIRUS
1. SQUAMOUS PAPILLOMA
Definition:
benign proliferation of stratified squamous epithelium resulting in a papillary or
verruciform mass
Etiology
Human papilloma virus (HPV) types 6 and 11?
Clinical features:
M=F; 30 50 years.
Site: Tongue; Lips; Soft palate (common); any oral surface.
Soft, painless, pedunculated, exophytic nodule with surface finger-like projections
(cauliflower-like).
Normal colour.
Solitary, 0.5mm; occasionally multiple lesions occur.
Histological features:
Non-Keratinised stratified (not acanthotic) squamous epithelium.
Finger-like projections with Fibrous connective tissue cores.
Sometimes inflammation in connective tissue.
Treatment:
Conservative surgical excision.
2. VERRUCA VULGARIS
Definition:
a benign virus-induced, focal hyperplasia of stratified squamous epithelium.
Etiology
HPV types 2, 4,.
Clinical features:
Frequent in children, but also in older people.
Site: skin of hands most common.
Painless papule, papillary projections, rough surface.
Usually sessile, 5mm diameter.
Oral lesions almost always white.
Histological features:
Hyperkeratotic stratified squamous epithelium, arranged in chevron-like projections.
Connective tissue cores, chronic inflammatory cells.
Rete ridges converge to centre of lesion, creating a cupping effect.
Prominent granular cell layer.
Koilocytes in superficial spinous layer.
Treatment:
CDE (Oral Pathology and Oral Medicine) 4 ORAL INFECTIONS
Conservative surgical excision.
Cryotherapy on skin and topical medication.
2/3 will disappear spontaneously, especially in children.
3. CONDYLOMA ACUMINATUM
Definition:
A virus-induced proliferation of stratified squamous epithelium of the genitalia, peri-anal
region, mouth and larynx.
Etiology
HPV types 6, 11.
High risk types 16, 18 also found, especially in anogenital lesions.
Clinical features:
Lesions usually develop at site of sexual contact.
More frequent in teenagers and young adults, but may affect any age group.
Oral lesions:
Labial mucosa, soft palate, lingual frenum, dorsum of tongue.
Sessile, pink, well-demarcated non-tender mass, with short, blunted surface projections.
Usually clustered.
1 3cm (sometimes larger).
Histological features:
Acanthotic stratified squamous epithelium, mildly keratotic with blunt broad surface
papillary projections, and thin connective tissue cores.
Keratin filled crypts between prominences.
Koilocytes in prickle cell zone (spinous layer).
Treatment:
Conservative surgical excision.
In the anogenital area, condylomata caused by HPV types 16 and 18 have been associated
with malignant transformation.
4. FOCAL EPITHELIAL HYPERPLASIA
Definition:
Virus-induced localized proliferation of squamous epithelium.
Etiology
HPV type 13, possibly 32.
Clinical features:
Usually seen in childhood; no gender bias.
Sites: Labial, buccal and lingual mucosa.
Multiple soft non-tender, smooth surfaced, flattened or rounded papules, small (3 10
mm) clustered, color of normal mucosa.
Cobblestone appearance.
Histological features:
Abrupt acanthosis of oral epithelium.
CDE (Oral Pathology and Oral Medicine) 5 ORAL INFECTIONS
Thickened mucosa extends upward, above normal surface, so that lesional rete ridges are
at same level as normal rete ridges.
Rete ridges wide, club-shaped or battle-axe shaped.
Koilocytes, and mitosoid cells.
Treatment:
Spontaneous regression.
5. ORAL SQUAMOUS CELL CARCINOMA
Evidence suggests that there is a role for one or more of HPV16, 18, and possibly 31, 33 in the pathogenesis of some
oral squamous cell carcinomas.
RNA Viruses:
A. PICORNA VIRUS: COXSACKIE
Picornavirus.
Coxsackie A viruses cause herpangina, hand foot and mouth disease, and acute
lymphonodular pharyngitis.
Most cases arise summer/early fall.
Spread: fecal-oral route.
Clinical features:
Mainly children; spread aided by crowding, poor hygiene.
Selflimiting disease.
1. Herpangina:
Multiple Coxsackie subtypes.
Sore throat, dysphagia, fever. Occasional cough, rhinorrhea, anorexia, vomiting,
headache, myalgia.
Oral lesions, confined to posterior: sites are soft palate, tonsil; begin as red macules and
petechiae, form vesicles and ulcerate (2-4mm).
Heals within 7 10 days.
2. Hand-foot-and-mouth disease.
Coxsackie subtypes A9 and A16.
Sore throat, dysphagia, fever. Occasional cough, rhinorrhea, anorexia, vomiting,
headache, myalgia. (flu-like symptoms).
Skin rash on palms and soles. Oral and hand lesions almost always present; other sites
variable.
Oral lesions similar to herpangina but not confined to posterior mouth.
3. Acute lymphonodular pharyngitis.
Sore throat, fever, mild headache.
Yellow to dark pink nodules develop on soft palate and/or tonsillar pillars.
Nodules are hyperplastic lymphoid aggregates.
Resolves within 7 10 days.
CDE (Oral Pathology and Oral Medicine) 6 ORAL INFECTIONS
Histology:
Epithelium shows inter- and intracellular edema; extensive spongiosis and formation of
intraepithelial vesicle in Herpangina and Hand Foot and Mouth Disease (not for Acute
lymphonodular pharyngitis).
Epithelial necrosis and ulceration follow.
Diagnosis:
Clinical features; rare culture and serology.
Treatment:
Disease is self-limiting.
Symptomatic in more severe cases.
B. RETROVIRUS
ACQUIRED IMMUNE DEFICIENCY SYNDROME (AIDS)
Definition:
a human immunodeficiency state caused by the human immunodeficiency virus (HIV)
and associated with several life-threatening opportunistic infections and malignant
neoplasms.
Etiology:
Human immunodeficiency virus (HIV).
Susceptible individuals and predisposing factors:
Homosexual/bisexual men (sexual intercourse).
Intravenous drug users (contaminated needles).
Haemophiliacs (via infected blood transfusions).
Heterosexual contacts (sexual intercourse).
Vertical transmission mother to child (in-utero).
Clinical features:
Fever, generalized malaise, unexplained weight loss, night sweats, lymphadenopathy
(persistent cervical, axillary and inguinal), diarrhoea, persistent cough, infections.
Associated infections:
Pneumocystis carinii (pneumocystis pneumonia).
Candidiasis (oral and genital).
Herpes (oral, genital, ocular, encephalitis).
Cytomegalovirus (CMV) in kidney, lung and brain.
Mycobacterium avium intracellulare.
Associated malignant neoplasms:
Kaposis sarcoma (hard palate, gingiva, skin).
Lymphoma.
Squamous cell carcinoma of the oral cavity.
Oral findings:
Hairy leukoplakia on lateral borders of tongue.
Candidiasis.
Recurrent herpes simplex infections.
Kaposis sarcoma association with HHV 8.
CDE (Oral Pathology and Oral Medicine) 7 ORAL INFECTIONS
Lymphoma (hard palate; tonsils; intra-bony in mandible and maxilla) some associated
with Epstein Barr virus.
Salivary gland cystic lymphoepithelial lesion.
AIDS periodontitis (rapidly progressive); necrotising ulcerative gingivitis.
Aphthous-like ulcers.
Treatment:
HAART highly active antiretroviral therapy.
Nucleoside reverse transcriptase inhibitors
o e.g. AZT (azidothymidine) [RETROVIR]
o Slows replication of HIV does not kill the virus.
o Viral cultures remain positive but fewer in number.
o Acts to inhibit reverse transcriptase which can terminate viral DNA-chain
elongation.
o Slows progress of disease but not a cure.
o Patients feel better.
Non-Nucleoside reverse transcriptase inhibitors e.g. nevirapine
Protease inhibitors.
CDE (Oral Pathology and Oral Medicine) 8 ORAL INFECTIONS
BACTERIAL INFECTIONS
Bacteria are prokaryotes: lack membrane bound nucleus and cell organelles.
Consist of cell wall:
Thick: Gram positive; Thin: Gram negative.
Cell membrane.
Most synthesize DNA, RNA and proteins.
Many have flagellae, and/or pili.
Healthy people may carry:
1012 bacteria on skin.
1010 in mouth.
1014 in GIT.
TUBERCULOSIS
Etiology:
Mycobacterium tuberculosis, an acid fast bacillus.
TB is a granulomatous disease characterized by granulomatous inflammation which
includes epithelioid histiocytes + multinucleated giant cells + lymphocytes.
Primarily a lung disease but can affect any organ.
Clinical features:
Chills, fever, weight loss, fatigue, malaise, persistent cough with haemoptysis.
Source of infection: air borne droplet.
Tests: BCG = Bacille Calmette-Guerin.
PPD = purified protein derivative (Mantoux test).
OT = old tuberculin.
Oral lesions: 20% of patients; usually ulcer of tongue. N.B. dentist is at risk of infection
from direct contact or droplet infection. Organisms are seen in 45% of oral washings.
Histology:
Granulomatous inflammation with or without caseous (cheese-like) necrosis.
Ziehl-Neelsen stains AFBs red.
Treatment:
INH = isoniazid.
Rifampin
Duration: 18 to 24 months.
Mycobacterium leprae: causes leprosy.
Mycobacterium avium intracellulare: seen in AIDS.
CDE (Oral Pathology and Oral Medicine) 9 ORAL INFECTIONS
SYPHILIS
Etiology:
Treponema pallidum (a spirochete).
Identified by silver stains (Warthin-Starry, Steiner or Leveditti).
Clinical features:
Transmission: a. Sexual intercourse with infected partner.
b. contact with open wound (e.g. dentists).
3 clinical stages occur for Acquired syphilis:
A. Primary syphilis (lesion is the Chancre).
Ulcer (chancre) appears 1-3 weeks after contact.
Site: penis, vulva, cervix (95% of cases).
Oral: lip, tongue, palate, tonsil, buccal mucosa.
Chancre is indurated, painless, (or painful + regional lymphadenopathy).
Ulcer exhibits many spirochetes if smeared.
Histology: ulcer with many plasma cells.
Heals within a few weeks.
B. Secondary syphilis (skin rash and mucous patches).
1-3 months after primary lesion.
Skin rash: macules and papules.
Oral: mucous patch and snail track ulcers.
Mucous patches are highly infectious.
Heals in a few weeks, but may recur many times.
C. Tertiary Syphilis:
1-3 or more years after secondary lesions.
Manifestations:
Gumma (necrotic tumour-like mass exhibiting granulomatous inflammation).
Gummatous perforation of the hard palate.
Syphilitic glossitis (previously associated with carcinoma).
Cardiovascular lesions: aortic aneurysms.
CNS: neuronal loss; dementia.
Not infectious.
Congenital syphilis:
Acquired in-utero from infected mother.
Rare today because of routine serologic tests.
Features:
frontal bossing of skull.
Short maxilla with high palatal vault.
Saddle nose.
Hypoplastic teeth (Hutchinsons incisors and Mulberry molars).
Rhagades: fissures around mouth.
Hutchinsons triad:
A. mulberry molars + Hutchinsons incisors.
Interstitial keratitis (scarred cornea).
8th nerve deafness.
Serologic tests for syphilis:
VDRL = venereal disease research laboratory test.
CDE (Oral Pathology and Oral Medicine) 10 ORAL INFECTIONS
Wasserman, STS = standard test for syphilis,
Treatment:
Antibiotics (penicillin).
ACTINOMYCOSIS
Etiology:
Actinomyces species (A. bovis, israeli). N.B. this organism is a bacterium, not a fungus,
although it has been called a ray fungus.
The organism attracts calcium, and causes calculus formation calculus in the pus
formed during such an infection has been termed sulphur granules.
Clinical features:
Cervicofacial (most common type; 66%).
Pulmonary.
Abdominal.
Histology:
Induces abscesses with fistula formation.
Diagnosis: calcified colonies of organisms in a sea of neutrophils (pus).
Treatment:
Penicillin or tetracycline.
GONORRHEA
Etiology:
Neisseria gonorrhoeae a gram negative paired coccus.
Clinical features:
Spread: sexual contact. Organism sensitive to drying and cannot penetrate intact stratified
squamous epithelium.
Acute purulent inflammation and discharge.
Males: anterior urethra affected. Females: cervix, endometrium, fallopian tubes.
Complications: bacteraemia, myalgia, arthralgia, polyarthritis, dermatitis with skin rash.
Oropharyngeal involvement in 20% of patients. Transmission by fellatio, kissing,
cunnilingus therefore majority reported in females or homosexual men.
Sore throat; diffuse oropharyngeal erythema. Requires a large dose for oral lesions since saliva is a hostile
environment for this bacterium.
Shallow, irregular painful ulcers. Edema with scattered pustules.
Diagnosis: gram stain shows gram negative diplococci (within neutrophils).
Treatment:
Cephalosporins (ceftriaxone) and doxycycline.
CDE (Oral Pathology and Oral Medicine) 11 ORAL INFECTIONS
FUNGAL INFECTIONS
Fungi are eukaryotes, which have thick cell walls and ergosterol-containing cell membranes.
Grow as budding yeasts or as slender filamentous hyphae.
Fungi may cause superficial or deep infections.
Superficial infections involve skin, mucosa, hair, nails.
Deep fungal infections spread systemically and invade tissue, destroying vital organs in
immunocompromised hosts, but heal in otherwise normal hosts.
CANDIDIASIS (CANDIDOSIS; MONILIASIS)
Etiology:
Candida albicans.
Most common oral fungal infection in humans.
Common commensal 30 -50% of people.
Spores are non-pathogenic; hyphae are pathogenic.
3 general factors determine whether clinical evidence of infections exists:
Immune status of the host.
Oral mucosal environment.
The strain of Candida albicans.
Clinical types of Candidiasis
1. Pseudomembranous candidiasis (Thrush).
Occurs in:
Infants who acquire infection at birth.
Adults using long-term broad spectrum antibiotics.
Diabetics.
Immune dysfunction: leukemia, HIV positive patients.
Chemotherapy and radiation treated patients.
Mucosa covered by white coating (pseudomembrane) resembling cottage cheese or
curdled milk.
Pseudomembrane can be scraped off, leaving red area.
Occurs on buccal mucosa, palate, tongue.
Smear with PAS stain reveals Candida hyphae.
2. Erythematous (atrophic) candidiasis.
a. Acute atrophic candidiasis.
Red bald tongue.
Follows course of broad spectrum antibiotics.
b. Central papillary atrophy of the tongue (Median rhomboid glossitis).
Well demarcated red zone in midline posterior tongue due to loss of filiform
papillae.
May be associated with Candidal infection at other sites in the mouth: termed
Chronic multifocal candidiasis.
c. Angular cheilitis (perlche).
Erythema, fissuring and scaling at commissures of mouth.
Causes: 20% Candida albicans alone.
CDE (Oral Pathology and Oral Medicine) 12 ORAL INFECTIONS
60% C. albicans and Staphylococcus aureus.
20% S. aureus alone.
Predisposing factors include iron deficiency anaemia, vitamin (riboflavin
deficiency), over-closed vertical dimension, immunosuppression.
d. Denture stomatitis (chronic atrophic candidiasis).
Erythema, sometimes with petechiae, on denture bearing surfaces of maxilla.
Asymptomatic; patient wears denture continuously.
Smears with PAS stain usually reveals Candida hyphae.
3. Chronic hyperplastic candidiasis.
White patch that cannot be removed by scraping.
Usually on anterior buccal mucosa.
Histology: Hyperparakeratosis, acanthosis of the epithelium; fungal hyphae and
neutrophil micro-abscesses (Munro abscesses) in superficial epithelium; chronic
inflammatory cell infiltrate in superficial connective tissue.
Diagnosis: presence of C. albicans hyphae in lesion, and resolution of the lesion after
antifungal therapy.
4. Mucocutaneous candidiasis.
Group of sporadic or inherited immune deficiency disorders which result in candidiasis
of the skin and mucous membranes.
Oral lesions appear as chronic hyperplastic candidiasis.
Treatment of candidiasis.
Nystatin (Mycostatin):
Effective and safe, but bitter taste may affect patient compliance.
Ketoconazole ((Nizoral):
Effective but can cause liver damage, therefore liver enzymes should be monitored
during treatment. Use minimal effective dose, since in large doses it can also cause
adrenal suppression and male hypogonadism.
Fluconazole (Diflucan):
More effective than ketoconazole, well absorbed, requires only once daily dosing.
Disadvantage: interaction with other drugs such as phenytoin (Dilantin), oral
hypoglycaemics and warfarin compounds.
MUCORMYCOSIS (ZYGOMYCOSIS; PHYCOMYCOSIS).
An opportunistic fungal infection occurring in debilitated patients, especially diabetics,
patients on chemotherapy, patients on steroids.
Etiology: Organisms of the class Zygomycetes, including Mucor and Rhizopus.
Organism exhibits large, non-septate hyphae which branch at obtuse angles.
Clinical features:
Affects various sites, but the rhinocerebral form is most relevant to the oral health care
provider.
Occurs mainly in diabetics with maxillary sinusitis.
May present as a hemorrhagic ulcer or maxillary alveolar ridge, as a result of extension
from the antrum.
Histology:
Necrotic tissue caused by vascular thrombosis; organisms tend to invade blood vessels.
CDE (Oral Pathology and Oral Medicine) 13 ORAL INFECTIONS
Organisms are present in superficial tissues or within sinus.
Chronic inflammatory cell infiltrate.
Treatment:
Control primary underlying disease (diabetics).
Surgically remove the necrotic tissue.
Amphotericin B.
OTHER ORAL FUNGAL DISEASES IN ONTARIO
Histoplasmosis - occasionally
Cryptococcosis - rarely
Coccidiodomycosis - rarely
Paracoccidiodomycosis - rarely
Blastomycosis - rarely
Aspergillosis - occasionally
Mucormycosis (Zygomycosis) - occasionally
CDE (Oral Pathology and Oral Medicine) 14 ORAL INFECTIONS
You might also like
- Alveolar bone formation and structureDocument16 pagesAlveolar bone formation and structuremirfanulhaqNo ratings yet
- Gingival InflammationDocument19 pagesGingival InflammationmirfanulhaqNo ratings yet
- Pros QuestionsDocument7 pagesPros QuestionsmirfanulhaqNo ratings yet
- Pros Exam 1 2002Document8 pagesPros Exam 1 2002mirfanulhaqNo ratings yet
- Pros Exam 1 2003Document8 pagesPros Exam 1 2003mirfanulhaqNo ratings yet
- Pros Exam 1 2002Document8 pagesPros Exam 1 2002mirfanulhaqNo ratings yet
- Comprehensive Periodontal Exam GuideDocument40 pagesComprehensive Periodontal Exam GuideKavin SandhuNo ratings yet
- Anticoagulation GuidelinesDocument2 pagesAnticoagulation GuidelinesmirfanulhaqNo ratings yet
- Adhesion SystemsDocument13 pagesAdhesion SystemsTolean AndreeviciNo ratings yet
- Pulp Protection Methods and MaterialsDocument13 pagesPulp Protection Methods and MaterialsmirfanulhaqNo ratings yet
- Peds Restorative PDFDocument4 pagesPeds Restorative PDFmirfanulhaqNo ratings yet
- Fundamentals of SalivaDocument15 pagesFundamentals of SalivasreedamNo ratings yet
- Wound Healing PDFDocument7 pagesWound Healing PDFmirfanulhaqNo ratings yet
- Management of Cracked TeethDocument6 pagesManagement of Cracked Teethsaifuddin suhri100% (2)
- Complications in Dentoalveolar Surgery PDFDocument37 pagesComplications in Dentoalveolar Surgery PDFmirfanulhaqNo ratings yet
- Making Sense of Mouth Ulceration 6Document3 pagesMaking Sense of Mouth Ulceration 6mirfanulhaqNo ratings yet
- 2 Saliva PhysiologyDocument20 pages2 Saliva PhysiologyvelangniNo ratings yet
- Pulp 2008 HandoutDocument7 pagesPulp 2008 HandoutNemanja MiticNo ratings yet
- Scully Oral UlcersDocument3 pagesScully Oral UlcersdeenmNo ratings yet
- Guide to Fluoride TherapyDocument4 pagesGuide to Fluoride TherapymirfanulhaqNo ratings yet
- Pulp Protection Methods and MaterialsDocument13 pagesPulp Protection Methods and MaterialsmirfanulhaqNo ratings yet
- Scully Oral UlcersDocument3 pagesScully Oral UlcersdeenmNo ratings yet
- Making Sense of Mouth Ulceration 4Document4 pagesMaking Sense of Mouth Ulceration 4mirfanulhaqNo ratings yet
- Oral Healthcare Considerations For The Pregnant WomanDocument4 pagesOral Healthcare Considerations For The Pregnant WomanmirfanulhaqNo ratings yet
- Making Sense of Mouth Ulceration 6Document3 pagesMaking Sense of Mouth Ulceration 6mirfanulhaqNo ratings yet
- Making Sense of Mouth Ulceration 5Document3 pagesMaking Sense of Mouth Ulceration 5mirfanulhaqNo ratings yet
- Making Sense of Mouth Ulceration 3Document4 pagesMaking Sense of Mouth Ulceration 3mirfanulhaqNo ratings yet
- Opath - Most Common ListDocument4 pagesOpath - Most Common ListmirfanulhaqNo ratings yet
- Scully Oral UlcersDocument3 pagesScully Oral UlcersdeenmNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Azeem English Magazine Vol. 22 Issue 2Document68 pagesAzeem English Magazine Vol. 22 Issue 2Raheel AsgharNo ratings yet
- Amity Institute of Occupational TherapyDocument28 pagesAmity Institute of Occupational Therapyamandeep kaurNo ratings yet
- LB 1 April 2019Document300 pagesLB 1 April 2019Talitha FameNo ratings yet
- Pediatric OSCE Pictures: For UndergraduatesDocument70 pagesPediatric OSCE Pictures: For UndergraduatesShehab MhmdNo ratings yet
- Varicella Infection Nursing Care PlanDocument5 pagesVaricella Infection Nursing Care PlanKismet SummonsNo ratings yet
- Biology of Blood and Marrow TransplantationDocument7 pagesBiology of Blood and Marrow Transplantationindah sariNo ratings yet
- NURSING CARE PLAN Chicken PoxDocument2 pagesNURSING CARE PLAN Chicken Poxderic87% (62)
- Opportunistic Infections PDFDocument88 pagesOpportunistic Infections PDFironbuang100% (1)
- Chain of InfectionDocument8 pagesChain of InfectionDonnaline Requina VillariasNo ratings yet
- 2nd MAPEH 4Document2 pages2nd MAPEH 4Edmar MejiaNo ratings yet
- Tabel IcdDocument214 pagesTabel IcdSusilo HendroNo ratings yet
- Fever and RashDocument18 pagesFever and RashJosiah Noella BrizNo ratings yet
- What Is Reye's SyndromeDocument3 pagesWhat Is Reye's SyndromeRanvabesa Cakra Laksa CitaNo ratings yet
- Approach To Fever With RashDocument35 pagesApproach To Fever With RashSenthilnathan ANo ratings yet
- Beauty Therapist - Participant HandbookDocument294 pagesBeauty Therapist - Participant HandbookNikid AlisonNo ratings yet
- Virology TableDocument10 pagesVirology TablekevinNo ratings yet
- Nclex Random Fact To StudyDocument431 pagesNclex Random Fact To StudyNeko Neko100% (1)
- Communicable Disease Nursing GuideDocument199 pagesCommunicable Disease Nursing GuideG Fab100% (2)
- Nsg6435 Soap Note 2Document7 pagesNsg6435 Soap Note 2Hephzibah Beulah100% (1)
- Opportunistic InfectionsDocument88 pagesOpportunistic InfectionszamadulaNo ratings yet
- Pediatrics Complete Study Guide 1Document116 pagesPediatrics Complete Study Guide 1Franko IvankaNo ratings yet
- Viral Skin Infections: Verrucae ValgarusDocument14 pagesViral Skin Infections: Verrucae Valgarusمسلم هاشم منافNo ratings yet
- ChickenpoxDocument5 pagesChickenpoxShan MunozNo ratings yet
- Dermatitis Area Del Pañal Usa 2017 7 PagDocument7 pagesDermatitis Area Del Pañal Usa 2017 7 PagOmaindhiNo ratings yet
- MICROBIOLOGY OLD EXAM QUESTIONS ON VIRUSES AND VIROLOGYDocument15 pagesMICROBIOLOGY OLD EXAM QUESTIONS ON VIRUSES AND VIROLOGYTijanaNo ratings yet
- Varicella Zoster InfectionDocument68 pagesVaricella Zoster InfectionChristelle Brookshiel Demayo Marba100% (1)
- Spelling Bee WordsDocument3 pagesSpelling Bee Wordskenpokarate0101No ratings yet
- Prevention and Control of InfectionsDocument21 pagesPrevention and Control of InfectionsSunil ThomasNo ratings yet
- Philippine Handbook On Adult Immunization 2012 PDFDocument140 pagesPhilippine Handbook On Adult Immunization 2012 PDFLinius CruzNo ratings yet
- Viral Exanthem (Main)Document94 pagesViral Exanthem (Main)Starlet Rhonadez Bito-onon OrielNo ratings yet