Professional Documents
Culture Documents
Hematology 2006 Sallan 128 32 PDF
Uploaded by
Mail27Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hematology 2006 Sallan 128 32 PDF
Uploaded by
Mail27Copyright:
Available Formats
Acute Lymphoblastic Leukemia
in Adults and Children
Session Chair: Charles Linker, MD
Speakers: Stephen E. Sallan, MD; Nicola Gökbuget, MD; and Ching-Hon Pui, MD
Myths and Lessons from the Adult/Pediatric
Interface in Acute Lymphoblastic Leukemia
Stephen E. Sallan
The development of effective therapy for children with understanding about why these outcome differences
acute lymphoblastic leukemia (ALL) is one of the great exist, and think that by extending successful pediatric
successes of clinical oncology, with long-term survival clinical programs to include adult patients with ALL, we
achieved in over 80% of patients. However, cure rates can directly compare uniformly treated adults and
for adults with ALL remain relatively low, with only children in terms of response to therapy, toxicity and
40% of patients cured. With an age-unrestricted, underlying biology.
biology-based approach, we anticipate a better
“The child is the father of the man”… tive. Although well-recognized age-related dissimilarities
William Wordsworth in the biology of ALL and event-free survival exist (Tables
2 and 3), the more favorable outcomes for older adoles-
Background cents treated on pediatric regimens in Table 1 cannot be
Within childhood acute lymphoblastic leukemia (ALL) explained by differences in patient characteristics. Nor
populations, older children have had inferior outcomes1 would one expect other potential “adult vs. pediatric”
and within adult ALL populations, younger adults have
had superior outcomes.2,3 In recent reports, “overlapping”
Table 1. Older child/young adult acute lymphoblastic
populations of older children and young adults have been
leukemia (ALL) outcomes.
compared for the likelihood of inducing a complete remis-
sion and long-term event-free survival (Table 1).4-8 Age in # CR 5-Yr EFS
None of the clinical trials listed in Table 1 was de- Country Nat’l Trial Years Pts (%) (%) Ref.
signed to be compared to its age-overlapping pediatric or US: CCG (P) 16-21 196 96 64* 4
adult counterpart; thus, the comparisons were all retrospec- CALGB (A) 103 93 38*
France: FRALLE 93 (P) 15-20 77 94 67 5
LALA94 (A) 100 83 41
Division of Hematology/Oncology, Children’s Hospital and Holland: DCOG (P) 15-18 47 98 69 6
HVON (A) 44 91 34
Department of Pediatrics, Harvard Medical School, Boston,
Massachusetts UK: ALL97 (P) 15-17 61 98 65 7
UKALLXII (A) 67 94 49
Supported in part by grant CA 68484 from the National Cancer Italy: AIEOP (P) 14-18 150 94 80** 8
Institute, National Institutes of Health, Bethesda, Maryland Gimema (A) 95 89 71**
Correspondence: Stephen Sallan, MD, Dana Farber Cancer Abbreviations: CR, complete remission; EFS, event-free
Institute, 44 Binney St, Rm 1642, Boston MA 02115-6084; survival; P, pediatric protocol; A, adult protocol
Phone 617-632-3316; Fax 617-632-5511; Email * 6-yr EFS
stephen_sallan@dfci.harvard.edu ** 2-year overall survival
128 American Society of Hematology
differences (for example, co-morbidities associated with smok- Table 2. Acute lymphoblastic leukemia (ALL): incidence &
ing, or host pharmacokinetic differences based on age) to biological differences.
play a substantial role in the findings summarized in Table 1.
Children Adults
There are clear differences between current adult and
Peak incidence 5 years 50 years
pediatric therapeutic approaches. For example, bone mar-
row transplantation in first remission is more common for % of Leukemias 80-85% 15%
adults (in part, because of the higher incidence of Philadel- Chromosomes
Ph+ 3% 30%
phia chromosome–positive ALL), and pediatric regimens MLL 1-2% 7%
generally include greater dose density of many chemothera- TEL/AML1 20% 2%
peutic agents (such as asparaginase, vincristine, cortico- Hyperdiploid 25% 5%
steroids and methotrexate). T-cell 10-15% 20-25%
What are some plausible explanations for these differ- Mature B 1-2% 3-5%
ences between pediatric and adult outcomes? In a thought-
ful, provocative and prescient editorial, Dr. Charles Schiffer
reflected on biological differences among the hosts and Table 3. Five-year event-free survival.
diseases, and also raised issues pertaining to clinical prac-
tice, such as the frequency of and familiarity with ALL Children Adults
protocols and care of such patients.9 In addition to recog- Pre-B > 80% 30-40%
nizing that ALL is the most common malignancy in chil- T-cell 75-80% 45-55%
dren and relatively rare in adult oncology populations, he Ph+ 20-25% < 10%
also noted that most children, but not most adults, with MLL 40-50% 20%
ALL were treated in the context of clinical trials, by expe- TEL/AML1 90% N/A
rienced support teams, and that many adults were not treated
at academic medical centers. The cultural differences be-
tween care of pediatric and adult ALL patients, described Frequency of and familiarity with ALL
as “disparities in treating attitudes” by Boissel and co-work- Although there might be as many adults with ALL as there
ers,5 was highlighted by Schiffer’s colorful and accurate are children with the disease11 (Figure 1), the relative fre-
description of pediatricians’ tight adherence to complex quency of the disease is markedly higher in young chil-
treatment protocols “…with a military precision on the basis dren. ALL represents about 15% of all malignancies in 1-
of near-religious conviction about the necessity of main- 15 year olds, 5% in 15-19 year olds, and < 10% of malig-
taining prescribed dose and schedule come hell, high wa- nancy in > 20 year olds.
ter, birthdays, Bastille Day, or Christmas.” Although the
necessity of such vigor has not been formally tested, the Adherence to protocol and
proof of the pudding is in the tasting. mitigating psychosocial factors
Although most of the drugs used for ALL today have ex-
Obstacles to Age-Unrestricted, isted for over four decades, little is known about their ideal
Biology-based Treatment antileukemia dose or the role of individual patient differ-
Why have adults with ALL not received the same chemo-
therapeutic regimens as children?
There are two principal hurdles: 1) systems of care,
and 2) regulatory impediments.
“Systems of care” and related differences
Referral patterns
Commonly held views suggest that pediatricians refer 15-
to 20-year-old patients to pediatric academic medical cen-
ters where (a) > 90% of patients are < 15 years old, and b) >
90% of patients with ALL are enrolled on clinical trials.
Similarly, internists frequently refer 15- to 20-year-old
patients to adult hospitals, mostly not academic medical cen-
ters, where a) > 90% of the patients are > 40 years old and b)
most patients with ALL are not entered on clinical trials.10
Figure 1. Incidence of acute lymphoblastic leukemia (ALL)
by age, SEER 1992-1999.
Hematology 2006 129
ences in drug metabolism. In pediatric practice, “pushing pharmaceutical company-sponsored trials) frequently es-
the dose” by using myelosuppression as the endpoint, as- tablish “biologically arbitrary” age limits for protocol eli-
sures delivery of the maximum dose for each child with gibility and evaluation. Thus, diseases such as ALL, whose
each course of chemotherapy. Although it is difficult to biology extends across a broad age spectrum, are usually
assess whether such rigid adherence to protocols is neces- approached as two diseases: childhood ALL (patients < 18
sary, Boissel and co-workers reported on one “therapeutic years old), and adult ALL (patients ≥ 18 years old). Such
practice” measure. They determined the median number of “age-restricted” criteria have played an integral role in our
days from the time of initial complete remission until the current understanding of the disease and its treatment. How-
time of the first postremission chemotherapy: 2 days in the ever, this approach, based on the single differentiating mea-
pediatric study and 7 days in the adult study; P = 0.002.5 sure—patient age—has until recently hampered clinical re-
Is this time-to-next-treatment measure a medical or psy- search across a broader spectrum of the disease. Although
chological problem? Have the older patients fully recov- likely a meaningful host variable, age, per se, is highly un-
ered physiologically, or are there other mitigating features likely to trump leukemia biology or the impact of an indi-
(e.g., “I need some time with my family”) resulting in de- vidual treatment regimen. Overcoming such well-institution-
lays in therapy? alized barriers to research remains a formidable challenge.
In the pediatric setting, in addition to the meticulous Recently, the Dana-Farber Pediatric ALL Consortium,
attention to detail by the pediatricians, a primary driver of a group of nine collaborating pediatric centers with a suc-
subsequent therapy is the caretaker, usually the mother. cessful record of ALL research and treatment,16 joined to-
(“What are we waiting for? The leukemia is growing back. gether with nine adult institutions to form a Dana-Farber
Let’s get going!”) Combined Adult/Pediatric ALL Consortium.
In anticipation of a common approach to the over 18-
Difficulties in comparisons year-old patients, we evaluated our oldest pediatric ALL
“Simple” apples-to-apples comparisons in a heterogenous population—those aged 15-18 years old.17 Among 844 pa-
disease such as ALL can be difficult, and occult differences tients treated on two consecutive protocols (Dana-Farber
in practices among internists and pediatricians might not 91-01 and 95-01) between 1991-2000, we found 51 (6%)
be appreciated. were in the 15- to 18-year-old population. Statistically sig-
For example, Table 1 demonstrates comparisons in the nificant biological characteristics at the time of diagnosis
percentage of complete remissions between older children included a higher proportion with T-cell ALL and a lower
and adults. Not shown is the time to enter complete remis- proportion with hyperdiploidy or the TEL/AML1 translo-
sion. All pediatric trials report complete remission at the cation compared to younger patients. Except for a lower
end of approximately 1 month of multiagent chemotherapy. incidence of complete remissions (1-14 year olds, 98% vs.
However, many adult trials report on the complete remis- 15-18 year olds, 94%; P = 0.01), there were no other statis-
sion rates after 2 months of treatment (Table 4). Although tically significant differences with regard to 5-year event-
the time to attain a complete remission was not of prognos- free survival (> 1-10 years old, 85%; > 10-15 years old,
tic importance in at least one adult trial,12 we found that in 77%; and >15-18 years old, 78%; P = 0.10). Patients 10
childhood ALL, the time to enter a complete remission had years old and older had more asparaginase-related pancre-
significant implications, and the difference between a com- atitis and thrombosis, but there were no differences between
plete remission in 1 month or 2 months was a matter of life the 10- to 14-year-old and 15- to 18-year-old populations.
or death for the majority of slow responders.15 An updated analysis of the efficacy of our pediatric regimen
for adult patients, 18-50 years old, appears as a 2006 Ameri-
Regulatory obstacles can Society of Hematology abstract (DeAngelo et al).
No diseases begin or end at age 18 years. But current re- We are now poised to investigate the biology of ALL
view systems of clinical trials (e.g., Institutional Review and its treatment across a broad age spectrum, and to have
Boards) and funding sources (e.g., cooperative groups and common treatment regimens for common disease among
patients ages 1-50 years old.
From our DFCI Combined Adult/Pediatric ALL Con-
Table 4. Time to complete remission in adult acute sortium, many myths have surfaced, and many lessons have
lymphoblastic leukemia (ALL) trials. been (and are being) learned.
% CR after One % CR after Two Myths and Lessons
Study Cycle of Chemo Cycles of Chemo
UKALLXII/ECOG12 51% 91%
Myth #1. It cannot be done!
CALGB 88113 62% 86% You cannot have a common approach to therapy for chil-
LALA-9413 72% 84% dren and adults. The disease biology, medical practices,
Hyper-CVAD 2 81% 92% regulations and cultures are incompatible with a uniform
DFCI pilot14 82% N/A approach to clinical research.
130 American Society of Hematology
Lesson #1. It can be done! the CSF, can be readily mitigated by the routine use of
(But it isn’t easy.) Finding common ground requires time, intrathecal chemotherapy at the time of the initial diagnos-
communication and compromise. We are confident that our tic lumbar puncture.
work within the DFCI Combined Adult/Pediatric ALL Con-
sortium, as well as similar efforts by others who are striving Myth #5. Who needs a parent or caregiver?
toward the same goals—improved outcome for all, dimin- The patient and his or her physician are sufficient for opti-
ished toxicity and a better understanding of leukemia biol- mal care and outcomes.
ogy—will be rewarding and result in lives saved and qual-
ity years of life added. Lesson #5. Never underestimate the value of a caregiver! The
best motivated patient and physician can have their well-
Myth #2. Adults do not tolerate asparaginase. intended treatments and outcomes enhanced by surrounding
It is generally assumed that adults are less tolerant to the themselves with “a mother figure”; in fact, parental surro-
acute and cumulative side effects of antileukemia drugs, gates, committed family members and loved ones, as well as
and asparaginase, a drug used in all pediatric ALL regi- an extended supportive team of professionals (especially
mens, is often cited as a prime example. nurses), are likely to assure optimal adherence to protocol,
emotional support, and (hopefully) better outcomes.
Lesson #2. Our initial adult protocol, a feasibility trial us-
ing one arm of our pediatric ALL regimen, includes 30 Conclusion
weeks of high-dose asparaginase therapy. Adults ages 18- Retrospective analyses clearly demonstrate that current
50 years old and children ages 10-18 years old tolerate pediatric therapeutic regimens are more effective than adult
multiple weekly asparaginase doses (≥ 12,500 IU/m2) with regimens for 16- to 21-year-old patients. Current and fu-
similar incidences of allergic reactions, pancreatitis and ture clinical trials will focus on “the ages of uncertainty”:
thrombosis. the 21- to 50-year-old population. Age-unrestricted, biol-
ogy-based therapy should be the standard of all patients
Myth #3. Adults have a high rate of therapy-related deaths. with ALL. Pediatricians and internists treating patients with
Some would argue against initiating combined adult/pedi- ALL have much to learn from one another. Such efforts are
atric clinical trials because the remission mortality in chil- likely to result in more cures and a higher quality of life
dren (now in the 1-2% range) is far less than in adults. among the survivors.
Lesson #3. In fact, the experience of Dutch6 and British7 References
investigators suggests that it is the practice of bone marrow 1. Irken G, Oren H, Gulen M, et al. Treatment outcome of
transplantation in first remission for non-Philadelphia chro- adolescents with acute lymphoblastic leukemia. Ann
Hematol. 2002;81:641-645.
mosome–positive ALL that accounts for the increased in- 2. Kantarjian H, Thomas D, O’Brien S, et al. Long-term follow-
cidence of therapy-related deaths. Given the paucity of data up results of hyperfractionated cyclophosphamide,
supporting the superiority of bone marrow transplantation vincristine, doxorubicin, and dexamethasone (Hyper-
in first remission, many now agree that use of chemotherapy CVAD), a dose-intensive regimen, in adult acute lymphocytic
leukemia. Cancer. 2004;101:2788-2801.
alone would result in both improved outcomes and in a 3. Larson RA, Dodge RK, Burns CP, et al. A five-drug remis-
lower incidence of therapy-related deaths. Our DFCI adult sion induction regimen with intensive consolidation for adults
pilot protocol and mature pediatric protocols have ~1% with acute lymphoblastic leukemia: Cancer and Leukemia
incidence of therapy-related deaths. Group B Study 8811. Blood. 1995;85:2025-2037.
4. Stock W, Sather H, Dodge RK, Bloomfield CD, Larson RA,
Nachman J. Outcome of adolescents and young adults with
Myth #4. Adults don’t have asymptomatic central nervous ALL: A comparison of Children’s Cancer Group (CCG) and
system (CNS) leukemia at diagnosis. Cancer and Leukemia Group B (CALGB) regimens. Blood.
And because they don’t, the practice of routine sampling 2000;96:467a.
5. Boissel N, Auclerc M-F, Lheritier V, et al. Should adolescents
of CSF at the time of diagnosis in asymptomatic patients is with acute lymphoblastic leukemia be treated as old children
variable among adult treatment regimens. or young adults? Comparison of the French FRALLE-93 and
LALA-94 trials. J Clin Oncol. 2003;21:774-780.
Lesson #4. ALL is always a systemic disease. About 2-3% 6. deBont JM, van der Holt B, Dekker AW, van der Does-van
den Berg A, Sonneveld P, Pieters R. Significant difference in
of children and adults have symptomatic CNS disease at outcome for adolescents with acute lymphoblastic leukemia
diagnosis and an additional 5-10% of asymptomatic chil- treated on pediatric vs adult protocols in the Netherlands.
dren and 5% of adults have lymphoblasts in their CSF dis- Leukemia. 2004;18:2032-2035.
ease at time of diagnosis. Routine lumbar puncture at the 7. Ramanujachar R, Richards S, Hann I, Webb D. Adolescents
with acute lymphoblastic leukaemia: Emerging from the
time of diagnosis and prior to initiating systemic chemo- shadow of paediatric and adult treatment protocols. Pediatr
therapy, as well as routine CNS treatment, should be part of Blood Cancer. 2006; [Epub ahead of print]
ALL management for all patients. An argument against this 8. Testi AM, Valsecchi MG, Conter V, et al. Difference in
practice, that one might inadvertently introduce blasts into outcome of adolescents with acute lymphoblastic leukemia
Hematology 2006 131
(ALL) enrolled in pediatric (AIEOP) and adult (GIMEMA) 13. Thomas X, Boiron J-M, Huguet F, et al. Outcome of
protocols. Blood. 2004;104:1954a. treatment in adults with acute lymphoblastic leukemia:
9. Schiffer CA. Differences in outcome in adolescents with acute analysis of the LALA-94 trial. J Clin Oncol. 2004;22:4075-
lymphoblastic leukemia: a consequence of better regimens? 4086.
Better doctors? Both? J Clin Oncol. 2003;21:760-7611. 14. Daniel D’Angelo, M.D. Personal Communication May 2006.
10. Bleyer A. The adolescent and young adult gap in cancer 15. Silverman LB, Gelber RD, Young ML, Dalton VK, Barr RD,
care and outcome. Curr Probl Pediatr Adolesc Health Care. Sallan SE. Induction failure in acute lymphoblastic leukemia
2005;35:182-217. of childhood. Cancer. 1999;85:1395-1404.
11. Bleyer A, O’Leary M, Barr R, Ries LAG (eds). Cancer 16. Silverman LB, Declerck L, Gelber RD, et al. Results of
Epidemiology in Older Adolescents and Young Adults 15 to Dana-Farber Cancer Institute Consortium protocols for
29 years of Age, including SEER Incidence and Survival: children with newly diagnosed acute lymphoblastic leukemia
1975-2000. National Cancer Institute, NIH Pub. No. 06-5767. (1981-1995). Leukemia. 2000;14:2247-2256.
Bethesda, MD 2006. 17. Barry E, DeAngelo DJ, Neuberg D, et al. Favorable outcome
12. Rowe JM, Buck G, Burnett AK, et al. Induction therapy for for adolescents with acute lymphoblastic leukemia treated
adults with acute lymphoblastic leukemia: Results of more on Dana Farber Cancer Institute ALL Consortium protocols.
than 1500 patients from the international ALL trial: MRC J Clin Oncol. In press.
UKALL XII/ECOG E 2993. Blood. 2005;106:3760-3767.
132 American Society of Hematology
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 35521Document12 pages35521Kyle MaogNo ratings yet
- The Amsterdam Preoperative Anxiety and Information.2Document7 pagesThe Amsterdam Preoperative Anxiety and Information.2Jose Rafael Villafan BernalNo ratings yet
- Annexure IDocument372 pagesAnnexure IsfarithaNo ratings yet
- PREP & COGENT - 13th and 14th December 2014Document6 pagesPREP & COGENT - 13th and 14th December 2014FdghNo ratings yet
- S11 XylitolDocument4 pagesS11 XylitolJholanda Ninggar BahtriaNo ratings yet
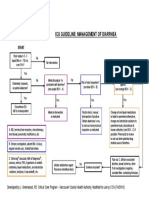
- Icu Guideline: Management of Diarrhea: StartDocument1 pageIcu Guideline: Management of Diarrhea: StartGracia VionaNo ratings yet
- Patient Profile-C in The WDocument17 pagesPatient Profile-C in The WPj TignimanNo ratings yet
- Handouts 1Document12 pagesHandouts 1banana_rockNo ratings yet
- Fey Lougawou (Wonder of The World Plant) PDFDocument7 pagesFey Lougawou (Wonder of The World Plant) PDFSalomon YvesNo ratings yet
- Changes in The Body: What Is Puberty?Document4 pagesChanges in The Body: What Is Puberty?Mitch MarananNo ratings yet
- SAOB AS OF December 31 2011Document5 pagesSAOB AS OF December 31 2011bacsecNo ratings yet
- Sterility Testing - Pics PDFDocument15 pagesSterility Testing - Pics PDFdepardieu1973100% (2)
- Essentials of Physical Medicine and Rehabilitation 2nd Ed. - W. Frontera, Et. Al., (Saunders, 2008) WW PDFDocument847 pagesEssentials of Physical Medicine and Rehabilitation 2nd Ed. - W. Frontera, Et. Al., (Saunders, 2008) WW PDFRecuperare100% (9)
- Suvarnprashan The Concept of Ayurveda Immunisation: Pharma Science Monitor 7 (4), Oct-Dec 2016Document5 pagesSuvarnprashan The Concept of Ayurveda Immunisation: Pharma Science Monitor 7 (4), Oct-Dec 2016AtulSanapNo ratings yet
- Psycho-Oncology - The 6 Phases of Cancer EbookDocument101 pagesPsycho-Oncology - The 6 Phases of Cancer EbookAndré Amorim100% (2)
- Medical Imaging and Pattern RecognitionDocument49 pagesMedical Imaging and Pattern RecognitionworkshoppeNo ratings yet
- Mwalya Wambua Final ProjectDocument49 pagesMwalya Wambua Final ProjectWILSON MACHARIANo ratings yet
- Application For Transfer in General ISMDocument2 pagesApplication For Transfer in General ISMThasreen sNo ratings yet
- Be Your Own Doctor With Acupressure - Dr. Dhiren GalaDocument69 pagesBe Your Own Doctor With Acupressure - Dr. Dhiren GalaParag Chhaper100% (2)
- Renal Nursing ReviewerDocument8 pagesRenal Nursing ReviewerGeraldine Waje100% (2)
- GoniometryDocument22 pagesGoniometryDuppala Sateesh KumarNo ratings yet
- Goris PDFDocument24 pagesGoris PDFAndrew WongNo ratings yet
- Immuno Cheat Sheet 1Document2 pagesImmuno Cheat Sheet 1yolo51No ratings yet
- V.Bontilao Sr. Integrated School Summative Test in English 7Document6 pagesV.Bontilao Sr. Integrated School Summative Test in English 7Nevaeh CarinaNo ratings yet
- Ophthalmology NotesDocument22 pagesOphthalmology NotesdrusmansaleemNo ratings yet
- Sadhana Intensive CourseDocument16 pagesSadhana Intensive Courseapi-241382210No ratings yet
- Chapter 7 - Adverse Drug Reaction and Medication ErrorsDocument6 pagesChapter 7 - Adverse Drug Reaction and Medication Errorsdlneisha61No ratings yet
- Gurkeerat Singh - Textbook of Orthodontics, 2nd EditionDocument5 pagesGurkeerat Singh - Textbook of Orthodontics, 2nd EditionndranNo ratings yet
- CVP Insertion Close Tube Thoracostomy RDocument6 pagesCVP Insertion Close Tube Thoracostomy RFaye Nadine T. CABURALNo ratings yet
- Anaesthetic Management of A Case With Severe Mitral Stenosis Posted For Emergency Caesarean SectionDocument2 pagesAnaesthetic Management of A Case With Severe Mitral Stenosis Posted For Emergency Caesarean SectionInternational Journal of Innovative Science and Research TechnologyNo ratings yet