Professional Documents
Culture Documents
Sanidad 112 PDF
Uploaded by
ElBuen John0 ratings0% found this document useful (0 votes)
7 views16 pageshi
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documenthi
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views16 pagesSanidad 112 PDF
Uploaded by
ElBuen Johnhi
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 16
2arriote Optician
€35930 Elements of refraction - part 3
Closing Date: 17/04/2014
i
Subjective refraction techniques, as the name suggests, rely on the patient’s response to obtain the refractive
correction that gives the best visual acuity. While itis prudent to say that this technique can only be performed on
patients who can communicate effectively, the development of computerised and projector test charts has
enabled the practitioner to adapt subjective techniques by using alternative targets to carry out a subjective
routine,
Before commencing your refraction, communication is of prime importance. Obtaining all the relevant
information necessary from the patient regarding their reason for visit, visual symptoms, previous ocular history
and so on is essential and allows you to adapt your examination to deal with the patient's concerns and help you
form your conclusions more easily.
(http:/assets.markallengroup.com/article-images/image-library/147/uploads/sites/9/2014/03/1a,jpg)
Figure 1: Measuring pupillary
Subjective refraction
Putting together a well thought out, structured routine to maximise pat
practitioner to work as quickly and as efficiently as possible. The subjective refraction should ideally be
performed in conditions that simulate the patient's normal viewing environment. For most, this will be in ambient
lighting and binocular viewing,
nt response and comfort will allow the
Performing the test in dim illumination will cause the pupils to dilate and increase spherical aberrations, which
could in turn have an impact on the refraction.
hitps:lwwnopticanontine.netvcstarchive!1 ans.
2am2018 Optician
Carrying out a binocular refraction (using a fogging lens rather than an occluder) can assist to control spherical
aberrations, help to relax accommodation and speed up the subjective routine as there is no need to carry out
binocular balancing. Binocular refraction can also be particularly useful when examining patients with refractive
conditions that can be further manifested by the use of an occluder, for example, hyperopia, pseudomyopia, latent
nystagmus and rotational phorias (cyclophorias).
Patients presenting with highly dominant eyes, unequal acuities and greatly fluctuating accommodation, will find
it difficult to perform a binocular refraction and they will report symptoms of diplopia.
It is not always apparent when a binocular or monocular refraction will be most appropriate for the patient. For
the purposes of these next two articles a monocular refraction will be described first and a brief explanation of
the binocular refraction technique will be illustrated later on.
Subjective routines can vary between practitioners and depend on the patient. Whatever order you choose to
carry out the subjective routine, it should flow effortlessly and have logical progression.
‘Always ensure you explain the test/procedure to the patient and what they may expect. Be clear and concise,
know how to explain the test you are conducting and keep it simple.
(http://assets.markallengroup.com/article-images/image-library/147/uploads/sites/9/2014/03/trial-frame-
billjpe)
Figure 2: Oculus trial frame
Overview of the subjective routine
? Measure the pupillary distance (PD)
2 it the trial frame
? Measure vision/visual acuity at distance and near
2 Determine and refine the best vision sphere (BVS)
Without retinoscopy
~ Fogging technique
hitps:lwwnopticanontine.netvcstarchive!1 26
2arriote Optician
Following retinoscopy
~ Fogging technique
~ Using +/-twirls
~ Duochrome
?.Check duochrome/circle of least confusion (where appropriate)
2Cross cylinder/fan and block
Jackson cross cyl
- Axis
-Power
Fan and block
2 Final sphere check
21.00 blur check
? Binocular balancing
? Binocular addition
? Binocular visual acuity
2 Recording the results.
‘The pupillary distance (PD)
Measuring the PD enables the practitioner to set up the trial frame correctly so that the optical centres are
correctly aligned for the patient to avoid induced prisms and aberrations.
Procedure for measuring the distance PD
2Sit directly in front of the patient and at the same eye level to avoid parallax
? Instruct the patient to look at your left eye, while you close your right eye. Rest the rule on the patient's
forehead and line up the outer edge of the PD ruler with the centre of the patient's right pupil (to avoid parallax)
? If your patient has dark brown eyes this may be difficult and therefore it may be easier to line the PD rule up
with the temporal limbus (the junction between the cornea and sclera)
? Keep the ruler in place, now direct the patient to look at your right eye while you close your left eye; look at the
scale of the ruler directly in line with the centre of the patient's left pupil (or nasal limbus) using your right eye
(this avoids parallax). The measurement between these two points is called the distance PD.
hitps:lwwnopticanontine.netvcstarchive!1 ai
You might also like
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Entendiendo FreeformDocument4 pagesEntendiendo FreeformElBuen JohnNo ratings yet
- Estructura Del Proyecto de InvestigaciónDocument2 pagesEstructura Del Proyecto de InvestigaciónElBuen JohnNo ratings yet
- Model Optometry Program CoursesDocument4 pagesModel Optometry Program CoursesElBuen JohnNo ratings yet
- Cvsejempdf PDFDocument1 pageCvsejempdf PDFdanielrhzNo ratings yet
- Estructura de TesisDocument2 pagesEstructura de TesisElBuen JohnNo ratings yet
- Reseña Docentes - AdministraciónDocument3 pagesReseña Docentes - AdministraciónElBuen JohnNo ratings yet
- Esquema Informe Final de Tesis 2017Document3 pagesEsquema Informe Final de Tesis 2017Ketty Laura VilcapomaNo ratings yet
- Calendario Internado Medicina 2017Document1 pageCalendario Internado Medicina 2017ElBuen JohnNo ratings yet
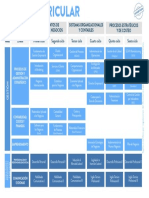
- Administracion de EmpresasDocument1 pageAdministracion de EmpresasElBuen JohnNo ratings yet
- Malla TraducciónDocument1 pageMalla TraducciónElBuen JohnNo ratings yet
- Have ... S - Cursos de Inglés y Repaso de Dudas PDFDocument4 pagesHave ... S - Cursos de Inglés y Repaso de Dudas PDFElBuen JohnNo ratings yet
- 308-Low Vision Case ReportDocument2 pages308-Low Vision Case ReportElBuen JohnNo ratings yet
- DebateDocument2 pagesDebateElBuen JohnNo ratings yet
- AMGridDocument1 pageAMGridElBuen JohnNo ratings yet
- Debate VocabularyDocument3 pagesDebate VocabularyElBuen JohnNo ratings yet
- 7 FourierDocument65 pages7 FourierElBuen JohnNo ratings yet
- DebateDocument2 pagesDebateElBuen JohnNo ratings yet
- AC1Document15 pagesAC1ElBuen JohnNo ratings yet
- Examen de Recuperación Óptica OftálmicaDocument1 pageExamen de Recuperación Óptica OftálmicaElBuen JohnNo ratings yet
- The Forgotten Man Who Transformed Journalism in AmericaDocument13 pagesThe Forgotten Man Who Transformed Journalism in AmericaElBuen JohnNo ratings yet
- 7 - 16 CLASS Final PDFDocument36 pages7 - 16 CLASS Final PDFElBuen JohnNo ratings yet
- MDDocument5 pagesMDElBuen JohnNo ratings yet
- Tras 2Document2 pagesTras 2ElBuen JohnNo ratings yet
- FourierDocument3 pagesFourierRedVisualPeruCompanyNo ratings yet
- Henry W Hofstetter, OD, PHD, FAAO 1914-2002 - Optometry and Vision ScienceDocument1 pageHenry W Hofstetter, OD, PHD, FAAO 1914-2002 - Optometry and Vision ScienceElBuen JohnNo ratings yet
- Cuales Son Las Consecuencias Que Esta ProvocaDocument3 pagesCuales Son Las Consecuencias Que Esta ProvocaElBuen JohnNo ratings yet
- Modern Pompeii: This Icelandic Town Buried in Ash and Brought Back to LifeDocument9 pagesModern Pompeii: This Icelandic Town Buried in Ash and Brought Back to LifeElBuen JohnNo ratings yet
- Tras 1Document2 pagesTras 1ElBuen JohnNo ratings yet
- Examen de Recuperación Óptica OftálmicaDocument1 pageExamen de Recuperación Óptica OftálmicaElBuen JohnNo ratings yet