Professional Documents
Culture Documents
Critical Care - Jean-Louis Vincent, Edward Abraham, Patrick Kochanek, Frederick A. Moore, Mitchell P. Fink - Textbook of Critical Care (2017, Elsevier) (Dragged)
Uploaded by
nh2411Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Critical Care - Jean-Louis Vincent, Edward Abraham, Patrick Kochanek, Frederick A. Moore, Mitchell P. Fink - Textbook of Critical Care (2017, Elsevier) (Dragged)
Uploaded by
nh2411Copyright:
Available Formats
CHAPTER 121 Septic Shock 843
121 Septic Shock
Jean-Louis Vincent
powerful vasodilator acting on vascular smooth muscle. Increased NO
INCIDENCE production is essentially due to the induction of inducible NO synthase
Septic shock is a form of acute circulatory shock that occurs secondary by proinflammatory cytokines. The formation of large quantities of NO
to severe infection. The incidence of septic shock may be rising, partly can also have secondary toxic effects on cells. NO can block mitochon-
related to medical progress that allows individuals to survive longer, drial respiration, directly by inhibiting cytochrome a,a3 and reacting
resulting in increased numbers of older, debilitated, or immunocom- with superoxide radicals, resulting in the production of peroxynitrite,
promised patients passing through the intensive care unit (ICU). Some which inhibits various phases of mitochondrial respiration.3 These
15% of ICU patients develop septic shock at one time or another, and effects result in depletion of cellular adenosine triphosphate and
the mortality rate is close to 50%.1,2 Somewhat lower mortality rates potentially have detrimental effects on cell function. It is important to
have been reported in some trials evaluating the effects of new thera- note that the inflammatory response also causes release of vasocon-
peutic interventions, but such studies include a number of exclusion strictor substances including thromboxane and endothelins.
criteria that are often associated with high mortality rates—cirrhosis, Other effects of the inflammatory reaction that accompanies septic
immunosuppression, and “do-not-resuscitate orders,” for example—so shock include expression of adhesion molecules on vascular endothe-
it is perhaps not surprising that mortality rates are lower in these lium and circulating cells (platelets, PMNs, and monocytes), allowing
therapeutic trials than in “real life.” adhesion of activated leukocytes and their migration to subendothelial
tissues. Alterations in intercellular endothelial junctions result in
increased capillary permeability and generalized edema. Alterations
ETIOLOGY OF SEPTIC SHOCK in coagulation and fibrinolysis complete the picture, with proinflam-
Septic shock is most often bacterial, but it can also be caused by a matory mediators creating a procoagulant state. Briefly, the activation
fungal or parasitic infection. In one-third of patients, no infectious of tissue factor on the surface of various cells, particularly monocytes
agent is identified.1,2 About half of the infections are nosocomial in and endothelial cells, initiates the coagulation system.4 In addition,
origin. Although an infection can arise anywhere, the lung is the most sepsis causes a significant reduction in plasma levels of natural
common source of infection (40%), followed by the abdomen (20%), anticoagulants such as protein C, protein S, and antithrombin by
indwelling venous and arterial catheters and primary bacteremias reducing their synthesis and increasing their consumption and clear-
(15%), and the urinary tract (10%).1,2 ance. Thrombolysis is also stimulated with an increase in the levels
of plasminogen activator inhibitor-1. The net result is a balance in
favor of procoagulant processes, often leading to disseminated intra-
PATHOPHYSIOLOGY OF SEPTIC SHOCK vascular coagulation and participating in the microcirculatory disor-
The pathophysiology of septic shock is complex. Essentially, the sys- der that leads to multiple organ failure and death in many patients
temic sepsis response starts with the recognition of an invading organ- with severe sepsis.
ism or its toxins. Among the bacterial factors, one of the best known During the sepsis response, antiinflammatory mediators including
toxins is lipopolysaccharide, which is part of the outer gram-negative IL-4 and IL-10 are also released, which limit the effects of proinflam-
bacterial membrane, but other bacterial-derived factors include lipo- matory mediators and can lead to a state of relative immunosuppres-
teichoic acid and peptidoglycan. In certain cases, essentially infections sion sometimes called immunoparalysis.5 Many patients are already
involving Staphylococcus aureus or β-hemolytic group A Streptococcus, immunosuppressed when sepsis is diagnosed.6
the formation of superantigens results in toxic shock syndrome.
The early humoral response involves the complement and contact
(kinin-kallikrein) systems. Immune cells, principally monocytes/
CLASSIFICATION
macrophages and polymorphonuclear neutrophils (PMNs), are not Patients with septic shock may be classified according to the letters
only able to recognize pathogenic agents and their products so they PIRO7 :
can phagocytose and destroy them but also release a series of mediators
that can activate other cells. Among cell membrane receptors impli-
cated in the recognition of pathogenic agents are the so-called Toll-like
P = Predisposing Factors
receptors. In response to cellular stimulation, intracellular signaling is Each patient has specific characteristics. For example, an individual
activated, resulting largely in the activation of transcriptional factors, receiving long-term immunosuppressant therapy requires a different
including nuclear factor kappa B, which in turn are responsible for the approach than someone who was previously healthy. Factors associated
initiation of proinflammatory reactions. A number of cytokines, two with lifestyle, such as alcoholism, may influence the course of septic
of the key players being tumor necrosis factor alpha (TNF-α) and shock.8 Patient age and sex may also be important. Increasingly, genet-
interleukin (IL)-1 that interact synergistically, are released by macro- ics is being considered, and studies are discovering the genetic factors
phages and other cells. TNF-α and IL-1 are particularly important that can influence the development of and survival from sepsis.9-11
proinflammatory cytokines whose administration in animals can Improved understanding of these aspects should help better direct
reproduce all features of septic shock including hypotension and therapeutic strategies.
development of multiple organ failure. A host of secondary mediators
including lipid mediators, oxygen free radicals, proteases, and arachi-
donic acid metabolites are also released by macrophages, PMNs, and
I = Infectious Insult
other cells. Vasodilator substances such as nitric oxide (NO) and This refers to the specific characteristics of the infection, that is, the
prostaglandins are released by endothelial cells and are responsible agent or pathogen involved (e.g., gram-positive vs. gram-negative,
for the early hemodynamic changes of sepsis. NO, in particular, is a bacteria vs. fungus), the source of sepsis (e.g., urinary tract vs.
Downloaded from ClinicalKey.com By Mahmoud El Morsy January 11, 2017. 843
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved
Downloaded from ClinicalKey.com at UCSI University January 11, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
844 PART 8 Infectious Diseases
respiratory tract), and the degree of extension of the infection (e.g., One may anticipate that patients with septic shock will have fever,
pneumonia confined to one lobe of one lung vs. generalized bilateral leukocytosis, and other typical features of sepsis, but this is not always
lung involvement, appendicitis vs. generalized peritonitis). All these true. Fever may be an important clue, but moderate fever can be
factors can influence the severity of sepsis response and the patient’s found in other types of shock. More important, fever is often absent
likely response to therapy. in patients with septic shock; in fact, hypothermia may be present
in 10% to 15% of cases, and this feature is associated with higher
mortality rates.14 Tachycardia can be the result of circulatory altera-
R = Host Response tions associated with any type of shock. Leukocytosis is also nonspe-
This refers to factors involved in the inflammatory response of the host cific and can be found in other types of circulatory failure; moreover,
to the infection and is assessed largely by the presence or absence of acute leukopenia may occur in sepsis due to peripheral trapping of
the signs and symptoms of sepsis (e.g., degree of elevation of white activated leukocytes and is also associated with a worse prognosis.
blood cell count, C-reactive protein [CRP], or procalcitonin). Each Lactic acidosis, a hallmark of all types of circulatory failure, is usually
patient mounts a different response dependent on various factors compensated by hyperventilation, so tachypnea is not specific for
including those previously discussed, and a patient’s response will vary septic shock.
with his or her clinical course and treatment. A more typical characteristic of septic shock is the hyperkinetic
pattern characterized by high cardiac output. Although such a hemo-
dynamic pattern is not entirely specific—it can be found in other
O = Organ Dysfunction inflammatory states such as polytrauma or pancreatitis or even ana-
This refers to the degree of organ dysfunction related to sepsis and can phylactic shock—it should alert the attending physician to a likely
be evaluated using various scoring systems, including the SOFA diagnosis of septic shock.
(sequential organ failure assessment) score,12 which uses objective,
readily available measures to quantify the dysfunction of six organ
systems (Table 121-1). Dysfunction of each organ is rated according to
HEMODYNAMIC CHANGES
a scale (0 [normal function] to 4 [organ failure]), and individual scores The inflammatory reaction causes intense vasodilation that increases
can then be summed to provide a total. Individual organ function as vascular capacity and results in a fall in arterial blood pressure. Hypo-
well as a composite score can thus be followed during the course of the volemia due to fluid loss (e.g., diarrhea, vomiting, or sweating) and
disease and treatment. alterations in capillary permeability contributes to hypotension, and
reduced myocardial contractility can further aggravate the hemody-
namic situation, although it is completely reversible when the septic
CLINICAL PRESENTATION shock resolves. The pathophysiology of reduced myocardial contrac-
It has been suggested that sepsis progresses in a continuum through to tility includes alterations in endothelial function, alterations in β-
septic shock, but in the clinical situation, such a progression is not adrenergic receptors, and alterations in myocardial calcium metabolism.
always so clear-cut or constant, and it is difficult to predict which These effects are caused largely by sepsis mediators such as TNF-α and
patients are going to develop septic shock and when. Septic shock can IL-1, oxygen free radicals, platelet activating factor, and NO, which all
develop very abruptly, without evidence of signs of sepsis in the pre- have negative inotropic effects.
ceding hours. After vascular filling as a result of volume resuscitation, the hemo-
Septic shock is characterized by the persistence of severe arterial dynamic status in septic shock is characterized by a fall in vascular tone
hypotension requiring vasopressor support, despite adequate fluid associated with reduced systemic vascular resistance and a raised
resuscitation, and the presence of perfusion abnormalities manifest by cardiac output. In addition, reduced myocardial contractility causes a
oliguria, reduced peripheral perfusion, and altered mental status. fall in the ventricular ejection fraction. Ejection volume and, particu-
Septic shock is typically associated with hyperlactatemia (blood lactate larly, cardiac output may be maintained by an increase in diastolic
concentrations above 2 mEq/L).13 volumes. Hence, there is myocardial depression or dysfunction without
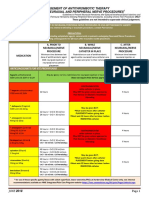
TABLE 121-1 The Sequential Organ Failure Assessment Score
SOFA SCORE 0 1 2 3 4
RESPIRATION
PaO2/FiO2, mm Hg >400 ≤400 ≤300 ≤200 with respiratory ≤100 with respiratory
support support
COAGULATION
Platelets × 103/mm3 >150 ≤150 ≤100 ≤50 ≤20
LIVER
Bilirubin, mg/dL (μmol/L) <1.2 (<20) 1.2-1.9 (20-32) 2.0-5.9 (33-101) 6.0-11.9 (102-204) >12.0 (>204)
CARDIOVASCULAR
Hypotension No hypotension MAP < 70 mm Hg Dopamine ≤5 or Dopamine >5 or Dopamine >15 or
dobutamine epinephrine ≤0.1 or epinephrine >0.1 or
(any dose)* norepinephrine ≤0.1* norepinephrine >0.1*
CENTRAL NERVOUS SYSTEM
Glasgow Coma Score 15 13-14 10-12 6-9 <6
RENAL
Creatinine, mg/dL (μmol/L) <1.2 (<110) 1.2-1.9 (110-170) 2.0-3.4 (171-299) 3.5-4.9 (300-440) or >5.0 (>440) or
or urine output <500 mL/d <200 mL/d
Data from Vincent JL, de Mendonca A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units. Results of a multicenter, prospective study.
Crit Care Med 1988;26:1793–800.
*Adrenergic agents administered for at least 1 hour (doses given are in μg/kg/min).
Downloaded from ClinicalKey.com at UCSI University January 11, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
CHAPTER 121 Septic Shock 845
any true cardiac failure (which would be associated with reduced
cardiac output).
MONITORING
Any patient with septic shock requires monitoring with an arterial
catheter to enable reliable and continuous assessment of arterial pres-
sure. Changes in systolic and pulse pressures in mechanically ventilated
patients during the respiratory cycle may also indicate a greater likeli-
hood of response to a fluid challenge; however, this sign is not reliable
when the patient triggers the ventilator.15 The arterial catheter also
facilitates blood sampling, notably for blood gas analysis.
Invasive Versus Less Invasive Monitoring
The role of the pulmonary artery catheter (PAC) in critically ill patients
has been questioned. However, although no study has conclusively
demonstrated positive effects of this type of monitoring on outcome,16
information obtained from the PAC may help in guiding patient
management in complex cases.17 The PAC is useful not only for moni-
toring pulmonary artery occlusion pressure (PAOP) and cardiac output
but also for assessment of mixed venous oxygen saturation (Svo2), a
highly useful parameter because a fall in Svo2 is generally indicative of
inadequate oxygen transport.
Less invasive monitoring techniques are increasingly being used.
Echocardiography can provide useful additional information, largely
to visualize the degree of ventricular filling and ejection volume.
However, echocardiography requires an experienced operator, gives no
information on the adequacy of cardiac output for the patient’s needs,
and is difficult to perform continuously, so information is usually
intermittent. Other less invasive methods of monitoring cardiac output FIGURE 121-1 ■ Representative examples of sublingual microvas-
include PiCCO, LidCO, transesophageal Doppler techniques, and even culature in a healthy volunteer (top panel) and in a patient with
bioimpedance or bioreactance techniques.18 However, measurement of septic shock (lower panel). Note decrease in density of small vessels
cardiac output in isolation is not very helpful in most critically ill in sepsis. (From De Backer D, Creteur J, Preiser JC, et al. Microvascular
patients. blood flow is altered in patients with sepsis. Am J Respir Crit Care Med
2002;166:98–104, with permission.)
Blood Lactate Levels
The blood lactate level is an important biological variable in determin-
ing the adequacy of perfusion and oxygenation. The normal blood observed (Fig. 121-1) and quantified in patients with sepsis.20 More-
lactate level is around 1 mEq/L, and hyperlactatemia becomes clearly over, the impact of therapeutic interventions on such changes can be
pathologic above a level of 2 mEq/L. Although hyperlactatemia is due monitored,21,22 opening the possibility that monitoring the microcircu-
to cellular hypoxia in other forms of circulatory shock, in septic shock, lation could be used to guide treatment.
additional mechanisms may play an important role in raising blood Near-infrared spectroscopy is a technique that uses the differential
lactate levels. In sepsis, blood lactate levels may be raised by an increase absorption properties of oxygenated and deoxygenated hemoglobin to
in cellular metabolism, by inhibition of pyruvate dehydrogenase, and evaluate tissue oxygenation (Sto2). Analysis of changes in Sto2 during
by reduced clearance. Repeated measurements enable one to assess the a circulatory stress test, such as a brief episode of forearm ischemia
efficacy of treatment19 and have a predictive value superior to derived (venous or arterial occlusion), may be more useful to quantify sepsis-
oxygenation parameters. The evolution of blood lactate levels enables induced microvascular dysfunction than an isolated Sto2 value.23
a global evaluation of the state of shock in response to treatment, Although these techniques have demonstrated clearly the presence
although in view of the relatively slow rate of change, blood lactate of alterations in the microcirculation in patients with sepsis, which are
levels cannot be used to guide resuscitation. associated with prognosis,24 further research is needed to fully evaluate
the relevance of these values to the early resuscitation and care of criti-
cally ill patients.
Peripheral Perfusion Parameters
Measurement of the gastric intramucosal pH or its derivatives (mucosal
Pco2 or the difference between the mucosal and arterial Pco2 [the Pco2
MANAGEMENT
gap]) is considered to reflect splanchnic perfusion and hence provide Septic shock, which systematically causes dysfunction of other organs,
an idea of the adequacy of regional oxygenation. However, these is a serious condition, and patients must be stabilized as a matter of
techniques may be influenced by technical considerations, including urgency. Management of the patient with septic shock involves three
the influence of gastric acid and enteral nutrition, and are not used inseparable components: treatment of the infection, cardiovascular
clinically. resuscitation, and modulation of the host response (Fig. 121-2).25
Other techniques for monitoring peripheral perfusion have been
developed. While the sublingual region is not a region that would
immediately seem to be of most interest, it is easily accessible, and
Treatment of Infection
using techniques of orthogonal polarization spectral or sidestream Infection must be treated effectively and rapidly. Antibiotics must be
darkfield imaging, heterogeneity of microcirculatory flow and reduced started quickly and must cover all likely organisms.26 The choice of
perfused vessel density and proportion of perfused vessels can be antibiotics may depend on local microbiological flora and resistance
Downloaded from ClinicalKey.com By Mahmoud El Morsy January 11, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved
Downloaded from ClinicalKey.com at UCSI University January 11, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
846 PART 8 Infectious Diseases
Treatment of Septic Shock
The Fluid Challenge Technique
TABLE 121-2
(with the TROL Mnemonic)
Hemodynamic Infection control
stabilization DEFINE EXAMPLE
Type of fluid Ringer’s lactate
Fluids Vasoactive Antibiotics Source Rate of infusion 200 mL in 10 min
agents control Objective Mean arterial pressure >75 mm Hg
Limits Central venous pressure 16 mm Hg
Modulation of the septic response
to fluid administration in order to minimize the risk of pulmonary
Corticosteroids Low-dose edema. In fluid replacement, it is preferable to use a fluid challenge
(in severe vasopressin? technique, in which filling pressures are measured at regular intervals
septic shock)? during fluid administration (Table 121-2).28 If cardiac output is moni-
FIGURE 121-2 ■ The three aspects of the treatment of septic
tored, one should ensure that it increases with fluid boluses, and
shock.
such fluid administration should be stopped when cardiac output
reaches a plateau.
There has been considerable debate as to which fluid should be used
in sepsis, but it is the quantity of fluid rather than the type of fluid per
patterns. Often, the microorganism(s) responsible for sepsis in an se that is of greatest importance. Because of their propensity for leakage
individual patient is not known for sure, and empiric broad-spectrum into the extravascular space, greater volumes of crystalloids are needed
antibiotics must be given to ensure adequate coverage. Such empiric to achieve the same effect as colloids,29 thus potentially increasing the
therapy must then be modified as soon as microbiology culture results risk of edema, but colloids are more expensive and carry their own
become available. risks. In particular, there has been considerable controversy about the
In addition to antibiotic treatment, any focus of infection must be use of albumin in critically ill patients, but the SAFE study suggested
removed or drained by emergency surgery if necessary. If no source is a decrease in mortality associated with albumin administration in
identified, a systematic search should be made based on the “big five”: patients with sepsis.30 Most clinicians would use some albumin in
lungs, abdomen, urine, wounds, and catheters. septic patients with significant hypoalbuminemia.
P = Pump (Vasoactive Agents)
Cardiovascular Resuscitation If fluid administration alone is unable to restore an adequate perfusion
The VIP rule proposed by Weil and Shubin27 should be followed. Each pressure, vasoactive agents are required. Catecholamines are preferred
patient is in fact a VIP, but the letters refer here to Ventilation, Infusion, for their rapid action and efficacy and their short half-lives. Adrenergic
and Pump. agents stimulate β1- (positive inotropes), β2- (essentially vasodilators
and bronchodilators), and α- (essentially vasoconstrictors) receptors
V = Ventilation to varying degrees. Dopamine also stimulates dopaminergic receptors,
All patients with septic shock must be generously oxygenated with the causing vasodilation primarily in the splanchnic and renal regions, but
aim of correcting any hypoxemia, regardless of whether it is due to the clinical relevance of this effect is doubtful.
inadequate cardiac output, pulmonary edema, or pulmonary disease. A randomized controlled study showed that dopamine use is
Severe cases need endotracheal intubation and mechanical ventilation. associated with increased adverse effects, notably arrhythmias, in
Noninvasive ventilation is not recommended in such hemodynami- patients with shock,31 and a meta-analysis indicated that dopamine
cally unstable patients. Even though it may represent a temporary administration is associated with higher mortality rates than norepi-
support rather than a treatment per se, mechanical ventilation allows nephrine in septic shock.32 Norepinephrine is, therefore, the preferred
not only an improvement in gaseous exchange but also has beneficial first-line vasopressor in patients with septic shock. Epinephrine should
hemodynamic effects, notably by reducing the oxygen requirement of not be used as a first-line vasopressor in patients with septic shock; it
the respiratory muscles. can have deleterious effects on splanchnic circulation and increase
cellular metabolism. Dobutamine is often added to vasopressor therapy,
I = Infusion particularly when using norepinephrine, to increase cardiac output by
Septic shock is accompanied by absolute and relative hypovolemia, the its positive inotropic effects.
result of various mechanisms: The place of vasopressin derivatives is not well defined. Patients
• External losses, which may be obvious, such as vomiting and with septic shock usually have a degree of relative vasopressin defi-
diarrhea, or less apparent, such as sweating ciency so that vasopressin supplementation may be warranted. Recent
• Internal losses via an increase in capillary permeability with studies have suggested that vasopressin is involved in endothelial
development of edema and sometimes liquid effusions (perito- protection so that early administration of vasopressin derivatives may
neal, pleural effusion) limit edema formation.33 This hypothesis is presently being tested in
• Increase in plasma volume associated with arterial and venous clinical trials.
dilatation
Hypovolemia needs to be corrected rapidly as it causes hemodynamic
instability both at the level of cardiac output and in terms of peripheral
Immunomodulation
perfusion. Clinical trials assessing drugs that limit the effects of proinflammatory
Assessment of an adequate volume state is essentially clinical: cytokines such as TNF-α (anti-TNF antibodies, TNF receptors) and
restoration of arterial pressure, improvement of cutaneous perfu- IL-1 (IL-1 receptor antagonist inhibitors) have not given convincing
sion, improved urine output, and improved mental state. The central results on beneficial effects of these agents on outcome, probably
venous pressure (CVP) can be a useful guide, but it is not possible to largely because such cytokines have multiple effects, beneficial as well
define in advance the CVP that should be reached in any individual as harmful. Administration of activated protein C (drotrecogin alfa
patient. Measurements of CVP or PAOP are primarily used as a limit [activated]) early in septic shock reduced mortality and morbidity in
Downloaded from ClinicalKey.com at UCSI University January 11, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
CHAPTER 121 Septic Shock 847
initial studies,34 but the drug was withdrawn from the market after a • Tidal volume should be limited, not only for hemodynamic
later negative placebo-controlled study.35 reasons but also to avoid a major inflammatory reaction.
The administration of large doses of corticosteroids for patients • Sedation must be avoided whenever possible. Administration of
with septic shock was proposed many years ago. More recently, the sedative drugs and analgesics should be titrated with respect to
concept of relative adrenal insufficiency has emerged, and administra- the needs of the individual patient. Reduced administration of
tion of moderate doses of corticosteroids (200 mg hydrocortisone in sedative agents can shorten the duration of mechanical ventila-
24 hours) in patients with septic shock has been proposed, but this is tion and ICU stay.47 ,48
also debated.36 ,37
The treatment of fever is controversial. Increased body temperature Renal Alterations
increases oxygen requirements, but the increased cellular metabolism Sepsis is the leading cause of acute renal failure in the ICU.49 Renal
may form part of the body’s natural defense. Animal studies have function can worsen as a result of combined circulatory changes and
suggested that control of fever is detrimental38 and that the release of inflammation. In addition, management of septic patients often
heat shock proteins in fever may have important protective effects.39 A involves administration of nephrotoxic agents—for example, amino-
multicenter study of acetaminophen in febrile ICU patients with sus- glycosides or contrast material for radiologic examinations.
pected infection showed that the drug was well tolerated but did not Unfortunately, there is no prophylactic approach to renal failure
reduce mortality.40 other than to try to maintain adequate renal perfusion and overall
High-flow hemofiltration techniques can remove a range of bacte- volume state. Administration of low (renal)-dose dopamine is ineffec-
rial products and mediators but are not without risk, notably because tive at preventing renal failure,50 and diuretics may be harmful.51
this process can remove beneficial products such as hormones and Renal replacement therapy is frequently necessary in septic patients.
medications, including antibiotics, as well as potentially harmful sub- In septic shock, continuous venovenous techniques, with or without
stances.41 Clinical studies have provided conflicting data regarding the dialysis, are generally preferred over intermittent techniques to facili-
effects of these techniques on outcomes.42 tate control of fluid balance.
Coagulation Alterations
Nutritional Support Coagulopathy is common in septic shock. A low platelet count is
Malnutrition can prolong the course of sepsis and increase the risk of common and may be associated with a prolonged prothrombin time
complications. When considering nutritional support in patients with and an activated partial thromboplastin time. Treatment of these
septic shock, several factors should be remembered: alterations revolves primarily around the cause, and there is no indica-
• There is no urgency to start nutritional support, unless the patient tion for heparin therapy. In severe cases associated with significant
is malnourished. bleeding, administration of fresh frozen plasma or platelet infusions
• The enteral route is preferable to the parenteral route. may be indicated.
• Enteral nutrition should not be started during the initial phase of
resuscitation. Although studies are limited, increasing the oxygen Hepatic Alterations
requirements of the gut is probably unwise in circulatory shock. Circulatory shock of any cause frequently results in the elevation of
However, as soon as the patient has achieved a degree of hemody- liver-associated enzyme levels, but the contribution of various organs
namic stability (after a maximum of 24-48 hours), enteral nutrition (e.g., muscles) to increased enzyme levels is difficult to quantify. Often
should be started. there is a rise in bilirubin levels after several days, without evidence of
• There is no urgency to start parenteral nutrition. Waiting a few days hemolysis, major hematomas, or biliary pathology. Supplementary
is acceptable. examinations such as ultrasound may be indicated to exclude any
• Careful control of blood glucose levels is recommended. Control of associated biliary pathology.
blood glucose levels has been shown to be associated with improved
outcomes,43 but hypoglycemia can be a problem with very strict Cerebral Function Alterations
blood glucose protocols. A suggested target glucose concentration Circulatory shock is typically accompanied by an alteration in intel-
is, therefore, 110 to 150 mg/dL.25,44 Variability in glucose levels lectual function, initially manifested as confusion without real coma.
should also be avoided.45 Cerebral alterations can be prolonged, and the patient is then said to
have septic encephalopathy. The exact cause of the encephalopathy is
unclear, although various mediators of sepsis have been implicated.
Organ Support Investigations are of little use except to exclude other causes. The
Organ dysfunction can involve any organ and can be quantified using electroencephalogram generally shows a slow diffuse slowing,52
the SOFA score (see Table 121-1). Techniques for individual organ whereas cerebral computed tomography and cerebrospinal fluid
support are covered in separate chapters, but an overview is given here. examination are normal. These alterations are usually fully reversible
with the resolution of shock.
Respiratory Alterations
Respiratory failure is a common complication of sepsis and is usually
characterized by hypoxemia. The diagnosis of acute respiratory distress
CONCLUSION
syndrome is made when the Pao2/Fio2 ratio is less than 300 mm Hg in Optimal treatment of a patient with septic shock requires a rapid and
the presence of bilateral infiltrates on a chest radiograph, with no effective management plan with the assistance of the full ICU team.
evidence of left heart failure.46 Infection control and achieving hemodynamic stability must be tackled
When starting a patient on mechanical ventilation, several factors simultaneously. Other interventions are currently undergoing clinical
need particular attention: trials, with the hope that they will improve the microcirculatory
• Worsening of arterial hypotension when starting mechanical changes of sepsis or beneficially modulate the host response. A better
ventilation suggests the presence of hypovolemia due to a reduc- characterization of patients with septic shock—for example, by using
tion in venous return (and hence in cardiac output) when the PIRO system—is necessary to appropriately titrate therapeutic
intrathoracic pressures are increased. interventions to individual patients.
Downloaded from ClinicalKey.com By Mahmoud El Morsy January 11, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved
Downloaded from ClinicalKey.com at UCSI University January 11, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
848 PART 8 Infectious Diseases
KEY POINTS
1. Septic shock affects about 15% of ICU patients and has a mortal- 4. Septic shock is defined as sepsis with organ dysfunction with
ity rate of close to 50%. persistent arterial hypotension requiring vasopressor administra-
2. Septic shock is most commonly caused by a bacterial infection, tion despite adequate fluid resuscitation, in the presence of
although fungi, viruses, and parasites can all be implicated. The perfusion abnormalities manifested by oliguria, reduced periph-
most common source of infection is the lung, followed by the eral perfusion, and/or altered mental status.
abdomen. 5. Blood lactate levels are typically raised in septic shock, and
3. Patients with sepsis can be classified according to their predis- persistently raised levels are a poor prognostic sign.
posing factors, the nature of the infection, degree of immune 6. Management of septic shock includes infection control, hemody-
response, and associated organ dysfunction. namic stabilization, and modulation of the host response.
ANNOTATED REFERENCES
De Backer D, Aldecoa C, Njimi H, et al. Dopamine versus norepinephrine in the treatment of septic shock: Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis
a metaanalysis. Crit Care Med 2012;40:7 25–7 30. and Septic Shock (Sepsis-3). JAMA 2016 ;315:8 01–8 10.
Meta-analysis demonstrating greater mortality and a higher incidence of arrhythmic events with Updated definitions and clinical criteria for diagnosis of sepsis and septic shock.
dopamine compared to norepinephrine administration.
Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for manage-
ment of severe sepsis and septic shock: 2012. Crit Care Med 2013;41:58 0–6 37 .
Evidence-based guidelines on all aspects of the management of patients with sepsis and septic shock.
References for this chapter can be found at expertconsult.com.
Downloaded from ClinicalKey.com at UCSI University January 11, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
CHAPTER 121 Septic Shock 848.e1
REFERENCES
1. Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R. Surviv-
Payen D. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 2006 ; 34: ing Sepsis Campaign: international guidelines for management of severe sepsis and septic shock,
344-53. 2012. Intensive Care Med 2013; 39: 16 5-228 .
2. Vincent JL, Marshall JC, Namendys-Silva SA, Francois B, Martin-Loeches I, Lipman J, Reinhart K, 26 . Vincent JL, Bassetti M, François B, Karam G, Chastre J, Torres A, Roberts JA, Taccone FS, Rello J,
Antonelli M, Pickkers P, Njimi H, Jimenez E, Sakr Y. Assessment of the worldwide burden of critical Calandra T, De Backer D, Welte T, Antonelli M. Advances in antibiotic therapy in the critically ill.
illness: the Intensive Care Over Nations (ICON) audit. Lancet Respir Med 2014; 2: 38 0-6 . Crit Care 2016 ; 17 : 133.
3. Radi R. Peroxynitrite, a stealthy biological oxidant. J Biol Chem 2013; 28 8 : 26 46 4-7 2. 27 . Weil MH, Shubin H. The “VIP” approach to the bedside management of shock. JAMA 196 9; 207 :
4. Simmons J, Pittet JF. The coagulopathy of acute sepsis. Curr Opin Anaesthesiol 2015; 28 : 227 -36 . 337 -40.
5. Hamers L, Kox M, Pickkers P. Sepsis-induced immunoparalysis: mechanisms, markers, and treatment 28 . Vincent JL, Weil MH. Fluid challenge revisited. Crit Care Med 2006 ; 34: 1333-7 .
options. Minerva Anestesiol 2015; 8 1: 426 -39. 29. Orbegozo CD, Gamarano BT, Njimi H, Vincent JL. Crystalloids versus colloids: exploring differences
6 . Davenport EE, Burnham KL, Radhakrishnan J, Humburg P, Hutton P, Mills TC, Rautanen A, Gordon in fluid requirements by systematic review and meta-regression. Anesth Analg 2015; 120: 38 9-402.
AC, Garrard C, Hill AVS, Hinds CJ, Knight JC. Genomic landscape of the individual host response 30. Finfer S, McEvoy S, Bellomo R, McArthur C, Myburgh J, Norton R. Impact of albumin compared to
and outcomes in severe sepsis. Lancet Respir Med 2016 ; 4: 259-7 1. saline on organ function and mortality of patients with severe sepsis. Intensive Care Med 2011; 37 :
7 . Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, 8 6 -96 .
Ramsay G. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit 31. De Backer D, Biston P, Devriendt J, Madl C, Chochrad D, Aldecoa C, Brasseur A, Defrance P, Got-
Care Med 2003; 31: 1250-6 . tignies P, Vincent JL. Comparison of dopamine and norepinephrine in the treatment of shock. N
8 . O’Brien JM, Jr., Lu B, Ali NA, Martin GS, Aberegg SK, Marsh CB, Lemeshow S, Douglas IS. Alcohol Engl J Med 2010; 36 2: 7 7 9-8 9.
dependence is independently associated with sepsis, septic shock, and hospital mortality among adult 32. De Backer D, Aldecoa C, Njimi H, Vincent JL. Dopamine versus norepinephrine in the treatment of
intensive care unit patients. Crit Care Med 2007 ; 35: 345-50. septic shock: a metaanalysis. Crit Care Med 2012; 40: 7 25-30.
9. Meyer NJ, Ferguson JF, Feng R, Wang F, Patel PN, Li M, Xue C, Qu L, Liu Y, Boyd JH, Russell JA, 33. He X, Su F, Taccone FS, Laporte R, Kjolbye AL, Zhang J, Xie K, Moussa MD, Reinheimer T, Vincent
Christie JD, Walley KR, Reilly MP. A functional synonymous coding variant in the IL1RN gene is JL. A selective V1A receptor agonist, selepressin, is superior to arginine vasopressin and to norepi-
associated with survival in septic shock. Am J Respir Crit Care Med 2014; 190: 6 56 -6 4. nephrine in ovine septic shock. Crit Care Med 2016 ; 44: 23-31.
10. Thair SA, Topchiy E, Boyd JH, Cirstea M, Wang C, Nakada TA, Fjell CD, Wurfel M, Russell JA, Walley 34. Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS,
KR. TNFAIP2 inhibits early TNFalpha-induced NF-x03BA;B signaling and decreases survival in Garber GE, Helterbrand JD, Ely EW, Fisher CJ, Jr. Efficacy and safety of recombinant human activated
septic shock patients. J Innate Immun 2016 ; 8 : 57 -6 6 . protein C for severe sepsis. N Engl J Med 2001; 344: 6 99-7 09.
11. Kompoti M, Michopoulos A, Michalia M, Clouva-Molyvdas PM, Germenis AE, Speletas M. Genetic 35. Ranieri VM, Thompson BT, Barie PS, Dhainaut JF, Douglas IS, Finfer S, Gardlund B, Marshall JC,
polymorphisms of innate and adaptive immunity as predictors of outcome in critically ill patients. Rhodes A, Artigas A, Payen D, Tenhunen J, Al-Khalidi HR, Thompson V, Janes J, Macias WL,
Immunobiology 2015; 220: 414-21. Vangerow B, Williams MD. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med
12. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, 2012; 36 6 : 2055-6 4.
Thijs LG. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/ 36 . Sprung CL, Annane D, Keh D, Moreno R, Singer M, Freivogel K, Weiss YG, Benbenishty J, Kalenka
failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of A, Forst H, Laterre PF, Reinhart K, Cuthbertson BH, Payen D, Briegel J. Hydrocortisone therapy for
Intensive Care Medicine. Intensive Care Med 1996 ; 22: 7 07 -10. patients with septic shock. N Engl J Med 2008 ; 358 : 111-24.
13. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard 37 . Volbeda M, Wetterslev J, Gluud C, Zijlstra JG, van der Horst IC, Keus F. Glucocorticosteroids for
GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, sepsis: systematic review with meta-analysis and trial sequential analysis. Intensive Care Med 2015;
Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions 41: 1220-34.
for Sepsis and Septic Shock (Sepsis-3). JAMA 2016 ; 315: 8 01-10. 38 . Su F, Nguyen ND, Wang Z, Cai Y, Rogiers P, Vincent JL. Fever control in septic shock: beneficial or
14. Kushimoto S, Gando S, Saitoh D, Mayumi T, Ogura H, Fujishima S, Araki T, Ikeda H, Kotani J, Miki harmful? Shock 2005; 23: 516 -20.
Y, Shiraishi S, Suzuki K, Suzuki Y, Takeyama N, Takuma K, Tsuruta R, Yamaguchi Y, Yamashita N, 39. Launey Y, Nesseler N, Malledant Y, Seguin P. Clinical review: fever in septic ICU patients–friend or
Aikawa N. The impact of body temperature abnormalities on the disease severity and outcome in foe? Crit Care 2011; 15: 222.
patients with severe sepsis: an analysis from a multicenter, prospective survey of severe sepsis. Crit 40. Young P, Saxena M, Bellomo R, Freebairn R, Hammond N, van Haren F, Holliday M, Henderson S,
Care 2013; 17 : R27 1. Mackle D, McArthur C, McGuinness S, Myburgh J, Weatherall M, Webb S, Beasley R. Acetamino-
15. Yang X, Du B. Does pulse pressure variation predict fluid responsiveness in critically ill patients? A phen for fever in critically Ill patients with suspected infection. N Engl J Med 2015; 37 3: 2215-24.
systematic review and meta-analysis. Crit Care 2014; 18 : 6 50. 41. Vincent JL. Sepsis: clearing the blood in sepsis. Nat Rev Nephrol 2009; 5: 559-6 0.
16 . Rajaram SS, Desai NK, Kalra A, Gajera M, Cavanaugh SK, Brampton W, Young D, Harvey S, Rowan 42. Zhou F, Peng Z, Murugan R, Kellum JA. Blood purification and mortality in sepsis: a meta-analysis
K. Pulmonary artery catheters for adult patients in intensive care. Cochrane Database Syst Rev 2013; of randomized trials. Crit Care Med 2013; 41: 2209-20.
2: CD003408 . 43. Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D,
17 . Vincent JL. The pulmonary artery catheter. J Clin Monit Comput 2012; 26 : 341-5. Ferdinande P, Lauwers P, Bouillon R. Intensive insulin therapy in critically ill patients. N Engl J Med
18 . Vincent JL, Rhodes A, Perel A, Martin GS, Della RG, Vallet B, Pinsky MR, Hofer CK, Teboul JL, de 2001; 345: 1359-6 7 .
Boode WP, Scolletta S, Vieillard-Baron A, De Backer D, Walley KR, Maggiorini M, Singer M. Clinical 44. Vincent JL. Blood glucose control in 2010: 110 to 150 mg/dL and minimal variability. Crit Care Med
review: update on hemodynamic monitoring–a consensus of 16 . Crit Care 2011; 15: 229. 2010; 38 : 993-5.
19. Dettmer M, Holthaus CV, Fuller BM. The impact of serial lactate monitoring on emergency depart- 45. Hermanides J, Vriesendorp TM, Bosman RJ, Zandstra DF, Hoekstra JB, Devries JH. Glucose vari-
ment resuscitation interventions and clinical outcomes in severe sepsis and septic shock: an obser- ability is associated with intensive care unit mortality. Crit Care Med 2010; 38 : 8 38 -42.
vational cohort study. Shock 2015; 43: 55-6 1. 46 . Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky
20. De Backer D, Hollenberg S, Boerma C, Goedhart P, Buchele G, Ospina-Tascon G, Dobbe I, Ince C. AS. Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012; 307 : 2526 -33.
How to evaluate the microcirculation: report of a round table conference. Crit Care 2007 ; 11: R101. 47 . Balzer F, Weiss B, Kumpf O, Treskatsch S, Spies C, Wernecke KD, Krannich A, Kastrup M. Early deep
21. Ospina-Tascon G, Neves AP, Occhipinti G, Donadello K, Buchele G, Simion D, Chierego ML, Silva sedation is associated with decreased in-hospital and two-year follow-up survival. Crit Care 2015;
TO, Fonseca A, Vincent JL, De Backer D. Effects of fluids on microvascular perfusion in patients 19: 197 .
with severe sepsis. Intensive Care Med 2010; 36 : 949-55. 48 . Strom T, Martinussen T, Toft P. A protocol of no sedation for critically ill patients receiving mechani-
22. Donati A, Damiani E, Luchetti M, Domizi R, Scorcella C, Carsetti A, Gabbanelli V, Carletti P, cal ventilation: a randomised trial. Lancet 2010; 37 5: 47 5-8 0.
Bencivenga R, Vink H, Adrario E, Piagnerelli M, Gabrielli A, Pelaia P, Ince C. Microcirculatory effects 49. Andrikos E, Tseke P, Balafa O, Cruz DN, Tsinta A, Androulaki M, Pappas M, Ronco C. Epidemiology
of the transfusion of leukodepleted or non-leukodepleted red blood cells in patients with sepsis: a of acute renal failure in ICUs: a multi-center prospective study. Blood Purif 2009; 28 : 239-44.
pilot study. Crit Care 2014; 18 : R33. 50. Bellomo R, Chapman M, Finfer S, Hickling K, Myburgh J. Low-dose dopamine in patients with early
23. Shapiro NI, Arnold R, Sherwin R, O’Connor J, Najarro G, Singh S, Lundy D, Nelson T, Trzeciak SW, renal dysfunction: a placebo-controlled randomised trial. Australian and New Zealand Intensive Care
Jones AE. The association of near-infrared spectroscopy-derived tissue oxygenation measurements Society (ANZICS) Clinical Trials Group. Lancet 2000; 356 : 2139-43.
with sepsis syndromes, organ dysfunction and mortality in emergency department patients with 51. Mehta RL, Pascual MT, Soroko S, Chertow GM. Diuretics, mortality, and nonrecovery of renal
sepsis. Crit Care 2011; 15: R223. function in acute renal failure. JAMA 2002; 28 8 : 2547 -53.
24. Ait-Oufella H, Bourcier S, Lehoux S, Guidet B. Microcirculatory disorders during septic shock. Curr 52. Hosokawa K, Gaspard N, Su F, Oddo M, Vincent JL, Taccone FS. Clinical neurophysiological assess-
Opin Crit Care 2015; 21: 27 1-5. ment of sepsis-associated brain dysfunction: a systematic review. Crit Care 2014; 18 : 6 7 4.
25. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL,
Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus
Downloaded from ClinicalKey.com By Mahmoud El Morsy January 11, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved
Downloaded from ClinicalKey.com at UCSI University January 11, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
You might also like
- Anesthesia ALL PDFDocument195 pagesAnesthesia ALL PDFYasir RasoolNo ratings yet
- American Heart Association Guidelines For CPR 2015: Christopher RyalinoDocument50 pagesAmerican Heart Association Guidelines For CPR 2015: Christopher RyalinoLightNo ratings yet
- ICU HandbookDocument146 pagesICU HandbookBulent InanNo ratings yet
- Fishman's Pulmonary Diseases and Disorders, 2008 (Dragged)Document11 pagesFishman's Pulmonary Diseases and Disorders, 2008 (Dragged)nh2411No ratings yet
- Critical Decisions in Emergency and Acute Care ElectrocardiographyFrom EverandCritical Decisions in Emergency and Acute Care ElectrocardiographyNo ratings yet
- Stop Anticoagulation Neuraxial AnesthesiaDocument3 pagesStop Anticoagulation Neuraxial AnesthesiaGihan NakhlehNo ratings yet
- Susan Mathews Case NotesDocument2 pagesSusan Mathews Case NotesHarshit Aggarwal80% (5)
- SRNA Orientation Checklist TitleDocument40 pagesSRNA Orientation Checklist Titleihtisham1No ratings yet
- Perioperative - Semester SummaryDocument67 pagesPerioperative - Semester SummaryPatricia Eleanor FranksNo ratings yet
- Ozone - A Wide Spectrum Healer by Gary Null PHDDocument20 pagesOzone - A Wide Spectrum Healer by Gary Null PHDangelakimba100% (4)
- Neuroanesthesia Crisis ManualDocument56 pagesNeuroanesthesia Crisis ManualChrismas BangunNo ratings yet
- Surgical InfectionsDocument310 pagesSurgical InfectionsOmar Ed ChavezNo ratings yet
- OB Rotation NotesDocument5 pagesOB Rotation NotesEricNo ratings yet
- Essential anesthesia room setup checklistDocument31 pagesEssential anesthesia room setup checklistnbrassarNo ratings yet
- AWARENESS UNDER ANESTHESIA: DEFINITION, TYPES, RISK FACTORS & PREVENTIONDocument27 pagesAWARENESS UNDER ANESTHESIA: DEFINITION, TYPES, RISK FACTORS & PREVENTIONagatakassaNo ratings yet
- Epidural AnesthesiaDocument5 pagesEpidural AnesthesiaImran MukhlessNo ratings yet
- Graphic Anaesthesia, second edition: Essential diagrams, equations and tables for anaesthesiaFrom EverandGraphic Anaesthesia, second edition: Essential diagrams, equations and tables for anaesthesiaNo ratings yet
- Advanced Cardiovascular Life Support (ACLS)Document2 pagesAdvanced Cardiovascular Life Support (ACLS)Vijay MgNo ratings yet
- Essentials of Anesthesia For Medical Students FinalDocument82 pagesEssentials of Anesthesia For Medical Students FinalEs LamNo ratings yet
- MN105613 PICU2022 Book ProofDocument60 pagesMN105613 PICU2022 Book ProofErwin Dela GanaNo ratings yet
- Upload 8Document2 pagesUpload 8cingyaNo ratings yet
- Antrim ED Handbook 2019Document238 pagesAntrim ED Handbook 2019Chris Jardine LiNo ratings yet
- Necrotizing Otitis 2022Document20 pagesNecrotizing Otitis 2022asmashNo ratings yet
- Telegram Cloud Document 4 5893461163299045618 PDFDocument232 pagesTelegram Cloud Document 4 5893461163299045618 PDFAndreea FlorinaNo ratings yet
- Case Files Emergency MedicineDocument480 pagesCase Files Emergency MedicinestarrnewmanpaNo ratings yet
- Lippincott S Anesthesia Review 1001 Questions And.20Document1 pageLippincott S Anesthesia Review 1001 Questions And.20Reem Salem0% (1)
- PRES MCQsDocument218 pagesPRES MCQsdoctorbilalsNo ratings yet
- PACU Monitoring Sheet - RR Record - SCT-CONDocument4 pagesPACU Monitoring Sheet - RR Record - SCT-CONFitz JaminitNo ratings yet
- Diploma Guide - EnglishDocument11 pagesDiploma Guide - EnglishAndra Victoria TitaNo ratings yet
- Neonatal ResuscitationDocument7 pagesNeonatal ResuscitationJavier López García100% (1)
- EDAIC MOCK TEST For Part 2 Exam From Team Targetedaic 4Document7 pagesEDAIC MOCK TEST For Part 2 Exam From Team Targetedaic 4Ramanan BothuNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanJewelyn Bronda100% (2)
- UKZN Handbook of AnaesthesiaDocument178 pagesUKZN Handbook of Anaesthesiajhqmpzg7sj100% (1)
- Obstetric Guidelines 2017Document288 pagesObstetric Guidelines 2017susnari100% (1)
- The Physiology Viva: Questions & Answers: Available NowDocument1 pageThe Physiology Viva: Questions & Answers: Available NowManoj VimalNo ratings yet
- Pathophysiology of Sepsis American Journal of PathologyDocument10 pagesPathophysiology of Sepsis American Journal of PathologyStella Gracia OctaricaNo ratings yet
- Stoelting Anasthesia and Co Existing Disease PDFDocument28 pagesStoelting Anasthesia and Co Existing Disease PDFEgidia SetyaNo ratings yet
- Avinash B Kumar MD Assistant Professor Anesthesiology and Critical Care Dec 2006Document29 pagesAvinash B Kumar MD Assistant Professor Anesthesiology and Critical Care Dec 2006sgod34No ratings yet
- TIVA Part I - Pharmacokinetic Principles and Methods of Delivery PDFDocument56 pagesTIVA Part I - Pharmacokinetic Principles and Methods of Delivery PDFMaria José RecheNo ratings yet
- EXM FFICM MCQ Candidate Instructions Jan2015Document4 pagesEXM FFICM MCQ Candidate Instructions Jan2015Sohail RazaNo ratings yet
- Cardiac/Cardiogenic Shock: Clinical Practice GuidelinesDocument3 pagesCardiac/Cardiogenic Shock: Clinical Practice GuidelinesAnonymous Yo0mStNo ratings yet
- CCSAP 2017book3 Sample ChapterDocument20 pagesCCSAP 2017book3 Sample ChapterMohanBabuNo ratings yet
- General AnestDocument35 pagesGeneral AnestMauz AshrafNo ratings yet
- Anesthesia For GeriatricDocument21 pagesAnesthesia For GeriatricintanNo ratings yet
- Anesthetic Consideration in Hypertensive PatientDocument11 pagesAnesthetic Consideration in Hypertensive PatientYosiAsmaraNo ratings yet
- Geriatric NeuroanesthesiDocument333 pagesGeriatric NeuroanesthesiAdi Wira HadiNo ratings yet
- Journal ClubDocument26 pagesJournal Clubysindhura23gmailcom100% (1)
- Paediatric Anaesthesia PDFDocument33 pagesPaediatric Anaesthesia PDFMarcelitaTaliaDuwiriNo ratings yet
- Anesthesia For Cesarean SectionDocument60 pagesAnesthesia For Cesarean Sectionmaheralrwimi100% (1)
- Adult Tachycardia (With Pulse) AlgorithmDocument1 pageAdult Tachycardia (With Pulse) AlgorithmJames ChoiNo ratings yet
- Complications of General Anesthesia (Summary)Document19 pagesComplications of General Anesthesia (Summary)Hassan.shehri100% (2)
- Advanced Cardiac Life SupportDocument37 pagesAdvanced Cardiac Life SupportRoy Acosta GumbanNo ratings yet
- Exm Fficm MCQ Sba ExamplequestionsDocument1 pageExm Fficm MCQ Sba ExamplequestionsMuhammad Asim RanaNo ratings yet
- Anesthesia - State of Narcosis, Analgesia, Relaxation, and Loss of Reflex. Effects of AnesthesiaDocument3 pagesAnesthesia - State of Narcosis, Analgesia, Relaxation, and Loss of Reflex. Effects of AnesthesiaJhevilin RMNo ratings yet
- NRNP 6675 15 Week 6 Midterm Exam Questions and Answers 2023Document11 pagesNRNP 6675 15 Week 6 Midterm Exam Questions and Answers 2023Nelson MandelaNo ratings yet
- 1) Vasoplegia During Cardiac Surgery Current Concepts and Management 2010Document5 pages1) Vasoplegia During Cardiac Surgery Current Concepts and Management 2010Carolina QuirogaNo ratings yet
- PALS Pulseless Arrest Algorithm: Kleinman, M. E. Et Al. Circulation 2010 122:S876-S908Document3 pagesPALS Pulseless Arrest Algorithm: Kleinman, M. E. Et Al. Circulation 2010 122:S876-S908YONE LENINNo ratings yet
- 5 ECG Interpretation With AnswersDocument48 pages5 ECG Interpretation With AnswersQusai Ibraheem100% (1)
- Prehospital Anesthesia HandbookDocument46 pagesPrehospital Anesthesia HandbookoscarNo ratings yet
- Internship Manual For MBBSDocument29 pagesInternship Manual For MBBSKoustav ChakrabortyNo ratings yet
- Coronary Artery Disease CAD PathophysiologyDocument5 pagesCoronary Artery Disease CAD PathophysiologyKusum RoyNo ratings yet
- Pulmo ThromboembolismDocument34 pagesPulmo ThromboembolismAlexander Santiago ParelNo ratings yet
- Anesthesia: A Comprehensive Review (5th Edition)Document1 pageAnesthesia: A Comprehensive Review (5th Edition)brakim23No ratings yet
- SOSD Phases of Fluid ResuscitationDocument8 pagesSOSD Phases of Fluid ResuscitationAvinash KumbharNo ratings yet
- Pharmacology of Cardiac Function: Section of Pharmacology of the International Union of Physiological SciencesFrom EverandPharmacology of Cardiac Function: Section of Pharmacology of the International Union of Physiological SciencesOtto KrayerNo ratings yet
- Studyprotocol Open AccessDocument6 pagesStudyprotocol Open Accessnh2411No ratings yet
- Randomized Controlled Trial of Vitamin D Supplementation in Children With Autism Spectrum DisorderDocument10 pagesRandomized Controlled Trial of Vitamin D Supplementation in Children With Autism Spectrum Disordernh2411No ratings yet
- Omega-3 and Polyunsaturated Fat For Prevention of Depression and Anxiety Symptoms: Systematic Review and Meta-Analysis of Randomised TrialsDocument8 pagesOmega-3 and Polyunsaturated Fat For Prevention of Depression and Anxiety Symptoms: Systematic Review and Meta-Analysis of Randomised Trialsnh2411No ratings yet
- Diagnostic Histopathology Volume Issue 2019 (Doi 10.1016/j.mpdhp.2019.07.004) Kousios, Andreas Roufosse, Candice - An Update On Paraprotein-Related Renal PathologyDocument14 pagesDiagnostic Histopathology Volume Issue 2019 (Doi 10.1016/j.mpdhp.2019.07.004) Kousios, Andreas Roufosse, Candice - An Update On Paraprotein-Related Renal Pathologynh2411No ratings yet
- Prosthetic Repair of Acutely Incarcerated Groin Hernias: A Prospective Clinical Observational Cohort StudyDocument6 pagesProsthetic Repair of Acutely Incarcerated Groin Hernias: A Prospective Clinical Observational Cohort Studynh2411No ratings yet
- GI Tract Protozoan Entamoeba histolyticaDocument25 pagesGI Tract Protozoan Entamoeba histolyticanh2411No ratings yet
- Acute scrotal pain: Evaluating important differentials in primary careDocument3 pagesAcute scrotal pain: Evaluating important differentials in primary carefbihansipNo ratings yet
- Journal Neuropediatri PDFDocument8 pagesJournal Neuropediatri PDFHalimah PramudiyantiNo ratings yet
- Obstruksi Usus (Bowel Obstruction)Document7 pagesObstruksi Usus (Bowel Obstruction)bhatubimNo ratings yet
- Percutaneous Laser Disk Decompression: A Review of The LiteratureDocument4 pagesPercutaneous Laser Disk Decompression: A Review of The Literaturenh2411No ratings yet
- (Doi 10.1002/14651858.cd000127.pub2) Duley, Lelia - Cochrane Database of Systematic Reviews (Reviews) - Magnesium Sulphate Versus Diazepam For Eclampsia PDFDocument65 pages(Doi 10.1002/14651858.cd000127.pub2) Duley, Lelia - Cochrane Database of Systematic Reviews (Reviews) - Magnesium Sulphate Versus Diazepam For Eclampsia PDFnh2411No ratings yet
- Structure and Function of the Skin ExplainedDocument9 pagesStructure and Function of the Skin Explainednh2411No ratings yet
- Management of Tinea Corporis, Tinea CrurisDocument10 pagesManagement of Tinea Corporis, Tinea CrurisRansidelenta Vistaprila ElmardaNo ratings yet
- 2018 ESC-EACTS Guidelines On Myocardial RevascularizationDocument96 pages2018 ESC-EACTS Guidelines On Myocardial RevascularizationTony Miguel Saba SabaNo ratings yet
- Deep Neck and Odontogenic Infections: Key PointsDocument12 pagesDeep Neck and Odontogenic Infections: Key Pointsnh2411No ratings yet
- Edema ParuDocument15 pagesEdema Parunh2411No ratings yet
- Structure and Function of the Skin ExplainedDocument9 pagesStructure and Function of the Skin Explainednh2411No ratings yet
- 1 s2.0 S0010782416303857 MainDocument9 pages1 s2.0 S0010782416303857 Mainnh2411No ratings yet
- Induced SputumDocument6 pagesInduced Sputumnh2411No ratings yet
- HEAMTURIADocument19 pagesHEAMTURIAnh2411No ratings yet
- Srep 34201Document11 pagesSrep 34201nh2411No ratings yet
- Glukoma TooDocument86 pagesGlukoma Toofegx_17No ratings yet
- Ecology of Microorganism 1Document16 pagesEcology of Microorganism 1nh2411No ratings yet
- 2014 2015 Tuition and Fees by Program PDFDocument23 pages2014 2015 Tuition and Fees by Program PDFnh2411No ratings yet
- Ovarian Cyst Management in PAG GuidelineDocument9 pagesOvarian Cyst Management in PAG Guidelinenh2411No ratings yet
- Srep 34201Document11 pagesSrep 34201nh2411No ratings yet
- Benazepril Hydrochloride (Drug Study)Document3 pagesBenazepril Hydrochloride (Drug Study)Franz.thenurse6888100% (1)
- Studies On The Stability of Chicken IgY in Different Sugars Complex Carbohydrates and Food MaterialsDocument12 pagesStudies On The Stability of Chicken IgY in Different Sugars Complex Carbohydrates and Food MaterialsJohnrel SecretariaNo ratings yet
- TranslateeDocument6 pagesTranslateeAmalia Tri UtamiNo ratings yet
- Lab Value MnemonicsDocument10 pagesLab Value MnemonicsSophia CuertoNo ratings yet
- Assessment of The Thorax and LungsDocument108 pagesAssessment of The Thorax and LungsJohn Martin Casihan100% (3)
- Predictions Using Data Mining and Case Based Reasoning A Case Study For RetinopathyDocument4 pagesPredictions Using Data Mining and Case Based Reasoning A Case Study For RetinopathyBiraj kumar BholNo ratings yet
- Sodium Chromate Anhydrous PDFDocument6 pagesSodium Chromate Anhydrous PDFErika WidiariniNo ratings yet
- Clinical Profile of Indian Children With Down SyndromeDocument5 pagesClinical Profile of Indian Children With Down SyndromeRicky Wahyu setiawanNo ratings yet
- Suz 183Document29 pagesSuz 183Benny Chris TantoNo ratings yet
- DR Putu Gde Hari WangsaDocument5 pagesDR Putu Gde Hari Wangsahariwangsa23No ratings yet
- Data FinalDocument72 pagesData FinalAchsan KamalNo ratings yet
- Listening d1Document4 pagesListening d1Ebin PauloseNo ratings yet
- HR-014 SSS Maternity Benefit AcknowledgementDocument1 pageHR-014 SSS Maternity Benefit AcknowledgementBETH CARANDANGNo ratings yet
- Pharmacology and The Older AdultDocument26 pagesPharmacology and The Older AdultJether Joy Hyacinth VelardeNo ratings yet
- Bloodstream Infection Event (Central Line-Associated Bloodstream Infection and Non-Central Line Associated Bloodstream Infection)Document50 pagesBloodstream Infection Event (Central Line-Associated Bloodstream Infection and Non-Central Line Associated Bloodstream Infection)Luthvia AnnisaNo ratings yet
- Template For Case ReportDocument2 pagesTemplate For Case ReportevanNo ratings yet
- Instructions For Use: Home Sperm Test For Male FertilityDocument2 pagesInstructions For Use: Home Sperm Test For Male FertilityRAVAN ZJNo ratings yet
- Corpectomy Cage Surgical TechniquesDocument18 pagesCorpectomy Cage Surgical TechniquesJulian VargasNo ratings yet
- Skills Math WorksheetDocument4 pagesSkills Math WorksheetBrennan MaguireNo ratings yet
- Afeccion Ocular y Blefaroconjuntivitis Por Leishmania de HumanosDocument4 pagesAfeccion Ocular y Blefaroconjuntivitis Por Leishmania de HumanosPilar Sanchez GuiraoNo ratings yet
- How to treat and prevent breast engorgementDocument1 pageHow to treat and prevent breast engorgementkurniaNo ratings yet
- Biosure RGDocument2 pagesBiosure RGJuan Martinez Del AngelNo ratings yet
- Amoxicillin Therapy Valid for Pneumonia in ChildrenDocument4 pagesAmoxicillin Therapy Valid for Pneumonia in ChildrenShofaajiNo ratings yet
- Ebp Picc Line - RevisedDocument6 pagesEbp Picc Line - Revisedapi-234544335No ratings yet
- Progress in Retinal and Eye Research: Contents Lists Available atDocument40 pagesProgress in Retinal and Eye Research: Contents Lists Available atSalsa BillaNo ratings yet
- Als CapstoneDocument9 pagesAls Capstoneapi-514758382No ratings yet