Professional Documents
Culture Documents
Peeping Painless Proptosis
Uploaded by
Putri YingOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Peeping Painless Proptosis
Uploaded by
Putri YingCopyright:
Available Formats
EMERGENC Y MED IC INE RESID EN CY CPC
Peeping Painless Proptosis
MAUREEN LLOYD, MD; XIAO CHI ZHANG, MD, MS; SARAH JOSEPH, MD;
JAY BARUCH, MD; MATTHEW SIKET, MD; WILLIAM BINDER, MD
From the Case Records of the Alpert Medical School of Her left extraocular motion (EOM) was intact, but her
Brown University Residency in Emergency Medicine right eye movement was restricted on superior temporal,
inferior temporal, superior nasal, and inferior nasal motions.
She was able to see fingers through her left proptotic eye, but
K E YWORDS: proptosis, retrobulbar hematoma, trauma,
unable to perceive light on her right eye. The patient denied
orbital tumor, emergency department, ophthalmology
diplopia and there was no appreciable afferent pupillary
defect. The remainder of her physical exam and trauma eval-
DR. XIAO CHI ZHANG: A 92-year-old woman with dementia uation was negative for any major deformities, contusions,
was brought to the emergency department (ED) from a nurs- ecchymosis, hematomas, lacerations or step-offs.
ing home for headache and “left eye bulge” after falling Initial blood work was unremarkable for acute metabolic
backward, striking her head on the ground. While the review or hematologic abnormalities. Imaging revealed a normal
of systems was limited due to the patient’s baseline demen- chest x-ray. A computed tomography (CT) scan of the brain,
tia, she only reported occipital headache, left knee pain and face, and neck revealed a soft-tissue mass within the left
denied any eye pain, changes in her vision and stated: “my orbital space without any obvious evidence of acute infarct,
right eye is my bad eye.” Her past medical history was signif- hemorrhage, mass or mass effect in the brain or facial frac-
icant for bilateral glaucoma, right orbital reconstruction due tures (Figure 2). The differential diagnosis for this mass
to childhood trauma, and coronary artery disease. Current included a retrobulbar hematoma, given the patient’s history
medications included aspirin/extended-release dipyridamole of trauma while on an antiplatelet agent.
(Aggrenox®), timolol, and latanoprost eye drops.
On arrival to the ED, the patient’s blood pressure was DR. NADINE HIMMELFARB: What were your immediate
154/66 mm Hg, pulse rate 63 beats/min, respiratory rate 20 concerns when you recognized the proptosis in the setting
breaths/min, temperature 36.5°C (97.7°F), and SaO2 96% on of head trauma?
room air. She was in no acute distress without any obvious
signs of external trauma. She was alert and oriented to her DR. SARAH JOSEPH: One of the most concerning pathol-
name, perseverated on her headache, and had reproducible ogies when confronted with a proptotic eye after head
left knee discomfort with active range of motion. Her exter- trauma is retrobulbar hematoma, especially in the setting of
nal ocular exam was significant for a left proptotic eye, with anti-platelet medication use. Retrobulbar hematoma is con-
a 3mm pupil that was reactive to light and a normal appear- sidered a true ophthalmologic emergency and a vision threat-
ing right eye with a surgical, 3mm pupil; there were no signs ening condition as it can rapidly lead to orbital compartment
of irritation or hyphema on either eye (Figure 1). syndrome (OCS), where the optic nerve experiences rapidly
Figure 1. Patient has a
left proptotic eye (white
arrowheads) with intact
corneal red reflexes
(white arrow), without
visual acuity or range of
motion deficits after a
traumatic head injury.
W W W. R I M E D . O R G | RIMJ ARCHIVES | A U G U S T W E B PA G E AUGUST 2016 RHODE ISLAND MEDICAL JOURNAL 40
EMERGENC Y MED IC INE RESID EN CY CPC
Figure 2. Non-Contrast CT Brain and Face after trau-
ma. Frontal (top) and coronal (bottom) views demon-
strating proptosis of the left orbit (white arrowheads)
with a lobulated hyperdense soft tissue mass (white
arrow) within the left orbit, initially concerning for
retrobulbar hematoma in the setting of head trauma.
elevated intraorbital pressure, resulting in
nerve ischemia and permanent blindness.1
DR. MICHELLE LIPPMANN: What are
some of the common clinical findings asso-
ciated with retrobulbar hematoma? What
are some of the other potentially traumatic
vision threatening pathologies that war-
rant an emergent ophthalmology consult?
DR. ZHANG: Patients with OCS often pres-
ent with decreased vision, severe eye pain
and proptosis. Additional concerning find-
ings include diplopia, periorbital swelling,
afferent pupillary defect (APD), diffuse
subconjunctival hemorrhage, chemosis,
tight eyelids and decreased retropulsion as
physical evidences of increased intraorbital
pressure (IOP).2 Fundoscopic exam may
also reveal vascular and optic disc edema
and the absence of spontaneous venous
pulsation (SVP). While our patient did have
a proptotic eye and a retrobulbar mass, she
did not endorse any new ocular complaints
and or new vision deficits, making her case
a clinical conundrum.
Other vision-threatening conditions that
require emergent ophthalmologist consultation include caus- DR. JOSEPH: In the setting of progressive vision loss and
tic eye exposures (ocular chemical burns) or direct ocular concern for OCS, clinicians should consider performing an
trauma (i.e. open globe ruptures) that require EM clinicians emergent lateral canthotomy.3 EM clinicians should con-
to either initiate immediate ocular irrigation or placing a pro- sider performing this vision saving procedure by identifying
tective barrier. Neither ophthalmology emergencies would the lateral canthus and incising the canthus at full thickness
present as painless proptosis without external irritation. to sever the lateral canthal tendon in order to release the
ocular pressure. After lateral canthotomy, efforts should be
DR. JESSICA SMITH: How do you explain the poor vision made to decrease IOP, including head-of-bed elevation, anal-
(count-fingers only) of the left eye and respective absence of gesia, antiemetics, and coagulopathy corrections. Visual acu-
afferent pupillary defect (APD)? ity and intraocular pressure should also be assessed every 15
minutes after the procedure until the patient demonstrates
DR. MAUREEN LLOYD: Great catch! We reviewed the objective and subjective improvements.4
patient’s records and she has always had better vision on her Complications may include eyelid droop, ptosis, or infec-
left eye than her right eye; at the ED bedside, the right eye tion, the former of which can be cosmetically addressed by
had no light perception. Even after the head trauma, the left an oculoplastic surgeon after OCS has been appropriately
eye was still the better seeing-eye. As a result, she did not addressed.4 It is imperative that patients with high suspi-
develop an APD because the left eye still offered more afferent cion of an open globe should not receive any examination or
input than the right eye. therapeutic procedures, such as IOP measurement or lateral
canthotomy. In such cases an eye shield should be placed
DR. WILLIAM BINDER: If this patient had a retrobulbar over the eye until the patient is emergently evaluated by
hematoma, what would be the ultimate therapy? an ophthalmologist.
W W W. R I M E D . O R G | RIMJ ARCHIVES | A U G U S T W E B PA G E AUGUST 2016 RHODE ISLAND MEDICAL JOURNAL 41
EMERGENC Y MED IC INE RESID EN CY CPC
DR. MARK GREVE: The patient appeared to have proptosis References
from a retrobulbar mass, but did not have severe eye pain or 1. Lima V, Burt B, Leibovitch I, et al. Orbital compartment syn-
drome: the ophthalmic surgical emergency. Surv Ophthalmol
vision loss. Was a lateral canthotomy performed?
2009; 54:441.
2. Sun MT, Chan WO, Selva D. Traumatic orbital compartment
DR. ZHANG: While this patient had every risk factor for a syndrome: importance of the lateral canthomy and cantholysis.
retrobulbar hematoma and a concerning CT imaging, we Emerg Med Australas 2014; 26:274.
were hesitant to perform this procedure as the patient did 3. Traumatic retrobulbar hemorrhage. In: The Wills Eye Manual:
Office and Emergency Room Diagnosis and Treatment of Eye
not have any orbital fractures, compromised visual acuity Disease, 5th ed, Ehlers JP, Shah CP (Eds), Lippincott Williams &
or EOM on the proptotic eye. We consulted ophthalmology Wilkins, Philadelphia 2008. p.30.
for the unusual presentation of retrobulbar hematoma and 4. Vassallo S, Hartstein M, Howard D, Stetz J. Traumatic retrobul-
bar hemorrhage: emergent decompression by lateral canthoto-
painless proptosis.
my and cantholysis. J Emerg Med 2002; 22:251.
DR. ROBERT TUBBS : What did the ophthalmologist find? Authors
Maureen Lloyd, MD, Division of Ophthalmology Residency, Alpert
DR. LLOYD: I was the consulting ophthalmologist. Because Medical School of Brown University.
we had low suspicion for ruptured globe injuries, I was able Xiao Chi Zhang, MD, MS, Department of Emergency Medicine,
Alpert Medical School of Brown University.
to measure the intraocular pressure (IOP) on both eyes and
Sarah Joseph, MD, Department of Emergency Medicine, Alpert
noted a lower IOP on the left proptotic eye than the right
Medical School of Brown University.
normal appearing eye (15 vs. 30 mm Hg). While pupillary dil-
Jay Baruch, MD, Associate Professor of Emergency Medicine,
atation in the setting of significant head trauma can interfere Alpert Medical School of Brown University.
with subsequent pupillary exams to discern potential mass Matthew Siket, MD, Assistant Professor of Emergency Medicine,
effect, the CT in this case did not reveal intracranial hemor- Alpert Medical School of Brown University.
rhage and we were able to dilate this patient for funduscopic William Binder, MD, Associate Professor of Emergency Medicine,
exam. A fully dilated slit lamp exam only revealed dilated Alpert Medical School of Brown University.
tortuous conjunctival vessels in the left proptotic eye, with
Correspondence
normal appearing cornea, anterior chamber, iris, lens and William Binder, MD
vitreous on both eyes without any fluorescein uptake. The Emergency Medicine Foundation
fundus exam, including disc, macula, and vessels of both 593 Eddy St.
eyes was also normal. Providence, RI 02903
Due to the reassuring ocular exam, we agreed to hold 401-444-5411
off on performing a lateral canthotomy in the absence of Fax 401-444-4307
impending vision loss and instead observed the patient for William_Binder@brown.edu
any further worsening or changes in vision.
DR. BINDER: Did the patient worsen?
DR. ZHANG: Two hours after the patient’s arrival, the ED
providers noted a gradual resolution of the patient’s propto-
sis. The initial CT finding was concerning for a retrobul-
bar hematoma in the setting of head trauma; however, this
read was reevaluated and the Hounsfield units were consid-
ered to be less consistent with blood, and more consistent
with a “lobulated hyperdense soft tissue mass within the
left orbit suspicious for tumor.” The tumor had apparently
been displaced by the trauma, and over time reverted back
to its previous position. The finding was discussed with the
patient’s family and a joint decision was made to withhold
any surgical intervention due to the patient’s age and goals
of care. The patient was ultimately discharged back to the
nursing home with outpatient ophthalmology follow-up for
diagnosis with a new, left orbital tumor. The patient con-
tinued to experience intermittent painless proptosis at the
nursing home after discharge, but never complained of any
visual disturbances.
W W W. R I M E D . O R G | RIMJ ARCHIVES | A U G U S T W E B PA G E AUGUST 2016 RHODE ISLAND MEDICAL JOURNAL 42
You might also like
- Homeopathic Alternatives To Conventional Drug TherapiesDocument239 pagesHomeopathic Alternatives To Conventional Drug Therapiesmr.mukundNo ratings yet
- Neuro-Ophthalmology: Introduction: James Goodwin, MD (Attending)Document4 pagesNeuro-Ophthalmology: Introduction: James Goodwin, MD (Attending)Mariano FioreNo ratings yet
- Label Nama Obat Di Rak ObatDocument6 pagesLabel Nama Obat Di Rak Obatanon_756054910No ratings yet
- Life-members-Indian Medico-Legal & Ethics Association (Imlea) - Mix State & Mix DepartmentDocument64 pagesLife-members-Indian Medico-Legal & Ethics Association (Imlea) - Mix State & Mix DepartmentKriti Kumari100% (1)
- Uveitis Diagnosis and Treatment GuideDocument72 pagesUveitis Diagnosis and Treatment GuideSafa Abdualrahaman Ali HamadNo ratings yet
- Cogan-Reese Syndrome - A Rare Case of Unilateral GlaucomaDocument8 pagesCogan-Reese Syndrome - A Rare Case of Unilateral GlaucomaDr. Abhishek OnkarNo ratings yet
- 7 - Ignacio Richelle PDFDocument2 pages7 - Ignacio Richelle PDFRichelle IgnacioNo ratings yet
- Post-Craniotomy Blindness in The Supine Position UDocument6 pagesPost-Craniotomy Blindness in The Supine Position UZezo AbdullahNo ratings yet
- Approaching Acute Vertigo With Diplopia - A Rare Skew Deviation in Vestibular NeuritisDocument7 pagesApproaching Acute Vertigo With Diplopia - A Rare Skew Deviation in Vestibular NeuritisRudolfGerNo ratings yet
- Clinical CasesDocument49 pagesClinical Casesnorfitri hadeyNo ratings yet
- Post-Thyroidectomy Visual Loss in A Patient With Comorbidities - Case ReportDocument4 pagesPost-Thyroidectomy Visual Loss in A Patient With Comorbidities - Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Oculomotor Nerve Palsy Case FileDocument2 pagesOculomotor Nerve Palsy Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Acute Orbital Compartment Syndrome (AOCSDocument3 pagesAcute Orbital Compartment Syndrome (AOCSFrancois Donatien De SadeNo ratings yet
- Orbital Apex Syndrome from Herpes Zoster OphthalmicusDocument4 pagesOrbital Apex Syndrome from Herpes Zoster OphthalmicusYosiita KartinaaNo ratings yet
- Traumatic Hyphema: A Teaching Case Report: Priscilla Lenihan, OD Dorothy Hitchmoth, OD, FAAODocument9 pagesTraumatic Hyphema: A Teaching Case Report: Priscilla Lenihan, OD Dorothy Hitchmoth, OD, FAAOMarshaNo ratings yet
- Orbital Apex Syndrome With Encephalitis A Rare and Serious Complication of Herpes Zoster Opthalmicus - Ludwig Melino Tjokrovonco 2Document12 pagesOrbital Apex Syndrome With Encephalitis A Rare and Serious Complication of Herpes Zoster Opthalmicus - Ludwig Melino Tjokrovonco 2Handi KrisnaniNo ratings yet
- A Rare Case of Terson Syndrome With Subarachnoid HemorrhageDocument12 pagesA Rare Case of Terson Syndrome With Subarachnoid HemorrhageNinaNo ratings yet
- Case 1: 70-Yr Man Complains of Sudden and Total Loss Vision in One Eye. No Pain or Other SymptomsDocument17 pagesCase 1: 70-Yr Man Complains of Sudden and Total Loss Vision in One Eye. No Pain or Other SymptomsCherry TamNo ratings yet
- Typical Optic Neuritis RevDocument6 pagesTypical Optic Neuritis RevAdhi AmertajayaNo ratings yet
- 100255-Article Text-1482-2-10-20220311Document6 pages100255-Article Text-1482-2-10-20220311Fachry RahmanNo ratings yet
- The Hyperacute Vestibular Syndrome Ear or BrainDocument2 pagesThe Hyperacute Vestibular Syndrome Ear or BrainDea CantikNo ratings yet
- Frontal Sinus Mucoceles Causing ProptosisDocument4 pagesFrontal Sinus Mucoceles Causing ProptosisAji Setia UtamaNo ratings yet
- Medicine: Sumatriptan-Induced Angle-Closure GlaucomaDocument4 pagesMedicine: Sumatriptan-Induced Angle-Closure GlaucomanidaNo ratings yet
- Neurosyphilis Masquerading As An Acute Adie's Tonic Pupil: Report of A CaseDocument6 pagesNeurosyphilis Masquerading As An Acute Adie's Tonic Pupil: Report of A CaseOlvaria MisfaNo ratings yet
- American Journal of Ophthalmology Case ReportsDocument3 pagesAmerican Journal of Ophthalmology Case ReportsElison Jaya PanggaloNo ratings yet
- Secondary Hemorrhage in Traumatic HyphemaDocument1 pageSecondary Hemorrhage in Traumatic HyphemaJennifer JaneNo ratings yet
- MainDocument4 pagesMainVicky ObandoNo ratings yet
- OcularuslecturepdfDocument115 pagesOcularuslecturepdfIyou MistitansNo ratings yet
- Iih EvaluationDocument19 pagesIih Evaluationapi-356382313No ratings yet
- Manager A 10 11 21 171674bDocument4 pagesManager A 10 11 21 171674bShirakawa AlmiraNo ratings yet
- Diagnosis and Surgical Management of Isolated InferiorDocument7 pagesDiagnosis and Surgical Management of Isolated InferiorKelly Herencia AnayaNo ratings yet
- Laporan Kasus NeurooftalmologiDocument12 pagesLaporan Kasus NeurooftalmologiPradistya Syifa YudiasariNo ratings yet
- 713full_221024_135448 (1)Document8 pages713full_221024_135448 (1)Olga Manco GuzmánNo ratings yet
- Fah Ling 2016Document2 pagesFah Ling 2016Anonymous OjlR4HLNo ratings yet
- SOAL NO BaruDocument16 pagesSOAL NO Barukautsar abiyogaNo ratings yet
- Fledelius 1999Document3 pagesFledelius 1999Uğur YaylaNo ratings yet
- Taiwan Journal of Ophthalmology: Hui-Chen Cheng, May-Yung Yen, An-Guor WangDocument3 pagesTaiwan Journal of Ophthalmology: Hui-Chen Cheng, May-Yung Yen, An-Guor WangOmarAlbeshreiNo ratings yet
- Acute Monocular Vision LossDocument9 pagesAcute Monocular Vision LossRoberto López MataNo ratings yet
- Journal Casereport 1Document5 pagesJournal Casereport 1Arif MohammadNo ratings yet
- Essential Infantile Esotropia An Unusual Case ReportDocument3 pagesEssential Infantile Esotropia An Unusual Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Bilateral Vision Loss Associated With Radiofrequency ExposureDocument5 pagesBilateral Vision Loss Associated With Radiofrequency ExposurePisj Belongs To WhatsappNo ratings yet
- Diagnosis and Management of Silent Sinus SyndromeDocument2 pagesDiagnosis and Management of Silent Sinus SyndromeRaja Fauzan FahleviNo ratings yet
- Herpes Zoster OphthalmicusDocument12 pagesHerpes Zoster OphthalmicusGio Vano NaihonamNo ratings yet
- tmp874C TMPDocument9 pagestmp874C TMPFrontiersNo ratings yet
- Self-Resolving Ischemic Third Nerve PalsyDocument10 pagesSelf-Resolving Ischemic Third Nerve PalsyYobbi ArisaputraNo ratings yet
- Compresi N Vascular GL - HeDocument2 pagesCompresi N Vascular GL - Hexwkpr7hfrsNo ratings yet
- Spontaneous Resolution of Ophthalmologic Symptoms Following Bilateral Traumatic Carotid Cavernous FistulaeDocument6 pagesSpontaneous Resolution of Ophthalmologic Symptoms Following Bilateral Traumatic Carotid Cavernous FistulaeMaria Angelina BunawanNo ratings yet
- Journal OphtalmologyDocument3 pagesJournal OphtalmologyFaza KeumalasariNo ratings yet
- Bilateral Facial Nerve (Bells) Palsy in A 24-Year-Old WomanDocument3 pagesBilateral Facial Nerve (Bells) Palsy in A 24-Year-Old WomanmimicamasoNo ratings yet
- Bilateral Facial Nerve (Bell's) Palsy in A 24-Year-Old Woman: A Case ReportDocument3 pagesBilateral Facial Nerve (Bell's) Palsy in A 24-Year-Old Woman: A Case Reportokto namikaNo ratings yet
- HLA B-27 Associated Anterior Uveitis: American Academy of Optometry: Case Report #1Document22 pagesHLA B-27 Associated Anterior Uveitis: American Academy of Optometry: Case Report #1Shabrina Amalia SuciNo ratings yet
- Sympathetic Ophthalmia After Vitreoretinal Surgery: A Report of Two CasesDocument11 pagesSympathetic Ophthalmia After Vitreoretinal Surgery: A Report of Two CasesAlexander RezaNo ratings yet
- Multiple Sclerosis With Ophthalmologic Onset - Case ReportDocument5 pagesMultiple Sclerosis With Ophthalmologic Onset - Case ReportVannyNo ratings yet
- Uveitis-Glaucoma-Hyphema (UGH) Syndrome - A Complex ComplicationDocument4 pagesUveitis-Glaucoma-Hyphema (UGH) Syndrome - A Complex ComplicationSalomon SalomonNo ratings yet
- Iridocorneal Endothelial Syndrome in A 14-Year-Old MaleDocument2 pagesIridocorneal Endothelial Syndrome in A 14-Year-Old MaleCamiCasasNo ratings yet
- Acute Retinal Necrosis Following Contralateral Herpes Zoster OphthalmicusDocument4 pagesAcute Retinal Necrosis Following Contralateral Herpes Zoster Ophthalmicusnurul_sharaswatiNo ratings yet
- Paradoxical Head Tilt in Unilateral Traumatic Superior Oblique PalsyDocument3 pagesParadoxical Head Tilt in Unilateral Traumatic Superior Oblique PalsyVasishta NadellaNo ratings yet
- Hypertensive Retinopathy Presenting as Angle Closure Glaucoma CaseDocument5 pagesHypertensive Retinopathy Presenting as Angle Closure Glaucoma CaseyunjaealwaysNo ratings yet
- MRI Findings in Post-Operative Bilateral Posterior Ischemic Optic NeuropathyDocument3 pagesMRI Findings in Post-Operative Bilateral Posterior Ischemic Optic NeuropathyJan JanNo ratings yet
- Bilateral Facial Nerve Palsy: Challenges in Diagnosis: Case ReportDocument3 pagesBilateral Facial Nerve Palsy: Challenges in Diagnosis: Case ReportPutri YunandaNo ratings yet
- Perebaikan DG Mandala - Terapi Cermin Kasus BRAO New 20 OktoberDocument9 pagesPerebaikan DG Mandala - Terapi Cermin Kasus BRAO New 20 OktoberAriandindi AriandiNo ratings yet
- PDF StrabismusDocument1 pagePDF StrabismusirawadiputraNo ratings yet
- ID Hubungan Tingkat Pengetahuan Pasien DiabDocument6 pagesID Hubungan Tingkat Pengetahuan Pasien DiabJoni TriliwijayaNo ratings yet
- Jurnal Wawan PDFDocument10 pagesJurnal Wawan PDFPutri YingNo ratings yet
- Jurnal Wawan PDFDocument10 pagesJurnal Wawan PDFPutri YingNo ratings yet
- Malingering and Factitious Disorder: Christopher Bass, Derick T WadeDocument10 pagesMalingering and Factitious Disorder: Christopher Bass, Derick T WadePutri YingNo ratings yet
- Factitious Disorders 2: Factitious Disorders and Malingering: Challenges For Clinical Assessment and ManagementDocument11 pagesFactitious Disorders 2: Factitious Disorders and Malingering: Challenges For Clinical Assessment and ManagementPutri YingNo ratings yet
- Jurnal Wawan PDFDocument10 pagesJurnal Wawan PDFPutri YingNo ratings yet
- KDocument8 pagesKPutri YingNo ratings yet
- Taira 2011Document5 pagesTaira 2011Putri YingNo ratings yet
- Isoniazid Induced AlopeciaDocument2 pagesIsoniazid Induced AlopeciaPutri YingNo ratings yet
- Effectiveness of antidepressants for depression in primary careDocument11 pagesEffectiveness of antidepressants for depression in primary carePutri YingNo ratings yet
- Factitious Disorders 2: Factitious Disorders and Malingering: Challenges For Clinical Assessment and ManagementDocument11 pagesFactitious Disorders 2: Factitious Disorders and Malingering: Challenges For Clinical Assessment and ManagementPutri YingNo ratings yet
- Maculopapular Drug Eruption Secondary To Pyrazinamide: Case Based LearningDocument4 pagesMaculopapular Drug Eruption Secondary To Pyrazinamide: Case Based LearningPutri YingNo ratings yet
- Effectiveness of Psychological Treatments For DepressiveDocument13 pagesEffectiveness of Psychological Treatments For DepressiveNathaly BerríoNo ratings yet
- Alcohol Use Disorder Severity and Reported Reasons Not To Seek Treatment: A Cross-Sectional Study in European Primary Care PracticesDocument10 pagesAlcohol Use Disorder Severity and Reported Reasons Not To Seek Treatment: A Cross-Sectional Study in European Primary Care PracticesPutri YingNo ratings yet
- A Case Report On Isoniazid Induced Bullous Drug ReactionDocument6 pagesA Case Report On Isoniazid Induced Bullous Drug ReactionPutri YingNo ratings yet
- Pone 0149818Document11 pagesPone 0149818rachel0301No ratings yet
- Severe Skin Rash and Liver Toxic Effects Caused by First-Line Anti-Tuberculosis Drugs: A Case ReportDocument4 pagesSevere Skin Rash and Liver Toxic Effects Caused by First-Line Anti-Tuberculosis Drugs: A Case ReportPutri YingNo ratings yet
- Ispub 11731Document4 pagesIspub 11731Putri YingNo ratings yet
- Case Report: Hypersensitivity Reaction and Tolerance Induction To EthambutolDocument4 pagesCase Report: Hypersensitivity Reaction and Tolerance Induction To EthambutolPutri YingNo ratings yet
- Ajp v1 Id1005Document2 pagesAjp v1 Id1005Putri YingNo ratings yet
- Isoniazid Induced Lupus Presenting As Oral Mucosal Ulcers With PancytopeniaDocument3 pagesIsoniazid Induced Lupus Presenting As Oral Mucosal Ulcers With PancytopeniaPutri YingNo ratings yet
- Ethionamide-Induced Pellagra: by Yashashree Gupta and Ira ShahDocument3 pagesEthionamide-Induced Pellagra: by Yashashree Gupta and Ira ShahPutri YingNo ratings yet
- Hold I Ness 1985Document6 pagesHold I Ness 1985Putri YingNo ratings yet
- Case Report: Hypersensitivity Reaction and Tolerance Induction To EthambutolDocument4 pagesCase Report: Hypersensitivity Reaction and Tolerance Induction To EthambutolPutri YingNo ratings yet
- Korelasi Karakteristik Dengan Penyebab Ketuban Pecah Dini Pada Ibu Bersalin Di Rsu Denisa GresikDocument9 pagesKorelasi Karakteristik Dengan Penyebab Ketuban Pecah Dini Pada Ibu Bersalin Di Rsu Denisa GresikEmilia Rizky FauziyahNo ratings yet
- Medi 96 E6346Document5 pagesMedi 96 E6346Putri YingNo ratings yet
- Commentary Antituberculosis Drug Induced Fixed Drug Eruption A Case Report PDFDocument2 pagesCommentary Antituberculosis Drug Induced Fixed Drug Eruption A Case Report PDFPutri YingNo ratings yet
- Ibrt 10 I 1 P 53Document4 pagesIbrt 10 I 1 P 53Putri YingNo ratings yet
- Case Report: Hypersensitivity Reaction and Tolerance Induction To EthambutolDocument4 pagesCase Report: Hypersensitivity Reaction and Tolerance Induction To EthambutolPutri YingNo ratings yet
- A Case of The Drug Reaction With Eosinophilia and Systemic Symptom (DRESS) Following Isoniazid TreatmentDocument4 pagesA Case of The Drug Reaction With Eosinophilia and Systemic Symptom (DRESS) Following Isoniazid TreatmentPutri YingNo ratings yet
- NAMA PENYAKIT YANG HARUS DAPAT DITANGANI DI LAYANAN PRIMERDocument5 pagesNAMA PENYAKIT YANG HARUS DAPAT DITANGANI DI LAYANAN PRIMERheru suhartoNo ratings yet
- Clinical Case Reports - 2023 - Lee - Reactivated Herpetic Gingivostomatitis With Secondary Herpes Associated ErythemaDocument7 pagesClinical Case Reports - 2023 - Lee - Reactivated Herpetic Gingivostomatitis With Secondary Herpes Associated ErythemaAhmad AbrorNo ratings yet
- Ectopic Pregnancy Modern Diagnosis and Management 2011 PG PDFDocument258 pagesEctopic Pregnancy Modern Diagnosis and Management 2011 PG PDFlidija_milosevic100% (1)
- Fact Sheet InterQual Criteria PortfolioDocument4 pagesFact Sheet InterQual Criteria PortfolioMora MDNo ratings yet
- Coronary Artery Bypass Surgery: UnderstandingDocument24 pagesCoronary Artery Bypass Surgery: UnderstandingNurArsitaPebruatiNo ratings yet
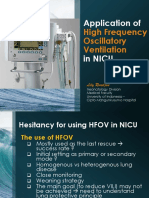
- Application HFOV in NICU - Lily RundjanDocument43 pagesApplication HFOV in NICU - Lily Rundjandiah ayu pitalokaNo ratings yet
- NURSING DIAGNOSIS #2 - HyperthermiaDocument3 pagesNURSING DIAGNOSIS #2 - HyperthermiaEnerolisa ParedesNo ratings yet
- Congestive Nephropathy: A Neglected Entity? Proposal For Diagnostic Criteria and Future PerspectivesDocument21 pagesCongestive Nephropathy: A Neglected Entity? Proposal For Diagnostic Criteria and Future PerspectivesMuhammad SyammNo ratings yet
- NCM 112 Guide to Caring for Patients with CancerDocument15 pagesNCM 112 Guide to Caring for Patients with CancerShiena Mae PelagioNo ratings yet
- KMC To Reduce Neonatal Mortality Hadi P Unair 29 Sept 2016Document63 pagesKMC To Reduce Neonatal Mortality Hadi P Unair 29 Sept 2016mimimomopipiNo ratings yet
- "Physiological Monitoring and Device Interface": Report by Jawia Mustapha BSN2-ADocument21 pages"Physiological Monitoring and Device Interface": Report by Jawia Mustapha BSN2-ADimple AnticamaraNo ratings yet
- Calvary Public Bruce Campus MapDocument2 pagesCalvary Public Bruce Campus MapAlana TindaleNo ratings yet
- K15 - Infeksi Sistem Saraf PusatDocument65 pagesK15 - Infeksi Sistem Saraf PusatZikri Putra Lan LubisNo ratings yet
- Heat StressDocument2 pagesHeat StressmmmmaqboolNo ratings yet
- For Printing Grand Case Group1Document37 pagesFor Printing Grand Case Group1Joco Bordeos AripNo ratings yet
- CF AdimeDocument3 pagesCF Adimeapi-302326926No ratings yet
- PHYSIOLOGICAL EFFECTS OF VALSALVA AND IPPVDocument27 pagesPHYSIOLOGICAL EFFECTS OF VALSALVA AND IPPVChaturika Bandara100% (1)
- Case Study Ms. K 2Document25 pagesCase Study Ms. K 2kelly rosali richardNo ratings yet
- End of Service Incubator 5400Document1 pageEnd of Service Incubator 5400Faizal FlNo ratings yet
- Plateau and Driving Pressure in The Presence of Spontaneous BreathingDocument2 pagesPlateau and Driving Pressure in The Presence of Spontaneous BreathingNaiana MotaNo ratings yet
- Prioritising HTA Funding: The Benefits and Challenges of Using Value of Information in AngerDocument20 pagesPrioritising HTA Funding: The Benefits and Challenges of Using Value of Information in AngerHammad AjaNo ratings yet
- Acquired Peripheral Neuropathies GuideDocument20 pagesAcquired Peripheral Neuropathies Guidefire_n_iceNo ratings yet
- Explanation 2020 1Document315 pagesExplanation 2020 1Reshma Shaji PnsNo ratings yet
- LOI, LOP, RenewalDocument37 pagesLOI, LOP, RenewalShajil VPNo ratings yet
- Introduction To JubileeDocument117 pagesIntroduction To Jubileeangela gnanaduraiNo ratings yet
- HIV Case (Week 2) - Antao, Alvarez, Hasan, Sanaani, UsmanDocument15 pagesHIV Case (Week 2) - Antao, Alvarez, Hasan, Sanaani, UsmanNUR-HATHI SANAANINo ratings yet
- 1986 7992 1 PBDocument8 pages1986 7992 1 PBSapna thakurNo ratings yet