Professional Documents
Culture Documents
11epidural Anesthesia
Uploaded by
Sry Rahayu0 ratings0% found this document useful (0 votes)
5 views3 pagesPerdarahan saluran cerna
Original Title
11Epidural Anesthesia
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPerdarahan saluran cerna
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views3 pages11epidural Anesthesia
Uploaded by
Sry RahayuPerdarahan saluran cerna
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 3
Gastrointestinal Bleeding
Jeffery A. Baker, MD
Key Points
‘© Agaressive resuscitative measures (intravenous access,
crystalloid bolus, and blood products) are necessary in
unstable patients with gastrointestinal (G1) bleeding.
‘© A negative nasogastric lavage does nct completely
exclude an upper Gi bleed.
‘© Abrisk upper Gi bleed should be considered in the
differential of patients who present with hematochezia.
INTRODUCTION
Gastrointestinal (G1) bleeding accounts for 5% of admis-
sions from the emergency department (ED). An interven-
tion is required to stop ongoing hemorrhage in 10% of
patients. Bleeding can occur anywhere along the GI tract,
and can be grossly divided into upper and lower sources.
Upper GI bleeding is defined as occurring proximal to the
ligament of Treitz (the suspensory ligament of the duode-
‘num). Lower Gl bleeding is defined as occurring distal to
the ligament of Treitz. Upper GI bleeding is 4-8 times
‘more common than lower GI bleeding.
Itis not always possible to clinically distinguish between,
‘upper and lower GI bleeding in the ED, but appearance of
the gastric contentsand stool can provide cluesto the source
of the hemorrhage. Hematemesis is the vomiting of blood
and indicates an upper GI bleed. “Coffee ground” emesis
‘suggests that the blood has partially digested and that bleed-
ing is either slow or has stopped. A nasogastric (NG) tube
aspirate positive for blood also indicates an upper GI source
of bleeding. NG lavage can be negative in 25% of patients
with an upper GI source of bleeding because the nasogastric
tube does not reliably pass the pylorus.
‘Melena is black, tarry stool that reflects the presence
of blood in the GI tract for more than 8 hours. At least
‘© Octreotide should be administered in patients with
liver disease and significant upper Gl bleeding, even
when the diagnosis of esophageal varices has not been
‘confirmed
‘© Emergent endoscopy should be arranged when active
upper GI bleeding Is present.
300 mL of blood must be present to produce melena.
Melena is 4 times more likely to be from an upper GI
source of bleeding and almost always reflects bleeding
proximal to the right side of the colon, Hematochezia is,
bright red or maroon-colored blood per rectum. It is 6
times more likely to be from a lower GI source. An excep-
tion is a rapid upper GI source of bleeding Hematochezia,
is present in 10% of upper GI bleeds.
‘The three most common causts of upper GI bleeding
are peptic ulcer disease, gastritis, and varices (Table 30-1).
Lower GI bleeding may be due to multiple causes, but
Table 30-1. Causes of upper Gi bleeding.
cause Percentage
Peptic ulcer (duodenal 2/3) 40%
Frosve gastits 25%
‘Varices (esophageal and gastric) 20%
‘Mallory Weiss tear 5%
‘Other (epistans, aartoenerc stu, carcino, 10%
‘caustic ingestion)
128
GASTROINTESMNAL BUEED@CG Fe
Table 30-2. Causes of lower Gi bleeding.
(Cause Percentage
Divertiaulsis so
Inflammatory bowel disease 13%
‘Hemorthois, ana fissure 11%
Neoplasia ™
Coagulpathy *
‘terovenous mattcmation 3
diverticulosis is most common (Table 30-2). Less common
causes include pseudomembranous colitis, infectious diar-
rhea, aortoenteric fistula, radiation colitis, mesenteric
ischemia, and Meckel diverticulum.
CLINICAL PRESENTATION
> History
In most cases, patients will report hematemesis, coffee-
‘ground emesis, hematochezia, or melena. The duration
and frequency of these symptoms should be elicited. For
hematemesis, itis important to determine whether blood
was present initially or appeared after several episodes of
vomiting. The latter history suggests a Mallory-Weiss tear.
‘A history compatible with cirrhosis (chronic alcohol use,
hepatitis, IV drug use) suggests varices. These patients
may abo have a coagulopathy, making control of hemor-
rhage more difficult. When bleeding has been slow but
chronic, the patient may present with lightheadedness,
fatigue, chest pain, or shortness of breath owing to anemia
without any knowledge of GI bleeding, Patients with pep-
tic ulcer disease may report epigastric abdominal pain
related to cating. Agents that increase the risk of peptic
ulcer disease include nonsteroidal anti-inflammatory
drugs (NSAIDs), aspirin, and cigarettes. Elderly patients
with acute hemorrhage may initially present with syncope
ornear-syncope.
> Physical Examination
Vital signs should be obtained immediately. When abnor~
malities are present, treatment is frequently necessary
before obtaining 2 thorough history. Tachycardia and
hypotension indicate hypovolemic shock and require
immediate resuscitation. Cool, pale, and clammy skin is
evidence of anemia or shock. The abdomen should be
thoroughly examined, noting areas of tenderness or perito-
nitis. Rectal examination should be performed with
Hemoccult testing. The presence of hemorrhoids should
be documented. They may or may not be the source of
lower GI bleeding. Examination should also elicit any evi-
dence of the stigmata of cirthosis including ascites, spider
angioma, jaundice, or palmar erythema.
DIAGNOSTIC STUDIES
> Laboratory
Complete blood count, electrolytes, renal function, and
coagulation studies should be obtained. Itis important to
remember that a normal hemoglobin valve does not rule
out a massive acute hemorrhage. Compensatory hemodi-
lution may not occur for 2-3 hours. Blood bank should be
contacted for immediate type and screen. Blood products
should be ordered for patients with unstable vital signs oF
significant blood loss. Upper Gl bleeding may elevate
blood urea nitrogen because of the digestion and absorp-
tion of hemoglobin.
> Imaging
Upright chest x-ray is indicated in patients with suspicion
of perforation oraspiration. The presence of free air under
the diaphragm is diagnostic of perforation and is a surgical
emergency. Routine imaging otherwise offers little clinical
value in GI bleeding.
> Electrocardiogram
‘An electrocardiogram shouldbe obtained on patients with
risk factors for coronary artery disease, patient with known
heart disease, or patients with symptoms concerning for
coronary ischemia. Silent ischemia can occur asa result of
decreased oxygen delivery related to biood loss.
PROCEDURES
Nasogastric aspiration should be performed on patients
suspected of having an upper GI bleed. Aspirate appearing
like gross blood or “coffee grounds” is evidence of an upper
Gl source. The stomach may then be lavaged with 200-300 mL.
saline to see if the aspirate clears. Note that false negatives
‘may occur with bleeding distal to the pylorus, and false
positives may occur from nasal trauma. NG aspiration is,
an especially uncomfortable and anxiety-provoking proce-
dure for the patient, and the use of topical anesthetic is,
advised. Although NG aspiration in GI bleeding is rou-
tinely performed, it will only yield a useful diagnostic,
result in a minority of cases.
MEDICAL DECISION MAKING
‘The exact location of GI bleedingis usually not determined
in the initial ED evaluation. Examination of any emesis,
stocl, or NG aspirate mey help to determine the general
location of the hemorrhage and direct further diagnostic
and treatment strategies (Figure 30-1).
TREATMENT
Patients with active GI bleeding should be placed on a car-
diac monitor with supplemental oxygen. Large peripheral
TV catheters should be inserted in unstable patients. If these
130 CHAPTER 30
Suspected GI
bleeding
Hematemesis/
positive NG
aspirate
Hematochezia/
negative NG
aspirate
A Figure 30-1. GI bleeding diagnostic algorithm.
GI, gastrointestinal; NG, nasogastric.
lines cannot be inserted, a large-bore (8F) central line should
bbe placed to maximize volume resuscitation. IV fluid bolus
of 1-2 L of normal saline should be administered. If the
patient remains unstable after the fluid bolus, administra
tion of packed red blood cells (RBCs) is indicated. Uncross-
‘matched type O blood is ordered for patients with unstable
vital signs and significant blood loss. If ¢ coagulopathy is
suspected, fresh-frozen plasma is also ordered.
For upper GI bleeding, histamine? antagonists are fre-
‘quently administered, although they have not been shown to
eof any benefit inthe acute setting. Proton pump inhibitors
decrease the rate of re-bleeding, Pantoprazcle 80 mgIV bolus
followed by 5 ma/hr infusion is recommended. Octreotide is
beneficial in decreasing the rate of bleeding, the incidence of
rebleeding, and morality by decreasing portal hypertension.
It is particularly useful in variceal bleeding, but may also
reduce bleeding from nonvariceal sources. Administer a
'50-meg IV bolus followed by 50 meg/hr IV drip. Emergent
endoscopy is indicated for patients with fresh blood in the
ING aspirate and hematochecia from an upper Gl source.
Patients with liver disease also benefit from early endoscopic
intervention. Surgical intervention may be required in
patients with uncontrolled hemorrhage, perforation, or
patients with liver disease and portal hypertension.
In the setting of « suspected lower GI source of bleeding,
consult gastroenterology and surgical services early in unsta-
ble patients. Diagnostic and therapeutic options include
angiography, technetium-labeled RBC scan, colonoscopy, or
surgical intervention for partial colectomy. Angiography
allows for localization and arterial embolization, whereas a
technetium-labeled RBC scan localizes the bleeding site only.
In emergent cases, colonoscopy misses the diagnosis in 409%
‘of cases because of poor bowel preparation. When the siteof
bleeding is identified during colonoscopy, it mey allow for
therapeutic interventions to stop bleeding, but is unsuccess-
ful in 20%6 of cases. Surgical intervention is required in cases
‘of massive lower GI bleeding when other therapies fal
DISPOSITION
D> Admission
Upper GI bleed. Mest patients with an upper GI bleed
require admission. Admission to an intensive care unit,
(ICU) setting should be strongly considered for patients
with unstable vital signs, age >75 years, persistent bleeding
that does not clear with NG lavage, presence of coagulopa-
thy or severe anemia (hematocrit <20%), evidence of portal
hypertension, or unstable comorbid conditions.
‘Lower GI blesd. Most patients with lower GI bleeding
will require admission. ICU admission is appropriate for
unstable patients, Mortality is higher in elderly patients
‘with comorbidities, and these features should prompt con-
sideration for admission to an intensive care setting.
> Discharge
Upper GI bleed. Discharge with clos: follow-up can be
arranged for reliable patients who meet al of the following
criteria: age <65 years, no comorbidities including coagulopa-
thy, no significant liver disease, normal vital signs, negative
NG lavage and no melena, and a hemoglobin >10 gm/dL.
Recent clinical scoring systems (Glasgow-Blatchford bleeding,
score) may help predict which patients can be safely dis-
charged from the ED without endoscopy.
Lower GI bleed. Young stable patients with normal
hemoglobin, no active bleeding, evidence of hemorrhoids
fr fissures as a possible source, and no evidence of portal
hypertension, coagulopathy, or other significant comor-
bidities may be discharged with close follow-up.
BMetsis ss
Lo BM. Lower gastrointestinal bleeding. In: Tiatinalli JE,
‘Stapcrynski JS. Ma OJ, Cline DM, Cydulka RK. Mecklr GD.
Tintinalli's Emergency Medicine: A Comprehensive Study Guide,
‘TWh ed. New York, NY: McGraw-Hill, 2011, pp. 545-548.
Overton DT. Upper gastrointestinal bleeding. In: Tintnali JE,
‘Stapczynshi JS, Ma OJ, Cline DM, Cydulka RK, MecKler GD.
Tintinalli's Emergency Medicine: A’ Comprehersive Study Guide.
‘th ed. New York, NY: McGraw-Hill, 2011, pp. 543-545.
‘Stanley AJ, AshleyD, Dalton HR, et al- Ourpatient management
‘of patients with low-risk upper-gastrointestinal haemor-
thage Multicentre validation and prospective evaluation.
Lancet. 2009;373:42.
You might also like
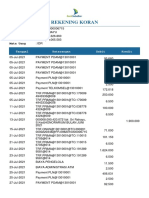
- Rekening Koran: No. Rekening Nama Nasabah Saldo Awal: Saldo Akhir: Mata UangDocument2 pagesRekening Koran: No. Rekening Nama Nasabah Saldo Awal: Saldo Akhir: Mata UangSry RahayuNo ratings yet
- Frequencies: Frequencies Variables Ony Ki /statistics Sum /order AnalysisDocument4 pagesFrequencies: Frequencies Variables Ony Ki /statistics Sum /order AnalysisSry RahayuNo ratings yet
- Rekening Koran: No. Rekening Nama Nasabah Saldo Awal: Saldo Akhir: Mata UangDocument1 pageRekening Koran: No. Rekening Nama Nasabah Saldo Awal: Saldo Akhir: Mata UangSry RahayuNo ratings yet
- Gambaran Radiologi Lesi Litik Pada Manus: Serial KasusDocument4 pagesGambaran Radiologi Lesi Litik Pada Manus: Serial KasusSry RahayuNo ratings yet
- Common Peroneal Nerve PalsyDocument3 pagesCommon Peroneal Nerve PalsySry RahayuNo ratings yet
- Jenis Jenis KontrasepsiDocument1 pageJenis Jenis KontrasepsiSry RahayuNo ratings yet
- BAB III Metode PenelitianDocument8 pagesBAB III Metode PenelitianSry RahayuNo ratings yet
- Jadwal Jaga Co-AsDocument2 pagesJadwal Jaga Co-AsSry RahayuNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)