Professional Documents
Culture Documents
Septic Shock
Uploaded by
yola_khairanisaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Septic Shock
Uploaded by
yola_khairanisaCopyright:
Available Formats
Septic Shock
Adam J. Schwarz, M.D. Assistant Professor of Pediatrics Medical Director, PICU University of Kansas Medical Center
I.
Definition:
Sepsis is a syndrome of systemic toxicity that results from the presence of infectious agents or their products in the blood. A patient may be bacteremic and not be septic. A bacteremic patient has circulating bacteria in the blood, and blood cultures may be positive, but if they do not have signs of systemic inflammation, than we do not technically say they are septic. It is estimated that everyone sustains some degree of bacteremia fairly frequently, such as after brushing our teeth. Thus we all are frequently bacteremic for a short period of time, but our body deals with the bacteria swiftly without an inflammatory cascade inducing a state of systemic toxicity. Sepsis, on the other hand, results from the bodys inflammatory response to components of infectious agents such as bacteria, viruses, or fungi, as well as to various toxins that these organisms may release. The Septic Inflammatory Response State, or SIRS, is the term used to describe the bodys response to the presence of infectious inducers of inflammation (Table 1). The body responds to the presence of these infectious agents or their products by releasing mediators of inflammation called cytokines. If the bodys inflammatory response is extremely profound, then the patient may present with the signs and symptoms we know of as overwhelming sepsis. Thus it is the bodys own response to these agents that results in the morbidity and mortality of sepsis. Table 1: Findings of the Systemic Inflammatory Response Syndrome
Table 1: Findings of the systemic Inflammatory Response Syndrome Tachypnea Tachycardia Fever or hypothermia (with evidence of infection) Hyperdynamic cardiac output in association with hypoperfusion CNS dysfunction Oliguria Metabolic acidosis Respiratory failure Renal failure Other organ system dysfunction
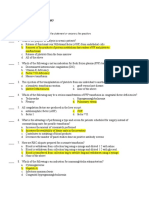
Table 2: Sepsis definitions 1. SIRS. 2 or more of the following: a) temperature >38.3C or<36C; b) tachycadia; c) tachypnea, d) WBC count >12,000/mm3 or < 4000/mm3 or >10% immature forms (bands). 2. Sepsis is defined as SIRS associated with suspected or confirmed infection. Positive blood cultures are not necessary. 3. Septic shock is cardiovascular collapse related to severe sepsis despite adequate fluid resuscitation. 4.far as specific causative agents go,hypoxemiavary with age and circumstance, and a detailed Organ dysfunction criteria are a) these will (PaO2/FiO2 ratio<300); b) acute As oliguria each organism (plt count<100,000, INR>1.5 or PTT>60s d) ileus e) discussion of c) coagulopathyis beyond the scope of this review. In short, however, any infectious agentHyperbilirubinemia that provokes a vigorous inflammatory response may induce sepsis. These may be gram (-) bacteria, such as the meningococcus or E. coli, or gram (+) organisms such as pneumococcus, Staph., group B strep (especially neonates), group A strep., etc These agents
61
release cellular components or toxins that stimulate the inflammatory host response. Gram (-) organisms, for example, have a cell wall that is composed of lipopolysaccharides (LPS), collectively called endotoxins, which are highly inflammatory. However, gram (+) organisms, which do not possess LPS (endotoxin) may also be extremely inflammatory and release other inducers of inflammation (such as peptidoglycans, teichoic acids, toxins such as toxic-shock stimulating toxin (TSST-1), etc) that can result in sepsis. In addition, viruses and fungi can also cause sepsis. As long as a vigorous inflammatory state results, we say that there is sepsis. If this inflammation gets out of control, the patient will be very sick and may even die. Mortality from different studies of sepsis across all ages varies from 10-80%, depending on the study, organisms, and enrollment criteria.
II.
Physiology of Sepsis
The SIRS can affect virtually any and all organ systems in the body.
A. Cardiovascular
The first major system we generally recognize as significantly affected by SIRS is the CV system. Sepsis leads to a decrease in tissue oxygen delivery. This is a critical concept, because sepsis MAY lead to INCREASED CARDIAC OUTPUT, or a clinical picture of BRISK CAPILLARY REFILL, WARM EXTREMITIES, and BOUNDING PULSES, and still be consistant with poor tissue oxygen delivery. The blood simply is not going where it is supposed to go. Thus a patient in septic shock may present with the clinical picture of cold extremities, weak pulses, and delayed capillary refill (cold shock), or they may have the
62
aforementioned brisk capillary refill and warm extremities with bounding pulses associated with overvigorous vasodilation (warm shock). The release of septic inflammatory mediators leads to the induction of the enzymes that synthesize nitric oxide (inducible nitric oxide synthase). Nitric oxide is a potent vasodilator. The result is inappropriate and often massive peripheral vasodilation. This reduces venous return to the heart (preload), as well as causing inappropriate distribution of blood flow to end-organs like the gut, the liver, the kidney, and the skin. Arterio-venous shunts that are normally closed may open that permit blood to bypass the capillaries and tissue beds, so the tissues never see oxygen-rich blood. In addition, the resulting vasodilation creates a much larger potential space for blood to run off into, reduces peripheral vascular resistance, and leads to a drop in diastolic blood pressure, a widened pulse pressure, or a fall on overall blood pressure. The heart will try to compensate by increasing cardiac output, leading to what is referred to as a hyperdynamic state. Heart rate is increased, afterload is reduced, and preload (leftventricular end-diastolic filling volume (LVEDV)) will also be reduced due to massive peripheral vasodilation. Cytokines can also directly depress myocardial contractility. Some authors refer to the presence of a myocardial depressant factor that is released in up to 50% of cases of septic shock, but we really arent sure what this MDF is. Speculation regarding TNF abounds, but it may be some other cytokine or combination of cytokines. Regardless of the cause, cardiac contractility can also be depressed during sepsis. The end result of all of these effects on the cardiovascular system is poor end-organ tissue oxygen delivery. The patient is tachycardic. He/she will have a widened pulse pressure (the difference between the systolic and diastolic blood pressure) and may be overall hypotensive. The signs of peripheral perfusion may be that of classic compensated shock, with cold extremities, weak pulses, and prolonged capillary refill secondary to the great drop in preload and relative intravascular volume as the patient is too vasodilated. However, the clinical picture of perfusion MAY be that of warm extremities with bounding pulses and brisk capillary refill if there is enough cardiac output to OVERPERFUSE the skin, while the rest of the body, other end-organs, and overall blood pressure is inadequate. The patient has a significant metabolic acidosis because of poor tissue oxygen delivery that makes the tissues metabolize anaerobically with the release of lactic acid. At the risk of foreshadowing the section on treatment of septic shock, hopefully it will be clear to you now that a patient in septic shock will need a lot of FLUID, and possibly inotropic support. Vigorous fluid resuscitation will fill the increased intravascular space created by NOinduced vasodilatation and improve preload. Inotropes will assist cardiac contractility (effect) and increase peripheral vascular resistance to increase central blood pressure (effect). Finally, poor cardiac perfusion and the need to stimulate contractility with inotropes, as well as possibly catheters that enter or traverse the right atrium, may precipitate the occurrence of cardiac arrhythmias.
B. Respiratory
A patient in septic shock will have a profound metabolic acidosis. In order to compensate and maintain a normal pH, the patient will attempt to hyperventilate in order to reduce the pCO2. This can take a lot of metabolic work to fuel the muscles of respiration, especially when the patient is poorly perfused to begin with. Normally we devote < 1% of our cardiac output and oxygen to breathe, but a patient in frank septic shock may consume up to 25-30% of their oxygen simply to fuel the muscles of respiration working hard to compensate for the profound metabolic lactic acidosis. It is therefore often very appropriate to intubate a patient in septic shock, even if their SaO2 is adequate with supplemental oxygen and their pCO2 is
63
actually low due to their tachypnea, in order to REDUCE THE METABOLIC WORK OF BREATHING. Let the ventilator do the work of breathing for the patient. In addition, many patients in septic shock develop ARDS and pulmonary edema. The necessary fluid resuscitation, coupled with the very real possibility that the alveolar-capillary membrane will be disrupted due to the inflammatory septic response, lead to pulmonary involvement and very often significant disease and respiratory failure. Thus, intubating early secures the airway and initiates control of the respiratory system. For ventilator management of respiratory failure and ARDS see those respective chapters and sections.
C. Infectious Disease
Obviously sepsis is, by definition, caused by the presence of some infectious agent. The presence of these infectious agents, or toxins produced by these organisms, are recognized by the body as a foreign invading substance and triggers a dynamic inflammatory response via the release of inflammatory mediators called cytokines. We therefore want to eliminate the source of the infection. Generally antibiotics are used to treat bacterial infections, which are the most common infectious class of organism. However, fungal infections would be treated by anti-fungal agents, and a few viral infections are treatable with certain specific antiviral agents. The important point to recognize, however, is that EVEN WITH TREATMENT WITH ANTIBIOTICS, the inflammatory pathways triggered by bacterial components may still be activated or augmented. In fact, it is possible that in some infections the act of suddenly killing all of the organisms with antibiotics may lead to massive release of bacterial byproducts and components that cause an increase in the septic inflammatory response state, resulting in acute and possibly irreversible decompensation of the patient and death.
D. Disseminated Intravascular Coagulation (D.I.C.)
DIC is a syndrome in which there is massive coagulation that occurs diffusely throughout the systemic circulatory system. As fibrin clots are deposited throughout the microvasculature, platelets are attracted, trapped, and damaged leading to thrombocytopenia. Red blood cells that pass through vessels laced with strands of fibrin or narrowed by coagulation are damaged and hemolyzed, leading to a microangiopathic hemolytic anemia. Coagulation factors are consumed, resulting in an increased PT and PTT. As the bodys compensatory fibrinolytic system frantically tries to keep up with the diffuse coagulation, fibrin is split into fragments (labeled X,Y,D, and E) collectively called fibrin degradation products (FDPs), which are themselves inhibitors of platelet aggregation. Thus DIC is a state of both rampant coagulation as well as fibrinolysis and inhibition of appropriate platelet function. The result is microvascular occlusion and tissue ischemia, as well as a bleeding diathesis resulting from the consumption of coagulation factors. Bleeding into the skin causes purpura. Poor perfusion to end-organs can result in skin mottling, cold or even black extremities, kidney failure, liver failure, CNS damage, gut injury, etc DIC results from the effect of microorganisms on the endothelial lining of blood vessels and components of the clotting cascade. For example, endotoxin can directly damage the vessel endothelial wall, exposing the very thrombogenic subendothelium and initiating the clotting cascade diffusely. Endotoxin can also directly activate factor XII, one of the initiators of coagulation, and it can bind a specific platelet receptor that furthers both thrombosis and platelet consumption. Other infectious agents can also trigger the coagulation cascade. SIRS associated shock from general cardiovascular compromise furthers microvascular ischemia and worsens DIC. Additionally, antigen-antibody complexes and the release of various inflammatory cytokines all can damage vascular endothelium, interfere with coagulation factors, decrease platelet function, and contribute to DIC. Laboratory findings generally reveal a prolonged PT and PTT in 50-75% of patients, but can be normal. Fibrinogen levels are usually depleted due to consumption, but the laboratory test
64
may count fibrinogen fragments in total fibrinogen levels and inaccurately report a normal level. Thrombocytopenia is common, as is increased FDP and D-dimer. FDP, however, may be increased in patients with liver dysfunction (since they are cleared by the liver) and not necessarily indicate DIC. Some patients will have fragmented RBCs on the peripheral smear (~50%), but the absence of schistocytes does not exclude the diagnosis. In short, an entire DIC profile needs to be interpreted in the patient known to be at risk for DIC. Evaluation of the PT, PTT, fibrinogen level, FDPs and D-dimer, CBC, and LFTs in association with the clinical condition of the patient should enable the diagnosis of DIC to be made. Finally, other clinical conditions can trigger DIC. These include any shock state, surgery, neonatal illness, obstetric accidents, head injury, and tumors.
E. Renal
Both shock and DIC affect the renal vasculature, reducing renal perfusion and causing tubule injury that results in both pre-renal and intrinsic renal failure, also know as acute tubular necrosis. This may lead to normovolemic, oliguric, or even anuric renal failure. Renal failure is defined by the inability to eliminate metabolic waste products and is indicated by the rise in BUN and creatine. So long as the patient maintains urine output, the potassium is generally adequately managed. In frank anuric renal failure hyperkalemia may complicate the clinical picture necessitating dialysis.
F. Gastrointestinal
The shock associated with sepsis, as well as with maldistribution of blood flow from microvascular occlusion with DIC or shunts leads to poor gut perfusion and ischemia. This may result in GI bleeding, gastritis, translocation of bacteria from within the gut to the bloodstream, and ileus.
G. CNS
Poor perfusion from shock can lead to CNS injury. The bleeding diathesis that results from DIC can lead to hemorrhagic stroke or localized infarction. In addition, the general septic state may result from or also be associated with meningitis that may result in localized infarcts, thrombosis, or hemorrhage
H. Endocrine
Severe cases of septic shock, notoriously meningococcemia, may result in infarction of the adrenal glands and a state of adrenal insufficiency. Controversy remains about the appropriate level of stress hormones such as cortisol in cases of severe sepsis.
III.
Treatment of Sepsis
A. Infectious Disease
Eliminate the source of infection. If there is a wound it may need to be drained. If there is another route of infection, such as a central line, that line should be removed and replaced. Antibiotics are the mainstay of therapy. If the organism is known along with its sensitivities, then antibiotics can be tailored to that bacteria or fungus. If the source of the sepsis remains unknown, than broad spectrum antibiotics are initiated. Antifungals may be needed if fungal infection is suspected or documented. Certain viruses might be treatable with antiviral therapy. Common broad spectrum antibiotics include third-generation cephalosporins such as cefotaxime, ceftriaxone, and ceftazidime. Imipenem or meropenem are sometimes used. Double-coverage for gram (-) organisms may be effected by adding gentamycin, and
65
occasionally broad-spectrum penicillins such as piperacillin or ticarcillin. Gram (+) organisms such as S. aureus, S. epidermidis, and PCN-resistant pneumococcus may be covered by vancomycin. Fungal sepsis should be treated with amphotericin. Viral sepsis with a member of the herpes family such as varicella or herpes can be treated with acyclovir. As noted above, simply killing the organism may not eliminate the problem once the septic inflammatory state has commenced The release of components of bacteria as they are killed may further stimulate the inflammatory septic reaction. A natural question would therefore be whether we could manipulate the bodys inflammatory response with anti-inflammatory agents such as steroids or specific anti-cytokine therapies such as anti-TNF antibodies or IL1 receptor antagonists etc The short answer to this important question is that, while animal studies of multiple anti-cytokine and anti-inflammatory agents have looked very promising, NO LARGE SCALE CONTROLLED TRIAL OF STEROIDS OR OTHER IMMUNOMODULATORY THERAPY IN HUMAN CLINICAL TRIALS HAS HAD A POSITIVE EFFECT ON RECOVERY AND SURVIVAL IN SEPSIS TO DATE. The same thing is true with respect to modulators of hypotension such as anti-N.O. agents. Thus we are left with simply attempting to eradicate the infection and its source, and support the disturbances in physiology that results from S.I.R.S.
B. Cardiovascular
The ability to adequately restore and provide oxygen delivery to the end-organ tissues is the critical goal in the treatment of sepsis. Recall that oxygen delivery is dependant upon cardiac output and arterial oxygen content. The formula for this is:
DO2 = CO x CaO2
Cardiac output is the product of heart rate (HR) and stroke volume (SV).
CO = HR x SV
Stroke volume is dependant upon LVEDV (preload), contractility, and afterload. Arterial oxygen content is dependant upon the amount of hemoglobin available for oxygen transport as well as by how much of that hemoglobin actually is saturated with oxygen (SaO2). Thus CaO2 is described by the formula:
CaO2 = (Hb x SaO2 x 1.34 ml O2/gm Hb) + (PaO2 x 0.0031)
Therefore, septic shock results, to a large extent, from disturbances in these variables that affect oxygen delivery. Since sepsis induces the production of N.O. resulting in massive vasodilation, both LVEDV (preload) and afterload are greatly reduced. Thus the patient in septic shock will need a lot of FLUID RESUSCITATION. Multiple 20cc/kg boluses of fluid, given as fast as possible, with reassessment of the patient at the end of the bolus and repeating as often as necessary, are required. For regular fluid boluses alone the initial fluid should be a crystalloid such as NS. It is tempting to give colloid boluses such as 5% albumin on the assumption that the colloid stays in the intravascular space better than crystalloid. However, there is often capillary leak that may result in the colloid leading out of the vessels into the tissue space. This may result in increasing tissue oncotic pressure, drawing fluid out of the intravascular space, and causing retention of such fluid in the extravascular space. Thus there should be a defensible reason why a colloid is chosen over crystalloid as a fluid bolus (significant hypoalbuminemia, for example). How much fluid to give or keep giving is often very difficult to determine. Unless the patient clearly improves and reverses the clinical state of shock immediately with fluid early on, it is often necessary to have an objective indicator of intravascular volume in order to help gauge the effectiveness of the fluid resuscitation. Patients in septic shock, should therefore have a central venous line with more than one lumen placed in order to administer the multiple fluid boluses and inotropes required, as well as to measure the pressure within the venous system returning to the heart in the form a CVP. Similar data can be obtained via a pulmonary artery
66
catheter (Swan-Ganz catheter) via measurement of the wedge pressure (PCWP). Typically a normal CVP measures 5-10 cm H2O. In the septic patient, fluid expansion to a generous CVP, generally > 12 cm H2O and often 15-18cm H2O, would suggest adequate expansion of intravascular volume. Similarly, if a PCWP is followed, fluid expansion to a wedge pressure of 18 cm H2O generally suggests appropriate fluid expansion. If the patient remains in shock once these parameters are met then further resuscitation is generally attempted by increasing inotropic support. The DO2 equation reveals how critical it is to avoid anemia and assure adequate oxygen carrying capacity. PRBCs should be administered in order to maintain the Hb above 10 (i.e. hematocrit >30). There is no data, however, that suggests that increasing the hemoglobin above 10-12 leads to any further increase in tissue oxygen utilization, and some concern that overtransfusion might increase blood viscosity that ultimately reduces oxygen delivery at hematocrits above 40. Arrhythmias are treated by either correcting any underlying cause of cardiac irritability such as catheter placement or reducing (if possible) IV inotrope dosages. Otherwise lidocaine can be used. Starting doses are a loading dose of 1-2 mg/kg followed by an infusion at a rate of 10-50 g/kg/min. Lidocaine, however, is a myocardial depressant so the lowest effective rate should be used. Since sepsis causes inappropriate peripheral vasodilation as well as depressing myocardial contractility, inotropes are generally required. There are several inotropic agents that may be useful in the treatment of septic shock. A detailed discussion of each of these may be found in the chapter on inotropes. Inotropes can both increase myocardial contractility and have variable effects on peripheral vascular resistance. Some inotropes are potent vasoconstrictors (i.e. epinephrine, norepinephrine), whereas others are mild (dobutamine) or potent (milrinone) vasodilators. Which inotropic combinations will be effective depends upon the clinical volume and contractile state of the patients cardiac system. For instance, increasing peripheral vasoconstriction in order to raise central blood pressure might result in furthering microvascular ischemia. However, if the patient has refractory hypotension and cannot even maintain the central blood pressure that perfuses the heart and the brain, the patient will not ultimately survive neurologically intact anyway. Thus, sometimes the risk of compromising end-organ perfusion must be assumed in order to restore perfusion to the most critical organs first, the brain and the heart, and accept and treat the consequences of renal, hepatic, skin ischemia, etc. later. Dopamine is often used in patients with septic shock, either alone or in combination with other inotropes. Dopamine is generally useful for its mixed effect on end-organ perfusion such as renal and splanchnic vasculature at low doses (2-5 g/kg/min). At intermediate doses the -1 effect assists myocardial contractility, and at higher doses the -effect may increase peripheral vasoconstriction and central blood pressure. Epinephrine is often considered the mainstay of inotropic support in the pediatric patient with septic shock. Epinephrine stimulates both - and - receptors so that there is both increased myocardial contractility and increased peripheral vasoconstriction. The peripheral vasoconstriction brings blood back into the central circulation but at the expense of peripheral end-organ perfusion. At high enough doses extremities will become severely ischemic and even turn dark and ultimately necrotic. Doses typically begin at 0.1 g/kg/min and are titrated up to effect and side-effects. In severe cases patients may be on doses of 2-3 g/kg/min or even higher. Dobutamine is almost a pure inotrope, with primarily 1 effects which effect cardiac contractility, and a little bit of 2 mediated peripheral vasodilation which might improve tissue
67
perfusion. There is no -effect. Typical doses begin at 5 g/kg/min and are increased generally to 20 g/kg/min. Norepinephrine (Levophed) is predominantly an -agonist that results in increased peripheral vasoconstriction and thus increase peripheral vascular resistance. Its role is as a pressor agent to increase blood pressure in the face of shock that persists after adequate fluid replacement. Some practitioners will provide the -effect with norepinephrine and inotropic effect with dobutamine. Others will rely on epinephrine. Typical doses of norepinephrine are similar to epinephrine and begin at 0.1 g/kg/min and are titrated upward to effect and side-effects. Milrinone is a phosphodiesterase inhibitor that works via a different mechanism than the catecholamines. It results in an increase in intracellular cAMP levels that results in increased cardiac inotropy as well as potent peripheral vasodilation. It may be useful in the treatment of shock in patients who have adequate intravascular volume but need increased cardiac contractility and better peripheral perfusion.
C. Respiratory
See respective chapters on mechanical ventilation and ARDS (if present).
D. DIC
The therapy for DIC in sepsis is very controversial. On the one hand there is consumption of the factors of coagulation, leading to a prolonged PT and PTT and consumption of platelets and fibrinogen which predisposes the patient to bleeding. Clinically this can be treated with FFP (clotting factors), platelets, and cryoprecipitate (fibrinogen). However, rampant coagulation in the microvasculature is what causes end-organ tissue ischemia. Adding more of the components of coagulation may be like adding fuel to the fire, worsening the maldistribution of tissue perfusion, and adversely affecting outcome. Thus it is generally agreed that, with ACTIVE BLEEDING, platelets, FFP, and cryoprecipitate should be given. Without active bleeding we may be hesitant to give these therapies despite a prolonged INR, PT, PTT, and low platelets and fibrinogen. Some clinicians advocate giving heparin therapy, or low-molecular weight heparin to slow down the coagulopathy. There are no studies to support demonstrate efficacy of heparin therapy. Similarly, there are some investigators looking at the use of antithrombin III (ATIII), which can be quite variable and low in sepsis. ATIII is an inhibitor of the coagulation cascade at many levels. However, despite some early suggestion in limited trials that it may have some use in treating DIC, there have been NO PLACEBO CONTROLLED TRIALS of ATIII replacement therapy that demonstrate a statistically significant improvement on outcome in adults or children in septic shock and DIC.
E. Endocrine
As mentioned above, there is some question whether patients in severe septic shock or pupura fulminans have adequate levels of circulating glucocorticoids to support their physiology when so severely stressed. Some clinicians might give a dose of 50-100 mg/m2/day of hydrocortisone and draw a serum cortisol level. If low than they might continue with replacement doses. Recently, a study of adult patients with septic shock who had survived 48 hours and were inotropic dependant showed some benefit when treated with supraphysiologic doses of hydrocortisone compared with controls(CCM 1998, 26(4) 645650). Treatment patients received 100 mg hydrocortisone IV tid for five days compared with placebo controls. At the end of 7 days, 68% of the steroid group had reversal of shock compared with 21% of controls, a difference of 47% (p<0.007). In addition, mortality was
68
only 32% in the steroid group compared with 65% in the controls (NS). Thus there may yet be a role for the selected use of glucocorticoids in the treatment of certain patients with septic shock.
F. Gastrointestinal
Gastritis or peptic ulceration should be prevented with the use of H-2 blockers such as ranitidine or pepcid, or coating the gastic mucosa with sucralfate. Nutrition may need to be supported with adequate TPN.
G. Renal
Renal support by reversing shock and restoring perfusion to the kidneys will hopefully prevent frank anuric renal failure. Improving perfusion via the use of dopaminergic doses of low-dose dopamine (0.5-4 g/kg/min) may improve renal blood flow and maintain diuresis. It is controversial whether the use of such therapy actually staves off or reverses renal failure. However, dopamine may convert anuric or severely oliguric renal failure to oliguric or normovolemic renal failure, allow maintainance of potassium homeostasis, and permit more effective diuresis.
69
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Disseminated Intravascular Coagulopathy Disseminated Intravascular Coagulation (DIC) Is A PathologicalDocument6 pagesDisseminated Intravascular Coagulopathy Disseminated Intravascular Coagulation (DIC) Is A PathologicalValarmathiNo ratings yet
- 4 Circulation Disorders PDFDocument69 pages4 Circulation Disorders PDFSetiawan SukmadjaNo ratings yet
- Bacterial Contamination in Blood Transfusion - Factors, PathogenesisDocument4 pagesBacterial Contamination in Blood Transfusion - Factors, PathogenesisjunaidiabdhalimNo ratings yet
- Disseminated Intravascular Coagulation - Background, Pathophysiology, EtiologyDocument11 pagesDisseminated Intravascular Coagulation - Background, Pathophysiology, Etiologyevi100% (2)
- Case DigestDocument301 pagesCase DigestChesca AsisNo ratings yet
- Nycocard Brochure 01 PDFDocument2 pagesNycocard Brochure 01 PDFelfarik sulistonNo ratings yet
- Acute Lymphocytic LeukemiaDocument8 pagesAcute Lymphocytic LeukemiaWendy EscalanteNo ratings yet
- College of Physicians and Surgeons of Ontario and Dr. YazdanfarDocument377 pagesCollege of Physicians and Surgeons of Ontario and Dr. YazdanfarOmar Ha-Redeye100% (1)
- Rash BookDocument12 pagesRash BookPhoebe UsmleNo ratings yet
- Chapter 44: Nursing Care of The Client With An Hematologic DisordersDocument18 pagesChapter 44: Nursing Care of The Client With An Hematologic DisordersfLOR_ZIANE_MAENo ratings yet
- Hematology & OncologyDocument94 pagesHematology & OncologyDaNy Chiriac100% (1)
- Disseminated Intravascular Coagulation: Keith Lewis, MDDocument37 pagesDisseminated Intravascular Coagulation: Keith Lewis, MDRitamaria100% (1)
- Pathology LMRP 2019Document52 pagesPathology LMRP 2019skNo ratings yet
- Unit 6 Flash Cards Hematology CoagulationDocument13 pagesUnit 6 Flash Cards Hematology CoagulationLois LipanovichNo ratings yet
- Diagnostic and Therapeutic Abdominal ParacentesisDocument16 pagesDiagnostic and Therapeutic Abdominal ParacentesisGonzalo Rubio RiquelmeNo ratings yet
- Maternal Child Nursing Care Perry Hockenberry Lowdermilk 5th Edition Test BankDocument20 pagesMaternal Child Nursing Care Perry Hockenberry Lowdermilk 5th Edition Test BankKristinSummersmwyr100% (32)
- Preeclampsia Risk Factors and Maternal-Fetal ComplicationsDocument18 pagesPreeclampsia Risk Factors and Maternal-Fetal ComplicationsMary BlancoNo ratings yet
- Transfusion TherapyDocument14 pagesTransfusion TherapyCMLNo ratings yet
- Hypothermia Alcohol Related IllnessDocument42 pagesHypothermia Alcohol Related IllnessSritharan GaneshamoorthyNo ratings yet
- HomicideDocument22 pagesHomicideniraj_sdNo ratings yet
- Review of Amniotic Fluid Embolism PathophysiologyDocument7 pagesReview of Amniotic Fluid Embolism PathophysiologyKinjal VasavaNo ratings yet
- 75-Practice Questions-Staff-Nurse Gov ExamDocument4 pages75-Practice Questions-Staff-Nurse Gov ExamPrakashNo ratings yet
- Ob RVG Panda ManilaDocument45 pagesOb RVG Panda ManilaMikaelle GasparNo ratings yet
- Coagulation Problems PPTDocument69 pagesCoagulation Problems PPTBao NguyenNo ratings yet
- Peds HemeImmune OUTLINEDocument10 pagesPeds HemeImmune OUTLINEAshleyNo ratings yet
- Jay ObDocument6 pagesJay ObJenxNo ratings yet
- Hematology: AnemiaDocument46 pagesHematology: AnemiaCyrus100% (1)
- Anticoagulants, Fibrinolytics, AntiplateletsDocument88 pagesAnticoagulants, Fibrinolytics, Antiplateletspmuawiyah25No ratings yet
- IM Shelf - AmbossDocument61 pagesIM Shelf - AmbossHaadi AliNo ratings yet
- Guidelines For The Use of Fresh-Frozen Plasma, CryoprecipitateDocument18 pagesGuidelines For The Use of Fresh-Frozen Plasma, CryoprecipitatemelaniefarahdillaNo ratings yet