Professional Documents
Culture Documents
PEDIA Nursing NCLEX Bullets Part 1
Uploaded by
Russel Myron Adriano AdvinculaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PEDIA Nursing NCLEX Bullets Part 1
Uploaded by
Russel Myron Adriano AdvinculaCopyright:
Available Formats
PEDIA Nursing NCLEX Bullets Part 1
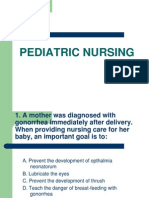
A child with HIV-positive blood should receive inactivated poliovirus vaccine (IPV) rather than oral poliovirus vaccine (OPV) immunization. To achieve postural drainage in an infant, place a pillow on the nurses lap and lay the infant across it. A child with cystic fibrosis should eat more calories, protein, vitamins, and minerals than a child without the disease. Infants subsisting on cows milk only dont receive a sufficient amount of iron (ferrous sulfate), which will eventually result in iron deficiency anemia. A child with an undiagnosed infection should be placed in isolation. An infant usually triples his birth weight by the end of his first year. Clinical signs of a dehydrated infant include lethargy, irritability, dry skin decreased tearing, decreased urinary output, and increased pulse. Appropriate care of a child with meningitis includes frequent assessment of neurologic signs (such as decreasing levels of consciousness, difficulty to arouse) and measuring the circumference of the head because subdural effusions and obstructive hydrocephalus can develop. Expected clinical findings in a newborn with cerebral palsy include reflexive hypertonicity and criss-crossing or scissoring leg movements. Papules, vesicles, and crust are all present at the same time in the early phase of chickenpox. Topical corticosteroids shouldnt be used on chickenpox lesions. A serving size of a food is usually 1 tablespoon for each year of age. The characteristic of fifth disease (erythema infectiosum) is erythema on the face, primarily the cheeks, giving a slapped face appearance. Adolescents may brave pain, especially in front of peers. Therefore, offer analgesics if pain is suspected or administer the medication if the client asks for it. Signs that a child with cystic fibrosis is responding to pancreatic enzymes are the absence of steatorrhea, improved appetite, and absence of abdominal pain. Roseola appears as discrete rose-pink macules that first appear on the trunk and that fade when pressure is applied. A ninety degree-ninety degree traction is used for fracture of a childs femur or tibia. One sign of developmental dysplasia is limping during ambulation. Circumcision wouldnt be performed on a male child with hypospadias because the foreskin may be needed during surgical reconstruction. Neonatal abstinence syndrome is manifested in central nervous system hyperirritability (for example, hyperactive Moro reflex) and gastrointestinal symptoms (watery stools). Classic signs of shaken baby syndrome are seizures, slow apical pulse difficulty breathing, and retinal hemorrhage. An infant born to an HIV-positive mother will usually receive AZT (zidovudine) for the first 6 weeks of life. Infants born to an HIV-positive mother should receive all immunizations of schedule. Blood pressure in the arms and legs is essentially the same in infants. When bottle-feeding a newborn with a cleft palate, hold the infants head in an upright position. Because of circulating maternal antibodies that will decrease the immune response, the measles, mumps, and rubella (MMR) vaccine shouldnt be given until the infant has reached 1 year of age. Before feeding an infant any fluid that has been warmed, test a drop of the liquid on your own skin to prevent burning the infant. A newborn typically wets 6 to 10 diapers per day. Although microwaving food and fluids isnt recommend for infants, its commonplace in the United States. Therefore the family should be toughs to test the temperature of the food or fluid against their own skin before allowing it to be consumed by the infant. The most adequate diet for an infant in the first 6 months of life is breast milk. An infant can usually chew food by 7 months, hold spoon by 9 month, and drink fluid from a cup by 1 year of age. Choking from mechanical obstruction is the leading cause of death (by suffocation) for infants younger than 1 year of age. Failure to thrive is a term used to describe an infant who falls below the fifth percentile for weight and height on a standard measurement chart. Developmental theories include Havighursts age periods and developmental tasks; Freuds five stages of development; Kohlbergs stages of moral development; Eriksons eight stages of development; and Piagets phases of cognitive development. The primary concern with infusing large volumes of fluid is circulatory overload. This is especially true in children and infants, and in clients with renal disease. Certain hazards present increased risk of harm to children and occur more often at different ages. For infants, more falls, burns, and suffocation occur; for toddlers, there are more burns, poisoning, and drowning for preschoolers, more playground equipment
accidents, choking, poisoning, and drowning; and for adolescents, more automobile accidents, drowning, fires, and firearm accidents.
A child in Bryants traction whos younger than age 3 or weighs less than 30 lb (13.6 kg) should have the buttocks slightly elevated and clear or the bed. The knees should be slightly flexed, and the legs should be extended at a right angle to the body. The body provides the traction mechanism. In an infant, a bulging fontanel is the most significant sign of increasing intracranial pressure.
NCLEX and Nursing Board Exam Maternal and Child Nursing Bullets
Unlike false labor, true labor produces regular rhythmic contractions, abdominal discomfort, progressive descent of the fetus, bloody show, and progressive effacement and dilation of the cervix. To help a mother break the suction of her breast-feeding infant, the nurse should teach her to insert a finger at the corner of the infants mouth. Administering high levels of oxygen to a premature neonate can cause blindness as a result of retrolental fibroplasia. Amniotomy is artificial rupture of the amniotic membranes. During pregnancy, weight gain averages 25 to 30 lb (11 to 13.5 kg). Rubella has a teratogenic effect on the fetus during the first trimester. It produces abnormalities in up to 40% of cases without interrupting the pregnancy. Immunity to rubella can be measured by a hemagglutination inhibition test (rubella titer). This test identifies exposure to rubella infection and determines susceptibility in pregnant women. In a woman, a titer greater than 1:8 indicates immunity. When used to describe the degree of fetal descent during labor, floating means the presenting part isnt engaged in the pelvic inlet, but is freely movable (ballotable) above the pelvic inlet. When used to describe the degree of fetal descent, engagement means when the largest diameter of the presenting part has passed through the pelvic inlet. Fetal station indicates the location of the presenting part in relation to the ischial spine. Its described as 1, 2, 3, 4, or 5 to indicate the number of centimeters above the level of the ischial spine; station 5 is at the pelvic inlet. Fetal station also is described as +1, +2, +3, +4, or +5 to indicate the number of centimeters it is below the level of the ischial spine; station 0 is at the level of the ischial spine. During the first stage of labor, the side-lying position usually provides the greatest degree of comfort, although the patient may assume any comfortable position. During delivery, if the umbilical cord cant be loosened and slipped from around the neonates neck, it should be clamped with two clamps and cut between the clamps. An Apgar score of 7 to 10 indicates no immediate distress, 4 to 6 indicates moderate distress, and 0 to 3 indicates severe distress. To elicit Moros reflex, the nurse holds the neonate in both hands and suddenly, but gently, drops the neonates head backward. Normally, the neonate abducts and extends all extremities bilaterally and symmetrically, forms a C shape with the thumb and forefinger, and first adducts and then flexes the extremities. Pregnancy-induced hypertension (preeclampsia) is an increase in blood pressure of 30/15 mm Hg over baseline or blood pressure of 140/95 mm Hg on two occasions at least 6 hours apart accompanied by edema and albuminuria after 20 weeks gestation. Positive signs of pregnancy include ultrasound evidence, fetal heart tones, and fetal movement felt by the examiner (not usually present until 4 months gestation Goodells sign is softening of the cervix. Quickening, a presumptive sign of pregnancy, occurs between 16 and 19 weeks gestation. Ovulation ceases during pregnancy. Any vaginal bleeding during pregnancy should be considered a complication until proven otherwise. To estimate the date of delivery using Ngeles rule, the nurse counts backward 3 months from the first day of the last menstrual period and then adds 7 days to this date. At 12 weeks gestation, the fundus should be at the top of the symphysis pubis. Cows milk shouldnt be given to infants younger than age 1 because it has a low linoleic acid content and its protein is difficult for infants to digest. If jaundice is suspected in a neonate, the nurse should examine the infant under natural window light. If natural light is unavailable, the nurse should examine the infant under a white light. The three phases of a uterine contraction are increment, acme, and decrement.
The intensity of a labor contraction can be assessed by the indentability of the uterine wall at the contractions peak. Intensity is graded as mild (uterine muscle is somewhat tense), moderate (uterine muscle is moderately tense), or strong (uterine muscle is boardlike). Chloasma, the mask of pregnancy, is pigmentation of a circumscribed area of skin (usually over the bridge of the nose and cheeks) that occurs in some pregnant women. The gynecoid pelvis is most ideal for delivery. Other types include platypelloid (flat), anthropoid (apelike), and android (malelike). Pregnant women should be advised that there is no safe level of alcohol intake. The frequency of uterine contractions, which is measured in minutes, is the time from the beginning of one contraction to the beginning of the next. Vitamin K is administered to neonates to prevent hemorrhagic disorders because a neonates intestine cant synthesize vitamin K. Before internal fetal monitoring can be performed, a pregnant patients cervix must be dilated at least 2 cm, the amniotic membranes must be ruptured, and the fetuss presenting part (scalp or buttocks) must be at station 1 or lower, so that a small electrode can be attached. Fetal alcohol syndrome presents in the first 24 hours after birth and produces lethargy, seizures, poor sucking reflex, abdominal distention, and respiratory difficulty. Variability is any change in the fetal heart rate (FHR) from its normal rate of 120 to 160 beats/minute. Acceleration is increased FHR; deceleration is decreased FHR. In a neonate, the symptoms of heroin withdrawal may begin several hours to 4 days after birth. In a neonate, the symptoms of methadone withdrawal may begin 7 days to several weeks after birth. In a neonate, the cardinal signs of narcotic withdrawal include coarse, flapping tremors; sleepiness; restlessness; prolonged, persistent, high-pitched cry; and irritability. The nurse should count a neonates respirations for 1 full minute. Chlorpromazine (Thorazine) is used to treat neonates who are addicted to narcotics. The nurse should provide a dark, quiet environment for a neonate who is experiencing narcotic withdrawal. In a premature neonate, signs of respiratory distress include nostril flaring, substernal retractions, and inspiratory grunting. Respiratory distress syndrome (hyaline membrane disease) develops in premature infants because their pulmonary alveoli lack surfactant. Whenever an infant is being put down to sleep, the parent or caregiver should position the infant on the back. (Remember back to sleep.) The male sperm contributes an X or a Y chromosome; the female ovum contributes an X chromosome. Fertilization produces a total of 46 chromosomes, including an XY combination (male) or an XX combination (female). The percentage of water in a neonates body is about 78% to 80%. To perform nasotracheal suctioning in an infant, the nurse positions the infant with his neck slightly hyperextended in a sniffing position, with his chin up and his head tilted back slightly. Organogenesis occurs during the first trimester of pregnancy, specifically, days 14 to 56 of gestation. After birth, the neonates umbilical cord is tied 1" (2.5 cm) from the abdominal wall with a cotton cord, plastic clamp, or rubber band. Gravida is the number of pregnancies a woman has had, regardless of outcome. Para is the number of pregnancies that reached viability, regardless of whether the fetus was delivered alive or stillborn. A fetus is considered viable at 20 weeks gestation. An ectopic pregnancy is one that implants abnormally, outside the uterus. The first stage of labor begins with the onset of labor and ends with full cervical dilation at 10 cm. The second stage of labor begins with full cervical dilation and ends with the neonates birth. The third stage of labor begins after the neonates birth and ends with expulsion of the placenta. In a full-term neonate, skin creases appear over two-thirds of the neonates feet. Preterm neonates have heel creases that cover less than two-thirds of the feet. The fourth stage of labor (postpartum stabilization) lasts up to 4 hours after the placenta is delivered. This time is needed to stabilize the mothers physical and emotional state after the stress of childbirth. At 20 weeks gestation, the fundus is at the level of the umbilicus. At 36 weeks gestation, the fundus is at the lower border of the rib cage. A premature neonate is one born before the end of the 37th week of gestation. Pregnancy-induced hypertension is a leading cause of maternal death in the United States. A habitual aborter is a woman who has had three or more consecutive spontaneous abortions. Threatened abortion occurs when bleeding is present without cervical dilation. A complete abortion occurs when all products of conception are expelled.
Hydramnios (polyhydramnios) is excessive amniotic fluid (more than 2,000 ml in the third trimester). Stress, dehydration, and fatigue may reduce a breast-feeding mothers milk supply. During the transition phase of the first stage of labor, the cervix is dilated 8 to 10 cm and contractions usually occur 2 to 3 minutes apart and last for 60 seconds. A nonstress test is considered nonreactive (positive) if fewer than two fetal heart rate accelerations of at least 15 beats/minute occur in 20 minutes. A nonstress test is considered reactive (negative) if two or more fetal heart rate accelerations of 15 beats/minute above baseline occur in 20 minutes. A nonstress test is usually performed to assess fetal well-being in a pregnant patient with a prolonged pregnancy (42 weeks or more), diabetes, a history of poor pregnancy outcomes, or pregnancy-induced hypertension. A pregnant woman should drink at least eight 8-oz glasses (about 2,000 ml) of water daily. When both breasts are used for breast-feeding, the infant usually doesnt empty the second breast. Therefore, the second breast should be used first at the next feeding. A low-birth-weight neonate weighs 2,500 g (5 lb 8 oz) or less at birth. A very-low-birth-weight neonate weighs 1,500 g (3 lb 5 oz) or less at birth. When teaching parents to provide umbilical cord care, the nurse should teach them to clean the umbilical area with a cotton ball saturated with alcohol after every diaper change to prevent infection and promote drying. Teenage mothers are more likely to have low-birth-weight neonates because they seek prenatal care late in pregnancy (as a result of denial) and are more likely than older mothers to have nutritional deficiencies. Linea nigra, a dark line that extends from the umbilicus to the mons pubis, commonly appears during pregnancy and disappears after pregnancy. Implantation in the uterus occurs 6 to 10 days after ovum fertilization. Placenta previa is abnormally low implantation of the placenta so that it encroaches on or covers the cervical os. In complete (total) placenta previa, the placenta completely covers the cervical os. In partial (incomplete or marginal) placenta previa, the placenta covers only a portion of the cervical os. Abruptio placentae is premature separation of a normally implanted placenta. It may be partial or complete, and usually causes abdominal pain, vaginal bleeding, and a boardlike abdomen. Cutis marmorata is mottling or purple discoloration of the skin. Its a transient vasomotor response that occurs primarily in the arms and legs of infants who are exposed to cold. The classic triad of symptoms of preeclampsia are hypertension, edema, and proteinuria. Additional symptoms of severe preeclampsia include hyperreflexia, cerebral and vision disturbances, and epigastric pain. Ortolanis sign (an audible click or palpable jerk that occurs with thigh abduction) confirms congenital hip dislocation in a neonate. The first immunization for a neonate is the hepatitis B vaccine, which is administered in the nursery shortly after birth. If a patient misses a menstrual period while taking an oral contraceptive exactly as prescribed, she should continue taking the contraceptive. If a patient misses two consecutive menstrual periods while taking an oral contraceptive, she should discontinue the contraceptive and take a pregnancy test. If a patient who is taking an oral contraceptive misses a dose, she should take the pill as soon as she remembers or take two at the next scheduled interval and continue with the normal schedule. If a patient who is taking an oral contraceptive misses two consecutive doses, she should double the dose for 2 days and then resume her normal schedule. She also should use an additional birth control method for 1 week. Eclampsia is the occurrence of seizures that arent caused by a cerebral disorder in a patient who has pregnancy-induced hypertension. In placenta previa, bleeding is painless and seldom fatal on the first occasion, but it becomes heavier with each subsequent episode. Treatment for abruptio placentae is usually immediate cesarean delivery. Drugs used to treat withdrawal symptoms in neonates include phenobarbital (Luminal), camphorated opium tincture (paregoric), and diazepam (Valium). Infants with Down syndrome typically have marked hypotonia, floppiness, slanted eyes, excess skin on the back of the neck, flattened bridge of the nose, flat facial features, spadelike hands, short and broad feet, small male genitalia, absence of Moros reflex, and a simian crease on the hands. The failure rate of a contraceptive is determined by the experience of 100 women for 1 year. Its expressed as pregnancies per 100 woman-years. The narrowest diameter of the pelvic inlet is the anteroposterior (diagonal conjugate). The chorion is the outermost extraembryonic membrane that gives rise to the placenta. The corpus luteum secretes large quantities of progesterone. From the 8th week of gestation through delivery, the developing cells are known as a fetus. In an incomplete abortion, the fetus is expelled, but parts of the placenta and membrane remain in the uterus.
The circumference of a neonates head is normally 2 to 3 cm greater than the circumference of the chest. After administering magnesium sulfate to a pregnant patient for hypertension or preterm labor, the nurse should monitor the respiratory rate and deep tendon reflexes. During the first hour after birth (the period of reactivity), the neonate is alert and awake. When a pregnant patient has undiagnosed vaginal bleeding, vaginal examination should be avoided until ultrasonography rules out placenta previa. After delivery, the first nursing action is to establish the neonates airway. Nursing interventions for a patient with placenta previa include positioning the patient on her left side for maximum fetal perfusion, monitoring fetal heart tones, and administering I.V. fluids and oxygen, as ordered. The specific gravity of a neonates urine is 1.003 to 1.030. A lower specific gravity suggests overhydration; a higher one suggests dehydration. The neonatal period extends from birth to day 28. Its also called the first 4 weeks or first month of life. A woman who is breast-feeding should rub a mild emollient cream or a few drops of breast milk (or colostrum) on the nipples after each feeding. She should let the breasts air-dry to prevent them from cracking. Breast-feeding mothers should increase their fluid intake to 2 to 3 qt (2,500 to 3,000 ml) daily. After feeding an infant with a cleft lip or palate, the nurse should rinse the infants mouth with sterile water. The nurse instills erythromycin in a neonates eyes primarily to prevent blindness caused by gonorrhea or chlamydia. Human immunodeficiency virus (HIV) has been cultured in breast milk and can be transmitted by an HIV-positive mother who breast-feeds her infant. A fever in the first 24 hours postpartum is most likely caused by dehydration rather than infection. Preterm neonates or neonates who cant maintain a skin temperature of at least 97.6 F (36.4 C) should receive care in an incubator (Isolette) or a radiant warmer. In a radiant warmer, a heat-sensitive probe taped to the neonates skin activates the heater unit automatically to maintain the desired temperature. During labor, the resting phase between contractions is at least 30 seconds. Lochia rubra is the vaginal discharge of almost pure blood that occurs during the first few days after childbirth. Lochia serosa is the serous vaginal discharge that occurs 4 to 7 days after childbirth. Lochia alba is the vaginal discharge of decreased blood and increased leukocytes thats the final stage of lochia. It occurs 7 to 10 days after childbirth. Colostrum, the precursor of milk, is the first secretion from the breasts after delivery. The length of the uterus increases from 2" (6.3 cm) before pregnancy to 12" (32 cm) at term. To estimate the true conjugate (the smallest inlet measurement of the pelvis), deduct 1.5 cm from the diagonal conjugate (usually 12 cm). A true conjugate of 10.5 cm enables the fetal head (usually 10 cm) to pass. The smallest outlet measurement of the pelvis is the intertuberous diameter, which is the transverse diameter between the ischial tuberosities. Electronic fetal monitoring is used to assess fetal well-being during labor. If compromised fetal status is suspected, fetal blood pH may be evaluated by obtaining a scalp sample. In an emergency delivery, enough pressure should be applied to the emerging fetuss head to guide the descent and prevent a rapid change in pressure within the molded fetal skull. After delivery, a multiparous woman is more susceptible to bleeding than a primiparous woman because her uterine muscles may be overstretched and may not contract efficiently. Neonates who are delivered by cesarean birth have a higher incidence of respiratory distress syndrome. The nurse should suggest ambulation to a postpartum patient who has gas pain and flatulence. Massaging the uterus helps to stimulate contractions after the placenta is delivered. When providing phototherapy to a neonate, the nurse should cover the neonates eyes and genital area. The narcotic antagonist naloxone (Narcan) may be given to a neonate to correct respiratory depression caused by narcotic administration to the mother during labor. In a neonate, symptoms of respiratory distress syndrome include expiratory grunting or whining, sandpaper breath sounds, and seesaw retractions. Cerebral palsy presents as asymmetrical movement, irritability, and excessive, feeble crying in a long, thin infant. The nurse should assess a breech-birth neonate for hydrocephalus, hematomas, fractures, and other anomalies caused by birth trauma. When a patient is admitted to the unit in active labor, the nurses first action is to listen for fetal heart tones. In a neonate, long, brittle fingernails are a sign of postmaturity. Desquamation (skin peeling) is common in postmature neonates. A mother should allow her infant to breast-feed until the infant is satisfied. The time may vary from 5 to 20 minutes. Nitrazine paper is used to test the pH of vaginal discharge to determine the presence of amniotic fluid.
A pregnant patient normally gains 2 to 5 lb (1 to 2.5 kg) during the first trimester and slightly less than 1 lb (0.5 kg) per week during the last two trimesters. Neonatal jaundice in the first 24 hours after birth is known as pathological jaundice and is a sign of erythroblastosis fetalis. A classic difference between abruptio placentae and placenta previa is the degree of pain. Abruptio placentae causes pain, whereas placenta previa causes painless bleeding. Because a major role of the placenta is to function as a fetal lung, any condition that interrupts normal blood flow to or from the placenta increases fetal partial pressure of arterial carbon dioxide and decreases fetal pH. Precipitate labor lasts for approximately 3 hours and ends with delivery of the neonate. Methylergonovine (Methergine) is an oxytocic agent used to prevent and treat postpartum hemorrhage caused by uterine atony or subinvolution. As emergency treatment for excessive uterine bleeding, 0.2 mg of methylergonovine (Methergine) is injected I.V. over 1 minute while the patients blood pressure and uterine contractions are monitored. Braxton Hicks contractions are usually felt in the abdomen and dont cause cervical change. True labor contractions are felt in the front of the abdomen and back and lead to progressive cervical dilation and effacement. The average birth weight of neonates born to mothers who smoke is 6 oz (170 g) less than that of neonates born to nonsmoking mothers. Culdoscopy is visualization of the pelvic organs through the posterior vaginal fornix. The nurse should teach a pregnant vegetarian to obtain protein from alternative sources, such as nuts, soybeans, and legumes. The nurse should instruct a pregnant patient to take only prescribed prenatal vitamins because over-the-counter high-potency vitamins may harm the fetus. High-sodium foods can cause fluid retention, especially in pregnant patients. A pregnant patient can avoid constipation and hemorrhoids by adding fiber to her diet. If a fetus has late decelerations (a sign of fetal hypoxia), the nurse should instruct the mother to lie on her left side and then administer 8 to 10 L of oxygen per minute by mask or cannula. The nurse should notify the physician. The side-lying position removes pressure on the inferior vena cava. Oxytocin (Pitocin) promotes lactation and uterine contractions. Lanugo covers the fetuss body until about 20 weeks gestation. Then it begins to disappear from the face, trunk, arms, and legs, in that order. In a neonate, hypoglycemia causes temperature instability, hypotonia, jitteriness, and seizures. Premature, postmature, small-forgestational-age, and large-for-gestational-age neonates are susceptible to this disorder. Neonates typically need to consume 50 to 55 cal per pound of body weight daily. Because oxytocin (Pitocin) stimulates powerful uterine contractions during labor, it must be administered under close observation to help prevent maternal and fetal distress. During fetal heart rate monitoring, variable decelerations indicate compression or prolapse of the umbilical cord. Cytomegalovirus is the leading cause of congenital viral infection. Tocolytic therapy is indicated in premature labor, but contraindicated in fetal death, fetal distress, or severe hemorrhage. Through ultrasonography, the biophysical profile assesses fetal well-being by measuring fetal breathing movements, gross body movements, fetal tone, reactive fetal heart rate (nonstress test), and qualitative amniotic fluid volume. A neonate whose mother has diabetes should be assessed for hyperinsulinism. In a patient with preeclampsia, epigastric pain is a late symptom and requires immediate medical intervention. After a stillbirth, the mother should be allowed to hold the neonate to help her come to terms with the death. Molding is the process by which the fetal head changes shape to facilitate movement through the birth canal. If a woman receives a spinal block before delivery, the nurse should monitor the patients blood pressure closely. If a woman suddenly becomes hypotensive during labor, the nurse should increase the infusion rate of I.V. fluids as prescribed. The best technique for assessing jaundice in a neonate is to blanch the tip of the nose or the area just above the umbilicus. During fetal heart monitoring, early deceleration is caused by compression of the head during labor. After the placenta is delivered, the nurse may add oxytocin (Pitocin) to the patients I.V. solution, as prescribed, to promote postpartum involution of the uterus and stimulate lactation. Pica is a craving to eat nonfood items, such as dirt, crayons, chalk, glue, starch, or hair. It may occur during pregnancy and can endanger the fetus. A pregnant patient should take folic acid because this nutrient is required for rapid cell division. A woman who is taking clomiphene (Clomid) to induce ovulation should be informed of the possibility of multiple births with this drug. If needed, cervical suturing is usually done between 14 and 18 weeks gestation to reinforce an incompetent cervix and maintain pregnancy. The suturing is typically removed by 35 weeks gestation. During the first trimester, a pregnant woman should avoid all drugs unless doing so would adversely affect her health.
Most drugs that a breast-feeding mother takes appear in breast milk. The Food and Drug Administration has established the following five categories of drugs based on their potential for causing birth defects: A, no evidence of risk; B, no risk found in animals, but no studies have been done in women; C, animal studies have shown an adverse effect, but the drug may be beneficial to women despite the potential risk; D, evidence of risk, but its benefits may outweigh its risks; and X, fetal anomalies noted, and the risks clearly outweigh the potential benefits. A patient with a ruptured ectopic pregnancy commonly has sharp pain in the lower abdomen, with spotting and cramping. She may have abdominal rigidity; rapid, shallow respirations; tachycardia; and shock. A patient with a ruptured ectopic pregnancy commonly has sharp pain in the lower abdomen, with spotting and cramping. She may have abdominal rigidity; rapid, shallow respirations; tachycardia; and shock. The mechanics of delivery are engagement, descent and flexion, internal rotation, extension, external rotation, restitution, and expulsion. A probable sign of pregnancy, McDonalds sign is characterized by an ease in flexing the body of the uterus against the cervix. Amenorrhea is a probable sign of pregnancy. A pregnant womans partner should avoid introducing air into the vagina during oral sex because of the possibility of air embolism. The presence of human chorionic gonadotropin in the blood or urine is a probable sign of pregnancy. Radiography isnt usually used in a pregnant woman because it may harm the developing fetus. If radiography is essential, it should be performed only after 36 weeks gestation. A pregnant patient who has had rupture of the membranes or who is experiencing vaginal bleeding shouldnt engage in sexual intercourse. Milia may occur as pinpoint spots over a neonates nose. The duration of a contraction is timed from the moment that the uterine muscle begins to tense to the moment that it reaches full relaxation. Its measured in seconds. The union of a male and a female gamete produces a zygote, which divides into the fertilized ovum. The first menstrual flow is called menarche and may be anovulatory (infertile). Spermatozoa (or their fragments) remain in the vagina for 72 hours after sexual intercourse. Prolactin stimulates and sustains milk production. Strabismus is a normal finding in a neonate. A postpartum patient may resume sexual intercourse after the perineal or uterine wounds heal (usually within 4 weeks after delivery). A pregnant staff member shouldnt be assigned to work with a patient who has cytomegalovirus infection because the virus can be transmitted to the fetus. Fetal demise is death of the fetus after viability. Respiratory distress syndrome develops in premature neonates because their alveoli lack surfactant. The most common method of inducing labor after artificial rupture of the membranes is oxytocin (Pitocin) infusion. After the amniotic membranes rupture, the initial nursing action is to assess the fetal heart rate. The most common reasons for cesarean birth are malpresentation, fetal distress, cephalopelvic disproportion, pregnancy-induced hypertension, previous cesarean birth, and inadequate progress in labor. Amniocentesis increases the risk of spontaneous abortion, trauma to the fetus or placenta, premature labor, infection, and Rh sensitization of the fetus. After amniocentesis, abdominal cramping or spontaneous vaginal bleeding may indicate complications. To prevent her from developing Rh antibodies, an Rh-negative primigravida should receive Rho(D) immune globulin (RhoGAM) after delivering an Rh-positive neonate. If a pregnant patients test results are negative for glucose but positive for acetone, the nurse should assess the patients diet for inadequate caloric intake. If a pregnant patients test results are negative for glucose but positive for acetone, the nurse should assess the patients diet for inadequate caloric intake. Rubella infection in a pregnant patient, especially during the first trimester, can lead to spontaneous abortion or stillbirth as well as fetal cardiac and other birth defects. A pregnant patient should take an iron supplement to help prevent anemia. Direct antiglobulin (direct Coombs) test is used to detect maternal antibodies attached to red blood cells in the neonate. Nausea and vomiting during the first trimester of pregnancy are caused by rising levels of the hormone human chorionic gonadotropin. Before discharging a patient who has had an abortion, the nurse should instruct her to report bright red clots, bleeding that lasts longer than 7 days, or signs of infection, such as a temperature of greater than 100 F (37.8 C), foul-smelling vaginal discharge, severe uterine cramping, nausea, or vomiting. When informed that a patients amniotic membrane has broken, the nurse should check fetal heart tones and then maternal vital signs.
The duration of pregnancy averages 280 days, 40 weeks, 9 calendar months, or 10 lunar months. The initial weight loss for a healthy neonate is 5% to 10% of birth weight. The normal hemoglobin value in neonates is 17 to 20 g/dl. Crowning is the appearance of the fetuss head when its largest diameter is encircled by the vulvovaginal ring. A multipara is a woman who has had two or more pregnancies that progressed to viability, regardless of whether the offspring were alive at birth. In a pregnant patient, preeclampsia may progress to eclampsia, which is characterized by seizures and may lead to coma. The Apgar score is used to assess the neonates vital functions. Its obtained at 1 minute and 5 minutes after delivery. The score is based on respiratory effort, heart rate, muscle tone, reflex irritability, and color. Because of the anti-insulin effects of placental hormones, insulin requirements increase during the third trimester. Gestational age can be estimated by ultrasound measurement of maternal abdominal circumference, fetal femur length, and fetal head size. These measurements are most accurate between 12 and 18 weeks gestation. Skeletal system abnormalities and ventricular septal defects are the most common disorders of infants who are born to diabetic women. The incidence of congenital malformation is three times higher in these infants than in those born to nondiabetic women. Skeletal system abnormalities and ventricular septal defects are the most common disorders of infants who are born to diabetic women. The incidence of congenital malformation is three times higher in these infants than in those born to nondiabetic women. The patient with preeclampsia usually has puffiness around the eyes or edema in the hands (for example, I cant put my wedding ring on.). Kegel exercises require contraction and relaxation of the perineal muscles. These exercises help strengthen pelvic muscles and improve urine control in postpartum patients. Symptoms of postpartum depression range from mild postpartum blues to intense, suicidal, depressive psychosis. The preterm neonate may require gavage feedings because of a weak sucking reflex, uncoordinated sucking, or respiratory distress. Acrocyanosis (blueness and coolness of the arms and legs) is normal in neonates because of their immature peripheral circulatory system. To prevent ophthalmia neonatorum (a severe eye infection caused by maternal gonorrhea), the nurse may administer one of three drugs, as prescribed, in the neonates eyes: tetracycline, silver nitrate, or erythromycin. Neonatal testing for phenylketonuria is mandatory in most states. The nurse should place the neonate in a 30-degree Trendelenburg position to facilitate mucus drainage. The nurse may suction the neonates nose and mouth as needed with a bulb syringe or suction trap. To prevent heat loss, the nurse should place the neonate under a radiant warmer during suctioning and initial delivery-room care, and then wrap the neonate in a warmed blanket for transport to the nursery. The umbilical cord normally has two arteries and one vein. When providing care, the nurse should expose only one part of an infants body at a time. Lightening is settling of the fetal head into the brim of the pelvis. If the neonate is stable, the mother should be allowed to breast-feed within the neonates first hour of life. The nurse should check the neonates temperature every 1 to 2 hours until its maintained within normal limits. At birth, a neonate normally weighs 5 to 9 lb (2 to 4 kg), measures 18" to 22" (45.5 to 56 cm) in length, has a head circumference of 13" to 14" (34 to 35.5 cm), and has a chest circumference thats 1" (2.5 cm) less than the head circumference. In the neonate, temperature normally ranges from 98 to 99 F (36.7 to 37.2 C), apical pulse rate averages 120 to 160 beats/minute, and respirations are 40 to 60 breaths/minute. The diamond-shaped anterior fontanel usually closes between ages 12 and 18 months. The triangular posterior fontanel usually closes by age 2 months. In the neonate, a straight spine is normal. A tuft of hair over the spine is an abnormal finding. Prostaglandin gel may be applied to the vagina or cervix to ripen an unfavorable cervix before labor induction with oxytocin (Pitocin). Supernumerary nipples are occasionally seen on neonates. They usually appear along a line that runs from each axilla, through the normal nipple area, and to the groin. Meconium is a material that collects in the fetuss intestines and forms the neonates first feces, which are black and tarry. The presence of meconium in the amniotic fluid during labor indicates possible fetal distress and the need to evaluate the neonate for meconium aspiration. To assess a neonates rooting reflex, the nurse touches a finger to the cheek or the corner of the mouth. Normally, the neonate turns his head toward the stimulus, opens his mouth, and searches for the stimulus. Harlequin sign is present when a neonate who is lying on his side appears red on the dependent side and pale on the upper side. Mongolian spots can range from brown to blue. Their color depends on how close melanocytes are to the surface of the skin. They most commonly appear as patches across the sacrum, buttocks, and legs. Mongolian spots are common in non-white infants and usually disappear by age 2 to 3 years.
Vernix caseosa is a cheeselike substance that covers and protects the fetuss skin in utero. It may be rubbed into the neonates skin or washed away in one or two baths. Caput succedaneum is edema that develops in and under the fetal scalp during labor and delivery. It resolves spontaneously and presents no danger to the neonate. The edema doesnt cross the suture line. Nevus flammeus, or port-wine stain, is a diffuse pink to dark bluish red lesion on a neonates face or neck. The Guthrie test (a screening test for phenylketonuria) is most reliable if its done between the second and sixth days after birth and is performed after the neonate has ingested protein. To assess coordination of sucking and swallowing, the nurse should observe the neonates first breast-feeding or sterile water bottle-feeding. To establish a milk supply pattern, the mother should breast-feed her infant at least every 4 hours. During the first month, she should breast-feed 8 to 12 times daily (demand feeding). To avoid contact with blood and other body fluids, the nurse should wear gloves when handling the neonate until after the first bath is given. If a breast-fed infant is content, has good skin turgor, an adequate number of wet diapers, and normal weight gain, the mothers milk supply is assumed to be adequate. In the supine position, a pregnant patients enlarged uterus impairs venous return from the lower half of the body to the heart, resulting in supine hypotensive syndrome, or inferior vena cava syndrome. Tocolytic agents used to treat preterm labor include terbutaline (Brethine), ritodrine (Yutopar), and magnesium sulfate. A pregnant woman who has hyperemesis gravidarum may require hospitalization to treat dehydration and starvation. Diaphragmatic hernia is one of the most urgent neonatal surgical emergencies. By compressing and displacing the lungs and heart, this disorder can cause respiratory distress shortly after birth. Common complications of early pregnancy (up to 20 weeks gestation) include fetal loss and serious threats to maternal health. Fetal embodiment is a maternal developmental task that occurs in the second trimester. During this stage, the mother may complain that she never gets to sleep because the fetus always gives her a thump when she tries. Visualization in pregnancy is a process in which the mother imagines what the child shes carrying is like and becomes acquainted with it. Hemodilution of pregnancy is the increase in blood volume that occurs during pregnancy. The increased volume consists of plasma and causes an imbalance between the ratio of red blood cells to plasma and a resultant decrease in hematocrit. Mean arterial pressure of greater than 100 mm Hg after 20 weeks of pregnancy is considered hypertension. The treatment for supine hypotension syndrome (a condition that sometimes occurs in pregnancy) is to have the patient lie on her left side. A contributing factor in dependent edema in the pregnant patient is the increase of femoral venous pressure from 10 mm Hg (normal) to 18 mm Hg (high). Hyperpigmentation of the pregnant patients face, formerly called chloasma and now referred to as melasma, fades after delivery. The hormone relaxin, which is secreted first by the corpus luteum and later by the placenta, relaxes the connective tissue and cartilage of the symphysis pubis and the sacroiliac joint to facilitate passage of the fetus during delivery. Progesterone maintains the integrity of the pregnancy by inhibiting uterine motility. Ladins sign, an early indication of pregnancy, causes softening of a spot on the anterior portion of the uterus, just above the uterocervical juncture. During pregnancy, the abdominal line from the symphysis pubis to the umbilicus changes from linea alba to linea nigra. In neonates, cold stress affects the circulatory, regulatory, and respiratory systems. Obstetric data can be described by using the F/TPAL system: F/T: Full-term delivery at 38 weeks or longer P: Preterm delivery between 20 and 37 weeks A: Abortion or loss of fetus before 20 weeks L: Number of children living (if a child has died, further explanation is needed to clarify the discrepancy in numbers). Parity doesnt refer to the number of infants delivered, only the number of deliveries. Women who are carrying more than one fetus should be encouraged to gain 35 to 45 lb (15.5 to 20.5 kg) during pregnancy. The recommended amount of iron supplement for the pregnant patient is 30 to 60 mg daily. Drinking six alcoholic beverages a day or a single episode of binge drinking in the first trimester can cause fetal alcohol syndrome. Chorionic villus sampling is performed at 8 to 12 weeks of pregnancy for early identification of genetic defects. In percutaneous umbilical blood sampling, a blood sample is obtained from the umbilical cord to detect anemia, genetic defects, and blood incompatibility as well as to assess the need for blood transfusions. The period between contractions is referred to as the interval, or resting phase. During this phase, the uterus and placenta fill with blood and allow for the exchange of oxygen, carbon dioxide, and nutrients.
In a patient who has hypertonic contractions, the uterus doesnt have an opportunity to relax and there is no interval between contractions. As a result, the fetus may experience hypoxia or rapid delivery may occur. Two qualities of the myometrium are elasticity, which allows it to stretch yet maintain its tone, and contractility, which allows it to shorten and lengthen in a synchronized pattern. During crowning, the presenting part of the fetus remains visible during the interval between contractions. Uterine atony is failure of the uterus to remain firmly contracted. The major cause of uterine atony is a full bladder. If the mother wishes to breast-feed, the neonate should be nursed as soon as possible after delivery. A smacking sound, milk dripping from the side of the mouth, and sucking noises all indicate improper placement of the infants mouth over the nipple. Before feeding is initiated, an infant should be burped to expel air from the stomach. Most authorities strongly encourage the continuation of breast-feeding on both the affected and the unaffected breast of patients with mastitis. Neonates are nearsighted and focus on items that are held 10" to 12" (25 to 30.5 cm) away. In a neonate, low-set ears are associated with chromosomal abnormalities such as Down syndrome. Meconium is usually passed in the first 24 hours; however, passage may take up to 72 hours. Boys who are born with hypospadias shouldnt be circumcised at birth because the foreskin may be needed for constructive surgery. In the neonate, the normal blood glucose level is 45 to 90 mg/dl. Hepatitis B vaccine is usually given within 48 hours of birth. Hepatitis B immune globulin is usually given within 12 hours of birth. HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome is an unusual variation of pregnancy-induced hypertension. Maternal serum alpha-fetoprotein is detectable at 7 weeks of gestation and peaks in the third trimester. High levels detected between the 16th and 18th weeks are associated with neural tube defects. Low levels are associated with Down syndrome. An arrest of descent occurs when the fetus doesnt descend through the pelvic cavity during labor. Its commonly associated with cephalopelvic disproportion, and cesarean delivery may be required. A late sign of preeclampsia is epigastric pain as a result of severe liver edema. In the patient with preeclampsia, blood pressure returns to normal during the puerperal period. To obtain an estriol level, urine is collected for 24 hours. An estriol level is used to assess fetal well-being and maternal renal functioning as well as to monitor a pregnancy thats complicated by diabetes. A pregnant patient with vaginal bleeding shouldnt have a pelvic examination. In the early stages of pregnancy, the finding of glucose in the urine may be related to the increased shunting of glucose to the developing placenta, without a corresponding increase in the reabsorption capability of the kidneys. A patient who has premature rupture of the membranes is at significant risk for infection if labor doesnt begin within 24 hours. Infants of diabetic mothers are susceptible to macrosomia as a result of increased insulin production in the fetus. To prevent heat loss in the neonate, the nurse should bathe one part of his body at a time and keep the rest of the body covered. A patient who has a cesarean delivery is at greater risk for infection than the patient who gives birth vaginally. The occurrence of thrush in the neonate is probably caused by contact with the organism during delivery through the birth canal. The nurse should keep the sac of meningomyelocele moist with normal saline solution. If fundal height is at least 2 cm less than expected, the cause may be growth retardation, missed abortion, transverse lie, or false pregnancy. Fundal height that exceeds expectations by more than 2 cm may be caused by multiple gestation, polyhydramnios, uterine myomata, or a large baby. A major developmental task for a woman during the first trimester of pregnancy is accepting the pregnancy. Unlike formula, breast milk offers the benefit of maternal antibodies. Spontaneous rupture of the membranes increases the risk of a prolapsed umbilical cord. A clinical manifestation of a prolapsed umbilical cord is variable decelerations. During labor, to relieve supine hypotension manifested by nausea and vomiting and paleness, turn the patient on her left side. If the ovum is fertilized by a spermatozoon carrying a Y chromosome, a male zygote is formed. Implantation occurs when the cellular walls of the blastocyte implants itself in the endometrium, usually 7 to 9 days after fertilization. Implantation occurs when the cellular walls of the blastocyte implants itself in the endometrium, usually 7 to 9 days after fertilization. Heart development in the embryo begins at 2 to 4 weeks and is complete by the end of the embryonic stage. Methergine stimulates uterine contractions.
The administration of folic acid during the early stages of gestation may prevent neural tube defects. With advanced maternal age, a common genetic problem is Down syndrome. With early maternal age, cephalopelvic disproportion commonly occurs. In the early postpartum period, the fundus should be midline at the umbilicus. A rubella vaccine shouldnt be given to a pregnant woman. The vaccine can be administered after delivery, but the patient should be instructed to avoid becoming pregnant for 3 months. A 16-year-old girl who is pregnant is at risk for having a low-birth-weight neonate. The mothers Rh factor should be determined before an amniocentesis is performed. Maternal hypotension is a complication of spinal block. After delivery, if the fundus is boggy and deviated to the right side, the patient should empty her bladder. Before providing a specimen for a sperm count, the patient should avoid ejaculation for 48 to 72 hours. The hormone human chorionic gonadotropin is a marker for pregnancy. Painless vaginal bleeding during the last trimester of pregnancy may indicate placenta previa. During the transition phase of labor, the woman usually is irritable and restless. Because women with diabetes have a higher incidence of birth anomalies than women without diabetes, an alpha-fetoprotein level may be ordered at 15 to 17 weeks gestation. To avoid puncturing the placenta, a vaginal examination shouldnt be performed on a pregnant patient who is bleeding. A patient who has postpartum hemorrhage caused by uterine atony should be given oxytocin as prescribed. Laceration of the vagina, cervix, or perineum produces bright red bleeding that often comes in spurts. The bleeding is continuous, even when the fundus is firm. Hot compresses can help to relieve breast tenderness after breast-feeding. The fundus of a postpartum patient is massaged to stimulate contraction of the uterus and prevent hemorrhage. A mother who has a positive human immunodeficiency virus test result shouldnt breast-feed her infant. Dinoprostone (Cervidil) is used to ripen the cervix. Breast-feeding of a premature neonate born at 32 weeks gestation can be accomplished if the mother expresses milk and feeds the neonate by gavage. If a pregnant patients rubella titer is less than 1:8, she should be immunized after delivery. The administration of oxytocin (Pitocin) is stopped if the contractions are 90 seconds or longer. For an extramural delivery (one that takes place outside of a normal delivery center), the priorities for care of the neonate include maintaining a patent airway, supporting efforts to breathe, monitoring vital signs, and maintaining adequate body temperature. Subinvolution may occur if the bladder is distended after delivery. The nurse must place identification bands on both the mother and the neonate before they leave the delivery room. Erythromycin is given at birth to prevent ophthalmia neonatorum. Pelvic-tilt exercises can help to prevent or relieve backache during pregnancy. Before performing a Leopold maneuver, the nurse should ask the patient to empty her bladder.
NCLEX and Nursing Board Exam Psychiatric Nursing Bullets Posted by Cedric on Jul 20, 2009
According to Kbler-Ross, the five stages of death and dying are denial, anger, bargaining, depression, and acceptance. Flight of ideas is an alteration in thought processes thats characterized by skipping from one topic to another, unrelated topic. La belle indiffrence is the lack of concern for a profound disability, such as blindness or paralysis that may occur in a patient who has a conversion disorder. Moderate anxiety decreases a persons ability to perceive and concentrate. The person is selectively inattentive (focuses on immediate concerns), and the perceptual field narrows. A patient who has a phobic disorder uses self-protective avoidance as an ego defense mechanism. In a patient who has anorexia nervosa, the highest treatment priority is correction of nutritional and electrolyte imbalances. A patient who is taking lithium must undergo regular (usually once a month) monitoring of the blood lithium level because the margin between therapeutic and toxic levels is narrow. A normal laboratory value is 0.5 to 1.5 mEq/L. Early signs and symptoms of alcohol withdrawal include anxiety, anorexia, tremors, and insomnia. They may begin up to 8 hours after the last alcohol intake.
Al-Anon is a support group for families of alcoholics. The nurse shouldnt administer chlorpromazine (Thorazine) to a patient who has ingested alcohol because it may cause oversedation and respiratory depression. Lithium toxicity can occur when sodium and fluid intake are insufficient, causing lithium retention. An alcoholic who achieves sobriety is called a recovering alcoholic because no cure for alcoholism exists. According to Erikson, the school-age child (ages 6 to 12) is in the industry-versus-inferiority stage of psychosocial development. When caring for a depressed patient, the nurses first priority is safety because of the increased risk of suicide. Echolalia is parrotlike repetition of another persons words or phrases. According to psychoanalytic theory, the ego is the part of the psyche that controls internal demands and interacts with the outside world at the conscious, preconscious, and unconscious levels. According to psychoanalytic theory, the superego is the part of the psyche thats composed of morals, values, and ethics. It continually evaluates thoughts and actions, rewarding the good and punishing the bad. (Think of the superego as the supercop of the unconscious.) According to psychoanalytic theory, the id is the part of the psyche that contains instinctual drives. (Remember i for instinctual and d for drive.) Denial is the defense mechanism used by a patient who denies the reality of an event. In a psychiatric setting, seclusion is used to reduce overwhelming environmental stimulation, protect the patient from self-injury or injury to others, and prevent damage to hospital property. Its used for patients who dont respond to less restrictive interventions. Seclusion controls external behavior until the patient can assume self-control and helps the patient to regain self-control. Tyramine-rich food, such as aged cheese, chicken liver, avocados, bananas, meat tenderizer, salami, bologna, Chianti wine, and beer may cause severe hypertension in a patient who takes a monoamine oxidase inhibitor. A patient who takes a monoamine oxidase inhibitor should be weighed biweekly and monitored for suicidal tendencies. If the patient who takes a monoamine oxidase inhibitor has palpitations, headaches, or severe orthostatic hypotension, the nurse should withhold the drug and notify the physician. Common causes of child abuse are poor impulse control by the parents and the lack of knowledge of growth and development. The diagnosis of Alzheimers disease is based on clinical findings of two or more cognitive deficits, progressive worsening of memory, and the results of a neuropsychological test. Memory disturbance is a classic sign of Alzheimers disease. Thought blocking is loss of the train of thought because of a defect in mental processing. A compulsion is an irresistible urge to perform an irrational act, such as walking in a clockwise circle before leaving a room or washing the hands repeatedly. A patient who has a chosen method and a plan to commit suicide in the next 48 to 72 hours is at high risk for suicide. The therapeutic serum level for lithium is 0.5 to 1.5 mEq/L. Phobic disorders are treated with desensitization therapy, which gradually exposes a patient to an anxiety-producing stimulus. Dysfunctional grieving is absent or prolonged grief. During phase I of the nurse-patient relationship (beginning, or orientation, phase), the nurse obtains an initial history and the nurse and the patient agree to a contract. During phase II of the nurse-patient relationship (middle, or working, phase), the patient discusses his problems, behavioral changes occur, and self-defeating behavior is resolved or reduced. During phase III of the nurse-patient relationship (termination, or resolution, phase), the nurse terminates the therapeutic relationship and gives the patient positive feedback on his accomplishments. According to Freud, a person between ages 12 and 20 is in the genital stage, during which he learns independence, has an increased interest in members of the opposite sex, and establishes an identity. According to Erikson, the identity-versus-role confusion stage occurs between ages 12 and 20.
Tolerance is the need for increasing amounts of a substance to achieve an effect that formerly was achieved with lesser amounts. Suicide is the third leading cause of death among white teenagers. Most teenagers who kill themselves made a previous suicide attempt and left telltale signs of their plans. In Eriksons stage of generativity versus despair, generativity (investment of the self in the interest of the larger community) is expressed through procreation, work, community service, and creative endeavors. Alcoholics Anonymous recommends a 12-step program to achieve sobriety. Signs and symptoms of anorexia nervosa include amenorrhea, excessive weight loss, lanugo (fine body hair), abdominal distention, and electrolyte disturbances. A serum lithium level that exceeds 2.0 mEq/L is considered toxic. Public Law 94-247 (Child Abuse and Neglect Act of 1973) requires reporting of suspected cases of child abuse to child protection services. The nurse should suspect sexual abuse in a young child who has blood in the feces or urine, penile or vaginal discharge, genital trauma that isnt readily explained, or a sexually transmitted disease. An alcoholic uses alcohol to cope with the stresses of life. The human personality operates on three levels: conscious, preconscious, and unconscious. Asking a patient an open-ended question is one of the best ways to elicit or clarify information. The diagnosis of autism is often made when a child is between ages 2 and 3. Defense mechanisms protect the personality by reducing stress and anxiety. Suppression is voluntary exclusion of stress-producing thoughts from the consciousness. In psychodrama, life situations are approximated in a structured environment, allowing the participant to recreate and enact scenes to gain insight and to practice new skills. Psychodrama is a therapeutic technique thats used with groups to help participants gain new perception and self-awareness by acting out their own or assigned problems. A patient who is taking disulfiram (Antabuse) must avoid ingesting products that contain alcohol, such as cough syrup, fruitcake, and sauces and soups made with cooking wine. A patient who is admitted to a psychiatric hospital involuntarily loses the right to sign out against medical advice. People who live in glass houses shouldnt throw stones and A rolling stone gathers no moss are examples of proverbs used during a psychiatric interview to determine a patients ability to think abstractly. (Schizophrenic patients think in concrete terms and might interpret the glass house proverb as If you throw a stone in a glass house, the house will break.) Signs of lithium toxicity include diarrhea, tremors, nausea, muscle weakness, ataxia, and confusion. A labile affect is characterized by rapid shifts of emotions and mood. Amnesia is loss of memory from an organic or inorganic cause. A person who has borderline personality disorder is demanding and judgmental in interpersonal relationships and will attempt to split staff by pointing to discrepancies in the treatment plan. Disulfiram (Antabuse) shouldnt be taken concurrently with metronidazole (Flagyl) because they may interact and cause a psychotic reaction. In rare cases, electroconvulsive therapy causes arrhythmias and death. A patient who is scheduled for electroconvulsive therapy should receive nothing by mouth after midnight to prevent aspiration while under anesthesia. Electroconvulsive therapy is normally used for patients who have severe depression that doesnt respond to drug therapy. For electroconvulsive therapy to be effective, the patient usually receives 6 to 12 treatments at a rate of 2 to 3 per week. During the manic phase of bipolar affective disorder, nursing care is directed at slowing the patient down because the patient may die as a result of self-induced exhaustion or injury.
For a patient with Alzheimers disease, the nursing care plan should focus on safety measures. After sexual assault, the patients needs are the primary concern, followed by medicolegal considerations. Patients who are in a maintenance program for narcotic abstinence syndrome receive 10 to 40 mg of methadone (Dolophine) in a single daily dose and are monitored to ensure that the drug is ingested. Stress management is a short-range goal of psychotherapy. The mood most often experienced by a patient with organic brain syndrome is irritability. Creative intuition is controlled by the right side of the brain. Methohexital (Brevital) is the general anesthetic thats administered to patients who are scheduled for electroconvulsive therapy. The decision to use restraints should be based on the patients safety needs. Diphenhydramine (Benadryl) relieves the extrapyramidal adverse effects of psychotropic drugs. In a patient who is stabilized on lithium (Eskalith) therapy, blood lithium levels should be checked 8 to 12 hours after the first dose, then two or three times weekly during the first month. Levels should be checked weekly to monthly during maintenance therapy. The primary purpose of psychotropic drugs is to decrease the patients symptoms, which improves function and increases compliance with therapy. Manipulation is a maladaptive method of meeting ones needs because it disregards the needs and feelings of others. If a patient has symptoms of lithium toxicity, the nurse should withhold one dose and call the physician. A patient who is taking lithium (Eskalith) for bipolar affective disorder must maintain a balanced diet with adequate salt intake. A patient who constantly seeks approval or assistance from staff members and other patients is demonstrating dependent behavior. Alcoholics Anonymous advocates total abstinence from alcohol. Methylphenidate (Ritalin) is the drug of choice for treating attention deficit hyperactivity disorder in children. Setting limits is the most effective way to control manipulative behavior. Violent outbursts are common in a patient who has borderline personality disorder. When working with a depressed patient, the nurse should explore meaningful losses. An illusion is a misinterpretation of an actual environmental stimulus. Anxiety is nonspecific; fear is specific. Extrapyramidal adverse effects are common in patients who take antipsychotic drugs. The nurse should encourage an angry patient to follow a physical exercise program as one of the ways to ventilate feelings. Depression is clinically significant if its characterized by exaggerated feelings of sadness, melancholy, dejection, worthlessness, and hopelessness that are inappropriate or out of proportion to reality. Free-floating anxiety is anxiousness with generalized apprehension and pessimism for unknown reasons. In a patient who is experiencing intense anxiety, the fight-or-flight reaction (alarm reflex) may take over. Confabulation is the use of imaginary experiences or made-up information to fill missing gaps of memory. When starting a therapeutic relationship with a patient, the nurse should explain that the purpose of the therapy is to produce a positive change. A basic assumption of psychoanalytic theory is that all behavior has meaning. Catharsis is the expression of deep feelings and emotions. According to the pleasure principle, the psyche seeks pleasure and avoids unpleasant experiences, regardless of the consequences. A patient who has a conversion disorder resolves a psychological conflict through the loss of a specific physical function (for example, paralysis, blindness, or inability to swallow). This loss of function is involuntary, but diagnostic tests show no organic cause. Chlordiazepoxide (Librium) is the drug of choice for treating alcohol withdrawal symptoms.
For a patient who is at risk for alcohol withdrawal, the nurse should assess the pulse rate and blood pressure every 2 hours for the first 12 hours, every 4 hours for the next 24 hours, and every 6 hours thereafter (unless the patients condition becomes unstable). Alcohol detoxification is most successful when carried out in a structured environment by a supportive, nonjudgmental staff. The nurse should follow these guidelines when caring for a patient who is experiencing alcohol withdrawal: Maintain a calm environment, keep intrusions to a minimum, speak slowly and calmly, adjust lighting to prevent shadows and glare, call the patient by name, and have a friend or family member stay with the patient, if possible. The therapeutic regimen for an alcoholic patient includes folic acid, thiamine, and multivitamin supplements as well as adequate food and fluids. A patient who is addicted to opiates (drugs derived from poppy seeds, such as heroin and morphine) typically experiences withdrawal symptoms within 12 hours after the last dose. The most severe symptoms occur within 48 hours and decrease over the next 2 weeks. Reactive depression is a response to a specific life event. Projection is the unconscious assigning of a thought, feeling, or action to someone or something else. Sublimation is the channeling of unacceptable impulses into socially acceptable behavior. Repression is an unconscious defense mechanism whereby unacceptable or painful thoughts, impulses, memories, or feelings are pushed from the consciousness or forgotten. Hypochondriasis is morbid anxiety about ones health associated with various symptoms that arent caused by organic disease. Denial is a refusal to acknowledge feelings, thoughts, desires, impulses, or external facts that are consciously intolerable. Reaction formation is the avoidance of anxiety through behavior and attitudes that are the opposite of repressed impulses and drives. Displacement is the transfer of unacceptable feelings to a more acceptable object. Regression is a retreat to an earlier developmental stage. According to Erikson, an older adult (age 65 or older) is in the developmental stage of integrity versus despair. Family therapy focuses on the family as a whole rather than the individual. Its major objective is to reestablish rational communication between family members. When caring for a patient who is hostile or angry, the nurse should attempt to remain calm, listen impartially, use short sentences, and speak in a firm, quiet voice. Ritualism and negativism are typical toddler behaviors. They occur during the developmental stage identified by Erikson as autonomy versus shame and doubt. Circumstantiality is a disturbance in associated thought and speech patterns in which a patient gives unnecessary, minute details and digresses into inappropriate thoughts that delay communication of central ideas and goal achievement. Idea of reference is an incorrect belief that the statements or actions of others are related to oneself. Group therapy provides an opportunity for each group member to examine interactions, learn and practice successful interpersonal communication skills, and explore emotional conflicts. Korsakoffs syndrome is believed to be a chronic form of Wernickes encephalopathy. Its marked by hallucinations, confabulation, amnesia, and disturbances of orientation. A patient with antisocial personality disorder often engages in confrontations with authority figures, such as police, parents, and school officials. A patient with paranoid personality disorder exhibits suspicion, hypervigilance, and hostility toward others. Depression is the most common psychiatric disorder. Adverse reactions to tricyclic antidepressant drugs include tachycardia, orthostatic hypotension, hypomania, lowered seizure threshold, tremors, weight gain, problems with erections or orgasms, and anxiety. The Minnesota Multiphasic Personality Inventory consists of 550 statements for the subject to interpret. It assesses personality and detects disorders, such as depression and schizophrenia, in adolescents and adults. Organic brain syndrome is the most common form of mental illness in elderly patients.
A person who has an IQ of less than 20 is profoundly retarded and is considered a total-care patient. Reframing is a therapeutic technique thats used to help depressed patients to view a situation in alternative ways. Fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil) are serotonin reuptake inhibitors used to treat depression. The early stage of Alzheimers disease lasts 2 to 4 years. Patients have inappropriate affect, transient paranoia, disorientation to time, memory loss, careless dressing, and impaired judgment. The middle stage of Alzheimers disease lasts 4 to 7 years and is marked by profound personality changes, loss of independence, disorientation, confusion, inability to recognize family members, and nocturnal restlessness. The last stage of Alzheimers disease occurs during the final year of life and is characterized by a blank facial expression, seizures, loss of appetite, emaciation, irritability, and total dependence. Threatening a patient with an injection for failing to take an oral drug is an example of assault. Reexamination of life goals is a major developmental task during middle adulthood. Acute alcohol withdrawal causes anorexia, insomnia, headache, and restlessness and escalates to a syndrome thats characterized by agitation, disorientation, vivid hallucinations, and tremors of the hands, feet, legs, and tongue. In a hospitalized alcoholic, alcohol withdrawal delirium most commonly occurs 3 to 4 days after admission. Confrontation is a communication technique in which the nurse points out discrepancies between the patients words and his nonverbal behaviors. For a patient with substance-induced delirium, the time of drug ingestion can help to determine whether the drug can be evacuated from the body. Treatment for alcohol withdrawal may include administration of I.V. glucose for hypoglycemia, I.V. fluid containing thiamine and other B vitamins, and antianxiety, antidiarrheal, anticonvulsant, and antiemetic drugs. The alcoholic patient receives thiamine to help prevent peripheral neuropathy and Korsakoffs syndrome. Alcohol withdrawal may precipitate seizure activity because alcohol lowers the seizure threshold in some people. Paraphrasing is an active listening technique in which the nurse restates what the patient has just said. A patient with Korsakoffs syndrome may use confabulation (made up information) to cover memory lapses or periods of amnesia. People with obsessive-compulsive disorder realize that their behavior is unreasonable, but are powerless to control it. When witnessing psychiatric patients who are engaged in a threatening confrontation, the nurse should first separate the two individuals. Patients with anorexia nervosa or bulimia must be observed during meals and for some time afterward to ensure that they dont purge what they have eaten. Transsexuals believe that they were born the wrong gender and may seek hormonal or surgical treatment to change their gender. Fugue is a dissociative state in which a person leaves his familiar surroundings, assumes a new identity, and has amnesia about his previous identity. (Its also described as flight from himself.) In a psychiatric setting, the patient should be able to predict the nurses behavior and expect consistent positive attitudes and approaches. When establishing a schedule for a one-to-one interaction with a patient, the nurse should state how long the conversation will last and then adhere to the time limit. Thought broadcasting is a type of delusion in which the person believes that his thoughts are being broadcast for the world to hear. Lithium should be taken with food. A patient who is taking lithium shouldnt restrict his sodium intake. A patient who is taking lithium should stop taking the drug and call his physician if he experiences vomiting, drowsiness, or muscle weakness. The patient who is taking a monoamine oxidase inhibitor for depression can include cottage cheese, cream cheese, yogurt, and sour cream in his diet. Sensory overload is a state in which sensory stimulation exceeds the individuals capacity to tolerate or process it. Symptoms of sensory overload include a feeling of distress and hyperarousal with impaired thinking and concentration.
In sensory deprivation, overall sensory input is decreased. A sign of sensory deprivation is a decrease in stimulation from the environment or from within oneself, such as daydreaming, inactivity, sleeping excessively, and reminiscing. The three stages of general adaptation syndrome are alarm, resistance, and exhaustion. A maladaptive response to stress is drinking alcohol or smoking excessively. Hyperalertness and the startle reflex are characteristics of posttraumatic stress disorder. A treatment for a phobia is desensitization, a process in which the patient is slowly exposed to the feared stimuli. Symptoms of major depressive disorder include depressed mood, inability to experience pleasure, sleep disturbance, appetite changes, decreased libido, and feelings of worthlessness. Clinical signs of lithium toxicity are nausea, vomiting, and lethargy. Asking too many why questions yields scant information and may overwhelm a psychiatric patient and lead to stress and withdrawal. Remote memory may be impaired in the late stages of dementia. According to the DSM-IV, bipolar II disorder is characterized by at least one manic episode thats accompanied by hypomania. The nurse can use silence and active listening to promote interactions with a depressed patient. A psychiatric patient with a substance abuse problem and a major psychiatric disorder has a dual diagnosis. When a patient is readmitted to a mental health unit, the nurse should assess compliance with medication orders. Alcohol potentiates the effects of tricyclic antidepressants. Flight of ideas is movement from one topic to another without any discernible connection. Conduct disorder is manifested by extreme behavior, such as hurting people and animals. During the tension-building phase of an abusive relationship, the abused individual feels helpless. In the emergency treatment of an alcohol-intoxicated patient, determining the blood-alcohol level is paramount in determining the amount of medication that the patient needs. Side effects of the antidepressant fluoxetine (Prozac) include diarrhea, decreased libido, weight loss, and dry mouth. Before electroconvulsive therapy, the patient is given the skeletal muscle relaxant succinylcholine (Anectine) by I.V. administration. When a psychotic patient is admitted to an inpatient facility, the primary concern is safety, followed by the establishment of trust. An effective way to decrease the risk of suicide is to make a suicide contract with the patient for a specified period of time. A depressed patient should be given sufficient portions of his favorite foods, but shouldnt be overwhelmed with too much food. The nurse should assess the depressed patient for suicidal ideation. Delusional thought patterns commonly occur during the manic phase of bipolar disorder. Apathy is typically observed in patients who have schizophrenia. Manipulative behavior is characteristic of a patient who has passive aggressive personality disorder. When a patient who has schizophrenia begins to hallucinate, the nurse should redirect the patient to activities that are focused on the here and now. When a patient who is receiving an antipsychotic drug exhibits muscle rigidity and tremors, the nurse should administer an antiparkinsonian drug (for example, Cogentin or Artane) as ordered. A patient who is receiving lithium (Eskalith) therapy should report diarrhea, vomiting, drowsiness, muscular weakness, or lack of coordination to the physician immediately. The therapeutic serum level of lithium (Eskalith) for maintenance is 0.6 to 1.2 mEq/L. Obsessive-compulsive disorder is an anxiety-related disorder. Al-Anon is a self-help group for families of alcoholics.
Desensitization is a treatment for phobia, or irrational fear. After electroconvulsive therapy, the patient is placed in the lateral position, with the head turned to one side. A delusion is a fixed false belief. Giving away personal possessions is a sign of suicidal ideation. Other signs include writing a suicide note or talking about suicide. Agoraphobia is fear of open spaces. A person who has paranoid personality disorder projects hostilities onto others. To assess a patients judgment, the nurse should ask the patient what he would do if he found a stamped, addressed envelope. An appropriate response is that he would mail the envelope. After electroconvulsive therapy, the patient should be monitored for post-shock amnesia. A mother who continues to perform cardiopulmonary resuscitation after a physician pronounces a child dead is showing denial. Transvestism is a desire to wear clothes usually worn by members of the opposite sex. Tardive dyskinesia causes excessive blinking and unusual movement of the tongue, and involuntary sucking and chewing. Trihexyphenidyl (Artane) and benztropine (Cogentin) are administered to counteract extrapyramidal adverse effects. To prevent hypertensive crisis, a patient who is taking a monoamine oxidase inhibitor should avoid consuming aged cheese, caffeine, beer, yeast, chocolate, liver, processed foods, and monosodium glutamate. Extrapyramidal symptoms include parkinsonism, dystonia, akathisia (ants in the pants), and tardive dyskinesia. One theory that supports the use of electroconvulsive therapy suggests that it resets the brain circuits to allow normal function. A patient who has obsessive-compulsive disorder usually recognizes the senselessness of his behavior but is powerless to stop it (ego-dystonia). In helping a patient who has been abused, physical safety is the nurses first priority. Pemoline (Cylert) is used to treat attention deficit hyperactivity disorder (ADHD). Clozapine (Clozaril) is contraindicated in pregnant women and in patients who have severe granulocytopenia or severe central nervous system depression. Repression, an unconscious process, is the inability to recall painful or unpleasant thoughts or feelings. Projection is shifting of unwanted characteristics or shortcomings to others (scapegoat). Hypnosis is used to treat psychogenic amnesia. Disulfiram (Antabuse) is administered orally as an aversion therapy to treat alcoholism. Ingestion of alcohol by a patient who is taking disulfiram (Antabuse) can cause severe reactions, including nausea and vomiting, and may endanger the patients life. Improved concentration is a sign that lithium is taking effect. Behavior modification, including time-outs, token economy, or a reward system, is a treatment for attention deficit hyperactivity disorder. For a patient who has anorexia nervosa, the nurse should provide support at mealtime and record the amount the patient eats. A significant toxic risk associated with clozapine (Clozaril) administration is blood dyscrasia. Adverse effects of haloperidol (Haldol) administration include drowsiness; insomnia; weakness; headache; and extrapyramidal symptoms, such as akathisia, tardive dyskinesia, and dystonia. Hypervigilance and dj vu are signs of posttraumatic stress disorder (PTSD). A child who shows dissociation has probably been abused. Confabulation is the use of fantasy to fill in gaps of memory. FUNDA BULLETS A blood pressure cuff thats too narrow can cause a falsely elevated blood pressure reading.
When preparing a single injection for a patient who takes regular and neutral protein Hagedorn insulin, the nurse should draw the regular insulin into the syringe first so that it does not contaminate the regular insulin. Rhonchi are the rumbling sounds heard on lung auscultation. They are more pronounced during expiration than during inspiration. Gavage is forced feeding, usually through a gastric tube (a tube passed into the stomach through the mouth). According to Maslows hierarchy of needs, physiologic needs (air, water, food, shelter, sex, activity, and comfort) have the highest priority. The safest and surest way to verify a patients identity is to check the identification band on his wrist. In the therapeutic environment, the patients safety is the primary concern. Fluid oscillation in the tubing of a chest drainage system indicates that the system is working properly. The nurse should place a patient who has a Sengstaken-Blakemore tube in semi-Fowler position. The nurse can elicit Trousseaus sign by occluding the brachial or radial artery. Hand and finger spasms that occur during occlusion indicate Trousseaus sign and suggest hypocalcemia. For blood transfusion in an adult, the appropriate needle size is 16 to 20G. Intractable pain is pain that incapacitates a patient and cant be relieved by drugs. In an emergency, consent for treatment can be obtained by fax, telephone, or other telegraphic means. Decibel is the unit of measurement of sound. Informed consent is required for any invasive procedure. A patient who cant write his name to give consent for treatment must make an X in the presence of two witnesses, such as a nurse, priest, or physician. The Z-track I.M. injection technique seals the drug deep into the muscle, thereby minimizing skin irritation and staining. It requires a needle thats 1" (2.5 cm) or longer. In the event of fire, the acronym most often used is RACE. (R) Remove the patient. (A) Activate the alarm. (C) Attempt to contain the fire by closing the door. (E) Extinguish the fire if it can be done safely. A registered nurse should assign a licensed vocational nurse or licensed practical nurse to perform bedside care, such as suctioning and drug administration. If a patient cant void, the first nursing action should be bladder palpation to assess for bladder distention. The patient who uses a cane should carry it on the unaffected side and advance it at the same time as the affected extremity. To fit a supine patient for crutches, the nurse should measure from the axilla to the sole and add 2" (5 cm) to that measurement. Assessment begins with the nurses first encounter with the patient and continues throughout the patients stay. The nurse obtains assessment data through the health history, physical examination, and review of diagnostic studies. The appropriate needle size for insulin injection is 25G and 5/8" long. Residual urine is urine that remains in the bladder after voiding. The amount of residual urine is normally 50 to 100 ml. The five stages of the nursing process are assessment, nursing diagnosis, planning, implementation, and evaluation. Assessment is the stage of the nursing process in which the nurse continuously collects data to identify a patients actual and potential health needs. Nursing diagnosis is the stage of the nursing process in which the nurse makes a clinical judgment about individual, family, or community responses to actual or potential health problems or life processes. Planning is the stage of the nursing process in which the nurse assigns priorities to nursing diagnoses, defines short-term and longterm goals and expected outcomes, and establishes the nursing care plan. Implementation is the stage of the nursing process in which the nurse puts the nursing care plan into action, delegates specific nursing interventions to members of the nursing team, and charts patient responses to nursing interventions. Evaluation is the stage of the nursing process in which the nurse compares objective and subjective data with the outcome criteria and, if needed, modifies the nursing care plan. Before administering any as needed pain medication, the nurse should ask the patient to indicate the location of the pain. Jehovahs Witnesses believe that they shouldnt receive blood components donated by other people. To test visual acuity, the nurse should ask the patient to cover each eye separately and to read the eye chart with glasses and without, as appropriate. When providing oral care for an unconscious patient, to minimize the risk of aspiration, the nurse should position the patient on the side. During assessment of distance vision, the patient should stand 20 (6.1 m) from the chart. For a geriatric patient or one who is extremely ill, the ideal room temperature is 66 to 76 F (18.8 to 24.4 C). Normal room humidity is 30% to 60%. Hand washing is the single best method of limiting the spread of microorganisms. Once gloves are removed after routine contact with a patient, hands should be washed for 10 to 15 seconds. To perform catheterization, the nurse should place a woman in the dorsal recumbent position. A positive Homans sign may indicate thrombophlebitis.
Electrolytes in a solution are measured in milliequivalents per liter (mEq/L). A milliequivalent is the number of milligrams per 100 milliliters of a solution. Metabolism occurs in two phases: anabolism (the constructive phase) and catabolism (the destructive phase). The basal metabolic rate is the amount of energy needed to maintain essential body functions. Its measured when the patient is awake and resting, hasnt eaten for 14 to 18 hours, and is in a comfortable, warm environment. The basal metabolic rate is expressed in calories consumed per hour per kilogram of body weight. Dietary fiber (roughage), which is derived from cellulose, supplies bulk, maintains intestinal motility, and helps to establish regular bowel habits. Alcohol is metabolized primarily in the liver. Smaller amounts are metabolized by the kidneys and lungs. Petechiae are tiny, round, purplish red spots that appear on the skin and mucous membranes as a result of intradermal or submucosal hemorrhage. Purpura is a purple discoloration of the skin thats caused by blood extravasation. According to the standard precautions recommended by the Centers for Disease Control and Prevention, the nurse shouldnt recap needles after use. Most needle sticks result from missed needle recapping. The nurse administers a drug by I.V. push by using a needle and syringe to deliver the dose directly into a vein, I.V. tubing, or a catheter. When changing the ties on a tracheostomy tube, the nurse should leave the old ties in place until the new ones are applied. A nurse should have assistance when changing the ties on a tracheostomy tube. A filter is always used for blood transfusions. A four-point (quad) cane is indicated when a patient needs more stability than a regular cane can provide. A good way to begin a patient interview is to ask, What made you seek medical help? When caring for any patient, the nurse should follow standard precautions for handling blood and body fluids. Potassium (K+) is the most abundant cation in intracellular fluid. In the four-point, or alternating, gait, the patient first moves the right crutch followed by the left foot and then the left crutch followed by the right foot. In the three-point gait, the patient moves two crutches and the affected leg simultaneously and then moves the unaffected leg. In the two-point gait, the patient moves the right leg and the left crutch simultaneously and then moves the left leg and the right crutch simultaneously. The vitamin B complex, the water-soluble vitamins that are essential for metabolism, include thiamine (B1), riboflavin (B2), niacin (B3), pyridoxine (B6), and cyanocobalamin (B12). When being weighed, an adult patient should be lightly dressed and shoeless. Before taking an adults temperature orally, the nurse should ensure that the patient hasnt smoked or consumed hot or cold substances in the previous 15 minutes. The nurse shouldnt take an adults temperature rectally if the patient has a cardiac disorder, anal lesions, or bleeding hemorrhoids or has recently undergone rectal surgery. In a patient who has a cardiac disorder, measuring temperature rectally may stimulate a vagal response and lead to vasodilation and decreased cardiac output. When recording pulse amplitude and rhythm, the nurse should use these descriptive measures: +3, bounding pulse (readily palpable and forceful); +2, normal pulse (easily palpable); +1, thready or weak pulse (difficult to detect); and 0, absent pulse (not detectable). The intraoperative period begins when a patient is transferred to the operating room bed and ends when the patient is admitted to the postanesthesia care unit. On the morning of surgery, the nurse should ensure that the informed consent form has been signed; that the patient hasnt taken anything by mouth since midnight, has taken a shower with antimicrobial soap, has had mouth care (without swallowing the water), has removed common jewelry, and has received preoperative medication as prescribed; and that vital signs have been taken and recorded. Artificial limbs and other prostheses are usually removed. Comfort measures, such as positioning the patient, rubbing the patients back, and providing a restful environment, may decrease the patients need for analgesics or may enhance their effectiveness. A drug has three names: generic name, which is used in official publications; trade, or brand, name (such as Tylenol), which is selected by the drug company; and chemical name, which describes the drugs chemical composition. To avoid staining the teeth, the patient should take a liquid iron preparation through a straw. The nurse should use the Z-track method to administer an I.M. injection of iron dextran (Imferon). An organism may enter the body through the nose, mouth, rectum, urinary or reproductive tract, or skin. In descending order, the levels of consciousness are alertness, lethargy, stupor, light coma, and deep coma. To turn a patient by logrolling, the nurse folds the patients arms across the chest; extends the patients legs and inserts a pillow between them, if needed; places a draw sheet under the patient; and turns the patient by slowly and gently pulling on the draw sheet. The diaphragm of the stethoscope is used to hear high-pitched sounds, such as breath sounds.
A slight difference in blood pressure (5 to 10 mm Hg) between the right and the left arms is normal. The nurse should place the blood pressure cuff 1" (2.5 cm) above the antecubital fossa. When instilling ophthalmic ointments, the nurse should waste the first bead of ointment and then apply the ointment from the inner canthus to the outer canthus. The nurse should use a leg cuff to measure blood pressure in an obese patient. If a blood pressure cuff is applied too loosely, the reading will be falsely elevated. Ptosis is drooping of the eyelid. A tilt table is useful for a patient with a spinal cord injury, orthostatic hypotension, or brain damage because it can move the patient gradually from a horizontal to a vertical (upright) position. To perform venipuncture with the least injury to the vessel, the nurse should turn the bevel upward when the vessels lumen is larger than the needle and turn it downward when the lumen is only slightly larger than the needle. To move a patient to the edge of the bed for transfer, the nurse should follow these steps: Move the patients head and shoulders toward the edge of the bed. Move the patients feet and legs to the edge of the bed (crescent position). Place both arms well under the patients hips, and straighten the back while moving the patient toward the edge of the bed. When being measured for crutches, a patient should wear shoes. The nurse should attach a restraint to the part of the bed frame that moves with the head, not to the mattress or side rails. The mist in a mist tent should never become so dense that it obscures clear visualization of the patients respiratory pattern. To administer heparin subcutaneously, the nurse should follow these steps: Clean, but dont rub, the site with alcohol. Stretch the skin taut or pick up a well-defined skin fold. Hold the shaft of the needle in a dart position. Insert the needle into the skin at a right (90-degree) angle. Firmly depress the plunger, but dont aspirate. Leave the needle in place for 10 seconds. Withdraw the needle gently at the angle of insertion. Apply pressure to the injection site with an alcohol pad. For a sigmoidoscopy, the nurse should place the patient in the knee-chest position or Sims position, depending on the physicians preference. Maslows hierarchy of needs must be met in the following order: physiologic (oxygen, food, water, sex, rest, and comfort), safety and security, love and belonging, self-esteem and recognition, and self-actualization. When caring for a patient who has a nasogastric tube, the nurse should apply a water-soluble lubricant to the nostril to prevent soreness. During gastric lavage, a nasogastric tube is inserted, the stomach is flushed, and ingested substances are removed through the tube. In documenting drainage on a surgical dressing, the nurse should include the size, color, and consistency of the drainage (for example, 10 mm of brown mucoid drainage noted on dressing). To elicit Babinskis reflex, the nurse strokes the sole of the patients foot with a moderately sharp object, such as a thumbnail. A positive Babinskis reflex is shown by dorsiflexion of the great toe and fanning out of the other toes. When assessing a patient for bladder distention, the nurse should check the contour of the lower abdomen for a rounded mass above the symphysis pubis. The best way to prevent pressure ulcers is to reposition the bedridden patient at least every 2 hours. Antiembolism stockings decompress the superficial blood vessels, reducing the risk of thrombus formation. In adults, the most convenient veins for venipuncture are the basilic and median cubital veins in the antecubital space. Two to three hours before beginning a tube feeding, the nurse should aspirate the patients stomach contents to verify that gastric emptying is adequate. People with type O blood are considered universal donors. People with type AB blood are considered universal recipients. Hertz (Hz) is the unit of measurement of sound frequency. Hearing protection is required when the sound intensity exceeds 84 dB. Double hearing protection is required if it exceeds 104 dB. Prothrombin, a clotting factor, is produced in the liver. If a patient is menstruating when a urine sample is collected, the nurse should note this on the laboratory request. During lumbar puncture, the nurse must note the initial intracranial pressure and the color of the cerebrospinal fluid. If a patient cant cough to provide a sputum sample for culture, a heated aerosol treatment can be used to help to obtain a sample. If eye ointment and eyedrops must be instilled in the same eye, the eyedrops should be instilled first. When leaving an isolation room, the nurse should remove her gloves before her mask because fewer pathogens are on the mask. Skeletal traction, which is applied to a bone with wire pins or tongs, is the most effective means of traction. The total parenteral nutrition solution should be stored in a refrigerator and removed 30 to 60 minutes before use. Delivery of a chilled solution can cause pain, hypothermia, venous spasm, and venous constriction. Drugs arent routinely injected intramuscularly into edematous tissue because they may not be absorbed. When caring for a comatose patient, the nurse should explain each action to the patient in a normal voice. Dentures should be cleaned in a sink thats lined with a washcloth. A patient should void within 8 hours after surgery.
An EEG identifies normal and abnormal brain waves. Samples of feces for ova and parasite tests should be delivered to the laboratory without delay and without refrigeration. The autonomic nervous system regulates the cardiovascular and respiratory systems. When providing tracheostomy care, the nurse should insert the catheter gently into the tracheostomy tube. When withdrawing the catheter, the nurse should apply intermittent suction for no more than 15 seconds and use a slight twisting motion. A low-residue diet includes such foods as roasted chicken, rice, and pasta. A rectal tube shouldnt be inserted for longer than 20 minutes because it can irritate the rectal mucosa and cause loss of sphincter control. A patients bed bath should proceed in this order: face, neck, arms, hands, chest, abdomen, back, legs, perineum. To prevent injury when lifting and moving a patient, the nurse should primarily use the upper leg muscles. Patient preparation for cholecystography includes ingestion of a contrast medium and a low-fat evening meal. While an occupied bed is being changed, the patient should be covered with a bath blanket to promote warmth and prevent exposure. Anticipatory grief is mourning that occurs for an extended time when the patient realizes that death is inevitable. The following foods can alter the color of the feces: beets (red), cocoa (dark red or brown), licorice (black), spinach (green), and meat protein (dark brown). When preparing for a skull X-ray, the patient should remove all jewelry and dentures. The fight-or-flight response is a sympathetic nervous system response. Bronchovesicular breath sounds in peripheral lung fields are abnormal and suggest pneumonia. Wheezing is an abnormal, high-pitched breath sound thats accentuated on expiration. Wax or a foreign body in the ear should be flushed out gently by irrigation with warm saline solution. If a patient complains that his hearing aid is not working, the nurse should check the switch first to see if its turned on and then check the batteries. The nurse should grade hyperactive biceps and triceps reflexes as +4. If two eye medications are prescribed for twice-daily instillation, they should be administered 5 minutes apart. In a postoperative patient, forcing fluids helps prevent constipation. A nurse must provide care in accordance with standards of care established by the American Nurses Association, state regulations, and facility policy. The kilocalorie (kcal) is a unit of energy measurement that represents the amount of heat needed to raise the temperature of 1 kilogram of water 1 C. As nutrients move through the body, they undergo ingestion, digestion, absorption, transport, cell metabolism, and excretion. The body metabolizes alcohol at a fixed rate, regardless of serum concentration. In an alcoholic beverage, proof reflects the percentage of alcohol multiplied by 2. For example, a 100-proof beverage contains 50% alcohol. A living will is a witnessed document that states a patients desire for certain types of care and treatment. These decisions are based on the patients wishes and views on quality of life. The nurse should flush a peripheral heparin lock every 8 hours (if it wasnt used during the previous 8 hours) and as needed with normal saline solution to maintain patency. Quality assurance is a method of determining whether nursing actions and practices meet established standards. The five rights of medication administration are the right patient, right drug, right dose, right route of administration, and right time. The evaluation phase of the nursing process is to determine whether nursing interventions have enabled the patient to meet the desired goals. Outside of the hospital setting, only the sublingual and translingual forms of nitroglycerin should be used to relieve acute anginal attacks. The implementation phase of the nursing process involves recording the patients response to the nursing plan, putting the nursing plan into action, delegating specific nursing interventions, and coordinating the patients activities. The Patients Bill of Rights offers patients guidance and protection by stating the responsibilities of the hospital and its staff toward patients and their families during hospitalization. To minimize omission and distortion of facts, the nurse should record information as soon as its gathered. When assessing a patients health history, the nurse should record the current illness chronologically, beginning with the onset of the problem and continuing to the present. When assessing a patients health history, the nurse should record the current illness chronologically, beginning with the onset of the problem and continuing to the present. A nurse shouldnt give false assurance to a patient. After receiving preoperative medication, a patient isnt competent to sign an informed consent form. When lifting a patient, a nurse uses the weight of her body instead of the strength in her arms.
A nurse may clarify a physicians explanation about an operation or a procedure to a patient, but must refer questions about informed consent to the physician. When obtaining a health history from an acutely ill or agitated patient, the nurse should limit questions to those that provide necessary information. If a chest drainage system line is broken or interrupted, the nurse should clamp the tube immediately. The nurse shouldnt use her thumb to take a patients pulse rate because the thumb has a pulse that may be confused with the patients pulse. An inspiration and an expiration count as one respiration. Eupnea is normal respiration. During blood pressure measurement, the patient should rest the arm against a surface. Using muscle strength to hold up the arm may raise the blood pressure. Major, unalterable risk factors for coronary artery disease include heredity, sex, race, and age. Inspection is the most frequently used assessment technique. Family members of an elderly person in a long-term care facility should transfer some personal items (such as photographs, a favorite chair, and knickknacks) to the persons room to provide a comfortable atmosphere. Pulsus alternans is a regular pulse rhythm with alternating weak and strong beats. It occurs in ventricular enlargement because the stroke volume varies with each heartbeat. The upper respiratory tract warms and humidifies inspired air and plays a role in taste, smell, and mastication. Signs of accessory muscle use include shoulder elevation, intercostal muscle retraction, and scalene and sternocleidomastoid muscle use during respiration. When patients use axillary crutches, their palms should bear the brunt of the weight. Activities of daily living include eating, bathing, dressing, grooming, toileting, and interacting socially. Normal gait has two phases: the stance phase, in which the patients foot rests on the ground, and the swing phase, in which the patients foot moves forward. The phases of mitosis are prophase, metaphase, anaphase, and telophase. The nurse should follow standard precautions in the routine care of all patients. The nurse should use the bell of the stethoscope to listen for venous hums and cardiac murmurs. The nurse can assess a patients general knowledge by asking questions such as Who is the president of the United States? Cold packs are applied for the first 20 to 48 hours after an injury; then heat is applied. During cold application, the pack is applied for 20 minutes and then removed for 10 to 15 minutes to prevent reflex dilation (rebound phenomenon) and frostbite injury. The pons is located above the medulla and consists of white matter (sensory and motor tracts) and gray matter (reflex centers). The autonomic nervous system controls the smooth muscles. A correctly written patient goal expresses the desired patient behavior, criteria for measurement, time frame for achievement, and conditions under which the behavior will occur. Its developed in collaboration with the patient. Percussion causes five basic notes: tympany (loud intensity, as heard over a gastric air bubble or puffed out cheek), hyperresonance (very loud, as heard over an emphysematous lung), resonance (loud, as heard over a normal lung), dullness (medium intensity, as heard over the liver or other solid organ), and flatness (soft, as heard over the thigh). The optic disk is yellowish pink and circular, with a distinct border. A primary disability is caused by a pathologic process. A secondary disability is caused by inactivity. Nurses are commonly held liable for failing to keep an accurate count of sponges and other devices during surgery. The best dietary sources of vitamin B6 are liver, kidney, pork, soybeans, corn, and whole-grain cereals. Iron-rich foods, such as organ meats, nuts, legumes, dried fruit, green leafy vegetables, eggs, and whole grains, commonly have a low water content. Collaboration is joint communication and decision making between nurses and physicians. Its designed to meet patients needs by integrating the care regimens of both professions into one comprehensive approach. Bradycardia is a heart rate of fewer than 60 beats/minute. A nursing diagnosis is a statement of a patients actual or potential health problem that can be resolved, diminished, or otherwise changed by nursing interventions. During the assessment phase of the nursing process, the nurse collects and analyzes three types of data: health history, physical examination, and laboratory and diagnostic test data. The patients health history consists primarily of subjective data, information thats supplied by the patient. The physical examination includes objective data obtained by inspection, palpation, percussion, and auscultation. When documenting patient care, the nurse should write legibly, use only standard abbreviations, and sign each entry. The nurse should never destroy or attempt to obliterate documentation or leave vacant lines. Factors that affect body temperature include time of day, age, physical activity, phase of menstrual cycle, and pregnancy.
The most accessible and commonly used artery for measuring a patients pulse rate is the radial artery. To take the pulse rate, the artery is compressed against the radius. In a resting adult, the normal pulse rate is 60 to 100 beats/minute. The rate is slightly faster in women than in men and much faster in children than in adults. Laboratory test results are an objective form of assessment data. The measurement systems most commonly used in clinical practice are the metric system, apothecaries system, and household system. Before signing an informed consent form, the patient should know whether other treatment options are available and should understand what will occur during the preoperative, intraoperative, and postoperative phases; the risks involved; and the possible complications. The patient should also have a general idea of the time required from surgery to recovery. In addition, he should have an opportunity to ask questions. A patient must sign a separate informed consent form for each procedure. During percussion, the nurse uses quick, sharp tapping of the fingers or hands against body surfaces to produce sounds. This procedure is done to determine the size, shape, position, and density of underlying organs and tissues; elicit tenderness; or assess reflexes. Ballottement is a form of light palpation involving gentle, repetitive bouncing of tissues against the hand and feeling their rebound. A foot cradle keeps bed linen off the patients feet to prevent skin irritation and breakdown, especially in a patient who has peripheral vascular disease or neuropathy. Gastric lavage is flushing of the stomach and removal of ingested substances through a nasogastric tube. Its used to treat poisoning or drug overdose. During the evaluation step of the nursing process, the nurse assesses the patients response to therapy. Bruits commonly indicate life- or limb-threatening vascular disease. O.U. means each eye. O.D. is the right eye, and O.S. is the left eye. To remove a patients artificial eye, the nurse depresses the lower lid. The nurse should use a warm saline solution to clean an artificial eye. A thready pulse is very fine and scarcely perceptible. Axillary temperature is usually 1 F lower than oral temperature. After suctioning a tracheostomy tube, the nurse must document the color, amount, consistency, and odor of secretions. On a drug prescription, the abbreviation p.c. means that the drug should be administered after meals. After bladder irrigation, the nurse should document the amount, color, and clarity of the urine and the presence of clots or sediment. After bladder irrigation, the nurse should document the amount, color, and clarity of the urine and the presence of clots or sediment. Laws regarding patient self-determination vary from state to state. Therefore, the nurse must be familiar with the laws of the state in which she works. Gauge is the inside diameter of a needle: the smaller the gauge, the larger the diameter. An adult normally has 32 permanent teeth. After turning a patient, the nurse should document the position used, the time that the patient was turned, and the findings of skin assessment. PERRLA is an abbreviation for normal pupil assessment findings: pupils equal, round, and reactive to light with accommodation. When percussing a patients chest for postural drainage, the nurses hands should be cupped. When measuring a patients pulse, the nurse should assess its rate, rhythm, quality, and strength. Before transferring a patient from a bed to a wheelchair, the nurse should push the wheelchairs footrests to the sides and lock its wheels. When assessing respirations, the nurse should document their rate, rhythm, depth, and quality. For a subcutaneous injection, the nurse should use a 5/8" 25G needle. The notation AA & O 3 indicates that the patient is awake, alert, and oriented to person (knows who he is), place (knows where he is), and time (knows the date and time). Fluid intake includes all fluids taken by mouth, including foods that are liquid at room temperature, such as gelatin, custard, and ice cream; I.V. fluids; and fluids administered in feeding tubes. Fluid output includes urine, vomitus, and drainage (such as from a nasogastric tube or from a wound) as well as blood loss, diarrhea or feces, and perspiration. After administering an intradermal injection, the nurse shouldnt massage the area because massage can irritate the site and interfere with results. When administering an intradermal injection, the nurse should hold the syringe almost flat against the patients skin (at about a 15degree angle), with the bevel up. To obtain an accurate blood pressure, the nurse should inflate the manometer to 20 to 30 mm Hg above the disappearance of the radial pulse before releasing the cuff pressure.
The nurse should count an irregular pulse for 1 full minute. A patient who is vomiting while lying down should be placed in a lateral position to prevent aspiration of vomitus. Prophylaxis is disease prevention. Body alignment is achieved when body parts are in proper relation to their natural position. Trust is the foundation of a nurse-patient relationship. Blood pressure is the force exerted by the circulating volume of blood on the arterial walls. Malpractice is a professionals wrongful conduct, improper discharge of duties, or failure to meet standards of care that causes harm to another. As a general rule, nurses cant refuse a patient care assignment; however, in most states, they may refuse to participate in abortions. A nurse can be found negligent if a patient is injured because the nurse failed to perform a duty that a reasonable and prudent person would perform or because the nurse performed an act that a reasonable and prudent person wouldnt perform. States have enacted Good Samaritan laws to encourage professionals to provide medical assistance at the scene of an accident without fear of a lawsuit arising from the assistance. These laws dont apply to care provided in a health care facility. A physician should sign verbal and telephone orders within the time established by facility policy, usually 24 hours. A competent adult has the right to refuse lifesaving medical treatment; however, the individual should be fully informed of the consequences of his refusal. Although a patients health record, or chart, is the health care facilitys physical property, its contents belong to the patient. Before a patients health record can be released to a third party, the patient or the patients legal guardian must give written consent. Under the Controlled Substances Act, every dose of a controlled drug thats dispensed by the pharmacy must be accounted for, whether the dose was administered to a patient or discarded accidentally. A nurse cant perform duties that violate a rule or regulation established by a state licensing board, even if they are authorized by a health care facility or physician. To minimize interruptions during a patient interview, the nurse should select a private room, preferably one with a door that can be closed. In categorizing nursing diagnoses, the nurse addresses life-threatening problems first, followed by potentially life-threatening concerns. The major components of a nursing care plan are outcome criteria (patient goals) and nursing interventions. Standing orders, or protocols, establish guidelines for treating a specific disease or set of symptoms. In assessing a patients heart, the nurse normally finds the point of maximal impulse at the fifth intercostal space, near the apex. The S1 heard on auscultation is caused by closure of the mitral and tricuspid valves. To maintain package sterility, the nurse should open a wrappers top flap away from the body, open each side flap by touching only the outer part of the wrapper, and open the final flap by grasping the turned-down corner and pulling it toward the body. The nurse shouldnt dry a patients ear canal or remove wax with a cotton-tipped applicator because it may force cerumen against the tympanic membrane. A patients identification bracelet should remain in place until the patient has been discharged from the health care facility and has left the premises. The Controlled Substances Act designated five categories, or schedules, that classify controlled drugs according to their abuse potential. Schedule I drugs, such as heroin, have a high abuse potential and have no currently accepted medical use in the United States. Schedule II drugs, such as morphine, opium, and meperidine (Demerol), have a high abuse potential, but currently have accepted medical uses. Their use may lead to physical or psychological dependence. Schedule III drugs, such as paregoric and butabarbital (Butisol), have a lower abuse potential than Schedule I or II drugs. Abuse of Schedule III drugs may lead to moderate or low physical or psychological dependence, or both. Schedule IV drugs, such as chloral hydrate, have a low abuse potential compared with Schedule III drugs. Schedule V drugs, such as cough syrups that contain codeine, have the lowest abuse potential of the controlled substances. Activities of daily living are actions that the patient must perform every day to provide self-care and to interact with society. Testing of the six cardinal fields of gaze evaluates the function of all extraocular muscles and cranial nerves III, IV, and VI. The six types of heart murmurs are graded from 1 to 6. A grade 6 heart murmur can be heard with the stethoscope slightly raised from the chest. The most important goal to include in a care plan is the patients goal. Fruits are high in fiber and low in protein, and should be omitted from a low-residue diet. The nurse should use an objective scale to assess and quantify pain. Postoperative pain varies greatly among individuals. Postmortem care includes cleaning and preparing the deceased patient for family viewing, arranging transportation to the morgue or funeral home, and determining the disposition of belongings. The nurse should provide honest answers to the patients questions.
Milk shouldnt be included in a clear liquid diet. When caring for an infant, a child, or a confused patient, consistency in nursing personnel is paramount. The hypothalamus secretes vasopressin and oxytocin, which are stored in the pituitary gland. The three membranes that enclose the brain and spinal cord are the dura mater, pia mater, and arachnoid. A nasogastric tube is used to remove fluid and gas from the small intestine preoperatively or postoperatively. Psychologists, physical therapists, and chiropractors arent authorized to write prescriptions for drugs. The area around a stoma is cleaned with mild soap and water. Vegetables have a high fiber content. The nurse should use a tuberculin syringe to administer a subcutaneous injection of less than 1 ml. For adults, subcutaneous injections require a 25G 1" needle; for infants, children, elderly, or very thin patients, they require a 25G to 27G " needle. Before administering a drug, the nurse should identify the patient by checking the identification band and asking the patient to state his name. To clean the skin before an injection, the nurse uses a sterile alcohol swab to wipe from the center of the site outward in a circular motion. The nurse should inject heparin deep into subcutaneous tissue at a 90-degree angle (perpendicular to the skin) to prevent skin irritation. If blood is aspirated into the syringe before an I.M. injection, the nurse should withdraw the needle, prepare another syringe, and repeat the procedure. The nurse shouldnt cut the patients hair without written consent from the patient or an appropriate relative. If bleeding occurs after an injection, the nurse should apply pressure until the bleeding stops. If bruising occurs, the nurse should monitor the site for an enlarging hematoma. When providing hair and scalp care, the nurse should begin combing at the end of the hair and work toward the head. The frequency of patient hair care depends on the length and texture of the hair, the duration of hospitalization, and the patients condition. Proper function of a hearing aid requires careful handling during insertion and removal, regular cleaning of the ear piece to prevent wax buildup, and prompt replacement of dead batteries. The hearing aid thats marked with a blue dot is for the left ear; the one with a red dot is for the right ear. A hearing aid shouldnt be exposed to heat or humidity and shouldnt be immersed in water. The nurse should instruct the patient to avoid using hair spray while wearing a hearing aid. The five branches of pharmacology are pharmacokinetics, pharmacodynamics, pharmacotherapeutics, toxicology, and pharmacognosy. The nurse should remove heel protectors every 8 hours to inspect the foot for signs of skin breakdown. Heat is applied to promote vasodilation, which reduces pain caused by inflammation. A sutured surgical incision is an example of healing by first intention (healing directly, without granulation). Healing by secondary intention (healing by granulation) is closure of the wound when granulation tissue fills the defect and allows reepithelialization to occur, beginning at the wound edges and continuing to the center, until the entire wound is covered. Keloid formation is an abnormality in healing thats characterized by overgrowth of scar tissue at the wound site. The nurse should administer procaine penicillin by deep I.M. injection in the upper outer portion of the buttocks in the adult or in the midlateral thigh in the child. The nurse shouldnt massage the injection site. An ascending colostomy drains fluid feces. A descending colostomy drains solid fecal matter. A folded towel (scrotal bridge) can provide scrotal support for the patient with scrotal edema caused by vasectomy, epididymitis, or orchitis. When giving an injection to a patient who has a bleeding disorder, the nurse should use a small-gauge needle and apply pressure to the site for 5 minutes after the injection. Platelets are the smallest and most fragile formed element of the blood and are essential for coagulation. To insert a nasogastric tube, the nurse instructs the patient to tilt the head back slightly and then inserts the tube. When the nurse feels the tube curving at the pharynx, the nurse should tell the patient to tilt the head forward to close the trachea and open the esophagus by swallowing. (Sips of water can facilitate this action.) Families with loved ones in intensive care units report that their four most important needs are to have their questions answered honestly, to be assured that the best possible care is being provided, to know the patients prognosis, and to feel that there is hope of recovery. Double-bind communication occurs when the verbal message contradicts the nonverbal message and the receiver is unsure of which message to respond to. A nonjudgmental attitude displayed by a nurse shows that she neither approves nor disapproves of the patient. Target symptoms are those that the patient finds most distressing.
A patient should be advised to take aspirin on an empty stomach, with a full glass of water, and should avoid acidic foods such as coffee, citrus fruits, and cola. For every patient problem, there is a nursing diagnosis; for every nursing diagnosis, there is a goal; and for every goal, there are interventions designed to make the goal a reality. The keys to answering examination questions correctly are identifying the problem presented, formulating a goal for the problem, and selecting the intervention from the choices provided that will enable the patient to reach that goal. Fidelity means loyalty and can be shown as a commitment to the profession of nursing and to the patient. Administering an I.M. injection against the patients will and without legal authority is battery. An example of a third-party payer is an insurance company. The formula for calculating the drops per minute for an I.V. infusion is as follows: (volume to be infused drip factor) time in minutes = drops/minute On-call medication should be given within 5 minutes of the call. Usually, the best method to determine a patients cultural or spiritual needs is to ask him. An incident report or unusual occurrence report isnt part of a patients record, but is an in-house document thats used for the purpose of correcting the problem. Critical pathways are a multidisciplinary guideline for patient care. When prioritizing nursing diagnoses, the following hierarchy should be used: Problems associated with the airway, those concerning breathing, and those related to circulation. The two nursing diagnoses that have the highest priority that the nurse can assign are Ineffective airway clearance and Ineffective breathing pattern. A subjective sign that a sitz bath has been effective is the patients expression of decreased pain or discomfort. For the nursing diagnosis Deficient diversional activity to be valid, the patient must state that hes bored, that he has nothing to do, or words to that effect. The most appropriate nursing diagnosis for an individual who doesnt speak English is Impaired verbal communication related to inability to speak dominant language (English). The family of a patient who has been diagnosed as hearing impaired should be instructed to face the individual when they speak to him. Before instilling medication into the ear of a patient who is up to age 3, the nurse should pull the pinna down and back to straighten the eustachian tube. To prevent injury to the cornea when administering eyedrops, the nurse should waste the first drop and instill the drug in the lower conjunctival sac. After administering eye ointment, the nurse should twist the medication tube to detach the ointment. When the nurse removes gloves and a mask, she should remove the gloves first. They are soiled and are likely to contain pathogens. Crutches should be placed 6" (15.2 cm) in front of the patient and 6" to the side to form a tripod arrangement. Listening is the most effective communication technique. Before teaching any procedure to a patient, the nurse must assess the patients current knowledge and willingness to learn. Process recording is a method of evaluating ones communication effectiveness. When feeding an elderly patient, the nurse should limit high-carbohydrate foods because of the risk of glucose intolerance. When feeding an elderly patient, essential foods should be given first. Passive range of motion maintains joint mobility. Resistive exercises increase muscle mass. Isometric exercises are performed on an extremity thats in a cast. A back rub is an example of the gate-control theory of pain. Anything thats located below the waist is considered unsterile; a sterile field becomes unsterile when it comes in contact with any unsterile item; a sterile field must be monitored continuously; and a border of 1" (2.5 cm) around a sterile field is considered unsterile. A shift to the left is evident when the number of immature cells (bands) in the blood increases to fight an infection. A shift to the right is evident when the number of mature cells in the blood increases, as seen in advanced liver disease and pernicious anemia. Before administering preoperative medication, the nurse should ensure that an informed consent form has been signed and attached to the patients record. A nurse should spend no more than 30 minutes per 8-hour shift providing care to a patient who has a radiation implant. A nurse shouldnt be assigned to care for more than one patient who has a radiation implant. Long-handled forceps and a lead-lined container should be available in the room of a patient who has a radiation implant. Usually, patients who have the same infection and are in strict isolation can share a room. Diseases that require strict isolation include chickenpox, diphtheria, and viral hemorrhagic fevers such as Marburg disease. For the patient who abides by Jewish custom, milk and meat shouldnt be served at the same meal.
Whether the patient can perform a procedure (psychomotor domain of learning) is a better indicator of the effectiveness of patient teaching than whether the patient can simply state the steps involved in the procedure (cognitive domain of learning). According to Erik Erikson, developmental stages are trust versus mistrust (birth to 18 months), autonomy versus shame and doubt (18 months to age 3), initiative versus guilt (ages 3 to 5), industry versus inferiority (ages 5 to 12), identity versus identity diffusion (ages 12 to 18), intimacy versus isolation (ages 18 to 25), generativity versus stagnation (ages 25 to 60), and ego integrity versus despair (older than age 60). When communicating with a hearing impaired patient, the nurse should face him. An appropriate nursing intervention for the spouse of a patient who has a serious incapacitating disease is to help him to mobilize a support system. Hyperpyrexia is extreme elevation in temperature above 106 F (41.1 C). Milk is high in sodium and low in iron. When a patient expresses concern about a health-related issue, before addressing the concern, the nurse should assess the patients level of knowledge. The most effective way to reduce a fever is to administer an antipyretic, which lowers the temperature set point. When a patient is ill, its essential for the members of his family to maintain communication about his health needs. Ethnocentrism is the universal belief that ones way of life is superior to others. When a nurse is communicating with a patient through an interpreter, the nurse should speak to the patient and the interpreter. In accordance with the hot-cold system used by some Mexicans, Puerto Ricans, and other Hispanic and Latino groups, most foods, beverages, herbs, and drugs are described as cold. Prejudice is a hostile attitude toward individuals of a particular group. Discrimination is preferential treatment of individuals of a particular group. Its usually discussed in a negative sense. Increased gastric motility interferes with the absorption of oral drugs. The three phases of the therapeutic relationship are orientation, working, and termination. Patients often exhibit resistive and challenging behaviors in the orientation phase of the therapeutic relationship. Abdominal assessment is performed in the following order: inspection, auscultation, palpation, and percussion. When measuring blood pressure in a neonate, the nurse should select a cuff thats no less than one-half and no more than twothirds the length of the extremity thats used. When administering a drug by Z-track, the nurse shouldnt use the same needle that was used to draw the drug into the syringe because doing so could stain the skin. Sites for intradermal injection include the inner arm, the upper chest, and on the back, under the scapula. When evaluating whether an answer on an examination is correct, the nurse should consider whether the action thats described promotes autonomy (independence), safety, self-esteem, and a sense of belonging. When answering a question on the NCLEX examination, the student should consider the cue (the stimulus for a thought) and the inference (the thought) to determine whether the inference is correct. When in doubt, the nurse should select an answer that indicates the need for further information to eliminate ambiguity. For example, the patient complains of chest pain (the stimulus for the thought) and the nurse infers that the patient is having cardiac pain (the thought). In this case, the nurse hasnt confirmed whether the pain is cardiac. It would be more appropriate to make further assessments. Veracity is truth and is an essential component of a therapeutic relationship between a health care provider and his patient. Beneficence is the duty to do no harm and the duty to do good. Theres an obligation in patient care to do no harm and an equal obligation to assist the patient. Nonmaleficence is the duty to do no harm. Fryes ABCDE cascade provides a framework for prioritizing care by identifying the most important treatment concerns. A = Airway. This category includes everything that affects a patent airway, including a foreign object, fluid from an upper respiratory infection, and edema from trauma or an allergic reaction. B = Breathing. This category includes everything that affects the breathing pattern, including hyperventilation or hypoventilation and abnormal breathing patterns, such as Korsakoffs, Biots, or Cheyne-Stokes respiration. C = Circulation. This category includes everything that affects the circulation, including fluid and electrolyte disturbances and disease processes that affect cardiac output. D = Disease processes. If the patient has no problem with the airway, breathing, or circulation, then the nurse should evaluate the disease processes, giving priority to the disease process that poses the greatest immediate risk. For example, if a patient has terminal cancer and hypoglycemia, hypoglycemia is a more immediate concern. E = Everything else. This category includes such issues as writing an incident report and completing the patient chart. When evaluating needs, this category is never the highest priority. When answering a question on an NCLEX examination, the basic rule is assess before action. The student should evaluate each possible answer carefully. Usually, several answers reflect the implementation phase of nursing and one or two reflect the assessment phase. In this case, the best choice is an assessment response unless a specific course of action is clearly indicated. Rule utilitarianism is known as the greatest good for the greatest number of people theory.
Egalitarian theory emphasizes that equal access to goods and services must be provided to the less fortunate by an affluent society. Active euthanasia is actively helping a person to die. Brain death is irreversible cessation of all brain function. Passive euthanasia is stopping the therapy thats sustaining life. A third-party payer is an insurance company. Utilization review is performed to determine whether the care provided to a patient was appropriate and cost-effective. A value cohort is a group of people who experienced an out-of-the-ordinary event that shaped their values. Voluntary euthanasia is actively helping a patient to die at the patients request. Bananas, citrus fruits, and potatoes are good sources of potassium. Good sources of magnesium include fish, nuts, and grains. Beef, oysters, shrimp, scallops, spinach, beets, and greens are good sources of iron. Intrathecal injection is administering a drug through the spine. When a patient asks a question or makes a statement thats emotionally charged, the nurse should respond to the emotion behind the statement or question rather than to whats being said or asked. The steps of the trajectory-nursing model are as follows: Step 1: Identifying the trajectory phase Step 2: Identifying the problems and establishing goals Step 3: Establishing a plan to meet the goals Step 4: Identifying factors that facilitate or hinder attainment of the goals Step 5: Implementing interventions Step 6: Evaluating the effectiveness of the interventions A Hindu patient is likely to request a vegetarian diet. Pain threshold, or pain sensation, is the initial point at which a patient feels pain. The difference between acute pain and chronic pain is its duration. Referred pain is pain thats felt at a site other than its origin. Alleviating pain by performing a back massage is consistent with the gate control theory. Rombergs test is a test for balance or gait. Pain seems more intense at night because the patient isnt distracted by daily activities. Older patients commonly dont report pain because of fear of treatment, lifestyle changes, or dependency. No pork or pork products are allowed in a Muslim diet. Two goals of Healthy People 2010 are: Help individuals of all ages to increase the quality of life and the number of years of optimal health Eliminate health disparities among different segments of the population. A community nurse is serving as a patients advocate if she tells a malnourished patient to go to a meal program at a local park. If a patient isnt following his treatment plan, the nurse should first ask why. Falls are the leading cause of injury in elderly people. Primary prevention is true prevention. Examples are immunizations, weight control, and smoking cessation. Secondary prevention is early detection. Examples include purified protein derivative (PPD), breast self-examination, testicular selfexamination, and chest X-ray. Tertiary prevention is treatment to prevent long-term complications. A patient indicates that hes coming to terms with having a chronic disease when he says, Im never going to get any better. On noticing religious artifacts and literature on a patients night stand, a culturally aware nurse would ask the patient the meaning of the items. A Mexican patient may request the intervention of a curandero, or faith healer, who involves the family in healing the patient. In an infant, the normal hemoglobin value is 12 g/dl. The nitrogen balance estimates the difference between the intake and use of protein. Most of the absorption of water occurs in the large intestine. Most nutrients are absorbed in the small intestine. When assessing a patients eating habits, the nurse should ask, What have you eaten in the last 24 hours? A vegan diet should include an abundant supply of fiber. A hypotonic enema softens the feces, distends the colon, and stimulates peristalsis. First-morning urine provides the best sample to measure glucose, ketone, pH, and specific gravity values.
To induce sleep, the first step is to minimize environmental stimuli. Before moving a patient, the nurse should assess the patients physical abilities and ability to understand instructions as well as the amount of strength required to move the patient. To lose 1 lb (0.5 kg) in 1 week, the patient must decrease his weekly intake by 3,500 calories (approximately 500 calories daily). To lose 2 lb (1 kg) in 1 week, the patient must decrease his weekly caloric intake by 7,000 calories (approximately 1,000 calories daily). To avoid shearing force injury, a patient who is completely immobile is lifted on a sheet. To insert a catheter from the nose through the trachea for suction, the nurse should ask the patient to swallow. Vitamin C is needed for collagen production. Only the patient can describe his pain accurately. Cutaneous stimulation creates the release of endorphins that block the transmission of pain stimuli. Patient-controlled analgesia is a safe method to relieve acute pain caused by surgical incision, traumatic injury, labor and delivery, or cancer. An Asian American or European American typically places distance between himself and others when communicating. The patient who believes in a scientific, or biomedical, approach to health is likely to expect a drug, treatment, or surgery to cure illness. Chronic illnesses occur in very young as well as middle-aged and very old people. The trajectory framework for chronic illness states that preferences about daily life activities affect treatment decisions. Exacerbations of chronic disease usually cause the patient to seek treatment and may lead to hospitalization. School health programs provide cost-effective health care for low-income families and those who have no health insurance. Collegiality is the promotion of collaboration, development, and interdependence among members of a profession. A change agent is an individual who recognizes a need for change or is selected to make a change within an established entity, such as a hospital. The patients bill of rights was introduced by the American Hospital Association. Abandonment is premature termination of treatment without the patients permission and without appropriate relief of symptoms. Values clarification is a process that individuals use to prioritize their personal values. Distributive justice is a principle that promotes equal treatment for all. Milk and milk products, poultry, grains, and fish are good sources of phosphate. The best way to prevent falls at night in an oriented, but restless, elderly patient is to raise the side rails. By the end of the orientation phase, the patient should begin to trust the nurse. Falls in the elderly are likely to be caused by poor vision. Barriers to communication include language deficits, sensory deficits, cognitive impairments, structural deficits, and paralysis. The three elements that are necessary for a fire are heat, oxygen, and combustible material. Sebaceous glands lubricate the skin. To check for petechiae in a dark-skinned patient, the nurse should assess the oral mucosa. To put on a sterile glove, the nurse should pick up the first glove at the folded border and adjust the fingers when both gloves are on. To increase patient comfort, the nurse should let the alcohol dry before giving an intramuscular injection. Treatment for a stage 1 ulcer on the heels includes heel protectors. Seventh-Day Adventists are usually vegetarians. Endorphins are morphinelike substances that produce a feeling of well-being. Pain tolerance is the maximum amount and duration of pain that an individual is willing to endure.
ENDOCRINE PRACTICE TEST
1. Nurse Ronn is assessing a client with possible Cushings syndrome. In a client with Cushings syndrome, the nurse would expect to find: a. Hypotension. b. Thick, coarse skin. c. Deposits of adipose tissue in the trunk and dorsocervical area. d. Weight gain in arms and legs. 2. A male client with primary diabetes insipidus is ready for discharge on desmopressin (DDAVP). Which instruction should nurse Lina provide?
a. Administer desmopressin while the suspension is cold. b. Your condition isnt chronic, so you wont need to wear a medical identification bracelet. c. You may not be able to use desmopressin nasally if you have nasal discharge or blockage. d. You wont need to monitor your fluid intake and output after you start taking desmopressin. 3. Nurse Wayne is aware that a positive Chvosteks sign indicate? a. Hypocalcemia b. Hyponatremia c. Hypokalemia d. Hypermagnesemia 4. In a 29-year-old female client who is being successfully treated for Cushings syndrome, nurse Lyzette would expect a decline in: a. Serum glucose level. b. Hair loss. c. Bone mineralization. d. Menstrual flow. 5. A male client has recently undergone surgical removal of a pituitary tumor. Dr. Wong prescribes corticotropin (Acthar), 20 units I.M. q.i.d. as a replacement therapy. What is the mechanism of action of corticotropin? a. It decreases cyclic adenosine monophosphate (cAMP) production and affects the metabolic rate of target organs. b. It interacts with plasma membrane receptors to inhibit enzymatic actions. c. It interacts with plasma membrane receptors to produce enzymatic actions that affect protein, fat, and carbohydrate metabolism. d. It regulates the threshold for water resorption in the kidneys. 6. Capillary glucose monitoring is being performed every 4 hours for a female client diagnosed with diabetic ketoacidosis. Insulin is administered using a scale of regular insulin according to glucose results. At 2 p.m., the client has a capillary glucose level of 250 mg/dl for which he receives 8 U of regular insulin. Nurse Vince should expect the doses: a. Onset to be at 2 p.m. and its peak to be at 3 p.m. b. Onset to be at 2:15 p.m. and its peak to be at 3 p.m. c. Onset to be at 2:30 p.m. and its peak to be at 4 p.m. d. Onset to be at 4 p.m. and its peak to be at 6 p.m. 7. A female client with Cushings syndrome is admitted to the medical-surgical unit. During the admission assessment, nurse Tyzz notes that the client is agitated and irritable, has poor memory, reports loss of appetite, and appears disheveled. These findings are consistent with which problem? a. Depression b. Neuropathy c. Hypoglycemia d. Hyperthyroidism 8. Nurse Ruth is assessing a client after a thyroidectomy. The assessment reveals muscle twitching and tingling, along with numbness in the fingers, toes, and mouth area. The nurse should suspect which complication? a. Tetany b. Hemorrhage c. Thyroid storm d. Laryngeal nerve damage 9. After undergoing a subtotal thyroidectomy, a female client develops hypothyroidism. Dr. Smith prescribes levothyroxine (Levothroid), 25 mcg P.O. daily. For which condition is levothyroxine the preferred agent? a. Primary hypothyroidism b. Graves disease c. Thyrotoxicosis d. Euthyroidism 10. Which of these signs suggests that a male client with the syndrome of inappropriate antidiuretic hormone (SIADH) secretion is experiencing complications? a. Tetanic contractions b. Neck vein distention c. Weight loss d. Polyuria 11. A female client with a history of pheochromocytoma is admitted to the hospital in an acute hypertensive crisis. To reverse hypertensive crisis caused by pheochromocytoma, nurse Lyka expects to administer: a. phentolamine (Regitine). b. methyldopa (Aldomet). c. mannitol (Osmitrol). d. felodipine (Plendil). 12. A male client with a history of hypertension is diagnosed with primary hyperaldosteronism. This diagnosis indicates that the clients hypertension is caused by excessive hormone secretion from which of the following glands? a. Adrenal cortex b. Pancreas
c. Adrenal medulla d. Parathyroid 13. Nurse Troy is aware that the most appropriate for a client with Addisons disease? a. Risk for infection b. Excessive fluid volume c. Urinary retention d. Hypothermia 14. Acarbose (Precose), an alpha-glucosidase inhibitor, is prescribed for a female client with type 2 diabetes mellitus. During discharge planning, nurse Pauleen would be aware of the clients need for additional teaching when the client states: a. If I have hypoglycemia, I should eat some sugar, not dextrose. b. The drug makes my pancreas release more insulin. c. I should never take insulin while Im taking this drug. d. Its best if I take the drug with the first bite of a meal. 15. A female client whose physical findings suggest a hyperpituitary condition undergoes an extensive diagnostic workup. Test results reveal a pituitary tumor, which necessitates a transphenoidal hypophysectomy. The evening before the surgery, nurse Jacob reviews preoperative and postoperative instructions given to the client earlier. Which postoperative instruction should the nurse emphasize? a. You must lie flat for 24 hours after surgery. b. You must avoid coughing, sneezing, and blowing your nose. c. You must restrict your fluid intake. d. You must report ringing in your ears immediately. 16. Dr. Kennedy prescribes glipizide (Glucotrol), an oral antidiabetic agent, for a male client with type 2 diabetes mellitus who has been having trouble controlling the blood glucose level through diet and exercise. Which medication instruction should the nurse provide? a. Be sure to take glipizide 30 minutes before meals. b. Glipizide may cause a low serum sodium level, so make sure you have your sodium level checked monthly. c. You wont need to check your blood glucose level after you start taking glipizide. d. Take glipizide after a meal to prevent heartburn. 17. For a diabetic male client with a foot ulcer, the physician orders bed rest, a wet-to-dry dressing change every shift, and blood glucose monitoring before meals and bedtime. Why are wet-to-dry dressings used for this client? a. They contain exudate and provide a moist wound environment. b. They protect the wound from mechanical trauma and promote healing. c. They debride the wound and promote healing by secondary intention. d. They prevent the entrance of microorganisms and minimize wound discomfort. 18. When instructing the female client diagnosed with hyperparathyroidism about diet, nurse Gina should stress the importance of which of the following? a. Restricting fluids b. Restricting sodium c. Forcing fluids d. Restricting potassium 19. Which nursing diagnosis takes highest priority for a female client with hyperthyroidism? a. Risk for imbalanced nutrition: More than body requirements related to thyroid hormone excess b. Risk for impaired skin integrity related to edema, skin fragility, and poor wound healing c. Body image disturbance related to weight gain and edema d. Imbalanced nutrition: Less than body requirements related to thyroid hormone excess 20. A male client with a tentative diagnosis of hyperosmolar hyperglycemic nonketotic syndrome (HHNS) has a history of type 2 diabetes that is being controlled with an oral diabetic agent, tolazamide (Tolinase). Which of the following is the most important laboratory test for confirming this disorder? a. Serum potassium level b. Serum sodium level c. Arterial blood gas (ABG) values d. Serum osmolarity 21. A male client has just been diagnosed with type 1 diabetes mellitus. When teaching the client and family how diet and exercise affect insulin requirements, Nurse Joy should include which guideline? a. Youll need more insulin when you exercise or increase your food intake. b. Youll need less insulin when you exercise or reduce your food intake. c. Youll need less insulin when you increase your food intake. d. Youll need more insulin when you exercise or decrease your food intake. 22. Nurse Noemi administers glucagon to her diabetic client, then monitors the client for adverse drug reactions and interactions. Which type of drug interacts adversely with glucagon? a. Oral anticoagulants b. Anabolic steroids c. Beta-adrenergic blockers d. Thiazide diuretics
23. Which instruction about insulin administration should nurse Kate give to a client? a. Always follow the same order when drawing the different insulins into the syringe. b. Shake the vials before withdrawing the insulin. c. Store unopened vials of insulin in the freezer at temperatures well below freezing. d. Discard the intermediate-acting insulin if it appears cloudy. 24. Nurse Perry is caring for a female client with type 1 diabetes mellitus who exhibits confusion, light-headedness, and aberrant behavior. The client is still conscious. The nurse should first administer: a. I.M. or subcutaneous glucagon. b. I.V. bolus of dextrose 50%. c. 15 to 20 g of a fast-acting carbohydrate such as orange juice. d. 10 U of fast-acting insulin. 25. For the first 72 hours after thyroidectomy surgery, nurse Jamie would assess the female client for Chvosteks sign and Trousseaus sign because they indicate which of the following? a. Hypocalcemia b. Hypercalcemia c. Hypokalemia d. Hyperkalemia
ANSWER AND RATIONALE 1. Answer C. Because of changes in fat distribution, adipose tissue accumulates in the trunk, face (moonface), and dorsocervical areas (buffalo hump). Hypertension is caused by fluid retention. Skin becomes thin and bruises easily because of a loss of collagen. Muscle wasting causes muscle atrophy and thin extremities. 2. Answer C. Desmopressin may not be absorbed if the intranasal route is compromised. Although diabetes insipidus is treatable, the client should wear medical identification and carry medication at all times to alert medical personnel in an emergency and ensure proper treatment. The client must continue to monitor fluid intake and output and receive adequate fluid replacement. 3. Answer A. Chvosteks sign is elicited by tapping the clients face lightly over the facial nerve, just below the temple. If the clients facial muscles twitch, it indicates hypocalcemia. Hyponatremia is indicated by weight loss, abdominal cramping, muscle weakness, headache, and postural hypotension. Hypokalemia causes paralytic ileus and muscle weakness. Clients with hypermagnesemia exhibit a loss of deep tendon reflexes, coma, or cardiac arrest. 4. Answer A. Hyperglycemia, which develops from glucocorticoid excess, is a manifestation of Cushings syndrome. With successful treatment of the disorder, serum glucose levels decline. Hirsutism is common in Cushings syndrome; therefore, with successful treatment, abnormal hair growth also declines. Osteoporosis occurs in Cushings syndrome; therefore, with successful treatment, bone mineralization increases. Amenorrhea develops in Cushings syndrome. With successful treatment, the client experiences a return of menstrual flow, not a decline in it. 5. Answer C. Corticotropin interacts with plasma membrane receptors to produce enzymatic actions that affect protein, fat, and carbohydrate metabolism. It doesnt decrease cAMP production. The posterior pituitary hormone, antidiuretic hormone, regulates the threshold for water resorption in the kidneys. 6. Answer C. Regular insulin, which is a short-acting insulin, has an onset of 15 to 30 minutes and a peak of 2 to 4 hours. Because the nurse gave the insulin at 2 p.m., the expected onset would be from 2:15 p.m. to 2:30 p.m. and the peak from 4 p.m. to 6 p.m. 7. Answer A. Agitation, irritability, poor memory, loss of appetite, and neglect of ones appearance may signal depression, which is common in clients with Cushings syndrome. Neuropathy affects clients with diabetes mellitus not Cushings syndrome. Although hypoglycemia can cause irritability, it also produces increased appetite, rather than loss of appetite. Hyperthyroidism typically causes such signs as goiter, nervousness, heat intolerance, and weight loss despite increased appetite. 8. Answer A. Tetany may result if the parathyroid glands are excised or damaged during thyroid surgery. Hemorrhage is a potential complication after thyroid surgery but is characterized by tachycardia, hypotension, frequent swallowing, feelings of fullness at the incision site, choking, and bleeding. Thyroid storm is another term for severe hyperthyroidism not a complication of thyroidectomy. Laryngeal nerve damage may occur postoperatively, but its signs include a hoarse voice and, possibly, acute airway obstruction. 9. Answer A. Levothyroxine is the preferred agent to treat primary hypothyroidism and cretinism, although it also may be used to treat secondary hypothyroidism. It is contraindicated in Graves disease and thyrotoxicosis because these conditions are forms of hyperthyroidism. Euthyroidism, a term used to describe normal thyroid function, wouldnt require any thyroid preparation.
10. Answer B. SIADH secretion causes antidiuretic hormone overproduction, which leads to fluid retention. Severe SIADH can cause such complications as vascular fluid overload, signaled by neck vein distention. This syndrome isnt associated with tetanic contractions. It may cause weight gain and fluid retention (secondary to oliguria). 11. Answer A. Pheochromocytoma causes excessive production of epinephrine and norepinephrine, natural catecholamines that raise the blood pressure. Phentolamine, an alpha-adrenergic blocking agent given by I.V. bolus or drip, antagonizes the bodys response to circulating epinephrine and norepinephrine, reducing blood pressure quickly and effectively. Although methyldopa is an antihypertensive agent available in parenteral form, it isnt effective in treating hypertensive emergencies. Mannitol, a diuretic, isnt used to treat hypertensive emergencies. Felodipine, an antihypertensive agent, is available only in extended-release tablets and therefore doesnt reduce blood pressure quickly enough to correct hypertensive crisis. 12. Answer A. Excessive secretion of aldosterone in the adrenal cortex is responsible for the clients hypertension. This hormone acts on the renal tubule, where it promotes reabsorption of sodium and excretion of potassium and hydrogen ions. The pancreas mainly secretes hormones involved in fuel metabolism. The adrenal medulla secretes the catecholamines epinephrine and norepinephrine. The parathyroids secrete parathyroid hormone. 13. Answer A. Addisons disease decreases the production of all adrenal hormones, compromising the bodys normal stress response and increasing the risk of infection. Other appropriate nursing diagnoses for a client with Addisons disease include Deficient fluid volume and Hyperthermia. Urinary retention isnt appropriate because Addisons disease causes polyuria. 14. Answer A. Acarbose delays glucose absorption, so the client should take an oral form of dextrose rather than a product containing table sugar when treating hypoglycemia. The alpha-glucosidase inhibitors work by delaying the carbohydrate digestion and glucose absorption. Its safe to be on a regimen that includes insulin and an alpha-glucosidase inhibitor. The client should take the drug at the start of a meal, not 30 minutes to an hour before. 15. Answer B. After a transsphenoidal hypophysectomy, the client must refrain from coughing, sneezing, and blowing the nose for several days to avoid disturbing the surgical graft used to close the wound. The head of the bed must be elevated, not kept flat, to prevent tension or pressure on the suture line. Within 24 hours after a hypophysectomy, transient diabetes insipidus commonly occurs; this calls for increased, not restricted, fluid intake. Visual, not auditory, changes are a potential complication of hypophysectomy. 16. Answer A. The client should take glipizide twice a day, 30 minutes before a meal, because food decreases its absorption. The drug doesnt cause hyponatremia and therefore doesnt necessitate monthly serum sodium measurement. The client must continue to monitor the blood glucose level during glipizide therapy. 17. Answer C. For this client, wet-to-dry dressings are most appropriate because they clean the foot ulcer by debriding exudate and necrotic tissue, thus promoting healing by secondary intention. Moist, transparent dressings contain exudate and provide a moist wound environment. Hydrocolloid dressings prevent the entrance of microorganisms and minimize wound discomfort. Dry sterile dressings protect the wound from mechanical trauma and promote healing. 18. Answer C. The client should be encouraged to force fluids to prevent renal calculi formation. Sodium should be encouraged to replace losses in urine. Restricting potassium isnt necessary in hyperparathyroidism. 19. Answer D. In the client with hyperthyroidism, excessive thyroid hormone production leads to hypermetabolism and increased nutrient metabolism. These conditions may result in a negative nitrogen balance, increased protein synthesis and breakdown, decreased glucose tolerance, and fat mobilization and depletion. This puts the client at risk for marked nutrient and calorie deficiency, making Imbalanced nutrition: Less than body requirements the most important nursing diagnosis. Options B and C may be appropriate for a client with hypothyroidism, which slows the metabolic rate. 20. Answer D. Serum osmolarity is the most important test for confirming HHNS; its also used to guide treatment strategies and determine evaluation criteria. A client with HHNS typically has a serum osmolarity of more than 350 mOsm/L. Serum potassium, serum sodium, and ABG values are also measured, but they arent as important as serum osmolarity for confirming a diagnosis of HHNS. A client with HHNS typically has hypernatremia and osmotic diuresis. ABG values reveal acidosis, and the potassium level is variable. 21. Answer B. Exercise, reduced food intake, hypothyroidism, and certain medications decrease the insulin requirements. Growth, pregnancy, greater food intake, stress, surgery, infection, illness, increased insulin antibodies, and certain medications increase the insulin requirements. 22. Answer A. As a normal body protein, glucagon only interacts adversely with oral anticoagulants, increasing the anticoagulant effects. It doesnt interact adversely with anabolic steroids, beta-adrenergic blockers, or thiazide diuretics.
23. Answer A. The client should be instructed always to follow the same order when drawing the different insulins into the syringe. Insulin should never be shaken because the resulting froth prevents withdrawal of an accurate dose and may damage the insulin protein molecules. Insulin also should never be frozen because the insulin protein molecules may be damaged. Intermediate-acting insulin is normally cloudy. 24. Answer C. This client is having a hypoglycemic episode. Because the client is conscious, the nurse should first administer a fast-acting carbohydrate, such as orange juice, hard candy, or honey. If the client has lost consciousness, the nurse should administer either I.M. or subcutaneous glucagon or an I.V. bolus of dextrose 50%. The nurse shouldnt administer insulin to a client whos hypoglycemic; this action will further compromise the clients condition. 25. Answer A. The client who has undergone a thyroidectomy is at risk for developing hypocalcemia from inadvertent removal or damage to the parathyroid gland. The client with hypocalcemia will exhibit a positive Chvosteks sign (facial muscle contraction when the facial nerve in front of the ear is tapped) and a positive Trousseaus sign (carpal spasm when a blood pressure cuff is inflated for a few minutes). These signs arent present with hypercalcemia, hypokalemia, or hyperkalemia.
ENDOCRINE PRACTICE TEST 1. An agitated, confused female client arrives in the emergency department. Her history includes type 1 diabetes mellitus, hypertension, and angina pectoris. Assessment reveals pallor, diaphoresis, headache, and intense hunger. A stat blood glucose sample measures 42 mg/dl, and the client is treated for an acute hypoglycemic reaction. After recovery, nurse Lily teaches the client to treat hypoglycemia by ingesting: a. 2 to 5 g of a simple carbohydrate. b. 10 to 15 g of a simple carbohydrate. c. 18 to 20 g of a simple carbohydrate. d. 25 to 30 g of a simple carbohydrate. 2. A female adult client with a history of chronic hyperparathyroidism admits to being noncompliant. Based on initial assessment findings, nurse Julia formulates the nursing diagnosis of Risk for injury. To complete the nursing diagnosis statement for this client, which related-to phrase should the nurse add? a. Related to bone demineralization resulting in pathologic fractures b. Related to exhaustion secondary to an accelerated metabolic rate c. Related to edema and dry skin secondary to fluid infiltration into the interstitial spaces d. Related to tetany secondary to a decreased serum calcium level 3. Nurse John is assigned to care for a postoperative male client who has diabetes mellitus. During the assessment interview, the client reports that hes impotent and says hes concerned about its effect on his marriage. In planning this clients care, the most appropriate intervention would be to: a. Encourage the client to ask questions about personal sexuality. b. Provide time for privacy. c. Provide support for the spouse or significant other. d. Suggest referral to a sex counselor or other appropriate professional. 4. During a class on exercise for diabetic clients, a female client asks the nurse educator how often to exercise. The nurse educator advises the clients to exercise how often to meet the goals of planned exercise? a. At least once a week b. At least three times a week c. At least five times a week d. Every day 5. a. b. c. d. Nurse Oliver should expect a client with hypothyroidism to report which health concerns? Increased appetite and weight loss Puffiness of the face and hands Nervousness and tremors Thyroid gland swelling
6. A female client with hypothyroidism (myxedema) is receiving levothyroxine (Synthroid), 25 mcg P.O. daily. Which finding should nurse Hans recognize as an adverse drug effect? a. Dysuria b. Leg cramps c. Tachycardia d. Blurred vision
7. A 67-year-old male client has been complaining of sleeping more, increased urination, anorexia, weakness, irritability, depression, and bone pain that interferes with her going outdoors. Based on these assessment findings, nurse Richard would suspect which of the following disorders? a. Diabetes mellitus b. Diabetes insipidus c. Hypoparathyroidism d. Hyperparathyroidism 8. a. b. c. d. 9. a. b. c. d. When caring for a male client with diabetes insipidus, nurse Juliet expects to administer: vasopressin (Pitressin Synthetic). furosemide (Lasix). regular insulin. 10% dextrose. The nurse is aware that the following is the most common cause of hyperaldosteronism? Excessive sodium intake A pituitary adenoma Deficient potassium intake An adrenal adenoma
10. A male client with type 1 diabetes mellitus has a highly elevated glycosylated hemoglobin (Hb) test result. In discussing the result with the client, nurse Sharmaine would be most accurate in stating: a. The test needs to be repeated following a 12-hour fast. b. It looks like you arent following the prescribed diabetic diet. c. It tells us about your sugar control for the last 3 months. d. Your insulin regimen needs to be altered significantly. 11. a. b. c. d. Following a unilateral adrenalectomy, nurse Betty would assess for hyperkalemia shown by which of the following? Muscle weakness Tremors Diaphoresis Constipation
12. Nurse Louie is developing a teaching plan for a male client diagnosed with diabetes insipidus. The nurse should include information about which hormone lacking in clients with diabetes insipidus? a. antidiuretic hormone (ADH). b. thyroid-stimulating hormone (TSH). c. follicle-stimulating hormone (FSH). d. luteinizing hormone (LH). 13. Early this morning, a female client had a subtotal thyroidectomy. During evening rounds, nurse Tina assesses the client, who now has nausea, a temperature of 105 F (40.5 C), tachycardia, and extreme restlessness. What is the most likely cause of these signs? a. Diabetic ketoacidosis b. Thyroid crisis c. Hypoglycemia d. Tetany 14. a. b. c. d. For a male client with hyperglycemia, which assessment finding best supports a nursing diagnosis of Deficient fluid volume? Cool, clammy skin Distended neck veins Increased urine osmolarity Decreased serum sodium level
15. When assessing a male client with pheochromocytoma, a tumor of the adrenal medulla that secretes excessive catecholamine, nurse April is most likely to detect: a. a blood pressure of 130/70 mm Hg. b. a blood glucose level of 130 mg/dl. c. bradycardia. d. a blood pressure of 176/88 mm Hg. 16. A male client is admitted for treatment of the syndrome of inappropriate antidiuretic hormone (SIADH). Which nursing intervention is appropriate?
a. b. c. d. 17. a. b. c. d. 18. a. b. c. d.
Infusing I.V. fluids rapidly as ordered Encouraging increased oral intake Restricting fluids Administering glucose-containing I.V. fluids as ordered A female client has a serum calcium level of 7.2 mg/dl. During the physical examination, nurse Noah expects to assess: Trousseaus sign. Homans sign. Hegars sign. Goodells sign. Which outcome indicates that treatment of a male client with diabetes insipidus has been effective? Fluid intake is less than 2,500 ml/day. Urine output measures more than 200 ml/hour. Blood pressure is 90/50 mm Hg. The heart rate is 126 beats/minute.
19. Jemma, who weighs 210 lb (95 kg) and has been diagnosed with hyperglycemia tells the nurse that her husband sleeps in another room because her snoring keeps him awake. The nurse notices that she has large hands and a hoarse voice. Which of the following would the nurse suspect as a possible cause of the clients hyperglycemia? a. Acromegaly b. Type 1 diabetes mellitus c. Hypothyroidism d. Deficient growth hormone 20. Nurse Kate is providing dietary instructions to a male client with hypoglycemia. To control hypoglycemic episodes, the nurse should recommend: a. Increasing saturated fat intake and fasting in the afternoon. b. Increasing intake of vitamins B and D and taking iron supplements. c. Eating a candy bar if light-headedness occurs. d. Consuming a low-carbohydrate, high-protein diet and avoiding fasting. 21. An incoherent female client with a history of hypothyroidism is brought to the emergency department by the rescue squad. Physical and laboratory findings reveal hypothermia, hypoventilation, respiratory acidosis, bradycardia, hypotension, and nonpitting edema of the face and pretibial area. Knowing that these findings suggest severe hypothyroidism, nurse Libby prepares to take emergency action to prevent the potential complication of: a. Thyroid storm. b. Cretinism. c. myxedema coma. d. Hashimotos thyroiditis. 22. A male client with type 1 diabetes mellitus asks the nurse about taking an oral antidiabetic agent. Nurse Jack explains that these medications are only effective if the client: a. prefers to take insulin orally. b. has type 2 diabetes. c. has type 1 diabetes. d. is pregnant and has type 2 diabetes. 23. When caring for a female client with a history of hypoglycemia, nurse Ruby should avoid administering a drug that may potentiate hypoglycemia. Which drug fits this description? a. sulfisoxazole (Gantrisin) b. mexiletine (Mexitil) c. prednisone (Orasone) d. lithium carbonate (Lithobid) 24. After taking glipizide (Glucotrol) for 9 months, a male client experiences secondary failure. Which of the following would the nurse expect the physician to do? a. Initiate insulin therapy. b. Switch the client to a different oral antidiabetic agent. c. Prescribe an additional oral antidiabetic agent. d. Restrict carbohydrate intake to less than 30% of the total caloric intake.
25. a. b. c. d.
During preoperative teaching for a female client who will undergo subtotal thyroidectomy, the nurse should include which statement? The head of your bed must remain flat for 24 hours after surgery. You should avoid deep breathing and coughing after surgery. You wont be able to swallow for the first day or two. You must avoid hyperextending your neck after surgery.
GASTROINSTESTINAL DSE TEST 1. Nurse Berlinda is assigned to a 41-year-old client who has a diagnosis of chronic pancreatitis. The nurse reviews the laboratory result, anticipating a laboratory report that indicates a serum amylase level of: a. 45 units/L b. 100 units/L c. 300 units/L d. 500 units/L 2. A male client who is recovering from surgery has been advanced from a clear liquid diet to a full liquid diet. The client is looking forward to the diet change because he has been bored with the clear liquid diet. The nurse would offer which full liquid item to the client? a. Tea b. Gelatin c. Custard d. Popsicle 3. Nurse Juvy is caring for a client with cirrhosis of the liver. To minimize the effects of the disorder, the nurse teaches the client about foods that are high in thiamine. The nurse determines that the client has the best understanding of the dietary measures to follow if the client states an intension to increase the intake of: a. Pork b. Milk c. Chicken d. Broccoli 4. Nurse Oliver checks for residual before administering a bolus tube feeding to a client with a nasogastric tube and obtains a residual amount of 150 mL. What is appropriate action for the nurse to take? a. Hold the feeding b. Reinstill the amount and continue with administering the feeding c. Elevate the clients head at least 45 degrees and administer the feeding d. Discard the residual amount and proceed with administering the feeding 5. A nurse is inserting a nasogastric tube in an adult male client. During the procedure, the client begins to cough and has difficulty breathing. Which of the following is the appropriate nursing action? a. Quickly insert the tube b. Notify the physician immediately c. Remove the tube and reinsert when the respiratory distress subsides d. Pull back on the tube and wait until the respiratory distress subsides 6. Nurse Ryan is assessing for correct placement of a nosogartric tube. The nurse aspirates the stomach contents and check the contents for pH. The nurse verifies correct tube placement if which pH value is noted? a. 3.5 b. 7.0 c. 7.35 d. 7.5 7. A nurse is preparing to remove a nasogartric tube from a female client. The nurse should instruct the client to do which of the following just before the nurse removes the tube? a. Exhale b. Inhale and exhale quickly c. Take and hold a deep breath d. Perform a Valsalva maneuver 8. Nurse Joy is preparing to administer medication through a nasogastric tube that is connected to suction. To administer the medication, the nurse would: a. Position the client supine to assist in medication absorption
b. Aspirate the nasogastric tube after medication administration to maintain patency c. Clamp the nasogastric tube for 30 minutes following administration of the medication d. Change the suction setting to low intermittent suction for 30 minutes after medication administration 9. A nurse is preparing to care for a female client with esophageal varices who has just has a Sengstaken-Blakemore tube inserted. The nurse gathers supplies, knowing that which of the following items must be kept at the bedside at all times? a. An obturator b. Kelly clamp c. An irrigation set d. A pair of scissors 10. Dr. Smith has determined that the client with hepatitis has contracted the infection form contaminated food. The nurse understands that this client is most likely experiencing what type of hepatitis? a. Hepatitis A b. Hepatitis B c. Hepatitis C d. Hepatitis D 11. a. b. c. d. A client is suspected of having hepatitis. Which diagnostic test result will assist in confirming this diagnosis? Elevated hemoglobin level Elevated serum bilirubin level Elevated blood urea nitrogen level Decreased erythrocycle sedimentation rate
12. The nurse is reviewing the physicians orders written for a male client admitted to the hospital with acute pancreatitis. Which physician order should the nurse question if noted on the clients chart? a. NPO status b. Nasogastric tube inserted c. Morphine sulfate for pain d. An anticholinergic medication 13. A female client being seen in a physicians office has just been scheduled for a barium swallow the next day. The nurse writes down which instruction for the client to follow before the test? a. Fast for 8 hours before the test b. Eat a regular supper and breakfast c. Continue to take all oral medications as scheduled d. Monitor own bowel movement pattern for constipation 14. The nurse is performing an abdominal assessment and inspects the skin of the abdomen. The nurse performs which assessment technique next? a. Palpates the abdomen for size b. Palpates the liver at the right rib margin c. Listens to bowel sounds in all for quadrants d. Percusses the right lower abdominal quadrant 15. Polyethylene glycol-electrlyte solution (GoLYTELY) is prescribed for the female client scheduled for a colonoscopy. The client begins to experience diarrhea following administration of the solution. What action by the nurse is appropriate? a. Start an IV infusion b. Administer an enema c. Cancel the diagnostic test d. Explain that diarrhea is expected 16. The nurse is caring for a male client with a diagnosis of chronic gastritis. The nurse monitors the client knowing that this client is at risk for which vitamin deficiency? a. Vitamin A b. Vitamin B12 c. Vitamin C d. Vitamin E 17. The nurse is reviewing the medication record of a female client with acute gastritis. Which medication, if noted on the clients record, would the nurse question? a. Digoxin (Lanoxin)
b. Furosemide (Lasix) c. Indomethacin (Indocin) d. Propranolol hydrochloride (Inderal) 18. The nurse is assessing a male client 24 hours following a cholecystectomy. The nurse noted that the T tube has drained 750 mL of greenbrown drainage since the surgery. Which nursing intervention is appropriate? a. Clamp the T tube b. Irrigate the T tube c. Notify the physician d. Document the findings 19. The nurse is monitoring a female client with a diagnosis of peptic ulcer. Which assessment findings would most likely indicate perforation of the ulcer? a. Bradycardia b. Numbness in the legs c. Nausea and vomiting d. A rigid, board-like abdomen 20. A male client with a peptic ulcer is scheduled for a vagotomy and the client asks the nurse about the purpose of this procedure. Which response by the nurse best describes the purpose of a vagotomy? a. Halts stress reactions b. Heals the gastric mucosa c. Reduces the stimulus to acid secretions d. Decreases food absorption in the stomach 21. a. b. c. d. The nurse is caring for a female client following a Billroth II procedure. Which postoperative order should the nurse question and verify? Leg exercises Early ambulation Irrigating the nasogastric tube Coughing and deep-breathing exercises
22. The nurse is providing discharge instructions to a male client following gastrectomy and instructs the client to take which measure to assist in preventing dumping syndrome? a. Ambulate following a meal b. Eat high carbohydrate foods c. Limit the fluid taken with meal d. Sit in a high-Fowlers position during meals 23. The nurse is monitoring a female client for the early signs and symptoms of dumping syndrome. Which of the following indicate this occurrence? a. Sweating and pallor b. Bradycardia and indigestion c. Double vision and chest pain d. Abdominal cramping and pain 24. The nurse is preparing a discharge teaching plan for the male client who had umbilical hernia repair. What should the nurse include in the plan? a. Irrigating the drain b. Avoiding coughing c. Maintaining bed rest d. Restricting pain medication 25. The nurse is instructing the male client who has an inguinal hernia repair how to reduce postoperative swelling following the procedure. What should the nurse tell the client? a. Limit oral fluid b. Elevate the scrotum c. Apply heat to the abdomen d. Remain in a low-fiber diet 26. The nurse is caring for a hospitalized female client with a diagnosis of ulcerative colitis. Which finding, if noted on assessment of the client, would the nurse report to the physician? a. Hypotension
b. Bloody diarrhea c. Rebound tenderness d. A hemoglobin level of 12 mg/dL 27. The nurse is caring for a male client postoperatively following creation of a colostomy. Which nursing diagnosis should the nurse include in the plan of care? a. Sexual dysfunction b. Body image, disturbed c. Fear related to poor prognosis d. Nutrition: more than body requirements, imbalanced 28. The nurse is reviewing the record of a female client with Crohns disease. Which stool characteristics should the nurse expect to note documented in the clients record? a. Diarrhea b. Chronic constipation c. Constipation alternating with diarrhea d. Stools constantly oozing form the rectum 29. The nurse is performing a colostomy irrigation on a male client. During the irrigation, the client begins to complain of abdominal cramps. What is the appropriate nursing action? a. Notify the physician b. Stop the irrigation temporarily c. Increase the height of the irrigation d. Medicate for pain and resume the irrigation 30. The nurse is teaching a female client how to perform a colostomy irrigation. To enhance the effectiveness of the irrigation and fecal returns, what measure should the nurse instruct the client to do? a. Increase fluid intake b. Place heat on the abdomen c. Perform the irrigation in the evening d. Reduce the amount of irrigation solution ANSWER AND RATIONALE 1. Answer C. The normal serum amylase level is 25 to 151 units/L. With chronic cases of pancreatitis, the rise in serum amylase levels usually does not exceed three times the normal value. In acute pancreatitis, the value may exceed five times the normal value. Options A and B are within normal limits. Option D is an extremely elevated level seen in acute pancreatitis. 2. Answer C. Full liquid food items include items such as plain ice cream, sherbet, breakfast drinks, milk, pudding and custard, soups that are strained, and strained vegetable juices. A clear liquid diet consists of foods that are relatively transparent. The food items in options A, B, and D are clear liquids. 3. Answer A. The client with cirrhosis needs to consume foods high in thiamine. Thiamine is present in a variety of foods of plant and animal origin. Pork products are especially rich in this vitamin. Other good food sources include nuts, whole grain cereals, and legumes. Milk contains vitamins A, D, and B2. Poultry contains niacin. Broccoli contains vitamins C, E, and K and folic acid 4. Answer A. Unless specifically indicated, residual amounts more than 100 mL require holding the feeding. Therefore options B, C, and D are incorrect. Additionally, the feeding is not discarded unless its contents are abnormal in color or characteristics. 5. Answer D. During the insertion of a nasogastric tube, if the client experiences difficulty breathing or any respiratory distress, withdraw the tube slightly, stop the tube advancement, and wait until the distress subsides. Options B and C are unnecessary. Quickly inserting the tube is not an appropriate action because, in this situation, it may be likely that the tube has entered the bronchus. 6. Answer A. If the nasogastric tube is in the stomach, the pH of the contents will be acidic. Gastric aspirates have acidic pH values and should be 3.5 or lower. Option B indicates a slightly acidic pH. Option C indicates a neutral pH. Option D indicates an alkaline pH. 7. Answer C. When the nurse removes a nasogastric tube, the client is instructed to take and hold a deep breath. This will close the epiglottis. This allows for easy withdrawal through the esophagus into the nose. The nurse removes the tube with one smooth, continuous pull. 8. Answer C. If a client has a nasogastric tube connected to suction, the nurse should wait up to 30 minutes before reconnecting the tube to the suction apparatus to allow adequate time for medication absorption. Aspirating the nasogastric tube will remove the medication just administered. Low intermittent suction also will remove the medication just administered. The client should not be placed in the supine position because of the risk for aspiration. 9. Answer C. When the client has a Sengstaken-Blakemore tube, a pair of scissors must be kept at the clients bedside at all times. The client needs to be observed for sudden respiratory distress, which occurs if the gastric balloon ruptures and the entire tube moves upward. If this occurs, the nurse immediately cuts all balloon lumens and removes the tube. An obturator and a Kelly clamp are kept at the bedside of a client with a tracheostomy. An irrigation set may be kept at the bedside, but it is not the priority item.
10. Answer A. Hepatitis A is transmitted by the fecal-oral route via contaminated food or infected food handlers. Hepatitis B, C, and D are transmitted most commonly via infected blood or body fluids. 11. Answer B. Laboratory indicators of hepatitis include elevated liver enzyme levels, elevated serum bilirubin levels, elevated erythrocyte sedimentation rates, and leukopenia. An elevated blood urea nitrogen level may indicate renal dysfunction. A hemoglobin level is unrelated to this diagnosis. 12. Answer C. Meperidine (Demerol) rather than morphine sulfate is the medication of choice to treat pain because morphine sulfate can cause spasms in the sphincter of Oddi. Options A, B, and D are appropriate interventions for the client with acute pancreatitis. 13. Answer A. A barium swallow is an x-ray study that uses a substance called barium for contrast to highlight abnormalities in the gastrointestinal tract. The client should fast for 8 to 12 hours before the test, depending on physician instructions. Most oral medications also are withheld before the test. After the procedure, the nurse must monitor for constipation, which can occur as a result of the presence of barium in the gastrointestinal tract. 14. Answer C. The appropriate sequence for abdominal examination is inspection, auscultation, percussion, and palpation. Auscultation is performed after inspection to ensure that the motility of the bowel and bowel sounds are not altered by percussion or palpation. Therefore, after inspecting the skin on the abdomen, the nurse should listen for bowel sounds. 15. Answer D. The solution GoLYTELY is a bowel evacuant used to prepare a client for a colonoscopy by cleansing the bowel. The solution is expected to cause a mild diarrhea and will clear the bowel in 4 to 5 hours. Options A, B, and C are inappropriate actions. 16. Answer B. Chronic gastritis causes deterioration and atrophy of the lining of the stomach, leading to the loss of the function of the parietal cells. The source of the intrinsic factor is lost, which results in the inability to absorb vitamin B12. This leads to the development of pernicious anemia. The client is not at risk for vitamin A, C, or E deficiency. 17. Answer C. Indomethacin (Indocin) is a nonsteroidal anti-inflammatory drug and can cause ulceration of the esophagus, stomach, or small intestine. Indomethacin is contraindicated in a client with gastrointestinal disorders. Furosemide (Lasix) is a loop diuretic. Digoxin is a cardiac medication. Propranolol (Inderal) is a -adrenergic blocker. Furosemide, digoxin, and propranolol are not contraindicated in clients with gastric disorders. 18. Answer D. Following cholecystectomy, drainage from the T tube is initially bloody and then turns to a greenish-brown color. The drainage is measured as output. The amount of expected drainage will range from 500 to 1000 mL/day. The nurse would document the output. 19. Answer D. Perforation of an ulcer is a surgical emergency and is characterized by sudden, sharp, intolerable severe pain beginning in the midepigastric area and spreading over the abdomen, which becomes rigid and board-like. Nausea and vomiting may occur. Tachycardia may occur as hypovolemic shock develops. Numbness in the legs is not an associated finding. 20. Answer C. A vagotomy, or cutting of the vagus nerve, is done to eliminate parasympathetic stimulation of gastric secretion. Options A, B, and D are incorrect descriptions of a vagotomy. 21. Answer C. In a Billroth II procedure, the proximal remnant of the stomach is anastomosed to the proximal jejunum. Patency of the nasogastric tube is critical for preventing the retention of gastric secretions. The nurse should never irrigate or reposition the gastric tube after gastric surgery, unless specifically ordered by the physician. In this situation, the nurse should clarify the order. Options A, B, and D are appropriate postoperative interventions. 22. Answer C. Dumping syndrome is a term that refers to a constellation of vasomotor symptoms that occurs after eating, especially following a Billroth II procedure. Early manifestations usually occur within 30 minutes of eating and include vertigo, tachycardia, syncope, sweating, pallor, palpitations, and the desire to lie down. The nurse should instruct the client to decrease the amount of fluid taken at meals and to avoid high-carbohydrate foods, including fluids such as fruit nectars; to assume a low-Fowlers position during meals; to lie down for 30 minutes after eating to delay gastric emptying; and to take antispasmodics as prescribed. 23. Answer A. Early manifestations of dumping syndrome occur 5 to 30 minutes after eating. Symptoms include vertigo, tachycardia, syncope, sweating, pallor, palpitations, and the desire to lie down. 24. Answer B. Coughing is avoided following umbilical hernia repair to prevent disruption of tissue integrity, which can occur because of the location of this surgical procedure. Bed rest is not required following this surgical procedure. The client should take analgesics as needed and as prescribed to control pain. A drain is not used in this surgical procedure, although the client may be instructed in simple dressing changes. 25. Answer B. Following inguinal hernia repair, the client should be instructed to elevate the scrotum and apply ice packs while in bed to decrease pain and swelling. The nurse also should instruct the client to apply a scrotal support when out of bed. Heat will increase swelling. Limiting oral fluids and a low-fiber diet can cause constipation. 26. Answer C. Rebound tenderness may indicate peritonitis. Bloody diarrhea is expected to occur in ulcerative colitis. Because of the blood loss, the client may be hypotensive and the hemoglobin level may be lower than normal. Signs of peritonitis must be reported to the physician. 27. Answer B. Body image, disturbed relates to loss of bowel control, the presence of a stoma, the release of fecal material onto the abdomen, the passage of flatus, odor, and the need for an appliance (external pouch). No data in the question support options A and C. Nutrition: less than body requirements, imbalanced is the more likely nursing diagnosis. 28. Answer A. Crohns disease is characterized by nonbloody diarrhea of usually not more than four to five stools daily. Over time, the diarrhea episodes increase in frequency, duration, and severity. Options B, C, and D are not characteristics of Crohns disease. 29. Answer B. If cramping occurs during a colostomy irrigation, the irrigation flow is stopped temporarily and the client is allowed to rest. Cramping may occur from an infusion that is too rapid or is causing too much pressure. The physician does not need to be notified. Increasing the height of the irrigation will cause further discomfort. Medicating the client for pain is not the appropriate action in this situation.
30. Answer A. To enhance effectiveness of the irrigation and fecal returns, the client is instructed to increase fluid intake and to take other measures to prevent constipation. Options B, C and D will not enhance the effectiveness of this procedure. GASTRO TEST 1. During preparation for bowel surgery, a male client receives an antibiotic to reduce intestinal bacteria. Antibiotic therapy may interfere with synthesis of which vitamin and may lead to hypoprothrombinemia? a. vitamin A b. vitamin D c. vitamin E d. vitamin K 2. a. b. c. d. When evaluating a male client for complications of acute pancreatitis, the nurse would observe for: increased intracranial pressure. decreased urine output. bradycardia. hypertension.
3. A male client with a recent history of rectal bleeding is being prepared for a colonoscopy. How should the nurse position the client for this test initially? a. Lying on the right side with legs straight b. Lying on the left side with knees bent c. Prone with the torso elevated d. Bent over with hands touching the floor 4. A male client with extreme weakness, pallor, weak peripheral pulses, and disorientation is admitted to the emergency department. His wife reports that he has been spitting up blood. A Mallory-Weiss tear is suspected, and the nurse begins taking a client history from the clients wife. The question by the nurse that demonstrates her understanding of Mallory-Weiss tearing is: a. Tell me about your husbands alcohol usage. b. Is your husband being treated for tuberculosis? c. Has your husband recently fallen or injured his chest? d. Describe spices and condiments your husband uses on food. 5. Which of the following nursing interventions should the nurse perform for a female client receiving enteral feedings through a gastrostomy tube? a. Change the tube feeding solutions and tubing at least every 24 hours. b. Maintain the head of the bed at a 15-degree elevation continuously. c. Check the gastrostomy tube for position every 2 days. d. Maintain the client on bed rest during the feedings. 6. A male client is recovering from a small-bowel resection. To relieve pain, the physician prescribes meperidine (Demerol), 75 mg I.M. every 4 hours. How soon after administration should meperidines onset of action occur? a. 5 to 10 minutes b. 15 to 30 minutes c. 30 to 60 minutes d. 2 to 4 hours 7. The nurse is caring for a male client with cirrhosis. Which assessment findings indicate that the client has deficient vitamin K absorption caused by this hepatic disease? a. Dyspnea and fatigue b. Ascites and orthopnea c. Purpura and petechiae d. Gynecomastia and testicular atrophy 8. a. b. c. d. Which condition is most likely to have a nursing diagnosis of fluid volume deficit? Appendicitis Pancreatitis Cholecystitis Gastric ulcer
9. While a female client is being prepared for discharge, the nasogastric (NG) feeding tube becomes clogged. To remedy this problem and teach the clients family how to deal with it at home, what should the nurse do? a. Irrigate the tube with cola. b. Advance the tube into the intestine. c. Apply intermittent suction to the tube. d. Withdraw the obstruction with a 30-ml syringe. 10. A male client with pancreatitis complains of pain. The nurse expects the physician to prescribe meperidine (Demerol) instead of morphine to relieve pain because: a. meperidine provides a better, more prolonged analgesic effect. b. morphine may cause spasms of Oddis sphincter. c. meperidine is less addictive than morphine. d. morphine may cause hepatic dysfunction. 11. Mandy, an adolescent girl is admitted to an acute care facility with severe malnutrition. After a thorough examination, the physician diagnoses anorexia nervosa. When developing the plan of care for this client, the nurse is most likely to include which nursing diagnosis? a. Hopelessness b. Powerlessness c. Chronic low self esteem d. Deficient knowledge 12. a. b. c. d. Which diagnostic test would be used first to evaluate a client with upper GI bleeding? Endoscopy Upper GI series Hemoglobin (Hb) levels and hematocrit (HCT) Arteriography
13. A female client who has just been diagnosed with hepatitis A asks, How could I have gotten this disease? What is the nurses best response? a. You may have eaten contaminated restaurant food. b. You could have gotten it by using I.V. drugs. c. You must have received an infected blood transfusion. d. You probably got it by engaging in unprotected sex. 14. When preparing a male client, age 51, for surgery to treat appendicitis, the nurse formulates a nursing diagnosis of Risk for infection related to inflammation, perforation, and surgery. What is the rationale for choosing this nursing diagnosis? a. Obstruction of the appendix may increase venous drainage and cause the appendix to rupture. b. Obstruction of the appendix reduces arterial flow, leading to ischemia, inflammation, and rupture of the appendix. c. The appendix may develop gangrene and rupture, especially in a middle-aged client. d. Infection of the appendix diminishes necrotic arterial blood flow and increases venous drainage. 15. A female client with hepatitis C develops liver failure and GI hemorrhage. The blood products that would most likely bring about hemostasis in the client are: a. whole blood and albumin. b. platelets and packed red blood cells. c. fresh frozen plasma and whole blood. d. cryoprecipitate and fresh frozen plasma. 16. a. b. c. d. 17. a. b. c. d. To prevent gastroesophageal reflux in a male client with hiatal hernia, the nurse should provide which discharge instruction? Lie down after meals to promote digestion. Avoid coffee and alcoholic beverages. Take antacids with meals. Limit fluid intake with meals. The nurse caring for a client with small-bowel obstruction would plan to implement which nursing intervention first? Administering pain medication Obtaining a blood sample for laboratory studies Preparing to insert a nasogastric (NG) tube Administering I.V. fluids
18. A female client with dysphagia is being prepared for discharge. Which outcome indicates that the client is ready for discharge? a. The client doesnt exhibit rectal tenesmus.
b. The client is free from esophagitis and achalasia. c. The client reports diminished duodenal inflammation. d. The client has normal gastric structures. 19. A male client undergoes total gastrectomy. Several hours after surgery, the nurse notes that the clients nasogastric (NG) tube has stopped draining. How should the nurse respond? a. Notify the physician b. Reposition the tube c. Irrigate the tube d. Increase the suction level 20. a. b. c. d. 21. a. b. c. d. What laboratory finding is the primary diagnostic indicator for pancreatitis? Elevated blood urea nitrogen (BUN) Elevated serum lipase Elevated aspartate aminotransferase (AST) Increased lactate dehydrogenase (LD) A male client with cholelithiasis has a gallstone lodged in the common bile duct. When assessing this client, the nurse expects to note: yellow sclerae. light amber urine. circumoral pallor. black, tarry stools.
22. Nurse Hannah is teaching a group of middle-aged men about peptic ulcers. When discussing risk factors for peptic ulcers, the nurse should mention: a. a sedentary lifestyle and smoking. b. a history of hemorrhoids and smoking. c. alcohol abuse and a history of acute renal failure. d. alcohol abuse and smoking. 23. a. b. c. d. While palpating a female clients right upper quadrant (RUQ), the nurse would expect to find which of the following structures? Sigmoid colon Appendix Spleen Liver
24. A male client has undergone a colon resection. While turning him, wound dehiscence with evisceration occurs. The nurses first response is to: a. call the physician. b. place saline-soaked sterile dressings on the wound. c. take a blood pressure and pulse. d. pull the dehiscence closed. 25. The nurse is monitoring a female client receiving paregoric to treat diarrhea for drug interactions. Which drugs can produce additive constipation when given with an opium preparation? a. Antiarrhythmic drugs b. Anticholinergic drugs c. Anticoagulant drugs d. Antihypertensive drugs 26. A male client is recovering from an ileostomy that was performed to treat inflammatory bowel disease. During discharge teaching, the nurse should stress the importance of: a. increasing fluid intake to prevent dehydration. b. wearing an appliance pouch only at bedtime. c. consuming a low-protein, high-fiber diet. d. taking only enteric-coated medications. 27. The nurse is caring for a female client with active upper GI bleeding. What is the appropriate diet for this client during the first 24 hours after admission? a. Regular diet b. Skim milk
c. Nothing by mouth d. Clear liquids 28. a. b. c. d. A male client has just been diagnosed with hepatitis A. On assessment, the nurse expects to note: severe abdominal pain radiating to the shoulder. anorexia, nausea, and vomiting. eructation and constipation. abdominal ascites.
29. A female client with viral hepatitis A is being treated in an acute care facility. Because the client requires enteric precautions, the nurse should: a. place the client in a private room. b. wear a mask when handling the clients bedpan. c. wash the hands after touching the client. d. wear a gown when providing personal care for the client. 30. a. b. c. d. Which of the following factors can cause hepatitis A? Contact with infected blood Blood transfusions with infected blood Eating contaminated shellfish Sexual contact with an infected person
ANSWER AND RATIONALE 1. Answer D. Intestinal bacteria synthesize such nutritional substances as vitamin K, thiamine, riboflavin, vitamin B12, folic acid, biotin, and nicotinic acid. Therefore, antibiotic therapy may interfere with synthesis of these substances, including vitamin K. Intestinal bacteria dont synthesize vitamins A, D, or E. 2. Answer B. Acute pancreatitis can cause decreased urine output, which results from the renal failure that sometimes accompanies this condition. Intracranial pressure neither increases nor decreases in a client with pancreatitis. Tachycardia, not bradycardia, usually is associated with pulmonary or hypovolemic complications of pancreatitis. Hypotension can be caused by a hypovolemic complication, but hypertension usually isnt related to acute pancreatitis. 3. Answer B. For a colonoscopy, the nurse initially should position the client on the left side with knees bent. Placing the client on the right side with legs straight, prone with the torso elevated, or bent over with hands touching the floor wouldnt allow proper visualization of the large intestine. 4. Answer A. A Mallory-Weiss tear is associated with massive bleeding after a tear occurs in the mucous membrane at the junction of the esophagus and stomach. There is a strong relationship between ethanol usage, resultant vomiting, and a Mallory-Weiss tear. The bleeding is coming from the stomach, not from the lungs as would be true in some cases of tuberculosis. A Mallory-Weiss tear doesnt occur from chest injuries or falls and isnt associated with eating spicy foods. 5. Answer A. Tube feeding solutions and tubing should be changed every 24 hours, or more frequently if the feeding requires it. Doing so prevents contamination and bacterial growth. The head of the bed should be elevated 30 to 45 degrees continuously to prevent aspiration. Checking for gastrostomy tube placement is performed before initiating the feedings and every 4 hours during continuous feedings. Clients may ambulate during feedings. 6. Answer B. Meperidines onset of action is 15 to 30 minutes. It peaks between 30 and 60 minutes and has a duration of action of 2 to 4 hours. 7. Answer C. A hepatic disorder, such as cirrhosis, may disrupt the livers normal use of vitamin K to produce prothrombin (a clotting factor). Consequently, the nurse should monitor the client for signs of bleeding, including purpura and petechiae. Dyspnea and fatigue suggest anemia. Ascites and orthopnea are unrelated to vitamin K absorption. Gynecomastia and testicular atrophy result from decreased estrogen metabolism by the diseased liver. 8. Answer B. Hypovolemic shock from fluid shifts is a major factor in acute pancreatitis. The other conditions are less likely to exhibit fluid volume deficit. 9. Answer A. The nurse should irrigate the tube with cola because its effervescence and acidity are suited to the purpose, its inexpensive, and its readily available in most homes. Advancing the NG tube is inappropriate because the tube is designed to stay in the stomach and isnt long enough to reach the intestines. Applying intermittent suction or using a syringe for aspiration is unlikely to dislodge the material clogging the tube but may create excess pressure. Intermittent suction may even collapse the tube. 10. Answer B. For a client with pancreatitis, the physician will probably avoid prescribing morphine because this drug may trigger spasms of the sphincter of Oddi (a sphincter at the end of the pancreatic duct), causing irritation of the pancreas. Meperidine has a somewhat shorter duration of action than morphine. The two drugs are equally addictive. Morphine isnt associated with hepatic dysfunction. 11. Answer C. Young women with Chronic low self esteem are at highest risk for anorexia nervosa because they perceive being thin as a way to improve their self-confidence. Hopelessness and Powerlessness are inappropriate nursing diagnoses because clients with anorexia
nervosa seldom feel hopeless or powerless; instead, they use food to control their desire to be thin and hope that restricting food intake will achieve this goal. Anorexia nervosa doesnt result from a knowledge deficit, such as one regarding good nutrition. 12. Answer A. Endoscopy permits direct evaluation of the upper GI tract and can detect 90% of bleeding lesions. An upper GI series, or barium study, usually isnt the diagnostic method of choice, especially in a client with acute active bleeding whos vomiting and unstable. An upper GI series is also less accurate than endoscopy. Although an upper GI series might confirm the presence of a lesion, it wouldnt necessarily reveal whether the lesion is bleeding. Hb levels and HCT, which indicate loss of blood volume, arent always reliable indicators of GI bleeding because a decrease in these values may not be seen for several hours. Arteriography is an invasive study associated with life-threatening complications and wouldnt be used for an initial evaluation. 13. Answer A. Hepatitis A virus typically is transmitted by the oral-fecal route commonly by consuming food contaminated by infected food handlers. The virus isnt transmitted by the I.V. route, blood transfusions, or unprotected sex. Hepatitis B can be transmitted by I.V. drug use or blood transfusion. Hepatitis C can be transmitted by unprotected sex. 14. Answer B. A client with appendicitis is at risk for infection related to inflammation, perforation, and surgery because obstruction of the appendix causes mucus fluid to build up, increasing pressure in the appendix and compressing venous outflow drainage. The pressure continues to rise with venous obstruction; arterial blood flow then decreases, leading to ischemia from lack of perfusion. Inflammation and bacterial growth follow, and swelling continues to raise pressure within the appendix, resulting in gangrene and rupture. Geriatric, not middle-aged, clients are especially susceptible to appendix rupture. 15. Answer D. The liver is vital in the synthesis of clotting factors, so when its diseased or dysfunctional, as in hepatitis C, bleeding occurs. Treatment consists of administering blood products that aid clotting. These include fresh frozen plasma containing fibrinogen and cryoprecipitate, which have most of the clotting factors. Although administering whole blood, albumin, and packed cells will contribute to hemostasis, those products arent specifically used to treat hemostasis. Platelets are helpful, but the best answer is cryoprecipitate and fresh frozen plasma. 16. Answer B. To prevent reflux of stomach acid into the esophagus, the nurse should advise the client to avoid foods and beverages that increase stomach acid, such as coffee and alcohol. The nurse also should teach the client to avoid lying down after meals, which can aggravate reflux, and to take antacids after eating. The client need not limit fluid intake with meals as long as the fluids arent gastric irritants. 17. Answer D. I.V. infusions containing normal saline solution and potassium should be given first to maintain fluid and electrolyte balance. For the clients comfort and to assist in bowel decompression, the nurse should prepare to insert an NG tube next. A blood sample is then obtained for laboratory studies to aid in the diagnosis of bowel obstruction and guide treatment. Blood studies usually include a complete blood count, serum electrolyte levels, and blood urea nitrogen level. Pain medication often is withheld until obstruction is diagnosed because analgesics can decrease intestinal motility. 18. Answer B. Dysphagia may be the reason why a client with esophagitis or achalasia seeks treatment. Dysphagia isnt associated with rectal tenesmus, duodenal inflammation, or abnormal gastric structures. 19. Answer A. An NG tube that fails to drain during the postoperative period should be reported to the physician immediately. It may be clogged, which could increase pressure on the suture site because fluid isnt draining adequately. Repositioning or irrigating an NG tube in a client who has undergone gastric surgery can disrupt the anastomosis. Increasing the level of suction may cause trauma to GI mucosa or the suture line. 20. Answer B. Elevation of serum lipase is the most reliable indicator of pancreatitis because this enzyme is produced solely by the pancreas. A clients BUN is typically elevated in relation to renal dysfunction; the AST, in relation to liver dysfunction; and LD, in relation to damaged cardiac muscle. 21. Answer A. Yellow sclerae may be the first sign of jaundice, which occurs when the common bile duct is obstructed. Urine normally is light amber. Circumoral pallor and black, tarry stools dont occur in common bile duct obstruction; they are signs of hypoxia and GI bleeding, respectively. 22. Answer D. Risk factors for peptic (gastric and duodenal) ulcers include alcohol abuse, smoking, and stress. A sedentary lifestyle and a history of hemorrhoids arent risk factors for peptic ulcers. Chronic renal failure, not acute renal failure, is associated with duodenal ulcers. 23. Answer D. The RUQ contains the liver, gallbladder, duodenum, head of the pancreas, hepatic flexure of the colon, portions of the ascending and transverse colon, and a portion of the right kidney. The sigmoid colon is located in the left lower quadrant; the appendix, in the right lower quadrant; and the spleen, in the left upper quadrant. 24. Answer B. The nurse should first place saline-soaked sterile dressings on the open wound to prevent tissue drying and possible infection. Then the nurse should call the physician and take the clients vital signs. The dehiscence needs to be surgically closed, so the nurse should never try to close it. 25. Answer B. Paregoric has an additive effect of constipation when used with anticholinergic drugs. Antiarrhythmics, anticoagulants, and antihypertensives arent known to interact with paregoric. 26. Answer A. Because stool forms in the large intestine, an ileostomy typically drains liquid waste. To avoid fluid loss through ileostomy drainage, the nurse should instruct the client to increase fluid intake. The nurse should teach the client to wear a collection appliance at all times because ileostomy drainage is incontinent, to avoid high-fiber foods because they may irritate the intestines, and to avoid enteric-coated medications because the body cant absorb them after an ileostomy 27. Answer C. Shock and bleeding must be controlled before oral intake, so the client should receive nothing by mouth. A regular diet is incorrect. When the bleeding is controlled, the diet is gradually increased, starting with ice chips and then clear liquids. Skim milk shouldnt be
given because it increases gastric acid production, which could prolong bleeding. A liquid diet is the first diet offered after bleeding and shock are controlled. 28. Answer B. Hallmark signs and symptoms of hepatitis A include anorexia, nausea, vomiting, fatigue, and weakness. Abdominal pain may occur but doesnt radiate to the shoulder. Eructation and constipation are common in gallbladder disease, not hepatitis A. Abdominal ascites is a sign of advanced hepatic disease, not an early sign of hepatitis A. 29. Answer C. To maintain enteric precautions, the nurse must wash the hands after touching the client or potentially contaminated articles and before caring for another client. A private room is warranted only if the client has poor hygiene for instance, if the client is unlikely to wash the hands after touching infective material or is likely to share contaminated articles with other clients. For enteric precautions, the nurse need not wear a mask and must wear a gown only if soiling from fecal matter is likely. 30. Answer C. Hepatitis A can be caused by consuming contaminated water, milk, or food especially shellfish from contaminated water. Hepatitis B is caused by blood and sexual contact with an infected person. Hepatitis C is usually caused by contact with infected blood, including receiving blood transfusions. GENITOURINARY test 1. a. b. c. d. The nurse is aware that the following findings would be further evidence of a urethral injury in a male client during rectal examination? A low-riding prostate The presence of a boggy mass Absent sphincter tone A positive Hemoccult
2. When a female client with an indwelling urinary (Foley) catheter insists on walking to the hospital lobby to visit with family members, nurse Rose teaches how to do this without compromising the catheter. Which client action indicates an accurate understanding of this information? a. The client sets the drainage bag on the floor while sitting down. b. The client keeps the drainage bag below the bladder at all times. c. The client clamps the catheter drainage tubing while visiting with the family. d. The client loops the drainage tubing below its point of entry into the drainage bag. 3. a. b. c. d. A female client has just been diagnosed with condylomata acuminata (genital warts). What information is appropriate to tell this client? This condition puts her at a higher risk for cervical cancer; therefore, she should have a Papanicolaou (Pap) smear annually. The most common treatment is metronidazole (Flagyl), which should eradicate the problem within 7 to 10 days. The potential for transmission to her sexual partner will be eliminated if condoms are used every time they have sexual intercourse. The human papillomavirus (HPV), which causes condylomata acuminata, cant be transmitted during oral sex.
4. A male client with bladder cancer has had the bladder removed and an ileal conduit created for urine diversion. While changing this clients pouch, the nurse observes that the area around the stoma is red, weeping, and painful. What should nurse Katrina conclude? a. The skin wasnt lubricated before the pouch was applied. b. The pouch faceplate doesnt fit the stoma. c. A skin barrier was applied properly. d. Stoma dilation wasnt performed. 5. a. b. c. d. The nurse is aware that the following laboratory values supports a diagnosis of pyelonephritis? Myoglobinuria Ketonuria Pyuria Low white blood cell (WBC) count
6. A female client with chronic renal failure (CRF) is receiving a hemodialysis treatment. After hemodialysis, nurse Sarah knows that the client is most likely to experience: a. hematuria. b. weight loss. c. increased urine output. d. increased blood pressure. 7. a. b. c. d. Nurse Lea is assessing a male client diagnosed with gonorrhea. Which symptom most likely prompted the client to seek medical attention? Rashes on the palms of the hands and soles of the feet Cauliflower-like warts on the penis Painful red papules on the shaft of the penis Foul-smelling discharge from the penis
8. a. b. c. d.
Nurse Agnes is reviewing the report of a clients routine urinalysis. Which value should the nurse consider abnormal? Specific gravity of 1.03 Urine pH of 3.0 Absence of protein Absence of glucose
9. A male client is scheduled for a renal clearance test. Nurse Maureen should explain that this test is done to assess the kidneys ability to remove a substance from the plasma in: a. 1 minute. b. 30 minutes. c. 1 hour. d. 24 hours. 10. A male client in the short-procedure unit is recovering from renal angiography in which a femoral puncture site was used. When providing postprocedure care, the nurse should: a. keep the clients knee on the affected side bent for 6 hours. b. apply pressure to the puncture site for 30 minutes. c. check the clients pedal pulses frequently. d. remove the dressing on the puncture site after vital signs stabilize. 11. a. b. c. d. A female client is admitted for treatment of chronic renal failure (CRF). Nurse Juliet knows that this disorder increases the clients risk of: water and sodium retention secondary to a severe decrease in the glomerular filtration rate. a decreased serum phosphate level secondary to kidney failure. an increased serum calcium level secondary to kidney failure. metabolic alkalosis secondary to retention of hydrogen ions.
12. Because of difficulties with hemodialysis, peritoneal dialysis is initiated to treat a female clients uremia. Which finding signals a significant problem during this procedure? a. Potassium level of 3.5 mEq/L b. Hematocrit (HCT) of 35% c. Blood glucose level of 200 mg/dl d. White blood cell (WBC) count of 20,000/mm3 13. a. b. c. d. 14. a. b. c. d. For a male client in the oliguric phase of acute renal failure (ARF), which nursing intervention is most important? Encouraging coughing and deep breathing Promoting carbohydrate intake Limiting fluid intake Providing pain-relief measures A female client requires hemodialysis. Which of the following drugs should be withheld before this procedure? Phosphate binders Insulin Antibiotics Cardiac glycosides
15. A client comes to the outpatient department complaining of vaginal discharge, dysuria, and genital irritation. Suspecting a sexually transmitted disease (STD), Dr. Smith orders diagnostic tests of the vaginal discharge. Which STD must be reported to the public health department? a. Chlamydia b. Gonorrhea c. Genital herpes d. Human papillomavirus infection 16. A male client with acute pyelonephritis receives a prescription for co-trimoxazole (Septra) P.O. twice daily for 10 days. Which finding best demonstrates that the client has followed the prescribed regimen? a. Urine output increases to 2,000 ml/day. b. Flank and abdominal discomfort decrease. c. Bacteria are absent on urine culture. d. The red blood cell (RBC) count is normal. 17. A 26-year-old female client seeks care for a possible infection. Her symptoms include burning on urination and frequent, urgent voiding of small amounts of urine. Shes placed on trimethoprim-sulfamethoxazole (Bactrim) to treat possible infection. Another medication is prescribed
to decrease the pain and frequency. Which of the following is the most likely medication prescribed? a. nitrofurantoin (Macrodantin) b. ibuprofen (Motrin) c. acetaminophen with codeine d. phenazopyridine (Pyridium) 18. A triple-lumen indwelling urinary catheter is inserted for continuous bladder irrigation following a transurethral resection of the prostate. In addition to balloon inflation, the nurse is aware that the functions of the three lumens include: a. Continuous inflow and outflow of irrigation solution. b. Intermittent inflow and continuous outflow of irrigation solution. c. Continuous inflow and intermittent outflow of irrigation solution. d. Intermittent flow of irrigation solution and prevention of hemorrhage. 19. a. b. c. d. Nurse Claudine is reviewing a clients fluid intake and output record. Fluid intake and urine output should relate in which way? Fluid intake should be double the urine output. Fluid intake should be approximately equal to the urine output. Fluid intake should be half the urine output. Fluid intake should be inversely proportional to the urine output.
20. After trying to conceive for a year, a couple consults an infertility specialist. When obtaining a history from the husband, nurse Jenny inquires about childhood infectious diseases. Which childhood infectious disease most significantly affects male fertility? a. Chickenpox b. Measles c. Mumps d. Scarlet fever 21. A male client comes to the emergency department complaining of sudden onset of sharp, severe pain in the lumbar region, which radiates around the side and toward the bladder. The client also reports nausea and vomiting and appears pale, diaphoretic, and anxious. The physician tentatively diagnoses renal calculi and orders flat-plate abdominal X-rays. Renal calculi can form anywhere in the urinary tract. What is their most common formation site? a. Kidney b. Ureter c. Bladder d. Urethra 22. A female client with acute renal failure is undergoing dialysis for the first time. The nurse in charge monitors the client closely for dialysis equilibrium syndrome, a complication that is most common during the first few dialysis sessions. Typically, dialysis equilibrium syndrome causes: a. confusion, headache, and seizures. b. acute bone pain and confusion. c. weakness, tingling, and cardiac arrhythmias. d. hypotension, tachycardia, and tachypnea. 23. Dr. Marquez prescribes norfloxacin (Noroxin), 400 mg P.O. twice daily, for a client with a urinary tract infection (UTI). The client asks the nurse how long to continue taking the drug. For an uncomplicated UTI, the usual duration of norfloxacin therapy is: a. 3 to 5 days. b. 7 to 10 days. c. 12 to 14 days. d. 10 to 21 days. 24. Nurse Joy is providing postprocedure care for a client who underwent percutaneous lithotripsy. In this procedure, an ultrasonic probe inserted through a nephrostomy tube into the renal pelvis generates ultrahigh-frequency sound waves to shatter renal calculi. The nurse should instruct the client to: a. limit oral fluid intake for 1 to 2 weeks. b. report the presence of fine, sandlike particles through the nephrostomy tube. c. notify the physician about cloudy or foul-smelling urine. d. report bright pink urine within 24 hours after the procedure. 25. A client is frustrated and embarrassed by urinary incontinence. Which of the following measures should nurse Bea include in a bladder retraining program? a. Establishing a predetermined fluid intake pattern for the client b. Encouraging the client to increase the time between voidings
c. Restricting fluid intake to reduce the need to void d. Assessing present elimination patterns 1. Answer B. When the urethra is ruptured, a hematoma or collection of blood separates the two sections of urethra. This may feel like a boggy mass on rectal examination. Because of the rupture and hematoma, the prostate becomes high riding. A palpable prostate gland usually indicates a nonurethral injury. Absent sphincter tone would refer to a spinal cord injury. The presence of blood would probably correlate with GI bleeding or a colon injury. 2. Answer B. To maintain effective drainage, the client should keep the drainage bag below the bladder; this allows the urine to flow by gravity from the bladder to the drainage bag. The client shouldnt lay the drainage bag on the floor because it could become grossly contaminated. The client shouldnt clamp the catheter drainage tubing because this impedes the flow of urine. To promote drainage, the client may loop the drainage tubing above not below its point of entry into the drainage bag. 3. Answer A. Women with condylomata acuminata are at risk for cancer of the cervix and vulva. Yearly Pap smears are very important for early detection. Because condylomata acuminata is a virus, there is no permanent cure. Because condylomata acuminata can occur on the vulva, a condom wont protect sexual partners. HPV can be transmitted to other parts of the body, such as the mouth, oropharynx, and larynx. 4. Answer B. If the pouch faceplate doesnt fit the stoma properly, the skin around the stoma will be exposed to continuous urine flow from the stoma, causing excoriation and red, weeping, and painful skin. A lubricant shouldnt be used because it would prevent the pouch from adhering to the skin. When properly applied, a skin barrier prevents skin excoriation. Stoma dilation isnt performed with an ileal conduit, although it may be done with a colostomy if ordered. 5. Answer C. Pyelonephritis is diagnosed by the presence of leukocytosis, hematuria, pyuria, and bacteriuria. The client exhibits fever, chills, and flank pain. Because there is often a septic picture, the WBC count is more likely to be high rather than low, as indicated in option D. Ketonuria indicates a diabetic state. 6. Answer B. Because CRF causes loss of renal function, the client with this disorder retains fluid. Hemodialysis removes this fluid, causing weight loss. Hematuria is unlikely to follow hemodialysis because the client with CRF usually forms little or no urine. Hemodialysis doesnt increase urine output because it doesnt correct the loss of kidney function, which severely decreases urine production in this disorder. By removing fluids, hemodialysis decreases rather than increases the blood pressure. 7. Answer D. Symptoms of gonorrhea in men include purulent, foul-smelling drainage from the penis and painful urination. Rashes on the palms of the hands and soles of the feet are symptoms of the secondary stage of syphilis. Cauliflower-like warts on the penis are a sign of human papillomavirus. Painful red papules on the shaft of the penis may be a sign of the first stage of genital herpes. 8. Answer B. Normal urine pH is 4.5 to 8; therefore, a urine pH of 3.0 is abnormal. Urine specific gravity normally ranges from 1.002 to 1.035, making this clients value normal. Normally, urine contains no protein, glucose, ketones, bilirubin, bacteria, casts, or crystals. Red blood cells should measure 0 to 3 per high-power field; white blood cells, 0 to 4 per high-power field. Urine should be clear, its color ranging from pale yellow to deep amber. 9. Answer A. The renal clearance test determines the kidneys ability to remove a substance from the plasma in 1 minute. It doesnt measure the kidneys ability to remove a substance over a longer period. 10. Answer C. After renal angiography involving a femoral puncture site, the nurse should check the clients pedal pulses frequently to detect reduced circulation to the feet caused by vascular injury. The nurse also should monitor vital signs for evidence of internal hemorrhage and should observe the puncture site frequently for fresh bleeding. The client should be kept on bed rest for several hours so the puncture site can seal completely. Keeping the clients knee bent is unnecessary. By the time the client returns to the short-procedure unit, manual pressure over the puncture site is no longer needed because a pressure dressing is in place. The nurse shouldnt remove this dressing for several hours and only if instructed to do so. 11. Answer A. A client with CRF is at risk for fluid imbalance dehydration if the kidneys fail to concentrate urine, or fluid retention if the kidneys fail to produce urine. Electrolyte imbalances associated with this disorder result from the kidneys inability to excrete phosphorus; such imbalances may lead to hyperphosphatemia with reciprocal hypocalcemia. CRF may cause metabolic acidosis, not metabolic alkalosis, secondary to inability of the kidneys to excrete hydrogen ions. 12. Answer D. An increased WBC count indicates infection, probably resulting from peritonitis, which may have been caused by insertion of the peritoneal catheter into the peritoneal cavity. Peritonitis can cause the peritoneal membrane to lose its ability to filter solutes; therefore, peritoneal dialysis would no longer be a treatment option for this client. Hyperglycemia occurs during peritoneal dialysis because of the high glucose content of the dialysate; its readily treatable with sliding-scale insulin. A potassium level of 3.5 mEq/L can be treated by adding potassium to the dialysate solution. An HCT of 35% is lower than normal. However, in this client, the value isnt abnormally low because of the daily blood samplings. A lower HCT is common in clients with chronic renal failure because of the lack of erythropoietin.
13. Answer C. During the oliguric phase of ARF, urine output decreases markedly, possibly leading to fluid overload. Limiting oral and I.V. fluid intake can prevent fluid overload and its complications, such as heart failure and pulmonary edema. Encouraging coughing and deep breathing is important for clients with various respiratory disorders. Promoting carbohydrate intake may be helpful in ARF but doesnt take precedence over fluid limitation. Controlling pain isnt important because ARF rarely causes pain. 14. Answer D. Cardiac glycosides such as digoxin should be withheld before hemodialysis. Hypokalemia is one of the electrolyte shifts that occur during dialysis, and a hypokalemic client is at risk for arrhythmias secondary to digitalis toxicity. Phosphate binders and insulin can be administered because they arent removed from the blood by dialysis. Some antibiotics are removed by dialysis and should be administered after the procedure to ensure their therapeutic effects. The nurse should check a formulary to determine whether a particular antibiotic should be administered before or after dialysis. 15. Answer B. Gonorrhea must be reported to the public health department. Chlamydia, genital herpes, and human papillomavirus infection arent reportable diseases. 16. Answer C. Co-trimoxazole is a sulfonamide antibiotic used to treat urinary tract infections. Therefore, absence of bacteria on urine culture indicates that the drug has achieved its desired effect. Although flank pain may decrease as the infection resolves, this isnt a reliable indicator of the drugs effectiveness. Co-trimoxazole doesnt affect urine output or the RBC count. 17. Answer D. Phenazopyridine may be prescribed in conjunction with an antibiotic for painful bladder infections to promote comfort. Because of its local anesthetic action on the urinary mucosa, phenazopyridine specifically relieves bladder pain. Nitrofurantoin is a urinary antiseptic with no analgesic properties. While ibuprofen and acetaminophen with codeine are analgesics, they dont exert a direct effect on the urinary mucosa. 18. Answer A. When preparing for continuous bladder irrigation, a triple-lumen indwelling urinary catheter is inserted. The three lumens provide for balloon inflation and continuous inflow and outflow of irrigation solution. 19. Answer B. Normally, fluid intake is approximately equal to the urine output. Any other relationship signals an abnormality. For example, fluid intake that is double the urine output indicates fluid retention; fluid intake that is half the urine output indicates dehydration. Normally, fluid intake isnt inversely proportional to the urine output. 20. Answer C. Mumps is the most significant childhood infectious disease affecting male fertility. Chickenpox, measles, and scarlet fever dont affect male fertility. 21. Answer A. The most common site of renal calculi formation is the kidney. Calculi may travel down the urinary tract with or without causing damage and may lodge anywhere along the tract or may stay within the kidney. The ureter, bladder, and urethra are less common sites of renal calculi formation. 22. Answer A. Dialysis equilibrium syndrome causes confusion, a decreasing level of consciousness, headache, and seizures. These findings, which may last several days, probably result from a relative excess of interstitial or intracellular solutes caused by rapid solute removal from the blood. The resultant organ swelling interferes with normal physiologic functions. To prevent this syndrome, many dialysis centers keep firsttime sessions short and use a reduced blood flow rate. Acute bone pain and confusion are associated with aluminum intoxication, another potential complication of dialysis. Weakness, tingling, and cardiac arrhythmias suggest hyperkalemia, which is associated with renal failure. Hypotension, tachycardia, and tachypnea signal hemorrhage, another dialysis complication. 23. Answer B. For an uncomplicated UTI, norfloxacin therapy usually lasts 7 to 10 days. Taking the drug for less than 7 days wouldnt eradicate such an infection. Taking it for more than 10 days isnt necessary. Only a client with a complicated UTI must take norfloxacin for 10 to 21 days. 24. Answer C. The client should report the presence of foul-smelling or cloudy urine. Unless contraindicated, the client should be instructed to drink large quantities of fluid each day to flush the kidneys. Sandlike debris is normal due to residual stone products. Hematuria is common after lithotripsy. 25. Answer D. The guidelines for initiating bladder retraining include assessing the clients intake patterns, voiding patterns, and reasons for each accidental voiding. Lowering the clients fluid intake wont reduce or prevent incontinence. The client should actually be encouraged to drink 1.5 to 2 L of water per day. A voiding schedule should be established after assessment.
GENITOURINARY TEST
1. After having transurethral resection of the prostate (TURP), a Mr. Locke returns to the unit with a three-way indwelling urinary catheter and continuous closed bladder irrigation. Which finding suggests that the clients catheter is occluded? a. The urine in the drainage bag appears red to pink. b. The client reports bladder spasms and the urge to void. c. The normal saline irrigant is infusing at a rate of 50 drops/minute. d. About 1,000 ml of irrigant have been instilled; 1,200 ml of drainage have been returned. 2. Nurse Myrna is inserting a urinary catheter into a client who is extremely anxious about the procedure. The nurse can facilitate the insertion by asking the client to: a. initiate a stream of urine. b. breathe deeply. c. turn to the side. d. hold the labia or shaft of penis. 3. A female adult client admitted with a gunshot wound to the abdomen is transferred to the intensive care unit after an exploratory laparotomy. Which assessment finding suggests that the client is experiencing acute renal failure (ARF)? a. Blood urea nitrogen (BUN) level of 22 mg/dl b. Serum creatinine level of 1.2 mg/dl c. Serum creatinine level of 1.2 mg/dl d. Urine output of 400 ml/24 hours 4. A 55-year old client with benign prostatic hyperplasia doesnt respond to medical treatment and is admitted to the facility for prostate gland removal. Before providing preoperative and postoperative instructions to the client, nurse Gail asks the surgeon which prostatectomy procedure will be done. What is the most widely used procedure for prostate gland removal? a. Transurethral resection of the prostate (TURP) b. Suprapubic prostatectomy c. Retropubic prostatectomy d. Transurethral laser incision of the prostate 5. A female client with suspected renal dysfunction is scheduled for excretory urography. Nurse July reviews the history for conditions that may warrant changes in client preparation. Normally, a client should be mildly hypovolemic (fluid depleted) before excretory urography. Which history finding would call for the client to be well hydrated instead? a. Cystic fibrosis b. Multiple myeloma c. Gout d. Myasthenia gravis 6. a. b. c. d. Nurse Kim is caring for a client who had a cerebrovascular accident (CVA). Which nursing intervention promotes urinary continence? Encouraging intake of at least 2 L of fluid daily Giving the client a glass of soda before bedtime Taking the client to the bathroom twice per day Consulting with a dietitian
7. When examining a female clients genitourinary system, nurse Sally assesses for tenderness at the costovertebral angle by placing the left hand over this area and striking it with the right fist. Normally, this percussion technique produces which sound? a. A flat sound b. A dull sound c. Hyperresonance d. Tympany 8. a. b. c. d. 9. a. b. c. d. A male client with chronic renal failure has a serum potassium level of 6.8 mEq/L. What should nurse Olivia assess first? Blood pressure Respirations Temperature Pulse Nurse Hazel is ware that the following is an appropriate nursing diagnosis for a client with renal calculi? Ineffective tissue perfusion Functional urinary incontinence Risk for infection Decreased cardiac output
10. A male client develops acute renal failure (ARF) after receiving I.V. therapy with a nephrotoxic antibiotic. Because the clients 24-hour urine output totals 240 ml, nurse Andy suspects that the client is at risk for: a. cardiac arrhythmia. b. paresthesia. c. dehydration. d. pruritus. 11. After undergoing transurethral resection of the prostate to treat benign prostatic hyperplasia, a male client returns to the room with continuous bladder irrigation. On the first day after surgery, the client reports bladder pain. What should nurse Andrew do first? a. Increase the I.V. flow rate. b. Notify the physician immediately. c. Assess the irrigation catheter for patency and drainage. d. Administer meperidine (Demerol), 50 mg I.M., as prescribed. 12. a. b. c. d. When performing a scrotal examination, nurse Paul finds a nodule. What should the nurse do next? Notify the physician. Change the clients position and repeat the examination. Perform a rectal examination. Transilluminate the scrotum.
13. A male client who has been treated for chronic renal failure (CRF) is ready for discharge. Nurse Bea should reinforce which dietary instruction? a. Be sure to eat meat at every meal. b. Monitor your fruit intake, and eat plenty of bananas. c. Increase your carbohydrate intake. d. Drink plenty of fluids, and use a salt substitute. 14. a. b. c. d. Nurse Wayne is aware that the following statements describing urinary incontinence in the elderly is true? Urinary incontinence is a normal part of aging. Urinary incontinence isnt a disease. Urinary incontinence in the elderly cant be treated. Urinary incontinence is a disease.
15. The client underwent a transurethral resection of the prostate gland 24 hours ago and is on continuous bladder irrigation. Nurse Yoly is aware that the following nursing interventions is appropriate? a. Tell the client to try to urinate around the catheter to remove blood clots. b. Restrict fluids to prevent the clients bladder from becoming distended. c. Prepare to remove the catheter. d. Use aseptic technique when irrigating the catheter. 16. A female client with a urinary tract infection is prescribed co-trimoxazole (trimethoprim-sulfamethoxazole). Nurse Don should provide which medication instruction? a. Take the medication with food. b. Drink at least eight 8-oz glasses of fluid daily. c. Avoid taking antacids during co-trimoxazole therapy. d. Dont be afraid to go out in the sun. 17. A male client is admitted for treatment of glomerulonephritis. On initial assessment, Nurse Rose detects one of the classic signs of acute glomerulonephritis of sudden onset. Such signs include: a. generalized edema, especially of the face and periorbital area. b. green-tinged urine. c. moderate to severe hypotension. d. polyuria. 18. A client reports experiencing vulvar pruritus. Which assessment factor may indicate that the client has an infection caused by Candida albicans? a. Cottage cheeselike discharge b. Yellow-green discharge c. Gray-white discharge d. Discharge with a fishy odor
19. A 24-year old female client has just been diagnosed with condylomata acuminata (genital warts). What information is appropriate to tell this client? a. This condition puts her at a higher risk for cervical cancer; therefore, she should have a Papanicolaou (Pap) smear annually. b. The most common treatment is metronidazole (Flagyl), which should eradicate the problem within 7 to 10 days. c. The potential for transmission to her sexual partner will be eliminated if condoms are used every time they have sexual intercourse. d. The human papillomavirus (HPV), which causes condylomata acuminata, cant be transmitted during oral sex. 20. Nurse Vic is monitoring the fluid intake and output of a female client recovering from an exploratory laparotomy. Which nursing intervention would help the client avoid a urinary tract infection (UTI)? a. Maintaining a closed indwelling urinary catheter system and securing the catheter to the leg b. Limiting fluid intake to 1 L/day c. Encouraging the client to use a feminine deodorant after bathing d. Encouraging the client to douche once a day after removal of the indwelling urinary catheter
21. a. b. c. d.
Nurse Eve is caring for a client who had a cerebrovascular accident (CVA). Which nursing intervention promotes urinary continence? Encouraging intake of at least 2 L of fluid daily Giving the client a glass of soda before bedtime Taking the client to the bathroom twice per day Consulting with a dietitian
22. A female client with an indwelling urinary catheter is suspected of having a urinary tract infection. Nurse Angel should collect a urine specimen for culture and sensitivity by: a. disconnecting the tubing from the urinary catheter and letting the urine flow into a sterile container. b. wiping the self-sealing aspiration port with antiseptic solution and aspirating urine with a sterile needle. c. draining urine from the drainage bag into a sterile container. d. clamping the tubing for 60 minutes and inserting a sterile needle into the tubing above the clamp to aspirate urine. 23. Nurse Grace is assessing a male client diagnosed with gonorrhea. Which symptom most likely prompted the client to seek medical attention? a. Rashes on the palms of the hands and soles of the feet b. Cauliflower-like warts on the penis c. Painful red papules on the shaft of the penis d. Foul-smelling discharge from the penis 24. Nurse Ethel is planning to administer a sodium polystyrene sulfonate (Kayexalate) enema to a client with a potassium level of 5.9 mEq/L. Correct administration and the effects of this enema would include having the client: a. retain the enema for 30 minutes to allow for sodium exchange; afterward, the client should have diarrhea. b. retain the enema for 30 minutes to allow for glucose exchange; afterward, the client should have diarrhea. c. retain the enema for 60 minutes to allow for sodium exchange; diarrhea isnt necessary to reduce the potassium level. d. retain the enema for 60 minutes to allow for glucose exchange; diarrhea isnt necessary to reduce the potassium level. 25. When caring for a male client with acute renal failure (ARF), Nurse Fatima expects to adjust the dosage or dosing schedule of certain drugs. Which of the following drugs would not require such adjustment? a. acetaminophen (Tylenol) b. gentamicin sulfate (Garamycin) c. cyclosporine (Sandimmune) d. ticarcillin disodium (Ticar) ANSWER AND RATIONALE 1. Answer B. Reports of bladder spasms and the urge to void suggest that a blood clot may be occluding the catheter. After TURP, urine normally appears red to pink, and normal saline irrigant usually is infused at a rate of 40 to 60 drops/minute or according to facility protocol. The amount of returned fluid (1,200 ml) should correspond to the amount of instilled fluid, plus the clients urine output (1,000 ml + 200 ml), which reflects catheter patency. 2. Answer B. When inserting a urinary catheter, facilitate insertion by asking the client to breathe deeply. Doing this will relax the urinary sphincter. Initiating a stream of urine isnt recommended during catheter insertion. Turning to the side or holding the labia or penis wont ease insertion, and doing so may contaminate the sterile field.
3. Answer D. ARF, characterized by abrupt loss of kidney function, commonly causes oliguria, which is demonstrated by a urine output of 400 ml/24 hours. A serum creatinine level of 1.2 mg/dl isnt diagnostic of ARF. A BUN level of 22 mg/dl or a temperature of 100.2 F (37.8 C) wouldnt result from this disorder. 4. Answer A. TURP is the most widely used procedure for prostate gland removal. Because it requires no incision, TURP is especially suitable for men with relatively minor prostatic enlargements and for those who are poor surgical risks. Suprapubic prostatectomy, retropubic prostatectomy, and transurethral laser incision of the prostate are less common procedures; they all require an incision. 5. Answer B. Fluid depletion before excretory urography is contraindicated in clients with multiple myeloma, severe diabetes mellitus, and uric acid nephropathy conditions that can seriously compromise renal function in fluid-depleted clients with reduced renal perfusion. If these clients must undergo excretory urography, they should be well hydrated before the test. Cystic fibrosis, gout, and myasthenia gravis dont necessitate changes in client preparation for excretory urography. 6. Answer A. By encouraging a daily fluid intake of at least 2 L, the nurse helps fill the clients bladder, thereby promoting bladder retraining by stimulating the urge to void. The nurse shouldnt give the client soda before bedtime; soda acts as a diuretic and may make the client incontinent. The nurse should take the client to the bathroom or offer the bedpan at least every 2 hours throughout the day; twice per day is insufficient. Consultation with a dietitian wont address the problem of urinary incontinence. 7. Answer B. Percussion over the costovertebral angle normally produces a dull, thudding sound, which is soft to moderately loud with a moderate pitch and duration. This sound occurs over less dense, mostly fluid-filled matter, such as the kidneys, liver, and spleen. In contrast, a flat sound occurs over highly dense matter such as muscle; hyperresonance occurs over the air-filled, overinflated lungs of a client with pulmonary emphysema or the lungs of a child (because of a thin chest wall); and tympany occurs over enclosed structures containing air, such as the stomach and bowel. 8. Answer D. An elevated serum potassium level may lead to a life-threatening cardiac arrhythmia, which the nurse can detect immediately by palpating the pulse. The clients blood pressure may change, but only as a result of the arrhythmia. Therefore, the nurse should assess blood pressure later. The nurse also can delay assessing respirations and temperature because these arent affected by the serum potassium level. 9. Answer C. Infection can occur with renal calculi from urine stasis caused by obstruction. Options A and D arent appropriate for this diagnosis, and retention of urine usually occurs, rather than incontinence. 10. Answer A. As urine output decreases, the serum potassium level rises; if it rises sufficiently, hyperkalemia may occur, possibly triggering a cardiac arrhythmia. Hyperkalemia doesnt cause paresthesia (sensations of numbness and tingling). Dehydration doesnt occur during this oliguric phase of ARF, although typically it does arise during the diuretic phase. In a client with ARF, pruritus results from increased phosphates and isnt associated with hyperkalemia. 11. Answer C. Although postoperative pain is expected, the nurse should make sure that other factors, such as an obstructed irrigation catheter, arent the cause of the pain. After assessing catheter patency, the nurse should administer an analgesic, such as meperidine, as prescribed. Increasing the I.V. flow rate may worsen the pain. Notifying the physician isnt necessary unless the pain is severe or unrelieved by the prescribed medication. 12. Answer D. A nurse who discovers a nodule, swelling, or other abnormal finding during a scrotal examination should transilluminate the scrotum by darkening the room and shining a flashlight through the scrotum behind the mass. A scrotum filled with serous fluid transilluminates as a red glow; a more solid lesion, such as a hematoma or mass, doesnt transilluminate and may appear as a dark shadow. Although the nurse should notify the physician of the abnormal finding, performing transillumination first provides additional information. The nurse cant uncover more information about a scrotal mass by changing the clients position and repeating the examination or by performing a rectal examination. 13. Answer C. In a client with CRF, unrestricted intake of sodium, protein, potassium, and fluid may lead to a dangerous accumulation of electrolytes and protein metabolic products, such as amino acids and ammonia. Therefore, the client must limit intake of sodium; meat, which is high in protein; bananas, which are high in potassium; and fluid, because the failing kidneys cant secrete adequate urine. Salt substitutes are high in potassium and should be avoided. Extra carbohydrates are needed to prevent protein catabolism. 14. Answer B. Urinary incontinence isnt a normal part of aging nor is it a disease. It may be caused by confusion, dehydration, fecal impaction, restricted mobility, or other causes. Certain medications, including diuretics, hypnotics, sedatives, anticholinergics, and antihypertensives, may trigger urinary incontinence. Most clients with urinary incontinence can be treated; some can be cured. 15. Answer D. If the catheter is blocked by blood clots, it may be irrigated according to physicians orders or facility protocol. The nurse should use sterile technique to reduce the risk of infection. Urinating around the catheter can cause painful bladder spasms. Encourage the client to drink fluids to dilute the urine and maintain urine output. The catheter remains in place for 2 to 4 days after surgery and is only removed with a physicians order.
16. Answer B. When receiving a sulfonamide such as co-trimoxazole, the client should drink at least eight 8-oz glasses of fluid daily to maintain a urine output of at least 1,500 ml/day. Otherwise, inadequate urine output may lead to crystalluria or tubular deposits. For maximum absorption, the client should take this drug at least 1 hour before or 2 hours after meals. No evidence indicates that antacids interfere with the effects of sulfonamides. To prevent a photosensitivity reaction, the client should avoid direct sunlight during co-trimoxazole therapy. 17. Answer A. Generalized edema, especially of the face and periorbital area, is a classic sign of acute glomerulonephritis of sudden onset. Other classic signs and symptoms of this disorder include hematuria (not green-tinged urine), proteinuria, fever, chills, weakness, pallor, anorexia, nausea, and vomiting. The client also may have moderate to severe hypertension (not hypotension), oliguria or anuria (not polyuria), headache, reduced visual acuity, and abdominal or flank pain. 18. Answer A. The symptoms of C. albicans include itching and a scant white discharge that has the consistency of cottage cheese. Yellowgreen discharge is a sign of Trichomonas vaginalis. Gray-white discharge and a fishy odor are signs of Gardnerella vaginalis. 19. Answer A. Women with condylomata acuminata are at risk for cancer of the cervix and vulva. Yearly Pap smears are very important for early detection. Because condylomata acuminata is a virus, there is no permanent cure. Because condylomata acuminata can occur on the vulva, a condom wont protect sexual partners. HPV can be transmitted to other parts of the body, such as the mouth, oropharynx, and larynx. 20. Answer A. Maintaining a closed indwelling urinary catheter system helps prevent introduction of bacteria; securing the catheter to the clients leg also decreases the risk of infection by helping to prevent urethral trauma. To flush bacteria from the urinary tract, the nurse should encourage the client to drink at least 10 glasses of fluid daily, if possible. Douching and feminine deodorants may irritate the urinary tract and should be discouraged. 21. Answer A. By encouraging a daily fluid intake of at least 2 L, the nurse helps fill the clients bladder, thereby promoting bladder retraining by stimulating the urge to void. The nurse shouldnt give the client soda before bedtime; soda acts as a diuretic and may make the client incontinent. The nurse should take the client to the bathroom or offer the bedpan at least every 2 hours throughout the day; twice per day is insufficient. Consultation with a dietitian wont address the problem of urinary incontinence. 22. Answer B. Most catheters have a self-sealing port for obtaining a urine specimen. Antiseptic solution is used to reduce the risk of introducing microorganisms into the catheter. Tubing shouldnt be disconnected from the urinary catheter. Any break in the closed urine drainage system may allow the entry of microorganisms. Urine in urine drainage bags may not be fresh and may contain bacteria, giving false test results. When there is no urine in the tubing, the catheter may be clamped for no more than 30 minutes to allow urine to collect. 23. Answer D. Symptoms of gonorrhea in men include purulent, foul-smelling drainage from the penis and painful urination. Rashes on the palms of the hands and soles of the feet are symptoms of the secondary stage of syphilis. Cauliflower-like warts on the penis are a sign of human papillomavirus. Painful red papules on the shaft of the penis may be a sign of the first stage of genital herpes. 24. Answer A. Kayexalate is a sodium exchange resin. Thus the client will gain sodium as potassium is lost in the bowel. For the exchange to occur, Kayexalate must be in contact with the bowel for at least 30 minutes. Sorbitol in the Kayexalate enema causes diarrhea, which increases potassium loss and decreases the potential for Kayexalate retention. 25. Answer A. Because acetaminophen is metabolized in the liver, its dosage and dosing schedule need not be adjusted for a client with ARF. In contrast, the dosages and schedules for gentamicin and ticarcillin, which are metabolized and excreted by the kidney, should be adjusted. Because cyclosporine may cause nephrotoxicity, the nurse must monitor both the dosage and blood drug level in a client receiving this drug. Questions Hematology 1. Ms. X is diagnosed with acquired immunodeficiency syndrome (AIDS). The nurse caring for this patient is aware that for a patient to be diagnosed with HIV she should have which condition? a. Infection of HIV, have a CD4+ T-cell count of 500 cells/microliter, history of acute HIV infection b. Infection with Tuberculosis, HIV and cytomegalovirus c. Infection of HIV, have a CD4+ T-cell count of >200 cells/microliter, history of acute HIV infection d. Infection with HIV, history of HIV infection and T-cell count below 200 cells/microliter 2. a. b. c. d. The nurse observes precaution in caring for Mr. X as HIV is most easily transmitted in: Vaginal secretions and urine Breast milk and tears Feces and saliva Blood and semen
3. Nurse Jaja is giving an injection to Ms. X. After giving an injection, the nurse accidentally stuck her finger with the needle when the client became very agitated. To determine if the nurse became infected with HIV when is the best time to test her for HIV antibodies? a. Immediately and repeat the test after 12 weeks b. Immediately and repeat the test after 4 weeks c. After a week and repeat the test in 4 months d. After a weeks and repeat the test in 6 months 4. a. b. c. d. 5. a. b. c. d. 6. a. b. c. d. 7. a. b. c. d. 8. a. b. c. d. 9. a. b. c. d. 10. a. b. c. d. 11. a. b. c. d. 12. a. b. c. d. The blood test first used to identify a response to HIV infection is: Western blot ELISA test CD4+ T-cell count CBC What is the main reason why it is difficult to develop a vaccine against HIV? HIV is still unknown to human HIV mutates easily HIV spreads rapidly throughout the body HIV matures easily Human Immunodeficiency virus belongs to which classifications? Rhabdovirus Rhinovirus Retrovirus Rotavirus Which organ is responsible for stimulating the production of red blood cells? Yellow marrow Red marrow Spleen Kidney In anemia, which of the following blood components is decreased? Erythrocytes Granulocytes Leukocytes Platelets The precursor of red blood cells is called: T cells B cells Stem cells Macrophage In erythropoiesis, the sequence of erythrocyte formation is chronologically described in which option? Stem cells, erythroblast, reticulocyte, erythrocytes Stem cells, reticulocyte, erythroblast, erythrocytes Erythroblast, stem cells, reticulocyte, erythrocytes Erythroblast, reticulocyte, stem cells, erythrocytes Which of the following is true of red blood cell? It is nucleated. It has a lifespan of 100 days Its production and formation depends on the action of the kidney It is produced in the yellow marrow Which type of immunoglobulin passes or crosses the placenta starting at the first trimester of pregnancy? IgG IgA IgM All of these
13. a. b. c. d. 14. a. b. c. d. 15. a. b. c. d. 16. a. b. c. d. 17. a. b. c. d. 18. a. b. c. d. 19. a. b. c. d. 20. a. b. c. d. 21. a. b. c. d. 22. a. b. c. d.
The first immunoglobulin produced by the body when the neonate is distressed, has acquired an infection or is challenged is: IgG IgA IgM All of these Which of the following is essential for the hemoglobin synthesis during RBC production? Folic Acid Iron Vitamin B12 All of these The age group most at risk for developing anemia is: 20-25 years old 26-32 years old 40-50 years old >65 years old Decreased number of platelets is called: Thrombectomy Thrombocytopenia Thrombocytopathy Thrombocytosis To improve the platelet count of a patient with an idiopathic thrombocytopenic purpura, this medication should be given: Vitamin K Methotrexate Corticosteroid Acetylsalicylic Acid B-cells are involved in which of the following types of immunity? Humoral immunity Cell-mediated immunity Antigen-mediated immunity All of these What is the life span of normal platelets? 3-4 months 1-2 months 1-3 days 7-10 days A patient is diagnosed with a systematic lupus erythematous (SLE). SLE primarily attacks which tissues? Heart Lung Nerve Connective A sign of neurologic involvement in SLE is manifested by: CVA Infection Psychosis Facial tic A classic sign of SLE is: Rashes over the cheeks and nose Weight loss Vomiting Difficulty urinating
23. A laboratory test result that supports the diagnosis of SLE is: a. Leukocytosis, elevated BUN and CREA
b. Pancytopenia, elevated antinuclear antibody (ANA) titer c. Thrombocytosis, elevated ESR d. None of these 24. a. b. c. d. 25. a. b. c. d. Which food should a client with leukemia avoid? Wheat bread Steak Orange All of these The average length of time from HIV infection to the development of AIDS is? Less than 3 years 5-7 years 10 years More than 10 years
ANSWER AND RATIONALE 1. Answer C. The three criteria for a client to be diagnosed with AIDS are the following: HIV positive CD4+ T-cell count below 200 cells/microliter Have one or more specific conditions that include acute infection of HIV
2. Answer D. Keyword: MOST EASILY. Rationale: HIV is MOST EASILY transmitted in blood, semen and vaginal secretions. However, it has been noted to be found in fecal materials, urine, saliva, tears and breast milk. 3. Answer A. Keyword: BEST TIME. Rationale: To determine if a preexisting infection is present a test should be done immediately and is repeated again in 3 months time (12 weeks) to detect seroconversion as a result of the needle stick. 4. Answer B. Keyword: FIRST. Rationale: The ELISA test is the first screening test for HIV. A Western blot test confirms a positive ELISA test. Other blood tests that support the diagnosis of HIV include CD4+ and CD8 + counts, CBC, immunoglobulin levels, p24 antigen assay, and quantitative ribonucleic acid assays. 5. Answer B. Keyword: MAIN REASON. Rationale: HIV was identified in 1983, thus, A is incorrect. By 1988 two strains of HIV existed, HIV-1 and HIV-2. Viruses spread rapidly and mature easily but these factors dont affect the potential for development against HIV. Mutating too easily makes it hard to create a vaccine against it. 6. Answer C. Rationale: HIV is a retrovirus that has a ribonucleic acid dependent reverse transcriptase. 7. Answer D. Keyword: STIMULATING THE PRODUCTION OF RBC. Rationale: Kidneys produce and release the hormone erythropoietin that is responsible for initiating the production of RBCs in the red marrow, thus, the correct answer is D. The Red Marrow is the site of RBC production. The spleen is responsible for removing the damage RBC. 8. Answer A. Rationale: Anemia is characterized by a decreased in the number of RBCs. 9. Answer C. Keyword: PRECURSOR. Rationale: the precursor of RBC is the stem cells in the red marrow. 10. Answer A. Rationale: Stem cells erythroblast- reticulocyte erythrocytes. Erythropoietin is the hormone that stimulates red blood cell production in the red marrow. Mature red blood cells are formed from stem cells in the bone marrow. With the presence of erythropoietin, red cell pathway starts to form proerythroblast from stem cells. At this point the cell still contains nucleus. However, as the development progresses the nucleus becomes smaller and the cytoplasm becomes basophilic due to the presence of ribosome, thus the cell is now called basophilic erythroblast. As the cell becomes older it also becomes smaller and eventually when it begins to produce hemoglobin it is now termed as polychromatic erythroblast. Later on the cytoplasm will become more eosinophilic and the cell is now called orthochromatic erythroblast, which will then extrude its nucleus as the cells slowly fill with hemoglobin before entering the circulation as reticulocytes. Reticulocytes will mature to form the anucleated red blood cells. 11. Answer C. Keyword: TRUE. Rationale: Kidneys produce and release the hormone erythropoietin that is responsible for initiating the production of RBCs in the red marrow. Red blood cells are anucleated cells (without nucleus) and have a life span of 120 days or 4 months.
12. Answer A. Keyword: PASSES/CROSSES THE PLACENTA. Rationale: There is only one immunoglobulin that passes or crosses that placenta, the IgG. IgG starts to cross the placenta at the first trimester of pregnancy. However, the largest amount of IgG transfer is noted during the third trimester of pregnancy. This type of immunoglobulin provides the fetus a passive immunity to possible bacterial and viral infections. However, the passive immunity it provides is only temporary. The immunity gradually disappears at about 6 to 8 months of life. The gradual disappearance of passive immunity, leads to the gradual production of larger quantities of immunoglobulin to replace the IgG from the mother. 13. Answer C. Keyword: FIRST IMMUNOGLOBULIN PRODUCED BY THE BODY. Rationale: IgM is the first immunoglobulin produced by the body when the neonate is distressed, has acquired an infection or is challenged. When a newborn is exposed to environmental antigens, production of IgM rapidly increases. This type of immunoglobulin provides protection from gram-negative bacteria. IgM cannot cross the placental barrier. In cases where large amount of IgM is found in the placenta, possible exposure to infection in the utero is probable 14. Answer B. Keyword: HEMOGLOBIN SYNTHESIS. Rationale: Dietary elements are essential for RBC production. The following are needed by the red marrow to produce erythrocytes: Iron for hemoglobin synthesis Folic Acid for DNA synthesis Vitamin B12 for DNA synthesis 15. Answer D. Keyword: MOST AT RISK. Rationale: The elderly are most at risk for anemia often due to financial concerns affecting protein intake or poor dentition that interferes with chewing meat. 16. Answer B. Keyword: DECREASED NUMBER OF PLATELETS. Rationale: thrombocytopenia is a decreased number of platelets. Thrombocytosis is an excess in the number of platelets. Thrombocytopathy is a platelet dysfunction. Thrombectomy is the surgical removal of a thrombus. 17. Answer C. Rationale: TO IMPROVE PLATELET COUNT. Rationale: Corticosteroid therapy can decrease antibody production and phagocytosis of the antibody-coated platelets, retaining more functioning platelets. Methotrexate can cause thrombocytopenia. Vitamin K is used to treat an excessive anticoagulable state from warfarin overload, and ASA decreases platelet aggregation. 18. Answer A. Keyword: B-CELLS. Rationale: B-Cells are responsible for humoral or immunoglobulin mediated immunity. T-cells are responsible for cell-mediated immunity. There is such thing as antigen-mediated immunity. 19. Answer D. Rationale: The life span of a normal platelet is 7-10 days. However, in idiopathic thrombocytopenia the life span is reduced to 13 days. 20. Answer D. Keyword: PRIMARILY. Rationale: SLE is a chronic, inflammatory, autoimmune disorder affecting primarily the connective tissues. It also affects the skin and kidneys and may affect the pulmonary, cardiac, neural and renal systems. 21. Answer C. Keyword: NEUROLOGICAL INVOLVEMENT. Rationale: neurologic involvement may be shown by: Psychosis Seizures Headaches 22. Answer A. Keyword: CLASSIC SIGN. Rationale: Although all these symptoms can be signs of SLE, the classic sign is the butterfly rash over the cheeks and nose. 23. Answer B. Keyword: SUPPORTS THE DIAGNOSIS. Rationale: lab findings for clients with SLE usually show: Pancytopenia Elevated ANA titer Decreased serum complement levels 24. Answer C. Keyword: AVOID. Rationale: a low-bacteria diet would be indicated. Raw fruits and vegetables are excluded in the clients diet. 25. Answer C. Keyword: AVERAGE LENGTH OF TIME. Rationale: epidemiologic studies show the average time from initial contact with HIV to the development of AIDS is 10 years. INTEGUMENTARY TEST
a. Ineffective airway clearance related to edema of the respiratory passages
b. Impaired physical mobility related to the disease process c. Disturbed sleep pattern related to facility environment d. Risk for infection related to breaks in the skin 2. a. b. c. d. In a female client with burns on the legs, which nursing intervention helps prevent contractures? Applying knee splints Elevating the foot of the bed Hyperextending the clients palms Performing shoulder range-of-motion exercises
3. A male client comes to the physicians office for treatment of severe sunburn. The nurse takes this opportunity to discuss the importance of protecting the skin from the suns damaging rays. Which instruction would best prevent skin damage? a. Minimize sun exposure from 1 to 4 p.m. when the sun is strongest. b. Use a sunscreen with a sun protection factor of 6 or higher. c. Apply sunscreen even on overcast days. d. When at the beach, sit in the shade to prevent sunburn. 4. A female client is brought to the emergency department with second- and third-degree burns on the left arm, left anterior leg, and anterior trunk. Using the Rule of Nines, what is the total body surface area that has been burned? a. 18% b. 27% c. 30% d. 36% 5. a. b. c. d. Which nursing intervention can help a client maintain healthy skin? Keep the client well hydrated. Avoid bathing the client with mild soap. Remove adhesive tape quickly from the skin. Recommend wearing tight-fitting clothes in hot weather.
6. A male client with psoriasis visits the dermatology clinic. When inspecting the affected areas, the nurse expects to see which type of secondary lesion? a. Scale b. Crust c. Ulcer d. Scar 7. A female adult client with atopic dermatitis is prescribed a potent topical corticosteroid, to be covered with an occlusive dressing. To address a potential client problem associated with this treatment, the nurse formulates the nursing diagnosis of Risk for injury. To complete the nursing diagnosis statement, the nurse should add which related-to phrase? a. Related to potential interactions between the topical corticosteroid and other prescribed drugs b. Related to vasodilatory effects of the topical corticosteroid c. Related to percutaneous absorption of the topical corticosteroid d. Related to topical corticosteroid application to the face, neck, and intertriginous sites 8. a. b. c. d. A male client is diagnosed with herpes simplex. Which statement about herpes simplex infection is true? During early pregnancy, herpes simplex infection may cause spontaneous abortion or premature delivery. Genital herpes simplex lesions are painless, fluid-filled vesicles that ulcerate and heal in 3 to 7 days Herpetic keratoconjunctivitis usually is bilateral and causes systemic symptoms. A client with genital herpes lesions can have sexual contact but must use a condom.
9. A female client with a severe staphylococcal infection is receiving the aminoglycoside gentamicin sulfate (Garamycin) by the I.V. route. The nurse should assess the client for which adverse reaction to this drug? a. Aplastic anemia b. Ototoxicity c. Cardiac arrhythmias d. Seizures 10. A male client is diagnosed with primary herpes genitalis. Which instruction should the nurse provide? a. Apply one applicator of terconazole intravaginally at bedtime for 7 days. b. Apply one applicator of tioconazole intravaginally at bedtime for 7 days.
c. Apply acyclovir ointment to the lesions every 3 hours, six times a day for 7 days. d. Apply sulconazole nitrate twice daily by massaging it gently into the lesions. 11. Nurse Bea plans to administer dexamethasone cream to a client who has dermatitis over the anterior chest How should the nurse apply this topical agent? a. With a circular motion, to enhance absorption b. With an upward motion, to increase blood supply to the affected area c. In long, even, outward, and downward strokes in the direction of hair growth d. In long, even, outward, and upward strokes in the direction opposite hair growth 12. a. b. c. d. 13. a. b. c. d. Nurse Meredith is caring for a wheelchair-bound client. Which piece of equipment impedes circulation to the area its meant to protect? Polyurethane foam mattress Ring or donut Gel flotation pad Water bed Nurse Rudolf documents the presence of a scab on a clients deep wound. The nurse identifies this as which phase of wound healing? Inflammatory Migratory Proliferative Maturation
14. In an industrial accident, a male client that weighs 155 lb (70 kg) sustained full-thickness burns over 40% of his body. Hes in the burn unit receiving fluid resuscitation. Which observation shows that the fluid resuscitation is benefiting the client? a. A urine output consistently above 100 ml/hour b. A weight gain of 4 lb (2 kg) in 24 hours c. Body temperature readings all within normal limits d. An electrocardiogram (ECG) showing no arrhythmias 15. A female client with herpes zoster is prescribed acyclovir (Zovirax), 200 mg P.O. every 4 hours while awake. The nurse should inform the client that this drug may cause: a. palpitations. b. dizziness. c. diarrhea. d. metallic taste. 16. A female client sees a dermatologist for a skin problem. Later, the nurse reviews the clients chart and notes that the chief complaint was intertrigo. This term refers to which condition? a. Spontaneously occurring wheals b. A fungus that enters the skins surface, causing infection c. Inflammation of a hair follicle d. Irritation of opposing skin surfaces caused by friction 17. A male client who has suffered a cerebrovascular accident (CVA) is too weak to move on his own. To help the client avoid pressure ulcers, the nurse should: a. turn him frequently. b. perform passive range-of-motion (ROM) exercises. c. reduce the clients fluid intake. d. encourage the client to use a footboard. 18. A male client visits the physicians office for treatment of a skin disorder. As a primary treatment, the nurse expects the physician to prescribe: a. an I.V. corticosteroid. b. an I.V. antibiotic. c. an oral antibiotic. d. a topical agent. 19. While in a skilled nursing facility, a male client contracted scabies, which is diagnosed the day after discharge. The client is living at her daughters home, where six other persons are living. During her visit to the clinic, she asks a staff nurse, What should my family do? The most accurate response from the nurse is: a. All family members will need to be treated. b. If someone develops symptoms, tell him to see a physician right away.
c. Just be careful not to share linens and towels with family members. d. After youre treated, family members wont be at risk for contracting scabies. 20. a. b. c. d. When caring for a male client with severe impetigo, the nurse should include which intervention in the plan of care? Placing mitts on the clients hands Administering systemic antibiotics as prescribed Applying topical antibiotics as prescribed Continuing to administer antibiotics for 21 days as prescribed
21. A female client with second- and third-degree burns on the arms receives autografts. Two days later, the nurse finds the client doing arm exercises. The nurse knows that this client should avoid exercise because it may: a. dislodge the autografts. b. increase edema in the arms. c. increase the amount of scarring. d. decrease circulation to the fingers. 22. Nurse Troy discovers scabies when assessing a client who has just been transferred to the medical-surgical unit from the day surgery unit. To prevent scabies infection in other clients, the nurse should: a. wash hands, apply a pediculicide to the clients scalp, and remove any observable mites. b. isolate the clients bed linens until the client is no longer infectious. c. notify the nurse in the day surgery unit of a potential scabies outbreak. d. place the client on enteric precautions. 23. Dr. Smith prescribes an emollient for a client with pruritus of recent onset. The client asks why the emollient should be applied immediately after a bath or shower. How should the nurse respond? a. This makes the skin feel soft. b. This prevents evaporation of water from the hydrated epidermis. c. This minimizes cracking of the dermis. d. This prevents inflammation of the skin. 24. Following a full-thickness (third-degree) burn of his left arm, a female client is treated with artificial skin. The client understands postoperative care of artificial skin when he states that during the first 7 days after the procedure, he will restrict: a. range of motion. b. protein intake. c. going outdoors. d. fluid ingestion. 25. a. b. c. d. 26. to: a. b. c. d. 27. a. b. c. d. A male client with a solar burn of the chest, back, face, and arms is seen in urgent care. The nurses primary concern should be: fluid resuscitation. infection. body image. pain management. The nurse is providing home care instructions to a client who has recently had a skin graft. Its most important that the client remember use cosmetic camouflage techniques. protect the graft from direct sunlight. continue physical therapy. apply lubricating lotion to the graft site. A male client is diagnosed with gonorrhea. When teaching the client about this disease, the nurse should include which instruction? Avoid sexual intercourse until youve completed treatment, which takes 14 to 21 days. Wash your hands thoroughly to avoid transferring the infection to your eyes. If you have intercourse before treatment ends, tell sexual partners of your status and have them wash well after intercourse. If you dont get treatment, you may develop meningitis and suffer widespread central nervous system (CNS) damage.
28. A female client with atopic dermatitis is prescribed medication for photochemotherapy. The nurse teaches the client about the importance of protecting the skin from ultraviolet light before drug administration and for 8 hours afterward and stresses the need to protect the eyes. After administering medication for photochemotherapy, the client must protect the eyes for: a. 4 hours. b. 8 hours.
c. 24 hours. d. 48 hours. 29. A female client with genital herpes simplex is being treated in the outpatient department. The nurse teaches her about measures that may prevent herpes recurrences and emphasizes the need for prompt treatment if complications arise. Genital herpes simplex increases the risk of: a. cancer of the ovaries. b. cancer of the uterus. c. cancer of the cervix. d. cancer of the vagina. 30. a. b. c. d. Which of the following is the initial intervention for a male client with external bleeding? Elevation of the extremity Pressure point control Direct pressure Application of a tourniquet
ANSWER AND RATIONALE 1. Answer A. When caring for a client with upper torso burns, the nurses primary goal is to maintain respiratory integrity. Therefore, option A should take the highest priority. Option B isnt appropriate because burns arent a disease. Option C and D may be appropriate, but dont command a higher priority than option A because they dont reflect immediately life-threatening problems. 2. Answer A. Applying knee splints prevents leg contractures by holding the joints in a position of function. Elevating the foot of the bed cant prevent contractures because this action doesnt hold the joints in a position of function. Hyperextending a body part for an extended time is inappropriate because it can cause contractures. Performing shoulder range-of-motion exercises can prevent contractures in the shoulders, but not in the legs. 3. Answer C. Sunscreen should be applied even on overcast days, because the suns rays are as damaging then as on sunny days. The sun is strongest from 10 a.m. to 2 p.m. (11 a.m. to 3 p.m. daylight saving time) not from 1 to 4 p.m. Sun exposure should be minimized during these hours. The nurse should recommend sunscreen with a sun protection factor of at least 15. Sitting in the shade when at the beach doesnt guarantee protection against sunburn because sand, concrete, and water can reflect more than half the suns rays onto the skin. 4. Answer D. The Rule of Nines divides body surface area into percentages that, when totaled, equal 100%. According to the Rule of Nines, the arms account for 9% each, the anterior legs account for 9% each, and the anterior trunk accounts for 18%. Therefore, this clients burns cover 36% of the body surface area. 5. Answer A. Keeping the client well hydrated helps prevent skin cracking and infection because intact healthy skin is the bodys first line of defense. To help a client maintain healthy skin, the nurse should avoid strong or harsh detergents and should use mild soap. The nurse shouldnt remove adhesive tape quickly because this action can strip or scrape the skin. The nurse should recommend wearing loose-fitting not tight-fitting clothes in hot weather to promote heat loss by evaporation. 6. Answer A. A scale is the characteristic secondary lesion occurring in psoriasis. Although crusts, ulcers, and scars also are secondary lesions in skin disorders, they dont accompany psoriasis. 7. Answer C. A potent topical corticosteroid may increase the clients risk for injury because it may be absorbed percutaneously, causing the same adverse effects as systemic corticosteroids. Topical corticosteroids arent involved in significant drug interactions. These preparations cause vasoconstriction, not vasodilation. A potent topical corticosteroid rarely is prescribed for use on the face, neck, or intertriginous sites because application on these areas may lead to increased adverse effects. 8. Answer A. Herpes simplex may be passed to the fetus transplacentally and, during early pregnancy, may cause spontaneous abortion or premature delivery. Genital herpes simplex lesions typically are painful, fluid-filled vesicles that ulcerate and heal within 1 to 2 weeks. Herpetic keratoconjunctivitis usually is unilateral and causes localized symptoms, such as conjunctivitis. A client with genital herpes lesions should avoid all sexual contact to prevent spreading the disease. 9. Answer B. The most significant adverse reactions to gentamicin and other aminoglycosides are ototoxicity (indicated by vertigo, tinnitus, and hearing loss) and nephrotoxicity (indicated by urinary cells or casts, oliguria, proteinuria, and reduced creatinine clearance). These adverse reactions are most common in elderly and dehydrated clients, those with renal impairment, and those receiving concomitant therapy with another potentially ototoxic or nephrotoxic drug. Gentamicin isnt associated with aplastic anemia, cardiac arrhythmias, or seizures. 10. Answer C. A client with primary herpes genitalis should apply topical acyclovir ointment in sufficient quantities to cover the lesions every 3 hours, six times a day for 7 days. Terconazole and tioconazole are used to treat vulvovaginal candidiasis. Sulconazole nitrate is used to treat tinea versicolor. 11. Answer C. When applying a topical agent, the nurse should begin at the midline and use long, even, outward, and downward strokes in the direction of hair growth. This application pattern reduces the risk of follicle irritation and skin inflammation. 12. Answer B. Rings or donuts arent to be used because they restrict circulation. Foam mattresses evenly distribute pressure. Gel pads redistribute with the clients weight. The water bed also distributes pressure over the entire surface. 13. Answer B. The scab formation is found in the migratory phase. It is accompanied by migration of epithelial cells, synthesis of scar tissue by
fibroblasts, and development of new cells that grow across the wound. In the inflammatory phase, a blood clot forms, epidermis thickens, and an inflammatory reaction occurs in the subcutaneous tissue. During the proliferative phase, the actions of the migratory phase continue and intensify, and granulation tissue fills the wound. In the maturation phase, cells and vessels return to normal and the scab sloughs off. 14. Answer A. In a client with burns, the goal of fluid resuscitation is to maintain a mean arterial blood pressure that provides adequate perfusion of vital structures. If the kidneys are adequately perfused, they will produce an acceptable urine output of at least 0.5 ml/kg/hour. Thus, the expected urine output of a 155-lb client is 35 ml/hour, and a urine output consistently above 100 ml/hour is more than adequate. Weight gain from fluid resuscitation isnt a goal. In fact, a 4-lb weight gain in 24 hours suggests third spacing. Body temperature readings and ECG interpretations may demonstrate secondary benefits of fluid resuscitation but arent primary indicators. 15. Answer C. Oral acyclovir may cause such adverse GI effects as diarrhea, nausea, and vomiting. It isnt associated with palpitations, dizziness, or a metallic taste. 16. Answer D. Intertrigo refers to irritation of opposing skin surfaces caused by friction. Spontaneously occurring wheals occur in hives. A fungus that enters the skin surface and causes infection is a dermatophyte. Inflammation of a hair follicle is called folliculitis. 17. Answer A. The most important intervention to prevent pressure ulcers is frequent position changes, which relieve pressure on the skin and underlying tissues. If pressure isnt relieved, capillaries become occluded, reducing circulation and oxygenation of the tissues and resulting in cell death and ulcer formation. During passive ROM exercises, the nurse moves each joint through its range of movement, which improves joint mobility and circulation to the affected area but doesnt prevent pressure ulcers. Adequate hydration is necessary to maintain healthy skin and ensure tissue repair. A footboard prevents plantar flexion and footdrop by maintaining the foot in a dorsiflexed position. 18. Answer D. Although many drugs are used to treat skin disorders, topical agents not I.V. or oral agents are the mainstay of treatment. 19. Answer A. When someone in a group of persons sharing a home contracts scabies, each individual in the home needs prompt treatment whether hes symptomatic or not. Towels and linens should be washed in hot water. Scabies can be transmitted from one person to another before symptoms develop. 20. Answer B. Impetigo is a contagious, superficial skin infection caused by beta-hemolytic streptococci. If the condition is severe, the physician typically prescribes systemic antibiotics for 7 to 10 days to prevent glomerulonephritis, a dangerous complication. The clients nails should be kept trimmed to avoid scratching; however, mitts arent necessary. Topical antibiotics are less effective than systemic antibiotics in treating impetigo. 21. Answer A. Because exercising the autograft sites may dislodge the grafted tissue, the nurse should advise the client to keep the grafted extremity in a neutral position. None of the other options results from exercise 22. Answer B. To prevent the spread of scabies in other hospitalized clients, the nurse should isolate the clients bed linens until the client is no longer infectious usually 24 hours after treatment begins. Other required precautions include using good hand-washing technique and wearing gloves when applying the pediculicide and during all contact with the client. Although the nurse should notify the nurse in the day surgery unit of the clients condition, a scabies epidemic is unlikely because scabies is spread through skin or sexual contact. This client doesnt require enteric precautions because the mites arent found on feces. 23. Answer B. Applying an emollient immediately after taking a bath or shower prevents evaporation of water from the hydrated epidermis, the skins upper layer. Although emollients make the skin feel soft, this effect occurs whether or not the client has just bathed or showered. An emollient minimizes cracking of the epidermis, not the dermis (the layer beneath the epidermis). An emollient doesnt prevent skin inflammation. 24. Answer A. To prevent disruption of the artificial skins adherence to the wound bed, the client should restrict range of motion of the involved limb. Protein intake and fluid intake are important for healing and regeneration and shouldnt be restricted. Going outdoors is acceptable as long as the left arm is protected from direct sunlight. 25. Answer D. With a superficial partial thickness burn such as a solar burn (sunburn), the nurses main concern is pain management. Fluid resuscitation and infection become concerns if the burn extends to the dermal and subcutaneous skin layers. Body image disturbance is a concern that has lower priority than pain management. 26. Answer B. To avoid burning and sloughing, the client must protect the graft from direct sunlight. The other three interventions are helpful to the client and his recovery but are less important. 27. Answer B. Adults and children with gonorrhea may develop gonococcal conjunctivitis by touching the eyes with contaminated hands. The client should avoid sexual intercourse until treatment is completed, which usually takes 4 to 7 days, and a follow-up culture confirms that the infection has been eradicated. A client who doesnt refrain from intercourse before treatment is completed should use a condom in addition to informing sex partners of the clients health status and instructing them to wash well after intercourse. Meningitis and widespread CNS damage are potential complications of untreated syphilis, not gonorrhea. 28. Answer D. To prevent eye discomfort, the client must protect the eyes for 48 hours after taking medication for photochemotherapy. Protecting the eyes for a shorter period increases the risk of eye injury. 29. Answer C. A female client with genital herpes simplex is at increased risk for cervical cancer. Genital herpes simplex isnt a risk factor for cancer of the ovaries, uterus, or vagina. 30. Answer C. Applying direct pressure to an injury is the initial step in controlling bleeding. For severe or arterial bleeding, pressure point control can be used. Pressure points are those areas where large blood vessels can be compressed against bone: femoral, brachial, facial, carotid, and temporal artery sites. Elevation reduces the force of flow, but direct pressure is the first step. A tourniquet may further damage the injured extremity and should be avoided unless all other measures have failed.
INTEGUMENTARY 1. a. b. c. d. 2. a. b. c. d. 3. a. b. c. d. Nurse Jay is performing wound care. Which of the following practices violates surgical asepsis? Holding sterile objects above the waist Considering a 1 edge around the sterile field as being contaminated Pouring solution onto a sterile field cloth Opening the outermost flap of a sterile package away from the body During the acute phase of a burn, the nurse in-charge should assess which of the following? Clients lifestyle Alcohol use Tobacco use Circulatory status Nurse Kate is changing a dressing and providing wound care. Which activity should she perform first? Assess the drainage in the dressing. Slowly remove the soiled dressing Wash hands thoroughly. Put on latex gloves.
4. Nurse May is caring for an elderly bedridden adult. To prevent pressure ulcers, which intervention should the nurse include in the plan of care? a. Turn and reposition the client at least once every 8 hours. b. Vigorously massage lotion into bony prominences. c. Post a turning schedule at the clients bedside. d. Slide the client, rather than lifting, when turning. 5. Nurse Jane formulates a nursing diagnosis of Impaired physical mobility for a client with third-degree burns on the lower portions of both legs. To complete the nursing diagnosis statement, the nurse should add which related-to phrase? a. Related to fat emboli b. Related to infection c. Related to femoral artery occlusion d. Related to circumferential eschar 6. The nurse is assessing for the presence of cyanosis in a male dark-skinned client. The nurse understands that which body area would provide the best assessment? a. Lips b. Sacrum c. Earlobes d. Back of the hands 7. a. b. c. d. 8. a. b. c. d. Which of the following individuals is least likely to be at risk of developing psoriasis? A 32 year-old-African American A woman experiencing menopause A client with a family history of the disorder An individual who has experienced a significant amount of emotional distress Which of the following clients would least likely be at risk of developing skin breakdown? A client incontinent of urine feces A client with chronic nutritional deficiencies A client with decreased sensory perception A client who is unable to move about and is confined to bed
9. The nurse prepares to care for a male client with acute cellulites of the lower leg. The nurse anticipates that which of the following will be prescribed for the client? a. Cold compress to the affected area b. Warm compress to the affected area c. Intermittent heat lamp treatments four times daily d. Alternating hot and cold compresses continuously
10. a. b. c. d.
The clinic nurse assesses the skin of a white characteristic is associated with this skin disorder? Clear, thin nail beds Red-purplish scaly lesions Oily skin and no episodes of pruritus Silvery-white scaly patches on the scalp, elbow, knees, and sacral regions
11. The clinic nurse notes that the physician has documented a diagnosis of herpes zoster (shingles) in the male clients chart. Based on an understanding of the cause of this disorder, the nurse determines that this definitive diagnosis was made following which diagnostic test? a. Patch test b. Skin biopsy c. Culture of the lesion d. Woos light examination 12. The nurse is assigned to care for a female client with herpes zoster (Shingles). Which of the following characteristics would the nurse expect to note when assessing the lesions of this infection? a. Clustered skin vesicles b. A generalized body rash c. Small blue-white spots with a red base d. A fiery red, edematous rash on the cheeks 13. a. b. c. d. When assessing a lesion diagnosed as malignant melanoma, the nurse in-charge most likely expects to note which of the following? An irregular shaped lesion A small papule with a dry, rough scale A firm, nodular lesion topped with crust A pearly papule with a central crater and a waxy border
14. The nurse prepares discharge instructions for a male client following cryosurgery for the treatment of a malignant skin lesion. Which of the following should the nurse include in the instruction? a. Avoid showering for 7 to 10 days b. Apply ice to the site to prevent discomfort c. Apply alcohol-soaked dressing twice a day d. Clean the site with hydrogen peroxide to prevent infection 15. Nurse Carl reviews the clients chart and notes that the physician has documented a diagnosis of paronychia. Based on this diagnosis, which of the following would the nurse expect to note during the assessment? a. Red shiny skin around the nail bed b. White taut skin in the popliteal area c. White silvery patches on the elbows d. Swelling of the skin near the parotid gland 16. A male client arrives at the emergency room and has experienced frostbites to the right hand. Which of the following would the nurse note on assessment of the clients hand? a. A pink, edematous hand b. A fiery red skin with edema in the nail beds c. Black fingertips surrounded by an erythematous rash d. A white color to the skin, which is insensitive to touch 17. The evening nurse reviews the nursing documentation in the male clients chart and notes that the day nurse has documented that the client has a stage II pressure ulcer in the sacral area. Which of the following would the nurse expect to note on assessment of the clients sacral area? a. Intact skin b. Full-thickness skin loss c. Exposed bone, tendon, or muscle d. Partial-thickness skin loss of the dermis 18. Nurse Ivy is implementing a teaching plan to a group of adolescents regarding the causes of acne. Which of the following is an appropriate nursing statement regarding the cause of this disorder? a. Acne is caused by oily skin b. The actual cause is not known c. Acne is caused by eating chocolate d. Acne is caused as a result of exposure to heat and humidity
19. The nurse is reviewing the health care record of a male clients scheduled to be seen at the health care clinic. The nurse determines that which of the following individuals is at the greatest risk for development of an integumentary disorder? a. An adolescent b. An older female c. A physical education teacher d. An outdoor construction worker 20. A male client schedule for a skin biopsy is concerned and asks the nurse how painful the procedure is. The appropriate response by the nurse is: a. There is no pain associated with this procedure b. The local anesthetic may cause a burning or stinging sensation c. A preoperative medication will be given so you will be sleeping and will not feel any pain d. There is some pain, but the physician will prescribe an opioid analgesic following the procedure 21. The nurse is teaching a female client with a leg ulcer about tissue repair and wound healing. Which of the following statements by the client indicates effective teaching? a. Ill limit my intake of protein. b. Ill make sure that the bandage is wrapped tightly. c. My foot should feel cold. d. Ill eat plenty of fruits and vegetables. 22. Following a full-thickness (third-degree) burn of his left arm, a male client is treated with artificial skin. The client understands postoperative care of artificial skin when he states that during the first 7 days after the procedure, he will restrict: a. range of motion. b. protein intake. c. going outdoors. d. fluid ingestion. 23. Following a small-bowel resection, a male client develops fever and anemia. The surface surrounding the surgical wound is warm to the touch and necrotizing fasciitis is suspected. Another manifestation that would most suggest necrotizing fasciitis is: a. erythema. b. leukocytosis. c. pressurelike pain. d. swelling. 24. While in a skilled nursing facility, a female client contracted scabies, which is diagnosed the day after discharge. The client is living at her daughters home, where six other persons are living. During her visit to the clinic, she asks a staff nurse, What should my family do? The most accurate response from the nurse is: a. All family members will need to be treated. b. If someone develops symptoms, tell him to see a physician right away. c. Just be careful not to share linens and towels with family members. d. After youre treated, family members wont be at risk for contracting scabies. 25. The nurse is assessing a male client admitted with second- and third-degree burns on the face, arms, and chest. Which finding indicates a potential problem? a. Partial pressure of arterial oxygen (PaO2) value of 80 mm Hg b. Urine output of 20 ml/hour c. White pulmonary secretions d. Rectal temperature of 100.6 F (38 C) 26. A female client exhibits s purplish bruise to the skin after a fall. The nurse would document this finding most accurately using which of the following terms? a. Purpura b. Petechiae c. Ecchymosis d. Erythema 27. An older clients physical examination reveals the presence of a number of bright red-colored lesions scattered on the trunk and tights. The nurse interprets that this indicates which of the following lesions due to alterations in blood vessels of the skin? a. Cherry angioma b. Spider angioma
c. Venous star d. Purpura 28. A nurse is reviewing the medical record of a male client to be admitted to the nursing unit and notes documentation of reticular skin lesions. The nurse expects that these lesions will appear to be: a. Ring-shaped b. Linear c. Shaped like an arc d. Net-like appearance 29. A male client seen in an ambulatory clinic has a butterfly rash across the nose. The nurse interprets that this finding is consistent with early manifestations of which of the following disorders? a. Hyperthyroidism b. Perncious anemia c. Cardiopulmonary disorders d. Systemic lupus erythematosus (SLE) 30. A female client with cellulites of the lower leg has had cultures done on the affected area. The nurse reading the culture report understands that which of the following organisms is not part of the normal flora of the skin? a. Staphylococcus epidermidis b. Staphylococcus aureus c. Escherichia coli (E. coli) d. Candida albicans ANSWER AND RATIONALE 1. Answer C. Pouring solution onto a sterile field cloth violates surgical asepsis because moisture penetrating the cloth can carry microorganisms to the sterile field via capillary action. The other options are practices that help ensure surgical asepsis. 2. Answer D. During the acute phase of a burn, the nurse should assess the clients circulatory and respiratory status, vital signs, fluid intake and output, ability to move, bowel sounds, wounds, and mental status. Information about the clients lifestyle and alcohol and tobacco use may be obtained later when the clients condition has stabilized. 3. Answer C. When caring for a client, the nurse must first wash her hands. Putting on gloves, removing the dressing, and observing the drainage are all parts of performing a dressing change after hand washing is completed. 4. Answer C. A turning schedule with a signing sheet will help ensure that the client gets turned and, thus, help prevent pressure ulcers. Turning should occur every 1 to 2 hours not every 8 hours for clients who are in bed for prolonged periods. The nurse should apply lotion to keep the skin moist but should avoid vigorous massage, which could damage capillaries. When moving the client, the nurse should lift rather than slide the client to avoid shearing. 5. Answer D. As edema develops on circumferential burns, eschar forms a tight, constricting band, compromising circulation to the extremity distal to the circumferential site and impairing physical mobility. This client isnt likely to develop fat emboli unless long bone or pelvic fractures are present. Infection doesnt alter physical mobility. A client with burns on the lower portions of both legs isnt likely to have femoral artery occlusion. 6. Answer A. In a dark-skinned client, the nurse examines the lips, tongue, nail beds, conjunctivae, and palms of the hands and soles of the feet at regular intervals for subtle color changes. In a client with cyanosis, the lips and tongue are gray; the palms, soles, conjunctivae, and nail beds have a bluish tinge. 7. Answer A. Psoriasis occurs equally among women and men, although the incidence is lower in darker skinned races and ethnic groups. A genetic predisposition has been recognized in some cases. Emotional distress, trauma, systemic illness, seasonal changes, and hormonal changes are linked to exacerbations. 8. Answer C. Bed or chair confinement, inability to move, loss of bowel or bladder control, poor nutrition, absent or inconsistent caregiving, and decreased sensory perception can contribute to the development of skin breakdown. The least likely risk, as presented in the options, is the decreased sensory perception. Options A, B, and D identify physiological conditions, which are the risk priorities. 9. Answer B. Cellulitis is a skin infection into deeper dermal and subcutaneous tissues that results in a deep red erythema without sharp borders and spreads widely throughout tissue spaces. Warm compresses may be used to decrease the discomfort, erythema, and edema. After tissue and blood cultures are obtained, antibiotics will be initiated. The nurse should provide supportive care as prescribed to manage symptoms such as fatigue, fever, chills, headache, and myalgia. Heat lamps can cause more disruption to already inflamed tissue. Cold compresses and alternating cold and hot compresses are not the best measures. 10. Answer D. Cellulitis is a skin infection into deeper dermal and subcutaneous tissues that results in a deep red erythema without sharp borders and spreads widely throughout tissue spaces. Warm compresses may be used to decrease the discomfort, erythema, and edema. After tissue and blood cultures are obtained, antibiotics will be initiated. The nurse should provide supportive care as prescribed to manage symptoms such as fatigue, fever, chills, headache, and myalgia. Heat lamps can cause more disruption to already inflamed tissue. Cold
compresses and alternating cold and hot compresses are not the best measures. 11. Answer C. With the classic presentation of herpes zoster, the clinical examination is diagnostic. A viral culture of the lesion provides the definitive diagnosis. Herpes zoster (shingles) is caused by a reactivation of the varicella-zoster virus, the virus that causes chickenpox. A patch test is a skin test that involves the administration of an allergen to the surface of the skin to identify specific allergies. A biopsy would provide a cytological examination of tissue. In a Woods light examination, the skin is viewed under ultraviolet light to identify superficial infections of the skin. 12. Answer A. The primary lesion of herpes zoster is a vesicle. The classic presentation is grouped vesicles on an erythematous base along a dermatome. Because the lesions follow nerve pathways, they do not cross the midline of the body. Options B, C, and D are incorrect descriptions of herpes zoster. 13. Answer A. A melanoma is an irregularly shaped pigmented papule or plaque with a red-, white-, or blue-toned color. Basal cell carcinoma appears as a pearly papule with a central crater and rolled waxy border. Squamous cell carcinoma is a firm, nodular lesion topped with a crust or a central area of ulceration. Actinic keratosis, a premalignant lesion, appears as a small macule or papule with a dry, rough, adherent yellow or brown scale. 14. Answer D. Cryosurgery involves the local application of liquid nitrogen to isolated lesions and causes cell death and tissue destruction. The nurse informs the client that swelling and increased tenderness of the treated area can occur when the skin thaws. Tissue freezing is followed by hemorrhagic blister formation in 1 to 2 days. The nurse instructs the client to clean the treatment site with hydrogen peroxide to prevent secondary infection. A topical antibiotic also may be prescribed. Application of a warm, damp washcloth intermittently to the site will provide relief from any discomfort. Alcohol-soaked dressings will cause irritation. The client does not need to avoid showering. 15. Answer A. Paronychia, or infection around the nail, is characterized by red, shiny skin, often associated with painful swelling. These infections frequently result from trauma, picking at the nail, or disorders such as dermatitis. Often, these become secondarily infected with bacteria or fungus, which later involves the nail. Warm soaks three or four times a day may reduce pain and pressure; however, incision and drainage of the inflamed site frequently are required. Options B, C, and D are incorrect. 16. Answer D. Assessment findings in frostbite include a white or blue color; the skin will be hard, cold, and insensitive to touch. As thawing occurs, flushing of the skin, the development of blisters or blebs, or tissue edema appears. Options A, B, and C are incorrect. 17. Answer D. In a stage II pressure ulcer, the skin is not intact. Partial-thickness skin loss of the dermis has occurred. It presents as a shallow open ulcer with a red-pink wound bed, without slough. It may also present as an intact, open or ruptured, serum-filled blister. The skin is intact in stage I. Full-thickness skin loss occurs in stage 3. Exposed bone, tendon, or muscle is present in stage 4. 18. Answer B. The actual cause of acne is unknown. Oily skin or the consumption of foods such as chocolate, nuts, or fatty foods are not causes of acne. Exacerbations that coincide with the menstrual cycle result from hormonal activity. Heat, humidity, and excessive perspiration may play a role in exacerbating acne but does not cause it. 19. Answer D. Prolonged exposure to the sun, unusual cold, or other conditions can damage the skin. The outdoor construction worker would fit into a high-risk category for the development of an integumentary disorder. An adolescent may be prone to the development of acne, but this does not occur in all adolescents. Immobility and lack of nutrition would increase the older persons risk but the older client is not at as high a risk as the outdoor construction worker. The physical education teacher is at low or no risk of developing an integumentary problem. 20. Answer B. Depending on the size and location of the lesion, a biopsy is usually a quick and almost painless procedure. The most common source of pain is the initial local anesthetic, which can produce a burning or stinging sensation. Preoperative medication is not necessary with this procedure. 21. Answer D. For effective tissue healing, adequate intake of protein, vitamin A, B complex, C, D, E, and K are needed. Therefore, the client should eat a high protein diet with plenty of fruits and vegetables to provide these nutrients. The bandage should be secure but not too tight to impede circulation to the area (needed for tissue repair). If the clients foot feels cold, circulation is impaired, thus inhibiting wound healing. 22. Answer A. To prevent disruption of the artificial skins adherence to the wound bed, the client should restrict range of motion of the involved limb. Protein intake and fluid intake are important for healing and regeneration and shouldnt be restricted. Going outdoors is acceptable as long as the left arm is protected from direct sunlight. 23. Answer C. Severe pressure like pain out of proportion to visible signs distinguishes necrotizing fasciitis from cellulitis. Erythema, leukocytosis, and swelling are present in both cellulitis and necrotizing fasciitis. 24. Answer A. When someone in a group of persons sharing a home contracts scabies, each individual in the home needs prompt treatment whether hes symptomatic or not. Towels and linens should be washed in hot water. Scabies can be transmitted from one person to another before symptoms develop. 25. Answer B. A urine output of less than 40 ml/hour in a client with burns indicates a fluid volume deficit. This clients PaO2 value falls within the normal range (80 to 100 mm Hg). White pulmonary secretions also are normal. The clients rectal temperature isnt significantly elevated and probably results from the fluid volume deficit. 26. Answer C. Ecchymosis is a type of purpuric lesion and also is known as a bruise. Purpura is an umbrella term that incorporates ecchymoses and petechiae. Petechiae are pinpoint hemorrhages and are another form of purpura. Erythema is an area of redness on the skin. 27. Answer A. Cherry angioma occurs with increasing age and has no clinical significance. It appears as a small, round, bright redcolored lesion on the trunk or extremities. Spider angiomas have a bright red center with legs that radiate outward. These lesions commonly are seen in liver disease and vitamin B deficiency, although they occasionally can occur without underlying pathology. A venous star results from increased pressure in veins, usually in the lower legs, and has an irregularly shaped bluish center with radiating branches. Purpura results from
hemorrhage into the skin. 28. Answer D. Reticular skin lesions resemble a net in appearance. Annular lesions are ring-shaped, whereas linear lesions appear in a straight line. Arciform lesions are shaped like an arc. 29. Answer D. An early sign of SLE is the appearance of a butterfly rash across the nose. Hyperthyroidism often leads to moist skin and increased perspiration. Pernicious anemia would be manifested by pallor of the skin. Cardiopulmonary disorders may lead to clubbing of the fingers. 30. Answer C. E. coli normally is found in the intestines and constitutes a common source of infection of wounds and the urinary system. The other microbes listed are part of the normal flora of the skin. OB-GYNE TEST Situation: During an Anatomy and Physiology class, the lecturer discussed about the female reproductive system. 1. a. b. c. d. 2. a. b. c. d. Estrogen, one of the hormones regulating cyclic activities in female reproductive system is responsible for which effect? Increases the quantity and pH of cervical mucus, causing it to become thin and watery and can be stretched to a distance of 10-13 cm. Inhibits the production of LH Increases endometrial tortuosity All of the above Jessa, 17 years old, is bleeding between periods of less than two weeks. This condition is an abnormality in the menstrual cycle known as: Metrorrhagia Menorrhagia Amenorrhea Dysmenorrheal
3. One factor of having a normal delivery is the size of the pelvis. Pelvis serves as the passageway for the passenger (fetus) during childbirth. The most ideal pelvis for childbirth is: a. Android b. Anthropoid c. Platypelloid d. Gynecoid 4. a. b. c. d. 5. a. b. c. d. An important landmark of the pelvis that determines the distance of the descent of the head is known as: Linea terminalis Sacrum Ischial spines Ischial tuberosities The permanent cessation of menstruation is: Amenorrhea Menopause Oligomenorrhea Hypomenorrhea
Situation: Mrs. Donna, pregnant for 16 weeks age of gestation (AOG), visits the health care facility for her prenatal check-up with her only son, Mark. During assessment the client told the nurse that previously she got pregnant twice. The first was with her only child, Mark, who was delivered at 35 weeks AOG and the other pregnancy was terminated at about 20 weeks AOG. 6. a. b. c. d. Based on the data obtained, Mrs. Donnas GTPAL score is: 20111 21111 30111 31111
7. Discomforts during pregnancy are discussed by the nurse to the Mrs. Donna. Which of the following, when complained by the client would alert the nurse? a. Easy fatigability b. Nausea and vomiting c. Edema of the lower extremities d. Heartburn
8. Psychological and emotional responses of pregnant women differ. However, general emotional response has been noted during pregnancy based on their gestational age. Mrs. Donna will most likely have which emotional response towards her pregnancy? a. Presents denial disbelief and sometimes repression. b. Has personal identification of the baby and realistic plans for future of the child. c. Fantasizes the appearance of the baby. d. Verbalizes fear of death during childbirth. 9. The nurse assisted Mrs. Donna to a dorsal recumbent position and is about to assess the fetal heart rate (FHR). Which of the following apparatus should the nurse use in auscultating for the FHR? a. Doppler apparatus b. Fetoscope c. Ultrasound d. Stethoscope 10. a. b. c. d. Mrs. Donna asked the nurse, when a fetal heart starts beating. The nurse correctly responded by stating: 3 weeks AOG 8 weeks AOG 12 weeks AOG 20 weeks AOG
Situation: Mrs. Dela Cruz is in labor and is brought to the emergency room with a ruptured bag of water. 11. a. b. c. d. The nurses initial action once the bag of water has ruptured is: Take the fetal heart tones Put the client to the bed immediately Perform an IE Take the womans temperature
12. Mrs. Dela Cruzs has contractions growing stronger which lasts for 40-60 seconds and occur approximately every 3-5 minutes. The doctor is about to perform an IE, the nurse expects that the clients cervical dilatation will be: a. 0-3 cm b. 4-7 cm c. 8-10 cm d. 11-13 cm 13. The doctor informed the woman that she is on station -1. Mrs. Dela Cruz asked the nurse, what does a station -1 means, the most appropriate response of the nurse is: a. It means that engagement has already occurred. b. The presenting part of your baby is at the entrance of the true pelvis or the largest diameter of the presenting part into the true pelvis. c. Your baby is still floating or ballotable d. The presenting part of your baby is at the vulvar ring of your reproductive organ. 14. The history of Mrs. Dela Cruz revealed that she is a multipara. When should the nurse transport the client from the labor room to the delivery room? a. When the cervical dilatation is 8 cm. b. When the cervical dilatation is 10 cm. c. When the cervical dilatation is 9 cm. d. When the client feels the urge to push. 15. a. b. c. d. Monitoring contractions is very important during labor. To monitor uterine contractions, what should the nurse do? Observe for the clients facial expression to know that the contraction has started or stopped. Instruct the client take note of the duration of her contractions. Offer ice chips to the woman. Spread the fingers lightly over the fundus to monitor the contraction.
16. Uterine contractions can occur because of the interplay of the contractile enzyme adenosine triphosphate and the influence some hormones. Which of the following least likely contributes to the occurrence of uterine contractions? a. Oxytocin b. Estrogen c. Prolactin d. All of the above
17. a. b. c. d. 18. a. b. c. d. 19. a. b. c. d. 20. a. b. c. d.
Dysfunctional labor may be caused by which of the following? Excessive or too early analgesia administration Exhausted mother Overdistention of the uterus All of the above The clients uterine contractions are hypotonic. The nurses top priority with hypotonic contractions during the intrapartal period is: Pain relief Psychological support Monitoring the lochia for possible bleeding Infection control For a woman experiencing hypotonic contractions, what should be done initially? Obtain an ultrasonic result Infusion of oxytocin Administration of analgesia Amniotomy The most important nursing consideration in a postpartal woman with a hypotonic contraction is: Assessment for infection Assessment for bleeding Assessment for FHR Assessment for womans coping mechanism
Situation: Bleeding during pregnancy is a serious case and should be managed immediately. 21. Mrs. Diane is diagnosed with Placenta Previa. The main difference with the bleeding in placenta previa and abruption placenta is that placenta previa has: a. Painful bleeding b. Rigid abdomen c. Bright-red blood d. Blood filled with clots 22. a. b. c. d. 23. a. b. c. d. In caring for a client diagnosed with placenta previa, the nurse should avoid which of the following? Inspecting the perineum Performing a Kleihauer-Betke test Performing a pelvic examination All of the above For the nurse to distinguish that the bleeding of the patient is placenta previa or abruption placenta what should she ask the woman? Whether there was accompanying pain What she has done for bleeding Estimation of blood loss All of the above
24. Continued bleeding may result to fetal distress. The nurse knows that the fetus is being compromised when she observed or note which of the following: a. Fetal tachycardia b. Fetal bradycardia c. Fetal thrashing d. All of the above 25. A woman in labor is diagnosed with abruption placenta. The nurse would expect which findings in the clients history that may contribute to the occurrence of the complication? a. Age of 24 years old b. Cigarette smoking c. Sleeping 8 hours per night d. Sitting for long period 1. Answer: A. Effects of estrogen: Inhibits the production of FSH
Causes hypertrophy of the myometrium Increases the quantity and pH of cervical mucus, causing it to become thin and watery and can be stretched to a distance of 10-13 cm. Effects of Progesterone Inhibits the production of LH Increases endometrial tortuosity Increased endometrial secretions Facilitates transport of the fertilized ovum through the fallopian tubes 2. Answer: A Abnormalities of Menstruation 1. Amenorrhea absence of menstrual flow 2. Dysmenorrhea painful menstruation 3. Oligomenorrhea scanty menstruation 4. Menorrhagia -excessive menstrual bleeding 5. Metrorrhagia bleeding between periods of less than 2 weeks 3. Answer: D. Gynecoid is the normal female pelvis. The inlet is well rounded. This is the most ideal pelvis for childbirth. Android male pelvis. Inlet has a narrow, shallow posterior portion and pointed anterior portion. Anthropoid transverse diameter is narrow and anteroposterior (AP) diameter of this pelvis is larger than normal. Platypelloid inlet is oval while AP diameter of this pelvis is shallow.
4. Answer: C. Ischial spines are the point of reference in determining the station (relationship of the fetal presenting part to the ischial spines). When the fetal head is at the level of the ischial spines the station is zero. When it is 1 cm above the ischial spines it is -1 and if 1 cm below the ischial spines it is +1. 5. Answer: B. The keyword here is permanent cessation. Thus, menopause is the correct answer. Amenorrhea is a temporary cessation of menses. Oligomenorrhea is a menstruation with scanty blood flow. Hypomenorrhea is an abnormally short duration of menstruation. 6. Answer: C. Gravida (G) number of pregnancy Term (T) number of full-term infants born (born at 37 weeks or after) Para (P) number of preterm infants born (born before 37 weeks) Abortion (A) number of spontaneous or induced abortions (pregnancy terminated before the age of viability). Age of viability is 24 weeks. Living children (L) number of living children. (Source: Maternal and Child Health Nursing by Adelle Pillitteri, 5th Ed. P.252)
Since Mrs Donna has two previous pregnancies and is presently pregnant (16 weeks), G is 3. Mark, her only child was born at 35 weeks AOG which falls under the preterm category. Thus, T is zero and P is 1. The other pregnancy was terminated at 20 weeks AOG which falls under abortion, hence A=1. Mark is her only living child, thereby, L=1. Her GTPAL score is: 30111, G=3 T=0 P=1 A=1 L=1 7. Answer: B. Morning sickness characterized by nausea and vomiting is only noted during the FIRST TRIMESTER of pregnancy (first 3 months). Excessive nausea and vomiting which persists more than 3 months is a condition called Hyperemesis gravidarum that requires immediate intervention to prevent starvation and dehydration. Management for hyperemesis gravidarum includes the administration of D5NSS 3L in 24 hours and complete bed rest. Easy fatigability is a consequence of the physiologic anemia of pregnancy (physiologic meaning it is normally expected during pregnancy, thus A is incorrect). Edema of the upper extremities not the lower extremities should alert the nurse because of the possibility of toxemia, hence C is incorrect. Heartburn during pregnancy is due to the increase progesterone which decreases gastric motility causing a reversed peristaltic wave leading to regurgitation of the stomach contents through the cardiac sphincter into the esophagus, causing irritation. 8. Answer: C. The client is in her second trimester of pregnancy (16 weeks AOG or 4 months), thus, she perceived the baby as a separate entity. Presenting denial and disbelief and sometime repression is the psychological/emotional response of a pregnant woman on her first trimester. Identifying the fetus and setting realistic plans for the childs future is noted during the third trimester of pregnancy. It is during this time also that the woman verbalizes fear of death. 9. Answer: A. Mrs. Donnas gestational age is 16 weeks (4 months). During this time, the fetal heart rate is audible with a Doppler apparatus. A fetal heart beat can be detected with a Doppler apparatus starting at 12 weeks AOG. By 8 weeks AOG, fetal heartbeat can be detected with an ultrasound. A fetal heart beat is detectable with fetoscope by the 20th week AOG. (Source: Foundations of Maternal-Newborn Nursing by Murray and McKinney/Saunders 4th Ed.) 10. Answer: A. Fetal heart starts beating at 3 weeks AOG. The heart at this time is consisting of two parallel tubes. By 8 weeks AOG, fetal heartbeat can be detected with an ultrasound. During 12 weeks AOG, the fetal heart rate is audible with a Doppler apparatus. A fetal heart beat
is detectable with fetoscope by the 20th week AOG. (Source: Foundations of Maternal-Newborn Nursing by Murray and McKinney/Saunders 4th Ed.) 11. Answer: B. The keyword is INITIAL ACTION. The important consideration before answering the question is to take a look at the situation. SITUATION: THE WOMAN IS IN THE Emergency Room or is seeking admission. A woman in labor seeking admission to the hospital (in the ER) and saying that her BOW has ruptured should BE PUT TO BED IMMEDIATELY and the fetal heart tones taken consequently. If a woman in the Labor Room says that her membranes have ruptured, the initial nursing action is to take the fetal heart tone. 12. Answer: B. The nurse would expect that the clients cervical dilatation is 4-7 cm as the contraction duration and interval is noted for clients who are in the active phase of the first stage of labor. The maximum cervical dilatation is 10 cm, thus, letter D should be eliminated first. The first stage of labor (stage of dilatation) is divided into three phases. Latent phase 0-3 cm cervical dilatation; contractions are short and mild lasting 20-40 seconds and occurring approximately every 5-10 minutes. Active phase 4-7 cm cervical dilatation; contractions grow stronger, lasting 40-60 seconds and occur at approximately every 3-5 minutes. Transition phase 8-10 cm cervical dilatation; contractions reach their peak of intensity, occurring every 2-3 minutes with a duration of 6090 seconds. 13. Answer: C. Station -1 means that the fetal presenting part is above the level of the ischial spines. Letter A is wrong because engagement is described as Station 0. Letter B is incorrect because the statement of nurse is describing the occurrence of engagement that is again station 0. Prior to engagement the fetus is said to be "floating" or ballottable, thus letter C is the best option. Letter D, is describing crowning which is described as Station +3 or +4. 14. Answer: A. Multiparas are transported to the DR when the cervical dilatation is 7-8 cm because in multiparas dilatation may proceed before effacement is completed. Effacement must occur at the end of dilatation, however, before the fetus can be safely pushed through the cervical canal; otherwise, cervical tearing could result. Primiparas are transported to the DR when the cervical dilatation is 9-10 cm. 15. Answer: D. The nurse should spread his/her fingers lightly over the fundus to monitor the uterine contractions. 16. Answer: C. Prolactin is the hormone that produces milk in mammary glands. Uterine contractions can occur because of the interplay of the contractile enzyme adenosine triphosphate and the influence some hormones and major electrolytes which are the following: Calcium Sodium Potassium Specific contractile proteins (actin and myosin) Epinephrine and norepinephrine Oxytocin Estrogen and progesterone Prostaglandins 17. Answer: D. Dysfunctional Labor is caused by the ff: Inappropriate use of analgesia Pelvic bone contraction that has narrowed the pelvic diameter so that a client cant pass (e.g. in a client with rickets) Poor fetal position Extension rather then extension of the fetal head Overdistention of the uterus Cervical rigidity Presence of a full rectum or bladder Mother becoming exhausted from labor Primigravid status 18. Answer: D. When the contractions are hypotonic, the length of labor is increased. When the cervix is dilated for a long period of time, both the uterus and fetus are at greater risk of infection. Hypotonic contractions are not exceedingly painful because of their lack of intensity. Monitoring of bleeding through evaluation of lochia is done during the postpartum period not the intrapartum period. 19. Answer: A. Initially, the nurse should obtain an ultrasonic confirmation ruling out a CPD or cephalopelvic disproportion. Thus, A is the best answer. Oxytocin is infused after the CPD is ruled out, because if CPD is present CS will be done. Analgesic administration will further decrease the intensity of uterine contractions as its inappropriate use is one of the reasons why hypotonic contractions occur. Amniotomy (artificial rupture of membrane) may be done after oxytocin is infused to speed up the labor
20. Answer: B. During the postpartum period, the uterus should be palpated and lochia should be assessed because contractions after birth may also be hypotonic that will result to bleeding. 21. Answer: C. In placenta previa the bleeding that occurs is abrupt, painless, bright-red and sudden to frighten a woman. With abruption placenta, the bleeding is painful, the abdomen is rigid or board-like and the blood is dark-red or filled with clots. 22. Answer: C. Never attempt a pelvic or rectal examination with painless bleeding late in pregnancy because any agitation of the cervix when there is placenta previa may initiate massive hemorrhage, possibly fatal to both the mother and the fetus. The perineum should be assessed or observed or inspected for bleeding by looking over the perenial pads. An Apt or Kleihauer-Betke test (test strip procedures) can be used to detect whether the blood is of fetal or maternal origin. 23. Answer: A. placenta previa presents bleeding without pain whilst the bleeding in abruptio placenta is painful. 24. Answer: D. Signs of fetal distress include: tachycardia, bradycardia, fetal thrashing and meconium-stained amniotic fluid. 25. Answer: B. Predisposing factors for abruptio placenta: Advanced maternal age Short-umbilical cord Chronic hypertensive disease PIH Direct trauma Vasoconstriction from cocaine or cigarette use NEURO 1. If a male client experienced a cerebrovascular accident (CVA) that damaged the hypothalamus, the nurse would anticipate that the client has problems with: a. body temperature control. b. balance and equilibrium. c. visual acuity. d. thinking and reasoning. 2. A female client admitted to an acute care facility after a car accident develops signs and symptoms of increased intracranial pressure (ICP). The client is intubated and placed on mechanical ventilation to help reduce ICP. To prevent a further rise in ICP caused by suctioning, the nurse anticipates administering which drug endotracheally before suctioning? a. phenytoin (Dilantin) b. mannitol (Osmitrol) c. lidocaine (Xylocaine) d. furosemide (Lasix) 3. After striking his head on a tree while falling from a ladder, a young man age 18 is admitted to the emergency department. Hes unconscious and his pupils are nonreactive. Which intervention would be the most dangerous for the client? a. Give him a barbiturate. b. Place him on mechanical ventilation. c. Perform a lumbar puncture. d. Elevate the head of his bed. 4. a. b. c. d. 5. a. b. c. d. When obtaining the health history from a male client with retinal detachment, the nurse expects the client to report: light flashes and floaters in front of the eye. a recent driving accident while changing lanes. headaches, nausea, and redness of the eyes. frequent episodes of double vision. Which nursing diagnosis takes highest priority for a client with Parkinsons crisis? Imbalanced nutrition: Less than body requirements Ineffective airway clearance Impaired urinary elimination Risk for injury
6. To encourage adequate nutritional intake for a female client with Alzheimers disease, the nurse should: a. stay with the client and encourage him to eat. b. help the client fill out his menu.
c. give the client privacy during meals. d. fill out the menu for the client. 7. The nurse is performing a mental status examination on a male client diagnosed with subdural hematoma. This test assesses which of the following? a. Cerebellar function b. Intellectual function c. Cerebral function d. Sensory function 8. Shortly after admission to an acute care facility, a male client with a seizure disorder develops status epilepticus. The physician orders diazepam (Valium) 10 mg I.V. stat. How soon can the nurse administer a second dose of diazepam, if needed and prescribed? a. In 30 to 45 seconds b. In 10 to 15 minutes c. In 30 to 45 minutes d. In 1 to 2 hours 9. A female client complains of periorbital aching, tearing, blurred vision, and photophobia in her right eye. Ophthalmologic examination reveals a small, irregular, nonreactive pupil a condition resulting from acute iris inflammation (iritis). As part of the clients therapeutic regimen, the physician prescribes atropine sulfate (Atropisol), two drops of 0.5% solution in the right eye twice daily. Atropine sulfate belongs to which drug classification? a. Parasympathomimetic agent b. Sympatholytic agent c. Adrenergic blocker d. Cholinergic blocker 10. Emergency medical technicians transport a 27-year-old iron worker to the emergency department. They tell the nurse, He fell from a two-story building. He has a large contusion on his left chest and a hematoma in the left parietal area. He has a compound fracture of his left femur and hes comatose. We intubated him and hes maintaining an arterial oxygen saturation of 92% by pulse oximeter with a manualresuscitation bag. Which intervention by the nurse has the highest priority? a. Assessing the left leg b. Assessing the pupils c. Placing the client in Trendelenburgs position d. Assessing level of consciousness 11. An auto mechanic accidentally has battery acid splashed in his eyes. His coworkers irrigate his eyes with water for 20 minutes, and then take him to the emergency department of a nearby hospital, where he receives emergency care for corneal injury. The physician prescribes dexamethasone (Maxidex Ophthalmic Suspension), two drops of 0.1% solution to be instilled initially into the conjunctival sacs of both eyes every hour; and polymyxin B sulfate (Neosporin Ophthalmic), 0.5% ointment to be placed in the conjunctival sacs of both eyes every 3 hours. Dexamethasone exerts its therapeutic effect by: a. increasing the exudative reaction of ocular tissue. b. decreasing leukocyte infiltration at the site of ocular inflammation. c. inhibiting the action of carbonic anhydrase. d. producing a miotic reaction by stimulating and contracting the sphincter muscles of the iris. 12. Nurse April is caring for a client who underwent a lumbar laminectomy 2 days ago. Which of the following findings should the nurse consider abnormal? a. More back pain than the first postoperative day b. Paresthesia in the dermatomes near the wounds c. Urine retention or incontinence d. Temperature of 99.2 F (37.3 C) 13. After an eye examination, a male client is diagnosed with open-angle glaucoma. The physician prescribes pilocarpine ophthalmic solution (Pilocar), 0.25% gtt i, OU q.i.d. Based on this prescription, the nurse should teach the client or a family member to administer the drug by: a. instilling one drop of pilocarpine 0.25% into both eyes daily. b. instilling one drop of pilocarpine 0.25% into both eyes four times daily. c. instilling one drop of pilocarpine 0.25% into the right eye daily. d. instilling one drop of pilocarpine 0.25% into the left eye four times daily. 14. A female client whos paralyzed on the left side has been receiving physical therapy and attending teaching sessions about safety. Which behavior indicates that the client accurately understands safety measures related to paralysis? a. The client leaves the side rails down.
b. The client uses a mirror to inspect the skin. c. The client repositions only after being reminded to do so. d. The client hangs the left arm over the side of the wheelchair. 15. A male client in the emergency department has a suspected neurologic disorder. To assess gait, the nurse asks the client to take a few steps; with each step, the clients feet make a half circle. To document the clients gait, the nurse should use which term? a. Ataxic b. Dystrophic c. Helicopod d. Steppage 16. a. b. c. d. A client, age 22, is admitted with bacterial meningitis. Which hospital room would be the best choice for this client? A private room down the hall from the nurses station An isolation room three doors from the nurses station A semiprivate room with a 32-year-old client who has viral meningitis A two-bed room with a client who previously had bacterial meningitis
17. A physician diagnoses a client with myasthenia gravis, prescribing pyridostigmine (Mestinon), 60 mg P.O. every 3 hours. Before administering this anticholinesterase agent, the nurse reviews the clients history. Which preexisting condition would contraindicate the use of pyridostigmine? a. Ulcerative colitis b. Blood dyscrasia c. Intestinal obstruction d. Spinal cord injury 18. A female client is admitted to the facility for investigation of balance and coordination problems, including possible Mnires disease. When assessing this client, the nurse expects to note: a. vertigo, tinnitus, and hearing loss. b. vertigo, vomiting, and nystagmus c. vertigo, pain, and hearing impairment. d. vertigo, blurred vision, and fever. 19. A male client with a conductive hearing disorder caused by ankylosis of the stapes in the oval window undergoes a stapedectomy to remove the stapes and replace the impaired bone with a prosthesis. After the stapedectomy, the nurse should provide which client instruction? a. Lie in bed with your head elevated, and refrain from blowing your nose for 24 hours. b. Try to ambulate independently after about 24 hours. c. Shampoo your hair every day for 10 days to help prevent ear infection. d. Dont fly in an airplane, climb to high altitudes, make sudden movements, or expose yourself to loud sounds for 30 days. 20. a. b. c. d. Nurse Oliver is monitoring a client for adverse reactions to dantrolene (Dantrium). Which adverse reaction is most common? Excessive tearing Urine retention Muscle weakness Slurred speech
21. The nurse is monitoring a male client for adverse reactions to atropine sulfate (Atropine Care) eyedrops. Systemic absorption of atropine sulfate through the conjunctiva can cause which adverse reaction? a. Tachycardia b. Increased salivation c. Hypotension d. Apnea 22. A male client is admitted with a cervical spine injury sustained during a diving accident. When planning this clients care, the nurse should assign highest priority to which nursing diagnosis? a. Impaired physical mobility b. Ineffective breathing pattern c. Disturbed sensory perception (tactile) d. Self-care deficient: Dressing/grooming 23. A male client has a history of painful, continuous muscle spasms. He has taken several skeletal muscle relaxants without experiencing relief. His physician prescribes diazepam (Valium), 2 mg P.O. twice daily. In addition to being used to relieve painful muscle spasms, diazepam also is recommended for:
a. b. c. d.
long-term treatment of epilepsy. postoperative pain management of laminectomy clients. postoperative pain management of diskectomy clients treatment of spasticity associated with spinal cord lesions.
24. A female client who was found unconscious at home is brought to the hospital by a rescue squad. In the intensive care unit, the nurse checks the clients oculocephalic (dolls eye) response by: a. introducing ice water into the external auditory canal. b. touching the cornea with a wisp of cotton. c. turning the clients head suddenly while holding the eyelids open. d. shining a bright light into the pupil. 25. While reviewing a clients chart, the nurse notices that the female client has myasthenia gravis. Which of the following statements about neuromuscular blocking agents is true for a client with this condition? a. The client may be less sensitive to the effects of a neuromuscular blocking agent. b. Succinylcholine shouldnt be used; pancuronium may be used in a lower dosage. c. Pancuronium shouldnt be used; succinylcholine may be used in a lower dosage. d. Pancuronium and succinylcholine both require cautious administration. 26. a. b. c. d. A male client is color blind. The nurse understands that this client has a problem with: rods. cones. lens. aqueous humor.
27. A female client who was trapped inside a car for hours after a head-on collision is rushed to the emergency department with multiple injuries. During the neurologic examination, the client responds to painful stimuli with decerebrate posturing. This finding indicates damage to which part of the brain? a. Diencephalon b. Medulla c. Midbrain d. Cortex 28. The nurse is assessing a 37-year-old client diagnosed with multiple sclerosis. Which of the following symptoms would the nurse expect to find? a. Vision changes b. Absent deep tendon reflexes c. Tremors at rest d. Flaccid muscles 29. The nurse is caring for a male client diagnosed with a cerebral aneurysm who reports a severe headache. Which action should the nurse perform? a. Sit with the client for a few minutes. b. Administer an analgesic. c. Inform the nurse manager. d. Call the physician immediately. 30. During recovery from a cerebrovascular accident (CVA), a female client is given nothing by mouth, to help prevent aspiration. To determine when the client is ready for a liquid diet, the nurse assesses the clients swallowing ability once each shift. This assessment evaluates: a. cranial nerves I and II. b. cranial nerves III and V. c. cranial nerves VI and VIII. d. cranial nerves IX and X. ANSWER AND RATIONALE 1. Answer A. The bodys thermostat is located in the hypothalamus; therefore, injury to that area can cause problems of body temperature control. Balance and equilibrium problems are related to cerebellar damage. Visual acuity problems would occur following occipital or optic nerve injury. Thinking and reasoning problems are the result of injury to the cerebrum.
2. Answer C. Administering lidocaine via an endotracheal tube may minimize elevations in ICP caused by suctioning. Although mannitol and furosemide may be given to reduce ICP, theyre administered parenterally, not endotracheally. Phenytoin doesnt reduce ICP directly but may be used to abolish seizures, which can increase ICP. However, phenytoin isnt administered endotracheally. 3. Answer C. The clients history and assessment suggest that he may have increased intracranial pressure (ICP). If this is the case, lumbar puncture shouldnt be done because it can quickly decompress the central nervous system and, thereby, cause additional damage. After a head injury, barbiturates may be given to prevent seizures; mechanical ventilation may be required if breathing deteriorates; and elevating the head of the bed may be used to reduce ICP. 4. Answer A. The sudden appearance of light flashes and floaters in front of the affected eye is characteristic of retinal detachment. Difficulty seeing cars in another driving lane suggests gradual loss of peripheral vision, which may indicate glaucoma. Headache, nausea, and redness of the eyes are signs of acute (angle-closure) glaucoma. Double vision is common in clients with cataracts. 5. Answer B. In Parkinsons crisis, dopamine-related symptoms are severely exacerbated, virtually immobilizing the client. A client confined to bed during such a crisis is at risk for aspiration and pneumonia. Also, excessive drooling increases the risk of airway obstruction. Because of these concerns, the nursing diagnosis of Ineffective airway clearance takes highest priority. Although the other options also are appropriate, they arent immediately life-threatening. 6. Answer A. Staying with the client and encouraging him to feed himself will ensure adequate food intake. A client with Alzheimers disease can forget how to eat. Allowing privacy during meals, filling out the menu, or helping the client to complete the menu doesnt ensure adequate nutritional intake. 7. Answer C. The mental status examination assesses functions governed by the cerebrum. Some of these are orientation, attention span, judgment, and abstract reasoning. Intellectual functioning isnt the only cerebral activity. Cerebellar function testing assesses coordination, equilibrium, and fine motor movement. Sensory function testing involves assessment of pain, light-touch sensation, and temperature discrimination. 8. Answer B. When used to treat status epilepticus, diazepam may be given every 10 to 15 minutes, as needed, to a maximum dose of 30 mg. The nurse can repeat the regimen in 2 to 4 hours, if necessary, but the total dose shouldnt exceed 100 mg in 24 hours. The nurse must not administer I.V. diazepam faster than 5 mg/minute. Therefore, the dose cant be repeated in 30 to 45 seconds because the first dose wouldnt have been administered completely by that time. Waiting longer than 15 minutes to repeat the dose would increase the clients risk of complications associated with status epilepticus. 9. Answer D. Atropine sulfate is a cholinergic blocker. It isnt a parasympathomimetic agent, a sympatholytic agent, or an adrenergic blocker. 10. Answer A. In the scenario, airway and breathing are established so the nurses next priority should be circulation. With a compound fracture of the femur, there is a high risk of profuse bleeding; therefore, the nurse should assess the site. Neurologic assessment is a secondary concern to airway, breathing, and circulation. The nurse doesnt have enough data to warrant putting the client in Trendelenburgs position. 11. Answer B. Dexamethasone exerts its therapeutic effect by decreasing leukocyte infiltration at the site of ocular inflammation. This reduces the exudative reaction of diseased tissue, lessening edema, redness, and scarring. Dexamethasone and other anti-inflammatory agents dont inhibit the action of carbonic anhydrase or produce any type of miotic reaction. 12. Answer C. Urine retention or incontinence may indicate cauda equina syndrome, which requires immediate surgery. An increase in pain on the second postoperative day is common because the long-acting local anesthetic, which may have been injected during surgery, will wear off. While paresthesia is common after surgery, progressive weakness or paralysis may indicate spinal nerve compression. A mild fever is also common after surgery but is considered significant only if it reaches 101 F (38.3 C). 13. Answer B. The abbreviation "gtt" stands for drop, "i" is the apothecary symbol for the number 1, OU signifies both eyes, and "q.i.d." means four times a day. Therefore, one drop of pilocarpine 0.25% should be instilled into both eyes four times daily. 14. Answer B. Using a mirror enables the client to inspect all areas of the skin for signs of breakdown without the help of staff or family members. The client should keep the side rails up to help with repositioning and to prevent falls. The paralyzed client should take responsibility for repositioning or for reminding the staff to assist with it, if needed. A client with left-side paralysis may not realize that the left arm is hanging over the side of the wheelchair. However, the nurse should call this to the clients attention because the arm can get caught in the wheel spokes or develop impaired circulation from being in a dependent position for too long. 15. Answer C. A helicopod gait is an abnormal gait in which the clients feet make a half circle with each step. An ataxic gait is staggering and unsteady. In a dystrophic gait, the client waddles with the legs far apart. In a steppage gait, the feet and toes raise high off the floor and the heel comes down heavily with each step.
16. Answer B. A client with bacterial meningitis should be kept in isolation for at least 24 hours after admission and, during the initial acute phase, should be as close to the nurses station as possible to allow maximal observation. Placing the client in a room with a client who has viral meningitis may cause harm to both clients because the organisms causing viral and bacterial meningitis differ; either client may contract the others disease. Immunity to bacterial meningitis cant be acquired; therefore, a client who previously had bacterial meningitis shouldnt be put at risk by rooming with a client who has just been diagnosed with this disease. 17. Answer C. Anticholinesterase agents such as pyridostigmine are contraindicated in a client with a mechanical obstruction of the intestines or urinary tract, peritonitis, or hypersensitivity to anticholinesterase agents. Ulcerative colitis, blood dyscrasia, and spinal cord injury dont contraindicate use of the drug. 18. Answer A. Mnires disease, an inner ear disease, is characterized by the symptom triad of vertigo, tinnitus, and hearing loss. The combination of vertigo, vomiting, and nystagmus suggests labyrinthitis. Mnires disease rarely causes pain, blurred vision, or fever. 19. Answer D. For 30 days after a stapedectomy, the client should avoid air travel, sudden movements that may cause trauma, and exposure to loud sounds and pressure changes (such as from high altitudes). Immediately after surgery, the client should lie flat with the surgical ear facing upward; nose blowing is permitted but should be done gently and on one side at a time. The clients first attempt at postoperative ambulation should be supervised to prevent falls caused by vertigo and light-headedness. The client must avoid shampooing and swimming to keep the dressing and the ear dry. 20. Answer C. The most common adverse reaction to dantrolene is muscle weakness. The drug also may depress liver function or cause idiosyncratic hepatitis. Muscle weakness is rarely severe enough to cause slurring of speech, drooling, and enuresis. Although excessive tearing and urine retention are adverse reactions associated with dantrolene use, they arent as common as muscle weakness 21. Answer A. Systemic absorption of atropine sulfate can cause tachycardia, palpitations, flushing, dry skin, ataxia, and confusion. To minimize systemic absorption, the client should apply digital pressure over the punctum at the inner canthus for 2 to 3 minutes after instilling the drops. The drug also may cause dry mouth. It isnt known to cause hypotension or apnea. 22. Answer B. Because a cervical spine injury can cause respiratory distress, the nurse should take immediate action to maintain a patent airway and provide adequate oxygenation. The other options may be appropriate for a client with a spinal cord injury particularly during the course of recovery but dont take precedence over a diagnosis of Ineffective breathing pattern. 23. Answer D. In addition to relieving painful muscle spasms, diazepam also is recommended for treatment of spasticity associated with spinal cord lesions. Diazepams use is limited by its central nervous system effects and the tolerance that develops with prolonged use. The parenteral form of diazepam can treat status epilepticus, but the drugs sedating properties make it an unsuitable choice for long-term management of epilepsy. Diazepam isnt an analgesic agent. 24. Answer C. To elicit the oculocephalic response, which detects cranial nerve compression, the nurse turns the clients head suddenly while holding the eyelids open. Normally, the eyes move from side to side when the head is turned; in an abnormal response, the eyes remain fixed. The nurse introduces ice water into the external auditory canal when testing the oculovestibular response; normally, the clients eyes deviate to the side of ice water introduction. The nurse touches the clients cornea with a wisp of cotton to elicit the corneal reflex response, which reveals brain stem function; blinking is the normal response. Shining a bright light into the clients pupil helps evaluate brain stem and cranial nerve III functions; normally, the pupil responds by constricting. 25. Answer D. The nurse must cautiously administer pancuronium, succinylcholine, and any other neuromuscular blocking agent to a client with myasthenia gravis. Such a client isnt less sensitive to the effects of a neuromuscular blocking agent. Either succinylcholine or pancuronium can be administered in the usual adult dosage to a client with myasthenia gravis. 26. Answer B. Cones provide daylight color vision, and their stimulation is interpreted as color. If one or more types of cones are absent or defective, color blindness occurs. Rods are sensitive to low levels of illumination but cant discriminate color. The lens is responsible for focusing images. Aqueous humor is a clear watery fluid and isnt involved with color perception. 27. Answer C. Decerebrate posturing, characterized by abnormal extension in response to painful stimuli, indicates damage to the midbrain. With damage to the diencephalon or cortex, abnormal flexion (decorticate posturing) occurs when a painful stimulus is applied. Damage to the medulla results in flaccidity. 28. Answer A. Vision changes, such as diplopia, nystagmus, and blurred vision, are symptoms of multiple sclerosis. Deep tendon reflexes may be increased or hyperactive not absent. Babinskis sign may be positive. Tremors at rest arent characteristic of multiple sclerosis; however, intentional tremors, or those occurring with purposeful voluntary movement, are common in clients with multiple sclerosis. Affected muscles are spastic, rather than flaccid.
29. Answer D. The headache may be an indication that the aneurysm is leaking. The nurse should notify the physician immediately. Sitting with the client is appropriate but only after the physician has been notified of the change in the clients condition. The physician will decide whether or not administration of an analgesic is indicated. Informing the nurse manager isnt necessary. 30. Answer D. Swallowing is a motor function of cranial nerves IX and X. Cranial nerves I, II, and VIII dont possess motor functions. The motor functions of cranial nerve III include extraocular eye movement, eyelid elevation, and pupil constriction. The motor function of cranial nerve V is chewing. Cranial nerve VI controls lateral eye movement. NEURO 1. A white female client is admitted to an acute care facility with a diagnosis of cerebrovascular accident (CVA). Her history reveals bronchial asthma, exogenous obesity, and iron deficiency anemia. Which history finding is a risk factor for CVA? a. Caucasian race b. Female sex c. Obesity d. Bronchial asthma 2. to: a. b. c. d. 3. a. b. c. d. The nurse is teaching a female client with multiple sclerosis. When teaching the client how to reduce fatigue, the nurse should tell the client take a hot bath. rest in an air-conditioned room increase the dose of muscle relaxants. avoid naps during the day A male client is having a tonic-clonic seizures. What should the nurse do first? Elevate the head of the bed. Restrain the clients arms and legs. Place a tongue blade in the clients mouth. Take measures to prevent injury.
4. A female client with Guillain-Barr syndrome has paralysis affecting the respiratory muscles and requires mechanical ventilation. When the client asks the nurse about the paralysis, how should the nurse respond? a. You may have difficulty believing this, but the paralysis caused by this disease is temporary. b. Youll have to accept the fact that youre permanently paralyzed. However, you wont have any sensory loss. c. It must be hard to accept the permanency of your paralysis. d. Youll first regain use of your legs and then your arms. 5. a. b. c. d. The nurse is working on a surgical floor. The nurse must logroll a male client following a: laminectomy. thoracotomy. hemorrhoidectomy. cystectomy.
6. A female client with a suspected brain tumor is scheduled for computed tomography (CT). What should the nurse do when preparing the client for this test? a. Immobilize the neck before the client is moved onto a stretcher. b. Determine whether the client is allergic to iodine, contrast dyes, or shellfish. c. Place a cap over the clients head. d. Administer a sedative as ordered. 7. a. b. c. d. During a routine physical examination to assess a male clients deep tendon reflexes, the nurse should make sure to: use the pointed end of the reflex hammer when striking the Achilles tendon. support the joint where the tendon is being tested. tap the tendon slowly and softly hold the reflex hammer tightly.
8. A female client is admitted in a disoriented and restless state after sustaining a concussion during a car accident. Which nursing diagnosis takes highest priority in this clients plan of care? a. Disturbed sensory perception (visual) b. Self-care deficient: Dressing/grooming c. Impaired verbal communication d. Risk for injury
9. A female client with amyotrophic lateral sclerosis (ALS) tells the nurse, Sometimes I feel so frustrated. I cant do anything without help! This comment best supports which nursing diagnosis? a. Anxiety b. Powerlessness c. Ineffective denial d. Risk for disuse syndrome 10. a. b. c. d. For a male client with suspected increased intracranial pressure (ICP), a most appropriate respiratory goal is to: prevent respiratory alkalosis. lower arterial pH. promote carbon dioxide elimination. maintain partial pressure of arterial oxygen (PaO2) above 80 mm Hg
11. Nurse Maureen witnesses a neighbors husband sustain a fall from the roof of his house. The nurse rushes to the victim and determines the need to opens the airway in this victim by using which method? a. Flexed position b. Head tilt-chin lift c. Jaw thrust maneuver d. Modified head tilt-chin lift 12. The nurse is assessing the motor function of an unconscious male client. The nurse would plan to use which plan to use which of the following to test the clients peripheral response to pain? a. Sternal rub b. Nail bed pressure c. Pressure on the orbital rim d. Squeezing of the sternocleidomastoid muscle 13. A female client admitted to the hospital with a neurological problem asks the nurse whether magnetic resonance imaging may be done. The nurse interprets that the client may be ineligible for this diagnostic procedure based on the clients history of: a. Hypertension b. Heart failure c. Prosthetic valve replacement d. Chronic obstructive pulmonary disorder 14. a. b. c. d. 15. a. b. c. d. A male client is having a lumbar puncture performed. The nurse would plan to place the client in which position? Side-lying, with a pillow under the hip Prone, with a pillow under the abdomen Prone, in slight-Trendelenburgs position Side-lying, with the legs pulled up and head bent down onto chest. The nurse is positioning the female client with increased intracranial pressure. Which of the following positions would the nurse avoid? Head mildline Head turned to the side Neck in neutral position Head of bed elevated 30 to 45 degrees
16. A female client has clear fluid leaking from the nose following a basilar skull fracture. The nurse assesses that this is cerebrospinal fluid if the fluid: a. Is clear and tests negative for glucose b. Is grossly bloody in appearance and has a pH of 6 c. Clumps together on the dressing and has a pH of 7 d. Separates into concentric rings and test positive of glucose 17. A male client with a spinal cord injury is prone to experiencing automatic dysreflexia. The nurse would avoid which of the following measures to minimize the risk of recurrence? a. Strict adherence to a bowel retraining program b. Keeping the linen wrinkle-free under the client c. Preventing unnecessary pressure on the lower limbs d. Limiting bladder catheterization to once every 12 hours 18. The nurse is caring for the male client who begins to experience seizure activity while in bed. Which of the following actions by the nurse would be contraindicated?
a. b. c. d. 19. a. b. c. d.
Loosening restrictive clothing Restraining the clients limbs Removing the pillow and raising padded side rails Positioning the client to side, if possible, with the head flexed forward The nurse is assigned to care for a female client with complete right-sided hemiparesis. The nurse plans care knowing that this condition: The client has complete bilateral paralysis of the arms and legs. The client has weakness on the right side of the body, including the face and tongue. The client has lost the ability to move the right arm but is able to walk independently. The client has lost the ability to move the right arm but is able to walk independently.
20. The client with a brain attack (stroke) has residual dysphagia. When a diet order is initiated, the nurse avoids doing which of the following? a. Giving the client thin liquids b. Thickening liquids to the consistency of oatmeal c. Placing food on the unaffected side of the mouth d. Allowing plenty of time for chewing and swallowing 21. The nurse is assessing the adaptation of the female client to changes in functional status after a brain attack (stroke). The nurse assesses that the client is adapting most successfully if the client: a. Gets angry with family if they interrupt a task b. Experiences bouts of depression and irritability c. Has difficulty with using modified feeding utensils d. Consistently uses adaptive equipment in dressing self 22. Nurse Kristine is trying to communicate with a client with brain attack (stroke) and aphasia. Which of the following actions by the nurse would be least helpful to the client? a. Speaking to the client at a slower rate b. Allowing plenty of time for the client to respond c. Completing the sentences that the client cannot finish d. Looking directly at the client during attempts at speech 23. as: a. b. c. d. A female client has experienced an episode of myasthenic crisis. The nurse would assess whether the client has precipitating factors such Getting too little exercise Taking excess medication Omitting doses of medication Increasing intake of fatty foods
24. The nurse is teaching the female client with myasthenia gravis about the prevention of myasthenic and cholinergic crises. The nurse tells the client that this is most effectively done by: a. Eating large, well-balanced meals b. Doing muscle-strengthening exercises c. Doing all chores early in the day while less fatigued d. Taking medications on time to maintain therapeutic blood levels 25. A male client with Bells palsy asks the nurse what has caused this problem. The nurses response is based on an understanding that the cause is: a. Unknown, but possibly includes ischemia, viral infection, or an autoimmune problem b. Unknown, but possibly includes long-term tissue malnutrition and cellular hypoxia c. Primary genetic in origin, triggered by exposure to meningitis d. Primarily genetic in origin, triggered by exposure to neurotoxins 26. The nurse has given the male client with Bells palsy instructions on preserving muscle tone in the face and preventing denervation. The nurse determines that the client needs additional information if the client states that he or she will: a. Exposure to cold and drafts b. Massage the face with a gentle upward motion c. Perform facial exercises d. Wrinkle the forehead, blow out the cheeks, and whistle 27. Female client is admitted to the hospital with a diagnosis of Guillain-Barre syndrome. The nurse inquires during the nursing admission interview if the client has history of:
a. b. c. d.
Seizures or trauma to the brain Meningitis during the last 5 years Back injury or trauma to the spinal cord Respiratory or gastrointestinal infection during the previous month.
28. A female client with Guillian-Barre syndrome has ascending paralysis and is intubated and receiving mechanical ventilation. Which of the following strategies would the nurse incorporate in the plan of care to help the client cope with this illness? a. Giving client full control over care decisions and restricting visitors b. Providing positive feedback and encouraging active range of motion c. Providing information, giving positive feedback, and encouraging relaxation d. Providing intravaneously administered sedatives, reducing distractions and limiting visitors 29. A male client has an impairment of cranial nerve II. Specific to this impairment, the nurse would plan to do which of the following to ensure client to ensure client safety? a. Speak loudly to the client b. Test the temperature of the shower water c. Check the temperature of the food on the delivery tray. d. Provide a clear path for ambulation without obstacles 30. A female client has a neurological deficit involving the limbic system. Specific to this type of deficit, the nurse would document which of the following information related to the clients behavior. a. Is disoriented to person, place, and time b. Affect is flat, with periods of emotional lability c. Cannot recall what was eaten for breakfast today d. Demonstrate inability to add and subtract; does not know who is president ANSWER AND RATIONALE 1. Answer C. Obesity is a risk factor for CVA. Other risk factors include a history of ischemic episodes, cardiovascular disease, diabetes mellitus, atherosclerosis of the cranial vessels, hypertension, polycythemia, smoking, hypercholesterolemia, oral contraceptive use, emotional stress, family history of CVA, and advancing age. The clients race, sex, and bronchial asthma arent risk factors for CVA. 2. Answer B. Fatigue is a common symptom in clients with multiple sclerosis. Lowering the body temperature by resting in an air-conditioned room may relieve fatigue; however, extreme cold should be avoided. A hot bath or shower can increase body temperature, producing fatigue. Muscle relaxants, prescribed to reduce spasticity, can cause drowsiness and fatigue. Planning for frequent rest periods and naps can relieve fatigue. Other measures to reduce fatigue in the client with multiple sclerosis include treating depression, using occupational therapy to learn energy conservation techniques, and reducing spasticity. 3. Answer D. Protecting the client from injury is the immediate priority during a seizure. Elevating the head of the bed would have no effect on the clients condition or safety. Restraining the clients arms and legs could cause injury. Placing a tongue blade or other object in the clients mouth could damage the teeth. 4. Answer A. The nurse should inform the client that the paralysis that accompanies Guillain-Barr syndrome is only temporary. Return of motor function begins proximally and extends distally in the legs. 5. Answer A. The client who has had spinal surgery, such as laminectomy, must be logrolled to keep the spinal column straight when turning. The client who has had a thoracotomy or cystectomy may turn himself or may be assisted into a comfortable position. Under normal circumstances, hemorrhoidectomy is an outpatient procedure, and the client may resume normal activities immediately after surgery. 6. Answer B. Because CT commonly involves use of a contrast agent, the nurse should determine whether the client is allergic to iodine, contrast dyes, or shellfish. Neck immobilization is necessary only if the client has a suspected spinal cord injury. Placing a cap over the clients head may lead to misinterpretation of test results; instead, the hair should be combed smoothly. The physician orders a sedative only if the client cant be expected to remain still during the CT scan. 7. Answer B. To prevent the attached muscle from contracting, the nurse should support the joint where the tendon is being tested. The nurse should use the flat, not pointed, end of the reflex hammer when striking the Achilles tendon. (The pointed end is used to strike over small areas, such as the thumb placed over the biceps tendon.) Tapping the tendon slowly and softly wouldnt provoke a deep tendon reflex response. The nurse should hold the reflex hammer loosely, not tightly, between the thumb and fingers so it can swing in an arc. 8. Answer D. Because the client is disoriented and restless, the most important nursing diagnosis is risk for injury. Although the other options may be appropriate, theyre secondary because they dont immediately affect the clients health or safety.
9. Answer B. This comment best supports a nursing diagnosis of Powerlessness because ALS may lead to locked-in syndrome, characterized by an active and functioning mind locked in a body that cant perform even simple daily tasks. Although Anxiety and Risk for disuse syndrome may be diagnoses associated with ALS, the clients comment specifically refers to an inability to act autonomously. A diagnosis of Ineffective denial would be indicated if the client didnt seem to perceive the personal relevance of symptoms or danger. 10. Answer C. The goal of treatment is to prevent acidemia by eliminating carbon dioxide. That is because an acid environment in the brain causes cerebral vessels to dilate and therefore increases ICP. Preventing respiratory alkalosis and lowering arterial pH may bring about acidosis, an undesirable condition in this case. It isnt necessary to maintain a PaO2 as high as 80 mm Hg; 60 mm Hg will adequately oxygenate most clients. 11. Answer C. If a neck injury is suspected, the jaw thrust maneuver is used to open the airway. The head tiltchin lift maneuver produces hyperextension of the neck and could cause complications if a neck injury is present. A flexed position is an inappropriate position for opening the airway. 12. Answer B. Motor testing in the unconscious client can be done only by testing response to painful stimuli. Nail bed pressure tests a basic peripheral response. Cerebral responses to pain are tested using sternal rub, placing upward pressure on the orbital rim, or squeezing the clavicle or sternocleidomastoid muscle. 13. Answer C. The client having a magnetic resonance imaging scan has all metallic objects removed because of the magnetic field generated by the device. A careful history is obtained to determine whether any metal objects are inside the client, such as orthopedic hardware, pacemakers, artificial heart valves, aneurysm clips, or intrauterine devices. These may heat up, become dislodged, or malfunction during this procedure. The client may be ineligible if significant risk exists. 14. Answer D. The client undergoing lumbar puncture is positioned lying on the side, with the legs pulled up to the abdomen and the head bent down onto the chest. This position helps open the spaces between the vertebrae. 15. Answer B. The head of the client with increased intracranial pressure should be positioned so the head is in a neutral midline position. The nurse should avoid flexing or extending the clients neck or turning the head side to side. The head of the bed should be raised to 30 to 45 degrees. Use of proper positions promotes venous drainage from the cranium to keep intracranial pressure down. 16. Answer D. Leakage of cerebrospinal fluid (CSF) from the ears or nose may accompany basilar skull fracture. CSF can be distinguished from other body fluids because the drainage will separate into bloody and yellow concentric rings on dressing material, called a halo sign. The fluid also tests positive for glucose. 17. Answer D. The most frequent cause of autonomic dysreflexia is a distended bladder. Straight catheterization should be done every 4 to 6 hours, and foley catheters should be checked frequently to prevent kinks in the tubing. Constipation and fecal impaction are other causes, so maintaining bowel regularity is important. Other causes include stimulation of the skin from tactile, thermal, or painful stimuli. The nurse administers care to minimize risk in these areas. 18. Answer B. Nursing actions during a seizure include providing for privacy, loosening restrictive clothing, removing the pillow and raising side rails in the bed, and placing the client on one side with the head flexed forward, if possible, to allow the tongue to fall forward and facilitate drainage. The limbs are never restrained because the strong muscle contractions could cause the client harm. If the client is not in bed when seizure activity begins, the nurse lowers the client to the floor, if possible, protects the head from injury, and moves furniture that may injure the client. Other aspects of care are as described for the client who is in bed. 19. Answer B. Hemiparesis is a weakness of one side of the body that may occur after a stroke. Complete hemiparesis is weakness of the face and tongue, arm, and leg on one side. Complete bilateral paralysis does not occur in this condition. The client with right-sided hemiparesis has weakness of the right arm and leg and needs assistance with feeding, bathing, and ambulating. 20. Answer A. Before the client with dysphagia is started on a diet, the gag and swallow reflexes must have returned. The client is assisted with meals as needed and is given ample time to chew and swallow. Food is placed on the unaffected side of the mouth. Liquids are thickened to avoid aspiration. 21. Answer D. Clients are evaluated as coping successfully with lifestyle changes after a brain attack (stroke) if they make appropriate lifestyle alterations, use the assistance of others, and have appropriate social interactions. Options A, B, and C are not adaptive behaviors. 22. Answer C. Clients with aphasia after brain attack (stroke) often fatigue easily and have a short attention span. General guidelines when trying to communicate with the aphasic client include speaking more slowly and allowing adequate response time, listening to and watching attempts to communicate, and trying to put the client at ease with a caring and understanding manner. The nurse would avoid shouting (because the client is not deaf), appearing rushed for a response, and letting family members provide all the responses for the client.
23. Answer C. Myasthenic crisis often is caused by undermedication and responds to the administration of cholinergic medications, such as neostigmine (Prostigmin) and pyridostigmine (Mestinon). Cholinergic crisis (the opposite problem) is caused by excess medication and responds to withholding of medications. Too little exercise and fatty food intake are incorrect. Overexertion and overeating possibly could trigger myasthenic crisis. 24. Answer D. Clients with myasthenia gravis are taught to space out activities over the day to conserve energy and restore muscle strength. Taking medications correctly to maintain blood levels that are not too low or too high is important. Muscle-strengthening exercises are not helpful and can fatigue the client. Overeating is a cause of exacerbation of symptoms, as is exposure to heat, crowds, erratic sleep habits, and emotional stress. 25. Answer A. Bells palsy is a one-sided facial paralysis from compression of the facial nerve. The exact cause is unknown, but may include vascular ischemia, infection, exposure to viruses such as herpes zoster or herpes simplex, autoimmune disease, or a combination of these factors. 26. Answer A. Prevention of muscle atrophy with Bells palsy is accomplished with facial massage, facial exercises, and electrical stimulation of the nerves. Exposure to cold or drafts is avoided. Local application of heat to the face may improve blood flow and provide comfort. 27. Answer D. Guillain-Barr syndrome is a clinical syndrome of unknown origin that involves cranial and peripheral nerves. Many clients report a history of respiratory or gastrointestinal infection in the 1 to 4 weeks before the onset of neurological deficits. Occasionally, the syndrome can be triggered by vaccination or surgery. 28. Answer C. The client with Guillain-Barr syndrome experiences fear and anxiety from the ascending paralysis and sudden onset of the disorder. The nurse can alleviate these fears by providing accurate information about the clients condition, giving expert care and positive feedback to the client, and encouraging relaxation and distraction. The family can become involved with selected care activities and provide diversion for the client as well. 29. Answer D. Cranial nerve II is the optic nerve, which governs vision. The nurse can provide safety for the visually impaired client by clearing the path of obstacles when ambulating. Testing the shower water temperature would be useful if there were an impairment of peripheral nerves. Speaking loudly may help overcome a deficit of cranial nerve VIII (vestibulocochlear). Cranial nerve VII (facial) and IX (glossopharyngeal) control taste from the anterior two thirds and posterior third of the tongue, respectively. 30. Answer B. The limbic system is responsible for feelings (affect) and emotions. Calculation ability and knowledge of current events relates to function of the frontal lobe. The cerebral hemispheres, with specific regional functions, control orientation. Recall of recent events is controlled by the hippocampus. ONCOLOGY 1. A male client has an abnormal result on a Papanicolaou test. After admitting, he read his chart while the nurse was out of the room, the client asks what dysplasia means. Which definition should the nurse provide? a. Presence of completely undifferentiated tumor cells that dont resemble cells of the tissues of their origin b. Increase in the number of normal cells in a normal arrangement in a tissue or an organ c. Replacement of one type of fully differentiated cell by another in tissues where the second type normally isnt found d. Alteration in the size, shape, and organization of differentiated cells 2. For a female client with newly diagnosed cancer, the nurse formulates a nursing diagnosis of Anxiety related to the threat of death secondary to cancer diagnosis. Which expected outcome would be appropriate for this client? a. Client verbalizes feelings of anxiety. b. Client doesnt guess at prognosis. c. Client uses any effective method to reduce tension. d. Client stops seeking information. 3. A male client with a cerebellar brain tumor is admitted to an acute care facility. The nurse formulates a nursing diagnosis of Risk for injury. Which related-to phrase should the nurse add to complete the nursing diagnosis statement? a. Related to visual field deficits b. Related to difficulty swallowing c. Related to impaired balance d. Related to psychomotor seizures 4. A female client with cancer is scheduled for radiation therapy. The nurse knows that radiation at any treatment site may cause a certain adverse effect. Therefore, the nurse should prepare the client to expect: a. hair loss.
b. stomatitis. c. fatigue. d. vomiting. 5. Nurse April is teaching a client who suspects that she has a lump in her breast. The nurse instructs the client that a diagnosis of breast cancer is confirmed by: a. breast self-examination. b. mammography. c. fine needle aspiration. d. chest X-ray. 6. A male client undergoes a laryngectomy to treat laryngeal cancer. When teaching the client how to care for the neck stoma, the nurse should include which instruction? a. Keep the stoma uncovered. b. Keep the stoma dry. c. Have a family member perform stoma care initially until you get used to the procedure. d. Keep the stoma moist. 7. A female client is receiving chemotherapy to treat breast cancer. Which assessment finding indicates a fluid and electrolyte imbalance induced by chemotherapy? a. Urine output of 400 ml in 8 hours b. Serum potassium level of 3.6 mEq/L c. Blood pressure of 120/64 to 130/72 mm Hg d. Dry oral mucous membranes and cracked lips 8. Nurse April is teaching a group of women to perform breast self-examination. The nurse should explain that the purpose of performing the examination is to discover: a. cancerous lumps. b. areas of thickness or fullness. c. changes from previous self-examinations. d. fibrocystic masses. 9. A client, age 41, visits the gynecologist. After examining her, the physician suspects cervical cancer. The nurse reviews the clients history for risk factors for this disease. Which history finding is a risk factor for cervical cancer? a. Onset of sporadic sexual activity at age 17 b. Spontaneous abortion at age 19 c. Pregnancy complicated with eclampsia at age 27 d. Human papillomavirus infection at age 32 10. A female client is receiving methotrexate (Mexate), 12 g/m2 I.V., to treat osteogenic carcinoma. During methotrexate therapy, the nurse expects the client to receive which other drug to protect normal cells? a. probenecid (Benemid) b. cytarabine (ara-C, cytosine arabinoside [Cytosar-U]) c. thioguanine (6-thioguanine, 6-TG) d. leucovorin (citrovorum factor or folinic acid [Wellcovorin]) 11. The nurse is interviewing a male client about his past medical history. Which preexisting condition may lead the nurse to suspect that a client has colorectal cancer? a. Duodenal ulcers b. Hemorrhoids c. Weight gain d. Polyps 12. Nurse Amy is speaking to a group of women about early detection of breast cancer. The average age of the women in the group is 47. Following the American Cancer Society guidelines, the nurse should recommend that the women: a. perform breast self-examination annually. b. have a mammogram annually. c. have a hormonal receptor assay annually. d. have a physician conduct a clinical examination every 2 years. 13. A male client with a nagging cough makes an appointment to see the physician after reading that this symptom is one of the seven warning signs of cancer. What is another warning sign of cancer?
a. b. c. d.
Persistent nausea Rash Indigestion Chronic ache or pain
14. For a female client newly diagnosed with radiation-induced thrombocytopenia, the nurse should include which intervention in the plan of care? a. Administering aspirin if the temperature exceeds 102 F (38.8 C) b. Inspecting the skin for petechiae once every shift c. Providing for frequent rest periods d. Placing the client in strict isolation 15. Nurse Lucia is providing breast cancer education at a community facility. The American Cancer Society recommends that women get mammograms: a. yearly after age 40. b. after the birth of the first child and every 2 years thereafter. c. after the first menstrual period and annually thereafter. d. every 3 years between ages 20 and 40 and annually thereafter. 16. a. b. c. d. Which intervention is appropriate for the nurse caring for a male client in severe pain receiving a continuous I.V. infusion of morphine? Assisting with a naloxone challenge test before therapy begins Discontinuing the drug immediately if signs of dependence appear Changing the administration route to P.O. if the client can tolerate fluids Obtaining baseline vital signs before administering the first dose
17. A 35 years old client with ovarian cancer is prescribed hydroxyurea (Hydrea), an antimetabolite drug. Antimetabolites are a diverse group of antineoplastic agents that interfere with various metabolic actions of the cell. The mechanism of action of antimetabolites interferes with: a. cell division or mitosis during the M phase of the cell cycle. b. normal cellular processes during the S phase of the cell cycle. c. the chemical structure of deoxyribonucleic acid (DNA) and chemical binding between DNA molecules (cell cyclenonspecific). d. one or more stages of ribonucleic acid (RNA) synthesis, DNA synthesis, or both (cell cyclenonspecific). 18. a. b. c. d. 19. a. b. c. d. 20. a. b. c. d. The ABCD method offers one way to assess skin lesions for possible skin cancer. What does the A stand for? Actinic Asymmetry Arcus Assessment When caring for a male client diagnosed with a brain tumor of the parietal lobe, the nurse expects to assess: short-term memory impairment. tactile agnosia. seizures. contralateral homonymous hemianopia. A female client is undergoing tests for multiple myeloma. Diagnostic study findings in multiple myeloma include: a decreased serum creatinine level. hypocalcemia. Bence Jones protein in the urine. a low serum protein level.
21. A 35 years old client has been receiving chemotherapy to treat cancer. Which assessment finding suggests that the client has developed stomatitis (inflammation of the mouth)? a. White, cottage cheeselike patches on the tongue b. Yellow tooth discoloration c. Red, open sores on the oral mucosa d. Rust-colored sputum 22. During chemotherapy, an oncology client has a nursing diagnosis of impaired oral mucous membrane related to decreased nutrition and immunosuppression secondary to the cytotoxic effects of chemotherapy. Which nursing intervention is most likely to decrease the pain of stomatitis? a. Recommending that the client discontinue chemotherapy b. Providing a solution of hydrogen peroxide and water for use as a mouth rinse
c. Monitoring the clients platelet and leukocyte counts d. Checking regularly for signs and symptoms of stomatitis 23. a. b. c. d. What should a male client over age 52 do to help ensure early identification of prostate cancer? Have a digital rectal examination and prostate-specific antigen (PSA) test done yearly. Have a transrectal ultrasound every 5 years. Perform monthly testicular self-examinations, especially after age 50. Have a complete blood count (CBC) and blood urea nitrogen (BUN) and creatinine levels checked yearly.
24. A male client complains of sporadic epigastric pain, yellow skin, nausea, vomiting, weight loss, and fatigue. Suspecting gallbladder disease, the physician orders a diagnostic workup, which reveals gallbladder cancer. Which nursing diagnosis may be appropriate for this client? a. Anticipatory grieving b. Impaired swallowing c. Disturbed body image d. Chronic low self-esteem 25. A male client is in isolation after receiving an internal radioactive implant to treat cancer. Two hours later, the nurse discovers the implant in the bed linens. What should the nurse do first? a. Stand as far away from the implant as possible and call for help. b. Pick up the implant with long-handled forceps and place it in a lead-lined container. c. Leave the room and notify the radiation therapy department immediately. d. Put the implant back in place, using forceps and a shield for self-protection, and call for help. 26. Jeovina, with advanced breast cancer is prescribed tamoxifen (Nolvadex). When teaching the client about this drug, the nurse should emphasize the importance of reporting which adverse reaction immediately? a. Vision changes b. Hearing loss c. Headache d. Anorexia 27. A female client with cancer is being evaluated for possible metastasis. Which of the following is one of the most common metastasis sites for cancer cells? a. Liver b. Colon c. Reproductive tract d. White blood cells (WBCs) 28. A 34-year-old female client is requesting information about mammograms and breast cancer. She isnt considered at high risk for breast cancer. What should the nurse tell this client? a. She should have had a baseline mammogram before age 30. b. She should eat a low-fat diet to further decrease her risk of breast cancer. c. She should perform breast self-examination during the first 5 days of each menstrual cycle. d. When she begins having yearly mammograms, breast self-examinations will no longer be necessary. 29. Nurse Brian is developing a plan of care for marrow suppression, the major dose-limiting adverse reaction to floxuridine (FUDR). How long after drug administration does bone marrow suppression become noticeable? a. 24 hours b. 2 to 4 days c. 7 to 14 days d. 21 to 28 days 30. The nurse is preparing for a female client for magnetic resonance imaging (MRI) to confirm or rule out a spinal cord lesion. During the MRI scan, which of the following would pose a threat to the client? a. The client lies still. b. The client asks questions. c. The client hears thumping sounds. d. The client wears a watch and wedding band. ANSWER AND RATIONALE
1.Answer D. Dysplasia refers to an alteration in the size, shape, and organization of differentiated cells. The presence of completely undifferentiated tumor cells that dont resemble cells of the tissues of their origin is called anaplasia. An increase in the number of normal cells in a normal arrangement in a tissue or an organ is called hyperplasia. Replacement of one type of fully differentiated cell by another in tissues where the second type normally isnt found is called metaplasia. 2.Answer A. Verbalizing feelings is the clients first step in coping with the situational crisis. It also helps the health care team gain insight into the clients feelings, helping guide psychosocial care. Option B is inappropriate because suppressing speculation may prevent the client from coming to terms with the crisis and planning accordingly. Option C is undesirable because some methods of reducing tension, such as illicit drug or alcohol use, may prevent the client from coming to terms with the threat of death as well as cause physiologic harm. Option D isnt appropriate because seeking information can help a client with cancer gain a sense of control over the crisis. 3.Answer C. A client with a cerebellar brain tumor may suffer injury from impaired balance as well as disturbed gait and incoordination. Visual field deficits, difficulty swallowing, and psychomotor seizures may result from dysfunction of the pituitary gland, pons, occipital lobe, parietal lobe, or temporal lobe not from a cerebellar brain tumor. Difficulty swallowing suggests medullary dysfunction. Psychomotor seizures suggest temporal lobe dysfunction. 4.Answer C. Radiation therapy may cause fatigue, skin toxicities, and anorexia regardless of the treatment site. Hair loss, stomatitis, and vomiting are site-specific, not generalized, adverse effects of radiation therapy. 5.Answer C. Fine needle aspiration and biopsy provide cells for histologic examination to confirm a diagnosis of cancer. A breast selfexamination, if done regularly, is the most reliable method for detecting breast lumps early. Mammography is used to detect tumors that are too small to palpate. Chest X-rays can be used to pinpoint rib metastasis. 6.Answer D. The nurse should instruct the client to keep the stoma moist, such as by applying a thin layer of petroleum jelly around the edges, because a dry stoma may become irritated. The nurse should recommend placing a stoma bib over the stoma to filter and warm air before it enters the stoma. The client should begin performing stoma care without assistance as soon as possible to gain independence in self-care activities. 7.Answer D. Chemotherapy commonly causes nausea and vomiting, which may lead to fluid and electrolyte imbalances. Signs of fluid loss include dry oral mucous membranes, cracked lips, decreased urine output (less than 40 ml/hour), abnormally low blood pressure, and a serum potassium level below 3.5 mEq/L. 8.Answer C. Women are instructed to examine themselves to discover changes that have occurred in the breast. Only a physician can diagnose lumps that are cancerous, areas of thickness or fullness that signal the presence of a malignancy, or masses that are fibrocystic as opposed to malignant. 9.Answer D. Like other viral and bacterial venereal infections, human papillomavirus is a risk factor for cervical cancer. Other risk factors for this disease include frequent sexual intercourse before age 16, multiple sex partners, and multiple pregnancies. A spontaneous abortion and pregnancy complicated by eclampsia arent risk factors for cervical cancer. 10.Answer D. Leucovorin is administered with methotrexate to protect normal cells, which methotrexate could destroy if given alone. Probenecid should be avoided in clients receiving methotrexate because it reduces renal elimination of methotrexate, increasing the risk of methotrexate toxicity. Cytarabine and thioguanine arent used to treat osteogenic carcinoma. 11.Answer D. Colorectal polyps are common with colon cancer. Duodenal ulcers and hemorrhoids arent preexisting conditions of colorectal cancer. Weight loss not gain is an indication of colorectal cancer. 12.Answer B. The American Cancer Society guidelines state, "Women older than age 40 should have a mammogram annually and a clinical examination at least annually [not every 2 years]; all women should perform breast self-examination monthly [not annually]." The hormonal receptor assay is done on a known breast tumor to determine whether the tumor is estrogen- or progesterone-dependent. 13.Answer C. Indigestion, or difficulty swallowing, is one of the seven warning signs of cancer. The other six are a change in bowel or bladder habits, a sore that does not heal, unusual bleeding or discharge, a thickening or lump in the breast or elsewhere, an obvious change in a wart or mole, and a nagging cough or hoarseness. Persistent nausea may signal stomach cancer but isnt one of the seven major warning signs. Rash and chronic ache or pain seldom indicate cancer. 14.Answer B. Because thrombocytopenia impairs blood clotting, the nurse should inspect the client regularly for signs of bleeding, such as petechiae, purpura, epistaxis, and bleeding gums. The nurse should avoid administering aspirin because it may increase the risk of bleeding. Frequent rest periods are indicated for clients with anemia, not thrombocytopenia. Strict isolation is indicated only for clients who have highly contagious or virulent infections that are spread by air or physical contact.
15.Answer A. The American Cancer Society recommends a mammogram yearly for women over age 40. The other statements are incorrect. Its recommended that women between ages 20 and 40 have a professional breast examination (not a mammogram) every 3 years. 16.Answer D. The nurse should obtain the clients baseline blood pressure and pulse and respiratory rates before administering the initial dose and then continue to monitor vital signs throughout therapy. A naloxone challenge test may be administered before using a narcotic antagonist, not a narcotic agonist. The nurse shouldnt discontinue a narcotic agonist abruptly because withdrawal symptoms may occur. Morphine commonly is used as a continuous infusion in clients with severe pain regardless of the ability to tolerate fluids. 17.Answer B. Antimetabolites act during the S phase of the cell cycle, contributing to cell destruction or preventing cell replication. Theyre most effective against rapidly proliferating cancers. Miotic inhibitors interfere with cell division or mitosis during the M phase of the cell cycle. Alkylating agents affect all rapidly proliferating cells by interfering with DNA; they may kill dividing cells in all phases of the cell cycle and may also kill nondividing cells. Antineoplastic antibiotic agents interfere with one or more stages of the synthesis of RNA, DNA, or both, preventing normal cell growth and reproduction. 18.Answer B. When following the ABCD method for assessing skin lesions, the A stands for "asymmetry," the B for "border irregularity," the C for "color variation," and the D for "diameter." 19.Answer B. Tactile agnosia (inability to identify objects by touch) is a sign of a parietal lobe tumor. Short-term memory impairment occurs with a frontal lobe tumor. Seizures may result from a tumor of the frontal, temporal, or occipital lobe. Contralateral homonymous hemianopia suggests an occipital lobe tumor. 20.Answer C. Presence of Bence Jones protein in the urine almost always confirms the disease, but absence doesnt rule it out. Serum calcium levels are elevated because calcium is lost from the bone and reabsorbed in the serum. Serum protein electrophoresis shows elevated globulin spike. The serum creatinine level may also be increased. 21.Answer C. The tissue-destructive effects of cancer chemotherapy typically cause stomatitis, resulting in ulcers on the oral mucosa that appear as red, open sores. White, cottage cheeselike patches on the tongue suggest a candidal infection, another common adverse effect of chemotherapy. Yellow tooth discoloration may result from antibiotic therapy, not cancer chemotherapy. Rust-colored sputum suggests a respiratory disorder, such as pneumonia. 22.Answer B. To decrease the pain of stomatitis, the nurse should provide a solution of hydrogen peroxide and water for the client to use as a mouth rinse. (Commercially prepared mouthwashes contain alcohol and may cause dryness and irritation of the oral mucosa.) The nurse also may administer viscous lidocaine or systemic analgesics as prescribed. Stomatitis occurs 7 to 10 days after chemotherapy begins; thus, stopping chemotherapy wouldnt be helpful or practical. Instead, the nurse should stay alert for this potential problem to ensure prompt treatment. Monitoring platelet and leukocyte counts may help prevent bleeding and infection but wouldnt decrease pain in this highly susceptible client. Checking for signs and symptoms of stomatitis also wouldnt decrease the pain. 23.Answer A. The incidence of prostate cancer increases after age 50. The digital rectal examination, which identifies enlargement or irregularity of the prostate, and PSA test, a tumor marker for prostate cancer, are effective diagnostic measures that should be done yearly. Testicular self-examinations wont identify changes in the prostate gland due to its location in the body. A transrectal ultrasound, CBC, and BUN and creatinine levels are usually done after diagnosis to identify the extent of the disease and potential metastases 24.Answer A. Anticipatory grieving is an appropriate nursing diagnosis for this client because few clients with gallbladder cancer live more than 1 year after diagnosis. Impaired swallowing isnt associated with gallbladder cancer. Although surgery typically is done to remove the gallbladder and, possibly, a section of the liver, it isnt disfiguring and doesnt cause Disturbed body image. Chronic low self-esteem isnt an appropriate nursing diagnosis at this time because the diagnosis has just been made. 25.Answer B. If a radioactive implant becomes dislodged, the nurse should pick it up with long-handled forceps and place it in a lead-lined container, then notify the radiation therapy department immediately. The highest priority is to minimize radiation exposure for the client and the nurse; therefore, the nurse must not take any action that delays implant removal. Standing as far from the implant as possible, leaving the room with the implant still exposed, or attempting to put it back in place can greatly increase the risk of harm to the client and the nurse from excessive radiation exposure. 26.Answer A. The client must report changes in visual acuity immediately because this adverse effect may be irreversible. Tamoxifen isnt associated with hearing loss. Although the drug may cause anorexia, headache, and hot flashes, the client need not report these adverse effects immediately because they dont warrant a change in therapy. 27.Answer A. The liver is one of the five most common cancer metastasis sites. The others are the lymph nodes, lung, bone, and brain. The colon, reproductive tract, and WBCs are occasional metastasis sites.
28.Answer B. A low-fat diet (one that maintains weight within 20% of recommended body weight) has been found to decrease a womans risk of breast cancer. A baseline mammogram should be done between ages 30 and 40. Monthly breast self-examinations should be done between days 7 and 10 of the menstrual cycle. The client should continue to perform monthly breast self-examinations even when receiving yearly mammograms. 29.Answer C. Bone marrow suppression becomes noticeable 7 to 14 days after floxuridine administration. Bone marrow recovery occurs in 21 to 28 days. 30.Answer D. During an MRI, the client should wear no metal objects, such as jewelry, because the strong magnetic field can pull on them, causing injury to the client and (if they fly off) to others. The client must lie still during the MRI but can talk to those performing the test by way of the microphone inside the scanner tunnel. The client should hear thumping sounds, which are caused by the sound waves thumping on the magnetic field. Test Questions for Oncologic Disorders
1. a. b. c. d.
A 25 year old patient is inquiring about the methods or ways to detect cancer earlier. The nurse least likely identify this method by stating: Annual chest x-ray. Annual Pap smear for sexually active women only. Annual digital rectal examination for persons over age 40. Yearly physical and blood examination
2. The removal of entire breast, pectoralis major and minor muscles and neck lymph nodes which is followed by skin grafting is a procedure called: a. Simple mastectomy b. Modified radical mastectomy c. Radiation therapy d. Radical mastectomy 3. a. b. c. d. Chemotherapy is one of the therapeutic modalities for cancer. This treatment is contraindicated to which of the following conditions? Recent surgery Pregnancy Bone marrow depression All of the above
4. The nurse is preparing Cyclophosphamide (Cytoxan). Safe handling of the drug should be implemented to protect the nurse from injury. Which of the following action by the nurse should be corrected? a. The nurse should wear mask and gloves. b. Air bubbles should be expelled on wet cotton. c. Label the hanging IV bottle with ANTINEOPLASTIC CHEMOTHERAPY sign. d. Vent vials after mixing. 5. a. b. c. d. Neoplasm can be classified as either benign or malignant. The following are characteristics of malignant tumor apart from: Metastasis Infiltrates surrounding tissues Encapsulated Poorly differentiated cells
6. On a clinic visit a client who has a relative with cancer, is asking about the warning signs that may relate to cancer. The nurse correctly identifies the warning signs of cancer by responding: a. If a sore healing took a month or more to heal, cancer should be suspected. b. Presence of dry cough is one of the warning signs of cancer. c. A lump located only in the breast area may suggest the presence of cancer. d. Sudden weight loss of unexplained etiology can be a warning sign of cancer. 7. a. b. c. d. In staging and grading neoplasm TNM system is used. TNM stands for: Time, neoplasm, mode of growth Tumor, node, metastasis Tumor, neoplasm, mode of growth Time, node, metastasis
8. Breast self examination (BSE) is one of the ways to detect breast cancer earlier. The nurse is conducting a health teaching to female clients in a clinic. During evaluation the clients are asked to state what they learned. Which of the following statement made by a client needs further teaching about BSE? a. BSE is done after menstruation. b. BSE palpation is done by starting at the center going to the periphery in a circular motion. c. BSE can be done in either supine or standing position. d. BSE should start from age 20. 9. a. b. c. d. A client had undergone radiation therapy (external). The expected side effects include the following apart from: Hair loss Ulceration of oral mucous membranes Constipation Headache
10. Nurse Janet is assigned in the oncology section of the hospital. Which of the following orders should the nurse question if a client is on radiation therapy? a. Analgesics before meals b. Saline rinses every 2 hours c. Aspirin every 4 hours d. Bland diet 11. a. b. c. d. Skin reactions are common in radiation therapy. Nursing responsibilities on promoting skin integrity should be promoted apart from: Avoiding the use of ointments, powders and lotion to the area Using soft cotton fabrics for clothing Washing the area with a mild soap and water and patting it dry not rubbing it. Avoiding direct sunshine or cold.
12. Nausea and vomiting is an expected side effect of chemotherapeutic drug use. Which of the following drug should be administered to a client on chemotherapy to prevent nausea and vomiting? a. Metochlopramide (Metozol) b. Succimer (Chemet) c. Anastrazole (Arimidex) d. Busulfan (Myleran) 13. Radiation protection is very important to implement when performing nursing procedures. When the nurse is not performing any nursing procedures what distance should be maintained from the client? a. 1 feet b. 2 feet c. 2.5 feet d. 3 feet 14. a. b. c. d. 15. a. b. c. d. The following are teaching guidelines regarding radiation therapy except: The therapy is painless To promote safety, the client is assisted by therapy personnel while the machine is in operation. The client may communicate all his concerns or needs or discomforts while the machine is operating. Safety precautions are necessary only during the time of actual irradiation. Contact of client on radiation therapy should be limited only to how many minutes to promote safety of the therapy personnel? 1 minute 3 minutes 5 minutes 10 minutes
16. A client is taking Cyclophosphamide (Cytoxan) for the treatment of lymphoma. The nurse is very cautious in administering the medication because this drug poses the fatal side effect of: a. Alopecia b. Myeloma c. CNS toxicity d. Hemorrhagic cystitis 17. Cytarabine (Ara-C) is an antimetabolite that can cause a common cytarabine syndrome which includes the following apart from: a. Fever
b. Myalgia c. Chest pain d. Diarrhea 18. a. b. c. d. 19. a. b. c. d. 20. a. b. c. d. 21. a. b. c. d. 22. a. b. c. d. To provide relief from the cytarabine syndrome, which drug is given? Analgesic Aspirin Steroids Allopurinol Chemotherapeutic agents have different specific classifications. The following medications are antineoplastic antibiotics except: Doxorubicin (Adriamycin) Fluorouracil (Adrucil) Mitoxantrone (Novantrone) Bleomycin (Blenoxane) Specific classification of the chemotherapeutic agent, Vincristine ((Oncovin) is: Hormone modulator Mitotic inhibitor Antineoplastic antibiotic Antimetabolite A client is diagnosed with progressive prostate cancer. The nurse expects which drug is given? Anstrazole (arimidex) Estramustine (Emcyt) Pclitaxel (Taxol) Irinotecan (Camptosar) A client taking a chemotherapeutic agent understands the effects of therapy by stating: I will avoid eating hot and spicy foods. I should stay in my room all the time. I should limit my fluid intake to about 500 ml per day. I should notify the physician immediately if a urine color change is observed.
23. A client is diagnosed with breast cancer. The tumor size is up to 5 cm with axillary and neck lymph node involvement. The client is in what stage of breast cancer? a. Stage I b. Stage II c. Stage III d. Stage IV 24. a. b. c. d. 25. is: a. b. c. d. The classic symptoms that define breast cancer includes the following except: pink peel skin Solitary, irregularly shaped mass Firm, nontender, nonmobile mass Abnormal discharge from the nipple Surgical procedure to treat breast cancer involves the removal of the entire breast, pectoralis major muscle and the axillary lymph nodes Simple mastectomy Modified radical mastectomy Halstead Surgery Radical mastectomy
ANSWER AND RATIONALE 1. Answer: B. Early detection of cancer is promoted by annual oral examination, monthly BSE from age 20, annual chest x-ray, yearly digital rectal examination for persons over age 40, annual Pap smear from age 40 and annual physical and blood examination. Letter B is wrong because it says Pap smear should be done yearly for sexually active women. All women should have an annual pap smear by age 40 and up whether sexually active or not. 2. Answer: D. Halstead surgery also called radical mastectomy involves the removal of entire breast, pectoralis major and minor muscles and neck lymph nodes. It is followed by skin grafting. Removal of the entire breast, pectoralis major muscle and the axillary lymph nodes is a
surgical procedure called modified radical mastectomy. Simple mastectomy is the removal of the entire breast but the pectoralis muscles and nipples remain intact. 3. Answer: D. chemotherapy is contraindicated in cases of infection (chemotherapeutic agents are immunosuppressive), recent surgery (chemotherapeutic agent may retard the healing process), impaired renal and hepatic function (drugs are nephrotoxic and hepatotoxic), recent radiation therapy (immunosuppressive treatment), pregnancy (drugs can cause congenital defects) and bone marrow depression (chemo. Agents may aggravate the condition). 4. Answer: A. The nurse should be corrected if she is only wearing mask and glove because gowns should also be worn in handling chemotherapeutic drugs. The vials should be vent after mixing to reduce the internal pressure. Air bubbles are expelled on wet cotton to prevent the spread of the chemotherapeutic agent particles. 5. Answer: C. Benign grows slowly, localized, encapsulated, well differentiated cells, no metastasis, not harmful to host Malignant Grows rapidly, infiltrates surrounding tissues, not encapsulated, poorly differentiated, metastasis present, always harmful
6. Answer: D. Unexplained sudden weight loss is a warning signal of cancer. Letter A is wrong because the sore in cancer does not heal. Nagging cough not dry cough and hoarseness of voice is a sign of cancer. Presence of lump is not limited to the breast only; it can grow elsewhere that is why letter C is wrong. 7. Answer: B. TNM stands for tumor, node, and metastasis. 8. Answer: B. This client needs further teaching as palpation in BSE should start at the periphery going to the center in a circular motion. 9. Answer: C. Diarrhea not constipation is the side effect of radiation therapy. 10. Answer: C. Radiation therapy makes the platelet count decrease. Thus, nursing responsibilities should be directed at promoting safety by avoiding episodes of hemorrhage or bleeding such as physical trauma and aspirin administration. Analgesics are given before meals to alleviate the pain caused by stomatitis. Bland diet and saline rinses every 2 hours should also be done to manage stomatitis. 11. Answer: C. No soap should be used on the skin of the client undergoing radiation. Soap and irritants and may cause dryness of the patients skin. Only water should be used in washing the area. 12. Answer A. Metochlopramide (Metozol) antiemetic. Succimer (Chemet) chelating agent for lead poisoning. Anastrazole (Arimidex) hormone regulator. Busulfan (Myleran) alkylating agent 13. Answer: A. The distance of at least 3 feet / 0.9 or 1 meter should be maintained when a nurse is not performing any nursing procedures. 14. Answer: B. To promote safety to the personnel, the client will remain alone in the treatment room while the machine is in operation. The client may voice out any concern throughout the treatment because a technologist is just outside the room observing through a window or closed circuit TV. There is no residual radioactivity after radiation therapy. Safety precautions are necessary only during the time of actual irradiation. The client may resume normal activities of daily living afterwards. 15. Answer C: Principles of Radiation protection follows the DTS system. Distance (D), Time (T) and Shielding (S). Distance at least 3 feet should be maintained when a nurse is not performing any nursing procedures. Time limit contact to 5 minutes each time. Shielding use lead shield during contact with client. 16. Answer: D. Hemorrhagic cystitis is the potentially fatal side effect of Cytoxan. Myeloma is an indication for giving this medication. Alopecia is a common side effect. 17. Answer: D. Cytarabine syndrome includes fever, myalgia, bone pain, chest pain, rash, conjunctivitis and malaise. No diarrhea is included in this syndrome thus; letter D is the best choice. 18. Answer: C. Steroids may be prescribed to promote relief from cytarabine syndrome. Allopurinol is given for hyperurecemia that will result from taking some chemotherapeutic agent. 19. Answer: B. Fluorouracil (Adrucil) is an antimetabolite. 20. Answer: B. Vincristine is a mitotic inhibitor 21. Answer: B. Anstrazole (arimidex)- treatment of advanced breast cancer in post menopausal women following tamoxifen therapy. Estramustine (Emcyt) palliative treatment of metastatic and progressive prostate cancer. Pclitaxel (Taxol) treatment of ovarian cancer, breast cancer and AIDS related to Kaposis sarcoma. Irinotecan (Camptosar)- treatment of metastatic colon or rectal cancer after treatment with 5-FU. 22. Answer: A. The client should prevent hot and spicy food because of the stomatitis side effect. The client should avoid people with infection but should not isolate himself in his room all the time. Fluid intake should be increased. Urine color change is normal. 23. Answer B. Stage I tumor size up to 2 cm. Stage II tumor size up to 5 cm with axillary and neck lymph node involvement. Stage III tumor size is more than 5 cm with axillary and neck lymph node involvement. Stage IV metastasis to distant organs (liver, lungs, bone and brain). 24. Answer A. Classic symptoms that define breast cancer includes: Firm, nontender, nonmobile mass. Solitary, irregularly shaped mass. Adherence to muscle or skin causing dimpling effect. Involvement of the upper outer quadrant or central nipple portion. Asymmetry of the breasts. Orange peel skin. Retraction of nipple. Abnormal discharge from nipple. 25. Answer: B. removal of the entire breast, pectoralis major muscle and the axillary lymph nodes is a surgical procedure called modified radical mastectomy. Simple mastectomy is the removal of the entire breast but the pectoralis muscles and nipples remain intact. Halstead surgery also called radical mastectomy involves the removal of entire breast, pectoralis major and minor muscles and neck lymph nodes. It is followed by skin grafting. PSYCHIATRIC
1. Flumazenil (Romazicon) has been ordered for a male client who has overdosed on oxazepam (Serax). Before administering the medication, nurse Gina should be prepared for which common adverse effect? a. Seizures b. Shivering c. Anxiety d. Chest pain 2. a. b. c. d. 3. a. b. c. d. 4. a. b. c. d. Nurse Tim is caring for a client diagnosed with bulimia. The most appropriate initial goal for a client diagnosed with bulimia is to: avoid shopping for large amounts of food control eating impulses identify anxiety-causing situations eat only three meals per day A female client whos at high risk for suicide needs close supervision. To best ensure the clients safety, nurse Gio should: check the client frequently at irregular intervals throughout the night assure the client that the nurse will hold in confidence anything the client says repeatedly discuss previous suicide attempts with the client disregard decreased communication by the client because this is common in suicidal clients Which of the following drugs should nurse Marlyn prepare to administer to a client with a toxic acetaminophen (Tylenol) level? deferoxamine mesylate (Desferal) succimer (Chemet) flumazenil (Romazicon) acetylcysteine (Mucomyst)
5. A male client is admitted to the substance abuse unit for alcohol detoxification. Which of the following medications is nurse Apple most likely to administer to reduce the symptoms of alcohol withdrawal? a. naloxone (Narcan) b. haloperidol (Haldol) c. magnesium sulfate d. chlordiazepoxide (Librium) 6. During postprandial monitoring, a female client with bulimia nervosa tells the nurse, You can sit with me, but youre just wasting your time. After you sat with me yesterday, I was still able to purge. Today, my goal is to do it twice. What is the nurses best response? a. I trust you not to purge. b. How are you purging and when do you do it? c. Dont worry. I wont allow you to purge today. d. I know its important for you to feel in control, but Ill monitor you for 90 minutes after you eat. 7. A male client admitted to the psychiatric unit for treatment of substance abuse says to the nurse, It felt so wonderful to get high. Which of the following is the most appropriate response? a. If you continue to talk like that, Im going to stop speaking to you. b. You told me you got fired from your last job for missing too many days after taking drugs all night. c. Tell me more about how it felt to get high. d. Dont you know its illegal to use drugs? 8. a. b. c. d. 9. a. b. c. d. For a female client with anorexia nervosa, nurse Jay is aware that which goal takes the highest priority? The client will establish adequate daily nutritional intake The client will make a contract with the nurse that sets a target weight The client will identify self-perceptions about body size as unrealistic The client will verbalize the possible physiological consequences of self-starvation When interviewing the parents of an injured child, which of the following is the strongest indicator that child abuse may be a problem? The injury isnt consistent with the history or the childs age The mother and father tell different stories regarding what happened The family is poor The parents are argumentative and demanding with emergency department personnel
10. For a female client with anorexia nervosa, nurse Rose plans to include the parents in therapy sessions along with the client. What fact should the nurse remember to be typical of parents of clients with anorexia nervosa? a. They tend to overprotect their children b. They usually have a history of substance abuse
c. They maintain emotional distance from their children d. They alternate between loving and rejecting their children 11. In the emergency department, a client with facial lacerations states that her husband beat her with a shoe. After the health care team repairs her lacerations, she waits to be seen by the crisis intake nurse, who will evaluate the continued threat of violence. Suddenly the clients husband arrives, shouting that he wants to finish the job. What is the first priority of the health care worker who witnesses this scene? a. Remaining with the client and staying calm b. Calling a security guard and another staff member for assistance c. Telling the clients husband that he must leave at once d. Determining why the husband feels so angry 12. a. b. c. d. 13. a. b. c. d. . Nurse Venus is caring for a client with bulimia. Strict management of dietary intake is necessary. Which intervention is also important? Fill out the clients menu and make sure she eats at least half of what is on her tray. Let the client eat her meals in private. Then engage her in social activities for at least 2 hours after each meal Let the client choose her own food. If she eats everything she orders, then stay with her for 1 hour after each meal Let the client eat food brought in by the family if she chooses, but she should keep a strict calorie count. Nurse Mary is assigned to care for a suicidal client. Initially, which is the nurses highest care priority? Assessing the clients home environment and relationships outside the hospital Exploring the nurses own feelings about suicide Discussing the future with the client Referring the client to a clergyperson to discuss the moral implications of suicide
14. A 24-year old client with anorexia nervosa tells the nurse, When I look in the mirror, I hate what I see. I look so fat and ugly. Which strategy should the nurse use to deal with the clients distorted perceptions and feelings? a. Avoid discussing the clients perceptions and feelings b. Focus discussions on food and weight c. Avoid discussing unrealistic cultural standards regarding weight d. Provide objective data and feedback regarding the clients weight and attractiveness 15. Nurse Desmond is caring for a client being treated for alcoholism. Before initiating therapy with disulfiram (Antabuse), the nurse teaches the client that he must read labels carefully on which of the following products? a. Carbonated beverages b. Aftershave lotion c. Toothpaste d. Cheese 16. a. b. c. d. 17. a. b. c. d. Nurse Faith is developing a plan of care for a client with anorexia nervosa. Which action should the nurse include in the plan? Restrict visits with the family until the client begins to eat Provide privacy during meals Set up a strict eating plan for the client Encourage the client to exercise, which will reduce her anxiety Nurse Tina is aware that the victims of domestic violence should be assessed for what important information? Reasons they stay in the abusive relationship (for example, lack of financial autonomy and isolation) Readiness to leave the perpetrator and knowledge of resources Use of drugs or alcohol History of previous victimization
18. A male client is hospitalized with fractures of the right femur and right humerus sustained in a motorcycle accident. Police suspect the client was intoxicated at the time of the accident. Laboratory tests reveal a blood alcohol level of 0.2% (200 mg/dl). The client later admits to drinking heavily for years. During hospitalization, the client periodically complains of tingling and numbness in the hands and feet. Nurse Gio realizes that these symptoms probably result from: a. acetate accumulation b. thiamine deficiency c. triglyceride buildup. d. a below-normal serum potassium level 19. A parent brings a preschooler to the emergency department for treatment of a dislocated shoulder, which allegedly happened when the child fell down the stairs. Which action should make the nurse suspect that the child was abused? a. The child cries uncontrollably throughout the examination b. The child pulls away from contact with the physician.
c. d. 20. a. b. c. d. 21. a. b. c. d.
The child doesnt cry when the shoulder is examined The child doesnt make eye contact with the nurse. When planning care for a client who has ingested phencyclidine (PCP), nurse Wayne is aware that the following is the highest priority? Clients physical needs Clients safety needs Clients psychosocial needs Clients medical needs The nurse is aware that the outcome criteria would be appropriate for a child diagnosed with oppositional defiant disorder? Accept responsibility for own behaviors Be able to verbalize own needs and assert rights. Set firm and consistent limits with the client Allow the child to establish his own limits and boundaries
22. A male client is found sitting on the floor of the bathroom in the day treatment clinic with moderate lacerations on both wrists. Surrounded by broken glass, she sits staring blankly at her bleeding wrists while staff members call for an ambulance. How should nurse Grace approach her initially? a. Enter the room quietly and move beside her to assess her injuries b. Call for staff back-up before entering the room and restraining her c. Move as much glass away from her as possible and sit next to her quietly d. Approach her slowly while speaking in a calm voice, calling her name, and telling her that the nurse is here to help her 23. A female client with anorexia nervosa describes herself as a whale. However, the nurses assessment reveals that the client is 5 8 (1.7 m) tall and weighs only 90 lb (40.8 kg). Considering the clients unrealistic body image, which intervention should nurse Angel be included in the plan of care? a. Asking the client to compare her figure with magazine photographs of women her age b. Assigning the client to group therapy in which participants provide realistic feedback about her weight c. Confronting the client about her actual appearance during one-on-one sessions, scheduled during each shift d. Telling the client of the nurses concern for her health and desire to help her make decisions to keep her healthy 24. Eighteen hours after undergoing an emergency appendectomy, a client with a reported history of social drinking displays these vital signs: temperature, 101.6 F (38.7 C); heart rate, 126 beats/minute; respiratory rate, 24 breaths/minute; and blood pressure, 140/96 mm Hg. The client exhibits gross hand tremors and is screaming for someone to kill the bugs in the bed. Nurse Melinda should suspect: a. a postoperative infection b. alcohol withdrawal c. acute sepsis. d. pneumonia. 25. Clonidine (Catapres) can be used to treat conditions other than hypertension. Nurse Sally is aware that the following conditions might the drug be administered? a. Phencyclidine (PCP) intoxication b. Alcohol withdrawal c. Opiate withdrawal d. Cocaine withdrawal ANSWER AND RATIONALE 1. Answer A. Seizures are the most common serious adverse effect of using flumazenil to reverse benzodiazepine overdose. The effect is magnified if the client has a combined tricyclic antidepressant and benzodiazepine overdose. Less common adverse effects include shivering, anxiety, and chest pain. 2. Answer C. Bulimic behavior is generally a maladaptive coping response to stress and underlying issues. The client must identify anxietycausing situations that stimulate the bulimic behavior and then learn new ways of coping with the anxiety. Controlling shopping for large amounts of food isnt a goal early in treatment. Managing eating impulses and replacing them with adaptive coping mechanisms can be integrated into the plan of care after initially addressing stress and underlying issues. Eating three meals per day isnt a realistic goal early in treatment. 3. Answer A. Checking the client frequently but at irregular intervals prevents the client from predicting when observation will take place and altering behavior in a misleading way at these times. Option B may encourage the client to try to manipulate the nurse or seek attention for having a secret suicide plan. Option C may reinforce suicidal ideas. Decreased communication is a sign of withdrawal that may indicate the client has decided to commit suicide; the nurse shouldnt disregard it (option D) 4. Answer D. The antidote for acetaminophen toxicity is acetylcysteine. It enhances conversion of toxic metabolites to nontoxic metabolites. Deferoxamine mesylate is the antidote for iron intoxication. Succimer is an antidote for lead poisoning. Flumazenil reverses the sedative effects of benzodiazepines. 5. Answer D. Chlordiazepoxide (Librium) and other tranquilizers help reduce the symptoms of alcohol withdrawal. Haloperidol (Haldol) may be
given to treat clients with psychosis, severe agitation, or delirium. Naloxone (Narcan) is administered for narcotic overdose. Magnesium sulfate and other anticonvulsant medications are only administered to treat seizures if they occur during withdrawal. 6. Answer D. This response acknowledges that the client is testing limits and that the nurse is setting them by performing postprandial monitoring to prevent self-induced emesis. Clients with bulimia nervosa need to feel in control of the diet because they feel they lack control over all other aspects of their lives. Because their therapeutic relationships with caregivers are less important than their need to purge, they dont fear betraying the nurses trust by engaging in the activity. They commonly plot purging and rarely share their secrets about it. An authoritarian or challenging response may trigger a power struggle between the nurse and client. 7. Answer B. Confronting the client with the consequences of substance abuse helps to break through denial. Making threats (option A) isnt an effective way to promote self-disclosure or establish a rapport with the client. Although the nurse should encourage the client to discuss feelings, the discussion should focus on how the client felt before, not during, an episode of substance abuse (option C). Encouraging elaboration about his experience while getting high may reinforce the abusive behavior. The client undoubtedly is aware that drug use is illegal; a reminder to this effect (option D) is unlikely to alter behavior. 8. Answer A. According to Maslows hierarchy of needs, all humans need to meet basic physiological needs first. Because a client with anorexia nervosa eats little or nothing, the nurse must first plan to help the client meet this basic, immediate physiological need. The nurse may give lesser priority to goals that address long-term plans (as in option B), self-perception (as in option C), and potential complications (as in option D). 9. Answer A. When the childs injuries are inconsistent with the history given or impossible because of the childs age and developmental stage, the emergency department nurse should be suspicious that child abuse is occurring. The parents may tell different stories because their perception may be different regarding what happened. If they change their story when different health care workers ask the same question, this is a clue that child abuse may be a problem. Child abuse occurs in all socioeconomic groups. Parents may argue and be demanding because of the stress of having an injured child. 10. Answer A. Clients with anorexia nervosa typically come from a family with parents who are controlling and overprotective. These clients use eating to gain control of an aspect of their lives. The characteristics described in options B, C, and D isnt typical of parents of children with anorexia. 11. Answer B. The health care worker who witnesses this scene must take precautions to ensure personal as well as client safety, but shouldnt attempt to manage a physically aggressive person alone. Therefore, the first priority is to call a security guard and another staff member. After doing this, the health care worker should inform the husband what is expected, speaking in concise statements and maintaining a firm but calm demeanor. This approach makes it clear that the health care worker is in control and may diffuse the situation until the security guard arrives. Telling the husband to leave would probably be ineffective because of his agitated and irrational state. Exploring his anger doesnt take precedence over safeguarding the client and staff. 12. Answer C. Allowing the client to select her own food from the menu will help her feel some sense of control. She must then eat 100% of what she selected. Remaining with the client for at least 1 hour after eating will prevent purging. Bulimic clients should only be allowed to eat food provided by the dietary department. 13. Answer B. The nurses values, beliefs, and attitudes toward self-destructive behavior influence responses to a suicidal client; such responses set the overall mood for the nurse-client relationship. Therefore, the nurse initially must explore personal feelings about suicide to avoid conveying negative feelings to the client. Assessment of the clients home environment and relationships may reveal the need for family therapy; however, conducting such an assessment isnt a nursing priority. Discussing the future and providing anticipatory guidance can help the client prepare for future stress, but this isnt a priority. Referring the client to a clergyperson may increase the clients trust or alleviate guilt; however, it isnt the highest priority. 14. Answer D. By focusing on reality, this strategy may help the client develop a more realistic body image and gain self-esteem. Option A is inappropriate because discussing the clients perceptions and feeling wouldnt help her to identify, accept, and work through them. Focusing discussions on food and weight would give the client attention for not eating, making option B incorrect. Option C is inappropriate because recognizing unrealistic cultural standards wouldnt help the client establish more realistic weight goals. 15. Answer B. Disulfiram may be given to clients with chronic alcohol abuse who wish to curb impulse drinking. Disulfiram works by blocking the oxidation of alcohol, inhibiting the conversion of acetaldehyde to acetate. As acetaldehyde builds up in the blood, the client experiences noxious and uncomfortable symptoms. Even alcohol rubbed onto the skin can produce a reaction. The client receiving disulfiram must be taught to read ingredient labels carefully to avoid products containing alcohol such as aftershave lotions. Carbonated beverages, toothpaste, and cheese dont contain alcohol and dont need to be avoided by the client. 16. Answer C. Establishing a consistent eating plan and monitoring the clients weight are important for this disorder. The family should be included in the clients care. The client should be monitored during meals not given privacy. Exercise must be limited and supervised. 17. Answer B. Victims of domestic violence must be assessed for their readiness to leave the perpetrator and their knowledge of the resources available to them. Nurses can then provide the victims with information and options to enable them to leave when they are ready. The reasons they stay in the relationship are complex and can be explored at a later time. The use of drugs or alcohol is irrelevant. There is no evidence to suggest that previous victimization results in a persons seeking or causing abusive relationships. 18. Answer B. Numbness and tingling in the hands and feet are symptoms of peripheral polyneuritis, which results from inadequate intake of vitamin B1 (thiamine) secondary to prolonged and excessive alcohol intake. Treatment includes reducing alcohol intake, correcting nutritional deficiencies through diet and vitamin supplements, and preventing such residual disabilities as foot and wrist drop. Acetate accumulation, triglyceride buildup, and a below-normal serum potassium level are unrelated to the clients symptoms. 19. Answer C. A characteristic behavior of abused children is lack of crying when they undergo a painful procedure or are examined by a health care professional. Therefore, the nurse should suspect child abuse. Crying throughout the examination, pulling away from the physician, and not making eye contact with the nurse are normal behaviors for preschoolers. 20. Answer B. The highest priority for a client who has ingested PCP is meeting safety needs of the client as well as the staff. Drug effects are unpredictable and prolonged, and the client may lose control easily. After safety needs have been met, the clients physical, psychosocial, and medical needs can be met.
21. Answer A. Children with oppositional defiant disorder frequently violate the rights of others. They are defiant, disobedient, and blame others for their actions. Accountability for their actions would demonstrate progress for the oppositional child. Options C and D arent outcome criteria but interventions. Option B is incorrect as the oppositional child usually focuses on his own needs. 22. Answer D. Ensuring the safety of the client and the nurse is the priority at this time. Therefore, the nurse should approach the client cautiously while calling her name and talking to her in a calm, confident manner. The nurse should keep in mind that the client shouldnt be startled or overwhelmed. After explaining that the nurse is there to help, the nurse should observe the clients response carefully. If the client shows signs of agitation or confusion or poses a threat, the nurse should retreat and request assistance. The nurse shouldnt attempt to sit next to the client or examine injuries without first announcing the nurses presence and assessing the dangers of the situation. 23. Answer D. A client with anorexia nervosa has an unrealistic body image that causes consumption of little or no food. Therefore, the client needs assistance with making decisions about health. Instead of protecting the clients health, options A, B, and C may serve to make the client defensive and more entrenched in her unrealistic body image. 24. Answer B. The clients vital signs and hallucinations suggest delirium tremens or alcohol withdrawal syndrome. Although infection, acute sepsis, and pneumonia may arise as postoperative complications, they wouldnt cause this clients signs and symptoms and typically would occur later in the postoperative course 25. Answer C. Clonidine is used as adjunctive therapy in opiate withdrawal. Benzodiazepines, such as chlordiazepoxide (Librium), and neuropleptic agents, such as haloperidol, are used to treat alcohol withdrawal. Benzodiazepines and neuropleptic agents are typically used to treat PCP intoxication. Antidepressants and medications with dopaminergic activity in the brain, such as fluoxotine (Prozac), are used to treat cocaine withdrawal. PSYCH
d. begin within 2 to 7 days 13. a. b. c. d. 14. a. b. c. d. 15. a. b. c. d. 16. a. b. c. d. 17. a. b. c. d. Nurse Helen is assigned to care for a client with anorexia nervosa. Initially, which nursing intervention is most appropriate for this client? Providing one-on-one supervision during meals and for 1 hour afterward Letting the client eat with other clients to create a normal mealtime atmosphere Trying to persuade the client to eat and thus restore nutritional balance Giving the client as much time to eat as desired A female client begins to experience alcoholic hallucinosis. Nurse Joy is aware that the best nursing intervention at this time? Keeping the client restrained in bed Checking the clients blood pressure every 15 minutes and offering juices Providing a quiet environment and administering medication as needed and prescribed Restraining the client and measuring blood pressure every 30 minutes Nurse Bella is aware that assessment finding is most consistent with early alcohol withdrawal? Heart rate of 120 to 140 beats/minute Heart rate of 50 to 60 beats/minute Blood pressure of 100/70 mm Hg Blood pressure of 140/80 mm Hg Nurse Amy is aware that the client is at highest risk for suicide? One who appears depressed, frequently thinks of dying, and gives away all personal possessions One who plans a violent death and has the means readily available One who tells others that he or she might do something if life doesnt get better soon One who talks about wanting to die Nurse Penny is aware that the following medical conditions is commonly found in clients with bulimia nervosa? Allergies Cancer Diabetes mellitus Hepatitis A
18. Ken, a high school student is referred to the school nurse for suspected substance abuse. Following the nurses assessment and interventions, what would be the most desirable outcome? a. The student discusses conflicts over drug use b. The student accepts a referral to a substance abuse counselor c. The student agrees to inform his parents of the problem d. The student reports increased comfort with making choice
19. A male client who reportedly consumes 1 qt of vodka daily is admitted for alcohol detoxification. To try to prevent alcohol withdrawal symptoms, Dr. Smith is most likely to prescribe which drug? a. clozapine (Clozaril) b. thiothixene (Navane) c. lorazepam (Ativan) d. lithium carbonate (Eskalith) 20. A male client is being treated for alcoholism. After a family meeting, the clients spouse asks the nurse about ways to help the family deal with the effects of alcoholism. Nurse Lily should suggest that the family join which organization? a. Al-Anon b. Make Today Count c. Emotions Anonymous d. Alcoholics Anonymous 21. A female client is admitted to the psychiatric clinic for treatment of anorexia nervosa. To promote the clients physical health, nurse Tair should plan to: a. severely restrict the clients physical activities b. weigh the client daily, after the evening meal c. monitor vital signs, serum electrolyte levels, and acid-base balance d. instruct the client to keep an accurate record of food and fluid intake 22. Kevin is remanded by the courts for psychiatric treatment. His police record, which dates to his early teenage years, includes delinquency, running away, auto theft, and vandalism. He dropped out of school at age 16 and has been living on his own since then. His history suggests maladaptive coping, which is associated with: a. antisocial personality disorder b. borderline personality disorder c. obsessive-compulsive personality disorder d. narcissistic personality disorder 23. Mark and May seek emergency crisis intervention because he slapped her repeatedly the night before. The husband indicates that his childhood was marred by an abusive relationship with his father. When intervening with this couple, nurse Gerry knows they are at risk for repeated violence because the husband: a. has only moderate impulse control b. denies feelings of jealousy or possessiveness c. has learned violence as an acceptable behavior d. feels secure in his relationship with his wife 24. A client whose husband just left her has a recurrence of anorexia nervosa. Nurse Vic caring for her realizes that this exacerbation of anorexia nervosa results from the clients effort to: a. manipulate her husband b. gain control of one part of her life c. commit suicide d. live up to her mothers expectations 25. A male client has approached the nurse asking for advice on how to deal with his alcohol addiction. Nurse Sally should tell the client that the only effective treatment for alcoholism is: a. Psychotherapy b. total abstinence c. Alcoholics Anonymous (AA) d. aversion therapy ANSWER AND RATIONALE 1. Answer C. The elevated ST segments in this clients ECG indicate myocardial ischemia. To reverse this problem, the physician is most likely to prescribe an infusion of nitroglycerin to dilate the coronary arteries. Lidocaine and procainamide are cardiac drugs that may be indicated for this client at some point but arent used for coronary artery dilation. If a cocaine user experiences ventricular fibrillation or asystole, the physician may prescribe epinephrine. However, this drug must be used with caution because cocaine may potentiate its adrenergic effects. 2. Answer C. Low self-esteem is the highest risk factor for anorexia nervosa. Constant dieting to get down to a "desirable weight" is characteristic of the disorder. Feeling inadequate when compared to peers indicates poor self-esteem. Most clients with anorexia nervosa dont like the way they look, and their self-perception may be distorted. A girl with cachexia may perceive herself to be overweight when she looks in
the mirror. Preferring fast food over healthy food is common in this age-group. Because of the absence of body fat necessary for proper hormone production, amenorrhea is common in a client with anorexia nervosa. 3. Answer C. Haloperidol is the drug of choice for treating Tourette syndrome. Prozac, Luvox, and Paxil are antidepressants and arent used to treat Tourette syndrome 4. Answer B. An open-ended statement or question is the most therapeutic response. It encourages the widest range of client responses, makes the client an active participant in the conversation, and shows the client that the nurse is interested in his feelings. Asking the client why he drove while intoxicated can make him feel defensive and intimidated. A judgmental approach isnt therapeutic. By giving advice, the nurse suggests that the client isnt capable of making decisions, thus fostering dependency. 5. Answer D. Alcohol withdrawal syndrome includes alcohol withdrawal, alcoholic hallucinosis, and alcohol withdrawal delirium (formerly delirium tremens). Signs of alcohol withdrawal include diaphoresis, tremors, nervousness, nausea, vomiting, malaise, increased blood pressure and pulse rate, sleep disturbance, and irritability. Although diarrhea may be an early sign of alcohol withdrawal, tachycardia not bradycardia is associated with alcohol withdrawal. Dehydration and an elevated temperature may be expected, but a temperature above 101 F indicates an infection rather than alcohol withdrawal. Pruritus rarely occurs in alcohol withdrawal. If withdrawal symptoms remain untreated, seizures may arise later. 6. Answer D. This client requires a vasodilator, such as nifedipine, to treat hypertension, and a beta-adrenergic blocker, such as esmolol, to reduce the heart rate. Lidocaine, an antiarrhythmic, isnt indicated because the client doesnt have an arrhythmia. Although nitroglycerin may be used to treat coronary vasospasm, it isnt the drug of choice in hypertension. 7. Answer B. The priority goal in alcohol withdrawal is maintaining the clients safety. Committing to a drug-free lifestyle, drinking plenty of fluids, and identifying personal strengths are important goals, but ensuring the clients safety is the nurses top priority. 8. Answer A. Behavioral clues that suggest the potential for violence include a rigid posture, restlessness, glaring, a change in usual behavior, clenched hands, overtly aggressive actions, physical withdrawal, noncompliance, overreaction, hostile threats, recent alcohol ingestion or drug use, talk of past violent acts, inability to express feelings, repetitive demands and complaints, argumentativeness, profanity, disorientation, inability to focus attention, hallucinations or delusions, paranoid ideas or suspicions, and somatic complaints. Violent clients rarely exhibit depression, silence, or hypervigilance. 9. Answer D. According to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, diagnostic criteria for psychoactive substance abuse include a maladaptive pattern of such use, indicated either by continued use despite knowledge of having a persistent or recurrent social, occupational, psychological, or physical problem caused or exacerbated by substance abuse or recurrent use in dangerous situations (for example, while driving). For this client, psychoactive substance dependence must be ruled out; criteria for this disorder include a need for increasing amounts of the substance to achieve intoxication (option A), increased time and money spent on the substance (option B), inability to fulfill role obligations (option C), and typical withdrawal symptoms. 10. Answer C. The predominant behavioral characteristic of the client with borderline personality disorder is impulsiveness, especially of a physically self-destructive sort. The observation that the client has scratched wrists doesnt substantiate the other options. 11. Answer A. Cocaine use may cause such cardiac complications as coronary artery spasm, myocardial infarction, dilated cardiomyopathy, acute heart failure, endocarditis, and sudden death. Cocaine blocks reuptake of norepinephrine, epinephrine, and dopamine, causing an excess of these neurotransmitters at postsynaptic receptor sites. Consequently, the drug is more likely to cause tachyarrhythmias than bradyarrhythmias. Although neurobehavioral deficits are common in neonates born to cocaine users, they are rare in adults. As craving for the drug increases, a person whos addicted to cocaine typically experiences euphoria followed by depression, not panic disorder 12. Answer C. Acute withdrawal symptoms from alcohol may begin 6 hours after the client has stopped drinking and peak 1 to 2 days later. Delirium tremens may occur 2 to 4 days even up to 7 days after the last drink. 13. Answer A. Because the client with anorexia nervosa may discard food or induce vomiting in the bathroom, the nurse should provide oneon-one supervision during meals and for 1 hour afterward. Option B wouldnt be therapeutic because other clients may urge the client to eat and give attention for not eating. Option C would reinforce control issues, which are central to this clients underlying psychological problem. Instead of giving the client unlimited time to eat, as in option D, the nurse should set limits and let the client know what is expected. 14. Answer C. Manifestations of alcoholic hallucinosis are best treated by providing a quiet environment to reduce stimulation and administering prescribed central nervous system depressants in dosages that control symptoms without causing oversedation. Although bed rest is indicated, restraints are unnecessary unless the client poses a danger to himself or others. Also, restraints may increase agitation and make the client feel trapped and helpless when hallucinating. Offering juice is appropriate, but measuring blood pressure every 15 minutes would interrupt the clients rest. To avoid overstimulating the client, the nurse should check blood pressure every 2 hours.
15. Answer A. Tachycardia, a heart rate of 120 to 140 beats/minute, is a common sign of alcohol withdrawal. Blood pressure may be labile throughout withdrawal, fluctuating at different stages. Hypertension typically occurs in early withdrawal. Hypotension, although rare during the early withdrawal stages, may occur in later stages. Hypotension is associated with cardiovascular collapse and most commonly occurs in clients who dont receive treatment. The nurse should monitor the clients vital signs carefully throughout the entire alcohol withdrawal process. 16. Answer B. The client at highest risk for suicide is one who plans a violent death (for example, by gunshot, jumping off a bridge, or hanging), has a specific plan (for example, after the spouse leaves for work), and has the means readily available (for example, a rifle hidden in the garage). A client who gives away possessions, thinks about death, or talks about wanting to die or attempting suicide is considered at a lower risk for suicide because this behavior typically serves to alert others that the client is contemplating suicide and wishes to be helped. 17. Answer C. Bulimia nervosa can lead to many complications, including diabetes, heart disease, and hypertension. The eating disorder isnt typically associated with allergies, cancer, or hepatitis A. 18. Answer B. All of the outcomes stated are desirable; however, the best outcome is that the student would agree to seek the assistance of a professional substance abuse counselor 19. Answer C. The best choice for preventing or treating alcohol withdrawal symptoms is lorazepam, a benzodiazepine. Clozapine and thiothixene are antipsychotic agents, and lithium carbonate is an antimanic agent; these drugs arent used to manage alcohol withdrawal syndrome. 20. Answer A. Al-Anon is an organization that assists family members to share common experiences and increase their understanding of alcoholism. Make Today Count is a support group for people with life-threatening or chronic illnesses. Emotions Anonymous is a support group for people experiencing depression, anxiety, or similar conditions. Alcoholics Anonymous is an organization that helps alcoholics recovers by using a twelve-step program. 21. Answer C. An anorexic client who requires hospitalization is in poor physical condition from starvation and may die as a result of arrhythmias, hypothermia, malnutrition, infection, or cardiac abnormalities secondary to electrolyte imbalances. Therefore, monitoring the clients vital signs, serum electrolyte level, and acid base balance is crucial. Option A may worsen anxiety. Option B is incorrect because a weight obtained after breakfast is more accurate than one obtained after the evening meal. Option D would reward the client with attention for not eating and reinforce the control issues that are central to the underlying psychological problem; also, the client may record food and fluid intake inaccurately. 22. Answer A. The clients history of delinquency, running away from home, vandalism, and dropping out of school are characteristic of antisocial personality disorder. This maladaptive coping pattern is manifested by a disregard for societal norms of behavior and an inability to relate meaningfully to others. In borderline personality disorder, the client exhibits mood instability, poor self-image, identity disturbance, and labile affect. Obsessive-compulsive personality disorder is characterized by a preoccupation with impulses and thoughts that the client realizes are senseless but cant control. Narcissistic personality disorder is marked by a pattern of self-involvement, grandiosity, and demand for constant attention. 23. Answer C. Family violence usually is a learned behavior, and violence typically leads to further violence, putting this couple at risk. Repeated slapping may indicate poor, not moderate, impulse control. Violent people commonly are jealous and possessive and feel insecure in their relationships 24. Answer B. By refusing to eat, a client with anorexia nervosa is unconsciously attempting to gain control over the only part of her life she feels she can control. This eating disorder doesnt represent an attempt to manipulate others or live up to their expectations (although anorexia nervosa has a high incidence in families that emphasize achievement). The client isnt attempting to commit suicide through starvation; rather, by refusing to eat, she is expressing feelings of despair, worthlessness, and hopelessness. 25. Answer B. Total abstinence is the only effective treatment for alcoholism. Psychotherapy, attendance at AA meetings, and aversion therapy are all adjunctive therapies that can support the client in his efforts to abstain. RESPI 1. A nurse is preparing to obtain a sputum specimen from a male client. Which of the following nursing actions will facilitate obtaining the specimen? a. Limiting fluid b. Having the client take deep breaths c. Asking the client to spit into the collection container d. Asking the client to obtain the specimen after eating
2. Nurse Joy is caring for a client after a bronchoscopy and biopsy. Which of the following signs, if noticed in the client, should be reported immediately to the physician? a. Dry cough b. Hermaturia c. Bronchospasm d. Blood-streaked sputum 3. A nurse is suctioning fluids from a male client via a tracheostomy tube. When suctioning, the nurse must limit the suctioning time to a maximum of: a. 1 minute b. 5 seconds c. 10 seconds d. 30 seconds 4. A nurse is suctioning fluids from a female client through an endotracheal tube. During the suctioning procedure, the nurse notes on the monitor that the heart rate is decreasing. Which if the following is the appropriate nursing intervention? a. Continue to suction b. Notify the physician immediately c. Stop the procedure and reoxygenate the client d. Ensure that the suction is limited to 15 seconds 5. A male adult client is suspected of having a pulmonary embolus. A nurse assesses the client, knowing that which of the following is a common clinical manifestation of pulmonary embolism? a. Dyspnea b. Bradypnea c. Bradycardia d. Decreased respirations 6. A slightly obese female client with a history of allergy-induced asthma, hypertension, and mitral valve prolapse is admitted to an acute care facility for elective surgery. The nurse obtains a complete history and performs a thorough physical examination, paying special attention to the cardiovascular and respiratory systems. When percussing the clients chest wall, the nurse expects to elicit: a. Resonant sounds. b. Hyperresonant sounds. c. Dull sounds. d. Flat sounds. 7. A male client who weighs 175 lb (79.4 kg) is receiving aminophylline (Aminophyllin) (400 mg in 500 ml) at 50 ml/hour. The theophylline level is reported as 6 mcg/ml. The nurse calls the physician who instructs the nurse to change the dosage to 0.45 mg/kg/hour. The nurse should: a. Question the order because its too low. b. Question the order because its too high. c. Set the pump at 45 ml/hour. d. Stop the infusion and have the laboratory repeat the theophylline measurement. 8. The nurse is teaching a male client with chronic bronchitis about breathing exercises. Which of the following should the nurse include in the teaching? a. Make inhalation longer than exhalation. b. Exhale through an open mouth. c. Use diaphragmatic breathing. d. Use chest breathing. 9. a. b. c. d. Which phrase is used to describe the volume of air inspired and expired with a normal breath? Total lung capacity Forced vital capacity Tidal volume Residual volume
10. A male client abruptly sits up in bed, reports having difficulty breathing and has an arterial oxygen saturation of 88%. Which mode of oxygen delivery would most likely reverse the manifestations? a. Simple mask b. Non-rebreather mask
c. Face tent d. Nasal cannula 11. A female client must take streptomycin for tuberculosis. Before therapy begins, the nurse should instruct the client to notify the physician if which health concern occurs? a. Impaired color discrimination b. Increased urinary frequency c. Decreased hearing acuity d. Increased appetite 12. A male client is asking the nurse a question regarding the Mantoux test for tuberculosis. The nurse should base her response on the fact that the: a. Area of redness is measured in 3 days and determines whether tuberculosis is present. b. Skin test doesnt differentiate between active and dormant tuberculosis infection. c. Presence of a wheal at the injection site in 2 days indicates active tuberculosis. d. Test stimulates a reddened response in some clients and requires a second test in 3 months. 13. A female adult client has a tracheostomy but doesnt require continuous mechanical ventilation. When weaning the client from the tracheostomy tube, the nurse initially should plug the opening in the tube for: a. 15 to 60 seconds. b. 5 to 20 minutes. c. 30 to 40 minutes. d. 45 to 60 minutes. 14. a. b. c. d. Nurse Oliver observes constant bubbling in the water-seal chamber of a closed chest drainage system. What should the nurse conclude? The system is functioning normally The client has a pneumothorax. The system has an air leak. The chest tube is obstructed.
15. A black client with asthma seeks emergency care for acute respiratory distress. Because of this clients dark skin, the nurse should assess for cyanosis by inspecting the: a. Lips. b. Mucous membranes. c. Nail beds. d. Earlobes. 16. a. b. c. d. 17. a. b. c. d. For a male client with an endotracheal (ET) tube, which nursing action is most essential? Auscultating the lungs for bilateral breath sounds Turning the client from side to side every 2 hours Monitoring serial blood gas values every 4 hours Providing frequent oral hygiene The nurse assesses a male clients respiratory status. Which observation indicates that the client is experiencing difficulty breathing? Diaphragmatic breathing Use of accessory muscles Pursed-lip breathing Controlled breathing
18. A female client is undergoing a complete physical examination as a requirement for college. When checking the clients respiratory status, the nurse observes respiratory excursion to help assess: a. Lung vibrations. b. Vocal sounds. c. Breath sounds. d. Chest movements. 19. A male client comes to the emergency department complaining of sudden onset of diarrhea, anorexia, malaise, cough, headache, and recurrent chills. Based on the clients history and physical findings, the physician suspects legionnaires disease. While awaiting diagnostic test results, the client is admitted to the facility and started on antibiotic therapy. What is the drug of choice for treating legionnaires disease? a. Erythromycin (Erythrocin) b. Rifampin (Rifadin)
c. Amantadine (Symmetrel) d. Amphotericin B (Fungizone) 20. A male client with chronic obstructive pulmonary disease (COPD) is recovering from a myocardial infarction. Because the client is extremely weak and cant produce an effective cough, the nurse should monitor closely for: a. Pleural effusion. b. Pulmonary edema. c. Atelectasis. d. Oxygen toxicity. 21. The nurse in charge is teaching a client with emphysema how to perform pursed-lip breathing. The client asks the nurse to explain the purpose of this breathing technique. Which explanation should the nurse provide? a. It helps prevent early airway collapse. b. It increases inspiratory muscle strength. c. It decreases use of accessory breathing muscles. d. It prolongs the inspiratory phase of respiration. 22. After receiving an oral dose of codeine for an intractable cough, the male client asks the nurse, How long will it take for this drug to work? How should the nurse respond? a. In 30 minutes b. In 1 hour c. In 2.5 hours d. In 4 hours 23. A male client suffers adult respiratory distress syndrome as a consequence of shock. The clients condition deteriorates rapidly, and endotracheal (ET) intubation and mechanical ventilation are initiated. When the high-pressure alarm on the mechanical ventilator sounds, the nurse starts to check for the cause. Which condition triggers the high-pressure alarm? a. Kinking of the ventilator tubing b. A disconnected ventilator tube c. An ET cuff leak d. A change in the oxygen concentration without resetting the oxygen level alarm 24. A female client with chronic obstructive pulmonary disease (COPD) takes anhydrous theophylline, 200 mg P.O. every 8 hours. During a routine clinic visit, the client asks the nurse how the drug works. What is the mechanism of action of anhydrous theophylline in treating a nonreversible obstructive airway disease such as COPD? a. It makes the central respiratory center more sensitive to carbon dioxide and stimulates the respiratory drive. b. It inhibits the enzyme phosphodiesterase, decreasing degradation of cyclic adenosine monophosphate, a bronchodilator. c. It stimulates adenosine receptors, causing bronchodilation. d. It alters diaphragm movement, increasing chest expansion and enhancing the lungs capacity for gas exchange. 25. A male client with pneumococcal pneumonia is admitted to an acute care facility. The client in the next room is being treated for mycoplasmal pneumonia. Despite the different causes of the various types of pneumonia, all of them share which feature? a. Inflamed lung tissue b. Sudden onset c. Responsiveness to penicillin. d. Elevated white blood cell (WBC) count 26. A client with Guillain-Barr syndrome develops respiratory acidosis as a result of reduced alveolar ventilation. Which combination of arterial blood gas (ABG) values confirms respiratory acidosis? a. pH, 5.0; PaCO2 30 mm Hg b. pH, 7.40; PaCO2 35 mm Hg c. pH, 7.35; PaCO2 40 mm Hg d. pH, 7.25; PaCO2 50 mm Hg 27. A male client admitted to an acute care facility with pneumonia is receiving supplemental oxygen, 2 L/minute via nasal cannula. The clients history includes chronic obstructive pulmonary disease (COPD) and coronary artery disease. Because of these history findings, the nurse closely monitors the oxygen flow and the clients respiratory status. Which complication may arise if the client receives a high oxygen concentration? a. Apnea b. Anginal pain c. Respiratory alkalosis d. Metabolic acidosis
28. At 11 p.m., a male client is admitted to the emergency department. He has a respiratory rate of 44 breaths/minute. Hes anxious, and wheezes are audible. The client is immediately given oxygen by face mask and methylprednisolone (Depo-medrol) I.V. At 11:30 p.m., the clients arterial blood oxygen saturation is 86% and hes still wheezing. The nurse should plan to administer: a. Alprazolam (Xanax). b. Propranolol (Inderal) c. Morphine. d. Albuterol (Proventil). 29. After undergoing a thoracotomy, a male client is receiving epidural analgesia. Which assessment finding indicates that the client has developed the most serious complication of epidural analgesia? a. Heightened alertness b. Increased heart rate c. Numbness and tingling of the extremities d. Respiratory depression 30. The nurse in charge formulates a nursing diagnosis of Activity intolerance related to inadequate oxygenation and dyspnea for a client with chronic bronchitis. To minimize this problem, the nurse instructs the client to avoid conditions that increase oxygen demands. Such conditions include: a. Drinking more than 1,500 ml of fluid daily. b. Being overweight. c. Eating a high-protein snack at bedtime. d. Eating more than three large meals a day. ANSWER AND RATIONALE 1. Answer B. To obtain a sputum specimen, the client should rinse the mouth to reduce contamination, breathe deeply, and then cough into a sputum specimen container. The client should be encouraged to cough and not spit so as to obtain sputum. Sputum can be thinned by fluids or by a respiratory treatment such as inhalation of nebulized saline or water. The optimal time to obtain a specimen is on arising in the morning. 2. Answer D. If a biopsy was performed during a bronchoscopy, blood-streaked sputum is expected for several hours. Frank blood indicates hemorrhage. A dry cough may be expected. The client should be assessed for signs of complications, which would include cyanosis, dyspnea, stridor, bronchospasm, hemoptysis, hypotension, tachycardia, and dysrhythmias. Hematuria is unrelated to this procedure. 3. Answer C. Hypoxemia can be caused by prolonged suctioning, which stimulates the pacemaker cells in the heart. A vasovagal response may occur, causing bradycardia. The nurse must preoxygenate the client before suctioning and limit the suctioning pass to 10 seconds. 4. Answer C. During suctioning, the nurse should monitor the client closely for side effects, including hypoxemia, cardiac irregularities such as a decrease in heart rate resulting from vagal stimulation, mucosal trauma, hypotension, and paroxysmal coughing. If side effects develop, especially cardiac irregularities, the procedure is stopped and the client is reoxygenated. 5. Answer A. The common clinical manifestations of pulmonary embolism are tachypnea, tachycardia, dyspnea, and chest pain. 6. Answer A. When percussing the chest wall, the nurse expects to elicit resonant sounds low-pitched, hollow sounds heard over normal lung tissue. Hyperresonant sounds indicate increased air in the lungs or pleural space; theyre louder and lower pitched than resonant sounds. Although hyperresonant sounds occur in such disorders as emphysema and pneumothorax, they may be normal in children and very thin adults. Dull sounds, normally heard only over the liver and heart, may occur over dense lung tissue, such as from consolidation or a tumor. Dull sounds are thudlike and of medium pitch. Flat sounds, soft and high-pitched, are heard over airless tissue and can be replicated by percussing the thigh or a bony structure. 7. Answer A. A therapeutic theophylline level is 10 to 20 mcg/ml. The client is currently receiving 0.5 mg/kg/hour of aminophylline. Because the clients theophylline level is sub-therapeutic, reducing the dose (which is what the physicians order would do) would be inappropriate. Therefore, the nurse should question the order. 8. Answer C. In chronic bronchitis the diaphragm is flat and weak. Diaphragmatic breathing helps to strengthen the diaphragm and maximizes ventilation. Exhalation should be longer than inhalation to prevent collapse of the bronchioles. The client with chronic bronchitis should exhale through pursed lips to prolong exhalation, keep the bronchioles from collapsing, and prevent air trapping. Diaphragmatic breathing not chest breathing increases lung expansion. 9. Answer C. Tidal volume refers to the volume of air inspired and expired with a normal breath. Total lung capacity is the maximal amount of air the lungs and respiratory passages can hold after a forced inspiration. Forced vital capacity is the vital capacity performed with a maximally forced expiration. Residual volume is the maximal amount of air left in the lung after a maximal expiration. 10. Answer B. A non-rebreather mask can deliver levels of the fraction of inspired oxygen (FIO2) as high as 100%. Other modes simple mask, face tent, and nasal cannula deliver lower levels of FIO2. 11. Answer C. Decreased hearing acuity indicates ototoxicity, a serious adverse effect of streptomycin therapy. The client should notify the physician immediately if it occurs so that streptomycin can be discontinued and an alternative drug can be prescribed. The other options arent associated with streptomycin. Impaired color discrimination indicates color blindness; increased urinary frequency and increased appetite accompany diabetes mellitus.
12. Answer B. The Mantoux test doesnt differentiate between active and dormant infections. If a positive reaction occurs, a sputum smear and culture as well as a chest X-ray are necessary to provide more information. Although the area of redness is measured in 3 days, a second test may be needed; neither test indicates that tuberculosis is active. In the Mantoux test, an induration 5 to 9 mm in diameter indicates a borderline reaction; a larger induration indicates a positive reaction. The presence of a wheal within 2 days doesnt indicate active tuberculosis. 13. Answer B. Initially, the nurse should plug the opening in the tracheostomy tube for 5 to 20 minutes, then gradually lengthen this interval according to the clients respiratory status. A client who doesnt require continuous mechanical ventilation already is breathing without assistance, at least for short periods; therefore, plugging the opening of the tube for only 15 to 60 seconds wouldnt be long enough to reveal the clients true tolerance to the procedure. Plugging the opening for more than 20 minutes would increase the risk of acute respiratory distress because the client requires an adjustment period to start breathing normally. 14. Answer C. Constant bubbling in the chamber indicates an air leak and requires immediate intervention. The client with a pneumothorax will have intermittent bubbling in the water-seal chamber. Clients without a pneumothorax should have no evidence of bubbling in the chamber. If the tube is obstructed, the nurse should notice that the fluid has stopped fluctuating in the water-seal chamber. 15. Answer B. Skin color doesnt affect the mucous membranes. The lips, nail beds, and earlobes are less reliable indicators of cyanosis because theyre affected by skin color. 16. Answer A. For a client with an ET tube, the most important nursing action is auscultating the lungs regularly for bilateral breath sounds to ensure proper tube placement and effective oxygen delivery. Although the other options are appropriate for this client, theyre secondary to ensuring adequate oxygenation. 17. Answer B. The use of accessory muscles for respiration indicates the client is having difficulty breathing. Diaphragmatic and pursedlip breathing are two controlled breathing techniques that help the client conserve energy. 18. Answer D. The nurse observes respiratory excursion to help assess chest movements. Normally, thoracic expansion is symmetrical; unequal expansion may indicate pleural effusion, atelectasis, pulmonary embolus, or a rib or sternum fracture. The nurse assesses vocal sounds to evaluate air flow when checking for tactile fremitus; after asking the client to say "99," the nurse palpates the vibrations transmitted from the bronchopulmonary system along the solid surfaces of the chest wall to the nurses palms. The nurse assesses breath sounds during auscultation. 19. Answer A. Erythromycin is the drug of choice for treating legionnaires disease. Rifampin may be added to the regimen if erythromycin alone is ineffective; however, it isnt administered first. Amantadine, an antiviral agent, and amphotericin B, an antifungal agent, are ineffective against legionnaires disease, which is caused by bacterial infection. 20. Answer C. In a client with COPD, an ineffective cough impedes secretion removal. This, in turn, causes mucus plugging, which leads to localized airway obstruction a known cause of atelectasis. An ineffective cough doesnt cause pleural effusion (fluid accumulation in the pleural space). Pulmonary edema usually results from left-sided heart failure, not an ineffective cough. Although many noncardiac conditions may cause pulmonary edema, an ineffective cough isnt one of them. Oxygen toxicity results from prolonged administration of high oxygen concentrations, not an ineffective cough. 21. Answer A. Pursed-lip breathing helps prevent early airway collapse. Learning this technique helps the client control respiration during periods of excitement, anxiety, exercise, and respiratory distress. To increase inspiratory muscle strength and endurance, the client may need to learn inspiratory resistive breathing. To decrease accessory muscle use and thus reduce the work of breathing, the client may need to learn diaphragmatic (abdominal) breathing. In pursed-lip breathing, the client mimics a normal inspiratoryexpiratory (I:E) ratio of 1:2. (A client with emphysema may have an I:E ratio as high as 1:4.) 22. Answer A. Codeines onset of action is 30 minutes. Its peak concentration occurs in about 1 hour; its half-life, in 2.5 hours; and its duration of action is 4 to 6 hours. 23. Answer A. Conditions that trigger the high-pressure alarm include kinking of the ventilator tubing, bronchospasm or pulmonary embolus, mucus plugging, water in the tube, coughing or biting on the ET tube, and the clients being out of breathing rhythm with the ventilator. A disconnected ventilator tube or an ET cuff leak would trigger the low-pressure alarm. Changing the oxygen concentration without resetting the oxygen level alarm would trigger the oxygen alarm. 24. Answer A. Anhydrous theophylline and other methylxanthine agents make the central respiratory center more sensitive to CO2 and stimulate the respiratory drive. Inhibition of phosphodiesterase is the drugs mechanism of action in treating asthma and other reversible obstructive airway diseases not COPD. Methylxanthine agents inhibit rather than stimulate adenosine receptors. Although these agents reduce diaphragmatic fatigue in clients with chronic bronchitis or emphysema, they dont alter diaphragm movement to increase chest expansion and enhance gas exchange. 25. Answer A. The common feature of all types of pneumonia is an inflammatory pulmonary response to the offending organism or agent. Although most types of pneumonia have a sudden onset, a few (such as anaerobic bacterial pneumonia and mycoplasmal pneumonia) have an insidious onset. Antibiotic therapy is the primary treatment for most types of pneumonia; however, the antibiotic must be specific for the causative agent, which may not be responsive to penicillin. A few types of pneumonia, such as viral pneumonia, arent treated with antibiotics. Although pneumonia usually causes an elevated WBC count, some types, such as mycoplasmal pneumonia, dont. 26. Answer D. In respiratory acidosis, ABG analysis reveals an arterial pH below 7.35 and partial pressure of arterial carbon dioxide (PaCO2) above 45 mm Hg. Therefore, the combination of a pH value of 7.25 and a PaCO2 value of 50 mm Hg confirms respiratory acidosis. A pH value of 5.0 with a PaCO2 value of 30 mm Hg indicates respiratory alkalosis. Options B and C represent normal ABG values, reflecting normal gas exchange in the lungs. 27. Answer A. Hypoxia is the main breathing stimulus for a client with COPD. Excessive oxygen administration may lead to apnea by removing that stimulus. Anginal pain results from a reduced myocardial oxygen supply. A client with COPD may have anginal pain from generalized vasoconstriction secondary to hypoxia; however, administering oxygen at any concentration dilates blood vessels, easing anginal pain. Respiratory alkalosis results from alveolar hyperventilation, not excessive oxygen administration. In a client with COPD, high oxygen concentrations decrease the ventilatory drive, leading to respiratory acidosis, not alkalosis. High oxygen concentrations dont cause metabolic acidosis.
28. Answer D. The client is hypoxemic because of bronchoconstriction as evidenced by wheezes and a subnormal arterial oxygen saturation level. The clients greatest need is bronchodilation, which can be accomplished by administering bronchodilators. Albuterol is a beta2 adrenergic agonist, which causes dilation of the bronchioles. Its given by nebulization or metered-dose inhalation and may be given as often as every 30 to 60 minutes until relief is accomplished. Alprazolam is an anxiolytic and central nervous system depressant, which could suppress the clients breathing. Propranolol is contraindicated in a client whos wheezing because its a beta2 adrenergic antagonist. Morphine is a respiratory center depressant and is contraindicated in this situation. 29. Answer D. Respiratory depression is the most serious complication of epidural analgesia. Other potential complications include hypotension, decreased sensation and movement of the extremities, allergic reactions, and urine retention. Typically, epidural analgesia causes central nervous system depression (indicated by drowsiness) as well as a decreased heart rate and blood pressure. 30. Answer B. Conditions that increase oxygen demands include obesity, smoking, exposure to temperature extremes, and stress. A client with chronic bronchitis should drink at least 2,000 ml of fluid daily to thin mucus secretions; restricting fluid intake may be harmful. The nurse should encourage the client to eat a high-protein snack at bedtime because protein digestion produces an amino acid with sedating effects that may ease the insomnia associated with chronic bronchitis. Eating more than three large meals a day may cause fullness, making breathing uncomfortable and difficult; however, it doesnt increase oxygen demands. To help maintain adequate nutritional intake, the client with chronic bronchitis should eat small, frequent meals (up to six a day). RESPI 1. The nurse is caring for a male client with a chest tube. If the chest drainage system is accidentally disconnected, what should the nurse plan to do? a. Place the end of the chest tube in a container of sterile saline. b. Apply an occlusive dressing and notify the physician. c. Clamp the chest tube immediately. d. Secure the chest tube with tape. 2. A male elderly client is admitted to an acute care facility with influenza. The nurse monitors the client closely for complications. What is the most common complication of influenza? a. Septicemia b. Pneumonia c. Meningitis d. Pulmonary edema 3. A female client has a tracheostomy but doesnt require continuous mechanical ventilation. When weaning the client from the tracheostomy tube, the nurse initially should plug the opening in the tube for: a. 15 to 60 seconds. b. 5 to 20 minutes. c. 30 to 40 minutes. d. 45 to 60 minutes. 4. Gina, a home health nurse is visiting a home care client with advanced lung cancer. Upon assessing the client, the nurse discovers wheezing, bradycardia, and a respiratory rate of 10 breaths/minute. These signs are associated with which condition? a. Hypoxia b. Delirium c. Hyperventilation d. Semiconsciousness 5. A male client with Guillain-Barr syndrome develops respiratory acidosis as a result of reduced alveolar ventilation. Which combination of arterial blood gas (ABG) values confirms respiratory acidosis? a. pH, 5.0; PaCO2 30 mm Hg b. pH, 7.40; PaCO2 35 mm Hg c. pH, 7.35; PaCO2 40 mm Hg d. pH, 7.25; PaCO2 50 mm Hg 6. A female client with interstitial lung disease is prescribed prednisone (Deltasone) to control inflammation. During client teaching, the nurse stresses the importance of taking prednisone exactly as prescribed and cautions against discontinuing the drug abruptly. A client who discontinues prednisone abruptly may experience: a. hyperglycemia and glycosuria. b. acute adrenocortical insufficiency. c. GI bleeding. d. restlessness and seizures.
7. A male client is admitted to the health care facility for treatment of chronic obstructive pulmonary disease. Which nursing diagnosis is most important for this client? a. Activity intolerance related to fatigue b. Anxiety related to actual threat to health status c. Risk for infection related to retained secretions d. Impaired gas exchange related to airflow obstruction 8. A male client abruptly sits up in bed, reports having difficulty breathing and has an arterial oxygen saturation of 88%. Which mode of oxygen delivery would most likely reverse the manifestations? a. Simple mask b. Non-rebreather mask c. Face tent d. Nasal cannula 9. A male adult client with cystic fibrosis is admitted to an acute care facility with an acute respiratory infection. Prescribed respiratory treatment includes chest physiotherapy. When should the nurse perform this procedure? a. Immediately before a meal b. At least 2 hours after a meal c. When bronchospasms occur d. When secretions have mobilized 10. On arrival at the intensive care unit, a critically ill female client suffers respiratory arrest and is placed on mechanical ventilation. The physician orders pulse oximetry to monitor the clients arterial oxygen saturation (SaO2) noninvasively. Which vital sign abnormality may alter pulse oximetry values? a. Fever b. Tachypnea c. Tachycardia d. Hypotension 11. The nurse is caring for a male client who recently underwent a tracheostomy. The first priority when caring for a client with a tracheostomy is: a. helping him communicate. b. keeping his airway patent. c. encouraging him to perform activities of daily living. d. preventing him from developing an infection. 12. a. b. c. d. 13. a. b. c. d. For a male client with chronic obstructive pulmonary disease, which nursing intervention would help maintain a patent airway? Restricting fluid intake to 1,000 ml/day Enforcing absolute bed rest Teaching the client how to perform controlled coughing Administering prescribed sedatives regularly and in large amounts The amount of air inspired and expired with each breath is called: tidal volume. residual volume. vital capacity. dead-space volume.
14. A male client with pneumonia develops respiratory failure and has a partial pressure of arterial oxygen of 55 mm Hg. Hes placed on mechanical ventilation with a fraction of inspired oxygen (FIO2) of 0.9. The nursing goal should be to reduce the FIO2 to no greater than: a. 0.21 b. 0.35 c. 0.5 d. 0.7 15. Nurse Mickey is administering a purified protein derivative (PPD) test to a homeless client. Which of the following statements concerning PPD testing is true? a. A positive reaction indicates that the client has active tuberculosis (TB). b. A positive reaction indicates that the client has been exposed to the disease. c. A negative reaction always excludes the diagnosis of TB. d. The PPD can be read within 12 hours after the injection.
16. Nurse Murphy administers albuterol (Proventil), as prescribed, to a client with emphysema. Which finding indicates that the drug is producing a therapeutic effect? a. Respiratory rate of 22 breaths/minute b. Dilated and reactive pupils c. Urine output of 40 ml/hour d. Heart rate of 100 beats/minute 17. a. b. c. d. 18. a. b. c. d. What is the normal pH range for arterial blood? 7 to 7.49 7.35 to 7.45 7.50 to 7.60 7.55 to 7.65 Before weaning a male client from a ventilator, which assessment parameter is most important for the nurse to review? Fluid intake for the last 24 hours Baseline arterial blood gas (ABG) levels Prior outcomes of weaning Electrocardiogram (ECG) results
19. Which of the following would be most appropriate for a male client with an arterial blood gas (ABG) of pH 7.5, PaCO2 26 mm Hg, O2 saturation 96%, HCO3 24 mEq/L, and PaO2 94 mm Hg? a. Administer a prescribed decongestant. b. Instruct the client to breathe into a paper bag. c. Offer the client fluids frequently. d. Administer prescribed supplemental oxygen. 20. A female client is receiving supplemental oxygen. When determining the effectiveness of oxygen therapy, which arterial blood gas value is most important? a. pH b. Bicarbonate (HCO3) c. Partial pressure of arterial oxygen (PaO2) d. Partial pressure of arterial carbon dioxide (PaCO2) 21. Nurse Julia is caring for a client who has a tracheostomy and temperature of 103 F (39.4 C). Which of the following interventions will most likely lower the clients arterial blood oxygen saturation? a. Endotracheal suctioning b. Encouragement of coughing c. Use of cooling blanket d. Incentive spirometry 22. For a male client who has a chest tube connected to a closed water-seal drainage system, the nurse should include which action in the plan of care? a. Measuring and documenting the drainage in the collection chamber b. Maintaining continuous bubbling in the water-seal chamber c. Keeping the collection chamber at chest level d. Stripping the chest tube every hour 23. Nurse Eve formulates a nursing diagnosis of Activity intolerance related to inadequate oxygenation and dyspnea for a client with chronic bronchitis. To minimize this problem, the nurse instructs the client to avoid conditions that increase oxygen demands. Such conditions include: a. drinking more than 1,500 ml of fluid daily. b. being overweight. c. eating a high-protein snack at bedtime. d. eating more than three large meals a day. 24. A black male client with asthma seeks emergency care for acute respiratory distress. Because of this clients dark skin, the nurse should assess for cyanosis by inspecting the: a. lips. b. mucous membranes. c. nail beds. d. earlobes.
25. A female client with asthma is receiving a theophylline preparation to promote bronchodilation. Because of the risk of drug toxicity, the nurse must monitor the clients serum theophylline level closely. The nurse knows that the therapeutic theophylline concentration falls within which range? a. 1 to 2 mcg/ml b. 2 to 5 mcg/ml c. 5 to 10 mcg/ml d. 10 to 20 mcg/ml 26. a. b. c. d. A male client is to receive I.V. vancomycin (Vancocin). When preparing to administer this drug, the nurse should keep in mind that: vancomycin should be infused over 60 to 90 minutes in a large volume of fluid. vancomycin may cause irreversible neutropenia. vancomycin should be administered rapidly in a large volume of fluid. vancomycin should be administered over 1 to 2 minutes as an I.V. bolus.
27. Before seeing a newly assigned female client with respiratory alkalosis, the nurse quickly reviews the clients medical history. Which condition is a predisposing factor for respiratory alkalosis? a. Myasthenia gravis b. Type 1 diabetes mellitus c. Extreme anxiety d. Narcotic overdose 28. At 11 p.m., a male client is admitted to the emergency department. He has a respiratory rate of 44 breaths/minute. Hes anxious, and wheezes are audible. The client is immediately given oxygen by face mask and methylprednisolone (Depo-medrol) I.V. At 11:30 p.m., the clients arterial blood oxygen saturation is 86% and hes still wheezing. The nurse should plan to administer: a. alprazolam (Xanax). b. propranolol (Inderal) c. morphine. d. albuterol (Proventil). 29. a. b. c. d. Pulmonary disease (COPD), which nursing action best promotes adequate gas exchange? Encouraging the client to drink three glasses of fluid daily Keeping the client in semi-Fowlers position Using a high-flow Venturi mask to deliver oxygen as prescribed Administering a sedative as prescribed
30. Nurse Joana is teaching a client with emphysema how to perform pursed-lip breathing. The client asks the nurse to explain the purpose of this breathing technique. Which explanation should the nurse provide? a. It helps prevent early airway collapse. b. It increases inspiratory muscle strength c. It decreases use of accessory breathing muscles. d. It prolongs the inspiratory phase of respiration. ANSWER AND RATIONALE 1. Answer A. If a chest drainage system is disconnected, the nurse may place the end of the chest tube in a container of sterile saline or water to prevent air from entering the chest tube, thereby preventing negative respiratory pressure. The nurse should apply an occlusive dressing if the chest tube is pulled out not if the system is disconnected. The nurse shouldnt clamp the chest tube because clamping increases the risk of tension pneumothorax. The nurse should tape the chest tube securely to prevent it from being disconnected, rather than taping it after it has been disconnected. 2. Answer B. Pneumonia is the most common complication of influenza. It may be either primary influenza viral pneumonia or pneumonia secondary to a bacterial infection. Other complications of influenza include myositis, exacerbation of chronic obstructive pulmonary disease, and Reyes syndrome. Myocarditis, pericarditis, transverse myelitis, and encephalitis are rare complications of influenza. Although septicemia may arise when any infection becomes overwhelming, it rarely results from influenza. Meningitis and pulmonary edema arent associated with influenza. 3. Answer B. Initially, the nurse should plug the opening in the tracheostomy tube for 5 to 20 minutes, and then gradually lengthen this interval according to the clients respiratory status. A client who doesnt require continuous mechanical ventilation already is breathing without assistance, at least for short periods; therefore, plugging the opening of the tube for only 15 to 60 seconds wouldnt be long enough to reveal the clients true tolerance to the procedure. Plugging the opening for more than 20 minutes would increase the risk of acute respiratory distress because the client requires an adjustment period to start breathing normally. 4. Answer A. As the respiratory center in the brain becomes depressed, hypoxia occurs, producing wheezing, bradycardia, and a decreased respiratory rate. Delirium is a state of mental confusion characterized by disorientation to time and place. Hyperventilation (respiratory rate greater than that metabolically necessary for gas exchange) is marked by an increased respiratory rate or tidal volume, or both. Semiconsciousness is a state of impaired consciousness characterized by limited motor and verbal responses and decreased orientation.
5. Answer D. In respiratory acidosis, ABG analysis reveals an arterial pH below 7.35 and partial pressure of arterial carbon dioxide (PaCO2) above 45 mm Hg. Therefore, the combination of a pH value of 7.25 and a PaCO2 value of 50 mm Hg confirms respiratory acidosis. A pH value of 5.0 with a PaCO2 value of 30 mm Hg indicates respiratory alkalosis. Options B and C represent normal ABG values, reflecting normal gas exchange in the lungs. 6. Answer B. Administration of a corticosteroid such as prednisone suppresses the bodys natural cortisol secretion, which may take weeks or months to normalize after drug discontinuation. Abruptly discontinuing such therapy may cause the serum cortisol level to drop low enough to trigger acute adrenocortical insufficiency. Hyperglycemia, glycosuria, GI bleeding, restlessness, and seizures are common adverse effects of corticosteroid therapy, not its sudden cessation. 7. Answer D. A patent airway and an adequate breathing pattern are the top priority for any client, making impaired gas exchange related to airflow obstruction the most important nursing diagnosis. The other options also may apply to this client but are less important. 8. Answer B. A non-rebreather mask can deliver levels of the fraction of inspired oxygen (FIO2) as high as 100%. Other modes simple mask, face tent and nasal cannula deliver lower levels of FIO2. 9. Answer B. The nurse should perform chest physiotherapy at least 2 hours after a meal to reduce the risk of vomiting and aspiration. Performing it immediately before a meal may tire the client and impair the ability to eat. Percussion and vibration, components of chest physiotherapy, may worsen bronchospasms; therefore, the procedure is contraindicated in clients with bronchospasms. Secretions that have mobilized (especially when suction equipment isnt available) are a contraindication for postural drainage, another component of chest physiotherapy. 10. Answer D. Hypotension, hypothermia, and vasoconstriction may alter pulse oximetry values by reducing arterial blood flow. Likewise, movement of the finger to which the oximeter is applied may interfere with interpretation of SaO2. All of these conditions limit the usefulness of pulse oximetry. Fever, tachypnea, and tachycardia dont affect pulse oximetry values directly. 11. Answer B. Maintaining a patent airway is the most basic and critical human need. All other interventions are important to the clients wellbeing but not as important as having sufficient oxygen to breathe. 12. Answer C. Controlled coughing helps maintain a patent airway by helping to mobilize and remove secretions. A moderate fluid intake (usually 2 L or more daily) and moderate activity help liquefy and mobilize secretions. Bed rest and sedatives may limit the clients ability to maintain a patent airway, causing a high risk of infection from pooled secretions. 13. Answer A. Tidal volume is the amount of air inspired and expired with each breath. Residual volume is the amount of air remaining in the lungs after forcibly exhaling. Vital capacity is the maximum amount of air that can be moved out of the lungs after maximal inspiration and expiration. Dead-space volume is the amount of air remaining in the upper airways that never reaches the alveoli. In pathologic conditions, dead space may also exist in the lower airways. 14. Answer C. An FO2 greater than 0.5 for as little as 16 to 24 hours can be toxic and can lead to decreased gas diffusion and surfactant activity. The ideal oxygen source is room air F IO 2 0.18 to 0.21. 15. Answer B. A positive reaction means the client has been exposed to TB; it isnt conclusive of the presence of active disease. A positive reaction consists of palpable swelling and induration of 5 to 15 mm. It can be read 48 to 72 hours after the injection. In clients with positive reactions, further studies are usually done to rule out active disease. In immunosuppressed clients, a negative reaction doesnt exclude the presence of active disease. 16. Answer A. In a client with emphysema, albuterol is used as a bronchodilator. A respiratory rate of 22 breaths/minute indicates that the drug has achieved its therapeutic effect because fewer respirations are required to achieve oxygenation. Albuterol has no effect on pupil reaction or urine output. It may cause a change in the heart rate, but this is an adverse, not therapeutic, effect. 17. Answer B. A pH less than 7.35 is indicative of acidosis; a pH above 7.45 indicates alkalosis. 18. Answer B. Before weaning a client from mechanical ventilation, its most important to have baseline ABG levels. During the weaning process, ABG levels will be checked to assess how the client is tolerating the procedure. Other assessment parameters are less critical. Measuring fluid volume intake and output is always important when a client is being mechanically ventilated. Prior attempts at weaning and ECG results are documented on the clients record, and the nurse can refer to them before the weaning process begins. 19. Answer B. The ABG results reveal respiratory alkalosis. The best intervention to raise the PaCO2 level would be to have the client breathe into a paper bag. All of the other options such as administering a decongestant, offering fluids frequently, and administering supplemental oxygen wouldnt raise the lowered PaCO2 level. 20. Answer C. The most significant and direct indicator of the effectiveness of oxygen therapy is the PaO2 value. Based on the PaO2 value, the nurse may adjust the type of oxygen delivery (cannula, venturi mask, or mechanical ventilator), flow rate, and oxygen percentage. The other options reflect the clients ventilation status, not oxygenation. 21. Answer A. Endotracheal suctioning removes secretions as well as gases from the airway and lowers the arterial oxygen saturation (SaO2) level. Coughing and incentive spirometry improves oxygenation and should raise or maintain oxygen saturation. Because of superficial vasoconstriction, using a cooling blanket can lower peripheral oxygen saturation readings, but SaO2 levels wouldnt be affected. 22. Answer A. The nurse should measure and document the amount of chest tube drainage regularly to detect abnormal drainage patterns, such as may occur with a hemorrhage (if excessive) or a blockage (if decreased). Continuous bubbling in the water-seal chamber indicates a leak in the closed chest drainage system, which must be corrected. The nurse should keep the collection chamber below chest level to allow fluids to drain into it. The nurse should not strip chest tubes because doing so may traumatize the tissue or dislodge the tube. 23. Answer B. Conditions that increase oxygen demands include obesity, smoking, exposure to temperature extremes, and stress. A client with chronic bronchitis should drink at least 2,000 ml of fluid daily to thin mucus secretions; restricting fluid intake may be harmful. The nurse should encourage the client to eat a high-protein snack at bedtime because protein digestion produces an amino acid with sedating effects that may ease the insomnia associated with chronic bronchitis. Eating more than three large meals a day may cause fullness, making breathing uncomfortable and difficult; however, it doesnt increase oxygen demands. To help maintain adequate nutritional intake, the client with chronic bronchitis should eat small, frequent meals (up to six a day). 24. Answer B. Skin color doesnt affect the mucous membranes. The lips, nail beds, and earlobes are less reliable indicators of cyanosis because theyre affected by skin color. 25. Answer D. The therapeutic serum theophylline concentration ranges from 10 to 20 mcg/ml. Values below 10 mcg/ml arent therapeutic. 26. Answer A. To avoid a hypotensive reaction from rapid I.V. administration, the nurse should infuse vancomycin slowly, over 60 to 90
minutes, in a large volume of fluid. Although neutropenia may occur in approximately 5% to 10% of clients receiving vancomycin, this adverse effect reverses rapidly when the drug is discontinued. 27. Answer C. Extreme anxiety may lead to respiratory alkalosis by causing hyperventilation, which results in excessive carbon dioxide (CO2) loss. Other conditions that may set the stage for respiratory alkalosis include fever, heart failure, and injury to the brains respiratory center, overventilation with a mechanical ventilator, pulmonary embolism, and early salicylate intoxication. Type 1 diabetes mellitus may lead to diabetic ketoacidosis; the deep, rapid respirations occurring in this disorder (Kussmauls respirations) dont cause excessive CO2 loss. Myasthenia gravis and narcotic overdose suppress the respiratory drive, causing CO2 retention, not CO2 loss; this may lead to respiratory acidosis, not alkalosis. 28. Answer D. The client is hypoxemic because of bronchoconstriction as evidenced by wheezes and a subnormal arterial oxygen saturation level. The clients greatest need is bronchodilation, which can be accomplished by administering bronchodilators. Albuterol is a beta2 adrenergic agonist, which causes dilation of the bronchioles. Its given by nebulization or metered-dose inhalation and may be given as often as every 30 to 60 minutes until relief is accomplished. Alprazolam is an anxiolytic and central nervous system depressant, which could suppress the clients breathing. Propranolol is contraindicated in a client whos wheezing because its a beta2 adrenergic antagonist. Morphine is a respiratory center depressant and is contraindicated in this situation. 29. Answer C. The client with COPD retains carbon dioxide, which inhibits stimulation of breathing by the medullary center in the brain. As a result, low oxygen levels in the blood stimulate respiration, and administering unspecified, unmonitored amounts of oxygen may depress ventilation. To promote adequate gas exchange, the nurse should use a Venturi mask to deliver a specified, controlled amount of oxygen consistently and accurately. Drinking three glasses of fluid daily wouldnt affect gas exchange or be sufficient to liquefy secretions, which are common in COPD. Clients with COPD and respiratory distress should be placed in high Fowlers position and shouldnt receive sedatives or other drugs that may further depress the respiratory center. 30. Answer A. Pursed-lip breathing helps prevent early airway collapse. Learning this technique helps the client control respiration during periods of excitement, anxiety, exercise, and respiratory distress. To increase inspiratory muscle strength and endurance, the client may need to learn inspiratory resistive breathing. To decrease accessory muscle use and thus reduce the work of breathing, the client may need to learn diaphragmatic (abdominal) breathing. In pursed-lip breathing, the client mimics a normal inspiratory-expiratory (I:E) ratio of 1:2. (A client with emphysema may have an I:E ratio as high as 1:4.) RESPI
a. 10 mcg/mL b. 12 mcg/mL c. 15 mcg/mL d. 18mcg/mL 2. Nurse Kim is caring for a client with a pneumothorax and who has had a chest tube inserted notes continuous gentle bubbling in the suction control chamber. What action is appropriate? a. Do nothing, because this is an expected finding. b. Immediately clamp the chest tube and notify the physician. c. Check for an air leak because the bubbling should be intermittent. d. Increase the suction pressure so that bubbling becomes vigorous. 3. A nurse has assisted a physician with the insertion of a chest tube. The nurse monitors the adult client and notes fluctuation of the fluid level in the water seal chamber after the tube is inserted. Based on this assessment, which action would be appropriate? a. Inform the physician. b. Continue to monitor the client. c. Reinforce the occlusive dressing. d. Encourage the client to deep-breathe. 4. The nurse caring for a male client with a chest tube turns the client to the side, and the chest tube accidentally disconnects. The initial nursing action is to: a. Call the physician. b. Place the tube in a bottle of sterile water. c. Immediately replace the chest tube system. d. Place the sterile dressing over the disconnection site. 5. a. b. c. d. Nurse Paul is assisting a physician with the removal of a chest tube. The nurse should instruct the client to: Exhale slowly. Stay very still. Inhale and exhale quickly. Perform the Valsalva maneuver.
6. While changing the tapes on a tracheostomy tube, the male client coughs and the tube is dislodged. The initial nursing action is to: a. Call the physician to reinsert the tube.
b. Grasp the retention sutures to spread the opening. c. Call the respiratory therapy department to reinsert the tracheotomy. d. Cover the tracheostomy site with a sterile dressing to prevent infection. 7. A nurse is caring for a male client immediately after removal of the endotracheal tube. The nurse reports which of the following signs immediately if experienced by the client? a. Stridor b. Occasional pink-tinged sputum c. A few basilar lung crackles on the right d. Respiratory rate of 24 breaths/min 8. An emergency room nurse is assessing a female client who has sustained a blunt injury to the chest wall. Which of these signs would indicate the presence of a pneumothorax in this client? a. A low respiratory b. Diminished breathe sounds c. The presence of a barrel chest d. A sucking sound at the site of injury 9. A nurse is caring for a male client hospitalized with acute exacerbation of chronic obstructive pulmonary disease. Which of the following would the nurse expect to note on assessment of this client? a. Hypocapnia b. A hyperinflated chest noted on the chest x-ray c. Increase oxygen saturation with exercise d. A widened diaphragm noted on the chest x-ray 10. A community health nurse is conducting an educational session with community members regarding tuberculosis. The nurse tells the group that one of the first symptoms associated with tuberculosis is: a. Dyspnea b. Chest pain c. A bloody, productive cough d. A cough with the expectoration of mucoid sputum 11. A nurse performs an admission assessment on a female client with a diagnosis of tuberculosis. The nurse reviews the results of which diagnostic test that will confirm this diagnosis? a. Bronchoscopy b. Sputum culture c. Chest x-ray d. Tuberculin skin test 12. The nursing instructor asks a nursing student to describe the route of transmission of tuberculosis. The instructor concludes that the student understands this information if the student states that the tuberculosis is transmitted by: a. Hand and mouth b. The airborne route c. The fecal-oral route d. Blood and body fluids 13. A nurse is caring for a male client with emphysema who is receiving oxygen. The nurse assesses the oxygen flow rate to ensure that it does not exceed: a. 1 L/min b. 2 L/min c. 6 L/min d. 10 L/min 14. A nurse instructs a female client to use the pursed-lip method of breathing and the client asks the nurse about the purpose of this type of breathing. The nurse responds, knowing that the primary purpose of pursed-lip breathing is to: a. Promote oxygen intake. b. Strengthen the diaphragm. c. Strengthen the intercostal muscles. d. Promote carbon dioxide elimination. 15. Nurse Hannah is preparing to obtain a sputum specimen from a client. Which of the following nursing actions will facilitate obtaining the specimen?
a. b. c. d.
Limiting fluids Having the clients take three deep breaths Asking the client to split into the collection container Asking the client to obtain the specimen after eating
16. A nurse is caring for a female client after a bronchoscope and biopsy. Which of the following signs, if noted in the client, should be reported immediately to the physicians? a. Dry cough b. Hematuria c. Bronchospasm d. Blood-streaked sputum 17. A nurse is suctioning fluids from a male client via a tracheostomy tube. When suctioning, the nurse must limit the suctioning time to a maximum of: a. 1 minute b. 5 seconds c. 10 seconds d. 30 seconds 18. A nurse is suctioning fluids from a female client through an endotracheal tube. During the suctioning procedure, the nurse notes on the monitor that the heart rate is decreasing. Which of the following is the appropriate nursing intervention? a. Continue to suction. b. Notify the physician immediately. c. Stop the procedure and reoxygenate the client. d. Ensure that the suction is limited to 15 seconds. 19. An unconscious male client is admitted to an emergency room. Arterial blood gas measurements reveal a pH of 7.30, a low bicarbonate level, a normal carbon dioxide level, a normal oxygen level, and an elevated potassium level. These results indicate the presence of: a. Metabolic acidosis b. Respiratory acidosis c. Overcompensated respiratory acidosis d. Combined respiratory and metabolic acidosis 20. A female client is suspected of having a pulmonary embolus. A nurse assesses the client, knowing that which of the following is a common clinical manifestation of pulmonary embolism? a. Dyspnea b. Bradypnea c. Bradycardia d. Decreased respiratory 21. a. b. c. d. A nurse teaches a male client about the use of a respiratory inhaler. Which action by the client indicates a need for further teaching? Inhales the mist and quickly exhales Removes the cap and shakes the inhaler well before use Presses the canister down with the finger as he breathes in Waits 1 to 2 minutes between puffs if more than one puff has been prescribed
22. A female client has just returned to a nursing unit following bronchoscopy. A nurse would implement which of the following nursing interventions for this client? a. Administering atropine intravenously b. Administering small doses of midazolam (Versed) c. Encouraging additional fluids for the next 24 hours d. Ensuring the return of the gag reflex before offering food or fluids 23. A nurse is assessing the respiratory status of a male client who has suffered a fractured rib. The nurse would expect to note which of the following? a. Slow deep respirations b. Rapid deep respirations c. Paradoxical respirations d. Pain, especially with inspiration 24. A female client with chest injury has suffered flail chest. A nurse assesses the client for which most distinctive sign of flail chest? a. Cyanosis
b. Hypotension c. Paradoxical chest movement d. Dyspnea, especially on exhalation 25. A male client has been admitted with chest trauma after a motor vehicle accident and has undergone subsequent intubation. A nurse checks the client when the high-pressure alarm on the ventilator sounds, and notes that the client has absence of breathe sounds in right upper lobe of the lung. The nurse immediately assesses for other signs of: a. Right pneumothorax b. Pulmonary embolism c. Displaced endotracheal tube d. Acute respiratory distress syndrome 26. A nurse is teaching a male client with chronic respiratory failure how to use a metered-dose inhaler correctly. The nurse instructs the client to: a. Inhale quickly b. Inhale through the nose c. Hold the breath after inhalation d. Take two inhalations during one breath 27. A nurse is assessing a female client with multiple trauma who is at risk for developing acute respiratory distress syndrome. The nurse assesses for which earliest sign of acute respiratory distress syndrome? a. Bilateral wheezing b. Inspiratory crackles c. Intercostal retractions d. Increased respiratory rate 28. A nurse is taking pulmonary artery catheter measurements of a male client with acute respiratory distress syndrome. The pulmonary capillary wedge pressure reading is 12mm Hg. The nurse interprets that this readings is: a. High and expected b. Low and unexpected c. Normal and expected d. Uncertain and unexpected 29. A nurse is assessing a male client with chronic airflow limitations and notes that the client has a barrel chest. The nurse interprets that this client has which of the following forms of chronic airflow limitations? a. Emphysema b. Bronchial asthma c. Chronic obstructive bronchitis d. Bronchial asthma and bronchitis 30. A nurse is caring for a female client diagnosed with tuberculosis. Which assessment, if made by the nurse, is inconsistent with the usual clinical presentation of tuberculosis and may indicate the development of a concurrent problem? a. Cough b. High-grade fever c. Chills and night sweats d. Anorexia and weight loss ANSWER AND RATIONALE 1. Answer A. The therapeutic range for the serum theophylline level is 10 to 20 mcg/mL. If the level is below the therapeutic range, the client may experience frequent exacerbations of the disorder. Although all the options identify values within the therapeutic range, option A is the option that reflects a need for compliance with medication. 2. Answer A. Continuous gentle bubbling should be noted in the suction control chamber. Option B is incorrect. Chest tubes should only be clamped to check for an air leak or when changing drainage devices (according to agency policy). Option C is incorrect. Bubbling should be continuous and not intermittent. Option D is incorrect because bubbling should be gentle. Increasing the suction pressure only increases the rate of evaporation of water in the drainage system. 3. Answer B. The presence of fluctuation of the fluid level in the water seal chamber indicates a patent drainage system. With normal breathing, the water level rises with inspiration and falls with expiration. Fluctuation stops if the tube is obstructed, if a dependent loop exists, if the suction is not working properly, or if the lung has reexpanded. Options A, C, and D are incorrect. 4. Answer B. If the chest drainage system is disconnected, the end of the tube is placed in a bottle of sterile water held below the level of the chest. The system is replaced if it breaks or cracks or if the collection chamber is full. Placing a sterile dressing over the disconnection site will not prevent complications resulting from the disconnection. The physician may need to be notified, but this is not the initial action.
5. Answer D. When the chest tube is removed, the client is asked to perform the Valsalva maneuver (take a deep breath, exhale, and bear down). The tube is quickly withdrawn, and an airtight dressing is taped in place. An alternative instruction is to ask the client to take a deep breath and hold the breath while the tube is removed. Options A, B, and C are incorrect client instructions. 6. Answer B. If the tube is dislodged accidentally, the initial nursing action is to grasp the retention sutures and spread the opening. If agency policy permits, the nurse then attempts immediately to replace the tube. Covering the tracheostomy site will block the airway. Options 1 and 3 will delay treatment in this emergency situation. 7. Answer A. The nurse reports stridor to the physician immediately. This is a high-pitched, coarse sound that is heard with the stethoscope over the trachea. Stridor indicates airway edema and places the client at risk for airway obstruction. Options B, C, and D are not signs that require immediate notification of the physician. 8. Answer B. This client has sustained a blunt or a closed chest injury. Basic symptoms of a closed pneumothorax are shortness of breath and chest pain. A larger pneumothorax may cause tachypnea, cyanosis, diminished breath sounds, and subcutaneous emphysema. Hyperresonance also may occur on the affected side. A sucking sound at the site of injury would be noted with an open chest injury. 9. Answer B. Clinical manifestations of chronic obstructive pulmonary disease (COPD) include hypoxemia, hypercapnia, dyspnea on exertion and at rest, oxygen desaturation with exercise, and the use of accessory muscles of respiration. Chest x-rays reveal a hyperinflated chest and a flattened diaphragm if the disease is advanced. 10. Answer D. One of the first pulmonary symptoms is a slight cough with the expectoration of mucoid sputum. Options A, B, and C are late symptoms and signify cavitation and extensive lung involvement. 11. Answer B. Tuberculosis is definitively diagnosed through culture and isolation of Mycobacterium tuberculosis. A presumptive diagnosis is made based on a tuberculin skin test, a sputum smear that is positive for acid-fast bacteria, a chest x-ray, and histological evidence of granulomatous disease on biopsy. 12. Answer B. Tuberculosis is an infectious disease caused by the bacillus Mycobacterium tuberculosis and is spread primarily by the airborne route. Options A, C, and D are incorrect. 13. Answer B. Oxygen is used cautiously and should not exceed 2 L/min. Because of the long-standing hypercapnia that occurs in emphysema, the respiratory drive is triggered by low oxygen levels rather than increased carbon dioxide levels, as is the case in a normal respiratory system. 14. Answer D. Pursed-lip breathing facilitates maximal expiration for clients with obstructive lung disease. This type of breathing allows better expiration by increasing airway pressure that keeps air passages open during exhalation. Options A, B, and C are not the purposes of this type of breathing. 15. Answer B. To obtain a sputum specimen, the client should rinse the mouth to reduce contamination, breathe deeply, and then cough into a sputum specimen container. The client should be encouraged to cough and not spit so as to obtain sputum. Sputum can be thinned by fluids or by a respiratory treatment such as inhalation of nebulized saline or water. The optimal time to obtain a specimen is on arising in the morning. 16. Answer C. If a biopsy was performed during a bronchoscopy, blood-streaked sputum is expected for several hours. Frank blood indicates hemorrhage. A dry cough may be expected. The client should be assessed for signs of complications, which would include cyanosis, dyspnea, stridor, bronchospasm, hemoptysis, hypotension, tachycardia, and dysrhythmias. Hematuria is unrelated to this procedure. 17. Answer C. Hypoxemia can be caused by prolonged suctioning, which stimulates the pacemaker cells in the heart. A vasovagal response may occur, causing bradycardia. The nurse must preoxygenate the client before suctioning and limit the suctioning pass to 10 seconds. 18. Answer C. During suctioning, the nurse should monitor the client closely for side effects, including hypoxemia, cardiac irregularities such as a decrease in heart rate resulting from vagal stimulation, mucosal trauma, hypotension, and paroxysmal coughing. If side effects develop, especially cardiac irregularities, the procedure is stopped and the client is reoxygenated. 19. Answer A. In an acidotic condition, the pH would be low, indicating the acidosis. In addition, a low bicarbonate level along with the low pH would indicate a metabolic state. Therefore, options B, C, and D are incorrect. 20. Answer A. The common clinical manifestations of pulmonary embolism are tachypnea, tachycardia, dyspnea, and chest pain. 21. Answer A. The client should be instructed to hold his or her breath for at least 10 to 15 seconds before exhaling the mist. Options B, C, and D are accurate instructions regarding the use of the inhaler. 22. Answer D. After bronchoscopy, the nurse keeps the client on NPO status until the gag reflex returns because the preoperative sedation and local anesthesia impair swallowing and the protective laryngeal reflexes for a number of hours. Additional fluids are unnecessary because no contrast dye is used that would need flushing from the system. Atropine and midazolam would be administered before the procedure, not after. 23. Answer D. Rib fractures are a common injury, especially in the older client, and result from a blunt injury or a fall. Typical signs and symptoms include pain and tenderness localized at the fracture site and exacerbated by inspiration and palpation, shallow respirations, splinting or guarding the chest protectively to minimize chest movement, and possible bruising at the fracture site. Paradoxical respirations are seen with flail chest. 24. Answer C. Flail chest results from fracture of two or more ribs in at least two places each. This results in a floating section of ribs. Because this section is unattached to the rest of the bony rib cage, this segment results in paradoxical chest movement. This means that the force of inspiration pulls the fractured segment inward, while the rest of the chest expands. Similarly, during exhalation, the segment balloons outward while the rest of the chest moves inward. This is a telltale sign of flail chest. 25. Answer A. Pneumothorax is characterized by restlessness, tachycardia, dyspnea, pain with respiration, asymmetrical chest expansion, and diminished or absent breath sounds on the affected side. Pneumothorax can cause increased airway pressure because of resistance to lung inflation. Acute respiratory distress syndrome and pulmonary embolism are not characterized by absent breath sounds. An endotracheal tube that is inserted too far can cause absent breath sounds, but the lack of breath sounds most likely would be on the left side because of the degree of curvature of the right and left main stem bronchi. 26. Answer C. Instructions for using a metered-dose inhaler include shaking the canister, holding it right side up, inhaling slowly and evenly through the mouth, delivering one spray per breath, and holding the breath after inhalation. 27. Answer D. The earliest detectable sign of acute respiratory distress syndrome is an increased respiratory rate, which can begin from 1 to 96 hours after the initial insult to the body. This is followed by increasing dyspnea, air hunger, retraction of accessory muscles, and cyanosis. Breath sounds may be clear or consist of fine inspiratory crackles or diffuse coarse crackles.
28. Answer C. The normal pulmonary capillary wedge pressure (PCWP) is 8 to 13 mm Hg, and the client is considered to have high readings if they exceed 18 to 20 mm Hg. The client with acute respiratory distress syndrome has a normal PCWP, which is an expected finding because the edema is in the interstitium of the lung and is noncardiac. 29. Answer A. The client with emphysema has hyperinflation of the alveoli and flattening of the diaphragm. These lead to increased anteroposterior diameter, referred to as barrel chest. The client also has dyspnea with prolonged expiration and has hyperresonant lungs to percussion. 30. Answer B. The client with tuberculosis usually experiences cough (productive or nonproductive), fatigue, anorexia, weight loss, dyspnea, hemoptysis, chest discomfort or pain, chills and sweats (which may occur at night), and a low-grade fever. RESPI DISORDERS 1. a. b. c. d. 2. a. b. c. d. A Mantoux test signifies exposure to Mycobacterium Tubercle Bacilli. The test is read for how many hours after injection? 1 hour 12-24 hours 48-72 hours 2 hours A nurse is about to perform a Mantoux test. The test is done by using which route? Intradermal Intramuscular Subcutaneous IM with the use of Z-track method
3. A client is suspected to have an HIV. The nurse knows that in the Mantoux test result, a client is considered positive with HV if he has an induration of: a. More than 10 mm b. 3mm c. 4 mm d. 5 mm 4. a. b. c. d. 5. a. b. c. d. 6. a. b. c. d. 7. a. b. c. d. 8. a. b. c. d. A client is about to undergo a chest x-ray. Which of the following should the nurse do first before the procedure? Secure a written consent Instruct the client not to eat anything at the night before the procedure Instruct the client to remove metals from the chest Administer atropine sulfate and valium before the procedure Mr. Lorenzo is schedule for a bronchography. Before the procedure the nurse least likely performs which of the following? Assist the client in a side-lying position Checking for allergies Instructing the client to be on NPO for 6-8 hours Administer atropine sulfate After thoracentesis the client should be placed on which position? Affected side Unaffected side Prone position Supine position The most important action the nurse should do before and after suctioning a client is: Placing the client in a supine position Making sure that suctioning takes only 10-15 seconds Evaluating for clear breath sounds Hyperventilating the client with 100% oxygen The position of a conscious client during suctioning is: Fowlers Supine position Side-lying Prone
9. A client is on chest tube. A three-way bottle system is used. The nurse expects that the suction bottle will normally have which of the following characteristics.
a. b. c. d.
Intermittent bubbling Continuous bubbling No bubbling None of the above
10. Before the nurses shift ended, the water seal bottle is observed to have an intermittent suctioning. The nurse should do which of the following? a. Check for an air leak b. Check for kinks in the tube c. Inform the physician immediately d. Make sure that the bottle is at least 2-3 feet below the level of the chest 11. a. b. c. d. 12. a. b. c. d. The physician is going to remove the chest tube from a client. The nurse should least likely prepare which of the following item? Sterile gauze Suture removal kit Empty bottles Adhesive tape While the chest tube is removed the nurse should instruct the patient to: Exhale deeply Inhale deeply Lie at the abdomen Hyperextend the neck
13. A client is brought to the ER with complaints of stuffy nose, headache, persistent cough, fever and post-nasal drip. Pain is complained by the client above the eyebrows. The diagnosis is sinusitis. Which of the following sinuses is affected? a. Maxillary b. Frontal c. Ethmoid d. Sphenoid 14. a. b. c. d. 15. a. b. c. d. Which of the following medications is avoided in sinusitis to prevent the risk of developing nasal polyps? Codeine Amoxicillin ASA Anti-infectives Which intervention is least likely done for sinutis? Increase fluid intake Cold wet packs Hot wet packs Rest
16. A client with sinusitis had undergone Caldwell-Luc Surgery. The nurse should instruct the client to do which of the following after the procedure? a. Chew on the unaffected side only. b. The client can wear dentures 5 days after. c. Sneezing should be avoided for a week after the surgery d. All of the above 17. A teen ager is diagnosed to have inflamed tonsils (tonsillitis). The patients history reveals recurrent tonsillitis episodes for about 6 times of the same year. The most appropriate intervention for the patient is: a. Promoting rest b. Increasing fluid intake c. Warm saline gargle d. Surgery 18. a. b. c. d. Before a tonsillectomy is performed, which of the following data is very crucial for the nurse to assess? Degree of pain URTI Drainage on the ears Respiration pattern
19. a. b. c. d. 20. a. b. c. d.
Mark underwent a tonsillectomy procedure. To promote comfort the following interventions should be done by the nurse except: Application of ice collar Assist the client to a semi-fowlers position with pillow support Assess for frequent swallowing of the patient Administration of acetaminophen Two days after tonsillectomy, Marks reported that his stool is black. Initially, the nurse should: Inform the physician Document the findings Obtain stool for analysis Check the clients vital signs
21. Asthma can be caused by extrinsic and intrinsic factors. Presence of these factors triggers the release of the chemical mediators which does not include: a. Serotonin b. Prostaglandin c. Bradykinin d. Adrenaline 22. a. b. c. d. 23. a. b. c. d. 24. a. b. c. d. 25. a. b. c. d. Presence of overdistended and non-functional alveoli is a condition called: Bronchitis Emphysema Empyema Atelectasis The accumulation of fluids in the pleural space is called: Pleural effusion Hemothorax Hydrothorax Pyothorax A client with COPD is instructed to follow what diet? High carbohydrate, low calorie and high protein diet High protein, high calorie and low carbohydrate diet High carbohydrate, low protein and high calorie diet High protein, high carbohydrate and high caloric diet Bronchodilators include the following apart from: Theophyline Terbutaline Metaproterenol Dipenhydramine
ANSWER AND RATIONALE 1. Answer: C. Mantoux test is read 48-72 hours after injection. 2. Answer: A. Mantoux tests are done intradermally. 3. Answer: D. Mantoux test is considered positive for Mycobacterium Tubercle Bacilli if the induration is 10 mm or more. For HIV positive clients, induration of 5mm is considered positive. 4. Answer: C. The client is instructed to remove metals from the chest. Consent, NPO post midnight and atropine sulfate administration are not needed for this procedure. 5. Answer: A. Nursing interventions before bronchogram: Secure written consent Check for allergies (seafoods and iodine or anesthesia) NPO 6-8 hours Pre-op meds: atropine sulfate and valium, topical anesthesia sprayed followed by local anesthetic into the larynx Have oxygen and antispasmodic agents ready Nursing Interventions after bronchogram Side-lying position
NPO until cough and gag reflex returns Cough and deep breathe clients Low grade fever common 6. Answer: D. After thoracentesis the client is placed or turned to the unaffected side to prevent leakage of fluid in the thoracic cavity. 7. Answer: D. The client should be hyperventilated with 100% oxygen before and after suctioning. 8. Answer: A. Position a conscious person who has a functional gag reflex in the semi fowlers position with the head turned to one side for oral suctioning or with the neck hyper extended for nasal suctioning. If the client is unconscious place the patient a lateral position facing you. 9. Answer: A. Suction bottle will have continuous suctioning while the water seal bottle will have an intermittent suctioning. 10. Answer: D. A water seal bottle is expected to be observed for intermittent bubbling. Therefore, the nurse should only make sure that bottle is at least 2-3 feet below the chest. Checking for an air leak would be the nurses action if the water seal has continuous bubbling. Kinks should be check for possible obstruction if no bubbling is noted in the water seal bottle. 11. Answer: C. In removal of the chest tube the nurse should prepare the following: Petrolatum gauze Suture removal kit Sterile gauze Adhesive tape 12. Answer: A. As the chest tube is removed the client should be instructed to exhale deeply and do valsalva maneuver. The client is placed in a semi-fowlers position before the chest tube is removed. 13. Answer: B. Because the pain is felt above the eyebrows the affected sinus is the frontal sinus. Pain assessment in sinusitis Maxillary: cheek and upper teeth Frontal: above eyebrows Ethmoid: in and around the eyes Sphenoid: behind eye, occiput, top of the head 14. Answer: C. ASA is avoided in sinusitis as it increases the risk of developing nasal polyps. 15. Answer: B. Management for sinusitis: Rest Increase fluids Hot wet packs Codeine Amoxicillin and other anti-infectives Nasal decongestants Irrigation of maxillary sinuses with warm NSS 16. Answer: A. After a Caldwell-Luc Operation (Radical Antrum Surgery) the following should be instructed to the client: Do not chew on the affected side Caution with oral hygiene to prevent trauma of incision Do not wear dentures for 10 days Do not blow nose for 2 weeks after the removal of the packing Avoid sneezing for two weeks after surgery 17. Answer: D. Surgery is indicated for patients with tonsillitis recurring 5-6 times a year. 18. Answer: B. The should assess for Upper respiratory tract infection (URTI). Coughing and sneezing postoperatively due to URTI may cause bleeding. 19. Answer: C. to promote comfort the nurse must administer acetaminophen to alleviate pain from the operation. Also, ice collar can be applied to decrease pain thus, promoting comforting. Assisting the client to the proper position after tonsillectomy (semi-fowlers) while supporting the position with pillows is also one way to promote comfort. The only choice that does not promote comfort but monitors for hemorrhage is the assessment for frequent swallowing, thus, it is the correct answer (C). 20. Answer: B. after tonsillectomy, the clients stool will be black or dark for a few days due to the swallowed blood. 21. Answer: D. Allergy (extrinsic) and inflammation (intrinsic) triggers the release of chemical mediators that causes narrowing of the airways and spasm. These mediators are: Serotonin Prostaglandin Bradykinin Histamine Leukotrienes 22. Answer: B. An overdistended and non-functional alveoli is a condition called emphysema. Atelectasis is the collapse of a part or the whole lung. Empyema is the presence of pus in the lung. 23. Answer: A. The strategy used in this item is the umbrella effect. Hemothorax (blood), hydrothorax (water) and pyothirax (pus; also called empyema) are all types of pleural effusion. The three choices are under pleural effusion (umbrella effect), thus the correct answer is A. 24. Answer: B. Diet for COPD: High calorie, high protein and low carbohydrate diet High caloric diet provides source of energy. High protein diet helps maintain integrity of alveolar walls. Low carbohydrate diet limits carbon dioxide production (natural end product). The client with COPD has difficulty exhaling carbon dioxide. 25. Answer: D. Benadryl (Dipenhydramine) is an antihistamine not bronchodilator.
BASIC CARE AND COMFORT 1. Nurse Jessie is caring for an elderly woman who has had a fractured hip repaired. In the first few days following the surgical repair, which of the following nursing measures will best facilitate the resumption of activities for this client? a. arranging for the wheelchair b. asking her family to visit c. assisting her to sit out of bed in a chair qid d. encouraging the use of an overhead trapeze 2. a. b. c. d. 3. a. b. c. d. What do you think is the most important nursing order in a client with major head trauma who is about to receive bolus enteral feeding? measure intake and output. check albumin level. monitor glucose levels. increase enteral feeding. What is the pathological process causing esophageal varices is ascites and edema. systemic hypertension. portal hypertension. dilated veins and varicesitis.
4. Which of the following interventions will help lessen the effect of GERD (acid reflux)? a. Elevate the head of the bed on 4-6 inch blocks. b. Lie down after eating. c. Increase fluid intake just before bedtime. d. Wear a girdle. 5. a. b. c. d. What is the main benefit of therapeutic massages is: to help a person with swollen legs to decrease the fluid retention. to help a person with duodenal ulcers feel better. to help damaged tissue in a diabetic to heal. to improve circulation and muscles tone.
6. Which of the following foods should be avoided by clients who are prone to develop heartburn as a result of gastroesophgeal reflux disease (GERD)? a. Lettuce b. Eggs c. Chocolate d. Butterscotch 7. a. b. c. d. 8. a. b. c. d. 9. a. b. c. d. Which of the following should be included in a plan of care for a client receiving total parenteral nutrition (TPN)? Withhold medications while the TPN is infusing. Change TPN solution every 24 hours. Flush the TPN line with water prior to initiating nutritional support. Keep client on complete bed rest during TPN therapy. Which of the following should be included in a plan of care for a client who is lactose intolerant? Remove all dairy products from the diet. Frozen yogurt can be included in the diet. Drink small amounts of milk on an empty stomach. Spread out selection of dairy products throughout the day. Pain tolerance in an elderly patient with cancer would: stay the same. be lowered. be increased. no effect on pain tolerance.
10. What is the main advantage of cutaneous stimulation in managing paint: a. costs less. b. restricts movement and decreases.
c. gives client control over pain syndrome. d. allows the family to care for the patient at home. 11. The nurse is instructing a 65 year-old female client diagnosed with osteoporosis. The most important instruction regarding exercise would be to a. exercise doing weight bearing activities b. exercise to reduce weight c. avoid exercise activities that increase the risk of fracture d. exercise to strengthen muscles and thereby protect bones 12. A client in a long term care facility complains of pain. The nurse collects data about the clients pain. The first step in pain assessment is for the nurse to a. have the client identify coping methods b. get the description of the location and intensity of the pain c. accept the clients report of pain d. determine the clients status of pain 13. a. b. c. d. Which statement best describes the effects of immobility in children? Immobility prevents the progression of language and fine motor development Immobility in children has similar physical effects to those found in adults Children are more susceptible to the effects of immobility than are adults Children are likely to have prolonged immobility with subsequent complications
14. After a myocardial infarction, a client is placed on a sodium restricted diet. When the nurse is teaching the client about the diet, which meal plan would be the most appropriate to suggest? a. 3 oz. broiled fish, 1 baked potato, cup canned beets, 1 orange, and milk b. 3 oz. canned salmon, fresh broccoli, 1 biscuit, tea, and 1 apple c. A bologna sandwich, fresh eggplant, 2 oz fresh fruit, tea, and apple juice d. 3 oz. turkey, 1 fresh sweet potato, 1/2 cup fresh green beans, milk, and 1 orange 15. a. b. c. d. A nurse is assessing several clients in a long term health care facility. Which client is at highest risk for development of decubitus ulcers? A 79 year-old malnourished client on bed rest An obese client who uses a wheelchair An incontinent client who has had 3 diarrhea stools An 80 year-old ambulatory diabetic client
16. Ms. Kelly. has had a CVA (cerebrovascular accident) and has severe right-sided weakness. She has been taught to walk with a cane. The nurse is evaluating her use of the cane prior to discharge. Which of the following reflects correct use of the cane? a. Holding the cane in her left hand, Ms. Kelly. moves the cane forward first, then her right leg, and finally her left leg b. Holding the cane in her right hand, Ms. Kelly. moves the cane forward first, then her left leg, and finally her right leg c. Holding the cane in her right hand, Ms. Kelly. moves the cane and her right leg forward, then moves her left leg forward. d. Holding the cane in her left hand, Ms. Kelly. moves the cane and her left leg forward, then moves her right leg forward 17. The nurse is instructing a woman in a low-fat, high-fiber diet. Which of the following food choices, if selected by the client, indicate an understanding of a low-fat, high-fiber diet? a. Tuna salad sandwich on whole wheat bread. b. Vegetable soup made with vegetable stock, carrots, celery, and legumes served with toasted oat bread c. Chefs salad with hard boiled eggs and fat-free dressing d. Broiled chicken stuffed with chopped apples and walnuts 18. An 85-year-old male patient has been bedridden for two weeks. Which of the following complaints by the patient indicates to the nurse that he is developing a complication of immobility? a. Stiffness of the right ankle joint b. Soreness of the gums c. Short-term memory loss. d. Decreased appetite. 19. An eleven-month-old infant is brought to the pediatric clinic. The nurse suspects that the child has iron deficiency anemia. Because iron deficiency anemia is suspected, which of the following is the most important information to obtain from the infants parents? a. Normal dietary intake. b. Relevant sociocultural, economic, and educational background of the family.
c. Any evidence of blood in the stools d. A history of maternal anemia during pregnancy 20. A 46-year-old female with chronic constipation is assessed by the nurse for a bowel training regimen. Which factor indicates further information is needed by the nurse? a. The clients dietary habits include foods high in bulk. b. The clients fluid intake is between 2500-3000 ml per day c. The client engages in moderate exercise each day d. The clients bowel habits were not discussed. ANSWER AND RATIONALE 1. Answer D. Exercise is important to keep the joints and muscles functioning and to prevent secondary complications. Using the overhead trapeze prevents hazards of immobility by permitting movement in bed and strengthening of the upper extremities in preparation for ambulation. Sitting in a wheelchair would require too great hip flexion initially. Asking her family to visit would not facilitate the resumption of activities. Sitting in a chair would cause too much hip flexion. The client initially needs to be in a low Fowlers position or taking a few steps (as ordered) with the aid of a walker. 2. Answer A. It is important to measure intake and output, which should equal. Enteral feeding are hyperosmotic agents pulling fluid from cells into vascular bed. Water given before feeding will present a hyperosmotic diuresis. I and O measures assess fluid balance. 3. Answer C. Esophageal varices results from increased portal hypertension. In portal hypertension, the liver cannot accept all of the fluid from the portal vein. The excess fluid will back flow to the vessels with lesser pressure, such as esophageal veins or rectal veins causing esophageal varices or hemorrhoids. 4. Answer A. Elevation of the head of the bed allows gravity to assist in decreasing the backflow of acid into the esophagus. Fluid does not flow uphill. The other three options all increase fluid backflow into the esophagus through position or increasing abdominal pressure. 5. Answer D. Particularly in the elderly adults, therapeutic massage will help improve circulation and muscle tone as well as the personal attention and social interaction that a good massage provides. A massage is contraindicated in any condition where massage to damaged tissue can dislodge a blood clot. 6. Answer C. Ingestion of chocolate can reduce lower esophageal sphincter (LES) pressure leading to reflux and clinical symptoms of GERD. All of the other foods do not affect LES pressure. 7. Answer B. TPN solutions should be changed every 24 hours in order to prevent bacterial overgrowth due to hypertonicity of the solution. Option 1 is incorrect; medication therapy can continue during TPN therapy. Option 3 is incorrect; flushing is not required because the initiation of TPN does not require a client to remain on bed rest during therapy. However, other clinical conditions of the client may affect mobility issues and warrant the clients being on bed rest. 8. Answer B. Clients who are lactose intolerant can digest frozen yogurt. Yogurt products are formed by bacterial action, and this action assists in the digestion of lactose. The freezing process further stops bacterial action so that limited lactase activity remains. Option 1 is incorrect; elimination of all dairy products can lead to significant clinical deficiencies of other nutrients. Option 3 is incorrect because drinking milk on an empty stomach can exacerbate clinical symptoms. Drinking milk with a meal may benefit the client because other foods, (especially fat) may decrease transit time and allow for increased lactase activity. Option 4 is incorrect because although individual tolerance should be acknowledged, spreading out the use of known dairy products will usually exacerbate clinical symptoms. 9. Answer B. There is potential for a lowered pain tolerance to exist with diminished adaptative capacity. 10. Answer C. Cutaneous stimulation allows the patient to have control over his pain and allows him to be in his own environment. Cutaneous stimulation increases movement and decreases pain. 11. Answer A. Weight bearing exercises are beneficial in the treatment of osteoporosis. Although loss of bone cannot be substantially reversed, further loss can be greatly reduced if the client includes weight bearing exercises along with estrogen replacement and calcium supplements in their treatment protocol. 12. Answer C. Although all of the options above are correct, the first and most important piece of information in this clients pain assessment is what the client is telling you about the pain the clients report. 13. Answer B. Care of the immobile child includes efforts to prevent complications of muscle atrophy, contractures, skin breakdown, decreased metabolism and bone demineralization. Secondary alterations also occur in the cardiovascular, respiratory and renal systems. Similar effects and alterations occur in adults. 14. Answer D. Canned fish and vegetables and cured meats are high in sodium. This meal does not contain any canned fish and/or vegetables or cured meats 15. Answer A. Weighing significantly less than ideal body weight increases the number and surface area of bony prominences which are susceptible to pressure ulcers. Thus, malnutrition is a major risk factor for decubiti, due in part to poor hydration and inadequate protein intake. 16. Answer A. When a person with weakness on one side uses a cane, there should always be two points of contact with the floor. When Ms. Kelly. moves the cane forward, she has both feet on the floor, providing stability. As she moves the weak leg, the cane and the strong leg provide support. Finally, the cane, which is even with the weak leg, provides stability while she moves the strong leg. She should not hold the cane with her weak arm. The use of the cane requires arm strength to ensure that the cane provides adequate stability when standing on the weak leg. The cane should be held in the left hand, the hand opposite the affected leg. If Ms. Kelly. moved the cane and her strong foot at the same time, she would be left standing on her weak leg at one point. This would be unstable at best; at worse, impossible 17. Answer B. Mayonnaise in tuna salad is high in fat. The whole wheat bread has some fiber. This choice shows a low-fat soup (which would have been higher in fat if made with chicken or beef stock) and high-fiber bread and soup contents (both the vegetables and the legumes). Salad is high in fiber, but hard boiled eggs are high in fat. There is some fiber in the apples and walnuts. The walnuts are high in fat, as is the chicken.
18. Answer A. Stiffness of a joint may indicate the beginning of a contracture and/or early muscle atrophy. Soreness of the gums is not related to immobility. Short-term memory loss is not related to immobility. Decreased appetite is unlikely to be related to immobility. 19. Answer A. Iron deficiency anemia occurs commonly in children 6 to 24 months of age. For the first 4 to 5 months of infancy iron stores laid down for the baby during pregnancy are adequate. When fetal iron stores are depleted, supplemental dietary iron needs to be supplied to meet the infants rapid growth needs. Iron deficiency may occur in the infant who drinks mostly milk, which contains no iron, and does not receive adequate dietary iron or supplemental iron. Daily dietary intake is much more related to the diagnosis of iron deficiency anemia than is sociocultural, economic, and educational background of the family. Iron deficiency anemia in an infant is very unlikely to be related to gastrointestinal bleeding. Anemia during pregnancy is unlikely to be the cause of the infants iron deficiency anemia. Fetal iron stores are drawn from the mother even if she is anemic. 20. Answer D. Foods high in bulk are appropriate. Exercise should be a part of a bowel training regimen. To assess the client for a bowel training program the factors causing the bowel alteration should be assessed. A routine for bowel elimination should be based on the clients previous bowel habits and alterations in bowel habits that have occurred because of illness or trauma. The client and the family should assist in the planning of the program which should include foods high in bulk, adequate exercise, and fluid intake of 2500-3000 ml. NURSING TEST QUESTION 1. Which of the following disorders is characterized by joint inflammation that is usually accompanied by pain and frequently accompanied by changes in structure? a. Synovitis b. Arthritis c. Bursitis d. Tendinitis 2. Which term refers to the expectoration of blood from the respiratory tract? a. A hemorrhage b. Hematopoiesis c. Hemoptysis d. Hemopexis 3. Which term describes lack of coordination in performing planned, purposeful movements, resulting from a neurologic deficit? a. Apraxia b. Ataxia c. Fasciculation d. Myokymia 4. An elevation in the partial pressure of carbon dioxide in arterial blood (PaCO2) indicates that the patient has: a. Hypernatremia b. Hypocalcemia c. Hypoxemia d. Hypercapnia
5. The latest laboratory values indicate that the patient has thrombocytopenia. The combining form penia means: a. Rupture b. Deficiency c. Formation d. Stupor 6. A patient is admitted to the hospital with a urine specific gravity of 1.030, a temperature of 102F (38.9 C), and flushed, dry skin. Based on these data, the nurse writes which of the following nursing diagnoses? a. Potential for impaired skin integrity b. Fluid volume deficit related to fever c. Potential for fluid volume deficit caused by fever d. Altered cardiopulmonary tissue perfusion related to fluid excess 7. The guidelines for writing an appropriate nursing diagnosis include all of the following except: a. State the diagnosis in terms of a problem, not a need b. Use nursing terminology to describe the patients response c. Use statements that assist in planning independent nursing interventions d. Use medical terminology to describe the probable cause of the patients response 8. Based on a physicians order for oxygen by nasal catheter at 3 liters/ minute, an appropriate nursing order would be: a. Cover the tip of the catheter with a water-soluble lubricant before insertion. b. Measure the length of the catheter from the tip of the patients nose to the tip of the earlobe before insertion c. Add sterile distilled water to the humidification container, as needed d. All of the above 9. A nurse observes a dazed and apparently confused co-worker taking two diazepam (Valium) tablets by mouth as the co-worker is about to pour medications. What should the nurse do? a. Call the head nurse immediately before the co-worker pours and administers the medications b. Pour the medications for the co-worker while she goes for a cup of coffee c. Report the co-worker to hospital security because she may be addicted to drugs d. Watch the co-worker closely and report the incident to the head nurse at the end of the day. 10. A nurse manager notices that one of the staff nurses is always 15 to 20 minutes late. When the nurse manager discusses the problem with her, the nurse says that she has been late because her sons nursery school does not open until 7 am. The nurse manager should respond by telling her to:
a. Ask one of the night nurses to cover for her b. See if a neighbor can take the child to school c. Find out if other schools open earlier d. Find some way to solve the problem and be on time 11. A nurse has just moved to a new state, where she has accepted employment in a hospital-based hemodialysis unit. She needs information about her specific duties in caring for hemodialysis patients. She will find this information in: a. Policy statements set by the National Kidney Foundation b. The states nurse practice act c. Medicare and Medicaid regulations d. The hospitals procedure manual 12. Which of the following is an example of nursing malpractice? a. The nurse administers penicillin to a patient with a documented history of allergy to the drug. The patient experiences an allergic reaction and has cerebral damage resulting from anoxia. b. The nurse applies a hot water bottle or a heating pad to the abdomen of a patient with abdominal cramping c. The nurse assists a patient out of bed with the bed locked in position; the patient slips and fractures his right humerus d. The nurse administers the wrong medication to a patient and the patient vomits. This information is documented and reported to the physician and the nursing supervisor 13. Therapeutic communication is a significant aspect of patient care. Which of the following statements most clearly defines this concept? a. Therapeutic communication conveys feelings of warmth, acceptance, and empathy from the nurse to the patient in a nonjudgmental atmosphere b. Therapeutic communication is a reciprocal interaction based on trust and aimed at identifying patient needs and developing mutual goals c. Therapeutic communication is the assessment component of the nursing process, in which the nurse gathers health history information from the patients perspective d. Therapeutic communication is an interactional process in which the nurse purposefully reviews and assesses the conversation and its potential outcomes 14. Many factors can become barriers to communication. In which of the following situations would communication least likely be hindered? a. Mr. S., a 30-year-old Vietnamese immigrant, is admitted to the hospital with a fractured tibia; he speaks limited English b. Ms. M., age 58 and unmarried, is admitted to the hospital for breast surgery c. Mrs. R, age 26, is admitted to the hospital for a scheduled cesarean section; this is her first admission d. Mr. G., age 78, arrives at the hospital by ambulance after suffering a stroke at home
15. The assessment component of the nursing process requires effective communication to elicit a complete, relevant history from the patient and to identify patient problems. What role does communication play in the other areas of the nursing process? a. In the planning phase, effective therapeutic communication helps to establish nursing care priorities and patient-oriented goals b. During the implementation phase, communication skills allow the nurse to assess the patients response to planned interventions c. During the evaluation phase, effective communication allows the nurse to find out from the patient if he is responding to treatment or if changes in treatment are necessary d. All of the above 16. All of the following would be considered objective assessment data for a patient admitted with diabetes mellitus except: a. + 2 urine glucose level; negative urine acetone level b. Chemstrip reading of 240 mg/dl c. Patient complaints of polydipsia d. Serum glucose level of 263 mg/dl 17. Which of the following statements about bowel sounds is accurate? a. Peristalsis causes bowel sounds b. Rapid, high-pitched, hyperactive bowel sounds indicate increased peristalsis c. Decreased bowel sounds can be a symptom of paralytic ileus d. All of the above 18. Independent nursing intervention commonly used for immobilized patients include all of the following except: a. Active or passive ROM exercises, body repositioning, and activities of daily living (ADLs) as tolerated b. Deep-breathing and coughing exercises with change of position every 2 hours c. Diaphragmatic and abdominal breathing exercises and increased hydration d. Weight bearing on a tilt table, total parenteral nutrition, and vitamin therapy 19. Independent nursing interventions commonly used for patients with pressure ulcers include: a. Changing the patients position regularly to minimize pressure b. Applying a drying agent such as an antacid to decrease moisture at the ulcer site c. Debriding the ulcer to remove necrotic tissue, which can impede healing d. Placing the patient in a whirlpool bath containing povidone-iodine solution as tolerated 20. A female patient has gained 24 lb after being admitted to the hospital. Im such a horse; I just cant stand myself like this, she tells the nurse. After assessing the patient, the nurse writes the following nursing diagnosis: Body image disturbance. To arrive at this diagnosis, the nurse should include which of the following assessment findings?
a. The patients perception of her body before the hospitalization and weight gain b. The significance the patient places on these changes c. The patients feelings about her body d. All of the above 21. Stressors cause the release of the mineralocorticoid aldosterone, which regulates sodium absorption and potassium excretion in the renal tubules, resulting in: a. The need for supplemental potassium b. The need for a low-sodium (500-mg) diet c. The conservation of water and maintenance of blood volume d. Increased diuresis 22. In planning the care of a patient who is exposed to multiple stressors such as separation from loved ones, anxiety about impending surgery, and concern about potential complications or death, the nurse must: a. Use both a structured and an unstructured format when interviewing the patient b. Know the stressors affecting the patient c. Develop the expected outcomes for each nursing diagnosis written for this patient d. All of the above 23. An accurate method of calculating the daily urine output of an incontinent patient wearing pads or diapers is to: a. Estimate the urine output b. Count the number of urine saturated pads c. Weigh a dry pad and each urine saturated pad and use a conversion calibration to calculate the urine output d. Weigh all the urine-saturated pads together and use a conversion calibration to calculate the urine output 24. A fashion model is admitted via the emergency room with facial and chest burns. Her hospital stay includes 10 days in the intensive care unit and 5 days on the regular hospital unit. The patient has not been eating or sleeping and refuses to perform her activities of daily living (ADLs). She refuses to work with speech and physical therapists. Which of the following nursing diagnoses might appears on the patients current care plan? a. Potential for noncompliance: Self-harm related to disturbed body image b. Self-care deficit related to knowledge deficit and disturbed body image c. Disturbance in self-concept: Personal identifying related to self-esteem d. Disturbance in self-concept related to altered thought process 25. White the nurse is providing a patients personal hygiene, she observes that his skin is excessively dry. During this procedure the patient tells her that he is very thirsty. An appropriate nursing diagnosis would be:
a. Potential for impaired skin integrity related to altered gland function b. Potential for impaired skin integrity related to dehydration c. Impaired skin integrity relate to dehydration d. Impaired skin integrity related to altered circulation ANSWER AND RATIONALE
1.
Answer B. Arthritis is characterized by joint inflammation that is usually accompanied by pain and frequently accompanied by changes in structure. Synovitis is the inflammation of the synovial membrane, typically resulting from a traumatic injury or an aseptic wound. Bursitis is the inflammation of a bursa, typically one located between a bony prominence and a muscle or tendon. Tendinitis is the inflammation of tendon. Answer C. Hemoptysis is the expectoration of blood from the respiratory tract. A hemorrhage is abnormal internal or external bleeding. Hematopoiesis is blood cell formation. Hemopexis is blood coagulation. Answer B. Ataxia is lack of coordination in performing planned, purposeful movements, typically resulting from a neurologic deficit. Apraxia is the inability to perform purposeful movements even though no neuromuscular deficit exists. Fasciculations are fine twitching movements. Myokymia is a transient, spontaneous movement that occurs in muscle groups after strenuous exercise. Answer D. Hypercapnia is an elevation in the partial pressure of carbon dioxide in arterial blood (PaCO2). Hypernatremia is an elevated level of sodium in venous blood (more than 145 mEq/liter). Hypocalcemia is a decreased level of calcium in venous blood (less than 9 mg/dl). Hypoxemia is a reduced level of oxygen in arterial blood (less than 80 mm Hg while breathing room air). Answer B. The combining form penia means deficiency, as in thrombocytopenia (deficiency in the number of circulating blood plates). Rrhexis is a combining form meaning rupture, as in enterorrhexis (rupture of the intestine). Plast is a combining form meaning formation, as in rhino-plasty (formation of a nose using plastic surgery). Narco is a combining form meaning stupor, as in narcolepsy (a condition marked by recurrent attacks of drowsiness and sleep). Answer B. Fluid volume deficit related to fever is the appropriate nursing diagnosis based on this assessment. Potential for impaired skin integrity states a possible patient response. Potential for fluid volume deficit caused by fever implies a cause-and-effect relationship, which a nursing diagnosis should never do. Altered cardiopulmonary tissue perfusion related to fluid excess is an incorrect diagnosis based on a misinterpretation of the data. Answer D. A nursing diagnosis is a statement about a patients actual or potential health problem that is within the scope of independent nursing intervention. Medical terminology is never a part of the nursing diagnosis. An appropriate nursing diagnosis would be ineffective breathing pattern related to chest pain rather than ineffective breathing pattern caused by angina. Answer D. A water-soluble lubricant must be applied to the tip of the catheter to decrease friction and the risk of injury to the patients nasal mucosa. (If petrolatum or mineral oil were applied to the catheter and then aspirated, the patient could develop a lipoid pneumonia) The distance from the tip of the nose to the tip of the earlobe is the approximate distance from the point of insertion to the oropharynx. Sterile distilled water must be used to humidity the oxygen because oxygen administered by itself is a dry gas that can irritate the mucosa. Answer A. Patient safety is the major concern in this situation. According to the International Council of Nurses Code for Nurses: The nurse [should] take appropriate action to safeguard the individual when his or her care is endangered by a co-worker or any other person. In this case, talking with the head nurse immediately would be the best way to safeguard the patients safety. The nurse isnt necessarily an addict, she may be abusing a prescription medication.
2.
3.
4.
5.
6.
7.
8.
9.
10. Answer D. It is the staff nurses responsibility to be on time. The nurse manager should not assume a responsibility that belongs to the nurse. 11. Answer D. Although Medicare and Medicaid regulations and suggestions made by such groups as the National Kidney Foundation may serve as guidelines, a hospitals procedure manual details how the nurse should perform her specific duties. A states nurse practice act defines the scope of practice within that state, but not the specifics for each area of practice.
12. Answer A. The three elements necessary to establishes nursing malpractice are nursing error (administering penicillin to a patient with a documented allergy to the drug), injury (cerebral damage), and proximal cause (administering the penicillin caused the cerebral damage). Applying a hot water bottle or healing pad to a patient without a physicians order does not include the three required components. Assisting a patient out of bed with the bed locked in position is the correct nursing practice; therefore, the fracture was not the result of malpractice. Administering an incorrect medication is a nursing error; however, if such action resulted in a serious illness or chronic problem, the nurse could be sued for malpractice. 13. Answer B. Therapeutic communication is a two way, deliberative interaction between the patient and nurse in which they establish mutually acceptable, achievable goals of care. Before the patient can feel comfortable discussing his problems, however, and atmosphere of trust and acceptance must be established. 14. Answer C. Many variables affect patient nurse communication, including the patients cultural beliefs, experiences with hospitalization, age, emotional needs, and problems with speech, hearing, or comprehension. A patient admitted to the hospital for the first time for a scheduled cesarean section is probably anxious, but she had time to plan for the procedure, does not bring negative experiences from previous hospitalizations, and in most cases looks forward to the birth. 15. Answer D. Therapeutic communication is a fundamental component at all phases of the nursing process. In the planning phase, it allows the patient and nurse to formulate mutually acceptable and patient-oriented goals, which are the basis for developing an individualized care plan. In the implementation phase, effective communication is necessary for teaching the patient, motivating him to achieve goals, and assessing patient outcomes. Finally, in the evaluation phase, it is required to determine how well the patient has responded to interventions. 16. Answer C. Objective data are those which can be measured, like glucose levels. A complaint of polydipsia is subjective information obtained from the patient. 17. Answer D. Peristalsis is the muscular, rhythmic movement in the bowel wall that pushes food along the digestive tract distally. Increased bowel motility is indicated by rapid, high-pitched, hyperactive bowel sounds. Decreased bowel sounds, caused by decreased bowel motility, can be the initial sign of paralytic ileus (adynamic intestinal obstruction resulting from the lack of peristalsis), a common occurrence following abdominal surgery. 18. Answer D. The use of a tilt table for weight-beating exercises, parenteral nutrition, and vitamin therapy are not independent nursing interventions because they require a physicians order. Unless specifically contraindicated, the independent nursing interventions listed in A, B, and C may be part of the nursing care plan for an immobilized patient. 19. Answer A. Independent nursing interventions for a patient with pressure ulcers commonly include changing his position several times each day to avoid pressure to any part of his body, especially the involved area. Drying agents, which are prescribed by a physician, are contraindicated because wounds need moisture to heal. Whirlpool therapy and chemical debridement must be prescribed, and surgical debridement is done by the physician. 20. Answer D. All of the choices will help the nurse determine the extent of the problem. For example, asking how the patient felt about her body before hospitalization will help the nurse determine whether the disturbed body image is a crisis brought on by the weight gain or a long-standing problem. Asking what the change means to her will reveal whether she feels she has control over what is happening or believes the change is permanent. Body image is also related to how we think we compare to others or whether others find us attractive. 21. Answer C. Because aldosterone regulates the bodys sodium and potassium levels, it acts as an adaptive mechanism in maintaining blood volume and conserving water. Supplemental potassium usually is given to a patient with a low serum potassium level or one who is receiving a diuretic or other medication such as digoxin that has a mild diuretic effect. A low-sodium diet is usually prescribed for a patient with a high serum sodium level, as in congestive heart failure (CHF), hypertension, or prolonged episodes of edema. Diuresis is increased naturally when a healthy patient increases his intake of fluids, especially those containing caffeine. Patients receiving diuretics also experience increased diuresis. 22. Answer D. Interviewing the patient in both a structured and an unstructured format is an important part of the initial nursing assessment. The structured format uses questions that require a yea-or-no answer to help the nurse obtain information; the unstructured format uses open-ended questions that allow the patient to express himself more fully. The interview helps the nurse and patient identify the stressors and develop appropriate outcomes. 23. Answer C. Calculating the difference in weight between a dry pad and a urine saturated pad using conversion calibration will provide an accurate measure of urine output. For example, if the difference between the dry pad and the urine-saturated pad is 200 g, the urine output would be 200 ml (1g = 1 ml). The other methods will provide only an estimate of urine output.
24. Answer C. Disturbances in self-concept may manifest themselves as signs and symptoms of depression, such as changes in sleep patterns, eating habits, and energy levels. The other nursing diagnoses are not supported by the given situation. 25. Answer C. An appropriate nursing diagnosis for a patient with excessively dry skin is Impaired skin integrity (actual not potential) in this case, related to dehydration because the patient complains of thirst. Altered circulation is not usually an etiologic factor for dry skin. GROWTH AND DEVT 1. The nurse is caring for the mother of a newborn. The nurse recognizes that the mother needs more teaching regarding cord care because she a. keeps the cord exposed to the air. b. washes her hands before sponge bathing her baby. c. washes the cord and surrounding area well with water at each diaper change. d. checks it daily for bleeding and drainage. 2. A client telephones the clinic to ask about a home pregnancy test she used this morning. The nurse understands that the presence of which hormone strongly suggests a woman is pregnant? a. Estrogen b. HCG c. Alpha-fetoprotein d. Progesterone 3. a. b. c. d. 4. a. b. c. d. The nurse is assessing a six-month-old child. Which developmental skills are normal and should be expected? Speaks in short sentences. Sits alone. Can feed self with a spoon. Pulling up to a standing position. While teaching a 10 year-old child about their impending heart surgery, the nurse should Provide a verbal explanation just prior to the surgery Provide the child with a booklet to read about the surgery Introduce the child to another child who had heart surgery three days ago Explain the surgery using a model of the heart
5. When caring for an elderly client it is important to keep in mind the changes in color vision that may occur. What colors are apt to be most difficult for the elderly to distinguish? a. Red and blue. b. Blue and gold. c. Red and green. d. Blue and green. 6. is a. b. c. d. While giving nursing care to a hospitalized adolescent, the nurse should be aware that the MAJOR threat felt by the hospitalized adolescent Pain management Restricted physical activity Altered body image Separation from family
7. A woman who is 32 years old and 35 weeks pregnant has had rupture of membranes for eight hours and is 4 cm dilated. Since she is a candidate for infection, the nurse should include which of the following in the care plan? a. Universal precautions. b. Oxytocin administration. c. Frequent temperature monitoring. d. More frequent vaginal examinations. 8. The nurse prepares for a Denver Screening test with a 3 year-old child in the clinic. The mother asks the nurse to explain the purpose of the test. The BEST response is to tell her that the test a. Measures potential intelligence b. Assesses a childs development c. Evaluates psychological responses d. Diagnoses specific problems
9. A 27-year-old woman has Type I diabetes mellitus. She and her husband want to have a child so they consulted her diabetologist, who gave her information on pregnancy and diabetes. Of primary importance for the diabetic woman who is considering pregnancy should be a. a review of the dietary modifications that will be necessary. b. early prenatal medical care. c. adoption instead of conception. d. understanding that this is a major health risk to the mother. 10. a. b. c. d. The nurse is planning care for an 18 month-old child. Which of the following should be included the in the childs care? Hold and cuddle the child often Encourage the child to feed himself finger food Allow the child to walk independently on the nursing unit Engage the child in games with other children
11. The nurse in an infertility clinic is discussing the treatment routine. The nurse advises the couple that the major stressor for couples being treated for infertility is usually a. having to tell their families. b. the cost of the interventions. c. the inconvenience of multiple tests. d. the right scheduling of sexual intercourse. 12. a. b. c. d. The nurse is assessing a four month-old infant. The nurse would anticipate finding that the infant would be able to Hold a rattle Bang two blocks Drink from a cup Wave bye-bye
13. The nurse is evaluating a new mother feeding her newborn. Which observation indicates the mother understands proper feeding methods for her newborn? a. Holding the bottle so the nipple is always filled with formula. b. Allowing her seven pound baby to sleep after taking 1 ounces from the bottle. c. Burping the baby every ten minutes during the feeding. d. Warming the formula bottle in the microwave for 15 seconds and giving it directly to the baby. 14. The nurse is caring for a pregnant client. The client asks how the doctor could tell she was pregnant just by looking inside. The nurse tells her the most likely explanation is that she had a positive Chadwicks sign, which is a a. Bluish coloration of the cervix and vaginal walls b. Pronounced softening of the cervix c. Clot of very thick mucous that obstructs the cervical canal d. Slight rotation of the uterus to the right 15. When caring for an elderly client it is important to keep in mind the changes in color vision that may occur. What colors are apt to be most difficult for the elderly to distinguish? a. Red and blue. b. Blue and gold. c. Red and green. d. Blue and green. 16. a. b. c. d. The nurses FIRST step in nutritional counseling/teaching for a pregnant woman is to Teach her how to meet the needs of self and her family Explain the changes in diet necessary for pregnant women Question her understanding and use of the food pyramid Conduct a diet history to determine her normal eating routines
17. A woman who is six months pregnant is seen in antepartal clinic. She states she is having trouble with constipation. To minimize this condition, the nurse should instruct her to a. increase her fluid intake to three liters/day. b. request a prescription for a laxative from her physician. c. stop taking iron supplements. d. take two tablespoons of mineral oil daily. 18. The nurse is observing children playing in the hospital playroom. She would expect to see 4 year-old children playing a. Competitive board games with older children
b. With their own toys along side with other children c. Alone with hand held computer games d. Cooperatively with other preschoolers 19. The nurse is caring for residents in a long term care setting for the elderly. Which of the following activities will be MOST effective in meeting the growth and development needs for persons in this age group? a. Aerobic exercise classes b. Transportation for shopping trips c. Reminiscence groups d. Regularly scheduled social activities 20. A pregnant woman is advised to alter her diet during pregnancy by increasing her protein and Vitamin C to meet the needs of the growing fetus. Which diet BEST meets the clients needs? a. Scrambled egg, hash browned potatoes, half-glass of buttermilk, large nectarine b. 3oz. chicken, C. corn, lettuce salad, small banana c. 1 C. macaroni, C. peas, glass whole milk, medium pear d. Beef, C. lima beans, glass of skim milk, C. strawberries ANSWER AND RATIONALE 1. Answer C. Exposure to air helps dry the cord. Good hand washing is the prime mechanism for preventing infection. Washing the surrounding area is fine but wetting the cord keeps it moist and predisposes it to infection. It is important to check for complications of bleeding and drainage that might occur. 2. Answer B. Human chorionic gonadotropin (HCG) is the biologic marker on which pregnancy tests are based. Reliability is about 98%, but the test does not positively confirm pregnancy. 3. Answer B. The child develops language skills between the ages of one and three. A six-month-old child is learning to sit alone. The child begins to use a spoon at 12-15 months of age. The baby pulls himself to a standing position about ten months of age. 4. Answer D. According to Piaget, the school age child is in the concrete operations stage of cognitive development. Using something concrete, like a model will help the child understand the explanation of the heart surgery. 5. Answer D. The elderly are better able to distinguish between red and blue because of the difference in wavelengths. The elderly are better able to distinguish between blue and gold because of the difference in wavelengths. The elderly are better able to distinguish between red and green because of the difference in wavelengths. Red and green color blindness is an inherited disorder that is unrelated to age. The elderly have poor blue-green discrimination. The effects of age are greatest on short wavelengths. These changes are related to the yellowing of the lens with age. 6. Answer C. The hospitalized adolescent may see each of these as a threat, but the major threat that they feel when hospitalized is the fear of altered body image, because of the emphasis on physical appearance. 7. Answer C. Universal precautions are necessary for all clients but a specific assessment of the clients temperature will give an indication the client is becoming infected. Oxytocin may be needed to induce labor if it is not progressing, but it is not done initially.Temperature elevation will indicate beginning infection. This is the most important measure to help assess the client for infections, since the lost mucous plug and the ruptured membranes increase the potential for ascending bacteria from the reproductive tract. This will infect the fetus, membranes, and uterine cavity. More frequent vaginal examinations are not recommended, as frequent vaginal exams can increase chances of infection. 8. Answer B. The Denver Developmental Test II is a screening test to assess children from birth through 6 years in personal/social, fine motor adaptive, language and gross motor development. A child experiences the fun of play during the test. 9. Answer B. A review of dietary modifications is important once the woman is pregnant. However, it is not of primary importance when considering pregnancy. Pregnancy makes metabolic control of diabetes more difficult. It is essential that the client start prenatal care early so that potential complications can be controlled or minimized by the efforts of the client and health care team. The alternative of adoption is not necessary just because the client is a diabetic. Many diabetic women have pregnancies with successful outcomes if they receive good care. While there is some risk to the pregnant diabetic woman, it is not considered a major health risk. The greater risk is to the fetus. 10. Answer B. According to Erikson, the toddler is in the stage of autonomy versus shame and doubt. The nurse should encourage increasingly independent activities of daily living. 11. Answer D. Having to tell families may also be a factor contributing to stress but is not the major stressor. Cost may also be a contributing factor to stress but is not usually the major factor. The inconvenience of multiple tests may also be a factor contributing to stress but is not usually the major factor. Sexual activity "on demand is the major cause of stress for most infertile couples. 12. Answer A. The age at which a baby will develop the skill of grasping a toy with help is 4 to 6 months. 13. Answer A. Holding the bottle so the nipple is always filled with formula prevents the baby from sucking air. Sucking air can cause gastric distention and intestinal gas pains. A seven-pound baby should be getting 50 calories per pound: 350 calories per day. Standardized formulas have 20 calories per ounce. This seven-pound baby needs 17.5 ounces per day. 17.5 ounces per day divided by 6-8 feedings equals 2-3 ounces per feeding. A normal newborn without feeding problems could be burped halfway through the feeding and again at the end. If burping needs to be at intervals, it should be done by ounces or half ounces, not minutes. Microwaving is not recommended as a method of warming due to the uneven heating of the formula. If used, the formula should be shaken after warming and the temperature then checked with a drop on the wrist. The recommended method of warming is to place the bottle in a pan of hot water to warm, and then check the temperature on the wrist before feeding.
14. Answer A. Chadwicks sign is a bluish-purple coloration of the cervix and vaginal walls, occurring at 4 weeks of pregnancy, that is caused by vasocongestion. 15. Answer D. The elderly are better able to distinguish between red and blue because of the difference in wavelengths. Red and green color blindness is an inherited disorder that is unrelated to age. The elderly have poor blue-green discrimination. The effects of age are greatest on short wavelengths. These changes are related to the yellowing of the lens with age. 16. Answer D. Assessment is always the first step in planning teaching for any client. 17. Answer A. In pregnancy, constipation results from decreased gastric motility and increased water reabsorption in the colon caused by increased levels of progesterone. Increasing fluid intake to three liters a day will help prevent constipation. The client should increase fluid intake, increase roughage in the diet, and increase exercise as tolerated. Laxatives are not recommended because of the possible development of laxative dependence or abdominal cramping. Iron supplements are necessary during pregnancy, as ordered, and should not be discontinued. The client should increase fluid intake, increase roughage in the diet, and increase exercise as tolerated. Laxatives are not recommended because of the possible development of laxative dependence or abdominal cramping. Mineral oil is especially bad to use as a laxative because it decreases the absorption of fat-soluble vitamins (A, D, E, K) if taken near mealtimes. 18. Answer D. Cooperative play is typical of the preschool period. 19. Answer C. According to Eriksons theory, older adults need to find and accept the meaningfulness of their lives, or they may become depressed, angry, and fear death. Reminiscing contributes to successful adaptation by maintaining self-esteem, reaffirming identity, and working through loss. 20. Answer D. Beef and beans are an excellent source of protein as is skim milk. Strawberries are a good source of Vitamin C.
Sample Questions for LEADERSHIP, MANAGEMENT, BIOETHICS AND RESEARCH Posted by Cedric on Jun 17, 2009 1. Ms. Castro is newly-promoted to a patient care manager position. She updates her knowledge on the theories in management and leadership in order to become effective in her new role. She learns that some managers have low concern for services and high concern for staff. Which style of management refers to this? a. b. c. d. Organization Man Impoverished Management Country Club Management Team Management
2. Her former manager demonstrated passion for serving her staff rather than being served. She takes time to listen, prefers to be a teacher first before being a leader, which is characteristic of a. b. c. d. Transformational leader Transactional leader Servant leader Charismatic leader
3. On the other hand, Ms. Castro notices that the Chief Nurse Executive has charismatic leadership style. Which of the following behaviors best describes this style? a. b. c. Possesses inspirational quality that makes followers gets attracted of him and regards him with reverence Acts as he does because he expects that his behavior will yield positive results Uses visioning as the core of his leadership
d. 4.
Matches his leadership style to the situation at hand.
Which of the following conclusions of Ms. Castro about leadership characteristics is TRUE? a. b. c. d. There is a high correlation between the communication skills of a leader and the ability to get the job done. A manager is effective when he has the ability to plan well. Assessment of personal traits is a reliable tool for predicting a managers potential. There is good evidence that certain personal qualities favor success in managerial role.
5.
She reads about Path Goal theory. Which of the following behaviors is manifested by the leader who uses this theory? a. b. c. d. Recognizes staff for going beyond expectations by giving them citations Challenges the staff to take individual accountability for their own practice Admonishes staff for being laggards. Reminds staff about the sanctions for non performance.
6.
One leadership theory states that leaders are born and not made, which refers to which of the following theories? a. b. c. d. Trait Charismatic Great Man Situational
7. She came across a theory which states that the leadership style is effective dependent on the situation. Which of the following styles best fits a situation when the followers are self-directed, experts and are matured individuals? a. b. c. d. Democratic Authoritarian Laissez faire Bureaucratic
8. She surfs the internet for more information about leadership styles. She reads about shared leadership as a practice in some magnet hospitals. Which of the following describes this style of leadership? a. Leadership behavior is generally determined by the relationship between the leaders personality and the specific situation Leaders believe that people are basically good and need not be closely controlled Leaders rely heavily on visioning and inspire members to achieve results Leadership is shared at the point of care.
b. c. d.
9. Ms. Castro learns that some leaders are transactional leaders. Which of the following does NOT characterize a transactional leader? a. b. c. d. Focuses on management tasks Is a caretaker Uses trade-offs to meet goals Inspires others with vision
10. She finds out that some managers have benevolent-authoritative style of management. Which of the following behaviors will she exhibit most likely? a. b. c. d. Have condescending trust and confidence in their subordinates Gives economic or ego awards Communicates downward to the staff Allows decision making among subordinates
11. Harry is a Unit Manager I the Medical Unit. He is not satisfied with the way things are going in his unit. Patient satisfaction rate is 60% for two consecutive months and staff morale is at its lowest. He decides to plan and initiate changes that will push for a turnaround in the condition of the unit. Which of the following actions is a priority for Harry? a. b. c. d. 12. Call for a staff meeting and take this up in the agenda. Seek help from her manager. Develop a strategic action on how to deal with these concerns. Ignore the issues since these will be resolved naturally.
She knows that there are external forces that influence changes in his unit. Which of the following is NOT an external force? a. b. c. d. Memo from the CEO to cut down on electrical consumption Demands of the labor sector to increase wages Low morale of staff in her unit Exacting regulatory and accreditation standards
13. After discussing the possible effects of the low patient satisfaction rate, the staff started to list down possible strategies to solve the problems head-on. Should they decide to vote on the best change strategy, which of the following strategies is referred to this? a. b. c. d. Collaboration Majority rule Dominance Compromise
14.
One staff suggests that they review the pattern of nursing care that they are using, which is described as a: a. b. c. d. job description system used to deliver care manual of procedure rules to be followed
15.
Which of the following is TRUE about functional nursing? a. b. c. d. Concentrates on tasks and activities Emphasizes use of group collaboration One-to-one nurse-patient ratio Provides continuous, coordinated and comprehensive nursing services
16.
Functional nursing has some advantages, which one is an EXCEPTION? a. b. c. d. Psychological and sociological needs are emphasized. Great control of work activities. Most economical way of delivering nursing services. Workers feel secure in dependent role
17.
He raised the issue on giving priority to patient needs. Which of the following offers the best way for setting priority? a. b. c. d. Assessing nursing needs and problems Giving instructions on how nursing care needs are to be met Controlling and evaluating the delivery of nursing care Assigning safe nurse: patient ratio
18.
Which of the following is the best guarantee that the patients priority needs are met? a. b. c. d. Checking with the relative of the patient Preparing a nursing care plan in collaboration with the patient Consulting with the physician Coordinating with other members of the team
19. When Harry uses team nursing as a care delivery system, he and his team need to assess the priority of care for a group of patients, which of the following should be a priority? a. Each patient as listed on the worksheet
b. c. d.
Patients who needs least care Medications and treatments required for all patients Patients who need the most care
20. She is hopeful that her unit will make a big turnaround in the succeeding months. Which of the following actions of Harry demonstrates that he has reached the third stage of change? a. b. c. d. Wonders why things are not what it used to be Finds solutions to the problems Integrate the solutions to his day-to-day activities Selects the best change strategy
21. Julius is a newly-appointed nurse manager of The Good Shepherd Medical Center, a tertiary hospital located within the heart of the metropolis. He thinks of scheduling planning workshop with his staff in order to ensure an effective and efficient management of the department. Should he decide to conduct a strategic planning workshop, which of the following is NOT a characteristic of this activity? a. b. c. d. 22. Long-term goal-setting Extends to 3-5 years in the future Focuses on routine tasks Determines directions of the organization
Which of the following statements refer to the vision of the hospital? a. b. c. d. The Good Shepherd Medical Center is a trendsetter in tertiary health care in the Philippines in the next five years Goal The officers and staff of The Good Shepherd Medical Center believe in the unique nature of the human person All the nurses shall undergo continuing competency training program. The Good Shepherd Medical Center aims to provide a patient-centered care in a total healing environment.
23. The statement, The Good Shepherd Medical Center aims to provide patient-centered care in a total healing environment refers to which of the following? a. b. c. d. Vision Goal Philosophy Mission
24. Julius plans to revisit the organizational chart of the department. He plans to create a new position of a Patient Educator who has a coordinating relationship with the head nurse in the unit. Which of the following will likely depict this organizational relationship? a. Box
b. c. d.
Solid line Broken line Dotted line
25. He likewise stresses the need for all the employees to follow orders and instructions from him and not from anyone else. Which of the following principles does he refer to? a. b. c. d. Scalar chain Discipline Unity of command Order
26. Julius orients his staff on the patterns of reporting relationship throughout the organization. Which of the following principles refer to this? a. b. c. d. Span of control Hierarchy Esprit d corps Unity of direction
27. He emphasizes to the team that they need to put their efforts together towards the attainment of the goals of the program. Which of the following principles refers to this? a. b. c. d. Span of control Unity of direction Unity of command Command responsibility
28. Julius stresses the importance of promoting esprit d corps among the members of the unit. Which of the following remarks of the staff indicates that they understand what he pointed out? a. b. c. d. 29. Lets work together in harmony; we need to be supportive of one another In order that we achieve the same results; we must all follow the directives of Julius and not from other managers. We will ensure that all the resources we need are available when needed. We need to put our efforts together in order to raise the bar of excellence in the care we provide to all our patients.
He discusses the goal of the department. Which of the following statements is a goal? a. b. Increase the patient satisfaction rate Eliminate the incidence of delayed administration of medications
c. d.
Establish rapport with patients. Reduce response time to two minutes.
30. He wants to influence the customary way of thinking and behaving that is shared by the members of the department. Which of the following terms refer to this? a. b. c. d. Organizational chart Cultural network Organizational structure Organizational culture
31. He asserts the importance of promoting a positive organizational culture in their unit. Which of the following behaviors indicate that this is attained by the group? a. b. c. d. Proactive and caring with one another Competitive and perfectionist Powerful and oppositional Obedient and uncomplaining
32. Stephanie is a new Staff Educator of a private tertiary hospital. She conducts orientation among new staff nurses in her department. Joseph, one of the new staff nurses, wants to understand the channel of communication, span of control and lines of communication. Which of the following will provide this information? a. b. c. d. Organizational structure Policy Job description Manual of procedures
33. Stephanie is often seen interacting with the medical intern during coffee breaks and after duty hours. What type of organizational structure is this? a. b. c. d. Formal Informal Staff Line
34. She takes pride in saying that the hospital has a decentralized structure. Which of the following is NOT compatible with this type of model? a. b. Flat organization Participatory approach
c. d. 35.
Shared governance Tall organization
Centralized organizations have some advantages. Which of the following statements are TRUE? 1. Highly cost-effective 2. Makes management easier 3. Reflects the interest of the worker 4. Allows quick decisions or actions. a. b. c. d. 1&2 2&4 2, 3& 4 1, 2, & 4
36.
Stephanie delegates effectively if she has authority to act, which is BEST defined as: a. b. c. d. having responsibility to direct others being accountable to the organization having legitimate right to act telling others what to do
37. Regardless of the size of a work group, enough staff must be available at all times to accomplish certain purposes. Which of these purposes is NOT included? a. b. c. d. 38. Meet the needs of patients Provide a pair of hands to other units as needed Cover all time periods adequately. Allow for growth and development of nursing staff.
Which of the following guidelines should be least considered in formulating objectives for nursing care? a. b. c. d. Written nursing care plan Holistic approach Prescribed standards Staff preferences
39. Stephanie considers shifting to transformational leadership. Which of the following statements best describes this type of leadership? a. Uses visioning as the essence of leadership.
b. c. d.
Serves the followers rather than being served. Maintains full trust and confidence in the subordinates Possesses innate charisma that makes others feel good in his presence.
40. As a manager, she focuses her energy on both the quality of services rendered to the patients as well as the welfare of the staff of her unit. Which of the following management styles does she adopt? a. b. c. d. Country club management Organization man management Team management Authority-obedience management
ANSWER AND RATIONALE 1. Answer: (C) Country Club Management Country club management style puts concern for the staff as number one priority at the expense of the delivery of services. He/she runs the department just like a country club where every one is happy including the manager. 2. Answer: (C) Servant leader Servant leaders are open-minded, listen deeply, try to fully understand others and not being judgmental 3. Answer: (A) Possesses inspirational quality that makes followers gets attracted of him and regards him with reverence Charismatic leaders make the followers feel at ease in their presence. They feel that they are in good hands whenever the leader is around. 4. Answer: (C) Assessment of personal traits is a reliable tool for predicting a managers potential. It is not conclusive that certain qualities of a person would make him become a good manager. It can only predict a managers potential of becoming a good one. 5. Answer: (A) Recognizes staff for going beyond expectations by giving them citations Path Goal theory according to House and associates rewards good performance so that others would do the same 6. Answer: (C) Great Man Leaders become leaders because of their birth right. This is also called Genetic theory or the Aristotelian theory 7. Answer: (C) Laissez faire Laissez faire leadership is preferred when the followers know what to do and are experts in the field. This leadership style is relationshiporiented rather than task-centered. 8. Answer: (D) Leadership is shared at the point of care. Shared governance allows the staff nurses to have the authority, responsibility and accountability for their own practice. 9. Answer: (D) Inspires others with vision Inspires others with a vision is characteristic of a transformational leader. He is focused more on the day-to-day operations of the department/unit. 10. Answer: (A) Have condescending trust and confidence in their subordinates Benevolent-authoritative managers pretentiously show their trust and confidence to their followers 11. Answer: (A) Call for a staff meeting and take this up in the agenda. This will allow for the participation of every staff in the unit. If they contribute to the solutions of the problem, they will own the solutions; hence the chance for compliance would be greater.
12. Answer: (C) Low morale of staff in her unit Low morale of staff is an internal factor that affects only the unit. All the rest of the options emanate from the top executive or from outside the institution. 13. Answer: (B) Majority rule Majority rule involves dividing the house and the highest vote wins.1/2 + 1 is a majority. 14. Answer: (B) system used to deliver care A system used to deliver care. In the 70s it was termed as methods of patient assignment; in the early 80s it was called modalities of patient care then patterns of nursing care in the 90s until recently authors called it nursing care systems. 15. Answer: (A) Concentrates on tasks and activities Functional nursing is focused on tasks and activities and not on the holistic care of the patients 16. Answer: (A) Psychological and sociological needs are emphasized. When the functional method is used, the psychological and sociological needs of the patients are neglected; the patients are regarded as tasks to be done 17. Answer: (A) Assessing nursing needs and problems This option follows the framework of the nursing process at the same time applies the management process of planning, organizing, directing and controlling 18. Answer: (B) Preparing a nursing care plan in collaboration with the patient The best source of information about the priority needs of the patient is the patient himself. Hence using a nursing care plan based on his expressed priority needs would ensure meeting his needs effectively. 19. Answer: (D) Patients who need the most care In setting priorities for a group of patients, those who need the most care should be number-one priority to ensure that their critical needs are met adequately. The needs of other patients who need less care ca be attended to later or even delegated to assistive personnel according to rules on delegation. 20. Answer: (C) Integrate the solutions to his day-to-day activities Integrate the solutions to his day-to-day activities is expected to happen during the third stage of change when the change agent incorporate the selected solutions to his system and begins to create a change. 21. Answer: (C) Focuses on routine tasks Strategic planning involves options A, B and D except C which is attributed to operational planning 22. Answer: (A) The Good Shepherd Medical Center is a trendsetter in tertiary health care in the Philippines in the next five years A vision refers to what the institution wants to become within a particular period of time. 23. Answer: (B) Goal B 24. Answer: (C) Broken line This is a staff relationship hence it is depicted by a broken line in the organizational structure 25. Answer: (C) Unity of command The principle of unity of command means that employees should receive orders coming from only one manager and not from two managers. This averts the possibility of sowing confusion among the members of the organization 26. Answer: (B) Hierarchy Hierarchy refers to the pattern of reporting or the formal line of authority in an organizational structure. 27. Answer: (B) Unity of direction Unity of direction means having one goal or one objective for the team to pursue; hence all members of the organization should put their efforts together towards the attainment of their common goal or objective.
28. Answer: (A) Lets work together in harmony; we need to be supportive of one another The principle of esprit d corps refers to promoting harmony in the workplace, which is essential in maintaining a climate conducive to work. 29. Answer: (A) Increase the patient satisfaction rate Goal is a desired result towards which efforts are directed. Options AB, C and D are all objectives which are aimed at specific end. 30. Answer: (D) Organizational culture An organizational culture refers to the way the members of the organization think together and do things around them together. Its their way of life in that organization 31. Stephanie is a new Staff Educator of a private tertiary hospital. She conducts orientation among new staff nurses in her department. Joseph, one of the new staff nurses, wants to understand the channel of communication, span of control and lines of communication. Which of the following will provide this information? 32. Answer: (A) Organizational structure Organizational structure provides information on the channel of authority, i.e., who reports to whom and with what authority; the number of people who directly reports to the various levels of hierarchy and the lines of communication whether line or staff. 33. Answer: (B) Informal This is usually not published and oftentimes concealed. 34. Answer: (D) Tall organization Tall organizations are highly centralized organizations where decision making is centered on one authority level. 35. Answer: (A) 1 & 2 Centralized organizations are needs only a few managers hence they are less expensive and easier to manage 36. Answer: (C) having legitimate right to act Authority is a legitimate or official right to give command. This is an officially sanctioned responsibility 37. Answer: (B) Provide a pair of hands to other units as needed Providing a pair of hands for other units is not a purpose in doing an effective staffing process. This is a function of a staffing coordinator at a centralized model. 38. Answer: (D) Staff preferences Staff preferences should be the least priority in formulating objectives of nursing care. Individual preferences should be subordinate to the interest of the patients. 39. Answer: (A) Uses visioning as the essence of leadership. Transformational leadership relies heavily on visioning as the core of leadership. 40. Answer: (C) Team management Team management has a high concern for services and high concern for staff. 1. Katherine is a young Unit Manager of the Pediatric Ward. Most of her staff nurses are senior to her, very articulate, confident and sometimes aggressive. Katherine feels uncomfortable believing that she is the scapegoat of everything that goes wrong in her department. Which of the following is the best action that she must take? a. b. c. d. Identify the source of the conflict and understand the points of friction Disregard what she feels and continue to work independently Seek help from the Director of Nursing Quit her job and look for another employment.
2. As a young manager, she knows that conflict occurs in any organization. Which of the following statements regarding conflict is NOT true? a. b. c. d. Can be destructive if the level is too high Is not beneficial; hence it should be prevented at all times May result in poor performance May create leaders
3. Katherine tells one of the staff, I dont have time to discuss the matter with you now. See me in my office later when the latter asks if they can talk about an issue. Which of the following conflict resolution strategies did she use? a. b. c. d. Smoothing Compromise Avoidance Restriction
4. Kathleen knows that one of her staff is experiencing burnout. Which of the following is the best thing for her to do? a. b. c. d. Advise her staff to go on vacation. Ignore her observations; it will be resolved even without intervention Remind her to show loyalty to the institution. Let the staff ventilate her feelings and ask how she can be of help.
5. She knows that performance appraisal consists of all the following activities EXCEPT: a. b. c. d. Setting specific standards and activities for individual performance. Using agency standards as a guide. Determine areas of strength and weaknesses Focusing activity on the correction of identified behavior.
6. Which of the following statements is NOT true about performance appraisal? a. b. c. d. Informing the staff about the specific impressions of their work help improve their performance. A verbal appraisal is an acceptable substitute for a written report Patients are the best source of information regarding personnel appraisal. The outcome of performance appraisal rests primarily with the staff.
7. There are times when Katherine evaluates her staff as she makes her daily rounds. Which of the following is NOT a benefit of conducting an informal appraisal? a. b. c. d. The staff member is observed in natural setting. Incidental confrontation and collaboration is allowed. The evaluation is focused on objective data systematically. The evaluation may provide valid information for compilation of a formal report.
8. She conducts a 6-month performance review session with a staff member. Which of the following actions is appropriate? a. b. c. d. She asks another nurse to attest the session as a witness. She informs the staff that she may ask another nurse to read the appraisal before the session is over. She tells the staff that the session is manager-centered. The session is private between the two members.
9. Alexandra is tasked to organize the new wing of the hospital. She was given the authority to do as she deems fit. She is aware that the director of nursing has substantial trust and confidence in her capabilities, communicates through downward and upward channels and usually uses the ideas and opinions of her staff. Which of the following is her style of management? a. b. c. d. Benevolent authoritative Consultative Exploitive-authoritative Participative
10. She decides to illustrate the organizational structure. Which of the following elements is NOT included? a. b. c. d. Level of authority Lines of communication Span of control Unity of direction
11. She plans of assigning competent people to fill the roles designed in the hierarchy. Which process refers to this? a. b. c. d. Staffing Scheduling Recruitment Induction
12. She checks the documentary requirements for the applicants for staff nurse position. Which one is NOT necessary? a. b. c. d. Certificate of previous employment Record of related learning experience (RLE) Membership to accredited professional organization Professional identification card
13. Which phase of the employment process includes getting on the payroll and completing documentary requirements? a. b. c. d. Orientation Induction Selection Recruitment
14. She tries to design an organizational structure that allows communication to flow in all directions and involve workers in decision making. Which form of organizational structure is this? a. b. c. d. Centralized Decentralized Matrix Informal
15. In a horizontal chart, the lowest level worker is located at the a. b. c. d. Left most box Middle Right most box Bottom
16. She decides to have a decentralized staffing system. Which of the following is an advantage of this system of staffing? a. b. c. d. greater control of activities Conserves time Compatible with computerization Promotes better interpersonal relationship
17. Aubrey thinks about primary nursing as a system to deliver care. Which of the following activities is NOT done by a primary nurse? a. b. c. d. Collaborates with the physician Provides care to a group of patients together with a group of nurses Provides care for 5-6 patients during their hospital stay. Performs comprehensive initial assessment
18. Which pattern of nursing care involves the care given by a group of paraprofessional workers led by a professional nurse who take care of patients with the same disease conditions and are located geographically near each other? a. b. c. d. Case method Modular nursing Nursing case management Team nursing
19. St. Raphael Medical Center just opened its new Performance Improvement Department. Ms. Valencia is appointed as the Quality Control Officer. She commits herself to her new role and plans her strategies to realize the goals and objectives of the department. Which of the following is a primary task that they should perform to have an effective control system? a. b. c. d. Make an interpretation about strengths and weaknesses Identify the values of the department Identify structure, process, outcome standards & criteria Measure actual performances
20. Ms. Valencia develops the standards to be followed. Among the following standards, which is considered as a structure standard? a. b. c. d. The patients verbalized satisfaction of the nursing care received Rotation of duty will be done every four weeks for all patient care personnel. All patients shall have their weights taken recorded Patients shall answer the evaluation form before discharge
21. When she presents the nursing procedures to be followed, she refers to what type of standards? a. b. c. d. Process Outcome Structure Criteria
22. The following are basic steps in the controlling process of the department. Which of the following is NOT included? a. b. c. d. Measure actual performance Set nursing standards and criteria Compare results of performance to standards and objectives Identify possible courses of action
23. Which of the following statements refers to criteria? a. b. c. d. Agreed on level of nursing care Characteristics used to measure the level of nursing care Step-by-step guidelines Statement which guide the group in decision making and problem solving
24. She wants to ensure that every task is carried out as planned. Which of the following tasks is NOT included in the controlling process? a. b. c. d. Instructing the members of the standards committee to prepare policies Reviewing the existing policies of the hospital Evaluating the credentials of all nursing staff Checking if activities conform to schedule
25. Ms. Valencia prepares the process standards. Which of the following is NOT a process standard? a. b. c. d. Initial assessment shall be done to all patients within twenty four hours upon admission. Informed consent shall be secured prior to any invasive procedure Patients reports 95% satisfaction rate prior to discharge from the hospital. Patient education about their illness and treatment shall be provided for all patients and their families.
26. Which of the following is evidence that the controlling process is effective? a. b. c. d. The things that were planned are done Physicians do not complain. Employees are contended There is an increase in customer satisfaction rate.
27. Ms. Valencia is responsible to the number of personnel reporting to her. This principle refers to:
a. b. c. d.
Span of control Unity of command Carrot and stick principle Esprit d corps
28. She notes that there is an increasing unrest of the staff due to fatigue brought about by shortage of staff. Which action is a priority? a. b. c. d. Evaluate the overall result of the unrest Initiate a group interaction Develop a plan and implement it Identify external and internal forces.
29. Kevin is a member of the Nursing Research Council of the hospital. His first assignment is to determine the level of patient satisfaction on the care they received from the hospital. He plans to include all adult patients admitted from April to May, with average length of stay of 3-4 days, first admission, and with no complications. Which of the following is an extraneous variable of the study? a. b. c. d. Date of admission Length of stay Age of patients Absence of complications
30. He thinks of an appropriate theoretical framework. Whose theory addresses the four modes of adaptation? a. b. c. d. Martha Rogers Sr. Callista Roy Florence Nightingale Jean Watson
31. He opts to use a self-report method. Which of the following is NOT TRUE about this method? a. b. c. d. Most direct means of gathering information Versatile in terms of content coverage Most accurate and valid method of data gathering Yields information that would be difficult to gather by another method
32. Which of the following articles would Kevin least consider for his review of literature? a. b. c. d. Story-Telling and Anxiety Reduction Among Pediatric Patients Turnaround Time in Emergency Rooms Outcome Standards in Tertiary Health Care Institutions Environmental Manipulation and Client Outcomes
33. Which of the following variables will he likely EXCLUDE in his study? a. b. c. d. Competence of nurses Caring attitude of nurses Salary of nurses Responsiveness of staff
34. He plans to use a Likert Scale to determine a. b. c. d. degree of agreement and disagreement compliance to expected standards level of satisfaction degree of acceptance
35. He checks if his instruments meet the criteria for evaluation. Which of the following criteria refers to the consistency or the ability to yield the same response upon its repeated administration?
a. b. c. d.
Validity Reliability Sensitivity Objectivity
36. Which criteria refer to the ability of the instrument to detect fine differences among the subjects being studied? a. b. c. d. Sensitivity Reliability Validity Objectivity
37. Which of the following terms refer to the degree to which an instrument measures what it is supposed to be measure? a. b. c. d. Validity Reliability Meaningfulness Sensitivity
38. He plans for his sampling method. Which sampling method gives equal chance to all units in the population to get picked? a. b. c. d. Random Accidental Quota Judgment
39. Raphael is interested to learn more about transcultural nursing because he is assigned at the family suites where most patients come from different cultures and countries. Which of the following designs is appropriate for this study? a. b. c. d. Grounded theory Ethnography Case study Phenomenology
40. The nursing theorist who developed transcultural nursing theory is a. b. c. d. Dorothea Orem Madeleine Leininger Betty Newman Sr. Callista Roy
ANSWER AND RATIONALE 1. Answer: (A) Identify the source of the conflict and understand the points of friction This involves a problem solving approach, which addresses the root cause of the problem. Answer: (B) Is not beneficial; hence it should be prevented at all times Conflicts are beneficial because it surfaces out issues in the open and can be solved right away. Likewise, members of the team become more conscientious with their work when they are aware that other members of the team are watching them. Answer: (C) Avoidance This strategy shuns discussing the issue head-on and prefers to postpone it to a later time. In effect the problem remains unsolved and both parties are in a lose-lose situation. Answer: (D) Let the staff ventilate her feelings and ask how she can be of help. Reaching out and helping the staff is the most effective strategy in dealing with burn out. Knowing that someone is ready to help makes the staff feel important; hence her self-worth is enhanced.
2.
3.
4.
5.
Answer: (D) Focusing activity on the correction of identified behavior. Performance appraisal deal with both positive and negative performance; is not meant to be a fault-finding activity Answer: (C) Patients are the best source of information regarding personnel appraisal. The patient can be a source of information about the performance of the staff but it is never the best source. Directly observing the staff is the best source of information for personnel appraisal. Answer: (C) The evaluation is focused on objective data systematically. Collecting objective data systematically can not be achieved in an informal appraisal. It is focused on what actually happens in the natural work setting. Answer: (D) The session is private between the two members. The session is private between the manager and the staff and remains to be so when the two parties do not divulge the information to others. Answer: (B) Consultative A consultative manager is almost like a participative manager. The participative manager has complete trust and confidence in the subordinate, always uses the opinions and ideas of subordinates and communicates in all directions.
6.
7.
8.
9.
10. Answer: (D) Unity of direction Unity of direction is a management principle, not an element of an organizational structure. 11. Answer: (A) Staffing Staffing is a management function involving putting the best people to accomplish tasks and activities to attain the goals of the organization. 12. Answer: (B) Record of related learning experience (RLE) Record of RLE is not required for employment purposes but it is required for the nurses licensure examination. 13. Answer: (B) Induction This step in the recruitment process gives time for the staff to submit all the documentary requirements for employment. 14. Answer: (B) Decentralized Decentralized structures allow the staff to make decisions on matters pertaining to their practice and communicate in downward, upward, lateral and diagonal flow. 15. Answer: (C) Rightmost box The leftmost box is occupied by the highest authority while the lowest level worker occupies the rightmost box. 16. Answer: (D) Promotes better interpersonal relationship Decentralized structures allow the staff to solve decisions by themselves, involve them in decision making; hence they are always given opportunities to interact with one another. 17. Answer: (B) Provides care to a group of patients together with a group of nurses This function is done in team nursing where the nurse is a member of a team that provides care for a group of patients. 18. Answer: (B) Modular nursing Modular nursing is a variant of team nursing. The difference lies in the fact that the members in modular nursing are paraprofessional workers. 19. Answer: (B) Identify the values of the department Identify the values of the department will set the guiding principles within which the department will operate its activities 20. Answer: (B) Rotation of duty will be done every four weeks for all patient care personnel. Structure standards include management system, facilities, equipment, materials needed to deliver care to patients. Rotation of duty is a management system. 21. Answer: (A) Process Process standards include care plans, nursing procedure to be done to address the needs of the patients.
22. Answer: (D) Identify possible courses of action This is a step in a quality control process and not a basic step in the control process. 23. Answer: (B) Characteristics used to measure the level of nursing care Criteria are specific characteristics used to measure the standard of care. 24. Answer: (A) Instructing the members of the standards committee to prepare policies Instructing the members involves a directing function. 25. Answer: (C) Patients reports 95% satisfaction rate prior to discharge from the hospital. This refers to an outcome standard, which is a result of the care that is rendered to the patient. 26. Answer: (A) The things that were planned are done Controlling is defined as seeing to it that what is planned is done. 27. Answer: (A) Span of control Span of control refers to the number of workers who report directly to a manager. 28. Answer: (B) Initiate a group interaction Initiate a group interaction will be an opportunity to discuss the problem in the open. 29. Answer: (C) Age of patients An extraneous variable is not the primary concern of the researcher but has an effect on the results of the study. Adult patients may be young, middle or late adult. 30. Answer: (B) Sr. Callista Roy Sr. Callista Roy developed the Adaptation Model which involves the physiologic mode, self-concept mode, role function mode and dependence mode 31. Answer: (C) Most accurate and valid method of data gathering The most serious disadvantage of this method is accuracy and validity of information gathered 32. Answer: (B) Turnaround Time in Emergency Rooms The article is for pediatric patients and may not be relevant for adult patients. 33. Answer: (C) Salary of nurses Salary of staff nurses is not an indicator of patient satisfaction, hence need not be included as a variable in the study. 34. Answer: (A) degree of agreement and disagreement Likert scale is a 5-point summated scale used to determine the degree of agreement or disagreement of the respondents to a statement in a study. 35. Answer: (B) Reliability Reliability is repeatability of the instrument; it can elicit the same responses even with varied administration of the instrument 36. Answer: (A) Sensitivity Sensitivity is an attribute of the instrument that allow the respondents to distinguish differences of the options where to choose from 37. Answer: (A) Validity Validity is ensuring that the instrument contains appropriate questions about the research topic 38. Answer: (A) Random Random sampling gives equal chance for all the elements in the population to be picked as part of the sample. 39. Answer: (B) Ethnography Ethnography is focused on patterns of behavior of selected people within a culture
40. Answer: (B) Madeleine Leininger Madeleine Leininger developed the theory on transcultural theory based on her observations on the behavior of selected people within a culture MANAGEMENT of Care Questions 1. Angelina, an R.N., reports to work looking unkempt. Maegan, another R.N., approaches when she notices her using uncoordinated movements. Angelinas breath reeks of peppermints and Maegan suspects Angelina may be intoxicated. What is the best initial nursing action for Maegan to take? a. Call the supervisor and report Angelina. b. Confront Angelina, saying that she feels she is intoxicated, and relieve her of her nursing duties immediately. c. Ignore the situation. d. Give Angelina a lecture about substance abuse and do nothing else. 2. Carol has a nasogastric tube after colon surgery. Which one of these tasks can be safely delegated to an unlicensed assistive personnel (UAP)? a. To observe the type and amount of nasogastric tube drainage b. Monitor the client for nausea or other complications c. Irrigate the nasogastric tube with the ordered irrigant d. Perform nostril and mouth care 3. Britney is admitted with a diagnosis of schizophrenia. The client refuses to take medication and states I dont think I need those medications. They make me too sleepy and drowsy. I insist that you explain their use and side effects. The nurse should understand that: a. a referral is needed to the psychiatrist who is to provide the client with answers b. the client has a right to know about the prescribed medications c. such education is an independent decision of the individual nurse whether or not to teach clients about their medications d. clients with schizophrenia are at a higher risk of psychosocial complications when they know about their medication side effects 4. James with a diagnosis of bipolar disorder has been referred to a local boarding home for consideration for placement. The social worker telephoned the hospital unit for information about the clients mental status and adjustment. The appropriate response of the nurse should be which of these statements? a. "I am sorry. Referral information can only be provided by the clients providers" b. "I can never give any information out by telephone. How do I know who you are?" c. "Since this is a referral, I can give you this information" d. "I need to get the clients written consent before I release any information to you" 5. a. b. c. d. A client tells the nurse, "I have something very important to tell you if you promise not to tell." The best response by the nurse is: "I must document and report any important information." "I cant make such a promise." "That depends on what you tell me." "I must report everything to the treatment team."
6. Helen, a nurse from the maternity unit is floated to the critical care unit because of staff shortage on the evening shift. Which client would be appropriate to assign to this nurse? A client with: a. Dopamine drip IV with vital signs monitored every 5 minutes b. a myocardial infarction that is free from pain and dysrhythmias c. a tracheotomy of 24 hours in some respiratory distress d. a pacemaker inserted this morning with intermittent capture 7. a. b. c. d. A client asks the nurse to call the police and states: I need to report that I am being abused by a nurse. The nurse should first: focus on reality orientation to place and person assist with the report of the clients complaint to the police obtain more details of the clients claim of abuse document the statement on the clients chart with a report to the manager
8. John, a client frequently admitted to the locked psychiatric unit repeatedly compliments and invites one of the nurses to go out on a date. The nurses response should be to: a. ask to not be assigned to this client or to work on another unit b. tell the client that such behavior is inappropriate c. inform the client that hospital policy prohibits staff to date clients d. discuss the boundaries of the therapeutic relationship with the client
9. A client continuously calls out to the nursing staff when anyone passes the clients door and asks them to do something in the room. The best response by the charge nurse would be to: a. keep the clients room door cracked to minimize the distractions b. assign 1 of the nursing staff to visit the client regularly c. reassure the client that 1 staff person will check frequently if the client needs anything d. arrange for each staff member to go into the clients room to check on needs every hour on the hour 10. The nurse is responsible for several elderly clients, including a client on bed rest with a skin tear and hematoma from a fall 2 days ago. What is the best care assignment for this client? a. Assign an RN to provide total care of the client b. Assign a nursing assistant to help the client with self-care activities c. Delegate complete care to an unlicensed assistive personnel d. Supervise a nursing assistant for skin care 11. A 24-year-old woman had surgery today. Her father, a physician but not her surgeon, enters the nursing station and asks for her chart. The best action for the nurse to take is: a. to give him the chart as requested. b. not to allow him to read the chart. c. to ask the attending surgeon if it is permissible for him to read the chart. d. to ask the client if she wants him to read her chart. 12. a. b. c. d. When assessing a client, it is important for the nurse to be informed about cultural issues related to the clients background because: Normal patterns of behavior may be labeled as deviant, immoral, or insane The meaning of the clients behavior can be derived from conventional wisdom Personal values will guide the interaction between persons from 2 cultures The nurse should rely on her knowledge of different developmental mental stages
13. Robin, an adult male is scheduled for exploratory surgery this morning. After he is premedicated for surgery the nurse reviews his chart and discovers that he has not signed a consent form. The nurses action is based on which of the following understandings? a. Since the client came to the hospital consent is implied even if the consent for the surgery has not been signed. b. All invasive procedures require a consent form. c. The nurse should have him sign a consent form immediately d. The nurse should have the next of kin sign the necessary consent form 14. Zantac is ordered for an adult client. The nurse mistakenly administered Xanax. What is the most appropriate action for the nurse to take? a. Notify the physician and document in the nurses notes that the physician was notified of the error. b. Notify the supervisor, complete a medication error incident report, and document in the nurses notes that an incident report was completed c. Notify the house supervisor, assess client carefully, and document only if adverse or untoward effects occur. d. Notify the physician, complete an incident report, and document the notification of the physician and any assessments made. 15. A client with Guillain-Barr syndrome has been on a ventilator for three weeks, and can communicate only with eye blinks because of quadriplegia. The intensive care nursing staff sometimes have no time for this tedious communication process. The clients family comes infrequently since they run a family-owned restaurant that does not close until visiting hours are over. How should the nurse respond to the familys request for exemption from visiting hours? a. Arrange for a volunteer to stay with the client during the day to provide for socialization needs and to facilitate communication with staff. b. Explain to the family that consistency in enforcing rules is important to prevent complaints from the families of other clients. c. Suggest that the family visit in shifts during the normal visiting hours, since the client needs to sleep at night. d. Make an exception to visiting regulations because of the long-term nature of the clients recovery and the need for family support. 16. An adult client has continued slow bleeding from the graft after repair of an abdominal aortic aneurysm. Because of the clients unstable condition, he is in the intensive care unit where visitors are limited to the family. The client insists on having a visit from a medicine man whom the family visits regularly. How should the nurse interpret this request? a. The principle of justice prohibits giving one client a privilege that other clients are not permitted. b. Faith healers do not meet the standards for clergy exemption from visitation rules. c. Medicine men are not approved by the hospital as legitimate health care providers. d. Provision of holistic care requires that the clients belief system is honored. 17. Mrs. Jefferson is an 88-year-old client at a long-term care facility. Prior to administering any medication or treatment to this client the nurse must confirm identity by: a. asking the client if she is Mrs. Jefferson. b. reading the clients identification bracelet
c. reading the clients medical record. d. asking the roommate to state the clients name. 18. After working with a very demanding client, a nursing assistant tells the nurse, "I have had it with that client. I just cant do anything that pleases him. Im not going in there again." The nurses BEST response is: a. "He has a lot of problems. You need to be patient with him." b. "I will talk with him and try to figure out what to do." c. "He is scared and taking it out on you. Lets try to figure out what to do." d. "Ignore him and get the rest of your work done. Someone else can take care of him tomorrow." 19. a. b. c. d. 20. a. b. c. d. A client frequently compliments and invites the nurse to go out. The nurse should: Minimize further contact with the client Tell the client that his/her behavior is inappropriate Tell the client that hospital policy prohibits dating clients Discuss the boundaries of the relationship with the client Which one of the following could be safely delegated by the nurse to the nursing assistant? Observe a clients self-administration of insulin Cleanse and dress a small decubitus ulcer Monitor a clients response to physical therapy Apply and care for a clients rectal pouch
1. Answer B. Calling the supervisor is a secondary measure after confronting the nurse and relieving the nurse of her duties. You cannot always assume the supervisor will be immediately available, and client safety should be addressed first. When another nurse is unable to perform her nursing duties due to substance abuse, she should not be allowed to continue them, as client safety is a primary concern. Ignoring the situation is against the professional code of conduct for nurses. Angelina needs to be relieved of her duties. She probably would not benefit from a lecture in her condition. 2. Answer D. Skin care around a nasogastric tube is a routine task that is appropriate for UAPs. The other tasks would be appropriate for a PN or RN to do since they are advanced skills or require evaluation. 3. Answer B. Clients have a right to informed consent which includes information about medications, treatments, and diagnostic studies. 4. Answer D. In order to release information about a client there must be a signed consent form with designation of to whom information can be given, and what information can be shared. 5. Answer B. Secrets are inappropriate in therapeutic relationships and are counterproductive to the therapeutic efforts of the interdisciplinary team. Secrets may be related to risk for harm to self or others. The nurse honors and helps clients to understand rights, limitations, and boundaries regarding confidentiality. 6. Answer B. This client is the most stable with minimal risk of complications or instability. The nurse can utilize basic nursing skills to care for this client. 7. Answer C. Obtain more details of the clients claim of abuse. The advocacy role of the professional nurse as well as the legal duty of the reasonable prudent nurse requires the investigation of claims of abuse or violation of rights. The nurse is legally accountable for actions delegated to others. The application of the nursing process requires that the nurse gather more information, further assessment, before documentation or the reporting of the complaint. 8. Answer D. The nurse-client relationship is one with professional not social boundaries. Consistent adherence to the limits of the professional relationship builds trust. 9. Answer B. Assign 1 of the nursing staff to visit the client regularly. Regular, frequent, planned contact by 1 staff member provides continuity of care and communicates to the client that care will be available when needed. 10. Answer D. Supervise a nursing assistant for skin care. The nursing assistant can inspect the skin while giving hygiene care, but the nurse should supervise skin care since assessment and analysis are needed. 11. Answer B. The nurse must maintain the clients right of confidentiality. Since he is not the clients physician and does not have a medical need to see her chart, he should not be allowed to read the chart without written permission from the client, who is above the age of majority. Since he is not the clients physician and does not have a medical need to see her chart, he should not be allowed to read the chart without written permission from the client, who is above the age of majority. It is not the attending surgeon who can give permission for him to review the chart, it is the client. The client must give written permission for unauthorized persons to review her chart. This client had surgery today and is probably not alert enough to give legal permission, which must be written. 12. Answer A. Culture is an important variable in the assessment of individuals. To work effectively with clients, the nurse must be aware of a cultural distinctive qualities 13. Answer B. It cannot be legally assumed that the client consents to a procedure for which he has not given consent. This is not legally defensible. All invasive procedures require informed consent. The surgery is prescheduled and described as exploratory and therefore is not an emergency. If the client is an adult and has not been declared incompetent the client must sign the form. This client should not have surgery performed without written consent. The nurse must notify the physician immediately. The client has been premedicated for surgery and is not alert. He cannot give legal consent when under the influence of mind-altering drugs. The client is an adult and there is no evidence that he has been declared incompetent to make his own decisions. The surgery is exploratory. There is no indication it is for an immediately life-threatening condition. It is not appropriate to ask the next of kin to sign his consent form. 14. Answer D. In addition to notifying the physician and documenting it, the nurse should complete an incident report. The physician must be notified. An incident report should be completed. However, no record of the incident report should appear in the nurses notes.
The physician must be notified. An incident report should be completed. However, no record of the incident report should appear in the nurses notes. The physician must be notified of the medication error. An incident report should be completed. However, no record of the incident report should appear in the nurses notes. The nurse should document that the physician was notified and any assessments completed. 15. Answer D. The need for family support is vital to prevent discouragement and depression. A volunteer will not take the place of family. The need for family support is vital to prevent discouragement and depression, even at the risk of offending the families of other patients. Loss of a breadwinner during the lengthy recovery process may add financial problems for the family. Guillain-Barr syndrome is characterized by the onset of ascending paralysis, which may include respiratory muscles. Persons with Guillain-Barr syndrome may remain ventilator-dependent for weeks, but have full consciousness. The prognosis for recovery from Guillain-Barr syndrome is good, but is very much dependent upon the level of supportive care during the acute stage. 16. Answer D. The clients spiritual needs must be met within the framework of his personal belief systems, even if those beliefs differ from those of the nursing staff. The clients spiritual needs must be met within the framework of his personal belief systems, even if those beliefs differ from those of the nursing staff. The clients spiritual needs must be met within the framework of his personal belief systems, even if those beliefs differ from those of the nursing staff. The clients spiritual needs must be met within the framework of his personal belief systems, even if those beliefs differ from those of the nursing staff. 17. Answer B. An alert, oriented client should be asked to state her full name so that there is no confusion in identity. The ID bracelet will confirm identity when the client is not alert or oriented to person. Reading the name on the clients ID bracelet is the most accurate way to confirm identity. Reading the clients medical record will not confirm identity. The roommate is not an accurate source for client identification. 18. Answer C. This response explains the clients behavior without belittling the nursing assistants feelings. The nursing assistant is encouraged to help solve the problem with the nurse. 19. Answer D. The nurse-client relationship is one with professional not social boundaries. Consistent adherence to the limits of the professional relationship builds trust. 20. Answer D. The RN may delegate the application and care of rectal pouches to a nursing assistant, who should be capable of performing this task . psychosocial Adaptation NCLEX Review Questions Posted by admin on Sep 04, 2010 1. A man is admitted to the nursing care unit with a diagnosis of cirrhosis. He has a long history of alcohol dependence. During the late evening following his admission, he becomes increasingly disoriented and agitated. Which of the following would the client be least likely to experience? a. Diaphoresis and tremors. b. Increased blood pressure and heart rate. c. Illusions. d. Delusions of grandeur. 2. Mr. Wilson, 35, is admitted for bipolar illness, manic phase, after assaulting his landlord in an argument over Mr. Wilsons staying up all night playing loud music. Mr. Wilsons is hyperactive, intrusive, and has rapid, pressured speech. He has not slept in three days and appears thin and disheveled. Which of the following is the most essential nursing action at this time? a. Providing a meal and beverage for Mr. Wilson to eat in the dining room. b. Providing linens and toiletries for Mr. Wilson to attend to his hygiene. c. Consulting with the psychiatrist to order a hypnotic to promote sleep. d. Providing for client safety by limiting his privileges. 3. a. b. c. d. Which of the following would best indicate to the nurse that a depressed client is improving? Reduced levels of anxiety. Changes in vegetative signs. Compliance with medications. Requests to talk to the nurse.
4. An elderly man is admitted to the hospital. He was alert and oriented during the admission interview. However, his family states that he becomes disruptive and disoriented around dinnertime. One night he was shouting furiously and didnt know where he was. He was sedated and the next morning he was fine. At dinnertime the disruptive behavior returned. The client is diagnosed as having sundown syndrome. The clients son asks the nurse what causes sundown syndrome. The nurses best response is that it is attributed to a. an underlying depression. b. inadequate cerebral flow. c. changes in the sensory environment. d. fluctuating levels of oxygen exchange. 5. The nurse is discussing electroconvulsive therapy (ECT) with a client who asks how long it will be before she feels better. The nurse explains that the beneficial effects of ECT usually occur within
a. b. c. d.
one week. three weeks. four weeks. six weeks.
6. The nurse is assessing a 17-year-old female who is admitted to the eating disorders unit with a history of weight fluctuation, abdominal pain, teeth erosion, receding gums, and bad breath. She states that her health has been a problem but there are no other concerns in her life. Which of the following assessments will be the least useful as the nurse develops the care plan? a. Information regarding recent mood changes. b. Family functioning using a genogram. c. Ability to socialize with peers. d. Whether she has a sexual relationship with a boyfriend. 7. A 34-year-old woman is admitted for treatment of depression. Which of these symptoms would the nurse be least likely to find in the initial assessment? a. inability to make decisions. b. feelings of hopelessness. c. family history of depression. d. increased interest in sex. 8. The nurse is planning care for a client who has a phobic disorder manifested by a fear of elevators. Which goal would need to be accomplished first? The client a. demonstrates the relaxation response when asked. b. verbalizes the underlying cause of the disorder. c. rides the elevator in the company of the nurse. d. role plays the use of an elevator. 9. A teenage female is admitted with the diagnosis of anorexia nervosa. Upon admission, the nurse finds a bottle of assorted pills in the clients drawer. The client tells the nurse that they are antacids for stomach pains. The best response by the nurse would be a. "These pills arent antacids since they are all different." b. "Some teenagers use pills to lose weight." c. "Tell me about your week prior to being admitted." d. "Are you taking pills to change your weight?" 10. A mother with a Roman Catholic belief has given birth in an ambulance on the way to the hospital. The neonate is in very critical condition with little expectation of surviving the trip to the hospital. Which of these requests should the nurse in the ambulance anticipate and be prepared to do? a. The refusal of any treatment for self and the neonate until she talks to a reader b. The placement of a rosary necklace around the neonates neck and not to remove it unless absolutely necessary c. Arrange for a church elder to be at the emergency department when the ambulance arrives so a "laying on hands" can be done d. Pour fluid over the forehead backwards towards the back of the head and say "I baptize you in the name of the father, the son and the holy spirit. Amen." 11. Which statement by the client during the initial assessment in the the emergency department is most indicative for suspected domestic violence? a. "I am determined to leave my house in a week." b. "No one else in the family has been treated like this." c. "I have only been married for 2 months." d. "I have tried leaving, but have always gone back." 12. a. b. c. d. 13. a. b. c. d. Which of these statements by the nurse reflects the best use of therapeutic interaction techniques? "You look upset. Would you like to talk about it?" "Id like to know more about your family. Tell me about them." "I understand that you lost your partner. I dont think I could go on if that happened to me." "You look very sad. How long have you been this way?" When planning the therapeutic milieu, it is MOST important to select group activities which Match the clients preferences Are consistent with clients skills Achieve clients therapeutic goals Build skills of group participation
14. A client was admitted to the psychiatric unit for severe depression. After several days, the client continues to withdraw from other clients. Which of the following would be the MOST appropriate statement by the nurse to promote interaction with other clients? a. "Your doctor thinks its good for you to spend time with others." b. "It is important for you to participate in group activities." c. "Painting this picture will help you feel better." d. "Come play Chinese Checkers with Gerry and me." 15. a. b. c. d. 16. a. b. c. d. The nurse can BEST ensure the safety of a demented client who wanders from the room by Repeatedly reminding the client of time and place Explaining the risks of becoming lost Using soft restraints Attaching a wander-guard sensor band to the clients wrist A client with paranoid thoughts refuses to eat because he believes the food is poisoned. The MOST appropriate initial action is to Taste the food in the clients presence Suggest that food be brought from home Simply state the food is not poisoned Inform the client he will be tube fed if he does not eat
17. The nurse is caring for a severely depressed client who has just been admitted to the in-client psychiatric unit. Which of the following is a PRIORITY of care? a. Nutrition b. Elimination c. Rest d. Safety 18. A nurse is teaching a stress-management program for client. Which of the following beliefs will the nurse advocate as a method of coping with stressful life events? a. Avoidance of stress is an important goal for living. b. Control over ones response to stress is possible. c. Most people have no control over their level of stress. d. Significant others are important to provide care and concern. 19. a. b. c. d. 20. a. b. c. d. A student nurse is caring for a 75-year-old client who is very confused. The students communication tools should include: written directions for bathing. speaking very loudly. gentle touch while guiding ADLs (activities of daily living). flat facial expression. When a husband takes out his work frustrations and anger by abusing his wife at home, the nurse would identify this crisis as which type? psychiatric emergency crisis developmental crisis anticipated life transition dispositional crisis
ANSWER AND RATIONALE 1. Answer D. Diaphoresis and tremors occur in the first phase of alcohol withdrawal. The blood pressure and heart rate increase in the first phase of alcohol withdrawal. Illusions are common in persons withdrawing from alcohol. Illusions occur most often in dim artificial lighting where the environment is not perceived accurately. Delusions of grandeur are symptomatic of manic clients, not clients withdrawing from alcohol. The symptoms and history of alcohol abuse suggest this client is in alcohol withdrawal. 2. Answer D. Food and fluids are necessary. However, Mr. Wilsons hyperactivity does not allow him to sit quietly to eat. Finger foods "on the run will provide needed nourishment. When hyperactivity decreases, then approach Mr. Wilsons. regarding hygiene and grooming needs. Medications will be ordered. However, a thorough evaluation must be done first. Mr. Wilson has been assaultive with the landlord and it is reasonable to expect that he may be with peers and staff. His mental illness produces a hyperactive state and poor judgment and impulse control. External controls such as limiting of unit privileges will assist in feelings of security and safety. 3. Answer B. Reduced levels of anxiety do not indicate an improvement in depressive symptoms. Vegetative signs such as insomnia, anorexia, psychomotor retardation, constipation, diminished libido, and poor concentration are biological responses to depression. Improvement in these signs indicates a lifting of the depression. Compliance with medications does not indicate improvement in depression. Requests to talk to the nurse vary. Requests may show trust in the nurse but are not a sign that depression has diminished. 4. Answer C. An underlying depression does not cause sundown syndrome. There is not sufficient evidence to suggest he has inadequate cerebral blood flow. Because the confusion occurs at sundown, the cause is probably changes in the sensory environment. Sundown
syndrome is related to environmental and sensory abnormalities that lead to acute confusion. Fluctuating levels of oxygen exchange do not cause sundown syndrome. 5. Answer A. Beneficial effects of ECT usually are evident after the first several treatments. Since treatments are administered at intervals of 48 hours, these effects are apparent after one week of therapy. Beneficial effects of ECT therapy are usually seen before three weeks. It takes three to four weeks for tricyclic antidepressants to take effect. Beneficial effects of ECT therapy are usually seen before four weeks. It takes three to four weeks for tricyclic antidepressants to take effect. Beneficial effects of ECT therapy are usually seen after the first few treatments. 6. Answer D. Information about mood changes is important to assess, as bulimia is often associated with affective disorders. Family functioning is the most essential point to assess, as it reveals if binge eating is triggered by conflict within the family. Information about ability to socialize with peers is important to assess, as it is possible the problem initiated with peer relationships. It is inappropriate to ask about her sexual relationships. 7. Answer D. Indecisiveness and fear of being wrong are common in depression. Depression creates feelings that nothing will ever improve. The risk of depression is increased when there is a family history. Interest in sex is markedly decreased in depression. 8. Answer A. The ability to use relaxation is basic to treatment of phobia. Clients with phobias are resistant to insight therapy. Riding the elevator accompanied by the nurse is an appropriate long-term goal. Role playing may be appropriate after the client has learned relaxation. 9. Answer C. This is an open-ended question which is nonjudgemental and allows for further discussion. The topic is also nonthreatening yet will give the nurse insight into the clients view of events leading up to admission. It is the only option that is client centered. The other options focus on the pills. 10. Answer D. Infant baptism is madatory in the Roman Catholic belief especially if a neonate is not expected to live. Anyone may perform this if an infant or child is gravely ill. Option A refers to the Christian Science belief. Option B is a belief of Russian Orthodoxy. Mormons believe of devine healing with the laying on of hands, as represented in option C. 11. Answer D. Victims develop a high tolerance for abuse. They blame themselves for being victimized. All members in the family suffer from the effects of abuse, even if they are not the actual victims. For these reasons, victims often have an extensive history of abuse and struggle for a long time before they can leave permanently. 12. Answer A. Giving broad opening statements and making observations are examples of therapeutic communication. The other options are too specific or focused to be therapeutic. 13. Answer C. Activity groups are used to enhance the therapeutic milieu and to meet the clinical and social needs of clients, e.g., to minimize withdrawal and regression, to develop self care skills, etc. 14. Answer D. This gradually engages the client in interactions with others and uses positive behavioral expectation. 15. Answer D. This type of identification band easily tracks the clients movements and ensures safety while wandering on the unit. 16. Answer C. This actions presents reality. 17. Answer D. Safety is a priority of care for the depressed client. Precautions to prevent suicide must be a part of the plan. 18. Answer B. When learning to manage stress, it is helpful to believe that one has the ability to control ones response to stress. It is impossible to avoid stress, which is a normal experience. Stress can be positive and growth enhancing as well as harmful. The belief that one has some control can minimize the stress response. 19. Answer C. Nonverbal, gentle touch is an important tool here. Providing appropriate forms of touch to reinforce caring feelings. Because tactile contacts vary considerably among individuals, families, and cultures, the nurse must be sensitive to the differences in attitudes and practices of clients and self. 20. Answer D. A dispositional crisis is a response to an external situational crisis. External anger at work is the dispositional crisis displaced to his wife through abuse. An anticipated life transition crisis is a crisis that is normal in the life cycle; transitional is one over which the person has no control. Developmental crisis occurs in response to triggering emotions related to unresolved conflict in ones life. This is called a developmental crisis based on Freudian psychology. Psychiatric emergency crisis is when the individuals general functioning has been severely impaired, and the individual has been rendered incompetent. PSYCHOSOCIAL INTEGRITY 1. a. b. c. d. 2. a. b. c. d. Nurse Rhea outcome criteria would be appropriate for a child diagnosed with oppositional defiant disorder? Accept responsibility for own behaviors Be able to verbalize own needs and assert rights Set firm and consistent limits with the client Allow the child to establish his own limits and boundaries The definition of nihilistic delusions is: A false belief about the functioning of the body Belief that the body is deformed or defective in a specific way False ideas about the self, others, or the world The inability to carry out motor activities
3. A client in an acute care setting tells nurse Gio, I dont think I can face going home tomorrow. The nurse replies, Do you want to talk more about it? The nurse is using which of the following techniques? a. Presenting reality b. Making observations
c. Restating d. Exploring 4. a. b. c. d. Nurse Ritchel is leading group therapy with psychiatric clients. During the working phase, what should the nurse do? Explain the purposes and goals of the group Offer advice to help resolve conflicts Encourage group cohesiveness Encourage a discussion of feelings of loss regarding termination of the group
5. A 20-year-old females pregnancy is confirmed at a clinic. She says her husband will be excited but is concerned because she herself isnt excited. She fears this may mean shell be a bad mother. Nurse Linda should respond by: a. Referring her to counseling b. Telling her such feelings are normal in the beginning of pregnancy c. Exploring her feelings d. Recommending she talk her feelings over with her husband 6. a. b. c. d. A male client is admitted with a diagnosis of schizotypal personality disorder. Which signs would this client exhibit during social situations? Aggressive behavior Paranoid thoughts Emotional affect Independence needs
7. During a group therapy session in the psychiatric unit, a client constantly interrupts with impulsive behavior and exaggerated stories that cast her as a hero or princess. She also manipulates the group with attention-seeking behaviors, such as sexual comments and angry outbursts. Nurse Lindsay realizes that these behaviors are typical of: a. Paranoid personality disorder b. Avoidant personality disorder c. Histrionic personality disorder d. Borderline personality disorder 8. A female client undergoes a total laryngectomy and tracheostomy formation. On discharge, nurse Aimee should give which instruction to the client and family? a. Clean the tracheostomy tube with alcohol and water. b. Family members should continue to talk to the client. c. Oral intake of fluids should be limited for 1 week only. d. Limit the amount of protein in the diet. 9. An 16-year-old boy is admitted to the facility after acting out his aggressions inappropriately at school. Predisposing factors to the expression of aggression include: a. Violence on television b. Passive parents c. An internal locus of control d. A single-parent family 10. a. b. c. d. Nurse Kim is working with a client who abuses alcohol. Which of the following facts should the nurse communicate to the client? Abstinence is the basis for successful treatment Attendance at Alcoholics Anonymous meetings every day will cure alcoholism For treatment to be successful, family members must participate An occasional social drink is acceptable behavior for the alcoholic
11. A man at a pizza parlor verbally confronts the waiter for lack of attentiveness. Later, in the back room, the waiter spits on the mans pizza. This is an example of a behavior typical of which disorder? a. Obsessive-compulsive b. Narcissistic c. Passive-aggressive d. Dependent 12. a. b. c. d. Which of the following groups of characteristics would nurse Tracy expect to see in the client with schizophrenia? Loose associations, grandiose delusions, and auditory hallucinations Periods of hyperactivity and irritability alternating with depression Delusions of jealousy and persecution, paranoia, and mistrust Sadness, apathy, feelings of worthlessness, anorexia, and weight loss
13. A client has approached nurse Joyce asking for advice on how to deal with his alcohol addiction. The nurse should tell the client that the only effective treatment for alcoholism is: a. Psychotherapy b. Total abstinence c. Alcoholics Anonymous (AA) d. Aversion therapy 14. While looking out the window, a client with schizophrenia remarks, That school across the street has creatures in it that are waiting for me. Which of the following terms best describes what the creatures represent? a. Anxiety attack b. Projection c. Hallucination d. Delusion 15. a. b. c. d. Nurse Vince is trying to establish rapport with a newly admitted client. Which technique blocks effective communication with a client? Using silence Asking open-ended questions Giving advice Reflecting
16. The parents of a 2 year old child arrive at a hospital to visit their child. The child is in the playroom when the parents arrive. When the parents enter the playroom, the child does not readily approach the parents. Nurse Rey interprets this behavior as indicating that: a. The child is withdrawn b. This is a normal pattern c. The child is self-centered d. The child has adjusted to the hospital setting 17. Nurse Danny is preparing a plan of care for a client who is a Jehovahs Witness. The client has been told that surgery is necessary. The nurse considers the clients religious preferences in developing the plan of care and documents that: a. Faith healing is practiced primarily b. Medication administration is not allowed c. Surgery is prohibited in this religious group d. The administration of blood and blood products is forbidden 18. Lou, a home care nurse is visiting an older female client whose husband died 6 months ago. Which behavior by the client indicates ineffective coping? a. Neglecting her personal grooming b. Looking at old snapshots of her family c. Participating in a senior citizens program d. Visiting her husbands grave once a month 19. Wendy, an ambulatory care nurse is discussing preoperative procedures with a Chinese-American client who is scheduled for surgery the following week. During the discussion, the client continually smiles and nods the head. The nurse interprets this nonverbal behavior as: a. Reflecting a cultural value b. An acceptance of the treatment c. The client is agreeable to the required procedures d. The client understands the preoperative procedures 20. Faith, A hospice nurse visits a client dying of ovarian cancer. During the visit, the client expresses that If I can just live long enough to attend my daughters graduation, Ill be ready to die. Which phase of coping is this client experiencing? a. Anger b. Denial c. Bargaining d. Depression 21. Lester, a nursing student is discussing cultural diversity issues in a clinical conference when a nursing instructor asks the student to describe ethnocentrism. Which statement by the student indicates a lack of understanding of the issue of ethnocentrism? a. It is a tendency to view ones own ways as best. b. It is acting in a manner that is superior to other cultures. c. It is imposing ones beliefs on individuals from another culture. d. It is believing that ones own way is the only acceptable way.
22. a. b. c. d.
A male client who has developed severe pulmonary edema would most likely exhibit which of the following? Mild anxiety Slight anxiety Extreme anxiety Moderate anxiety
23. Karen, a nurse educator asks a student to list the five categories of complementary and alternative medicine (CAM), developed by the National Center for Complementary and Alternative Medicine (NCCAM), to a group of nursing students. Which of the following, if stated by the nursing student, would indicate an understanding of the five categories of CAM? a. Herbology, hydrotherapy, acupuncture, nutrition, and chiropractic care b. Mind-body medicine, traditional Chinese medicine, homeopathy, naturopathy, and healing touch c. Biologically based practices, body-based practices, magnetic therapy, massage therapy, and Trager body work d. Whole medical systems, mind-body medicine, biologically based practices, manipulative and body-based practices, and energy medicine 24. Nurse Gretchen is bathing a hospitalized Native American client of the Navajo culture and notes that the client avoids eye contact during the procedure. The nurse makes which interpretation about the clients behavior? a. The client is depressed b. The client is displaying disrespectful mannerisms c. The client is displaying behavior that is a common cultural action d. The client is humiliated because of the cared for by someone else. 25. Claudine, a nurse educator is providing in-service education to the nursing staff regarding trans-cultural nursing care when a staff member asks the nurse educator to describe the concept of acculturation. The appropriate response is which of the following? a. It is a subjective perspective of the persons heritage and a sense of belonging to a group. b. It is a group of individuals in a society who are culturally distinct and have a unique identity. c. It is a process of learning a different culture to adapt to a new of changing environment. d. It is a group that shares some of the characteristics of the larger population group of which it is a part. ANSWER AND RATIONALE 1. A. Children with oppositional defiant disorder frequently violate the rights of others. They are defiant, disobedient, and blame others for their actions. Accountability for their actions would demonstrate progress for the oppositional child. Options C and D arent outcome criteria but interventions. Option B is incorrect as the oppositional child usually focuses on his own needs. 2. C. Nihilistic delusions are false ideas about the self, others, or the world. Somatic delusions involve a false belief about the functioning of the body. Body dysmorphic disorder is characterized by a belief that the body is deformed or defective in a specific way. Apraxia is the inability to carry out motor activities. 3. D. The nurse is using the technique of exploring because shes willing to delve further into the clients concern. She isnt presenting reality or making observations or simply restating. The nurse is encouraging the client to explore his feelings. 4. C. During the working phase, or the middle phase of a group, the nurse continues to encourage cohesiveness among its members. During the orientation phase, or the initial phase, the nurse leading the group should explain the purpose and goals of the group. During the termination phase, or the final phase, the leader encourages a discussion of feelings associated with termination. When leading a group, the nurse should act as a facilitator; offering advice isnt appropriate. The group members should work together to resolve conflicts. 5. B. Misgivings and fears are common in the beginning of pregnancy. It doesnt necessarily mean that she requires counseling at this time. Exploring her feelings may help her understand her concerns more deeply but wont provide reassurance that her feelings are normal. She may benefit by discussing her feelings with her husband, but the husband also needs to be reassured that these feelings are normal at this time. 6. B. Clients with schizotypal personality disorder experience excessive social anxiety that can lead to paranoid thoughts. Aggressive behavior is uncommon, although these clients may experience agitation with anxiety. Their behavior is emotionally cold with a flattened affect, regardless of the situation. These clients demonstrate a reduced capacity for close or dependent relationships. 7. C. This clients behaviors are typical of histrionic personality disorder, which is marked by excessive emotionality and attention seeking. The client constantly seeks and demands attention, approval, or praise; may be seductive in behavior, appearance, or conversation; and is uncomfortable except when she is the center of attention. Typically, a client with paranoid personality disorder is suspicious, cold, hostile, and argumentative. Avoidant personality disorder is characterized by anxiety, fear, and social isolation. Borderline personality disorder is characterized by impulsive, unpredictable behavior and unstable, intense interpersonal relationships. 8. B. Commonly, family members are reluctant to talk to a client who has had a total laryngectomy and can no longer speak. To promote a supportive environment, the nurse should encourage family members to continue normal communication. The nurse should teach the client to clean the tracheostomy tube with hydrogen peroxide and rinse it with sterile saline solution, to consume oral fluids as desired, and to eat protein-rich foods to promote healing. 9. A. Violence on television has been correlated with an increase in aggressive behavior. Passive parents contribute to acting-out behaviors but not specifically to violence. An internal locus of control leads to a positive sense of self-esteem and isnt related to violence or aggression. There is no direct correlation between single-parent families and violence. 10. A. The foundation of any treatment for alcoholism is abstinence. Attendance at Alcoholics Anonymous is helpful to some individuals to maintain strict abstinence. Participation in treatment by the family is beneficial to both the client and the family but isnt essential. Abstinence requires refraining from social drinking. 11. C. This is an example of a negative attitude and passive-agressive behavior to word demands for adequate performance. People with this
disorder wont confront or discuss issues with others but will go to great lengths to "get even." Obsessive-compulsive disorder involves rituals or rules that interfere with normal functioning. A person with a narcissistic personality has an exaggerated sense of self-worth. A person with a dependent personality is submissive and frequently apologizes and backs down when confronted. 12. A. Loose associations, grandiose delusions, and auditory hallucinations are all characteristic of the classic schizophrenic client. These clients arent able to care for their physical appearance. They frequently hear voices telling them to do something either to themselves or to others. Additionally, they verbally ramble from one topic to the next. Periods of hyperactivity and irritability alternating with depression are characteristic of bipolar or manic disease. Delusions of jealousy and persecution, paranoia, and mistrust are characteristics of paranoid disorders. Sadness, apathy, feelings of worthlessness, anorexia, and weight loss are characteristics of depression. 13. B. Total abstinence is the only effective treatment for alcoholism. Psychotherapy, attendance at AA meetings, and aversion therapy are all adjunctive therapies that can support the client in his efforts to abstain. 14. D. A delusion is a false belief based on a misrepresentation of a real event or experience. Although anxiety can increase delusional responses, it isnt considered the primary symptom. Projection is falsely attributing to another person ones own unacceptable feelings. Hallucinations, which characterize most psychoses, are perceptual disorders of the five senses; the client may see, taste, feel, smell, or hear something in the absence of external stimulation. 15. C. Giving advice blocks rather than promotes effective communication with a client. The other options promote effective communication. 16. B. The phases through which young children progress when separated from their parents include protest, despair, and denial or detachment. 17. D. Among Jehovahs Witnesses, surgery is not prohibited, but the administration of blood and blood products is forbidden. Faith healing is forbidden in this religious group. Administration of medication is an acceptable practice, except if the medication is derived from blood products. 18. A. Coping mechanisms are behavior used to decrease stress and anxiety. In response to a death, ineffective coping is manifested by an extremem behavior that in some cases may be harmful to the individual physically or psychologically. 19. A. Nodding or smiling by a Chinese-American client may reflect only the cultural value of interpersonal harmony. This nonverbal behavior may not be an indication of agreement with the speaker, an acceptance of the treatment, or an understanding of the procedure. 20. C. Bargaining identifies a behavior in which the individual is willing to do anything to avoid loss or change prognosis or fate. 21. C. Ethnocentrism is a tendency to view ones own way of life as the most desirable, acceptable, or best and to act in a superior manner toward another culture. Cultural imposition is the tendency to impose ones own beliefs, values, and patterns of behavior on individuals from another culture. 22. C. Pulmonary edema causes the client to be extremely agitated and anxious. The client may complain of a sense of drowning, suffocation, or something. 23. D. The five categories of complementary and alternative medicine (CAM) include whole medical systems, mind-body medicine, biologically based practices, manipulative and body-based practices, and energy medicine. The other options contain therapies within each category of CAM. 24. C. Native American clients often avoid eye contact when being cared for by health care personnel. In this culture, eye contact is considered a sign of disrespect. Therefore, this clients action is culturally appropriate behavior. Options A, B, and D are inappropriate interpretations of the clients behavior. 25. C. Acculturation is a process of learning a different culture to adapt to a new or changing environment. Option A describes ethnic identity. Option B describes an ethnic group. Option D describes a subculture.
You might also like
- Mark Fredderick R. Abejo RN, MAN: Maternal and Child Nursing BulletsDocument10 pagesMark Fredderick R. Abejo RN, MAN: Maternal and Child Nursing BulletsMark DaenosNo ratings yet
- Obstetric Nursing Human Sexuality SexualityDocument30 pagesObstetric Nursing Human Sexuality SexualityKim RamosNo ratings yet
- NCLEX Neurology Practice TestDocument6 pagesNCLEX Neurology Practice Testojoj2206No ratings yet
- Test Maternal and PediaDocument11 pagesTest Maternal and PediaDefensor Pison GringgoNo ratings yet
- Muscles and Muscle Tissue: Muscle Overview Muscle SimilaritiesDocument11 pagesMuscles and Muscle Tissue: Muscle Overview Muscle SimilaritiesHerne BalberdeNo ratings yet
- IntegumentaryDocument8 pagesIntegumentaryRamon Carlo AlmiranezNo ratings yet
- Head to-Toe-Assessment Complete Guide - Nightingale CollegeDocument1 pageHead to-Toe-Assessment Complete Guide - Nightingale CollegeDabon RusselNo ratings yet
- Nursing MnemonicsDocument2 pagesNursing MnemonicsJamie ElizabethNo ratings yet
- MCNDocument69 pagesMCNGem M. Mah0% (1)
- ODB Documentation NLE PDFDocument2 pagesODB Documentation NLE PDFElizabella Henrietta TanaquilNo ratings yet
- Distinction College - Final ExamDocument15 pagesDistinction College - Final Examannieciaamara16No ratings yet
- Our Daily Bread - LEOPOLDDocument4 pagesOur Daily Bread - LEOPOLDJonas Marvin AnaqueNo ratings yet
- Chapter 09 - Visual and Auditory ProblemsDocument7 pagesChapter 09 - Visual and Auditory ProblemscariNo ratings yet
- Maternal (Well-Client) : Framework of Maternal and Child CareDocument3 pagesMaternal (Well-Client) : Framework of Maternal and Child CarealallaallalaNo ratings yet
- Fundamentals of Nursing NCLEX Practice Quiz 2 (30 Items) : About Privacy Disclaimer ContactDocument26 pagesFundamentals of Nursing NCLEX Practice Quiz 2 (30 Items) : About Privacy Disclaimer ContactAkia Cayasan BayaNo ratings yet
- Pediatric Nursing CA Sir Archie Alviz 04-09-2022Document3 pagesPediatric Nursing CA Sir Archie Alviz 04-09-2022Jonah MaasinNo ratings yet
- Question A Ire NursingDocument49 pagesQuestion A Ire NursingNosreffej MonarcaNo ratings yet
- Maternal and Child Health Nursing NCLEX Questions Part 1Document9 pagesMaternal and Child Health Nursing NCLEX Questions Part 1Trisha ArizalaNo ratings yet
- Cancer Types, Causes, Symptoms & TreatmentDocument169 pagesCancer Types, Causes, Symptoms & TreatmentDardarConstantinoNo ratings yet
- Maternal Board Anticipated Close Door Coaching Nle Nov 2023Document10 pagesMaternal Board Anticipated Close Door Coaching Nle Nov 2023Sophian D. DalumaNo ratings yet
- Integrated Management of Childhood IllnessesDocument65 pagesIntegrated Management of Childhood IllnessesJocel LañasNo ratings yet
- Astigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedDocument12 pagesAstigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedLynden BulanNo ratings yet
- University of Luzon College of Nursing Ns-Ii2 P Oxygenation ProblemsDocument10 pagesUniversity of Luzon College of Nursing Ns-Ii2 P Oxygenation ProblemsAhmad BaolayyanNo ratings yet
- Medical-Surgical Nursing Exam: Burns (40 QuestionsDocument5 pagesMedical-Surgical Nursing Exam: Burns (40 QuestionscatneskaNo ratings yet
- Cardiac Practice TestDocument7 pagesCardiac Practice TestroseNo ratings yet
- Chapter - 001 Health Promotion in Middle-Aged AdultsDocument10 pagesChapter - 001 Health Promotion in Middle-Aged AdultsTrixie AlvarezNo ratings yet
- NCM 102 Lec RespiDocument26 pagesNCM 102 Lec RespiLindsay NateNo ratings yet
- What is Fetal Alcohol Syndrome in 38 charactersDocument2 pagesWhat is Fetal Alcohol Syndrome in 38 charactersKrystal Cowley Miller100% (1)
- English ReviewDocument8 pagesEnglish ReviewC SmithNo ratings yet
- Drainage normal after sigmoid colostomyDocument35 pagesDrainage normal after sigmoid colostomyJackie AbarraNo ratings yet
- Home Care and The Childbearing and Childrearing Family Home Care and The Childbearing and Childrearing FamilyDocument20 pagesHome Care and The Childbearing and Childrearing Family Home Care and The Childbearing and Childrearing FamilyBridget Shienne DaculaNo ratings yet
- Pediatric NursingDocument4 pagesPediatric Nursingjustjesko0lNo ratings yet
- Maternal and Child NursingDocument31 pagesMaternal and Child Nursingasdfghjkl100% (1)
- Quiz answers with feedback on nursing questionsDocument7 pagesQuiz answers with feedback on nursing questionsArlene FerrerNo ratings yet
- Vital SignsDocument13 pagesVital SignsMarcus, RN100% (3)
- Impact of Family Environment On Socio-Emotional Adjustment of Adolescent Girls in Rural Areas of Western OdishaDocument9 pagesImpact of Family Environment On Socio-Emotional Adjustment of Adolescent Girls in Rural Areas of Western OdishaDr. Manoranjan Tripathy100% (1)
- Test Taking Strategies for Nursing ExamsDocument104 pagesTest Taking Strategies for Nursing ExamsPaul Lexus Gomez LorenzoNo ratings yet
- Medical Colleges of Northern Philippines Clinical Practicum ExamDocument4 pagesMedical Colleges of Northern Philippines Clinical Practicum ExamKaren Mae Santiago AlcantaraNo ratings yet
- SIR BORNIE E E N T POST TEST EditedDocument12 pagesSIR BORNIE E E N T POST TEST EditedHarvey T. Dato-onNo ratings yet
- References: NCSBN's Review For The NCLEX-PN ExaminationDocument5 pagesReferences: NCSBN's Review For The NCLEX-PN Examinationbapimirab6540% (1)
- Maternal and Child Nursing Module 1: Obstetric Nursing OverviewDocument18 pagesMaternal and Child Nursing Module 1: Obstetric Nursing Overviewjanina myka100% (1)
- Pediatric Nursing Edited)Document1 pagePediatric Nursing Edited)Dominique RamosNo ratings yet
- OB Review QuestionsDocument15 pagesOB Review QuestionsDarlene HuynhNo ratings yet
- Neurocardio NursingDocument101 pagesNeurocardio NursingMatt Lao DionelaNo ratings yet
- Maternal and Child Preboard Answer KeyDocument11 pagesMaternal and Child Preboard Answer KeyMichelle Gambol100% (1)
- Periop 8Document18 pagesPeriop 8Bern GervacioNo ratings yet
- Pediatric Nursing Student HandoutsDocument17 pagesPediatric Nursing Student HandoutsPaulAliboghaNo ratings yet
- Pedia SlidesDocument26 pagesPedia SlidesCharles Gerard B. BeluanNo ratings yet
- Integratedhealt 150201183122 Conversion Gate02 PDFDocument145 pagesIntegratedhealt 150201183122 Conversion Gate02 PDFVhince PiscoNo ratings yet
- Community Health NursingDocument23 pagesCommunity Health NursingMimi Vee100% (1)
- Chapter 17 The Breasts and AxillaeDocument4 pagesChapter 17 The Breasts and AxillaeKhanh HoangNo ratings yet
- Maternal ExamDocument52 pagesMaternal ExamRandyNo ratings yet
- Obstetrics and GynecologyDocument36 pagesObstetrics and GynecologyLeiNo ratings yet
- Psychiatric Nursing 1Document11 pagesPsychiatric Nursing 1api-3731845100% (1)
- My Reviewer On Funda Epaphras Joel T. MilitarDocument82 pagesMy Reviewer On Funda Epaphras Joel T. MilitarEpaphras Joel MilitarNo ratings yet
- BulletsDocument14 pagesBulletsstuffednurseNo ratings yet
- NP1Document32 pagesNP1Louie Anne Cardines Angulo100% (1)
- Methyldopa Drug DataDocument3 pagesMethyldopa Drug DataLaurel Joshua Reyes DauzNo ratings yet
- Varicella Zoster VirusDocument11 pagesVaricella Zoster VirusJayaram SNo ratings yet
- Module 1Document3 pagesModule 1Anonymous jhhtrnfNo ratings yet
- Charles LawDocument12 pagesCharles LawLerr Real RelleNo ratings yet
- November 2017 (v1) QP - Paper 4 CIE Chemistry IGCSEDocument16 pagesNovember 2017 (v1) QP - Paper 4 CIE Chemistry IGCSEGhulam Mehar Ali ShahNo ratings yet
- Bladder StonesDocument20 pagesBladder StonesRiean AuliaNo ratings yet
- ANGLICISMSDocument14 pagesANGLICISMSManuel Jorquera100% (1)
- Soil Formation - Print - Quizizz 1Document5 pagesSoil Formation - Print - Quizizz 1Gabriella HartleyNo ratings yet
- Laboratory Notebook: Aquatic Ecology and ResourcesDocument7 pagesLaboratory Notebook: Aquatic Ecology and ResourcesAireen Diamsim MaltoNo ratings yet
- Schools Division of Roxas CityDocument4 pagesSchools Division of Roxas CityHuge Propalde EstolanoNo ratings yet
- Autorefractometro GRK 7000Document82 pagesAutorefractometro GRK 7000Wilson CepedaNo ratings yet
- Role of Victims in Commission of CrimeDocument16 pagesRole of Victims in Commission of CrimeBEST OF ONE PIECENo ratings yet
- Menstrual Hygiene PDFDocument8 pagesMenstrual Hygiene PDFFarha AamirNo ratings yet
- Elo TecDocument2 pagesElo TecMimi MimiNo ratings yet
- PH 611: CO2 Release in RespirationDocument2 pagesPH 611: CO2 Release in RespirationAcuCJamNo ratings yet
- CareerAssessments-Emotional Control-2023-05-02Document2 pagesCareerAssessments-Emotional Control-2023-05-02Kaumadee WeerasingheNo ratings yet
- The Basics of Profit Planning for Your Small BusinessDocument1 pageThe Basics of Profit Planning for Your Small BusinessRodj Eli Mikael Viernes-IncognitoNo ratings yet
- Clerking Sheet 1Document8 pagesClerking Sheet 1Precious ChaiNo ratings yet
- Indian Economy On The Eve of IndependenceDocument5 pagesIndian Economy On The Eve of IndependenceAshiga RajendaranNo ratings yet
- A tribute to my mother's handsDocument3 pagesA tribute to my mother's handsAnonymous qAegy6GNo ratings yet
- (Vikhroli West) : Raj LegacyDocument4 pages(Vikhroli West) : Raj LegacyNEHA NNo ratings yet
- Rabor vs CSC - Retirement age extension disputeDocument2 pagesRabor vs CSC - Retirement age extension disputeGladys Bustria OrlinoNo ratings yet
- 3G3EV Installation ManualDocument55 pages3G3EV Installation ManualHajrudin SinanovićNo ratings yet
- RRL - Airbag SystemDocument3 pagesRRL - Airbag Systemclarice fNo ratings yet
- Elastosil® M 4642 A/B: Product DescriptionDocument2 pagesElastosil® M 4642 A/B: Product DescriptionhemantrulzNo ratings yet
- Power Quality SolutionDocument40 pagesPower Quality Solutionshankar ammantryNo ratings yet
- Child Development: Resilience & Risk, A Course SyllabusDocument17 pagesChild Development: Resilience & Risk, A Course SyllabusJane GilgunNo ratings yet
- Presented By: Bhagyashree KaleDocument58 pagesPresented By: Bhagyashree KaleSupriya JajnurkarNo ratings yet
- Nadilla Choerunnisa 2B S.KepDocument3 pagesNadilla Choerunnisa 2B S.KepNadilla ChoerunnisaNo ratings yet
- Filipino Street FoodsDocument5 pagesFilipino Street FoodsMs. 37o?sANo ratings yet