Professional Documents
Culture Documents
CHD With NCP
Uploaded by
Johanna Kirsten F. DaguioOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CHD With NCP
Uploaded by
Johanna Kirsten F. DaguioCopyright:
Available Formats
Coronary heart disease
Coronary heart disease (CHD) is a narrowing of the small blood vessels that supply blood and oxygen to the heart. CHD is also called coronary artery disease. Causes Coronary heart disease (CHD) is the leading cause of death in the United States for men and women. Coronary heart disease is caused by the buildup of plaque in the arteries to your heart. This may also be called hardening of the arteries. Fatty material and other substances form a plaque build-up on the walls of your coronary arteries. The coronary arteries bring blood and oxygen to your heart. This build up causes the arteries to get narrow. As a result, blood flow to the heart can slow down or stop.
A risk factor for heart disease is something that increases your chance of getting it. You cannot change some risk factors for heart disease, but others you can change. The risk factors for heart disease that you CANNOT change are: Your age. The risk of heart disease increases with age. Your gender. Men have a higher risk of getting heart disease than women who are still getting their menstrual period. After menopause, the risk for women is closer to the risk for men. See: Heart disease and women Your genes. If your parents or other close relatives had heart disease, you are at higher risk. Your race. African Americans, Mexican Americans, American Indians, Hawaiians, and some Asian Americans also have a higher risk for heart problems.
Many things increase your risk for heart disease: Diabetes is a strong risk factor for heart disease. High blood pressure increases your risks of heart disease and heart failure. Extra cholesterol in your blood builds up inside the walls of your heart's arteries (blood vessels). Smokers have a much higher risk of heart disease. Chronic kidney disease can increase your risk. People with narrowed arteries in another part of the body (examples are stroke and poor blood flow to the legs) are more likely to have heart disease. Substance abuse (such as cocaine) Being overweight Not getting enough exercise, and feeling depressed or having excess stress are other risk factors.
Symptoms Symptoms may be very noticeable, but sometimes you can have the disease and not have any symptoms. Chest pain or discomfort (angina) is the most common symptom. You feel this pain when the heart is not getting enough blood or oxygen. How bad the pain is varies from person to person. It may feel heavy or like someone is squeezing your heart. You feel it under your breast bone (sternum), but also in your neck, arms, stomach, or upper back. The pain usually occurs with activity or emotion, and goes away with rest or a medicine called nitroglycerin. Other symptoms include shortness of breath and fatigue with activity (exertion).
Women, elderly people, and people with diabetes are more likely to have symptoms other than chest pain, such as: Fatigue Shortness of breath Weakness
See: Heart failure for symptoms of heart failure Exams and Tests Many tests help diagnose CHD. Usually, your doctor will order more than one test before making a diagnosis. Tests may include: Coronary angiography/arteriography -- an invasive test that evaluates the heart arteries under xray CT angiography -- a non invasive way to perform coronary angiography Echocardiogram Electrocardiogram (ECG) Electron-beam computed tomography (EBCT) to look for calcium in the lining of the arteries -- the more calcium, the higher your chance for CHD Exercise stress test Heart CT scan Magnetic resonance angiography Nuclear stress test
Treatment You may be asked to take one or more medicines to treat blood pressure, diabetes, or high cholesterol levels. Follow your doctor's directions closely to help prevent coronary artery disease from getting worse. Goals for treating these conditions in people who have coronary artery disease:
Blood pressure less than or equal to 140/90 (even lower for some patients with diabetes, kidney disease, or heart failure) Glycosylated hemoglobin (HbA1c) levels less than or equal to 7% for people with diabetes LDL cholesterol level less than or equal to 100 mg/dL (even lower for some patients)
Treatment depends on your symptoms and how severe the disease is. Your doctor may give you one or more medicines to treat CHD, including: ACE inhibitors to lower blood pressure and protect your heart and kidneys Aspirin, with or without clopidogrel (Plavix) or prasugrel (Effient) to help prevent blood clots from forming in your arteries Beta-blockers to lower heart rate, blood pressure, and oxygen use by the heart Calcium channel blockers to relax arteries, lower blood pressure, and reduce strain on the heart Diuretics ("water pills") to lower blood pressure and treat heart failure Nitrates (such as nitroglycerin) to stop chest pain and improve blood flow to the heart Statins to lower cholesterol
NEVER ABRUPTLY STOP TAKING ANY OF THESE DRUGS. Always talk to your doctor first. Stopping these drugs suddenly can make your angina worse or cause a heart attack. Your doctor may refer you to a cardiac rehabilitation program to help improve your heart's fitness. Procedures and surgeries used to treat CHD include: Angioplasty and stent placement, called percutaneous coronary interventions (PCIs) Coronary artery bypass surgery Minimally invasive heart surgery
LIVE A HEALTHY LIFESTYLE Some of the risks for heart disease that you CAN change are: Do not smoke or use tobacco. Get plenty of exercise, at least 30 minutes a day on at least 5 days a week (talk to your doctor first). Maintain a healthy weight. Men and women should aim for a body mass index (BMI) between 18.5 and 24.9. Get checked and treated for depression. Women who are at high risk for heart disease should take omega-3 fatty acid supplements. If you drink alcohol, limit yourself to no more than one drink per day for women, and no more than two drinks per day for men.
Nutrition is important to your heart health, and it will help control some of your heart disease risk factors. See also: Heart disease and diet Choose a diet rich in fruits, vegetables, and whole grains.
Choose lean proteins, such as chicken, fish, beans, and legumes. Eat low-fat dairy products, such as 1% milk and low-fat yogurt. Avoid sodium (salt) and fats found in fried foods, processed foods, and baked goods. Eat fewer animal products that contain cheese, cream, or eggs. Read labels, and stay away from "saturated fat" and anything that contains "partiallyhydrogenated" or "hydrogenated" fats. These products are usually loaded with unhealthy fats.
Outlook (Prognosis) Everyone recovers differently. Some people can maintain a healthy life by changing their diet, stopping smoking, and taking medications exactly as the doctor prescribes. Others may need medical procedures such as angioplasty or surgery. Although everyone is different, early detection of CHD generally results in a better outcome. When to Contact a Medical Professional If you have any risk factors for CHD, contact your doctor to discuss prevention and possible treatment. Immediately contact your health care provider, call the local emergency number (such as 911), or go to the emergency room if you have: Angina or chest pain Shortness of breath Symptoms of a heart attack
Alternative Names Coronary artery disease; Arteriosclerotic heart disease; CHD; CAD
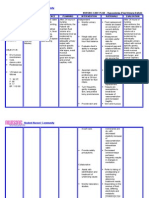
Decreased Cardiac Output
Cad causes narrowing of blood vessels. This condition leads to intense pressure exerted on the walls of the blood vessels. The bodys compensatory mechanism is to increase the work load of the heart and thus the patient has decreased cardiac output.
Assessment
Nursing Scientific diagnosis explanation Decreased cardiac output r/t increased vascular resistance
Planning
Nursing Rationale interventions
Expected outcome
S=
O= The patient may manifest: >restlessness >increased bp > cold clammy skin >decreased peripheral pulses
Cad causes > assess Short term: narrowing of patients blood vessels. After 2-3 condition hours of This condition nursing leads to intense interventions, > monitor and record pressure the patient vital signs exerted on the will verbalize walls of the understanding > encourage blood vessels. of disease patient to process. The bodys verbalize
shall have > for baseline verbalized data Understanding of disease > to make client express process. his feelings Long term: concerns > to improve Compensatory Long term: venous return The patient mechanism is shall have > encourage to increase the After two patient to > to reduce participated in work load of days of activities to change stress the heart and nursing decrease in the position thus the interventions every two > to divert hearts patient has the patient hours attention and workload decreased will help patient cardiac output. participate in > encourage lessen activities to patient to do experienced decrease in relaxation pain and the hearts techniques anxiety workload > encourage patient to engage in divertional activities such as chatting with family and friends. > reinforced > to prevent further complications of the disease
> to determine Short term: possible The patient problems
low salt and low fat diet
Ineffective Tissue Perfusion
Assessment Nursing diagnosis Ineffective tissue O> the perfusion patient r/t manifested decreased the following: cardiac output S> o Scientific explanation Objectives Nursing Rationale interventions Expected outcome
>shortness of breath >fatigue The pt. May manifest: > pallor > cool temperature > decrease pulse > decrease urine output
The oxygen Short term: >assess pt.s >to have baseline Short term: content of condition. data. After 3 The pt. Shall arterial blood hours of ni, >monitor and >to have have is almost all the pt. Will record v/s. baseline data demonstrated bound to hgb. be able to behaviors on and this are In anemia, the demonstrate >note color usually altered how to have oxygen behaviors on and in the condition. effective content will how to have temperature airways. therefore fall effective of the skin. >cool, pale skin airways. in proportion is indicative of Long term: decrease >monitor to the Long term: peripheral peripheral tissue The patient reduction in shall be free perfusion. pulse. hgb After 1- 2 from concentration, days of ni, >provide a >decrease pulse shortness of even through the patient is indicative of breath. warmth the po2 is will free environment. decreased tissue normal. The from perfusion from normal shortness of >encourage vasoconstriction compensatory breath. active rom. of the vessels. to restore >a warm oxygen >monitor urine output. environment delivery is an promotes increase in vasodilation cardiac output.
which decreases preload and promotes tissue perfusion. >rom helps decreases venous pooling and promotes
tissue perfusion. >decreased tissue perfusion to the kidneys may result in oliguria.
Acute Pain
Assessment Nursing Scientific Objectives diagnosis explanation S> o Acute pain Nursing interventions Rationale Expected outcome
O> the pt. May manifest: > restlessness > pain scale of 9/10 > chest pain > irritability > (+) guarded behavior > (+) facial grimaces > crying > v/s change >
Coronary After 3 hours >assess pt.s >to have baseline The pt.s so artery of ni, the pt. condition. will verbalize data. disease Will verbalize understanding >monitor and >to have (CAD) is understanding of pts record v/s. baseline data caused by a of pts condition and and this are narrowing condition and usually altered health >assess pains of the health in the condition. teachings location and arteries that teachings given intensity/severity given to supply the to provide provide arising with. >to have heart comfort and baseline data for comfort and planning and muscle with relieve of pain. >provide relieve of pain interventions. and pt. Will comfort blood. measures like When the Long term demonstrate stretching of >to provide non- behavior of arteries After 2 days linens and narrow, being relieved of ni, the pt. assisting in pharmacological blood flow Will from pain and position. is reduced. demonstrate will be free Pain The reduced behavior of > provide management. from the blood flow being relieved diversional complications from pain and activities like causes the >to divert pt.s of the will be free having heart condition. attention. from the conversation w/ muscle to complications the pt. >to prevent receive less of the fatigue. oxygen then condition. >stress to pt the it needs to importance of >to reduce pain. function providing properly. adequate rest When
diaphoresis > sleep disturbance > increase rr and pulse
ischemia occurs patients typically develop angina or chest pain originating from the heart. It has been described as chest pain or discomfort that has a squeezing or pressurelike quality, usually felt behind the breastbone (sternum), but sometimes felt in the shoulders, arms, neck, jaws, or back.
period to the pt. >administer meds as ordered.
Activity Intolerance
Assessment Nursing diagnosis S= Activity Scientific Objectives explanation Interventions Rationale Outcomes
O= the patient may
Due to the Short term: > monitor disease and record intolerance condition, After 4 hours vital signs of nursing the patient
> for baseline data
Short term:
interventions > teach
> to
The patient shall have identified
manifest: r/t
lost te and health method to conserve and used teachings, increase energy techniques energy the patient activity to enhance general reserve will be able level > to reduce activity and has to use intolerance. fatigue weakness increased identified > plan care need to techniques to with rest Long term: > to adapt to enhance periods minimize the pain of activity between frustrations The patient angina. intolerance. activities shall have Because of participated > to Long term: > provide protect that she willingly in positive necessary from has limited atmosphere injury activities. movement. After 2-4 days of The nursing > assist with > to reduce inability to interventions, activities pain perform the patient activities of will be able > promote > to daily living to participate comfort minimize is also due willingly in measures pain to fatigue. necessary
activities.
> encourage participation and diversion of activities
Fatigue
Assessment Nursing Scientific Objectives diagnosi explanation s Short term: Interventions Rationale Outcomes
Fatigue Fatigue is an overwhelmin O= the patient g sense of may manifest: exhaustion resulting to > decreased verbalization capacity to of perform overwhelming S=
lack of
After 2 hours of nursing >determine >to enhances interventions, ability to commitment to the patient participate in promoting will be able to activities/leve optimal verbalize l of mobility. outcomes understanding of condition
> monitor vital > to provide signs baseline data
Short term:
The patient shall have verbalized understanding of condition and causative factors.
energy; >compromise d libido; >lethargic or listless > drowsiness > disinterest in surroundings >decreased performance >weight gain
activities at the usual level. This is due to the patients poor physical condition brought about by the disease condition.
and causative >establish >to maximize Long term: factors. realistic participation activity goals The patient Long term: with client >to encourage shall have patients performed adls and After 3 days >plan care to cooperation allow participate in of nursing desired interventions, individually > to adequate rest maintain/increas activities/leve the patient will be able to periods, e strength and l of activity. perform adls schedule muscle tone and activities for to enhance sense and participate in periods when of well-being. client has the desired activities/leve most energy >to lessen l of activity. fatigue >provide environment conducive >give medication as doctors ordered
You might also like
- Pathophysiology Diagram of Congestive Heart FailureDocument3 pagesPathophysiology Diagram of Congestive Heart FailureLeng Royo BrionesNo ratings yet
- NCP - Impaired Gas Exchange (COPD)Document3 pagesNCP - Impaired Gas Exchange (COPD)Karen Joy ItoNo ratings yet
- Case Study Ugib Lower MBDocument65 pagesCase Study Ugib Lower MBQuolette Constante100% (1)
- Hypovolemia Nursing Care PlanDocument2 pagesHypovolemia Nursing Care PlanLyn Reyes100% (1)
- NCP - Poststreptococcal GlomerulonephritisDocument12 pagesNCP - Poststreptococcal GlomerulonephritisAya BolinasNo ratings yet
- Risk For InfectionDocument1 pageRisk For InfectionEuanne OrellanoNo ratings yet
- CASE STUDY PheumoniaDocument5 pagesCASE STUDY PheumoniaEdelweiss Marie CayetanoNo ratings yet
- Abcess CellulitisDocument60 pagesAbcess CellulitisKirk Kevin PolanteNo ratings yet
- Deficient KnowledgeDocument3 pagesDeficient KnowledgeCamilleAnneRoseRabinoNo ratings yet
- X. Nursing Care Plan: ObjectiveDocument6 pagesX. Nursing Care Plan: ObjectiveRenea Joy ArruejoNo ratings yet
- Soapie Charting: Date/ Time/ ShiftDocument2 pagesSoapie Charting: Date/ Time/ Shiftspain michaelisNo ratings yet
- Managing Acute Renal PainDocument22 pagesManaging Acute Renal PainMaricris S. Sampang100% (1)
- NCP Knowledge Deficit PDFDocument2 pagesNCP Knowledge Deficit PDFskylertNo ratings yet
- NCP For DRDocument1 pageNCP For DRvalencia222No ratings yet
- DP Discharge Plan@@@@@@@@Document6 pagesDP Discharge Plan@@@@@@@@Maemae SumalinogNo ratings yet
- NCP PTBDocument2 pagesNCP PTBMack Jhed AnarconNo ratings yet
- Nursing Care Plan For Angina Pectoris NCPDocument2 pagesNursing Care Plan For Angina Pectoris NCPkarthi karthi100% (1)
- NCP AnxietyDocument1 pageNCP AnxietyUnang MagnayeNo ratings yet
- Risk For Fluid ImbalanceDocument8 pagesRisk For Fluid Imbalanceapi-277522722100% (1)
- Modified Radical MastectomyDocument6 pagesModified Radical Mastectomymetch isulatNo ratings yet
- Pain NCP BillrothDocument2 pagesPain NCP BillrotharjayNo ratings yet
- Calcium channel blocker and antacid drug studiesDocument28 pagesCalcium channel blocker and antacid drug studiessfkjalkhsafgNo ratings yet
- Family Nursing Care Plan for ConstipationDocument4 pagesFamily Nursing Care Plan for ConstipationErika CadawanNo ratings yet
- NCP and DrugsDocument13 pagesNCP and DrugsApRil ANn ChUa BingcangNo ratings yet
- NCP-Case Presentation (CHF)Document4 pagesNCP-Case Presentation (CHF)Jessamine EnriquezNo ratings yet
- Drug Study CADocument8 pagesDrug Study CAAna Marie Besa Battung-ZalunNo ratings yet
- Impaired Tissue PerfusionDocument2 pagesImpaired Tissue PerfusionLyka Mae Imbat - PacnisNo ratings yet
- NCP 1Document6 pagesNCP 1Maedine Urbano-BrionesNo ratings yet
- Diabetes InsipidusDocument48 pagesDiabetes InsipidusAhmed Fraz MamoonNo ratings yet
- NCP FeuDocument2 pagesNCP FeuFejlean Angelica AntineoNo ratings yet
- NCP For UTIDocument3 pagesNCP For UTIlachrymoseai100% (4)
- NCP Risk For InfectionDocument6 pagesNCP Risk For InfectionCazze SunioNo ratings yet
- DrugDocument3 pagesDrugPeace Andong PerochoNo ratings yet
- NCP CvaDocument7 pagesNCP CvaEmerson SilverioNo ratings yet
- ATRACURIUM BESYLATE - Atracurium Besylate Injection: Page 1 of 9Document9 pagesATRACURIUM BESYLATE - Atracurium Besylate Injection: Page 1 of 9chyntiaNo ratings yet
- NCP BronchopneumoniaDocument8 pagesNCP BronchopneumoniaCrisantaCasliNo ratings yet
- NCPDocument2 pagesNCPNichole Audrey SaavedraNo ratings yet
- Pathophysiology of Appendicitis: Causes and SymptomsDocument2 pagesPathophysiology of Appendicitis: Causes and SymptomsSherry Mae Rizza GonzalesNo ratings yet
- Drug StudyDocument13 pagesDrug StudylouiseordonoNo ratings yet
- NCP Inactivity ToleranceDocument16 pagesNCP Inactivity ToleranceChrisTine M. MoralesNo ratings yet
- CEPHALOSPORINSDocument18 pagesCEPHALOSPORINSVikas SharmaNo ratings yet
- Acute Confusion Nursing DiagnosisDocument4 pagesAcute Confusion Nursing Diagnosisasmika danaNo ratings yet
- NCP of CavDocument3 pagesNCP of CavHenry Roque TagalagNo ratings yet
- ER equipments & drugsDocument3 pagesER equipments & drugsApple LlanesNo ratings yet
- NCP LeukemiaDocument5 pagesNCP LeukemiaTriciaNo ratings yet
- Fdar Psyche 3Document1 pageFdar Psyche 3Aziil LiizaNo ratings yet
- UoB Nursing Students' Case Study on Normal Spontaneous Vaginal DeliveryDocument21 pagesUoB Nursing Students' Case Study on Normal Spontaneous Vaginal DeliveryJaysellePuguonTabijeNo ratings yet
- NCP AgnDocument2 pagesNCP Agnj3nann3No ratings yet
- Pathophysiology of Diabetes MellitusDocument2 pagesPathophysiology of Diabetes MellitusShelly_Ann_Del_9959No ratings yet
- Activity IntoleranceDocument2 pagesActivity IntoleranceDiane AbanillaNo ratings yet
- Hemothorax HandoutsDocument2 pagesHemothorax HandoutsJunathan L. DelgadoNo ratings yet
- NCP 2 QiDocument3 pagesNCP 2 QiKarlo Tuazon SedigoNo ratings yet
- NCP For Impaired Oral Mucous MembraneDocument11 pagesNCP For Impaired Oral Mucous MembraneRYAN SAPLADNo ratings yet
- NCP UreteroDocument1 pageNCP UreteroCerie Anne OlayNo ratings yet
- ASSESSMENT EXPLANATION OF THE OBJECTIVES NURSING INTERVENTIONS RATIONALE EVALUATIONDocument5 pagesASSESSMENT EXPLANATION OF THE OBJECTIVES NURSING INTERVENTIONS RATIONALE EVALUATIONRussel SantosNo ratings yet
- Bhs Inggrs TransletDocument6 pagesBhs Inggrs TransletArif AshariNo ratings yet
- Coronary Heart DiseaseDocument13 pagesCoronary Heart DiseaseLea Recto VinuyaNo ratings yet
- Biology ProjectDocument13 pagesBiology ProjectFelicia Charles0% (1)
- Heart Attack Risk Factors and Symptoms ExplainedDocument12 pagesHeart Attack Risk Factors and Symptoms ExplainedHazwan AkmalNo ratings yet
- Case Study For Coronary Artery DiseaseDocument8 pagesCase Study For Coronary Artery DiseaseGabbii CincoNo ratings yet
- G, HJDocument5 pagesG, HJArif Rahman HakimNo ratings yet
- High Percentage of Sleep Disturbances Can Affect The Recovery of The PatientDocument1 pageHigh Percentage of Sleep Disturbances Can Affect The Recovery of The PatientMatt SinnungNo ratings yet
- Perioperative NursingDocument88 pagesPerioperative Nursingfairwoods100% (3)
- Elective Neck Dissection in Tongue CancerDocument6 pagesElective Neck Dissection in Tongue CancerDiah HayustiningsihNo ratings yet
- Acosta-Urquidi 2019 - HealingDocument2 pagesAcosta-Urquidi 2019 - HealingNassos VionisNo ratings yet
- Emergency Room Rotation Requirements: Pamantasan NG Lungsod NG MaynilaDocument12 pagesEmergency Room Rotation Requirements: Pamantasan NG Lungsod NG MaynilaMarco BaltazarNo ratings yet
- Health and Sickness in The Light of IslaamDocument6 pagesHealth and Sickness in The Light of IslaamIbn SadiqNo ratings yet
- Human Development Nursing QuestionsDocument12 pagesHuman Development Nursing QuestionsMary SingletonNo ratings yet
- Joc 911151Document8 pagesJoc 911151Daniel BorgesNo ratings yet
- Bachelor of Physiotherpy: "A Case Study of Leprosy"Document9 pagesBachelor of Physiotherpy: "A Case Study of Leprosy"NATIONAL XEROXNo ratings yet
- ReferensiDocument126 pagesReferensiFatchul ChoiriNo ratings yet
- Management of Unconscious PatientDocument51 pagesManagement of Unconscious PatientEmenike Donald Ejieji50% (2)
- MBBS FINAL PROFESSIONAL MODEL QUESTIONS FOR ANNUAL 2009 MEDICINE (MCQSDocument9 pagesMBBS FINAL PROFESSIONAL MODEL QUESTIONS FOR ANNUAL 2009 MEDICINE (MCQSemmaazizNo ratings yet
- Distal Radius FractureDocument16 pagesDistal Radius FractureDeneishMuruNo ratings yet
- Level Worksheet: 2 DripDocument3 pagesLevel Worksheet: 2 DripDiksha AhluwaliaNo ratings yet
- CGHS RATE AHMEDABAD 2021Document51 pagesCGHS RATE AHMEDABAD 2021Chirag KoradiaNo ratings yet
- 16Document4 pages16Charmaine Gem Aganon PeregrinoNo ratings yet
- Mnemonic For CSDocument23 pagesMnemonic For CSJavier Presser80% (5)
- Obat TeratogenikDocument24 pagesObat TeratogenikHidayat BazeherNo ratings yet
- Rijsummin Amalisyton Fajtanibuhu Laalakum Tuflihun." It Means: "Oh Ye TheDocument2 pagesRijsummin Amalisyton Fajtanibuhu Laalakum Tuflihun." It Means: "Oh Ye TheyesbingitNo ratings yet
- Acupuncture Core Therapy: Shakujyū ChiryōDocument15 pagesAcupuncture Core Therapy: Shakujyū ChiryōFernando IglesiasNo ratings yet
- First Twenty Years of Little Traverse HospitalDocument11 pagesFirst Twenty Years of Little Traverse HospitalHarbor Springs Area Historical SocietyNo ratings yet
- Sewage Treatment PlantDocument11 pagesSewage Treatment Plantjaffna86% (7)
- Alem Mehari ReportDocument67 pagesAlem Mehari Reportetayhailu100% (5)
- Postural Alignment For Voice Production PDFDocument10 pagesPostural Alignment For Voice Production PDFMarianela Guerrero Mesías100% (1)
- CNS Vital Signs Interpretation Guide: Business OfficeDocument15 pagesCNS Vital Signs Interpretation Guide: Business OfficeJason WeaverNo ratings yet
- Quick Cleanse 15 Day DetoxDocument44 pagesQuick Cleanse 15 Day DetoxAnonymous YtbUfrXYNo ratings yet
- Varcarolis CH 1Document21 pagesVarcarolis CH 1Catlyn ChatpmanNo ratings yet
- Types of Salt Compared: Himalayan vs Kosher vs Sea vs TableDocument7 pagesTypes of Salt Compared: Himalayan vs Kosher vs Sea vs TableThanabalan MunuswamyNo ratings yet
- Dr. Ginger Bowler: Energy Medicine ExpertDocument3 pagesDr. Ginger Bowler: Energy Medicine ExpertlskerponfblaNo ratings yet