Professional Documents
Culture Documents
Migraine
Uploaded by
Rose Athena SibalaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Migraine
Uploaded by
Rose Athena SibalaCopyright:
Available Formats
Migraine Headaches Migraine is the most common form of disabling headache that prompts patients to seek care from
doctors. Migraines are sometimes classified as occurring with aura (previously called classic migraine) or without aura (previously called common migraine). There may be up to four phases to a migraine: prodrome phase, auras, the attack, and the postdrome phase. These phases may not occur in every patient or every headache. Prodrome. The prodrome phase is a group of vague symptoms that may precede a migraine attack by several hours, or even a day or two. Prodrome symptoms include: y Sensitivity to light or sound y Changes in appetite, including decreased appetite or food cravings y Thirst y Fatigue and drowsiness y Mood changes, including depression, irritability, or restlessness Auras. Auras are sensory disturbances that occur before the migraine attack in 1 in 5 patients. Visually, auras are referred to as being positive or negative: y Positive auras include bright or shimmering light or shapes at the edge of the field of vision called scintillating scotoma. They can enlarge and fill the line of vision. Other positive aura experiences are zigzag lines or stars. y Negative auras are dark holes, blind spots, or tunnel vision (inability to see to the side). y Patients may have mixed positive and negative auras. This is a visual experience that is sometimes described as a fortress with sharp angles around a dark center. Other neurologic symptoms may occur at the same time as the aura, although they are less common. They include: y Speech disturbances y Tingling, numbness, or weakness in an arm or leg y Perceptual disturbances such as space or size distortions y Confusion Migraine Attack. If untreated, attacks usually last from 4 - 72 hours. A typical migraine attack produces the following symptoms: y Throbbing pain on one side of the head. The word migraine, in fact, is derived from the Greek word hemikrania, meaning "half of the head" because the pain of migraine often occurs on one side. Pain also sometimes spreads to affect the entire head. y Pain worsened by physical activity y Nausea, sometimes with vomiting y Visual symptoms y Facial tingling or numbness y Extreme sensitivity to light and noise y Looking pale and feeling cold Less common symptoms include tearing and redness in one eye, swelling of the eyelid, and nasal congestion, including runny nose. (Such symptoms are more common in certain other headaches, notably cluster headaches.) Postdrome. After a migraine attack, there is usually a postdrome phase, in which patients may feel exhausted and mentally foggy for a while. Chronic Migraine (Transformed Migraine) In some cases, patients eventually experience on-going and chronic migraine (also called transformed migraine). Chronic migraines typically begin as episodic headaches when patients are in their teens or 20s, which then increase in frequency over time. Headaches generally occur at least 50% of the days over a month, and often on a daily or near-daily basis. The majority of chronic migraines are caused by overuse of analgesic migraine medications, both prescription pain reliever drugs and over-the-counter analgesic medications. Medication overuse headaches are also called rebound headaches. Obesity and caffeine overuse are other factors that may increase the risk of episodic migraine transforming to chronic migraine. Chronic migraines can resemble tension headaches and it is sometimes difficult to differentiate between them. Both types of headaches can co-exist. In addition to throbbing pain on one side of the head, chronic migraine is marked by gastrointestinal symptoms such as nausea and vomiting. Many patients with chronic migraine also suffer from depression. Other Migraine Variations Although migraine is considered to be a specific chronic illness, it has various presentations that occur in different individuals. Menstrual Migraines. Migraines are often tied to a woman's menstrual cycle, typically in the first days preceding or beginning menstruation. Estrogen and progesterone fluctuations may play a role. About half of women with migraines report an association with menstruation. Compared to migraines that occur at other times of the month, menstrual migraines tend to be more severe, last longer, and not have auras. Triptan drugs can provide relief and may also help prevent these types of migraines.
Basilar Migraine. Considered a subtype of migraine with aura, this migraine starts in the basilar artery, which forms at the base of the skull. It occurs mainly in young people. Symptoms may include vertigo (the room spins), ringing in the ears, slurred speech, unsteadiness, possibly loss of consciousness, and severe headaches. Abdominal Migraine. This migraine tends to occur in children who have a family history of migraine. Periodic migraine attacks are accompanied by abdominal pain, and often nausea and vomiting. Ophthalmoplegic Migraine. This very rare headache tends to occur in younger adults. The pain centers around one eye and is usually less intense than in a standard migraine. It may be accompanied by vomiting, double vision, a droopy eyelid, and paralysis of eye muscles. Attacks can last from hours to months. A computed tomography (CT) or magnetic resonance imaging (MRI) scan may be needed to rule out an aneurysm (a rupture blood vessel) in the brain. Retinal Migraine. Symptoms of retinal migraine are short-term blind spots or total blindness in one eye that lasts less than an hour. A headache may precede or occur with the eye symptoms. Sometimes retinal migraines develop without headache. Other eye and neurologic disorders must be ruled out. Familial Hemiplegic Migraine. This is a very rare inherited genetic migraine disease. It can cause temporary paralysis on one side of the body, vision problems, and vertigo. These symptoms occur about 10 - 90 minutes before the headache. Status Migrainosus. This is a serious and rare migraine. It is so severe and lasts so long that it requires hospitalization. Causes Until recently, abnormalities of blood vessel (vascular) systems in the head were thought to be mainly responsible for migraines. Now, however, doctors tend to believe that migraine starts with an underlying central nervous system disorder. When triggered by various stimuli, this disorder sets off a chain of neurologic and biochemical events, some of which subsequently affect the brain's vascular system. No experimental model fully explains the migraine process. There is certainly a strong genetic component in migraine with or without auras. Researchers have located a single genetic mutation responsible for the very rare familial hemiplegic migraine, but several genes are likely to be involved in the great majority of migraine cases. Numerous chemicals, structures, nerve pathways, and other players involved in the process are under investigation. These include: y Peptides. Stress or some unknown factor triggers the release of certain protein fragments called peptides (Substance P, calcitonin gene-related peptide, and others). These peptides dilate blood vessels and produce an inflammatory response that triggers over-excitation of the nerve cells in the trigeminal pathway. [This nerve pathway runs from the brain stem to the head and face. These nerves spread to the meninges (the membrane covering of the brain.)] y Abnormal Calcium Channels. Some migraines may be due to abnormalities in the channels within cells that transport the electrical ions calcium, magnesium, sodium, and potassium. Calcium channels appear to play a particularly critical role in migraine. y Serotonin and Other Neurotransmitter Levels. Neurotransmitters are chemical messengers in the brain. Serotonin is a neurotransmitter (chemical messenger in the brain) that is important for sleep, well-being, and other factors that affect quality of life. Abnormalities in serotonin levels have been observed in both tensiontype and migraine headache sufferers. Altered levels of other neurotransmitters, importantly dopamine and stress hormones, also occur with migraine and tension-type headaches, and could trigger the events in the brain leading to migraine. y Reduced Magnesium Levels. Magnesium deficiencies have been observed in people with both tension-type and migraine headaches. Reduced levels could be a destabilizing factor, causing the nerves in the brain to misfire, possibly even accounting for the auras that many sufferers experience. y Nitric Oxide. Other research suggests that nitric oxide may be important in triggering in most primary headaches (tension-type, cluster, and migraines). y Estrogen Fluctuations in Women. Tension-type headaches and migraine headaches are slightly more common in females during adolescence and adulthood. Most likely hormonefluctuations, rather than whether levels are elevated or low, trigger headaches. Migraine Triggers A wide range of events and conditions can alter conditions in the brain that bring on nerve excitation and trigger migraines. They include, but are not limited to: y Emotional stress y Intense physical exertion (such as exercise, lifting, or even bowel movements or sexual activity) y Abrupt weather changes y Bright or flickering lights y Odors y High altitude y Travel motion y Lack of sleep y Skipping meals y Certain types of foods, and chemicals contained in them. More than 100 foods and beverages may potentially trigger migraine headache. Caffeine is one such trigger. Caffeine withdrawal can also trigger migraines in people who are accustomed to caffeine. Red wine and beer are also common triggers. Preservatives and additives (such as nitrates, nitrites, and MSG) can also trigger attacks. Doctors recommend that patients keep a headache diary to track which foods trigger migraine.
Risk Factors Gender About 75% of all migraine sufferers are women. Migraine is more prevalent among women throughout the world and in every culture. Although the incidence of migraine is similar for boys and girls during childhood, it increases in girls after puberty. Migraine most commonly affects women between the ages of 20 - 45. Fluctuations of female hormones, such as estrogen and progesterone, appear to increase the risk for migraines and their severity in some women. About half of women with migraines report headaches associated with their menstrual cycle. For some women, migraines also tend to be worse during the first trimester of pregnancy, but improve during the last trimester. Age Migraine headaches typically affect people between the ages of 15 - 55. However, migraine also affects about 5 10% of all children. Unlike migraine in adults, migraines in children occur equally in boys and girls. Studies indicate that many children with migraine eventually stop having attacks when they reach adulthood or transition to less severe tension-type headaches. Children with a family history of migraine may be more likely to continue having migraines. Family History Migraines tend to run in families. About 70 - 80% of patients with migraine have a family history of the condition. Medical Conditions Associated with Migraines Many people with migraine have or have a history of depression, anxiety, stroke, epilepsy, irritable bowel syndrome, or high blood pressure. These conditions do not necessarily increase the risk for migraine, but they are associated with it. Prognosis For many people, migraines eventually go into remission and sometimes disappear completely, particularly as they age. Estrogen decline after menopause may be responsible for remission in some older women. Complications Risk for Stroke and Heart Disease. Migraine or severe headache is a risk factor for stroke in both men and women, especially before age 50. Research indicates that migraine may also increase the risk for other types of heart problems. Migraine with aura appears to carry a higher risk for stroke than migraine without aura, especially for women. Because of this, it is very important that women with migraine avoid other stroke risks such as smoking and possibly birth control pills. Some studies suggest that people who have migraine with aura are more likely than people without migraine to have cardiovascular risk factors (high cholesterol, high blood pressure) that increase the risk for stroke. [For more information, see In-Depth Report #45: Stroke.] Emotional Disorders and Quality of Life. Migraines have a significant negative impact on quality of life, family relations, and work productivity. Studies indicate that people with migraines have poorer social interactions and emotional health than patients with many chronic medical illnesses, including asthma, diabetes, and arthritis. Anxiety (particularly panic disorders) and major depression are also strongly associated with migraines. A National Headache Foundation-sponsored survey of migraine sufferers reported that: y 90% of people with migraines could not function normally on the day of a migraine attack y 80% experienced abnormal sensitivity to light and noise y 75% experienced nausea and vomiting y 30% required bed rest y 25% missed at least 1 day of work due to migraine in past 3 months Diagnosis Anyone, including children, with recurring or persistent headaches should consult a doctor. There are no blood tests or imaging techniques that can be used to diagnose migraine headaches. A diagnosis will be made on the basis of medical history and physical exam, and, if necessary, tests may be necessary to rule out other diseases or conditions that may be causing the headaches. It is important to choose a doctor who is sensitive to the needs of headache sufferers and aware of the latest advances in treatment.
Diagnostic Criteria for Migraine A diagnosis of migraine is usually made on the basis of repeated attacks (at least 5) that meet the following criteria: y Headache attacks that last 4 - 72 hours y Headache has at least two of the following characteristics: Location on one side of the head; throbbing pain; moderate or severe pain intensity; pain worsened by normal physical activity (walking, climbing stairs) y During the headache, the patient experiences one or both of the following characteristics: Nausea or vomiting; extreme sensitivity to light or sound y The headache cannot be attributed to another disorder Headache Diary The patient should try to recall what seems to bring on the headache and anything that relieves it. Keeping a headache diary is a useful way to identify triggers that bring on headaches, as well as to track the duration and frequency of headache attacks. Some tips include: y Note all conditions, including any foods eaten, preceding an attack. Often two or more triggers interact to produce a headache. For example, a combination of weather changes and fatigue can make headaches more likely than the presence of just one of these events. y Keep a migraine record for at least three menstrual cycles. For women, this can help to confirm or refute a diagnosis of menstrual migraine.
y Track medications. This is important for identifying possible medication-overuse (rebound) headache or chronic (transformed) migraine. y Attempt to define the intensity of the headache using a number system, such as: 1 = Mild, barely noticeable 2 = Noticeable, but does not interfere with work/activities 3 = Distracts from work/activities 4 = Makes work/activities very difficult 5 = Incapacitating Medical and Personal History The patient should report any other conditions that might be associated with headache, including: y Any chronic or recent illness and their treatments y Any injuries, particularly head or back injuries y Any uncharacteristic dietary changes y Any current medications or recent withdrawals from any drugs, including over-the-counter or natural remedies y Any history of caffeine, alcohol, or drug abuse y Any serious stress, depression, and anxiety The doctor will also need a general medical and family history of headaches or diseases, such as epilepsy, that may increase their risk. Migraine tends to run in families. Physical Examination In order to diagnose a chronic headache, the doctor will examine the head and neck and will usually perform a neurologic examination, which includes a series of simple exercises to test strength, reflexes, coordination, and sensation. The doctor may ask questions to test short-term memory and related aspects of mental function. Differentiating Between Migraine and Other Types of Headaches
Differentiating Between Migraines and Tension Headaches. Migraines and tension headaches have some similar characteristics, but also some important differences: y Migraine pain is throbbing, while tension-type headache pain is usually a steady ache y Migraine pain may affect only one side of the head while tension-type headache pain typically affects both sides of the head y Migraine pain, but not tension-type pain, worsens with head movement y Migraine headaches, but not tension-type headaches, may be accompanied by nausea or vomiting, sensitivity to light and sound, or aura Differentiating Between Migraines and Sinus Headaches. Many primary headaches, including migraine, are misdiagnosed as sinus headaches, causing patients to be treated inappropriately with antibiotics. Many patients who think they have sinus headaches may actually have had a migraine. Sinus headaches occur in the front of the face, usually around the eyes, across the cheeks, or over the forehead. They are usually mild in the morning and increase during the day and are usually accompanied by fever, runny nose, congestion, and general debilitation. It is also possible for patients to have migraines with sinus symptoms. A real sinus headache is a sign of an acute sinus infection, which responds to treatment with decongestants. Patients who do not respond or who have severe sinusitis should receive antibiotics. If sinus headaches seem to recur, the patient is likely experiencing migraines. Treating Migraine Attacks Many effective headache remedies are available for treating a migraine attack. Still, many patients are treated with unapproved drugs, including opoids and barbiturates that can be potentially addictive or dangerous. The main types of medications for treating a migraine attack are: y Pain relievers [usually nonprescription nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen] y Ergotamines y Triptans It is best to treat a migraine attack as soon as symptoms first occur. Doctors generally recommend: y Start with nonprescription pain relievers for mild-to-moderate attacks. If migraine pain is severe, a prescription version of an NSAID may be recommended. y A triptan is generally the next drug of choice.
y Ergotamine drugs tend to be less effective than triptans but are helpful for some patients. y Depending on the severity of the attacks, and accompanying symptoms, the doctor may recommend taking a triptan or ergotamine drug in tablet, injection, or suppository form. The doctor may also prescribe specific medications for treating symptoms such as nausea. Try to guard against medication overuse, which can cause a rebound effect. Nearly all pain relief drugs used for migraine can cause rebound headache, and patients should not take any the drugs more than 9 days per month. If you find that you need to use acute migraine treatment more frequently, talk to your doctor about preventive medications. Preventing Migraine Attacks Preventive strategies for migraine include both drug treatment and behavioral therapy or lifestyle adjustments. Patients should consider using preventive migraine drugs if they have: y Migraines that are not helped by acute treatment drugs y Frequent attacks (more than once per week) y Side effects from acute treatment drugs or contraindications to taking them The main preventive drug treatments for migraine are: y Beta-blocker drugs [usually propranolol (Inderal) or timolol (Blocadren)] y Anti-seizure drugs [usually divalproex (Depakote) or topiramate (Topamax)] y Tricyclic antidepressants [usually amitriptyline (Elavil)] A preventive medication strategy needs to be carefully tailored to an individual patient, taking into account the patient's medical history and co-existing medical conditions. These drugs can have serious side effects. A preventive medication is usually started at a low dose, and then gradually increased. It may take 2 - 3 months for a drug to achieve its full effect. Preventive treatment may be needed for 6 - 12 months or longer. Most patients take preventive medications on a daily basis, but some patients may use these drugs intermittently (for example, for preventing menstrual migraine). Patients can also help prevent migraines by identifying and avoiding potential triggers, such as specific foods. Relaxation therapy and stress reduction techniques may also help. Treatment Approaches for Children Migraine Treatment for Children. Most children with migraines may need only mild pain relievers and home remedies (such as ginger tea) to treat their headaches. The American Academy of Neurology's practice guidelines for children and adolescents recommend the following drug treatments: y For children age 6 years and older, ibuprofen (Advil) is recommended. Acetaminophen (Tylenol) may also be effective. Acetaminophen works faster than ibuprofen, but the effects of ibuprofen last longer. y For adolescents age 12 years and older, sumaptriptan (Imitrex) nasal spray is recommended. Migraine Prevention for Children. Non-medication methods, including biofeedback and muscle relaxation techniques may be helpful. If these methods fail, then preventive drugs may be used, although evidence is weak on the effectiveness of standard migraine preventive drugs in children. Withdrawing from Medications If medication overuse causes rebound migraines to develop, the patient cannot recover without stopping the drugs. (If caffeine is the culprit, a person may need only to reduce coffee or tea drinking to a reasonable level, not necessarily stop drinking it altogether.) The patient can usually stop abruptly or gradually. The patient should expect the following: y Most headache drugs can be stopped abruptly, but the patient should talk to their doctor first. Certain nonheadache medications, such as anti-anxiety drugs or beta-blockers, require gradual withdrawal under medical supervision. y If the patient chooses to taper off standard headache medications, withdrawal should be completed within three days. y The patient may take other pain medicines during the first days. Examples of drugs that may be used include dihydroergotamine (with or without metoclopramide), NSAIDs (in mild cases), corticosteroids, or valproate. y Patients must expect their headaches to get worse after they stop taking their medications, no matter which method they use. Most people feel better within 2 weeks, although headache symptoms can persist up to 16 weeks (and in rare cases even longer). y If the symptoms do not respond to treatment and cause severe nausea and vomiting, the patient may need to be hospitalized. Medications for Treating Migraine Attacks Many different medications are used to treat migraines. However, the Food and Drug Administration (FDA) has specifically approved only the following types of drugs for treating migraine attacks: y Non-prescription drugs. Excedrin Migraine, Advil Migraine, and Motrin Migraine Pain y Prescription drugs. Triptans and ergotamine Other types of drugs, including opioids and barbiturates, are sometimes prescribed off-label for migraine treatment. Opioids and barbiturates have not been approved by the FDA for migraine relief, and they can be addictive. All FDA-approved migraine treatments are approved only for adults. No migraine products have officially been approved for use in children. Pain Relievers Some patients with mild migraines respond well to over-the-counter (OTC) painkillers, particularly if they take a full dose of the medicine at the very first sign of an attack. OTC pain relievers, also called analgesics, include:
y Nonsteroidal anti-inflammatory drugs such as ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin. The FDA-approved migraine products Advil Migraine and Motrin Migraine Pain both contain ibuprofen. y Acetaminophen (Tylenol). The FDA-approved migraine product Excedrin Migraine contains acetaminophen, as well as aspirin and caffeine. There are also prescription-only NSAIDs. These include diclofenac (Cataflam), which is taken by mouth, and ketorolac (Toradol), which is given by injection. NSAID Side Effects. High dosages and long-term use of NSAIDs can increase the risk for heart attack, stroke, kidney problems, and stomach bleeding. Aspirin does not increase the risk for heart problems, but it can cause other NSAID-related side effects. Triptans Triptans (also referred to as serotonin agonists) were the first drugs specifically developed for use against migraine. They are the most important migraine drugs currently available. They help maintain serotonin levels in the brain, and so specifically target one of the major components in the migraine process. Triptans are recommended as first-line drugs for adult patients with moderate-to-severe migraines when NSAIDs are not effective. Triptans have the following benefits: y They are effective for most patients with migraine, as well as patients with combination tension and migraine headaches. y They do not have the sedative effect of other migraine drugs. y Withdrawal after overuse appears to be shorter and less severe than with other migraine medications Sumatriptan. Sumatriptan (Imitrex) has the longest track record and is the most studied of all triptans. It is available as a fast-dissolving pill, nasal spray, or injection. Injected sumatriptan works the fastest of all the triptans and is the most effective, but it can cause pain at the injection site. The nasal spray form bypasses the stomach and is absorbed more quickly than the oral form. Some patients report relief as soon as 15 minutes after administration. The spray tends to work less well when a person has nasal congestion from cold or allergy. It may also leave a bad taste. Sumatriptan is effective for many patients, but headache recurs in 20 - 40% of people within 24 hours after taking the drug. Other Triptans. Newer triptans include almotriptan (Axert), zolmitriptan (Zomig), naratriptan (Amerge), rizatriptan (Maxalt), frovatriptan (Frova), and eletriptan (Relpax). Treximet combines in one pill both sumatriptan and the anti-inflammatory pain reliever naproxen (Aleve, Naprosyn). Triptans are also being investigated for prevention under certain circumstances, such as menstrual migraines, but benefits appear limited. Although triptans, (like all migraine medications), are approved only for adults, researchers are investigating zolmitriptan for treating migraines in adolescents. Side Effects. Side effects of triptans may include: y Tingling and numbness in the toes y Sensations of warmth y Discomfort in the ear, nose, and throat y Nausea y Drowsiness y Dizziness y Muscle weakness y Heaviness, pain, or both in the chest. (About 40% of patients taking sumatriptan experience these symptoms, and they are major factors in discontinuing the drug. Newer drugs, such as almotriptan, produce fewer chest symptoms.) y Rapid heart rate Complications of Triptans. The following are potentially serious problems. y Complications of heart and circulation. Triptans narrow (constrict) blood vessels. Because of this effect, spasms in the blood vessels may occur and cause serious side effects, including stroke and heart attack. Such events are rare, but patients with an existing history or risk factors for these conditions should generally avoid triptans. y Serotonin syndrome. Serotonin syndrome is a life-threatening condition that occurs from an excess of the brain chemical serotonin. Triptan drugs used to treat migraine, as well as certain types of antidepressant medications, can increase serotonin levels. These antidepressant drugs include serotonin reuptake inhibitors (SSRIs) -- such as fluoxetine (Prozac), paroxetine (Paxil), and sertraline (Zoloft) -- and selective serotonin/norepinephrine reuptake inhibitors (SNRIs), such as duloxetine (Cymbalta) and venlafaxine (Effexor). It is very important that patients not combine a triptan drug with a SSRI or SNRI drug. Serotonin syndrome is most likely to occur when starting or increasing the dose of a triptan or antidepressant drug. Symptoms include restlessness, hallucinations, rapid heartbeat, tremors, increased body temperature, diarrhea, nausea, and vomiting. You should seek immediate medical care if you have these symptoms. The following people should avoid triptans or take them with caution and only with the advisement of a doctor: y Anyone with a history or any risk factors for stroke, uncontrolled diabetes, high blood pressure, or heart disease. y People taking antidepressants that increase serotonin levels. y Children and adolescents. They may be safe, but controlled studies are needed to confirm this. (Triptans should not, in any case, be the first-line treatment for children.) y People with basilar or hemiplegic migraines. (Triptans are not indicated for these migraineurs.) y There is no evidence to date of any higher risk for birth defects in pregnant women who take triptans. Still, women should be cautious about taking any medications during pregnancy and discuss any possible adverse effects with their doctors.
Ergotamine (Ergot) Drugs containing ergotamine (commonly called ergots) constrict smooth muscles, including those in blood vessels, and are useful for migraine. They were the first anti-migraine drugs available. Ergotamine is available by prescription in the following preparations: y Dihydroergotamine (DHE) is an ergot derivative. It is administered as a nasal spray form (Migranal) or by injection, which can be performed at home. y Ergotamine is available tablets taken by mouth, tablets taken under the tongue (sublingual), and rectal suppositories. Some of the tablet forms of ergotamine contain caffeine. Ergotamine's role since the introduction of triptans is now less certain. Only the rectal forms of ergotamine are superior to rectal triptans. Injected, oral, and nasal-spray forms are all inferior to the triptans. Ergotamine may still be helpful for patients with status migrainous or those with frequent recurring headaches. Side Effects. Side effects of ergotamine include: y Nausea y Dizziness y Tingling sensations y Muscle cramps y Chest or abdominal pain The following are potentially serious problems: y Toxicity. Ergotamine is toxic at high levels. y Adverse effects on blood vessels. Ergot can cause persistent blood vessel contractions, which may pose a danger for people with heart disease or risk factors for heart attack or stroke. y Internal scarring (fibrosis). Scarring can occur in the areas around the lungs, heart, or kidneys. It is often reversible if the drug is stopped. The following patients should avoid ergots: y Pregnant women. Ergots can cause miscarriage. y People over age 60. y Patients with serious, chronic health problems, particularly those with heart and circulation conditions. Ergotamine can interact with other medications, such as antifungal drugs and some antibiotics. All ergotamine products approved by the Food and Drug Administration (FDA) contain a "black box" warning in the prescription label explaining these drug interactions. The five FDA-approved ergotamine products are: y Migergot suppository (marketed by G and W Labs) y Ergotamine Tartrate and Caffeine tablets (marketed by Mikart and West Ward) y Cafergot tablets (marketed by Sandoz) y Ergomar sublingual tablets (marketed by Rosedale Therapeutics) Opioids If the pain is very severe and does respond to other drugs, doctors may try painkillers containing opioids. Opioid drugs include morphine, codeine, meperidine (Demerol), and oxycodone (Oxycontin)]. Butorphanol is an opioid in nasal spray form that may be useful as a rescue treatment when others fail. Opioids are not approved for migraine treatment and should not be used as first-line therapy. Nevertheless, many opioid products are prescribed to patients with migraine, sometimes with dangerous results. For example, following reports of several drug-related deaths, the Food and Drug Administration has warned that the cancer pain pill fentanyl (Fentora) should not be used to treat patients with migraine or others conditions for which the drug is not specifically approved. Side Effects. Side effects for all opioids include drowsiness, impaired judgment, nausea, and constipation. There is a risk for addiction, and these drugs can become ineffective with long-term use for chronic migraines. Doctors should not prescribe opioids to patients at risk for drug abuse, including those with personality or psychiatric disorders. Drugs Used for Nausea and Vomiting Metoclopramide (Reglan) is used in combinations with other drugs to treat the nausea and vomiting that occurs with other drugs and with migraine itself. Metoclopramide and other anti-nausea drugs, such as domperidone (Motilium), may help the intestine better absorb migraine medications. Medications for Preventing Migraine Attacks The Food and Drug Administration has approved four drugs for prevention of migraine: y Propanolol (Inderal) y Timolol (Blacadrene) y Divalproex sodium (Depakote) y Topiramate (Topamax) Propanolol and timolol are beta-blocker drugs. Divalproex and topiramate are anti-seizure drugs. Many other drugs are also being used or investigated for preventing migraines. Beta-Blockers Beta-blockers are usually prescribed to reduce high blood pressure. Some beta-blockers, however, are also useful in reducing the frequency of migraine attacks and their severity when they occur. Propranolol (Inderal) and timolol (Blocadren) have been approved specifically for prevention of migraine. Metoprolol (Toprol), atenolol (Tenormin), and nadolol (Corgard) are also being studied for migraine prevention. Side Effects. Side effects may include: y Fatigue and lethargy are common. y Some people experience vivid dreams and nightmares, depression, and memory loss. y Dizziness and lightheadedness may occur upon standing. y Exercise capacity may be reduced. y Other side effects may include cold extremities, asthma, decreased heart function, gastrointestinal problems, and sexual dysfunction.
If side effects occur, the patient should call a doctor, but it is extremely important not to stop the drug abruptly. Some evidence suggests that people with migraines who have had a stroke should avoid beta-blockers. Anti-Seizure Drugs Anti-seizure drugs, also called anticonvulsant drugs, are commonly used for treating epilepsy and bipolar disorder. Divalproex sodium (Depakote) and topiramate (Topamax) are the only anti-seizure drugs that are approved for migraine prevention. However, if patients do not respond to either of these drugs, doctors may try other types of anti-seizure medications. Divalproex Sodium (Depakote). Divalproex sodium (Depakote) was first approved in 1996 for migraine prevention. A once-a-day formulation of divalproex (Depakote ER) was approved in 2000. Doctors sometimes prescribe a similar drug, valproate (Depakene). Pregnant patients should not use these drugs, as they may cause birth defects. Topiramate (Topamax). In 2004, the Food and Drug Administration approved topiramate for prevention of migraines in adults. Topiramate's most common side effect is a tingling sensation in the arms and legs. Weight loss is also a side effect. Other Anti-Seizure Drugs Under Investigation. Researchers are studying other types of anti-seizure drugs for migraine prevention, including levetiracetam (Keppra), gabapentin (Neurontin), and pregabalin (Lyrica). Side Effects. Anti-seizure medication side effects vary by drug but may include: y Nausea and vomiting y Diarrhea y Cramps y Hair loss y Dizziness y Sleepiness y Blurred vision y Weight gain y Valproate and divalproex can cause serious side effects of inflammation of the pancreas (pancreatitis) and damage to the liver Tricyclic and Other Antidepressants Amitriptyline (Elavil, Endep), a tricyclic antidepressant drug, has been used for many years as a first-line treatment for migraine prevention. It may work best for patients who also have depression or insomnia. Tricyclics can have significant side effects, including disturbances in heart rhythms, and can be fatal in overdose. Although other tricyclic antidepressants may have fewer side effects than amitritpyline, they do not appear to be particularly effective for migraine prevention. Researchers have investigated newer types of antidepressants, including serotonin-reuptake inhibitors (SSRIs), such as fluoxetine (Prozac). However, studies to date do not indicate that SSRIs are helpful for migraine prevention. Behavioral Treatments Behavioral techniques that reduce stress and empower the patient may help some people with migraines. They generally include: y Biofeedback therapy y Relaxation techniques y Cognitive-behavioral therapy Behavioral methods may help counteract the tendency for muscle contraction and uneven blood flow associated with some headaches. They may be particularly beneficial for children, adolescents, and pregnant and nursing women, and anyone who cannot take most migraine medications. Studies generally find that these techniques work best when used in combination with medications. Biofeedback. Many studies have demonstrated that biofeedback is effective for reducing migraine headache frequency. Biofeedback training teaches the patient to monitor and modify physical responses, such as muscle tension, using special instruments for feedback. Relaxation Therapy. Relaxation therapy techniques include relaxation response, progressive muscle relaxation, visualization, and deep breathing. Muscle relaxation techniques are simple and easy to learn, and can be effective. Some patients may also find that relaxation techniques combined with applying a cold compress to the forehead may help provide some pain relief during attacks. Some commercially available products use a pad containing a gel that cools the skin for several hours. Cognitive Behavioral Therapy. Cognitive-behavioral therapy (CBT) teaches patients how to recognize and cope with stressors in their life. It can help patients understand how their thoughts and behavior patterns may affect their symptoms, and how to change the way the body responds to anticipated pain. CBT may be included with stress management techniques. Research indicates that CBT is most effective when combined with relaxation training or biofeedback. Acupuncture Acupuncture is a Chinese medicine technique that uses thin needles to stimulate specific points aligned with energy pathways in the body. Studies have showed mixed results on the benefits of acupuncture for preventing migraine. Lifestyle Changes Making a few minor changes in your lifestyle can make your migraines more bearable. Improving sleep habits is important for everyone, and especially those with headaches. What you eat also has a huge impact on migraines, so dietary changes can be extremely beneficial, too. Avoid Food Triggers. Avoiding foods that trigger migraine is an important preventive measure. Common food triggers include monosodium glutamate (MSG), processed lunch meats that contain nitrates, dried fruits that contain sulfites, aged cheese, alcohol and red wine, chocolate, and caffeine. However, peoples responses to triggers differ. Keeping a headache diary that tracks diet and headache onset can help identify individual food triggers.
Eat Regularly. Eating regularly is important to prevent low blood sugar. People with migraines who fast periodically for religious reasons might consider taking preventive medications. Stay Physically Active. Exercise is certainly helpful for relieving stress. An analysis of several studies reported that aerobic exercise in particular might help prevent migraines. It is important, however, to warm up gradually before beginning a session, since sudden, vigorous exercise might actually precipitate or aggravate a migraine attack. Limit Estrogen-Containing Medications. Medications that contain estrogen, such as oral contraceptives and hormone replacement therapy, may trigger migraines or make them worse. Talk to your doctor about whether you should stop taking these types of medications or reduce the dosage. Herbs and Supplements Manufacturers of herbal remedies and dietary supplements do not need Food and Drug Administration approval to sell their products. Just like a drug, herbs and supplements can affect the body's chemistry, and therefore have the potential to produce side effects that may be harmful. There have been several reported cases of serious and even lethal side effects from herbal products. Patients should always check with their doctors before using any herbal remedies or dietary supplements. Riboflavin (Vitamin B2). Some studies have found that people who take vitamin B2 experience a reduction in the frequency of migraine attacks (although not on duration or severity). Vitamin B2 is generally safe, although some people taking high doses develop diarrhea. Magnesium Supplements. Some studies have reported a higher rate of magnesium deficiencies in some patients with migraine, such as those with menstrual migraines. Magnesium helps relax blood vessels. Some patients report that magnesium supplements help provide relief. Feverfew. Feverfew is the most studied herbal remedy for headaches and may help in some cases. However, like all effective headache remedies, overuse can cause a rebound effect. Fish Oil. Some studies suggest that omega-3 fatty acids, which are found in fish oil, have anti-inflammatory and nerve protecting actions. These fatty acids can be found in oily fish, such as salmon, mackerel, or sardines. They can also be obtained in supplements of specific omega-3 compounds (DHA-EPA). Ginger. In general, herbal medicines should never be used by children or pregnant or nursing women without medical counsel. One exception may be ginger, which has no side effects and can be eaten in powder or fresh form, as long as quantities are not excessive. Some people have reported less pain and frequency of migraines while taking ginger, and children can take it without danger. Ginger is also a popular home remedy for relieving nausea.
You might also like
- Pebc Evaluating Exam Sample QuestionDocument39 pagesPebc Evaluating Exam Sample Questionmahyar_ro79% (14)
- New England Journal of Medicine Volume 383 Issue 19 2020 (Doi 10.1056 - NEJMra1915327) Ropper, Allan H. Ashina, Messoud - MigraineDocument11 pagesNew England Journal of Medicine Volume 383 Issue 19 2020 (Doi 10.1056 - NEJMra1915327) Ropper, Allan H. Ashina, Messoud - MigraineMarija Sekretarjova100% (1)
- What is migraine and how can it be managedDocument6 pagesWhat is migraine and how can it be managedEliza SitinjakNo ratings yet
- Thyroid DrugsDocument6 pagesThyroid DrugsThe Real UploaderNo ratings yet
- Recipe Testing and Evaluation ReportDocument10 pagesRecipe Testing and Evaluation Reportapi-437135014No ratings yet
- Clinical Pathway Guidelines of Food Poisoning and Chemical Poisoning1Document3 pagesClinical Pathway Guidelines of Food Poisoning and Chemical Poisoning1Winna Tapia Tabiosa UbolNo ratings yet
- Diabetic and Endocrine Emergencies GuideDocument21 pagesDiabetic and Endocrine Emergencies Guidejoko5157No ratings yet
- Diagnosis and Management of HeadacheDocument12 pagesDiagnosis and Management of HeadacheRay BoettgerNo ratings yet
- Maternity Newborn and Womens Health Nursing A Case Based Approach First Edition Ebook PDFDocument62 pagesMaternity Newborn and Womens Health Nursing A Case Based Approach First Edition Ebook PDFbenjamin.waterman189100% (48)
- 120 Naplex CalculationsDocument51 pages120 Naplex CalculationsWil Lester100% (1)
- CSF AnalysisDocument6 pagesCSF Analysisfrederico_No ratings yet
- Hypocalcemia College PresentationDocument40 pagesHypocalcemia College PresentationClaudia IrimieNo ratings yet
- Basic Paediatric Protocols - Revised - Sept2010Document47 pagesBasic Paediatric Protocols - Revised - Sept2010Aravind Kumar100% (1)
- THYROIDDocument100 pagesTHYROIDFrance PalNo ratings yet
- Surgical Anatomy of the Thyroid GlandDocument86 pagesSurgical Anatomy of the Thyroid GlandsmrutuNo ratings yet
- Food Poisoning Final Print!Document3 pagesFood Poisoning Final Print!Joeven HilarioNo ratings yet
- Approach To Unconscious PatientDocument23 pagesApproach To Unconscious Patienttantw880% (1)
- GoitreDocument6 pagesGoitreJohn Vladimir A. BulagsayNo ratings yet
- Management of Thyroid DisordersDocument53 pagesManagement of Thyroid DisordersAnityo S AthmadjaNo ratings yet
- Health, Stress, and CopingDocument43 pagesHealth, Stress, and CopingKar Gayee100% (1)
- Diagnostic Approach To HeadacheDocument7 pagesDiagnostic Approach To HeadachedanlaytonNo ratings yet
- Personal HygieneDocument32 pagesPersonal Hygienemahaberani_z100% (1)
- Skin PathogensDocument4 pagesSkin PathogensEhi EdialeNo ratings yet
- HeadacheDocument92 pagesHeadacheMilap Shah100% (1)
- HyperthyroidDocument12 pagesHyperthyroidChristine Joy PepitoNo ratings yet
- Thyroid Disease: Presentation By: Pimundu Vicent Audo Ritah Tutor: Dr. Fualal JaneDocument41 pagesThyroid Disease: Presentation By: Pimundu Vicent Audo Ritah Tutor: Dr. Fualal JaneEsther AumaNo ratings yet
- Anti-Depressant Drugs: Presented by L.Nithish Shankar Ii Year Mbbs KGMCDocument17 pagesAnti-Depressant Drugs: Presented by L.Nithish Shankar Ii Year Mbbs KGMCÑiťhišh Śhankąŕ LóganáthánNo ratings yet
- Headache NewDocument17 pagesHeadache NewHaris PeaceNo ratings yet
- CSF AnalysisDocument12 pagesCSF AnalysismedicoprakashNo ratings yet
- Necrotizing Fasciitis: Early Biopsy Key for Aggressive TreatmentDocument6 pagesNecrotizing Fasciitis: Early Biopsy Key for Aggressive TreatmentVirtues GracesNo ratings yet
- Diabetes For EMS ProvidersDocument58 pagesDiabetes For EMS ProvidersPaulhotvw67100% (2)
- Complications of Intravenous TherapyDocument37 pagesComplications of Intravenous TherapyCarl Elexer Cuyugan Ano100% (3)
- USMLE Step 2 Lesson on Thyroid DiseaseDocument4 pagesUSMLE Step 2 Lesson on Thyroid DiseaseMavra zNo ratings yet
- Water Parks TubingDocument12 pagesWater Parks TubingKOLD News 13No ratings yet
- Non-Opioid Analgesics and Types of AnesthesiaDocument31 pagesNon-Opioid Analgesics and Types of AnesthesiaIvonnie Mae MaeNo ratings yet
- ExerciseDocument2 pagesExercisenit_in10No ratings yet
- GoutDocument13 pagesGoutManprit BoparaiNo ratings yet
- FIRST AID by Dr. Qasim AhmedDocument80 pagesFIRST AID by Dr. Qasim AhmedFaheem KhanNo ratings yet
- Grave'S Disease: Farida Ulfa 1510211057Document11 pagesGrave'S Disease: Farida Ulfa 1510211057farida ulfaNo ratings yet
- Pelvic Inflammatory DiseaseDocument47 pagesPelvic Inflammatory DiseaseNur Aliya IshakNo ratings yet
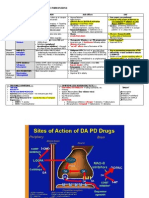
- Pharmacologic TX For Idiopathic Parkinsons: Strategy Class / Drug MOA Side Effects USEDocument2 pagesPharmacologic TX For Idiopathic Parkinsons: Strategy Class / Drug MOA Side Effects USEnicdeepNo ratings yet
- TBI FinalDocument28 pagesTBI Finalawais mpNo ratings yet
- Upper Gi BleedingDocument3 pagesUpper Gi BleedingIkhwan HafrizNo ratings yet
- HemiplegiaDocument17 pagesHemiplegiaStefany CelineNo ratings yet
- GERD ManagementDocument43 pagesGERD ManagementpashaNo ratings yet
- HypocalcemiaDocument23 pagesHypocalcemiarayrrn00No ratings yet
- Skin Rashes in ChildrenDocument11 pagesSkin Rashes in ChildrenwiladamanikNo ratings yet
- MigraineDocument38 pagesMigraineManju PriyaNo ratings yet
- Headache: Thomas Kwiatkowski and Kumar AlagappanDocument11 pagesHeadache: Thomas Kwiatkowski and Kumar AlagappanS100% (1)
- Approach To Internal Medicine Cases: Vince Edward C. Araneta, MD, FPAFP, CSPSHDocument31 pagesApproach To Internal Medicine Cases: Vince Edward C. Araneta, MD, FPAFP, CSPSHKenneth NuñezNo ratings yet
- Drugs Affecting Myometrium1 PDFDocument9 pagesDrugs Affecting Myometrium1 PDFЛариса ТкачеваNo ratings yet
- Bleeding Disorder (Paediatrics)Document95 pagesBleeding Disorder (Paediatrics)Nurul Afiqah Mohd YusoffNo ratings yet
- Lillian's Restaurant Service Flow ChartDocument1 pageLillian's Restaurant Service Flow ChartYannick Harvey100% (1)
- Disorders of Parathyroid Glands: Hyperparathyroidism and HypoparathyroidismDocument52 pagesDisorders of Parathyroid Glands: Hyperparathyroidism and HypoparathyroidismDr. Akash GuptaNo ratings yet
- Endocrine Disorders 1234399857677955 1Document130 pagesEndocrine Disorders 1234399857677955 1api-19824701No ratings yet
- Pleural DiseasesDocument4 pagesPleural DiseasesJennifer DayNo ratings yet
- Essential Enteral and Parenteral Nutrition GuideDocument64 pagesEssential Enteral and Parenteral Nutrition GuideHeba IyadNo ratings yet
- ZofranOndansetron Dr. A. Alisher PPT 14.08.2011 LECTURE... IFTARDocument58 pagesZofranOndansetron Dr. A. Alisher PPT 14.08.2011 LECTURE... IFTARAlisher Agzamov100% (1)
- Gastrointestinal Tract Drugs: Pharmacist Marwan QasimDocument20 pagesGastrointestinal Tract Drugs: Pharmacist Marwan QasimWaliNo ratings yet
- Understanding Alcoholism: Causes, Symptoms, Diagnosis and TreatmentDocument3 pagesUnderstanding Alcoholism: Causes, Symptoms, Diagnosis and TreatmentKaren JulaoNo ratings yet
- Major Depressive Disorder PDFDocument22 pagesMajor Depressive Disorder PDFapi-545811586No ratings yet
- Anatomy of Thyroid GlandDocument12 pagesAnatomy of Thyroid GlandBinbinbabu BinuNo ratings yet
- CHF Drugs Guide: Key Medications for Treating Congestive Heart FailureDocument21 pagesCHF Drugs Guide: Key Medications for Treating Congestive Heart Failuremohsen mirdamadiNo ratings yet
- Migraine Headaches - University of Maryland Medical Center PDFDocument22 pagesMigraine Headaches - University of Maryland Medical Center PDFAl Hasyr SarminNo ratings yet
- What Is MigraineDocument12 pagesWhat Is MigraineKARL PASCUANo ratings yet
- Path o Physiology TablesDocument4 pagesPath o Physiology TablesRose Athena SibalaNo ratings yet
- Epistaxis & TonsillectomyDocument1 pageEpistaxis & TonsillectomyRose Athena SibalaNo ratings yet
- CHN Family HealthDocument4 pagesCHN Family HealthRose Athena SibalaNo ratings yet
- Rose Athena Baja-Sibala, RNDocument22 pagesRose Athena Baja-Sibala, RNRose Athena SibalaNo ratings yet
- Quiz 1: General MOADocument38 pagesQuiz 1: General MOASajeda A. HadiNo ratings yet
- Migraine and Tension-Type Headache: Azmin Kahriman, MD Shuhan Zhu, MDDocument11 pagesMigraine and Tension-Type Headache: Azmin Kahriman, MD Shuhan Zhu, MDAlim GhazaniNo ratings yet
- Chapter 80 - Headache DisordersDocument41 pagesChapter 80 - Headache Disordersalina ignatNo ratings yet
- Formulation and Evaluation of Thermosensitive Intranasal in Situ Gel of Sumatriptan Succinate by Using A Blend of PolymersDocument9 pagesFormulation and Evaluation of Thermosensitive Intranasal in Situ Gel of Sumatriptan Succinate by Using A Blend of PolymersabikeshNo ratings yet
- Module 10Document5 pagesModule 10Yuki Xairah TunayNo ratings yet
- Treatment of Headaches in The ED With Lower Cervical Intramuscular Bupivacaine Injections: A 1-Year Retrospective Review of 417 PatientsDocument9 pagesTreatment of Headaches in The ED With Lower Cervical Intramuscular Bupivacaine Injections: A 1-Year Retrospective Review of 417 PatientsLarry B. Mellick, MDNo ratings yet
- HAMP FormularyDocument45 pagesHAMP FormularykgnmatinNo ratings yet
- Acute Treatment of Migraine in Adults - UpToDateDocument42 pagesAcute Treatment of Migraine in Adults - UpToDateClaudio Avalos MorenoNo ratings yet
- Review Article: Cluster Headache-Acute and Prophylactic TherapyDocument24 pagesReview Article: Cluster Headache-Acute and Prophylactic TherapyPurna Adi PutraNo ratings yet
- The Treatment of Migraine Headaches in Children and AdolescentsDocument11 pagesThe Treatment of Migraine Headaches in Children and Adolescentsdo leeNo ratings yet
- Mock Test 1 Part A Summer 2006Document53 pagesMock Test 1 Part A Summer 2006Alida Rautenbach0% (1)
- Test 2Document15 pagesTest 2Ding DialyzerNo ratings yet
- Penggolongan Obat 1Document27 pagesPenggolongan Obat 1Dias Angga PerdanaNo ratings yet
- Pharmacotherapy of MigraineDocument74 pagesPharmacotherapy of MigraineAvin GupthaNo ratings yet
- Diagnosing and Managing MigrainesDocument41 pagesDiagnosing and Managing MigrainesmichaelwillsonNo ratings yet
- GenericsDocument1 pageGenericsvikasbansal227No ratings yet
- IMITREX (Sumatriptan Succinate) InjectionDocument22 pagesIMITREX (Sumatriptan Succinate) InjectionmulkideepakNo ratings yet
- Iron-rich foods for sickle cell anemiaDocument24 pagesIron-rich foods for sickle cell anemiaZyla MalinaoNo ratings yet
- Daftar Pustaka Case CephalgiaDocument3 pagesDaftar Pustaka Case Cephalgiakatherine rinovaNo ratings yet
- Jurnal SarafDocument20 pagesJurnal SarafAndreas NatanNo ratings yet
- GepantsDocument14 pagesGepantsmatheus galvãoNo ratings yet
- Instructions For Use of Disposable Sumatriptan Injection (Autoinjector)Document6 pagesInstructions For Use of Disposable Sumatriptan Injection (Autoinjector)Lina BuitragoNo ratings yet
- Response of Cluster Headache To Kudzu (Complete)Document15 pagesResponse of Cluster Headache To Kudzu (Complete)Andy RotsaertNo ratings yet
- Migraine-Headache Overview 2019Document11 pagesMigraine-Headache Overview 2019Yuri BrosgolNo ratings yet
- Department of Family Medicine Fpe Headache Syndrome: - Vanaveera Pandian SwethaDocument106 pagesDepartment of Family Medicine Fpe Headache Syndrome: - Vanaveera Pandian SwethaSuba Saravanan 12No ratings yet