Professional Documents
Culture Documents
Spinal Cord Injury
Uploaded by
cruz_johnraymondOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Spinal Cord Injury
Uploaded by
cruz_johnraymondCopyright:
Available Formats
SPINAL CORD INJURY
Definition, Etiology, Causative Factors
A spinal cord injury (SCI) refers to any injury to the spinal cord. Spinal cord injuries are most often traumatic, caused by lateral bending, dislocation, rotation, axial loading, and hyperflexion or hyperextension of the cord or cauda equina. Also, it can also be of a non-traumatic origin, as in the case of cancer, infection, intervertebral disc disease, vertebral injury and spinal cord vascular disease. The predominant risk factors for SCI include age, gender, and alcohol and drug use. Young people aged 16 to 30 suffer more than half of the new SCIs each year. SCI occurs almost four times more often in males than females. The most common cause of SCI is motor vehicle crashes, which account for 35% of the injuries. Violence-related injures account for nearly as many SCIs (30%), with falls causing 19% and sports-related injuries causing 8%. The vertebrae most frequently involved in SCI are the 5th, 6th, and 7th cervical (neck), the 12th thoracic, and the 1st lumbar vertebrae. These vertebrae are the most susceptible because there is a greater range of mobility in the vertebral column in these areas.
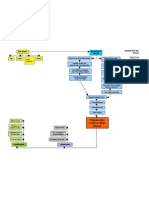
Pathophysiology Damage to the spinal cord ranges from transient concussion (from which the patient fully recovers) to contusion, laceration, and compression of the cord substance (either alone or in combination), to complete transection of the cord (which renders the patient paralyzed below the level of the injury). SCIs can be separated into two categories: primary injuries and secondary injuries. Primary injuries are the result of the initial insult or trauma and are usually permanent. Secondary injuries are usually the result of a contusion or tear injury, in which the nerve fibers begin to swell and disintegrate. A secondary chain of events produces ischemia, hypoxia, edema, and hemorrhagic lesions, which in turn result in destruction of myelin and axons. These secondary reactions, believed to be the principal causes of spinal cord degeneration at the level of injury, are now thought to be reversible 4 to 6 hours after injury. Therefore, if the cord has not suffered irreparable damage, some method of early treatment is needed to prevent partial damage from developing into total and permanent damage. Signs and Symptoms
Manifestations depend on the type and level of injury. The type of injury refers to the extent of injury to the spinal cord itself. Incomplete spinal cord lesions are classified according to the area of spinal cord damage: central, lateral, anterior, or posterior. A complete spinal cord lesion can result in paraplegia (paralysis of the lower body) or quadriplegia (paralysis of all four extremities).
Incomplete Spinal Cord Lesions Central Cord Syndrome Characteristics: Motor deficits (in the upper extremities compared to the lower extremities; sensory loss varies but is more pronounced in the upper extremities); bowel/bladder dysfunction is variable, or function may be completely preserved. Cause: Injury or edema of the central cord, usually of the cervical area.
Anterior Cord Syndrome Characteristics: Loss of pain, temperature, and motor function is noted below the level of the lesion; light touch, position, and vibration sensation remain intact. Cause: The syndrome may be caused by acute disk herniation or hyperflexion injuries associated with fracture-dislocation of vertebra. It also may occur as a result of injury to the anterior spinal artery, which supplies the anterior two thirds of the spinal cord. Brown-Sequard Syndrome (Lateral Cord Syndrome) Characteristics: Ipsilateral paralysis or paresis is noted, together with ipsilateral loss of touch, pressure, and vibration and contralateral loss of pain and temperature. Cause: The lesion is caused by a transverse hemisection of the cord (half of the cord is transected from north to south), usually as a result of a knife or missile injury, fracturedislocation of a unilateral articular process, or possibly an acute ruptured disk. Posterior Cord Syndrome Posterior cord syndrome can also occur, but is very rare. Damage to the posterior portion of the spinal cord and/or interruption to the posterior spinal artery causes the loss of proprioception and epicritic sensation (e.g.: stereognosis, graphesthesia) below the level of injury. Motor function, sense of pain, and sensitivity to light touch remain intact.
Complete Spinal Cord Lesions Cervical Level Cervical (neck) injuries usually result in full or partial tetraplegia (Quadriplegia). However, depending on the specific location and severity of trauma, limited function may be retained.
Injuries at the C-1/C-2 levels will often result in loss of breathing, necessitating mechanical ventilators or phrenic nerve pacing. C3 vertebrae and above : Typically results in loss of diaphragm function, necessitating the use of a ventilator for breathing. C4 : Results in significant loss of function at the biceps and shoulders. C5 : Results in potential loss of function at the shoulders and biceps, and complete
loss of function at the wrists and hands.
C6 : Results in limited wrist control, and complete loss of hand function. C7 and T1 : Results in lack of dexterity in the hands and fingers, but allows for limited use of arms.
Patients with complete injuries above C7 typically cannot handle activities of daily living and cannot function independently. Additional signs and symptoms of cervical injuries include:
Inability or reduced ability to regulate heart rate, blood pressure, sweating and hence body temperature. Autonomic dysreflexia or abnormal increases in blood pressure, sweating, and other autonomic responses to pain or sensory disturbances.
Thoracic Level
Complete injuries at or below the thoracic spinal levels result in paraplegia. Functions of the hands, arms, neck, and breathing are usually not affected.
T1 to T8: Results in the inability to control the abdominal muscles. Accordingly, trunk stability is affected. The lower the level of injury, the less severe the effects. T9 to T12: Results in partial loss of trunk and abdominal muscle control.
Lumbosacral The effects of injuries to the lumbar or sacral regions of the spinal cord are decreased control of the legs and hips, urinary system, and anus.
Bowel and bladder function is regulated by the sacral region of the spine. In that regard, it is very common to experience dysfunction of the bowel and bladder, including infections of the bladder and anal incontinence, after traumatic injury. Sexual function is also associated with the sacral spinal segments, and is often affected after injury. During apsychogenic sexual experience, signals from the brain are sent to the sacral parasympathetic cell bodies at spinal levels S2-S4 and in case of men, are then relayed to the penis where they trigger an erection. A spinal cord lesion of descending fibers to levels S2-S4 could, therefore, potentially result in the loss of psychogenic erection. A reflexogenic erection, on the other hand, occurs as a result of direct physical contact to the penis or other erotic areas such as the ears, nipples or neck, and thus not involving descending fibers from the brain. A reflex erection is involuntary and can occur without sexually stimulating thoughts. The nerves that control a man's ability to have a reflex erection are located in the sacral nerves (S2-S4) of the spinal cord and could be affected after a spinal cord injury at this level.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Drug StudyDocument14 pagesDrug Studycruz_johnraymond100% (1)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Philippine College of Physicians Daily Census Ward Hospital de Los Santos-Sti Medical CenterDocument22 pagesPhilippine College of Physicians Daily Census Ward Hospital de Los Santos-Sti Medical Centercruz_johnraymondNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Chapter VIII CDXDocument25 pagesChapter VIII CDXcruz_johnraymondNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Incomplete Abortion Causes and TreatmentDocument3 pagesIncomplete Abortion Causes and Treatmentcruz_johnraymondNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- DEFIBRILLATORDocument3 pagesDEFIBRILLATORcruz_johnraymondNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Book Review QuestionsDocument4 pagesBook Review Questionscruz_johnraymondNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- 2ERDocument3 pages2ERcruz_johnraymondNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Case Pres Drugs-CruzDocument7 pagesCase Pres Drugs-Cruzcruz_johnraymondNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Philosophy OF MAN - NumerologyDocument34 pagesPhilosophy OF MAN - Numerologycruz_johnraymond0% (1)
- In Another Country Plot SummeryDocument4 pagesIn Another Country Plot Summerysubto100% (2)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Cerebral ContusionDocument88 pagesCerebral ContusionHeaNo ratings yet
- Week#1 AphroditeDocument4 pagesWeek#1 AphroditeFrancisco Javier González GNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- H's and T's of ACLS: A Guide to Differential DiagnosisDocument4 pagesH's and T's of ACLS: A Guide to Differential DiagnosisAnusha Verghese100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Harry Potter Spell ListDocument4 pagesHarry Potter Spell ListEriss RefuerzoNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Adial Orearm Lap: Tor ChiuDocument5 pagesAdial Orearm Lap: Tor ChiuAlNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Netball RulesDocument24 pagesNetball RulesJasmineTeongNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Doberman Pinscher Breed StandardsDocument4 pagesDoberman Pinscher Breed StandardsMorgan Rai LoweNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- MUHS - BPT - 2016 - 4 - Summer - B.P.TH - 51411 Musculoskeletal PhysiotherapyDocument2 pagesMUHS - BPT - 2016 - 4 - Summer - B.P.TH - 51411 Musculoskeletal PhysiotherapyYuvraj AtholeNo ratings yet
- Instruction Manual Guide D'Utilisation Manual de InstruccionesDocument68 pagesInstruction Manual Guide D'Utilisation Manual de InstruccioneslanzeaNo ratings yet
- TCM Patterns Explained: Toxic Heat, Phlegm, Stasis, DeficiencyDocument14 pagesTCM Patterns Explained: Toxic Heat, Phlegm, Stasis, DeficiencyCarleta Stan100% (1)
- CVA620Document80 pagesCVA620Emi DNo ratings yet
- Anatomy II LabDocument48 pagesAnatomy II LabAddicted Outaku اوتاكوNo ratings yet
- Spanish SquatDocument7 pagesSpanish Squatapi-551757456No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Mandibular Nerve BlocksDocument4 pagesMandibular Nerve BlocksNafyiza BaNo ratings yet
- HIRA Fabrication WorkshopDocument316 pagesHIRA Fabrication WorkshopChethan100% (1)
- Snapping Knee Caused by The Gracilis Tendon: A Case Report With An Anatomical StudyDocument5 pagesSnapping Knee Caused by The Gracilis Tendon: A Case Report With An Anatomical StudyDavid BertossiNo ratings yet
- Niel - Camorongan - Project Proposal - First AidawarenessDocument2 pagesNiel - Camorongan - Project Proposal - First AidawarenessJuvielyn JuanNo ratings yet
- ABC TraumaDocument27 pagesABC TraumarikarzNo ratings yet
- Weatherby Vanguard Bolt Action RifleDocument22 pagesWeatherby Vanguard Bolt Action RifleJon MorenoNo ratings yet
- Club Foot CtevDocument82 pagesClub Foot CtevtuyulgaulNo ratings yet
- Magee 6th Edition - OPA - Table of ContentsDocument4 pagesMagee 6th Edition - OPA - Table of ContentsRonny Araya AbarcaNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Multi-Specialty Trauma Management GuideDocument163 pagesMulti-Specialty Trauma Management Guideizwan taufikNo ratings yet
- Liston's forgotten splintDocument4 pagesListon's forgotten splintPriyank GuptaNo ratings yet
- Étude Du Centre de Traitement Des Lésions Cérébrales de L'université de DalhousieDocument41 pagesÉtude Du Centre de Traitement Des Lésions Cérébrales de L'université de DalhousieRadio-Canada100% (2)
- Ling Wu Case NotesDocument3 pagesLing Wu Case NotesOana Maria Grigore77% (13)
- Trestles and StagingDocument2 pagesTrestles and Stagingdak comeiNo ratings yet
- Posterior Tibialis Tendonitis StudyDocument6 pagesPosterior Tibialis Tendonitis StudyShane WetzelNo ratings yet
- Degenerative Disc Disease Concept MapDocument1 pageDegenerative Disc Disease Concept MapashleydeanNo ratings yet
- Meniscus TearsDocument29 pagesMeniscus Tearsmaulana ilhamNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)