Professional Documents
Culture Documents
Gender Differences in Ischemic Heart Disease: Ryotaro Wake and Minoru Yoshiyama
Uploaded by
Chirag ParmarOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gender Differences in Ischemic Heart Disease: Ryotaro Wake and Minoru Yoshiyama
Uploaded by
Chirag ParmarCopyright:
Available Formats
234
Recent Patents on Cardiovascular Drug Discovery, 2009, 4, 234-240
Gender Differences in Ischemic Heart Disease
Ryotaro Wake* and Minoru Yoshiyama
Department of Internal Medicine and Cardiology, Osaka City University, Graduate School of Medicine, Osaka, Japan
Received: January 12, 2009; Accepted: February 13, 2009; Revised: May 4, 2009
Abstract: Coronary artery disease (CAD) is a leading cause of mortality and morbidity in most developed countries. Gender-related differences have been found in the presentation, prevalence, and clinical outcomes of CAD in many studies. Compared to women, men present with ST-segment elevation myocardial infarction more often and have a higher prevalence of CAD. These findings indicate that gender may have an important influence on CAD. Appropriate diagnosis, prevention, recent patent inventions, and treatment will improve the care of all patients. It is therefore necessary to consider the differences in the features of ischemic heart disease between men and women when examining patients. Novel drugs for tailor-made therapy based on gender differences should be developed for the treatment of CAD in future.
Keywords: Coronary Artery Disease (CAD), gender difference, ischemic heart disease, risk factor, noninvasive testing, prevention & treatment. INTRODUCTION Coronary artery disease (CAD) is a leading cause of mortality and morbidity in most developed countries [1]. Many studies have found gender-related differences in the presentations, prevalence, and clinical outcomes of CAD [24]. CAD first presents itself in women approximately 10 years later than in men, most commonly after menopause [5]. Compared to women, men present with ST-segment elevation myocardial infarction (MI) more often and have a higher prevalence of CAD adjusted for age [6, 7]. However, younger women experience more adverse outcomes after MI and coronary artery bypass grafting surgery than men [8]. A greater proportion of women than men with MI die of sudden cardiac arrest before reaching hospital [3, 9]. Previous reports have shown a 20% reduction in total mortality among patients randomized to exercise-based cardiac rehabilitation compared with controls receiving usual care [10]. The outcome was however similar between men and women, although only 20% of all participants were women in many reports. Women are less likely than men to participate in cardiac rehabilitation after acute MI [10]. Next, he prevalence of microvascular angina is higher in women than men. Takotsubo cardiomyopathy is more prevalent in women than in men [11]. These findings indicate that gender difference may have an important influence on cardiovascular physiology and pathology [12, 13]. In many developing countries, a large budget is expended for the treatment of CAD, and it is necessary to minimize the influence of risk factors. The burden of CAD on women and the global economy will continue to increase [5]. In addition to population-based and macroeconomic interventions, interventions in individual patients are key to reducing the
*Address correspondence to this author at the Department of Internal Medicine and Cardiology, Osaka City University, Graduate School of Medicine, Osaka, Japan; 1-4-3 Asahi-machi, Abeno-ku, Osaka, 545-8585, Japan; Tel: +81-79-272-8555; Fax: +81-79-272-8550; E-mail: ryotaro_wake@yahoo.co.jp 1574-8901/09 $100.00+.00
incidence of CAD globally [14]. Prevention of CAD is paramount to the health of every woman and every nation. There have been numerous clinical trials that have a bearing on CAD prevention in women [15]. Women (XX) and men (XY) differ in their genetic complement by a single chromosome out of the 46 that are present in the human species. However, this single chromosomal difference affects both the expression of disease and the psychosocial and behavioral characteristics and work environments of individuals, which may reduce or increase the susceptibility to cardiovascular diseases. In future, novel drugs for tailor-made therapy of CAD based on gender differences may be developed. This review discusses gender differences in the features of ischemic heart disease and the possibilities of future developments in treatments. CLINICAL RISK FACTORS ARTERY DISEASE IN WOMEN OF CORONARY
It is important to classify women as being at high, intermediate, or low risk for CAD. Classification may be based on clinical criteria and the Framingham global risk score [16]. A woman found to have coronary calcification or increased carotid intimal thickness may be at low risk for CAD on the basis of the Framingham risk score, but she may be actually at intermediate or high risk for a future CAD event. We should take several factors into consideration, including medical and lifestyle histories, Framingham risk score, family history of CAD, and other genetic conditions (e.g., familial hypercholesterolemia), since these affect the decisions about the aggressiveness of preventive therapy. Novel CAD risk factors (e.g., high-sensitivity C-reactive protein [17]) and novel screening technologies (e.g., coronary calcium scoring) should help guide preventive interventions. Further research is needed on the benefits, risks, and costs associated with such strategies. There are
2009 Bentham Science Publishers Ltd.
Gender Differences in Ischemic Heart Disease
Recent Patents on Cardiovascular Drug Discovery, 2009, Vol. 4, No. 3
235
many unique opportunities for early detection of CAD in women; for example, in pregnancy, preeclampsia may be an early indicator of CAD risk [18, 19]. In addition, maternal placental syndromes in combination with traditional cardiovascular risk factors, such as prepregnancy hypertension or diabetes mellitus, obesity, dyslipidemia, and metabolic syndrome, may be additive in defining CAD risk in women [18]. Future research should evaluate the potential for events or medical contact during unique phases in a womans life, such as adolescence, pregnancy, and menopause, to identify women at high risk, and determine the effectiveness of preventive interventions during critical periods. The diagnosis of CAD in women presents challenges not observed in case of men. Differences in the epidemiology of CAD between men and women show that women are generally at a lower risk than their male counterparts until the seventh decade of life. For both asymptomatic and symptomatic women, the choice of initial test is guided by classification into low, intermediate, or high pretest risk categories. Asymptomatic intermediate-risk women have lower event rates. In symptomatic women, noninvasive diagnostic studies (exercise ECG and cardiac imaging studies) are recommended for those who are at an intermediate to high pretest likelihood of CAD [20]. Therapeutic decisionmaking is guided by the extent and severity of inducible ischemia. Thus, referral of low-likelihood women (for example, premenopausal women with less than one risk factor and nonanginal/atypical symptoms) will be associated with a high rate of false positives. Smoking is an important risk factor for vascular diseases. Vascular disease risk was most quickly reduced by cessation of smoking compared with other associated factors. The beneficial effect of quitting on the risk for death from CHD was realized within 5 years, whereas the risks for death from chronic obstructive pulmonary disease and lung cancer did not approach those of women who had never smoked until the age of 20 and 30 years, respectively [21]. It may never be
Table 1. Effect of Estrogen on Atherosclerosis
Favorable Lipids LDL-cholesterol HDL-cholesterol Coagulation Fibrinolysis Inflammation Adhesion Endothelial Function Blood Pressure ACE activity Nitric oxide Endothelin-1 Plasminogen 12 PAI-1 Fibrinogen Adhesion molecules
too late for women to quit smoking in order to reduce the risk for vascular diseases. A blood pressure-lowering treatment provided similar protection against major cardiovascular events in men and women [22]. FEATURES OF CORONARY ARTERY PATHOLOGY IN WOMEN Men have a greater burden of atheroma and eccentric atheroma in coronary arteries compared to women. A study reported that plaque rupture in patients with sudden coronary death was more frequent in men than in women [23]. Men have more severe structural and functional abnormalities in the epicardial coronary arteries than women. These factors may influence the higher incidence rates of CAD and ST-segment MI in men compared to women. With regard to the lower cardiac event rate in female patients, several mechanisms have been proposed to explain the cardioprotective effect of sex hormones in women [12]. We show the effect of sex hormones in ischemic heart disease in Table 1. Women had lower rates of obstructive CAD at angiography when evaluated for symptoms suggestive of myocardial ischemia [24]. Among angiographic CAD patients, atheroma volume in women is less than that in men, despite the presence of more cardiovascular risk factors in women. Women had slightly lower coronary vasodilator reserve even with normal coronary angiographic results [25]. Endothelialindependent microvascular dysfunction was an independent predictor of adverse outcomes in patients with mild CAD [26]. It has been suggested that the mechanism of myocardial ischemia in women may be localized to the microvascular coronary arteries and that abnormal micro-vascular function may have prognostic implications [27]. Takotsubo cardiomyopathy is more prevalent in women than in men. Because the onset of this syndrome is often
Unfavorable Trigriceride
Factor VII AT III CRP
Angiotensinogen
VSMC migration, proliferation
PAI-1: Plasminogen Activator Inhibitor-1, AT III: Antithrombin III, ACE: Angiotensinogen Converting Enzyme, VSMC: Vascular Smooth Muscle Cell.
236 Recent Patents on Cardiovascular Drug Discovery, 2009, Vol. 4, No. 3
Wake and Yoshiyama
preceded by emotional or physical stress, catecholaminemediated multivessel epicardial spasm, microvascular coronary spasm, or possible direct catecholamine-mediated myocyte injury have been advocated as possible pathophysiological mechanisms [11]. DIAGNOSIS AND PROGNOSIS Electrocardiography Changes in electrocardiography (ECG) during exercise have been reported to be of diminished accuracy in women as a result of more frequent changes in resting ST-T wave, lower ECG voltage, and hormonal factors such as endogenous estrogen in premenopausal women and hormone replacement therapy in postmenopausal women [28-30]. In a meta-analysis of exercise ECG studies in women, sensitivity was 61% and specificity was 70%, compared to 72% and 77%, respectively, in men [20]. From a cohort of symptomatic women who were referred for exercise treadmill testing followed by coronary angiography, significant coronary stenosis (more than 75%) was observed in 19%, 35%, and 89% of low-, moderate-, and high-risk women, respectively, based on Duke treadmill score risk categories [31]. Maximal exercise capacity and heart rate recovery measurements can aid in estimation of near- and long-term outcome in large cohorts of women [32]. Recent reports have noted that a simple measure such as heart rate recovery (at 1 or 2 min after exercise) have substantial prognostic value. Women engage less often in physical exercise programs, have lower functional capacity, and show a greater functional decline during their menopausal years. Because of their lower work capacity on exercise tests (on average 5-7 min) as a result of premature peripheral fatigue, it is difficult to provoke myocardial ischemia [33]. Women who exercise less than 5 metabolic equivalents (METs) are at an increased risk for death [34]. Women expected to perform less than 5 METs may be better evaluated by pharmacological stress imaging. However, women who have inducible ischemia at low workloads (less than 5 METs) have a higher likelihood of obstructive CAD and may be referred for coronary angiography. The exercise ECG test has a high negative predictive value in women with a low pretest probability of CAD and a low-risk Duke treadmill score [20]. The diagnostic and prognostic accuracy of the exercise ECG stress test in symptomatic women with suspected CAD is increased by the inclusion of additional parameters in the interpretation of the ST-segment response to exercise. Echocardiography Stress echocardiography can provide information about the presence of left ventricular systolic or diastolic dysfunction, valvular heart disease, and the extent of infarction and stress-induced ischemia. Exercise echocardiography may be performed with a treadmill or by supine or upright bicycle exercise. Exercise stress echocardiography is a physiological investigation and the most widely available method for evaluation of CAD. However, exercise capacity is often impaired in aged or diabetic patients and the workload
required to produce stress-induced myocardial ischemia might not be achieved by such patients. Stress echocardiography provides significantly higher specificity and accuracy than the standard exercise ECG testing in women [35]. Stress echocardiography has demonstrated good diagnostic accuracy for detecting or excluding significant CAD, with a mean sensitivity of 81%, specificity of 86%, and an overall accuracy of 84% [35-38]. There appears to be no significant effect of gender on the diagnostic accuracy of exercise echocardiography. A study of dobutamine stress echocardiography (DSE) revealed an overall sensitivity of 80% and specificity of 84% [36]. Similar to exercise stress echocardiography, DSE appears to have similar diagnostic accuracy in detecting CAD in both women and men. Cardiac events occur less frequently in women than in men. This difference is compatible with the lower prevalence and lesser sensitivity of detection of CAD in women compared to men. No gender differences have been reported in the prognostic value of exercise stress echocardiography in a large population. The low specificity of exercise ECG testing in women, especially in young and middle-aged women, may lead to a higher rate of unnecessary angiography and higher expense, particularly if stress imaging is not used before coronary angiography in a sequential testing strategy. Stress echocardiography with exercise or dobutamine is an effective and highly accurate noninvasive means of detecting ischemic heart disease and risk-stratifying symptomatic women with an intermediate to high pretest likelihood of CAD. Stress echocardiography provides incremental value over exercise ECG and clinical variables in women with suspected or known coronary heart disease. Stress echocardiography is recommended for symptomatic women with an intermediate or high pretest probability of CAD (women with suspected CAD must also have an abnormal resting ECG). Previous reports demonstrated that pharmacological stress echocardiography provides independent prognostic information in both men and women [39, 40]. Myocardial Perfusion Gated myocardial perfusion single-photon emission computed tomography (SPECT) is a nuclear-based technique that provides a combination of test elements that are used to diagnose and risk-stratify women. Myocardial perfusion imaging, however, has been reported to have technical limitations in women, including false-positive results due to breast attenuation and small left ventricular chamber size [41]. The accuracy of 201Tl SPECT imaging, for example, is reduced in patients with small hearts, and these patients are more likely to be women than men. When 201Tl is used as the radioisotope in women, false-positive test results may occur due to soft tissue attenuation (e.g., breast attenuation) in the anterior and anterolateral segments [41].
Gender Differences in Ischemic Heart Disease
Recent Patents on Cardiovascular Drug Discovery, 2009, Vol. 4, No. 3
237
For women, the lower-energy isotope 201Tl has been largely supplanted by technetium-based imaging agents that improve accuracy. In comparing the diagnostic accuracy of 201Tl with gated 99mTc-sestamibi SPECT in women, the sensitivity for detecting CAD was 80%, and test specificity improved dramatically from 67% for 201Tl to 92% for gated 99mTc-sestamibi SPECT [42]. Pharmacological stress SPECT also merits consideration, given the higher incidence of decreased exercise capacity and advanced age for women, as discussed previously [41, 43]. Vasodilator pharmacological stress perfusion imaging has been shown to be more accurate than exercise perfusion imaging in identification of CAD in both men and women with left bundle-branch block [43]. Adenosine 99mTcsestamibi imaging was reported to have 91% sensitivity and 86% specificity for detecting significant coronary artery stenoses of more than 50% [44]. Myocardial perfusion imaging has powerful predictive value with regard to the development of subsequent cardiac death or MI or the need for coronary revascularization [4547], regardless of sex [33]. Prognosis worsens commensurate with the number of vascular territories involved, with 3-year survival rates ranging from 99% for women without ischemia to 85% in women who had three-vessel ischemia [33]. In addition, pharmacological stress was recently shown to be effective in the risk stratification of diabetic women with suspected and known CAD. The CAD mortality for nondiabetic women with a moderately abnormal scan was 2.8% compared with 4.1% in diabetic women [45]. Cardiac Computed Tomography The diagnostic accuracy of coronary computed tomography (CT) angiography is not greater than that of invasive coronary angiography. Although the risk of adverse events for invasive coronary angiography is generally considered to be low, significant and potential life-threatening complications can arise, including not only coronary artery dissection, but also arrhythmia, stroke, hemorrhage, MI, and death [48]. The negative predictive value at the patient and vessel levels establishes coronary CT angiography as an effective non-invasive alternative to invasive coronary angiography in ruling out obstructive coronary artery stenosis. New generation 64-MDCT systems permit acquisition of cardiac studies in less than 10s, allowing faster contrast injection rates and lower contrast volume requirements, and reducing the number of artifacts related to inadequate breathholding and heart rate variability [49, 50]. Cardiac CT detects and quantifies the amount of coronary artery calcium (CAC), a marker of atherosclerotic disease burden. Calcification does not occur in a normal vessel wall; it therefore indicates the presence of atherosclerosis, but is not specific for luminal obstruction. CAC scores approximate the total atherosclerotic plaque burden. However, the absence of detectable CAC has a negative predictive value of 100%. Although these findings are consistent with the concept that the calcified plaque burden
parallels the overall plaque burden, CAC testing is not appropriate as an alternative for angiographic disease detection because of the modest relationship between CAC and obstructive CAD [50]. The greatest potential for CAC detection could be as a marker for CAD prognosis in asymptomatic women. The presence and severity of CAC has independent and incremental value when added to clinical or historical data in the estimation of death or nonfatal MI [51, 52]. In case of women, risk-adjusted relative risk ratios for all-cause mortality were elevated 2.5-, 3.7-, 6.3-, and 12.3fold for calcium scores of 11-100, 101-400, 401-1000, and > 1000, respectively (P < 0.0001), compared with a score of < 10. CAC testing for CAD risk detection should be limited to clinically selected women at an intermediate risk for CAD. Cardiovascular Magnetic Resonance Imaging Cardiovascular magnetic resonance imaging (CMR) has the potential to evaluate the presence of CAD by multiple techniques, including direct visualization of coronary stenoses [53] (analogous to conventional catheter-driven coronary angiography) [54]; evaluation of myocardial perfusion [55, 56] and metabolism [57] (similar to SPECT imaging); assessment of abnormal wall motion during stress [58] (similar to echocardiography); and identification of infarcted myocardium by delayed hyperenhancement imaging [59]. Myocardial perfusion techniques demonstrate abnormalities of myocardial metabolism and perfusion in women with syndrome X (i.e., chest pain in the absence of significant epicardial CAD). Prognostic data with CMR have recently become available and suggest that this technique is accurate for estimating risk. TREATMENT Studies have shown that percutaneous coronary intervention (PCI) is a more effective reperfusion strategy for acute coronary syndrome than intravenous thrombolysis [60]. The advantage of primary PCI over thrombolytic therapy was greater for women than men [61]. Primary PCI reduced the risk of intracranial bleeding and improved survival in women [62]. Mortality from acute MI (AMI) was higher in women than in men, consistent with the results of most previous studies [61, 63, 64]. This poorer outcome in women was likely related to the facts that compared to men, women with AMI were older, underwent PCI less frequently, and had higher incidences of coronary risk factors, such as hyperlipidemia, diabetes mellitus, and hypertension. The use of a drug-eluting stent makes the outcome after PCI better than that after the use of a bare metal stent. There is no difference between men and women in the outcome [65]. On the other hand, the most important benefit of PCI in chronic stable CAD may be the relief of symptoms [66]. Statin therapy is effective for chronic stable CAD [67].
238 Recent Patents on Cardiovascular Drug Discovery, 2009, Vol. 4, No. 3
Wake and Yoshiyama
Women experience more bleeding than men with antiplatelet therapy and/or anticoagulant therapy as they often have a smaller body size, resulting in excessive dosing. These agents should be used with regard to the patients body size [68]. In a primary prevention trial in women, aspirin lowered the risk of stroke without affecting the risk of MI. On the other hand, in men, aspirin lowered the risk of MI without affecting the risk of stroke [69, 70]. Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers for blood pressure control are contraindicated in women contemplating pregnancy and in those who are pregnant. The perception of the risks and benefits of hormone replacement therapy (HRT) and the time when the therapy should be initiated has changed dramatically since the publication of the Womens Health Initiative trial in 2002. This study of women in whom HRT was initiated on average 13 years after menopause did not reveal long-term benefits for cardiovascular outcomes [71]. However, combined HRT started many years after menopause can improve healthrelated quality of life [72]. Reports show 20% reduction in total mortality among patients randomized to exercise-based cardiac rehabilitation compared with controls receiving usual care. The outcome is similar between men and women, although only 20% of all participants were women in many reports. Women are less likely than men to participate in cardiac rehabilitation after acute MI [10]. This may be one reason for the poor outcome in women with AMI. Cardiac rehabilitation should be recommended to more women after AMI. RECENT PATENTS A recent invention is based on the discovery of genetic polymorphisms that are associated with MI. The invention relates to nucleic acid molecules containing the polymorphisms, variant proteins encoded by such nucleic acid molecules, reagents for detecting the polymorphic nucleic acid molecules and proteins, methods of using the nucleic acid and proteins, and methods of using reagents for their detection [73]. It identifies humans with an increased risk for developing recurrent MI based on the evaluation of nucleic acid samples for the presence or absence of a singlenucleotide polymorphism (SNP) at position 101 of SEQ ID NO: 21398 or its complement. The presence of at least one G allele at the SNP identifies the human as having an increased risk for recurrent MI compared with a human with two A alleles at the SNP. A recent large population study showed that the gene is associated with acute coronary syndrome [74]. Methods for the diagnosis and evaluation of acute coronary syndromes were disclosed in a patent. Patient test samples were analyzed for the presence and amounts of members of a panel of markers comprising one or more specific markers for myocardial injury and one or more nonspecific markers for myocardial injury. The patent covers a variety of markers for assembling a panel of markers for such diagnosis and evaluation. The invention provides methods for early detection and differentiation of stable angina, unstable angina, and MI. It includes methods to
provide rapid, sensitive, and specific assays that can greatly increase the number of patients who can receive beneficial treatment and therapy, reduce the costs associated with incorrect diagnosis, and provide important information about the prognosis of the patient [75]. Another patent describes a method for in vitro diagnosis and/or risk stratification of an adverse event in post-MI patients by means of proADM. The method includes determination of the marker pro-adrenomedullin or a partial sequence or fragment of it or a sequence contained in a marker combination (panel, cluster) in a post-MI patient. The patent covers the step of determining the level of proadrenomedullin or partial peptides or fragments of them from a post-MI patient; a significantly elevated level of proadrenomedullin correlates with a greater risk of an adverse event in the patient [76]. Another significant disclosure provides methods for diagnosing and/or treating subjects who either have or are at a risk for developing acute coronary syndrome. The invention also provides isolated nucleotide sequences and arrays comprising nucleotide sequences that may be used for the treatment and/or diagnosis of subjects who either have or are at a risk for developing acute coronary syndrome [77]. CONCLUSIONS Appropriate diagnosis, prevention, and treatment will improve the care of all CAD patients. Since there are gender differences in ischemic heart disease, it is necessary to consider these differences when examining men and women with ischemic heart disease. CURRENT & FUTURE DEVELOPMENTS We have found many gender differences in CAD. The development of novel drugs and therapeutic methods for tailor-made therapy of CAD based on gender differences is required. ACKNOWLEDGEMENTS None declared. CONFLICT OF INTEREST There is no conflict of interest. REFERENCES
[1] Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics - 2007 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2007; 115(5): e69-e171. Bairey Merz CN, Shaw LJ, Reis SE, et al. Insights from the NHLBI - Sponsored Women's Ischemia Syndrome Evaluation (WISE) Study. Part II: Gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol 2006; 47(3): S21-S29. Shaw LJ, Bairey Merz CN, Pepine CJ, et al. Insights from the NHLBI-Sponsored Women's Ischemia Syndrome Evaluation (WISE) Study. Part I: Gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J Am Coll Cardiol 2006; 47(3): S4-S20.
[2]
[3]
Gender Differences in Ischemic Heart Disease [4] Wake R, Takeuchi M, Yoshikawa J, Yoshiyama M. Effects of gender on prognosis of patients with known or suspected coronary artery disease undergoing contrast-enhanced dobutamine stress echocardiography. Circ J 2007; 71(7): 1060-1066. Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases. Part I: General considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001; 104(22): 2746-2753. Heer T, Schiele R, Schneider S, et al. Gender differences in acute myocardial infarction in the era of reperfusion (the MITRA registry). Am J Cardiol 2002; 89(5): 511-517. Kosuge M, Kimura K, Ishikawa T, et al. Differences between men and women in terms of clinical features of ST-segment elevation acute myocardial infarction. Circ J 2006; 70(3): 222-226. Vaccarino V, Abramson JL, Veledar E, Weintraub WS. Sex differences in hospital mortality after coronary artery bypass surgery: Evidence for a higher mortality in younger women. Circulation 2002; 105(10): 1176-1181. Thom T, Haase N, Rosamond W, et al. Heart disease and stroke statistics - 2006 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2006; 113(6): e85-e151. Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: Systematic review and meta-analysis of randomized controlled trials. Am J Med 2004; 116(10): 682-692. Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005; 352(6): 539-548. Mendelsohn ME, Karas RH. Molecular and cellular basis of cardiovascular gender differences. Science 2005; 308(5728): 15831587. Pepine CJ. Ischemic heart disease in women: Facts and wishful thinking. J Am Coll Cardiol 2004; 43(10): 1727-1730. Strong K, Mathers C, Leeder S, Beaglehole R. Preventing chronic diseases: How many lives can we save? Lancet 2005; 366(9496): 1578-1582. Kotseva K, Wood D, De Backer G, De Bacquer D, Pyorala K, Keil U. Cardiovascular prevention guidelines in daily practice: A comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet 2009; 373(9667): 929-940. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002; 106(25): 3143-3421. Ridker PM, Danielson E, Fonseca FA, et al. Reduction in Creactive protein and LDL cholesterol and cardiovascular event rates after initiation of rosuvastatin: A prospective study of the JUPITER trial. Lancet 2009; 373(9670): 1175-1182. Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA. Cardiovascular health after maternal placental syndromes (CHAMPS): Population-based retrospective cohort study. Lancet 2005; 366(9499): 1797-1803. Wilson BJ, Watson MS, Prescott GJ, et al. Hypertensive diseases of pregnancy and risk of hypertension and stroke in later life: Results from cohort study. BMJ 2003; 326(7394): 845. Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: Summary article: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation 2002; 106(14): 18831892. Kenfield SA, Stampfer MJ, Rosner BA, Colditz GA. Smoking and smoking cessation in relation to mortality in women. JAMA 2008; 299(17): 2037-2047. Turnbull F, Woodward M, Neal B, et al. Do men and women respond differently to blood pressure-lowering treatment? Results of prospectively designed overviews of randomized trials. Eur Heart J 2008; 29(21): 2669-2680. Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from sudden coronary death: A comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol 2000; 20(5): 1262-1275. Sharaf BL, Pepine CJ, Kerensky RA, et al. Detailed angiographic analysis of women with suspected ischemic chest pain (pilot phase data from the NHLBI-sponsored Women's Ischemia Syndrome
Recent Patents on Cardiovascular Drug Discovery, 2009, Vol. 4, No. 3
239
[25]
[5]
[26]
[6]
[27]
[7] [8]
[28]
[9]
[29]
[10]
[30]
[11]
[31]
[12] [13] [14]
[32]
[33]
[15]
[34] [35]
[16]
[17]
[18]
[36] [37]
[19] [20]
[38]
[39]
[21]
[40]
[22]
[41]
[23]
[42]
[24]
Evaluation [WISE] Study Angiographic Core Laboratory). Am J Cardiol 2001; 87(8): 937-941. Kern MJ, Bach RG, Mechem CJ, et al. Variations in normal coronary vasodilatory reserve stratified by artery, gender, heart transplantation and coronary artery disease. J Am Coll Cardiol 1996; 28(5): 1154-1160. Britten MB, Zeiher AM, Schachinger V. Microvascular dysfunction in angiographically normal or mildly diseased coronary arteries predicts adverse cardiovascular long-term outcome. Coron Artery Dis 2004; 15(5): 259-264. Johnson BD, Shaw LJ, Buchthal SD, et al. Prognosis in women with myocardial ischemia in the absence of obstructive coronary disease: Results from the National Institutes of Health-National Heart, Lung, and Blood Institute-Sponsored Women's Ischemia Syndrome Evaluation (WISE). Circulation 2004; 109(24): 29932999. Rosano GM, Webb CM, Chierchia S, et al. Natural progesterone, but not medroxyprogesterone acetate, enhances the beneficial effect of estrogen on exercise-induced myocardial ischemia in postmenopausal women. J Am Coll Cardiol 2000; 36(7): 2154-2159. Schulman SP, Thiemann DR, Ouyang P, et al. Effects of acute hormone therapy on recurrent ischemia in postmenopausal women with unstable angina. J Am Coll Cardiol 2002; 39(2): 231-237. Waters DD, Gordon D, Rossouw JE, et al. Women's Ischemic Syndrome Evaluation: Current status and future research directions: report of the National Heart, Lung and Blood Institute workshop: October 2-4, 2002. Section 4: Lessons from hormone replacement trials. Circulation 2004; 109(6): e53-e55. Alexander KP, Shaw LJ, Shaw LK, Delong ER, Mark DB, Peterson ED. Value of exercise treadmill testing in women. J Am Coll Cardiol 1998; 32(6): 1657-1664. Mora S, Redberg RF, Cui Y, et al. Ability of exercise testing to predict cardiovascular and all-cause death in asymptomatic women: A 20-year follow-up of the lipid research clinics prevalence study. JAMA 2003; 290(12): 1600-1607. Marwick TH, Shaw LJ, Lauer MS, et al. The noninvasive prediction of cardiac mortality in men and women with known or suspected coronary artery disease. Economics of Noninvasive Diagnosis (END) Study Group. Am J Med 1999; 106(2): 172-178. Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief selfadministered questionnaire to determine functional capacity (the Duke Activity Status Index). Am J Cardiol 1989; 64(10): 651-654. Cheitlin MD, Armstrong WF, Aurigemma GP, et al. ACC/AHA/ ASE 2003 guideline update for the clinical application of echocardiography: summary article: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation 2003; 108(9): 1146-1162. Kim C, Kwok YS, Heagerty P, Redberg R. Pharmacologic stress testing for coronary disease diagnosis: A meta-analysis. Am Heart J 2001; 142(6): 934-944. Kwok Y, Kim C, Grady D, Segal M, Redberg R. Meta-analysis of exercise testing to detect coronary artery disease in women. Am J Cardiol 1999; 83(5): 660-666. Lewis JF, Lin L, McGorray S, et al. Dobutamine stress echocardiography in women with chest pain. Pilot phase data from the National Heart, Lung and Blood Institute Women's Ischemia Syndrome Evaluation (WISE). J Am Coll Cardiol 1999; 33(6): 1462-1468. Biagini E, Elhendy A, Bax JJ, et al. Seven-year follow-up after dobutamine stress echocardiography: Impact of gender on prognosis. J Am Coll Cardiol 2005; 45(1): 93-97. Cortigiani L, Dodi C, Paolini EA, Bernardi D, Bruno G, Nannini E. Prognostic value of pharmacological stress echocardiography in women with chest pain and unknown coronary artery disease. J Am Coll Cardiol 1998; 32(7): 1975-1981. Mieres JH, Shaw LJ, Hendel RC, et al. American Society of Nuclear Cardiology consensus statement: Task Force on Women and Coronary Artery Disease - The role of myocardial perfusion imaging in the clinical evaluation of coronary artery disease in women [correction]. J Nucl Cardiol 2003; 10(1): 95-101. Taillefer R, DePuey EG, Udelson JE, Beller GA, Latour Y, Reeves F. Comparative diagnostic accuracy of Tl-201 and Tc-99m sestamibi SPECT imaging (perfusion and ECG-gated SPECT) in
240 Recent Patents on Cardiovascular Drug Discovery, 2009, Vol. 4, No. 3 detecting coronary artery disease in women. J Am Coll Cardiol 1997; 29(1): 69-77. Klocke FJ, Baird MG, Lorell BH, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging). Circulation 2003; 108(11): 1404-1418. Amanullah AM, Berman DS, Hachamovitch R, Kiat H, Kang X, Friedman JD. Identification of severe or extensive coronary artery disease in women by adenosine technetium-99m sestamibi SPECT. Am J Cardiol 1997; 80(2): 132-137. Berman DS, Kang X, Hayes SW, et al. Adenosine myocardial perfusion single-photon emission computed tomography in women compared with men. Impact of diabetes mellitus on incremental prognostic value and effect on patient management. J Am Coll Cardiol 2003; 41(7): 1125-1133. Galassi AR, Azzarelli S, Tomaselli A, et al. Incremental prognostic value of technetium-99m-tetrofosmin exercise myocardial perfusion imaging for predicting outcomes in patients with suspected or known coronary artery disease. Am J Cardiol 2001; 88(2): 101-106. Sharir T, Germano G, Kavanagh PB, et al. Incremental prognostic value of post-stress left ventricular ejection fraction and volume by gated myocardial perfusion single photon emission computed tomography. Circulation 1999; 100(10): 1035-1042. Bashore TM, Bates ER, Berger PB, et al. American College of Cardiology/Society for Cardiac Angiography and Interventions Clinical Expert Consensus Document on cardiac catheterization laboratory standards. A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol 2001; 37(8): 2170-2214. Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: Results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 2008; 52(21): 1724-1732. Miller JM, Rochitte CE, Dewey M, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 2008; 359(22): 2324-2336. Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA 2004; 291(2): 210-215. Kondos GT, Hoff JA, Sevrukov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: A 37month follow-up of 5635 initially asymptomatic low- to intermediate-risk adults. Circulation 2003; 107(20): 2571-2576. Kim WY, Danias PG, Stuber M, et al. Coronary magnetic resonance angiography for the detection of coronary stenoses. N Engl J Med 2001; 345(26): 1863-1869. Hundley WG, Hillis LD, Hamilton CA, et al. Assessment of coronary arterial restenosis with phase-contrast magnetic resonance imaging measurements of coronary flow reserve. Circulation 2000; 101(20): 2375-2381. Nagel E, Klein C, Paetsch I, et al. Magnetic resonance perfusion measurements for the noninvasive detection of coronary artery disease. Circulation 2003; 108(4): 432-437. Schwitter J, DeMarco T, Kneifel S, et al. Magnetic resonancebased assessment of global coronary flow and flow reserve and its relation to left ventricular functional parameters: A comparison with positron emission tomography. Circulation 2000; 101(23): 2696-2702. Buchthal SD, den Hollander JA, Merz CN, et al. Abnormal myocardial phosphorus-31 nuclear magnetic resonance spectroscopy in women with chest pain but normal coronary angiograms. N Engl J Med 2000; 342(12): 829-835. [58]
Wake and Yoshiyama Nagel E, Lehmkuhl HB, Bocksch W, et al. Noninvasive diagnosis of ischemia-induced wall motion abnormalities with the use of high-dose dobutamine stress MRI: Comparison with dobutamine stress echocardiography. Circulation 1999; 99(6): 763-770. Kim RJ, Wu E, Rafael A, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med 2000; 343(20): 1445-1453. Weaver WD, Simes RJ, Betriu A, et al. Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: A quantitative review. JAMA 1997; 278(23): 2093-2098. Tamis-Holland JE, Palazzo A, Stebbins AL, et al. Benefits of direct angioplasty for women and men with acute myocardial infarction: Results of the Global Use of Strategies To Open Occluded Arteries in Acute Coronary Syndromes Angioplasty (GUSTO II-B) Angioplasty Substudy. Am Heart J 2004; 147(1): 133-139. Stone GW, Grines CL, Browne KF, et al. Comparison of inhospital outcome in men versus women treated by either thrombolytic therapy or primary coronary angioplasty for acute myocardial infarction. Am J Cardiol 1995; 75(15): 987-992. Lansky AJ, Pietras C, Costa RA, et al. Gender differences in outcomes after primary angioplasty versus primary stenting with and without abciximab for acute myocardial infarction: Results of the Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications (CADILLAC) trial. Circulation 2005; 111(13): 1611-1618. Vakili BA, Kaplan RC, Brown DL. Sex-based differences in early mortality of patients undergoing primary angioplasty for first acute myocardial infarction. Circulation 2001; 104(25): 3034-3038. Moses JW, Leon MB, Popma JJ, et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med 2003; 349(14): 1315-1323. Trikalinos TA, Alsheikh-Ali AA, Tatsioni A, Nallamothu BK, Kent DM. Percutaneous coronary interventions for non-acute coronary artery disease: A quantitative 20-year synopsis and a network metaanalysis. Lancet 2009; 373(9667): 911-918. Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: Prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005; 366(9493): 1267-1278. Alexander KP, Chen AY, Newby LK, et al. Sex differences in major bleeding with glycoprotein IIb/IIIa inhibitors: Results from the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) initiative. Circulation 2006; 114(13): 1380-1387. US Preventive Services Task Force recommendation statement. Aspirin for the prevention of cardiovascular disease. Ann Intern Med 2009; 150(6): 396-404. Ridker PM, Cook NR, Lee IM, et al. A randomized trial of lowdose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 2005; 352(13): 1293-1304. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results From the Women's Health Initiative randomized controlled trial. JAMA 2002; 288(3): 321-333. Welton AJ, Vickers MR, Kim J, et al. Health related quality of life after combined hormone replacement therapy: Randomised controlled trial. BMJ 2008; 337: a1190. Cargill, M., Devlin, J., Iakoubova, O.: US20097482117 (2009). The Wellcome Trust Case Control Consortium. Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature 2007; 447(7145): 661-678. Valkirs, G., Dahlen, J., Buechler, K.F., Kirchick, H.: US20087361473 (2008). Ng, L.L., Bergmann, A., Struck, J., Morgenthaler, N., Papassotiriou, J.: US20080213746 (2008). Cresci, S., McLeod, H.L., Kelly, D.P., Spertus, J.A.: US20080108712 (2008).
[43]
[59]
[60]
[44]
[61]
[45]
[62]
[46]
[63]
[47]
[64]
[48]
[65] [66]
[49]
[67]
[68]
[50] [51]
[69]
[52]
[70] [71]
[53]
[54]
[72]
[55] [56]
[73] [74]
[75] [76] [77]
[57]
You might also like
- Genetics Practice NCLEX Questions HandoutDocument6 pagesGenetics Practice NCLEX Questions HandoutAlvin L. Rozier100% (3)
- GABBARD - Term Psychodynamic Psychotherapy (Extrait) - 1Document6 pagesGABBARD - Term Psychodynamic Psychotherapy (Extrait) - 1Moëa NmtNo ratings yet
- Enteric-Coated Serratiopeptidase Product InfoDocument2 pagesEnteric-Coated Serratiopeptidase Product Infoamin138ir0% (2)
- Chapter 017Document18 pagesChapter 017wn4tb100% (2)
- Update On The Pathophysiology and Medical Treatment of Peripheral Artery DiseaseDocument20 pagesUpdate On The Pathophysiology and Medical Treatment of Peripheral Artery DiseaseRumah Sakit J. H. Awaloei ManadoNo ratings yet
- Peripheral Arterial Disease in Patients With Diabetes: State-Of-The-Art PaperDocument9 pagesPeripheral Arterial Disease in Patients With Diabetes: State-Of-The-Art PaperdonkeyendutNo ratings yet
- Adi Id EvDocument21 pagesAdi Id EvKumar AdityaNo ratings yet
- Vascular Medicine UpdatesDocument19 pagesVascular Medicine Updatessam samiNo ratings yet
- Primary and Secondary Prevention of Coronary Artery DiseaseDocument24 pagesPrimary and Secondary Prevention of Coronary Artery DiseaseNatalia GeofaniNo ratings yet
- Causes of Changes in Carotid Intima-Media Thickness: A Literature ReviewDocument10 pagesCauses of Changes in Carotid Intima-Media Thickness: A Literature ReviewSorin ParalescuNo ratings yet
- Menopause & Physical Exercise-3Document10 pagesMenopause & Physical Exercise-3Ana Carolina ChaconNo ratings yet
- Gender Differences in Cardiovascular Disease: Short CommunicationDocument3 pagesGender Differences in Cardiovascular Disease: Short CommunicationMoh SuprayogiNo ratings yet
- Report Information From Proquest: 13 February 2013 20:51Document21 pagesReport Information From Proquest: 13 February 2013 20:51Ina PNo ratings yet
- Primary and Secondary Prevention of Coronary Artery Disease - Overview, Risk AsseDocument32 pagesPrimary and Secondary Prevention of Coronary Artery Disease - Overview, Risk Asseליסה לרנרNo ratings yet
- Epidemiology, Risk Factors, and Natural History of Peripheral Artery DiseaseDocument20 pagesEpidemiology, Risk Factors, and Natural History of Peripheral Artery Diseasesnyder120792No ratings yet
- Gender Differences in the Pathogenesis and Management of Heart DiseaseFrom EverandGender Differences in the Pathogenesis and Management of Heart DiseaseNo ratings yet
- Young Adults' Awareness of Heart Disease RisksDocument33 pagesYoung Adults' Awareness of Heart Disease RisksSaida Pagayao100% (1)
- Appelman - Sex Differences in Cardiovascular Risk Factors - 2015Document8 pagesAppelman - Sex Differences in Cardiovascular Risk Factors - 2015MIRIAM VIDURRIZAGANo ratings yet
- 02 El SherifDocument7 pages02 El SherifAlfun IqbalNo ratings yet
- 1 s2.0 S1050173819300015 MainDocument8 pages1 s2.0 S1050173819300015 MainQFB. Alberto GuadarramaNo ratings yet
- An Update On Menopausal Hormone Replacement Therapy in Women and Cardiovascular DiseaseDocument8 pagesAn Update On Menopausal Hormone Replacement Therapy in Women and Cardiovascular DiseaseAlmas TNo ratings yet
- Diagnosis of Early Risks, Management of Risks, and Reduction of Vascular DiseasesDocument11 pagesDiagnosis of Early Risks, Management of Risks, and Reduction of Vascular DiseasesasclepiuspdfsNo ratings yet
- Blog Blood TestsDocument2 pagesBlog Blood Testsapi-284182568No ratings yet
- 2012 Rheumatoid Arthritis Cardiovascular Manifestations Pathogenesis and TherapyDocument7 pages2012 Rheumatoid Arthritis Cardiovascular Manifestations Pathogenesis and Therapytony zhaoNo ratings yet
- Research Papers On Coronary Heart DiseaseDocument5 pagesResearch Papers On Coronary Heart Diseasekrqovxbnd100% (1)
- Dent Clin N Am 50 (2006) 483-491Document9 pagesDent Clin N Am 50 (2006) 483-491lalajanNo ratings yet
- Cardiovascular Safety Profile of Currently Available Diabetic DrugsDocument17 pagesCardiovascular Safety Profile of Currently Available Diabetic Drugsvina_nursyaidahNo ratings yet
- Cardiovascular Risk Factors ThesisDocument4 pagesCardiovascular Risk Factors Thesisjennyrichardsonwashington100% (2)
- Acute Ischemic Stroke UpdateDocument38 pagesAcute Ischemic Stroke Updatenarendra wahyuNo ratings yet
- Psychology of Women 401 807Document407 pagesPsychology of Women 401 807Alessio TinerviaNo ratings yet
- Cardiovascular Disease PHD ThesisDocument6 pagesCardiovascular Disease PHD Thesisafknawjof100% (2)
- 44440-Article Text-150799-1-10-20200205Document11 pages44440-Article Text-150799-1-10-20200205audiNo ratings yet
- Cardiovascular Pathophysiology in Chronic Kidney Disease: Opportunities To Transition From Disease To HealthDocument8 pagesCardiovascular Pathophysiology in Chronic Kidney Disease: Opportunities To Transition From Disease To HealthABNo ratings yet
- EBP - Coronary Artery Disease in WomenDocument13 pagesEBP - Coronary Artery Disease in WomenYary MayorNo ratings yet
- Association Between Acute Myocardial Infarction, Lipid Profile and Smoking HabitDocument5 pagesAssociation Between Acute Myocardial Infarction, Lipid Profile and Smoking HabitIOSRjournalNo ratings yet
- Risksfactor PDFDocument50 pagesRisksfactor PDFLuthie SinghNo ratings yet
- R245 FullDocument11 pagesR245 FullYuliana WiralestariNo ratings yet
- Role of Hypertension and Obesity As Risk Factors For IhdDocument5 pagesRole of Hypertension and Obesity As Risk Factors For IhdMohammad Mujtaba GhaffariNo ratings yet
- A Brief Review of Biomarkers For Preventing and Treating Cardiovascular DiseasesDocument4 pagesA Brief Review of Biomarkers For Preventing and Treating Cardiovascular DiseasesZhenquan JiaNo ratings yet
- Pi Is 1078588416300533Document4 pagesPi Is 1078588416300533npr00No ratings yet
- Hormone Therapy and Cardiovascular DiseaseDocument7 pagesHormone Therapy and Cardiovascular Diseaseosama saeedNo ratings yet
- Module 1 - Sample PaperDocument7 pagesModule 1 - Sample PaperknuckleheadNo ratings yet
- Senka Mesihovic-Dinarevic, Chapter IDocument7 pagesSenka Mesihovic-Dinarevic, Chapter Ivaria5No ratings yet
- Impact of Diabetes On Coronary ArteryDocument7 pagesImpact of Diabetes On Coronary ArteryGuruh FitriantoNo ratings yet
- Gender Differences in Disease Manifestation and PresentationDocument5 pagesGender Differences in Disease Manifestation and PresentationGustavo Anzola100% (1)
- Peripheral Arterial DiseaseDocument8 pagesPeripheral Arterial DiseaseSILVIA FERNANDA CASTILLO GOYENECHENo ratings yet
- Literature Review On Coronary Artery DiseaseDocument6 pagesLiterature Review On Coronary Artery Diseaseea726gej100% (1)
- Published,, Noval Anti-Cancer TherapiesDocument10 pagesPublished,, Noval Anti-Cancer Therapiesshayma rafatNo ratings yet
- Diabetes, The Metabolic Syndrome, and Ischemic Stroke: Epidemiology and Possible MechanismsDocument10 pagesDiabetes, The Metabolic Syndrome, and Ischemic Stroke: Epidemiology and Possible MechanismsFelia AlyciaNo ratings yet
- Research Paper On Coronary Artery DiseaseDocument5 pagesResearch Paper On Coronary Artery Diseaseaflbuagdw100% (1)
- Cardiovascular Update: Professional PracticeDocument5 pagesCardiovascular Update: Professional PracticeJiearNo ratings yet
- DefiniciónDocument51 pagesDefiniciónKrissia SalvadorNo ratings yet
- Strategies For The Prevention of Coronary Artery Disease Complications - Can We Do Better?Document19 pagesStrategies For The Prevention of Coronary Artery Disease Complications - Can We Do Better?akbar011512No ratings yet
- Review Article: Investigation On Cardiovascular Risk Prediction Using Physiological ParametersDocument22 pagesReview Article: Investigation On Cardiovascular Risk Prediction Using Physiological ParametersNnaemeka NwobodoNo ratings yet
- Exercício em Pacientes Com CâncerDocument20 pagesExercício em Pacientes Com CâncerDrDermeval Reis JuniorNo ratings yet
- Premature Atherosclerotic Cardiovascular Disease Trends in INcidence, Related Risk FactorDocument14 pagesPremature Atherosclerotic Cardiovascular Disease Trends in INcidence, Related Risk FactorAda DaiNo ratings yet
- Mittal Maturitas 2022 P4 Versus MPA Plus TDL Estradiol On CV Markers RCTDocument36 pagesMittal Maturitas 2022 P4 Versus MPA Plus TDL Estradiol On CV Markers RCTPaul PIETTENo ratings yet
- Coronary Artery Disease Literature ReviewDocument4 pagesCoronary Artery Disease Literature Reviewaflsvwoeu100% (1)
- Total Lipid Profile Levels As BdjasDocument12 pagesTotal Lipid Profile Levels As BdjasAnonymous tG35SYROzENo ratings yet
- Coronary Diseases Modeling of Some Risk Factors Using Artificial Intelligence TechniquesDocument5 pagesCoronary Diseases Modeling of Some Risk Factors Using Artificial Intelligence TechniquesIJARP PublicationsNo ratings yet
- Framing Cardiovascular Disease Event Risk Prediction: EditorialDocument3 pagesFraming Cardiovascular Disease Event Risk Prediction: EditorialGaluh Kresna BayuNo ratings yet
- Https/www-Uptodate-Com Consultaremota Upb Edu Co/contents/management-Of-CDocument34 pagesHttps/www-Uptodate-Com Consultaremota Upb Edu Co/contents/management-Of-CMichael Amarillo CorreaNo ratings yet
- Hendro Susilo-Af and StrokeDocument7 pagesHendro Susilo-Af and StrokeyudisNo ratings yet
- Clinical practice: Managing cardiovascular risk in menopauseDocument6 pagesClinical practice: Managing cardiovascular risk in menopauseMicaela CalvopiñaNo ratings yet
- 1 s2.0 S0960977613003135 MainDocument10 pages1 s2.0 S0960977613003135 MainChirag ParmarNo ratings yet
- Twenty19 Smart Student Resume GuideDocument46 pagesTwenty19 Smart Student Resume GuidePraful ChandraNo ratings yet
- RejuvenationDocument5 pagesRejuvenationChirag ParmarNo ratings yet
- 5 Steps to Draw a State Machine DiagramDocument8 pages5 Steps to Draw a State Machine DiagramChirag ParmarNo ratings yet
- Who Guidlines Pregnancy Woman 2010 PDFDocument117 pagesWho Guidlines Pregnancy Woman 2010 PDFAna Di JayaNo ratings yet
- Hard QuestionDocument183 pagesHard QuestionWidodo Muis100% (1)
- TCS Weekly Update - 30th Aug 2013Document6 pagesTCS Weekly Update - 30th Aug 2013Chirag ParmarNo ratings yet
- ReviewDocument6 pagesReviewChirag ParmarNo ratings yet
- Pharmaceutical Industry. Ed. Jamuna Carroll. Detroit: Greenhaven Press, 2009Document4 pagesPharmaceutical Industry. Ed. Jamuna Carroll. Detroit: Greenhaven Press, 2009api-348564225No ratings yet
- Manual of Clinical Nutrition2013Document458 pagesManual of Clinical Nutrition2013Jeffrey Wheeler100% (9)
- Monkey Bite ProtocolDocument2 pagesMonkey Bite ProtocolOngky AristianNo ratings yet
- Dental Consent FormDocument16 pagesDental Consent FormArnav Gupta100% (1)
- Form 5Document10 pagesForm 5api-248999232No ratings yet
- 2014 Fokke GBS Brighton Brain 2014Document11 pages2014 Fokke GBS Brighton Brain 2014Hikmat SatriaNo ratings yet
- TopicalpaincontrolmedicationDocument47 pagesTopicalpaincontrolmedicationJ C Torres FormalabNo ratings yet
- Daytrana For ADHDDocument4 pagesDaytrana For ADHDdcowan100% (1)
- Model of Decision MakingDocument34 pagesModel of Decision MakingPalalikesjujubesNo ratings yet
- Screenshot 2022-12-14 at 4.16.40 PMDocument1 pageScreenshot 2022-12-14 at 4.16.40 PMPrisha SoniNo ratings yet
- Transactional Analysis: Understanding Behavior Through Parent, Adult, Child TheoryDocument1 pageTransactional Analysis: Understanding Behavior Through Parent, Adult, Child TheoryForam ShahNo ratings yet
- Cardioversion and DefibrillationDocument12 pagesCardioversion and DefibrillationNAGARAJ100% (1)
- PsychiaDocument9 pagesPsychiaNoel RafaelNo ratings yet
- Public School Teachers Awareness On ADHD Survey FormDocument3 pagesPublic School Teachers Awareness On ADHD Survey Formchichur jenNo ratings yet
- Fuss Et Al-1996-Dental Traumatology PDFDocument11 pagesFuss Et Al-1996-Dental Traumatology PDFDIANANo ratings yet
- Jambi Cardiology Update WorkshopDocument3 pagesJambi Cardiology Update WorkshopFahrurrozi SyarifNo ratings yet
- National Tuberculosis Program OverviewDocument21 pagesNational Tuberculosis Program OverviewJames RiedNo ratings yet
- Larry Nassar Ingham County AffidavitDocument5 pagesLarry Nassar Ingham County AffidavitDeadspinNo ratings yet
- Competency Based Job Analysis and Performance Management of Non-Medical Staff at Apollo Hospitals, DhakaDocument107 pagesCompetency Based Job Analysis and Performance Management of Non-Medical Staff at Apollo Hospitals, DhakaChayan ArdNo ratings yet
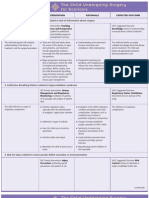
- NURSING CARE PLAN The Child Undergoing Surgery For ScoliosisDocument3 pagesNURSING CARE PLAN The Child Undergoing Surgery For ScoliosisscrewdriverNo ratings yet
- Roxonin LeafletDocument2 pagesRoxonin LeafletmohammedfirasatNo ratings yet
- Breast Abscess After Autologous Fat TransferDocument3 pagesBreast Abscess After Autologous Fat TransferInternational Journal of Innovative Science and Research Technology100% (1)
- What Is Mindfulness?Document2 pagesWhat Is Mindfulness?Vaseem SyedNo ratings yet
- Task 1: Critical AnalysisDocument4 pagesTask 1: Critical AnalysismohdnasrulNo ratings yet
- Compilation of Notes If Marijuana Will Be Legalized in The PhilippinesDocument42 pagesCompilation of Notes If Marijuana Will Be Legalized in The PhilippinesLajilaNo ratings yet
- Clinical Pharmacology in Healthcare, Teaching and ResearchDocument80 pagesClinical Pharmacology in Healthcare, Teaching and ResearchVNcomer100% (1)