Professional Documents
Culture Documents
Extrahepatic HCV
Uploaded by
neoraistlinOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Extrahepatic HCV
Uploaded by
neoraistlinCopyright:
Available Formats
http://www.utdol.com/online/content/topic.do?
topicKey=heptitis/8737&selectedTitle=10~150&source=search_result
Extrahepatic manifestations of hepatitis C virus infection Author Sanjiv Chopra, MD Section Editor Adrian M Di Bisceglie, MD Deputy Editor Peter A L Bonis, MD
Last literature review version 17.1: January 2009 | This topic last updated: November 17, 2008
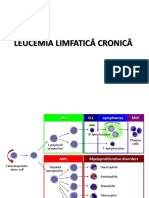
(More) INTRODUCTION The hepatitis C virus (HCV) is a cause of both acute and chronic hepatitis. In addition, several extrahepatic diseases have been associated with chronic HCV infection, and in most cases appear to be directly related to the viral infection. These include [1-4]:
Hematologic diseases such as cryoglobulinemia and lymphoma Autoimmune disorders such as thyroiditis and the presence of autoantibodies Renal disease Dermatologic conditions such as lichen planus and porphyria cutanea tarda
In one series of 321 patients, at least one extrahepatic manifestation was observed in 38 percent (show table) [3]. These features of HCV infection will be reviewed here. The clinical manifestations of acute and chronic hepatitis due to HCV are discussed separately. (See "Clinical features and natural history of hepatitis C virus infection"). HEMATOLOGIC DISORDERS HCV infection is associated with a number of hematologic disorders including essential mixed cryoglobulinemia, monoclonal gammopathies (which may be associated with multiple myeloma), and lymphoma and less commonly monoclonal gammopathies. Essential mixed cryoglobulinemia Mixed cryoglobulinemia is a lymphoproliferative disorder that can lead to deposition of circulating immune complexes in small to medium sized blood vessels. It often presents with the clinical triad of palpable purpura, arthralgias, and weakness, but can also involve the kidneys, peripheral nerves, and brain. (See "Clinical manifestations and diagnosis of essential mixed cryoglobulinemia"). HCV infection appears to have an etiologic role in most patients with essential mixed cryoglobulinemia. As an example, three studies of 101 patients with this disorder found that 95 (95 percent) had one or more of the following signs of HCV infection [5-7]:
Circulating anti-HCV antibodies The presence of polyclonal IgG anti-HCV antibodies within the cryoprecipitate HCV RNA in the plasma and particularly the cryoprecipitate
Another report prospectively evaluated the prevalence of cryoglobulins in 226 patients with chronic liver disease [8]. Of the 127 with chronic HCV infection, cryoglobulins were found in 69 (54 percent), frequently with anti-HCV antibody and HCV RNA concentrated in the cryoprecipitates (show figure 1). The incorporation of virus and antibody into the cryoprecipitate may sometimes reduce serum levels of anti-HCV and HCV RNA below detectable levels; this must be kept in mind when attempting to diagnose HCV infection in these patients. (See "Diagnostic approach to hepatitis C virus infection"). The association of mixed cryoglobulinemia with HCV infection may be linked to the ability of the virus to bind to B lymphocytes via CD81 [9]. Binding lowers the activation threshold of these cells, thereby facilitating the production of autoantibodies.
Further evidence for a causal relationship between HCV and essential mixed cryoglobulinemia is the demonstration of antiHCV antibodies in the vessel walls of skin biopsies obtained from patients with mixed cryoglobulinemia and cutaneous vasculitis. In addition, cryoglobulin levels decrease and skin lesions and symptoms improve in association with a reduction in HCV virus when patients respond to treatment with interferon alfa (show figure 2) [8,10,11]. (See "Treatment of essential mixed cryoglobulinemia"). Unfortunately, not all patients with HCV infection and cryoglobulinemia respond to interferon treatment. In addition, a reduction in cryoglobulin titers is not directly associated with a decrease in serum alanine aminotransferase (ALT) or HCV RNA. Treatment of patients with cryoglobulinemia due to HCV should be based upon the presence of cryoglobulinemia symptoms rather than the usual criteria used in patients with chronic hepatitis alone. (See "Treatment of chronic hepatitis C virus infection: Recommendations for adults"). On the other hand, cryoglobulinemia has been associated with the presence of advanced fibrosis; thus, many patients have relatively advanced chronic hepatitis potentially warranting treatment [12]. The response should be assessed by symptomatic improvement of cryoglobulinemia, a reduction in cryocrit, and an increase in serum complement levels. Complete responses may be more common in patients with low pretreatment levels of viremia and with high dose interferon regimens [13]. Patients whose clinical manifestations of mixed cryoglobulinemia are not controlled by, or are not appropriate for antiviral treatment, may be candidates for investigational therapies. Rituximab has shown promise in initial studies. (See "Treatment of essential mixed cryoglobulinemia"). Monoclonal gammopathies Hepatitis C may be a risk factor for the development of monoclonal gammopathies. Prior to the development of tests for the hepatitis C virus, the prevalence of monoclonal gammopathies was noted to be increased in patients with chronic liver disease [14]. The ability to test for the hepatitis C virus permitted identification of patients who may be at greatest risk. A study of 239 HCV-positive patients compared to 98 HCV-negative controls (76 with chronic hepatitis B, 9 with alcoholic liver disease, and 13 with primary biliary cirrhosis) made the following observations [15]:
Monoclonal bands were detected in 11 percent (compared to 1 percent of a control, age-matched population) The incidence peaked in the seventh decade Nine of the 26 patients with a monoclonal band had either a smoldering myeloma or multiple myeloma (see "Diagnosis and differential diagnosis of multiple myeloma"). Monoclonal gammopathy was most often associated with HCV genotype 2a/c
Lymphoma Multiple reports have described an association between HCV infection and B-cell non-Hodgkins lymphoma (NHL). A meta-analysis that included 48 studies concluded that the prevalence of HCV in patients with B-cell NHL was 15 percent, much higher than the general population (around 1.5 percent) and in patients with other hematologic malignancies (2.9 percent) suggesting that HCV has an etiologic role [16]. A large cohort study of United States Veterans published after the meta-analysis estimated the risk of NHL was increased by about 28 percent (HR 1.28, 95% CI 1.12-1.45) compared with non-HCV infected individuals [17]. The risk was also increased for Waldenstrom macroglobulinemia and cryoglobulinemia but not other hematologic malignancies. A later case-control study found that the risk was increased for diffuse large B-cell lymphoma, marginal zone lymphoma, and lymphoplasmacytic lymphoma, but not follicular lymphoma [18]. The strongest association with HCV infection with lymphoma is in the subset of patients with immunocytoma, a low-grade malignancy that has previously been associated with cryoglobulinemia [19,20]. HCV RNA has been isolated from the involved lymph nodes of some of these patients. Primary hepatic lymphoma has also been reported in association with HCV [21]. In addition, HCV has been described in gastric mucosa in association with MALT lymphomas (now called extranodal marginal zone B cell lymphoma of MALT type according to the REAL classification), raising the possibility that HCV, like Helicobacter pylori, may play an etiologic role in this low grade lymphoma [22-24]. (See "Association between Helicobacter pylori infection and gastrointestinal malignancy"). It has also been suggested that HCV cryoglobulinemia could progress to a NHL. In one study, for example, 24 patients with chronic HCV infection and clinically active cryoglobulinemia were identified from a population of approximately 1500 patients
with chronic HCV seen at a tertiary care referral center [25]. Sixteen of these 24 patients agreed to undergo molecular genetic testing and cellular flow analysis on bone marrow aspirates and biopsies. Nine (56 percent) had abnormal bone marrow morphology including seven (44 percent) with focal lymphoid aggregates that were suspicious for lymphoma, and two (13 percent) that were consistent with NHL. One of these two patients also had flow cytometric and molecular findings that were diagnostic of B-cell NHL. A trend toward increased clinical severity of cryoglobulinemia was noted among the nine patients who had bone marrow samples suspicious for lymphoma. No patients had systemic symptoms associated with lymphoma or were treated with chemotherapy. However, the distinction between lymphoma and lymphoid infiltrates on bone marrow specimens can be difficult, which was reflected by the observation that only one patient (6 percent) had molecular and flow-cytometric evidence supporting a diagnosis of NHL [25]. A higher proportion (30 percent) of patients with HCV, cryoglobulinemia and bone marrow specimens suspicious for NHL were found to have flow cytometric findings consistent with NHL in another report [6]. These data support the hypothesis that cryoglobulinemia may arise from chronic stimulation of the immune system by HCV, which may predispose to a lymphoproliferative disorder. (See "Clinical manifestations and diagnosis of essential mixed cryoglobulinemia"). The subsequent steps leading to the development of a lymphoproliferative disorder are uncertain. As mentioned above, patients with HCV are more likely than controls to have t(14;18) translocation with overexpression of the antiapoptotic bcl-2 proto-oncogene [26] and bcl-2 rearrangements [27-29], suggesting that bcl-2 may be a contributing factor to lymphoma development [26]. Some HCV-associated lymphomas produce soluble immunoglobulins directed against the E2 protein (an HCV envelope glycoprotein) [30]. This observation supports the hypothesis that some HCV-associated lymphomas originate from B cells that were initially activated by the HCV-E2 protein. The population attributable risk of HCV to lymphoma (ie, the proportion of the population whose lymphoma is caused by HCV) is probably low, and an association with HCV and lymphoma has not been detected in all reports [31]. Nevertheless, the development of unexplained anemia or lymphadenopathy in a patient with HCV and clinically active cryoglobulinemia should raise concern about an underlying lymphoproliferative disorder [6]. Whether treatment of the underlying HCV infection could be effective in such patients is uncertain [29]. Regression of splenic lymphoma was described in association with HCV treatment in a case series [32]. (See "Clinical manifestations, pathologic features, and diagnosis of splenic marginal zone lymphoma", section on Pathogenesis and see "Treatment of the indolent non-Hodgkin lymphomas" section on HCV infection). Whether treatment of HCV reduces the risk of lymphoma has not been well studied but data are suggestive of a protective effect in patients who achieve a sustained virologic response. One of the largest studies to focus on this issue included 501 patients with HCV who had received treatment with interferon-based therapy who were compared with 2078 consecutive patients who had not received therapy [33]. The annual incidence of lymphoma in patients with HCV was estimated to be 0.23 percent. The risk was reduced significantly in patients who achieved a sustained virologic response compared with those who did not achieve a sustained response and compared with untreated controls. DIABETES MELLITUS HCV infection has been linked to diabetes mellitus in several studies [34-43]. A meta-analysis of 34 studies estimated that the risk was increased by almost 70 percent in HCV-infected patients compared with non-infected controls (OR 1.67, 95% CI 1.28-2.06) [44]. The risk was also increased compared with patients with chronic HBV infection and in patients with HCV/HIV coinfection compared with those with HIV infection alone. Some studies have identified risk factors for the development of diabetes mellitus in HCV infected patients such as older age, obesity, severe liver fibrosis, and a family history of diabetes mellitus [45]. Patients undergoing liver transplantation for HCV also appear to be at increased risk, compared to other liver diseases, for developing diabetes mellitus following transplantation [46]. The cause of these associations is unknown, but their magnitude may be overestimated based because of the following factors [47]:
Patients with diabetes have more parenteral exposures than the general population, placing them at increased risk for transmission of viruses.
Not all studies are controlled for the presence of cirrhosis, which may be associated with impaired glucose tolerance.
HCV has also been linked to insulin resistance without overt diabetes [48]. The insulin resistance may contribute to fibrosis progression, particularly with HCV genotypes 1 and 4 and high serum RNA levels [48,49]. Insulin resistance may also impair the response to antiviral therapy with interferon and ribavirin. Achievement of a sustained virologic response to interferonbased therapy was associated with a reduced incidence of development of diabetes mellitus in one report [50]. AUTOIMMUNE DISORDERS A number of autoimmune disorders have been associated with HCV infection, including autoantibody formation, thyroid disease, sialadenitis, and autoimmune thrombocytopenic purpura. Autoantibodies Autoantibodies are common in patients with chronic HCV infection; antinuclear antibodies, antibodies directed against the Fc portion of IgG (rheumatoid factor), anticardiolipin antibodies, smooth muscle antibodies, or antithyroid antibodies are detected in 40 to 65 percent of patients [3,51,52]. These antibodies are typically present in low titer, and do not appear to influence the presentation or course of infection; they are not usually associated with extrahepatic disease. However, their presence may result in diagnostic difficulties; as an example, the HCV-infected patient with arthralgias, arthritis, and rheumatoid factor positivity may be initially misdiagnosed as having rheumatoid arthritis. In this setting, testing for other RA-associated autoantibodies infrequently observed in patients with HCV infection, such as anti-citrullinated peptide (eg, anti-cyclic citrullinated peptide or CCP) antibodies, may be helpful diagnostically [53]. (See "Origin and utility of measurement of rheumatoid factors"). Autoantibodies may first become detectable or can increase in titer during interferon treatment. (See "Principles of interferon therapy in liver disease and the induction of autoimmunity"). However, since their presence does not affect the disease course or the response to treatment, autoantibody formation is not a reason to stop therapy. (See "Management of treatment induced side effects for chronic hepatitis C"). Antibodies to actin and to liver/kidney microsomes (anti-LKM-1) are characteristic of types 1 and 2 autoimmune hepatitis, respectively. (See "Clinical manifestations and diagnosis of autoimmune hepatitis"). These antibodies have been detected in some patients with chronic HCV infection, particularly in Europe [54-56]. Most patients with hepatitis C and anti-LKM-1 antibodies, as well as other types of non-organ-specific autoantibodies, appear to benefit from interferon to the same extent as patients with chronic hepatitis C without such antibodies. However, such patients need meticulous monitoring during interferon treatment, since flares of aminotransferases without subsequent clearance of HCV RNA have been observed [57,58]. This observation suggests that these patients may behave as if they had autoimmune hepatitis. In support of this hypothesis is the finding that when patients with chronic hepatitis C with or without anti-LKM-1 antibodies were compared, the viral load was lower in the patients with anti-LKM-1 antibodies even though both groups had disease of similar severity [59]. Furthermore, some of these patients have responded to prednisone and azathioprine, directed against presumed autoimmune hepatitis [60,61]. One possible method of determining whether the hepatitis is primarily due to HCV or autoimmune hepatitis is that the anti-LKM-1 antibodies in patients with HCV are directed at different epitopes of cytochrome P450 2D6 (CYP2D6, the target antigen) from that seen with autoimmune hepatitis [62,63]. Thyroid disease Thyroid disorders are common in patients with chronic HCV, particularly women [64,65]. One of the largest studies included 630 consecutive patients with HCV (without cirrhosis) who were compared with 389 subjects from an iodine-deficient area, another control group of 268 persons from an area of iodine sufficiency, and 86 patients with chronic hepatitis B [65]. Mean TSH levels were significantly higher and free T3 and T4 levels significantly lower in patients with HCV than in all other groups. Patients with HCV were more likely than controls to have hypothyroidism (13 versus 3 to 5 percent), anti-thyroglobulin antibodies (17 versus 9 to 10 percent), and anti-thyroidperoxidase antibodies (21 versus 10 to 13 percent). Another report suggested that thyroid abnormalities were seen predominantly in women [64]. (See "Pathogenesis of Hashimoto's thyroiditis (chronic autoimmune thyroiditis)").
Overall, antithyroid antibodies are present in 5 to 17 percent of patients with HCV infection, and thyroid disease, primarily hypothyroidism, occurs in 2 to 13 percent of patients [64,65]. The highest prevalence of both thyroid antibodies and thyroid disease is found in older women. However, whether or not the prevalence is higher than in age- and sex-matched controls is controversial [66,67]. A separate issue is the development of thyroid disease in patients with HCV infection who are treated with interferon alfa. (See "Principles of interferon therapy in liver disease and the induction of autoimmunity", section on Thyroid disease and see "Management of treatment induced side effects for chronic hepatitis C"). Sialadenitis A lymphocytic sialadenitis suggestive of Sjgren's syndrome has been described in patients with chronic HCV infection [68,69]. A study of 137 patients with Sjgren's syndrome and HCV suggested that the clinical and immunologic features were indistinguishable from Sjgren's syndrome in patients without HCV [69]. (See "Classification and diagnosis of Sjgren's syndrome"). Autoimmune thrombocytopenic purpura Anti-HCV antibodies occur in 10 to 19 percent of patients with autoimmune thrombocytopenic purpura (ITP). Some of these patients acquired anti-HCV antibodies passively following use of IVIG with a high titer of anti-HCV antibodies, while others developed actual infection following transfusion of HCV-infected blood products employed for the treatment of ITP (eg, contaminated IVIG). In other cases, ITP developed following the acquisition of HCV infection, or during its treatment [70]. Myasthenia gravis An association between myasthenia gravis (MG) and hepatitis C virus infection has been suggested in case reports [71,72], although a causal association has not been clearly established [73]. MG has also been described in association with administration of interferon, possibly because of exacerbation of preexisting subclinical disease [74,75]. Sarcoidosis Sarcoidosis has been described in association with HCV, mostly in the setting of antiviral therapy. (See "Management of treatment induced side effects for chronic hepatitis C"). OCULAR DISEASE HCV infection has been associated with a variety ophthalmologic disorders including dry eyes, corneal ulcers (Mooren's ulcer), uveitis, and scleritis [76-79], and sicca syndrome in patients with HCV-related Sjogren's syndrome [69]. In addition, ophthalmologic disorders (retinal hemorrhages, cotton wool spots, and rarely retinal artery or vein obstruction) can occur during interferon therapy. (See "Management of treatment induced side effects for chronic hepatitis C"). RENAL DISEASE Glomerular disease may occur in patients with chronic HCV infection. The most common patterns are membranoproliferative glomerulonephritis (usually associated with essential mixed cryoglobulinemia) and, less frequently, membranous nephropathy [80,81]. Several series have reported that anti-HCV antibodies are nearly universal in patients with both membranoproliferative disease and cryoglobulinemia; the pathogenesis appears to relate to deposition of immune complexes containing anti-HCV and HCV RNA in the glomeruli. (See "Renal disease with hepatitis C virus infection"). Interferon alfa is indicated in patients with mixed cryoglobulinemia and membranoproliferative glomerulonephritis. A number of studies have reported a beneficial response to antiviral therapy in this setting, and the reduction in proteinuria correlates with a fall in HCV RNA [5,80,82]. However, long-term responses to interferon are unusual; maintenance treatment may be required, and renal function is often not improved by treatment. DERMATOLOGIC DISEASE A variety of dermatologic diseases may be associated with HCV infection [83]. The response to treatment of the underlying HCV is variable [84]. Porphyria cutanea tarda Porphyria cutanea tarda (PCT) is a skin disease caused by a reduction of hepatic uroporphyrinogen decarboxylase activity that is characterized by photosensitivity, skin fragility, bruising, and vesicles or bullae that can become hemorrhagic. There is a strong association between the sporadic form of PCT and HCV infection. The precise mechanism by which HCV infection might cause or act as a trigger for PCT in predisposed subjects is not known. (See "Porphyria cutanea tarda and hepatitis C virus infection").
All patients with PCT should be screened for HCV infection, as well as other potential precipitating factors. Treatment with interferon alfa should be considered in HCV-infected patients. Phlebotomy to deplete patients of excess iron is an important step prior to considering antiviral therapy since many of the symptoms of PCT improve with phlebotomy. Leukocytoclastic vasculitis A leukocytoclastic vasculitis may occur in conjunction with essential mixed cryoglobulinemia, presenting clinically with palpable purpura and petechiae that usually involve the lower extremities (show picture 1). (See "Clinical manifestations and diagnosis of essential mixed cryoglobulinemia"). Skin biopsy demonstrates cutaneous vasculitis with dermal blood vessel destruction associated with neutrophilic infiltration in and around the vessel wall (show histology 1A-1B). Other tissues, particularly the lower extremity peripheral nerves, may show similar vasculitic changes involving the vasa nervorum [85]. This may be manifested clinically as a peripheral neuropathy which, as in other forms of vasculitis, is typically asymmetric (also called a mononeuritis multiplex). (See "Clinical manifestations of vasculitic neuropathy"). Lichen planus Lichen planus (LP) is characterized by flat-topped, violaceous, pruritic papules with a generalized distribution. It can also involve mucus membranes, hair, and nails. LP may be mediated through the cellular immune response, although the actual precipitating mechanism is not known [86]. Skin biopsy demonstrates a dense lymphocytic infiltration in the upper dermis. LP can be seen in patients with a variety of liver diseases, particularly advanced liver disease; anti-HCV antibodies are present in 10 to 40 percent of these patients but a cause-and-effect relation is uncertain [1]. There are also reports of the development or exacerbation of lichen planus during interferon treatment for chronic HCV; the lesions improved when interferon was stopped [87]. (See "Management of treatment induced side effects for chronic hepatitis C"). Necrolytic acral erythema Necrolytic acral erythema is a pruritic, psoriasis-like skin disease characterized by a sharply marginated, erythematous to hyperpigmented plaques with variable scale and erosion on the lower extremities. In a series of 30 patients who presented with the disorder, all were found to have antibodies to HCV [88]. Biopsy specimens showed psoriaform changes, keratinocyte necrosis and papillomatosis. Improvement was observed in a patient who had been treated for HCV with interferon alfa (and subsequent relapse nine months after discontinuation). Topical and systemic corticosteroids had a variable benefit. Other reports have confirmed improvement with interferon alfa and also suggested a benefit from oral zinc sulfate [89-91]. MUSCULOSKELETAL Hepatitis C-associated osteosclerosis is a rare disorder characterized by a marked increase in bone mass during adult life. While most cases have been reported in patients with a history of intravenous drug abuse, it has also been seen with hepatitis C after blood transfusion [92]. Periosteal, endosteal and trabecular bone thickening occurs throughout the skeleton with the exception of the cranium. During active disease, forearm and leg pain are common, bone remodeling (turnover) is high, and bone mineral density is two- to threefold higher than age-matched norms. The increased remodeling may respond to bisphosphonates or calcitonin, but spontaneous remission has also been described. Abnormalities in insulin-like growth factors (IGF-1 and IGF-II) or their binding proteins may contribute to the increase in bone formation in this disorder [93]. Arthritis is noted in 2 to 20 percent of HCV patients. The arthritis is an evanescent rheumatoid-like picture in two-thirds of the cases and an oligoarthritis in the rest. (See "Specific viruses that cause arthritis"). MYOCARDITIS AND CARDIOMYOPATHY HCV has been associated with myocarditis and cardiomyopathy in reports from Japan. The pathogenesis is unclear. (See "Etiology and pathogenesis of myocarditis"). NEUROCOGNITIVE DYSFUNCTION Several studies have suggested that HCV infection may be associated with neurocognitive dysfunction even without advanced liver disease. The potential mechanisms are unclear. (See "Clinical manifestations and diagnosis of hepatic encephalopathy"). INFORMATION FOR PATIENTS Educational materials on this topic are available for patients. (See "Patient information: Hepatitis C"). We encourage you to print or e-mail this topic review, or to refer patients to our public web site, www.uptodate.com/patients, which includes this and other topics.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Bb3 WHO Classification of Tumors of Haemopoietic and Lymphoid Tissues 4th 2008 PGDocument422 pagesBb3 WHO Classification of Tumors of Haemopoietic and Lymphoid Tissues 4th 2008 PGLoredana Milea Ex Lefter100% (1)
- Non-Hodgkin Lymphoma: Andrew M. Evens Kristie A. Blum EditorsDocument343 pagesNon-Hodgkin Lymphoma: Andrew M. Evens Kristie A. Blum EditorsBianca100% (1)
- Atlas of Spleen Pathology and Histhology CompletDocument173 pagesAtlas of Spleen Pathology and Histhology CompletAncamed NycoletaNo ratings yet
- Core Pathology Stevens 2009Document695 pagesCore Pathology Stevens 2009Mikel SilvaNo ratings yet
- WHO 5th Edition Classification 2023Document57 pagesWHO 5th Edition Classification 2023mohamaed abbasNo ratings yet
- PET - CT Applications, A GUIDEDocument412 pagesPET - CT Applications, A GUIDEayodeji78100% (1)
- B CellDocument291 pagesB CellDiana Mitrea0% (1)
- Clinical and Radiological Features of Mesenteric Panniculitis: A Critical OverviewDocument12 pagesClinical and Radiological Features of Mesenteric Panniculitis: A Critical OverviewriyanysidikNo ratings yet
- Non Hodgkin Lymphoma by Dr. AnumDocument43 pagesNon Hodgkin Lymphoma by Dr. AnumHumar HaiderNo ratings yet
- Round Cell TumorsDocument86 pagesRound Cell TumorsMadhura ShekatkarNo ratings yet
- OcuandAdnexalLymphom PDFDocument126 pagesOcuandAdnexalLymphom PDFJovan PopovićNo ratings yet
- CD 22 AberranteDocument7 pagesCD 22 AberranteKATHERINE ALEXANDRA ESCARRAGA CORREALNo ratings yet
- Marginal Zone Lymphoma: State-of-the-Art TreatmentDocument15 pagesMarginal Zone Lymphoma: State-of-the-Art TreatmentzonderNo ratings yet
- Non-Hodgkin Lymphoma: Medicine March 2017Document9 pagesNon-Hodgkin Lymphoma: Medicine March 2017devaaNo ratings yet
- ASH Hematology Review Series - Indolent LymphomasDocument77 pagesASH Hematology Review Series - Indolent LymphomasИван НегарэNo ratings yet
- PDFDocument86 pagesPDFXuan TuanNo ratings yet
- Introduction To The B-Cell LymphomasDocument13 pagesIntroduction To The B-Cell LymphomasANo ratings yet
- B-Cell LymphomaDocument77 pagesB-Cell LymphomaH.B.ANo ratings yet
- Imunohistochimie LNHDocument4 pagesImunohistochimie LNHHaralambie SarbuNo ratings yet
- UntitledDocument731 pagesUntitledAlvaro Delfor Umpiri MirandaNo ratings yet
- Linfoma Conjuntival 2023Document12 pagesLinfoma Conjuntival 2023Miguel HernandezNo ratings yet
- 5th Ed WHO 2022 HematolymphoidDocument29 pages5th Ed WHO 2022 Hematolymphoids_duttNo ratings yet
- Curs5 Hematologie AnvDocument59 pagesCurs5 Hematologie AnvRaluca PăunaNo ratings yet
- Treatment of Sjögren's Syndrome - Constitutional and Non-Sicca Organ-Based Manifestations - UpToDateDocument31 pagesTreatment of Sjögren's Syndrome - Constitutional and Non-Sicca Organ-Based Manifestations - UpToDateGabriel Fernandez FigueroaNo ratings yet
- Shankland NHL Lancet Review PDFDocument10 pagesShankland NHL Lancet Review PDFNadhila ByantNo ratings yet
- A Systematic Approach To The Cutaneous Lymphoid Infiltrates PDFDocument22 pagesA Systematic Approach To The Cutaneous Lymphoid Infiltrates PDFJuan Eduardo Rocha AguirreNo ratings yet
- BY: Moses Kazevu (BSC Human Biology)Document40 pagesBY: Moses Kazevu (BSC Human Biology)Moses Jr KazevuNo ratings yet
- DUR Packet 6 2018aDocument189 pagesDUR Packet 6 2018aDaniel ThanapalNo ratings yet
- IHC LymphomaDocument21 pagesIHC LymphomaNGUYEN QUYNHNo ratings yet
- White Blood Cells and Its Disorders: Key PointsDocument24 pagesWhite Blood Cells and Its Disorders: Key PointsskNo ratings yet