Professional Documents
Culture Documents
Five High-Risk Practice
Uploaded by
Micah SaberOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Five High-Risk Practice
Uploaded by
Micah SaberCopyright:
Available Formats
Five High-Risk Practice Areas for Nurses Enrolled in ISNAP
Anna Beaman, Courtney Foughty, Stephen Schmalz, Angela M. McNelis, PhD, RN, Sara Horton-Deutsch, PhD, RN and Pamela OHaver Day, CNS, RN
Indiana University Purdue University Indianapolis IU School of Nursing 2010
Abstract The purpose of this study was to examine the characteristics of nurses enrolled in the Indiana State Nurses Assistance Program (ISNAP) and to identify the top five areas where they practice. The sample consisted of 552 subjects who are currently in or have completed the ISNAP program. Known practice areas (n = 336) with the highest numbers of nurses in ISNAP were geriatrics (n = 142, 42.3%), medical-surgical (n = 71, 21.1%), emergency (n = 50, 14.9%), home care (n = 37, 11%), and critical care (n=36, 11%). An investigation into these risk areas showed that opiates and alcohol were the most frequently abused drugs in each of these practice areas. Across all practice areas the nurses were predominantly female, had a mean age of 40 years old, did not divert drugs, worked full-time in a hospital as Registered Nurses (RNs), and worked in an urban area. There were similar frequencies of employer and self-referrals to the treatment program. Differences were predominantly seen in geriatrics, where relatively more nurses were Licensed Practical Nurses (LPNs), worked in a nursing home, with equal representation in urban and rural practice sites. Findings suggest that there is a need for further monitoring in a system where nurses are practicing more autonomously and caring for vulnerable patients. Findings also indicate more education related to addictions and treatment is needed at the individual and institutional level. Introduction/Review of Literature The problem of licensed health care professionals who use and abuse illegal or prescription drugs and alcohol is pervasive and widespread. This is evidenced by the fact that most of the 50 states currently operate peer assistance programs that provide monitoring, supervision, and direction to registered and licensed practical nurses who are substance dependent or abusers. According to the American Nurses Association, 6 to 8% have a problem serious enough to interfere with their ability to practice (Talbert, 2009), and approximately 10% have some level of drug or alcohol problem (Blazer & Mansfield, 1995). Shaw et al. (2004) found nurses live and work in environments with intense and ubiquitous triggers to relapse. Characteristics of high-
risk practice factors specific to nurses include working variable shifts, long hours, high-stress patient care, pain associated with injuries, and access to medications. Past research found that nurses were more likely to use substances when workplace access to substances increased (p < 0.001), when their social networks contained more drug users, and when religiosity decreased (p < 0.001) (Trinkoff, Zhou, Storr, & Soeken, 2000). Other researchers have looked at characteristics of dependent nurses and found a majority of chemically dependent nurses were Caucasian and worked in major cities. The mean age of substance-abusing nurses was 38.8 years, they had been practicing on average for 9.5 years, and most were referred to a treatment program when they were about 40 years old (Clark & Farnworth, 2006; Finke, Williams, & Stanley, 1996). Clark and Farnsworth (2006) found no difference in age or gender between those who were successful and those who were unsuccessful in a peer assistance program, and they were unable to explain the reason why some nurses were successful and others failed. Tipton (2005) found in peer assistance programs for impaired nurse there were103 participants who worked in an inpatient acute care setting with the predominant practice areas being medical-surgical, critical care, maternal-child, and emergency room. The Indiana State Nurses Assistance Program (ISNAP) is a program funded by nurses licensure fees collected by the Indiana State Board of Nursing offering consultation, referral, and monitoring for nurses whose practice is impaired or potentially impaired, because of the use, abuse, or dependency relative to alcohol or other drugs. As of January 1, 2010, ISNAP had 589 nurses enrolled in the program out of the 115,526 nurses licensed in Indiana (.05%). The present study focused on the characteristics of nurses who have recently participated in ISNAP, their experience with their treatment process, and the characteristics of those who successfully completed the program as compared to those who relapsed or failed the program. Our assumption was that recognition of these characteristics might aide in early detection and intervention. Methods A secondary analysis of data from the ISNAP database was conducted using statistical software SPSS 16.0 for Windows. Complete data were available for 552 subjects and were used for this study. Data were analyzed using descriptive statistics. Results Findings show that practice areas with the highest frequencies of nurses were geriatrics (n = 142, 42.3), medical-surgical (n = 71, 21.1%), emergency (n = 50, 14.9%), home care (n = 37, 11%), and critical care (n = 36, 11%). The subjects were predominantly female (88.7%), had mean age of 41 years old, worked full time in a hospital, were Registered Nurses (RNs), did not divert drugs from their patients, and worked in an urban area. The Indiana Bureau of Labor Statistics reported the proportion of registered female nurses was 94.4% at the end of 2005 and 91.7% at the end of 2008, thus our sample reflects state trends. Table 1 indicates the frequency of female and male nurses in each high-risk practice area. There were similar frequencies of employer and self-referrals to the treatment program. Few differences were seen among sites, except for geriatrics. In the geriatric setting, relatively more nurses were Licensed Practical Nurses (LPNs) working in nursing homes. There was more equal
representation in urban and rural practice sites than in the other practice areas. Figure 1 indicates how many RNs and LPNs work in each of the high-risk practice areas. In all five areas, opiates and alcohol were the most frequently stated drugs of choice. Marijuana, cocaine, amphetamines, and methamphetamines were also reported as used by only a few nurses in the study. Conclusion Results indicate that the high-risk practice areas in Indiana are similar to those on the national level. Areas where nurses work more autonomously and have greater access to controlled substances appear to be where impaired nurses are working. Opiates and alcohol were the two primary drugs of choice for nurses in this sample. Data about diversion was not included in this study, so more information is needed to determine if opiates were obtained this way, and if so, the mechanisms in place at institutions that safeguard against this problem. The study was limited by missing data and the variables available for analysis. Based on the literature review, future studies should include variables such as social networks, family history, co-morbidity, spirituality, treatment modalities, stress, and information related to relapse. Substantial data related to these factors is contained in client files and not in the current database. Thus, future research efforts should include a chart review of the clients who have completed or are currently enrolled in the program and expansion of the database. Also, more research could include differentiating between associate-prepared RNs and baccalaureateprepared RNs. All findings will be disseminated to ISNAP and the Indiana State Board of Nursing. Implications for Practice Knowing the high-risk areas and frequently used drugs will allow us to identify nurses who may be at risk for substance use disorders. Interventions would focus on education surrounding the science of addictions, recognition of signs and symptoms of substance use and abuse, and creating environments conducive to recovery and retention. Findings indicate that nurses at all levels of educational preparation, ranging from LPNs to advanced practice nurses, are at risk for chemical dependency. Therefore, all nurses should be included in education programs related to addictions. This should include higher level nurse managers and administrators to promote treatment to the affected nurses.
References Blazer L.K., & Mansfield P.K. (1995). A comparison of substance use rates among female nurses, clerical workers, and blue-collar workers. Journal of Advanced Nursing 21, 305-313. Clark, C., & Farnsworth, J. (2006). Program for recovering nurses: An evaluation. MEDSURG Nursing, 15 (4), 223-230. Finke, L., Williams, J., & Stanley, R. (1996). Nurses referred to a peer assistance program for alcohol and drug problems. Archives of Psychiatric Nursing, 10 (5), 319-324. Shaw, M., McGovern, M., Angres, D., & Rawal, P. (2004, September). Physicians and nurses with substance use disorders. Journal of Advanced Nursing, 47(5), 561-571. Talbert, JA.J., (2009). Substance abuse among nurses. Clinical Journal of Oncology Nursing, 13(1), 17-19. Tipton, P.H. (2005). Predictors of Relapse for Nurses Participating in a Peer Assistance Program [Doctoral Disertation]. Denton, Texas: Texas Women's University. Trinkoff, A., Zhou, Q., Storr, C., & Soeken, K. (2000). Workplace access, negative proscriptions, job strain, and substance use in registered nurses. Nursing Research, 49(2), 8390.
Table 1 Females and Males for Each High-Risk Practice Area: In each of the high-risk areas, the number of females in the ISNAP program was significantly greater than the number of males. Geriatrics MedicalSurgical n=63 (88.7%) n=8 (11.3%) Emergency Department n=43 (86%) n=7 (14%) Home/Public Health n=30 (81.1%) n=7 (18.9%) Critical Care
Female Male
n=121 (85.2%) n=21 (14.8%)
n=25 (71.4%) n=10* (28.6%)
*One participant did not disclose gender
Geriatrics ED Med-Surg Home/ Public Health
Figure 1 Highest Degree in Top 5 High Risk Areas: The highest risk area was geriatrics. This was followed by medical-surgical, emergency, home and public health, and critical care.
You might also like
- Methamphetamine Use Disorder - Epidemiology, Clinical Manifestations, Course, Assessment, and Diagnosis - UpToDate PDFDocument16 pagesMethamphetamine Use Disorder - Epidemiology, Clinical Manifestations, Course, Assessment, and Diagnosis - UpToDate PDFMelissandre100% (1)
- The Codependency Workbook Simple Practices For Developing and Maintaining Your Independence - CompressDocument184 pagesThe Codependency Workbook Simple Practices For Developing and Maintaining Your Independence - CompressНиколай Кожухаренко50% (2)
- Jon R. Webb - Understanding Forgiveness and Addiction - Theory, Research, and Clinical Application (2021, Routledge) - Libgen - LiDocument239 pagesJon R. Webb - Understanding Forgiveness and Addiction - Theory, Research, and Clinical Application (2021, Routledge) - Libgen - LiAmine Aggoune100% (1)
- PsycDocument365 pagesPsycRui CunhaNo ratings yet
- The Psychological Science of AddictionDocument11 pagesThe Psychological Science of Addictiontiggyd100% (3)
- Complementary and Alternative Medicine On Oncology NursingDocument9 pagesComplementary and Alternative Medicine On Oncology NursingAurora Violeta Zapata RuedaNo ratings yet
- Errors of Omission: How Missed Nursing Care Imperils PatientsFrom EverandErrors of Omission: How Missed Nursing Care Imperils PatientsNo ratings yet
- Beyond Addiction by Jeffrey Foote, Carrie Wilkens ..Document254 pagesBeyond Addiction by Jeffrey Foote, Carrie Wilkens ..jenNo ratings yet
- Nurse Perceptions of Medication ErrorsDocument9 pagesNurse Perceptions of Medication ErrorsMoisés PonceNo ratings yet
- Drug Education Course Description Provides OverviewDocument22 pagesDrug Education Course Description Provides OverviewChavez RechelleNo ratings yet
- Chapter 26: Clients With Substance Abuse DisordersDocument6 pagesChapter 26: Clients With Substance Abuse DisordersMia MabaylanNo ratings yet
- Medication ErrorsDocument8 pagesMedication ErrorsMaricris Ambonan BawagNo ratings yet
- The Nurses' Knowledge and Attitudes Towards The Palliative CareDocument10 pagesThe Nurses' Knowledge and Attitudes Towards The Palliative CareZein AhmadNo ratings yet
- RRL 8 Part 3Document55 pagesRRL 8 Part 3Joshua Christian Gan0% (1)
- 210 1437 1 PB LibreDocument62 pages210 1437 1 PB Librezozorina21No ratings yet
- UP Manila Journal AbstractsDocument6 pagesUP Manila Journal AbstractsPrincess Anne LantinNo ratings yet
- The Staff Nurse-FinalDocument31 pagesThe Staff Nurse-FinalQuin Valent MalikNo ratings yet
- The Relationship Between Nurses Work HoursDocument31 pagesThe Relationship Between Nurses Work HoursZaty ChaiyOkkNo ratings yet
- Research PaperDocument14 pagesResearch Paperapi-455600000No ratings yet
- Research PaperDocument14 pagesResearch Paperapi-455767165No ratings yet
- A Pilot Study Quantifying Filipino Nurses' Perception of StressDocument8 pagesA Pilot Study Quantifying Filipino Nurses' Perception of StressVinna Mae DatoNo ratings yet
- Fitzpatrick OriginalDocument6 pagesFitzpatrick OriginalKristianus S PulongNo ratings yet
- Abostrofic SytosisDocument17 pagesAbostrofic Sytosisasaad biqaiNo ratings yet
- 420 Research PaperDocument12 pages420 Research Paperapi-372913673No ratings yet
- Burnout, Job Dissatisfaction and Missed Care Among Maternity NursesDocument6 pagesBurnout, Job Dissatisfaction and Missed Care Among Maternity Nursesazeem chaudhary100% (1)
- Challenges To Implementation of The Pharmaceutical Care Practice in Davao City.Document11 pagesChallenges To Implementation of The Pharmaceutical Care Practice in Davao City.JessieLynMolinaNo ratings yet
- Impact of Language Barrier On Acutecaremedical Professionals Is Dependent Upon RoleDocument4 pagesImpact of Language Barrier On Acutecaremedical Professionals Is Dependent Upon Roleravibunga4489No ratings yet
- Patient Preference For Physician Gender in The Emergency DepartmentDocument12 pagesPatient Preference For Physician Gender in The Emergency DepartmentLuciaNo ratings yet
- Personal Use and Professional Recommendations of Complementary and Alternative Medicine by Hong Kong Registered NursesDocument6 pagesPersonal Use and Professional Recommendations of Complementary and Alternative Medicine by Hong Kong Registered NursesWilyanto YangNo ratings yet
- How To Change Nurses' Behavior Leading To Medication Administration Errors Using A Survey Approach in United Christian HospitalDocument10 pagesHow To Change Nurses' Behavior Leading To Medication Administration Errors Using A Survey Approach in United Christian HospitalyyNo ratings yet
- Journal 1-Mental HealthDocument8 pagesJournal 1-Mental HealthLely AshariNo ratings yet
- Written Assignment 5 Corrected Final PaperDocument18 pagesWritten Assignment 5 Corrected Final Paperapi-401934380No ratings yet
- Medication ErrorsDocument8 pagesMedication ErrorsFarmisa MannanNo ratings yet
- Why Physicians and Nurses Ask (Or Don 'T) About Partner Violence: A Qualitative AnalysisDocument12 pagesWhy Physicians and Nurses Ask (Or Don 'T) About Partner Violence: A Qualitative Analysisionut pandelescuNo ratings yet
- Home Health Nurses' Perspectives and Care Processes Related To Older Persons With Frailty and Depression: A Mixed Method Pilot StudyDocument20 pagesHome Health Nurses' Perspectives and Care Processes Related To Older Persons With Frailty and Depression: A Mixed Method Pilot StudyFitriani WidyastantiNo ratings yet
- EBP Deliverable Module 2Document6 pagesEBP Deliverable Module 2Marian SmithNo ratings yet
- Pretreatment and in-treatment factors predict dropout from substance use disorder treatmentDocument11 pagesPretreatment and in-treatment factors predict dropout from substance use disorder treatmentFabian Giraud100% (1)
- Medication Errors 111765Document7 pagesMedication Errors 111765akko aliNo ratings yet
- Diabetes Spectr 2007 Derr 177 85Document9 pagesDiabetes Spectr 2007 Derr 177 85Juankarloz MedinaNo ratings yet
- Attributable To The Use of Medications (: Near MissesDocument4 pagesAttributable To The Use of Medications (: Near MissesdudijohNo ratings yet
- 0rder 343 NRS-493-ASSIGNMENT 3 Literature ReviewDocument6 pages0rder 343 NRS-493-ASSIGNMENT 3 Literature Reviewjoshua chegeNo ratings yet
- 2018 - Khalil & LeeDocument12 pages2018 - Khalil & LeeazeemathmariyamNo ratings yet
- An Environmental Scan of The Role of Nurses in Preventing Fetal Alcohol Spectrum DisordersDocument9 pagesAn Environmental Scan of The Role of Nurses in Preventing Fetal Alcohol Spectrum DisordersnilamsaryNo ratings yet
- Compliance With Hand Therapy Programs - Therapist and Patients PerceptionsDocument10 pagesCompliance With Hand Therapy Programs - Therapist and Patients PerceptionssammyrasaNo ratings yet
- Review of Related Literature and Studies Me ForeignDocument8 pagesReview of Related Literature and Studies Me ForeignJan BularioNo ratings yet
- JournalDocument8 pagesJournalFaye Margaret LagrimasNo ratings yet
- Factors That Contribute To Medication ErrorsDocument1 pageFactors That Contribute To Medication ErrorsFortuna Corazon RoldanNo ratings yet
- Pain Management JournalDocument7 pagesPain Management JournalPengurus Pusat HipgabiNo ratings yet
- 31-Main Text-217-5-10-20201110Document15 pages31-Main Text-217-5-10-20201110Jefferson AculaNo ratings yet
- NR Thesis1Document40 pagesNR Thesis1ceicai100% (1)
- J9Document7 pagesJ9hudarulNo ratings yet
- Impact of Nursing Diagnoses On Patient and Organisational Outcomes: A Systematic Literature ReviewDocument43 pagesImpact of Nursing Diagnoses On Patient and Organisational Outcomes: A Systematic Literature ReviewLucas Teles IanniNo ratings yet
- Strengthening Pharmacy Practice in Vietnam: Findings of A Training Intervention StudyDocument9 pagesStrengthening Pharmacy Practice in Vietnam: Findings of A Training Intervention StudySarahNo ratings yet
- Mortensene Issueanalysispaper Nurs450Document18 pagesMortensene Issueanalysispaper Nurs450api-284786443No ratings yet
- Self Medication PatientsDocument7 pagesSelf Medication PatientsSophia Denella FelizardoNo ratings yet
- Reed - Reflection Paper Nurs631Document10 pagesReed - Reflection Paper Nurs631api-215994182No ratings yet
- Medication Administration Error 3Document16 pagesMedication Administration Error 3Priya bhattiNo ratings yet
- Clinician BurnoutDocument7 pagesClinician Burnoutfgump123No ratings yet
- Hospital Nurse Staffing PDFDocument7 pagesHospital Nurse Staffing PDFmku 2017No ratings yet
- Burnout Syndrome and Nurse-To-Patient Ratio in The WorkplaceDocument21 pagesBurnout Syndrome and Nurse-To-Patient Ratio in The WorkplaceAbdalla ShaboNo ratings yet
- The Effect of Emergency Department Crowding On Patient Outcomes: A Literature ReviewDocument4 pagesThe Effect of Emergency Department Crowding On Patient Outcomes: A Literature ReviewRohon EzekielNo ratings yet
- Medication Knowledge, Certainty, and Risk of Errors in Health Care: A Cross-Sectional StudyDocument9 pagesMedication Knowledge, Certainty, and Risk of Errors in Health Care: A Cross-Sectional Studymeci_asyikNo ratings yet
- Aappq PDFDocument11 pagesAappq PDFNalau Sapu RataNo ratings yet
- Workplace Empowerment PDFDocument7 pagesWorkplace Empowerment PDFMonica PalaciosNo ratings yet
- Medication Administration ErrorsDocument16 pagesMedication Administration ErrorspriyaNo ratings yet
- NAPNAP Position Statement On The Acute Care Pediatric Nurse PractitionerDocument17 pagesNAPNAP Position Statement On The Acute Care Pediatric Nurse PractitionerMichael Greg Pengson LambiguitNo ratings yet
- Factors Influencing Paediatric Nurses' Responses To Medication AdministrationDocument4 pagesFactors Influencing Paediatric Nurses' Responses To Medication AdministrationYuni AstutiNo ratings yet
- Approach To Nursing Assessment 1Document5 pagesApproach To Nursing Assessment 1Taiye OkondoNo ratings yet
- ADocument1 pageAMicah SaberNo ratings yet
- Lesson 8 RespiDocument6 pagesLesson 8 RespiMicah SaberNo ratings yet
- Jikik 78Document1 pageJikik 78Micah SaberNo ratings yet
- Adult Schedule Easy ReadDocument2 pagesAdult Schedule Easy Readtummalapalli venkateswara raoNo ratings yet
- TGR3Document1 pageTGR3Micah SaberNo ratings yet
- New Microsoft Office PowerPoint 2007 PresentationDocument1 pageNew Microsoft Office PowerPoint 2007 PresentationsukhvinderhimaniNo ratings yet
- New Microsoft Office PowerPoint PresentationDocument1 pageNew Microsoft Office PowerPoint PresentationMicah SaberNo ratings yet
- SFSFSFDocument1 pageSFSFSFMicah SaberNo ratings yet
- New Microsoft Office PowerPoint PresentationDocument1 pageNew Microsoft Office PowerPoint PresentationMicah SaberNo ratings yet
- S4U790 Document SummaryDocument1 pageS4U790 Document SummaryMicah SaberNo ratings yet
- New Microsoft Office PowerPoint PresentationDocument1 pageNew Microsoft Office PowerPoint PresentationMicah SaberNo ratings yet
- New Microsoft Office PowerPoint PresentationDocument1 pageNew Microsoft Office PowerPoint PresentationMicah SaberNo ratings yet
- New Microsoft Office PowerPoint 2007 PresentationDocument1 pageNew Microsoft Office PowerPoint 2007 PresentationsukhvinderhimaniNo ratings yet
- HelloDocument1 pageHelloMicah SaberNo ratings yet
- DadqaDocument1 pageDadqaMicah SaberNo ratings yet
- ScdsdsDocument1 pageScdsdsMicah SaberNo ratings yet
- Ineffective Coping RT Recent Changes in Health StatusDocument2 pagesIneffective Coping RT Recent Changes in Health StatusMicah SaberNo ratings yet
- Manual FastalcoholDocument14 pagesManual FastalcoholMicah SaberNo ratings yet
- MilestonesDocument2 pagesMilestonesMicah SaberNo ratings yet
- What Is HirschsprungDocument4 pagesWhat Is HirschsprungMicah SaberNo ratings yet
- Manual FastalcoholDocument14 pagesManual FastalcoholMicah SaberNo ratings yet
- ProfessionalismDocument3 pagesProfessionalismHanafiah HussinNo ratings yet
- Pref CardDocument1 pagePref CardMicah SaberNo ratings yet
- Chapter 22 Module Substance Related DisorderDocument5 pagesChapter 22 Module Substance Related DisorderCheetah GemmaNo ratings yet
- Addiction Homework AssignmentsDocument4 pagesAddiction Homework Assignmentsvnwmruilf100% (1)
- Cannabis 051815Document31 pagesCannabis 051815Shubhrima KhanNo ratings yet
- Full Download Test Bank For Drugs Behaviour and Society Canadian Edition Carl Hart Download PDF Full ChapterDocument36 pagesFull Download Test Bank For Drugs Behaviour and Society Canadian Edition Carl Hart Download PDF Full Chapterpaltrilybelial.femebs100% (14)
- Hudson Litchfield News 1-6-2017Document12 pagesHudson Litchfield News 1-6-2017Area News Group100% (1)
- Bio Investigatory ProjectDocument16 pagesBio Investigatory Projectprism1702No ratings yet
- The Commonwealth of Kentucky v. The Kroger CompanyDocument60 pagesThe Commonwealth of Kentucky v. The Kroger CompanyWKYTNo ratings yet
- Nancy,,, GITARI PROJECTDocument46 pagesNancy,,, GITARI PROJECTjohn mwambuNo ratings yet
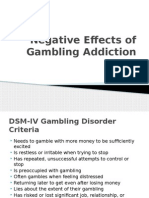
- Gambling Addiction PowerpointDocument11 pagesGambling Addiction PowerpointEK200620No ratings yet
- The Body Environment Mind and Spirit Bems Pathway of Addiction Causality and Curative InterventionsDocument6 pagesThe Body Environment Mind and Spirit Bems Pathway of Addiction Causality and Curative InterventionsHerald Scholarly Open AccessNo ratings yet
- Template Proposal by WilkinsDocument87 pagesTemplate Proposal by WilkinsHernando VaydalNo ratings yet
- Karakoula 20161Document15 pagesKarakoula 20161dnyNo ratings yet
- Issue Guide 1Document24 pagesIssue Guide 1api-664300441No ratings yet
- Case Management For Addiction Professionals: Module 1-TrainingDocument27 pagesCase Management For Addiction Professionals: Module 1-TraininglissarlissaaNo ratings yet
- NURSING and SUBSTANCE USE DISORDERSDocument150 pagesNURSING and SUBSTANCE USE DISORDERSmabelaNo ratings yet
- Journal Problematic Internet UseDocument6 pagesJournal Problematic Internet UseYosepha HutaurukNo ratings yet
- Ministry of Social Justice EmpowermentDocument113 pagesMinistry of Social Justice Empowermentkapilsaggi2526No ratings yet
- Improving Medical Students' Attitude Toward Patients With Substance Use Problems Through Addiction Medicine EducationDocument10 pagesImproving Medical Students' Attitude Toward Patients With Substance Use Problems Through Addiction Medicine EducationMutiara UtamiNo ratings yet
- SCID-5-RV Changes to Organization and Diagnostic CoverageDocument6 pagesSCID-5-RV Changes to Organization and Diagnostic CoverageCarla MariaNo ratings yet
- Case StudyDocument12 pagesCase Studyapi-662404021No ratings yet
- How Students Benefit From School DiversityDocument7 pagesHow Students Benefit From School Diversitymilagros curiNo ratings yet
- Introduction To Social Work An Advocacy Based Profession Social Work in The New Century 2nd Edition Ebook PDFDocument62 pagesIntroduction To Social Work An Advocacy Based Profession Social Work in The New Century 2nd Edition Ebook PDFmary.krueger918100% (41)