Professional Documents
Culture Documents
BLOK 12 - IT 9 - Farmakokinetik 2 - STZ
Uploaded by
IzzarIzzarCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BLOK 12 - IT 9 - Farmakokinetik 2 - STZ
Uploaded by
IzzarIzzarCopyright:
Available Formats
Pharmacokinetics
Sutomo Tanzil
Dept.of Pharmacology, Faculty of
Medicine, Sriwijaya University
The movement of drug molecules
across cellular barriers (1)
To traverse cellular barriers (e.g.GI mucosa,
renal tubule, blood-brain barrier, placenta),
drugs have to cross lipid membranes.
Drugs cross lipid membranes mainly (a) by
passive diffusional transfer and (b) carrier-
mediated transfer
The main factor t/ determines the rate of
passive diffusional transfer across membranes
is a drugs lipid solubility. Molecular weight is
a less important factor.
The movement of drug molecules
across cellular barriers (2)
With weak acids or bases only the unionised
forms can diffuse across lipid membrane; this
gives rise to pH partition.
pH partition means t/ weak acids tend to
accumulate in compartments of relatively high
pH, whereas weak bases do the reverse.(ion
trapping phenomenon)
Carrier-mediated transport is important for
some drugs t/ are chemically related to
endogenous substances.
Passive diffusional transfer
Lipid solubility
pH & ionization
Not selective, no energy required,
not saturable, cannot be inhibited
pH partition & ion trapping
Most drugs across cell membrane
by this transfer.
Carrier-mediated Transport(CMT)
Carrier molecule: a protein which binds molecules or ions, and
releases them on the other side of the membrane.
CMT may operate without energy by facilitating the process of
transfer in the direction of its electrochemical gradient and the
mechanism is called facilitated diffusion. Eg.the transfer of
glucose across a muscle cell membrane mediated by GLUT4.
CMT can also occur against an electrochemical gradient and is
called active transport. Eg.: sodium pumps, Na-Ca exchange.
CMT shows the characteristic of saturation, and can be inhibited
competitively by a second ligand that binds the carrier.
Intravenous administration (i.v)
Absorption circumvented w/ potentially immediate
effects. Suitable for large volume & for irritating
substances.
Valuable for emergency use
Permits titration of dosage
Usually required for high-molecular weight protein
and peptide drugs
Increased risk of adverse effects
The solution must be injected slowly as a rule
Not suitable for oily solutions or poorly soluble
substances.
Subcutaneous administration (s.c)
Absorption is prompt, from aqueous
solution, slow and sustained from
repository preparations.
Suitable for poorly soluble
suspensions and for instillation of
slow-release implants
Not suitable for large volumes
Possible pain or necrosis from
irritating substances.
Intramuscular administration (i.m.)
Absorption is prompt from aqueous
solution, slow and sustained from
repository preparations.
Suitable for moderate volumes, oily
vehicles, and some irritating substances.
Precluded during anticoagulant therapy,
and may interfere w/ interpretation of
certain diagnostic tests (e.g.creatine
kinase)
Oral/Enteral administration
Absorption is variable, depends on many
factors
Most common method of drug adminis-
tration.It is also the safest,most conve-
nient, and most economical.
Disadvantages include limitation of
absorption of some drugs because of their
physical characteristics (eg.water
solubility), it also requires patient
compliance
Bioavailability is potentially erratic and
incomplete.
Drug absorption and bioavailability
Drugs w/ low lipid solubility are poorly absorbed from the
gut.
A few drugs (eg.levodopa) are absorbed by CMT.
Absorption from the gut depends on: -GI motility, -GI pH,
particle size, -physicochemical interaction with gut
contents (eg. Ca and tetracycline antibiotics)
Bioavailability is the fraction of an ingested dose of a
drug that gains acces to the systemic circulation. It may
be low because absorption is incomplete, or because the
drug is metabolised in the gut wall or liver before reaching
the systemic circulation.
Bioequivalence implies that if one formulation of a drug
is substituted for another no clinical untoward
consequences will ensue.
Methods for delaying absorption
Addition of adrenaline (epinephrine)
to a local anesthetic
slow-release form : procaine-
penicillin,medroxyprogesterone
acetate, testosterone propionat,
flufenazine decanoate
Insulin zinc suspensions
Subcutaneous implantation of solid
pellets
Drug distribution (V
d
)
V
d
: the volume of plasma that would contain the
total body content of the drug at a concentration
equal to that in the plasma.
Lipid insoluble drugs :confined to plasma and the
interstitial fluids; most do not enter the brain .
Lipid-soluble drugs reach all compartments, and
may accumulate in fat.
For drugs that accumulate outside the plasma
compartment (eg. in fat, or being bound to tissues)
V
d
may exceed total body volume.
Drug metabolism
Phase I reactions:oxidation,reduction & hydrolysis.
These usually form more reactive products,sometimes
pharmacologically active, toxic or carcinogenic. Phase I
oftenly involve cytochrome P450 enzymes.
Phase II reactions : conjugation (eg.glucuronidation) of
a reactive group (often inserted during phase I) and
form inactive and readily excretable products.
Some conjugated products are excreted via bile, are
reactivated in the intestine and then reabsorbed.
Induction of enzymes by other drugs and chemicals
can greatly accelerate hepatic drug metabolism.
Some drugs show rapid first-pass hepatic
metabolism, and thus poor oral bioavailability.
Inhibition of P450
Ketoconazole (an antifungal) which
forms a complex with CYP3A4,
causes a non-competitive inhibition
with a risk of a fatal cardiac
arrhythmia if the drug is given
concomitantly with terfenadine (an
antihistamine).
Induction of P450
Enzyme inducers: ethanol,rifampicin,
carbamazepine,increase the activity of
microsomal oxidase and conjugating
systems when administered repeatedly
Glomerular filtration
Drugs w/ MW <20,000 can cross
the glomerular filter, but plasma
albumin (MW 68,000) cannot.
If a drugs is highly bound to plasma
albumin (eg. Warfarin 98% bound),
its concentration in glomerular
filtrate is very low (only 2%
warfarin).
Tubular secretion
20% of renal plasma flow is filtered through the
glomerulus, leaving 80% of the delivered drug to pass
on to the peritubular capillaries of the proximal tubule.
Here drug molecules are transferred to the tubular
lumen by 2 independent carrier systems.One of these
transport acidic drugs, while the other handles organic
bases.
These active transport can transport drug molecules
against an electrochemical gradient and can, therefore
, reduce the plasma concentration nearly to zero. Since
80% of the drug delivered to the kidney is presented to
the carrier, tubular secretion is potentially the most
effective mechanism of renal drug elimination, even
when most of the drug is bound to plasma protein (e.g.
penicillin)
Diffusion across the renal tubule
As the glomerular filtrate traverses the
tubule, water is reabsorbed, so that the
volume of urine only about 1% of the
filtrate.
High-lipid soluble drugs are excreted
slowly,while polar &low lipid soluble drugs
remain in the tubule & its concentration in
the urine is 100 times >than in plasma.
The ion-trapping effect :a basic drug is
more rapidly excreted in an acid urine,
because the low pH within the tubule
favours ionization and thus inhibits
reabsorption.
Biliary excretion and enterohepatic
circulation
Liver cells transfer various substances, including
drugs, from plasma to bile by means of transport
systems similar to those of the renal tubule and
which involve P-glycoprotein.
Drug conjugates (particularly glucoronides) are
concentrated in the bile and delivered to the
intestine where the glucuronide is usually
hydrolysed, releasing active drug once more. Free
drugs can then be reabsorbed and the cycle
repeated (enterohepatic circulation).
Examples :morphine, ethinylestradiol, and
rifampicin.
Effect of variation in rate of absorption
Absorption rate constant , k
abs
, is
directly proportional to the amount
of drug which is still unabsorbed
Area under the curve (AUC) is
directly proportional to the total
amount of drug that enters the
plasma.
Oral Bioavailability = AUC
oral
/ AUC
iv
Intravenous bioavailability = 100%
Saturation kinetics
E.g. Ethanol, phenytoin, salicylate
The rate of disappearance of ethanol
from the plasma is constant at about 4
mmol/L per hour irrespective of its
plasma concentration.
Also oftenly termed as zero-order
kinetics
The rate of drug metabolism by hepatic
enzymes reaches a maximum at low
plasma concentration.
References and Further Reading
Brunton,L.L.; et al.(2006). Goodman &
Gilmans The Pharmacological Basis of
Therapeutics, 11
th
Ed.,McGraw-Hill
Medical Publishing Division, USA.
Katzung,B.G.(2007).Basic&Clinical
Pharmacology,10
th
Ed., McGraw-Hill,USA.
Rang & Dale (2003). Pharmacology, 5
th
Ed.,Churchill Livingstone, London, UK.
Staf Pengajar Dep.Farmakologi FK Unsri
(2008). Kumpulan Kuliah Farmakologi,
Edisi 2, EGC,Jakarta.
You might also like
- Laporan GadungDocument7 pagesLaporan GadungIzzarIzzarNo ratings yet
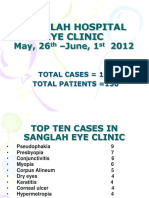
- Sanglah Hospital Operating Theater: Total Operations: 7Document7 pagesSanglah Hospital Operating Theater: Total Operations: 7IzzarIzzarNo ratings yet
- SanglahDocument13 pagesSanglahIzzarIzzarNo ratings yet
- Emergency Activity 9-13 Agustus 2010Document4 pagesEmergency Activity 9-13 Agustus 2010IzzarIzzarNo ratings yet
- OK Sanglah 9 - 14 JuneDocument7 pagesOK Sanglah 9 - 14 JuneIzzarIzzarNo ratings yet
- Emergency Activity June 9 - June 14 2012Document4 pagesEmergency Activity June 9 - June 14 2012IzzarIzzarNo ratings yet
- Sanjiwani Hospital Eye Clinic ReportDocument15 pagesSanjiwani Hospital Eye Clinic ReportIzzarIzzarNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Physical Fitness TestDocument8 pagesPhysical Fitness Testalaskador03No ratings yet
- Babinski and Other Pyramidal Reflexes Without VideosDocument12 pagesBabinski and Other Pyramidal Reflexes Without VideosMaurizio SeverinoNo ratings yet
- Team Performance ModelDocument17 pagesTeam Performance ModelAdewumi Samson Segun100% (1)
- Patient Confidentiality Part BDocument6 pagesPatient Confidentiality Part BSojiNo ratings yet
- Ujjwala Saga PDFDocument84 pagesUjjwala Saga PDFRishi ModiNo ratings yet
- Allopurinol: Gouty Nephropathy and Renal DialysisDocument3 pagesAllopurinol: Gouty Nephropathy and Renal DialysisAnonymous G26HIUtzVNo ratings yet
- Disobsession - FRANCISCO C. XAVIER, WALDO VIEIRADocument94 pagesDisobsession - FRANCISCO C. XAVIER, WALDO VIEIRASpiritism USA100% (3)
- Good Governance IndexDocument112 pagesGood Governance IndexWilliam ObengNo ratings yet
- User Manual: Listening To LifeDocument12 pagesUser Manual: Listening To LifeVitor FilipeNo ratings yet
- Get ShreddedDocument17 pagesGet ShreddedSlevin_KNo ratings yet
- BICOM Treatment of Chronic Fatigue and FibromyalgiaCFS ReportDocument15 pagesBICOM Treatment of Chronic Fatigue and FibromyalgiaCFS ReportAnahata Fraydon100% (1)
- Clinical Features of GingivitisDocument26 pagesClinical Features of GingivitisVanissa KarisNo ratings yet
- Udall, JN Et Al (1984) The Tolerance and Nutritional ValueDocument8 pagesUdall, JN Et Al (1984) The Tolerance and Nutritional ValueDavid WilsonNo ratings yet
- OSHA Standard For Fixed Ladders SummaryDocument12 pagesOSHA Standard For Fixed Ladders SummarysesabcdNo ratings yet
- Manual de Servicio Ventilador Bear Cub 750psvDocument64 pagesManual de Servicio Ventilador Bear Cub 750psvVladimir BorjaNo ratings yet
- Timetable Theory-August 2023Document22 pagesTimetable Theory-August 2023SueNo ratings yet
- Krav Maga To Empower KidsDocument7 pagesKrav Maga To Empower KidshectorhugoarNo ratings yet
- Kinesiotape en DisfoniaDocument5 pagesKinesiotape en DisfoniaingridspulerNo ratings yet
- Essential workout guideDocument31 pagesEssential workout guidejo nemesisNo ratings yet
- SPECIAL WORKSHOP ANNOUNCEMENT-with Keshe NotesDocument4 pagesSPECIAL WORKSHOP ANNOUNCEMENT-with Keshe NotesAhmad AriesandyNo ratings yet
- Burket's Oral Medicine 13th Ed Michael GlickDocument1,139 pagesBurket's Oral Medicine 13th Ed Michael GlickMahima GoodwaniNo ratings yet
- TG 6 Refractive ErrorDocument11 pagesTG 6 Refractive ErrorNovi AdriNo ratings yet
- Incident Report PortfolioDocument2 pagesIncident Report Portfolioapi-397923551No ratings yet
- Intelligent Dosing of RonozymeDocument25 pagesIntelligent Dosing of RonozymeRaymundus Genty Laras100% (1)
- Carrillo & Associates, Inc: Rosa Antonia Carrillo, MSODDocument3 pagesCarrillo & Associates, Inc: Rosa Antonia Carrillo, MSODalberto1954No ratings yet
- Kriya Sharir Syllabus 1st Year BamsDocument5 pagesKriya Sharir Syllabus 1st Year BamsHArshil KumArNo ratings yet
- Family Welfare Programme in IndiaDocument25 pagesFamily Welfare Programme in IndiaTirumalesha DadigeNo ratings yet
- 2011 Fyi Report DocumentDocument110 pages2011 Fyi Report DocumentSmart Horizons Lifetime Training SolutionsNo ratings yet
- 6 - ADKAR Reinforcement Ebook PDFDocument14 pages6 - ADKAR Reinforcement Ebook PDFHenrique NarcisoNo ratings yet
- VW50180 en 2000-07-01Document3 pagesVW50180 en 2000-07-01Bruno BrasseurNo ratings yet